Abstract
Background
Although recommendations to prevent COVID-19 healthcare-associated infections (HAIs) have been proposed, data on their effectivity are currently limited.
Objective
The aim was to evaluate the effectivity of a program of control and prevention of COVID-19 in an academic general hospital in Spain.
Methods
We captured the number of COVID-19 cases and the type of contact that occurred in hospitalized patients and healthcare personnel (HCP). To evaluate the impact of the continuous use of a surgical mask among HCP, the number of patients with COVID-19 HAIs and accumulated incidence of HCP with COVID-19 was compared between the preintervention and intervention periods.
Results
Two hundred fifty-two patients with COVID-19 have been admitted to the hospital. Seven of them had an HAI origin (6 in the preintervention period and 1 in the intervention period). One hundred forty-two HCP were infected with SARS-CoV-2. Of them, 22 (15.5%) were attributed to healthcare (2 in the emergency department and none in the critical care departments), and 120 (84.5%) were attributed to social relations in the workplace or during their non–work-related personal interactions. The accumulated incidence during the preintervention period was 22.3 for every 1000 HCP and 8.2 for every 1000 HCP during the intervention period. The relative risk was 0.37 (95% confidence interval, 0.25 to 0.55) and the attributable risk was −0.014 (95% confidence interval, −0.020 to −0.009).
Conclusions
A program of control and prevention of HAIs complemented with the recommendation for the continuous use of a surgical mask in the workplace and social environments of HCP effectively decreased the risk of COVID-19 HAIs in admitted patients and HCP.
Key Words: COVID-19, control and prevention program, effectivity, healthcare personnel, surgical mask, healthcare-associated infection
The COVID-19 pandemic caused by SARS-CoV-2 comprises globally at least 11,125,245 confirmed cases and 528,204 deaths.1 In Europe, up until July 5, 2020, 2,774,221 cases have been diagnosed,1 of which 250,545 were reported in Spain alone. Spain is currently the third country in Europe with most confirmed cases of COVID-19.2 Healthcare personnel (HCP) are at high risk of infection and transmission of COVID-19.3 In China and Italy, up to 10% of the cases occurred among HCP.4,5 In Spain, until May 11, 40,961 cases of infected HCP have been reported.6
The healthcare system, already facing an unprecedented challenge, could be further destabilized if the numbers of HCP are unable to meet the demand of patients requiring care.7 To protect patients and HCP, measures to prevent the spread of infections within healthcare institutions must be prioritized.8 In this setting, COVID-19 outbreaks can occur because of several mechanisms: transmission from HCP to patients, transmission from patients to HCP, and transmission among HCP.8 As recognized by the World Health Organization (WHO), institutions should establish programs for the control and prevention (PC&P) of healthcare-associated infections (HAIs).9 The PC&P have already been proven to be beneficial in the context of other respiratory infections, such as influenza10–13 and other SARS-related diseases.14,15
Although recommendations to prevent COVID-19 HAIs have been proposed and discussed,8 most of the evidence for these recommendations are based on our knowledge on their effect over other disease causative agents.10–16 Data on the effectivity of these measures to specifically prevent COVID-19 HAIs are currently very limited.17,18
On January 9, the Infectious Disease Board of the Alicante University General Hospital (AUGH) was informed that a cluster of cases with pneumonia of unknown etiology was being reported in Wuhan.19 This notification allowed for the early planning of a PC&P of COVID-19 (Table 1).
TABLE 1.
Program for the Control and Prevention of COVID-19 HAIs Implemented in 2020, AUGH, Spain
| Specific Measures | Target Population | Epidemiologic Chain Intervention | Implementation Date | Implementation Area |
|---|---|---|---|---|
| Respiratory hygiene measures | Patients with respiratory infection symptoms: fever, cough, and/or breathing difficulties | Infection source: patients | Annually since 2015—during the flu season | Emergency department triage |
| Expanded droplet and contact precautions*† | HCP assisting patients with suspicion of a respiratory infection | Mode of transmission: patients to HCP | Routine | Areas established for the care of patients with suspicion of acute respiratory infection‡ |
| Expanded droplet and contact precautions with eye protection† | HCP caring for patients with confirmed COVID-19 | Mode of transmission: patients to HCP | Since February 1, 2020, (included) for the care of patients with COVID-19 infection | Areas established for the care of patients with confirmed COVID-19‡ |
| SA: limitation of the free circulation. | All the people in Spain | Infection source: patients, visitors, and HCP | Since March 15, 202010 | All the population covered by the AUGH Health Department |
| Continuous use of a surgical mask§ | All HCP | Infection source: asymptomatic HCP to patients, other HCP, or visitors Mode of transmission: asymptomatic HCP, patients, or visitors to HCP |
Since March 19, 2020 | During its time at the workplace and in all social and family environments |
| Restricted visitor policy∥ | Admitted patient visitors | Infection source: asymptomatic visitors | Since March 23, 2020 (included) | All the hospital |
*Implemented until the microbiological results indicate the necessity to follow standard or more specific isolation precautions.
