Abstract
BACKGROUND
High school (HS) sport-related concussions (SRCs) remain a public health concern in the United States.
OBJECTIVE
To describe patterns in symptom prevalence, symptom resolution time (SRT), and return-to-play time (RTP) for SRCs sustained in 20 HS sports during the 2013/14-2017/18 academic years.
METHODS
A convenience sample of athletic trainers reported concussion information to the HS RIOTM surveillance system. Symptom prevalence, average number of symptoms, and SRT and RTP distributions were examined and compared by event type (practice, competition), injury mechanism (person contact, nonperson contact), sex, and contact level (collision, high contact, and low contact) with chi-square tests and Wilcoxon rank-sum tests.
RESULTS
Among all SRCs (n = 9542), headache (94.5%), dizziness (73.8%), and difficulty concentrating (56.0%) were commonly reported symptoms. On average, 4.7 ± 2.4 symptoms were reported per SRC. Overall, 51.3% had symptoms resolve in <7 d, yet only 7.9% had RTP < 7 d. Differential prevalence of amnesia was seen between practice and competition-related SRCs (8.8% vs 13.0%; P < .001); nonperson-contact and person-contact SRCs (9.3% vs 12.7%; P < .001); and female and male SRCs in low-contact sports (5.8% vs 17.5%; P < .001). Differential prevalence of loss of consciousness was seen between practice and game-related SRCs (1.3% vs 3.2%; P < .001); and female and male SRCs in high contact sports (1.2% vs 4.0%; P < .001). Differential longer SRT (>21 d) was seen between new and recurrent SRCs (9.4% vs 15.9%; P < .001).
CONCLUSION
Headache was the most commonly reported symptom. Notable group differences in the prevalence of amnesia, loss of consciousness, and SRT may be associated with more severe SRCs, warranting further attention.
Keywords: Concussion, Symptoms, Head injuries, Youth sports
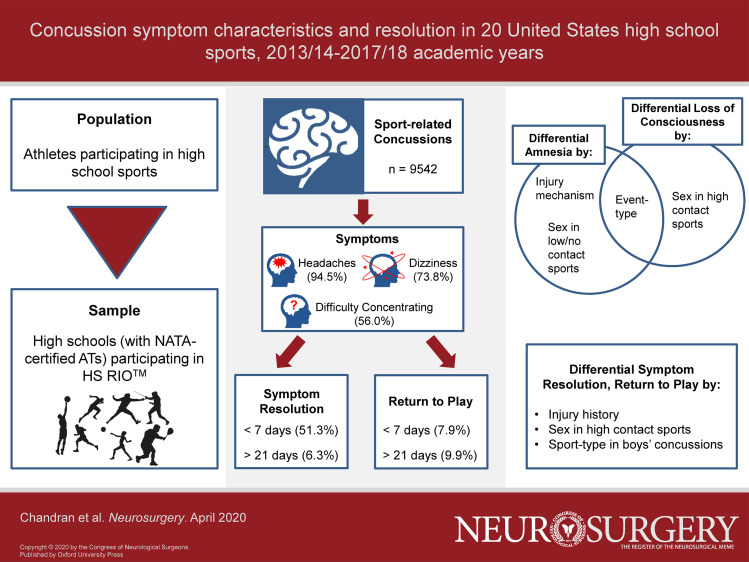
Graphical Abstract
Graphical Abstract.
ABBREVIATIONS
- AT
athletic trainer
- HS
high school
- IQR
interquartile range
- LOC
loss of consciousness
- NATA
National Athletic Trainers’ Association
- RTP
return-to-play time
- SRC
sport-related concussion
- SRT
symptom resolution time
Sport-related concussions (SRCs) are a major public health concern.1-4 Particular attention has focused on concussions in youth and high school (HS) athlete populations.5,6 Existing research has aided in developing safety policies and preventive measures,7 though routine epidemiological updates are needed to capture the evolving scope of SRCs in HS sports.8 With that said, there exist few large-sample studies examining concussion symptom prevalence, and outcomes such as symptom resolution times (SRT) and return-to-play times (RTP) following concussions, in this population.
Symptom presentations are important considerations as SRCs are diagnosed through symptom endorsement, and initial symptom burden has been previously linked with injury prognosis and recovery.9,10 Athletes can present with a wide array of complaints,11-16 and emerging evidence points to sex- and event-type differences in symptom presentation,17 as well as to sex differences in symptom severity at onset among HS athletes.18 Moreover, sex differences in SRT have also been reported in youth athletes.6,19 Accordingly, the purpose of this descriptive epidemiological study was to describe patterns in symptom prevalence, SRT, and RTP for HS SRCs during the 2013/14-2017/18 academic years. It was hypothesized that differential symptom prevalence and outcomes would be observed by event type and injury mechanism, as well as between female and male SRCs.