†Different specific recommendations for low- and high-risk activities where aerosols are generated. When performing aerosol-generating procedures, a well-fitted respirator (N-95/FFP2/FFP3) is used: endotracheal intubation, open suctioning, manual ventilation before intubation, noninvasive positive pressure ventilation, tracheotomy, cardiopulmonary resuscitation bronchoscopy, and high-frequency oscillatory ventilation.
‡These areas: the emergency department, medicine wards, and intensive care unit.
§Recommendation for the continuous use of a surgical mask every time you are going to be less than 1 meter of a patient, in the relationship with other HCP and your cohabitants, and during other the rest of social interactions.
∥Except for pediatric, dependent, or patients at the end of life.
On March 11, the WHO proclaimed that the COVID-19 outbreak had reached the level of pandemic. The state of alarm (SA) was declared on March 14 by the Spanish Government, and the following measures were established: restrictions on the movement of people (people were only allowed outside in public to buy food, pharmaceuticals, or essential goods or to address essential work and circumstances) and the temporary closure of schools, nonessential commercial activity, and hospitality venues.
On March 19, the Infectious Disease Board of the AUGH took the decision to recommend the continuous use of a surgical mask by all HCP. The surgical mask, also known as a medical face mask, is a medical device that covers the mouth, nose, and chin and provides protection against infections transmitted by droplets. Requirements for medical masks are defined in EN (14683:2019). This decision was taken based on the data from the COVID-19 Epidemiological Surveillance System in the institution. This allowed to detect the following: (1) HAI cases in patients admitted for other pathologies, (2) infection cases on HCP due to nonprotected contacts with patients on which there was no suspicion of infection, and (3) that the main source of infection in HCP with COVID-19 was the nonprotected contacts in social interactions with other HCP or outside the working environment. This was endorsed on March 31 by the European Centre for Disease Prevention and Control when they suggested that the use of surgical mask among the HCP could diminish disease transmission in healthcare environments.6 This strategy was supported by the confirmation that SARS-CoV-2 was transmitted through respiratory droplets20 and the growing evidence showing that asymptomatic carriers could be infectious in this phase.21
In the context of a high level of uncertainty regarding the supply of personal protective equipment (PPE), we proposed to evaluate the global effectivity of the PC&P of COVID-19 at the AUGH and, specifically, the impact of the continuous use of a surgical mask by all HCP in the institution.
METHODS
Hospital Characteristics
This observational study was performed in Spain, at the AUGH. It is the main institution of a health department, along with 12 primary care centers. The AUGH is an academic general hospital with more than 850 beds, including 34 in the medical intensive care unit and 18 in the surgical intensive care unit. The health department employs approximately 3900 HCP.
Surveillance Period
We evaluated the overall effectivity of the PC&P of COVID-19 HAIs (Table 1) and specifically the impact of 2 strategies: the SA and the continuous use of surgical masks by HCP. To evaluate the 2 strategies, the accumulated incidence (AI) of COVID-19 cases of the SA preintervention (10-day period) was compared with that of the SA intervention period (also a 10-day period).
To define these periods, the average COVID-1922 incubation period was identified as 6 days. The SA was declared on Saturday, March 14, and came into effect on Monday, March 16. As such, the SA preintervention case period was defined as 10 days before the SA measures were effective (from March 12 to March 21, 2020) and the SA intervention case period as the 10 days after (from March 22 to March 31, 2020).
The recommended use of surgical masks by all HCP in the healthcare department was established on March 19, 2020, and came into effect on March 20, 2020. With this in mind, the mask SA preintervention case period was defined from March 16 to March 25 and the mask SA intervention case period was defined from March 26 to April 4, 2020.
Case Definition
Patients with confirmed diagnosis of COVID-19 were included. They are defined as having respiratory tract infection symptoms (e.g., fever, cough, and breathing difficulties), a positive microbiological test for SARS-CoV-2 by polymerase chain reaction of a respiratory tract sample, and time since admission of less than 24 hours.23 The infection was classified as follows: (1) an HAI, if the symptoms started after day 6 of admission (taking into account that the mean incubation period is 6 days22) or (2) community onset, when the symptoms started before admission or on the first 6 days after admission.
Criteria for COVID-19 in HCP included symptoms of respiratory tract infections and positive microbiological test as defined previously. The type of infection was classified according to the exposure in the previous 14 days after the initiation of their symptoms: (1) healthcare associated, when a HCP has been exposed to a patient with suspected or confirmed COVID-19,23 this could occur during healthcare duties, carrying diagnostic tests, or during therapeutic procedures; (2) workplace relationships between HCP (one-on-one interactions, professional meetings, breaktime interactions, etc.), in which one of the HCP had been declared as a suspected or confirmed COVID-19 case; and (3) other relationships (when a HCP has been exposed outside the workplace to any suspected or confirmed COVID-19 case). In case of exposure to 2 types of different types of cases, the index case is considered to be the one involved in a nonprotected interaction. In case of contact with a suspicious or confirmed COVID-19 case with adequate PPE and a social contact with asymptomatic people, the index case will be considered the infected patient, even if the interaction occurred using protective equipment.
Data Collection
Electronic clinical records and direct interviews were used to collect all the epidemiological data. Data were collected from 2 sources, the COVID-19 Cases Surveillance System (all confirmed cases undergo an epidemiologic survey). The survey includes the following: age, sex, occupation, date when the first symptoms occurred, risk factors for COVID-19 infection in the 14 days before the initiation of the symptoms, microbiological confirmation date, and hospital admission date. The other data source is the HCP Contact Evaluation Program: all HCP who have been in contact with confirmed COVID-19 cases are identified and evaluated. We collect the following data: age, sex, professional category, type of contact (close, sporadic, or undetermined), contact reason (healthcare associated, workplace relationships, or other relationships), type of contact (protected or nonprotected), and the HCP’s department.
A close contact is considered when a person has been within a 2-meter distance for at least 15 minutes with a confirmed or suspected case23; a sporadic contact is considered if not; and an undetermined contact is considered when no exposure to a person with symptoms could be identified. The contact is considered nonprotected when it does not comply with the precautions established in Table 1.
Statistical Analysis
The number of patients admitted for COVID-19 is described based on the day of admission (except for HAI cases where the first day of symptoms is shown). The number, the evolution by day, and the type of contact with a confirmed COVID-19 index case among HCP are described. To describe the characteristics, the absolute and relative frequencies of each of the variable’s categories were used. To study whether there were any differences, the χ2 test was performed. To evaluate the impact of the declaration of the SA and the continuous use of a surgical mask among HCP, the number of patients with COVID-19 HAIs between the preintervention and SA intervention periods was compared. To compare the incidence of COVID-19 cases among HCP, the AI between both periods (exposition and SA preintervention periods) was calculated, and to quantify the magnitude of the association and the impact, relative risk (RR) and attributable risk (AR) were calculated using the following equations with their respective 95% confidence intervals (95% CIs):
The preventable fraction (PF) was also calculated:
The level of statistical significance used was P < 0.05. All these calculations were made with IBM-SPSS V.25.0. This study was approved by the institution’s research ethics committee (Reference Number: 200127). The committee determined that written approval from all participants in the study was not required.
RESULTS
Since the first case was reported on March 5, until this report was submitted on April 5, 2020, 252 patients with confirmed COVID-19 have been admitted to the AUGH after the daily pattern shown in Figure 1A. Of them, 7 were classified as having an HAI origin (diagnosis during preintervention or intervention period and beginning of symptoms after the admission in our institution on days 11, 12, 13, 17, 25, 37, and 58). Six of them showed symptoms during the preintervention period, and one of them shows symptoms in the intervention period with respect to the continuous use of a surgical mask among HCP.
FIGURE 1.
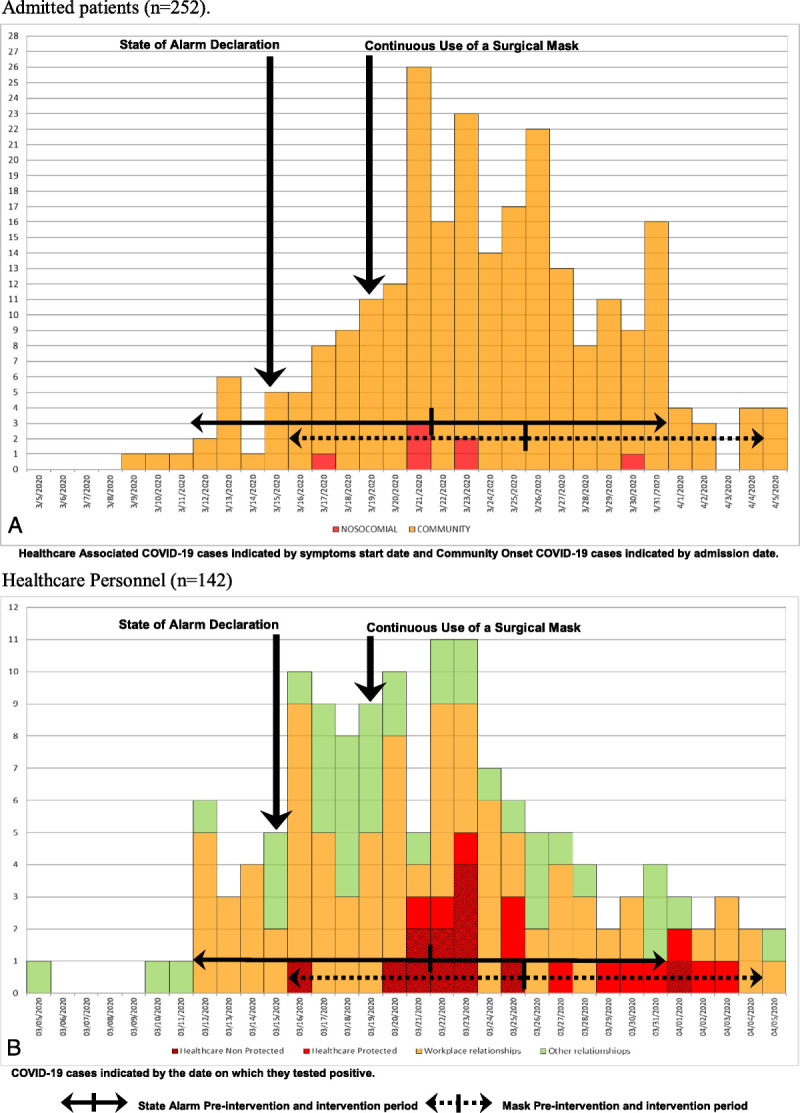
Daily incidence of confirmed COVID-19 cases in the AUGH, Alicante, Spain, March 5 to April 5, 2020.
From March 5 to April 5, 2020, 1918 HCP were evaluated. Of these, 677 presented symptoms. The total number of HCP with confirmed COVID-19 was 142, 14 were admitted to the hospital, 2 needed to be admitted to the intensive care unit, and none of them died. The daily incidence of confirmed cases can be observed in Figure 1B. Of them, 22 (15.5%) confirmed infections among HCP were healthcare associated, 81 (57.0%) were related to workplace relationships, and 39 (27.5%) were related to other relationships outside the workplace. The demographic characteristics of HCP diagnosed with COVID-19 organized by the type of risk exposure are shown in Table 2. Of the 22 HCP to which the infection was attributed to patient care, 11 (50%) were explained by a nonprotected contact. Of those, 10 went ill in the preintervention period to the implementation of the use of a surgical mask and 1 in the intervention period. There were 2 HCP with healthcare-associated COVID-19 in the emergency department and none in critical care departments.
TABLE 2.
Characteristics of HCP Diagnosed With COVID-19 According to the Type of Contact With the Suspected Index Case, March 5 to April 5, 2020 (n = 142), AUGH, Spain
| Total (n = 142) | Healthcare (n = 22) | Workplace Social Interactions (n = 81) | Other Social Interactions (n = 39) | P* | |||||
|---|---|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | % | n | ||
| Age group | 0.154 | ||||||||
| <30 | 13.4 | 19 | 9.1 | 2 | 16.0 | 13 | 10.3 | 4 | |
| 30–44 | 38.7 | 55 | 22.7 | 5 | 43.2 | 35 | 38.5 | 15 | |
| 45–59 | 33.8 | 48 | 36.4 | 8 | 30.9 | 25 | 38.5 | 15 | |
| ≥60 | 14.1 | 20 | 31.8 | 7 | 9.9 | 8 | 12.8 | 5 | |
| Sex | 0.295 | ||||||||
| Male | 24.6 | 35 | 31.8 | 7 | 19.8 | 16 | 30.8 | 12 | |
| Female | 75.4 | 107 | 68.2 | 15 | 80.2 | 65 | 69.2 | 27 | |
| Professional category | 0.845 | ||||||||
| Physicians | 38.7 | 55 | 40.9 | 9 | 34.6 | 28 | 46.2 | 18 | |
| Nurses | 28.9 | 40 | 27.3 | 6 | 33.3 | 27 | 20.5 | 8 | |
| Nurse’s aide/technician | 19.0 | 27 | 18.2 | 4 | 19.8 | 16 | 17.9 | 7 | |
| Others | 13.4 | 19 | 13.6 | 3 | 12.3 | 10 | 15.4 | 6 | |
| Contact type | 0.097 | ||||||||
| Close | 76.1 | 108 | 54.5 | 12 | 81.5 | 66 | 76.9 | 30 | |
| Occasional | 16.9 | 24 | 31.8 | 7 | 14.8 | 12 | 12.8 | 5 | |
| Unknown | 7.0 | 10 | 13.6 | 3 | 3.7 | 3 | 10.3 | 4 | |
| Department | Not evaluated | ||||||||
| Emergency department† | 2.8 | 4 | 9.1 | 2 | 0.0 | 0 | 5.1 | 2 | |
| MICU‡ | 0.7 | 1 | 0.0 | 0 | 0.0 | 0 | 2.6 | 1 | |
| SICU + surgical area§ | 19.7 | 28 | 0.0 | 0 | 30.9 | 25 | 7.7 | 3 | |
| Medical floors | 27.5 | 39 | 36.4 | 8 | 23.5 | 19 | 30.8 | 12 | |
| Surgical floors | 8.5 | 12 | 13.6 | 3 | 9.9 | 8 | 2.6 | 1 | |
| Pediatric areas∥ | 2.1 | 3 | 4.5 | 1 | 2.5 | 2 | 0.0 | 0 | |
| Central services¶ | 21.1 | 30 | 4.5 | 1 | 19.8 | 16 | 33.3 | 13 | |
| PCC# | 12.7 | 18 | 22.7 | 5 | 12.3 | 10 | 7.7 | 3 | |
| Other areas** | 4.9 | 7 | 9.1 | 2 | 1.2 | 1 | 10.3 | 4 | |
*Statistical significance.
†Adult emergency department.
‡Medical intensive care unit.
§Surgical intensive care unit and surgical area.
∥Pediatric areas: emergency department, medical intensive care unit and surgical intensive care unit.
¶Central services: radiology, laboratory medicine, pathology, and preventive medicine.
#Primary care centers.
**Other areas: management and administration, laundry, cleaning, and maintenance.
The AI of COVID-19 among HCP during preintervention period until the declaration of the SA was 17.9 for every 1000 HCP, and the risk of COVID-19 during intervention period was 14.6 for every 1000 HCP. The RR of exposed versus nonexposed was 0.81 (0.57 to 1.15), and the AR was −0.003 (−0.009 to −0.002) as shown in Table 3.
TABLE 3.
Accumulated Incidence of COVID-19 Cases by 1000 HCP in the Preintervention and Intervention Periods Regarding the Declaration of the SA, March 12–31, 2020 (n = 127), and the Order for Continuous Use of a Surgical Mask, March 16 to April 4, 2020 (n = 119), AUGH, Spain
| Intervention Period Incidence | Preintervention Period Incidence | RR (95% CI) | AR (95% CI) | |||
|---|---|---|---|---|---|---|
| ‰ | n | ‰ | n | |||
| SA | ||||||
| Total (n = 127) | 14.6 | 57 | 17.9 | 70 | 0.81 (0.57 to 1.15) | −0.003 (−0.009 to −0.002) |
| Healthcare associated (n = 18) | 3.6 | 14 | 1.0 | 4 | 3.53 (1.15 to 10.62) | 0.002 (0.000 to 0.005) |
| Workplace social interactions (n = 75) | 7.7 | 30 | 11.5 | 45 | 0.67 (0.42 to 1.06) | −0.004 (−0.008 to 0.000) |
| Other social interactions (n = 34) | 3.3 | 13 | 5.3 | 21 | 0.62 (0.31 to 1.23) | −0.002 (−0.005 to 0.000) |
| Continuous use of surgical masks | ||||||
| Total (n = 119) | 8.2 | 32 | 22.3 | 87 | 0.37 (0.25 to 0.55) | −0.014 (−0.020 to −0.009) |
| Healthcare associated (n = 22) | 1.8 | 7 | 3.8 | 15 | 0.47 (0.20 to 1.14) | −0.002 (−0.004 to 0.000) |
| Workplace social interactions (n = 66) | 4.4 | 17 | 12.6 | 49 | 0.35 (0.20 to 0.60) | −0.008 (−0.012 to −0.004) |
| Other social interactions (n = 31) | 2.1 | 8 | 5.9 | 23 | 0.35 (0.16 to 0.78) | −0.004 (−0.007 to −0.001) |
The AI of COVID-19 among HCP during the preintervention period until the implementation of the continuous use of a surgical mask was 22.3 for every 1000 HCP, and the risk during the intervention period was 8.2 for every 1000 HCP. The RR was 0.37 (0.25 to 0.55) and the AR was −0.014 (−0.020 to −0.009). Derived from the previous data, the PF among the exposed was 63.0%.
The evolution of the weekly incidence of confirmed COVID-19 cases among admitted patients and the incidence of COVID-19 cases among HCP in epidemiologic weeks 11, 12, 13, and 14 is shown in Figure 2.
FIGURE 2.
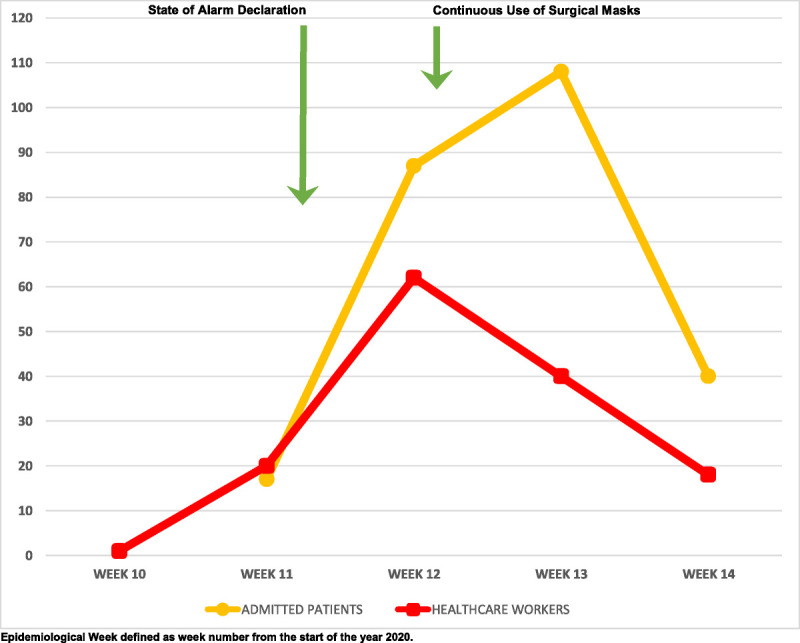
Incidence by epidemiologic week of COVID-19 cases in admitted patients (n = 252) and HCP (n = 142) in the AUGH, Alicante, Spain, March to April 2020.
DISCUSSION
The evidence presented here demonstrates the positive effects of the PC&P of COVID-19 HAIs in hospitalized patients and HCP; the data specifically demonstrate that the use of masks not only reduces the spread of SARS-CoV-2 from symptomatic persons but also reduces the transmission rate from asymptomatic persons. The implications of this outcome are significant for the prevention of COVID-19 among healthcare workers and vulnerable patient populations treated in the healthcare system. It is necessary to constantly re-evaluate the control and prevention strategies associated with patient care and implement any necessary changes to avoid HAIs and thus protect both patients and HCP.
The results obtained show that the recommendations are having a positive impact on the incidence of COVID-19 on hospitalized patients and HCP. Both collectives were given priority when making polymerase chain reaction tests for SARS-CoV-2 acknowledging the limited availability of trial tests during this period for 2 reasons: on hospitalized patients, it was required to understand the etiology of the disease to implement the optimal treatment and to establish the expanded isolation precautions measures; and for symptomatic HCP (independently of the severity of the disease), being able to establish home isolation and to control their reincorporation into the workforce with guaranteed safety. As previously proposed in China,4 the transmission derived from patient care does not seem to be the main mechanism of transmission among HCP, where most cases were tracked back to confirmed case in the household and most of the cases where attributed to community transmission.
Interpreting the data of affected HCP requires careful analysis. The number of affected HCP was 142 up until April 5, which constitutes 3.6% of the 3900 workers. These data contain both HAIs and the community-acquired infections classified as “other relationships.” On top of this, the personnel considered as HCP entails not only the clinical-based personnel (mainly physicians, nurses, and medical assistants) but also any other worker in the institution who may not be involved in direct patient care.
When the decision that all HCP had to continuously wear a surgical mask was made, there was a high level of uncertainty regarding the supply of PPE. That same day, the hospital had in stores 12,000 masks for approximately 3900 staff. Then, there was an actual shortfall of PPE, but this situation required to tightly control the distribution of equipment. At the same time, the staff was educated in the fair usage of the PPE as well as the best practice shown for low- and high-risk maneuvers (aerosol-generating procedures). Several outcomes were taken into consideration when making this decision. On one side, the potential shortfall of equipment was due to overprotection of personnel. On the other hand, there was the risk of not being able to control the source of infection represented by asymptomatic personnel working as usual who could transmit the infection. The decision was based on data from the Epidemiological Surveillance System of COVID-19 cases in the center. Then, it was evident that there was sustained SARS-CoV-2 transmission within the community and hospital environment and that more aggressive PC&P measures were required. If the use of surgical mask by all HCP had not been implemented, the reduction in incidence from March 25 (Figs. 1A, B) would not have taken place. This is due to the close environment nature of the hospital, and nonprotected contact between patients (potentially asymptomatic carriers) and HCP and among HCP (potentially asymptomatic carriers) themselves would have continued until the whole HCP and patient cohort would have been infected.
This study highlights that 2 specific measures, in the context of a holistic PC&P, effectively reduce the incidence of COVID-19 cases. On one hand, the declaration of SA that limited the free movement of people in the country was effective in reducing the number of cases, in line with what previous studies have suggested.24 On the other hand, the continuous use of a surgical mask among HCP was also effective in reducing the number of COVID-19 cases. This shed some light into the debate of their universal use in a healthcare setting; in addition, it raises the question on the potential effectivity of these measures in controlling the COVID-19 infection among the general population. However, this answer is outside of the scope of this article. Nevertheless, this underlines the importance of the rational use of mask in a time of limited resources.25 Results also advocate for the creation in times of stability of a strategic stock of masks ready to be used during the recurring respiratory-based infectious diseases. As in these potential pandemics, this measure in conjunction of a PC&P has been proven successful.10–16 The results show that the implementation of a surgical mask for all HCP resulted in a reduction of affected professionals but do not necessarily imply that this would be down exclusively to this measure. We believe that it is necessary to highlight that the use of surgical masks by all HCP on its own is not enough and could be detrimental if it does not go in hand with all the PC&P measures26 aimed to break the chain of infection (Table 1).
In a time of constant changes, it is critical to also cater for a collective of professionals24 and authorities25 that constantly question the suitability of the measures taken. This behavior can lead to personnel not following the PC&P and thus increases the risk of patients and HCP. As the WHO states, it is important to observe, analyze, and inform the interested parties with data on infections relating to patient care to prevent against them.27 In this regard, we believe that it is of utmost importance to include these strategies as part of continued medical education so that professionals are familiarized with these concepts before the initiation of the crisis. In addition, we believe that their support with the adequate resources allows for the monitorization of the potential outbreaks and ensures the implementation of rapid responses for its control.
Limitations of This Study
This study has various limitations: (1) the unknown level of compliance and correct usage of the PPE; (2) the possible overestimation of HCP cases linked to patient care, as the nonprotected asymptomatic contacts during social interactions in the workplace are not considered as a potential source; (3) the possible overestimation of patient cases linked to healthcare assistance, as cases are considered HAIs even when a protected contact happened in the workplace and an unprotected asymptomatic contact occurred outside; and (4) the observational nature of this study, which is based on data from the typical working conditions of a disease surveillance system.
CONCLUSIONS
Each center should undertake a detailed epidemiological analysis of COVID-19 cases among hospitalized patients and HCP to determine which of them can be considered HAIs. Close monitoring of COVID-19 cases by PC&P of HAIs, allows for the deployment of targeted approaches suitable to the specific needs and resources of each center in a timely and effective manner. Specifically, healthcare institutions should widely adopt the use of surgical masks by HCP to limit COVID-19 transmission mechanism and to eliminate HCP as a source of COVID-19 infection.
ACKNOWLEDGMENTS
The authors thank Álvaro Sánchez Vela for his contribution in the editing and critical review of the manuscript.
Footnotes
The authors disclose no conflict of interest.
Contributor Information
Paula Gras-Valentí, Email: paulagrasvalenti@gmail.com.
Juan G. Mora-Muriel, Email: juanguau@hotmail.com.
Pablo Chico-Sánchez, Email: chico_pab@gva.es.
Natividad Algado-Sellés, Email: natialgado@gmail.com.
Victor M. Soler-Molina, Email: soler30@gmail.com.
María Hernández-Maldonado, Email: hernandez_marmal@gva.es.
Ana S. Lameiras-Azevedo, Email: lameiras_ana@gva.es.
Natali J. Jiménez Sepúlveda, Email: jimenez_natsep@gva.es.
Isel L. Gómez Sotero, Email: gomez_ise@gva.es.
César O. Villanueva-Ruiz, Email: villanueva_ces@gva.es.
Julio Barrenengoa-Sañudo, Email: barrenengoa_jul@gva.es.
Marina Fuster-Pérez, Email: fuster_marper@gva.es.
Sandra Cánovas-Jávega, Email: canovas_san@gva.es.
Patricia Cerezo-Milan, Email: cerezo_pat@gva.es.
Miranda Monerris-Palmer, Email: monerris_mir@gva.es.
Pere Llorens-Soriano, Email: llorens_ped@gva.es.
Esperanza Merino-Lucas, Email: merino_luc@gva.es.
Juan C. Rodríguez-Diaz, Email: rodriguez_juadia@gva.es.
Joan Gil-Carbonell, Email: joangilcarbonell@gmail.com.
Rosario Sánchez-Martínez, Email: sanchez_rosmar@gva.es.
Rogelio Pastor-Cesteros, Email: rogeliopastorcesteros@gmail.com.
Luis Mena-Esquivias, Email: mena_lui@gva.es.
Maria Galiana-Ivars, Email: mgivars@gmail.com.
Francisco A. Jaime-Sánchez, Email: franciscoangelj@yahoo.es.
Cesar Margarit-Ferri, Email: cmargarit69@gmail.com.
Javier Gonzalez-deDios, Email: javiergonzalezdedios@gmail.com.
German Lloret, Email: lloret_ger@gva.es.
Miguel A. García-Alonso, Email: garcia_manalo@gva.es.
Pablo Sánchez-Vela, Email: sanchezp@mskcc.org.
REFERENCES
- 1.WHO . Coronavirus disease 2019 (COVID-19) situation report – 167, 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200705-covid-19-sitrep-167.pdf?sfvrsn=17e7e3df_4. Accessed July 26, 2020.
- 2.Ministerio de Sanidad, Direccion General de Salud Publica, Calidad e Innovación . Actualización no 156. Enfermedad por el coronavirus (COVID-19). 05.07.2020, 2020. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Actualizacion_156_COVID-19.pdf. Accessed July 26, 2020.
- 3.Zhou P Huang Z Xiao Y, et al. Protecting Chinese healthcare workers while combating the 2019 novel coronavirus. Infect Control Hosp Epidemiol. 2020;41:745–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mission WCJ. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19), 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdfwww.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed July 26, 2020.
- 5.Sanità TC-TfotDoIDatISISd . Integrated surveillance of COVID-19 in Italy (Ordinanza n. 640), 2020. Available at: https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_29marzo%20ENG.pdf. Accessed July 26, 2020.
- 6.Red Nacional de Vigilancia Epidemiológica . Análisis de los casos de COVID-19 en personal sanitario notificados a la RENAVE hasta el 10 de mayo en España. Available at: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/COVID-19%20en%20personal%20sanitario%2029%20de%20mayo%20de%202020.pdf. Accessed July 26, 2020.
- 7.Armocida B Formenti B Ussai S, et al. The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020;5:e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ECDC . Infection prevention and control and preparedness for COVID-19 in healthcare settings. Stockholm: ECDC, 2020. Available at: https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings. Accessed July 26, 2020. [Google Scholar]
- 9.WHO . Guidelines on core components of infection prevention and control programs at the national and acute health care facility level: WHO; 2016. Available at: https://www.who.int/gpsc/ipc-components-guidelines/en/. Accessed July 26, 2020. [PubMed]
- 10.Cheng VC Tai JW Wong LM, et al. Prevention of nosocomial transmission of swine-origin pandemic influenza virus A/H1N1 by infection control bundle. J Hosp Infect. 2010;74:271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong VW, Cowling BJ, Aiello AE. Hand hygiene and risk of influenza virus infections in the community: a systematic review and meta-analysis. Epidemiol Infect. 2014;142:922–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cowling BJ Chan KH Fang VJ, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151:437–446. [DOI] [PubMed] [Google Scholar]
- 13.Suess T Remschmidt C Schink SB, et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: results from a cluster randomised trial; Berlin, Germany, 2009-2011. BMC Infect Dis. 2012;12:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu J Xu F Zhou W, et al. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerg Infect Dis. 2004;10:210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yen MY Lin YE Lee CH, et al. Taiwan’s traffic control bundle and the elimination of nosocomial severe acute respiratory syndrome among healthcare workers. J Hosp Infect. 2011;77:332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leung NHL Chu DKW Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng VCC Wong SC Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong SCY Kwong RT Wu TC, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO . Pneumonia of unknown cause—China, 2020. Available at: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. Accessed July 11, 2020.
- 20.WHO . Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations, 2020. Available at: https://https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendationswww.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed July 11, 2020.
- 21.Wei WE Li Z Chiew CJ, et al. Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:411–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill. 2020;25:2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.IdSC III. PROCEDIMIENTO DE ACTUACIÓN FRENTE A CASOS DE INFECCIÓN POR EL NUEVO CORONAVIRUS (SARS-CoV-2), 2020. Available at: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Procedimiento_COVID_19.pdf. Accessed July 11, 2020.
- 24.Prem K Liu Y Russell TW, et al. Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group . The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feng S Shen C Xia N, et al. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8:434–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klompas M Morris CA Sinclair J, et al. Universal masking in hospitals in the Covid-19 era. N Engl J Med. 2020;382:e63. [DOI] [PubMed] [Google Scholar]
- 27.WHO . 2019 novel coronavirus (2019-nCoV): strategic preparedness and response plan, 2020. Available at: https://https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdfamongst.who.int/docs/default-source/coronaviruse/srp-04022020.pdf. Accessed July 11, 2020.