METHODS
Data originated from the National High School Sports-Related Injury Surveillance System (HS RIOTM), an internet-based sports injury surveillance system, during the 2013/14-2017/18 academic years. The study was deemed exempt by the Colorado Multiple Institutional Review Board, Aurora, Colorado, as it utilized surveillance data. The methodology of the surveillance system has been described previously, and is summarized below.20
Sample
HSs with at least one National Athletic Trainers’ Association (NATA)-affiliated certified athletic trainer (AT) were invited to participate in this study, and data were collected in 2 panels. Participating schools were classified into 8 strata based on school characteristics. In the first panel, a random sample of 100 schools were recruited annually from these strata, to report data for nine sports (boys’ football, wrestling, soccer, basketball, and baseball; girls’ volleyball, soccer, basketball, and softball). Those schools not selected in the national sample were still able to participate as part of an expanded convenience sample (ie, the second data collection panel). This expanded sample included schools recruited annually that reported data for any of the 9 previously mentioned sports as well as additional sports that were less commonly sponsored (eg, boys’ cross country, ice hockey, lacrosse, swimming, and track and field; girls’ cross country, field hockey, lacrosse, swimming, and track and field; and cheerleading). ATs at schools selected for the nationally representative sample were also able to contribute data to the second panel by reporting for sports other than the 9 original sports of interest. Data from both panels were utilized in this study.
The 20 sports included in this study were as follows: boys’ football, wrestling, soccer, basketball, baseball, cross country, ice hockey, lacrosse, swimming/diving, and track and field, girls’ volleyball, soccer, basketball, softball, cross country, field hockey, lacrosse, swimming/diving, and track and field; and cheerleading.
Data Collection and Definitions
ATs at participating schools reported injury data to HS RIOTM on a weekly basis. For each SRC, ATs completed a report that included information on injury characteristics such as event type (practice, competition), injury mechanism, and whether the injury was recurrent (determined in some cases based on self-reported SRCs from previous seasons or non-HS sport settings). ATs also provided data on clinically observed/assessed symptom presentation, SRT (days between when the athlete first reported concussion symptoms and when all assessed concussion symptoms had dissipated), and RTP (number of days between injury and return to activity at a level that would allow competition). SRT and RTP were both recorded as ordinal variables within HS RIOTM (see Table 1 for detailed definitions). ATs were able to update the reported information throughout the course of the reporting period of a season.
TABLE 1.
Definitions of Main Outcomes of Interest, Accompanied by Estimated Measures of Interest, Comparisons Made, and Statistical Analyses Used for Examinations of Concussions Among High School Athletes in 20 Sports, 2013/14-2017/18 Academic Years
| Outcome | Definition | Measure of interest |
|---|---|---|
| Symptom presentation | A list of symptoms (amnesia, difficulty concentrating, confusion/disorientation, dizziness/unsteadiness, headache, hyperexcitability, irritability, loss of consciousness, nausea, tinnitus, light sensitivity, noise sensitivity, foggy, and potential ‘other’ symptoms) were evaluated for all SRCs (dichotomized as yes/no). Multiple symptoms could be reported for each SRC. As clinicians were presented with the aforementioned subset of options for symptom selection, all reported concussions were retained for analysis even if no associated symptoms were reported | Calculated as the proportion of SRCs reported with a given symptom among all SRCs |
| Symptom count | Overall count of symptoms reported (from 15 symptoms options) | Discrete symptom count |
| Symptom Resolution Time (SRT) | The time between when the athlete first reported concussion symptoms and when all assessed concussion symptoms had dissipated (ordinally recorded within HS RIOTM) | Proportions of SRCs with values of SRT <7 and >21 d (SRT was recorded as less than 15 min, 15-29 min, 30-59 min, 1-11 h, 12-23 h, 1-2 d, 3-6 d, 7-9 d, 10-21 d, 22 d or more, within the surveillance system. Categories were combined for analysis) |
| Return-to-play time (RTP) | Defined as the number of days between injury and return to activity at a level that would allow competition (ordinally recorded within HS RIOTM) | Proportions of SRCs with values of RTP <7 and >21 d. For RTP >21 d, SRCs that resulted in a medical disqualification (for the season or career) were included. (RTP was recorded as less than 1, 1-2, 3-6, 7-9, 10-21, 22 d or more, medical disqualification for season, medical disqualification for career, athlete chooses not to continue, athlete released from team (no medical disqualification), season ended before athlete returned to activity, within the surveillance system. Categories were combined for analysis) |
A reportable SRC (1) resulted from participation in a school-sanctioned practice or competition, and (2) required medical attention by a trained medical professional (such as an AT or physician). All diagnosed SRCs were reported regardless of time loss following the injury. Injuries occurring outside of practice and competition (such as during weight training) were excluded.
Concussion consensus statements were available to medical staff during the entirety of the study period,11,21 and diagnoses were made by the onsite trained medical professional. ATs are trained to detect and diagnose injuries; previous research has found ATs to have high agreement with physicians in diagnosing injuries and to provide higher-quality data compared with nonmedically trained individuals such as coaches or players.22,23 Internal validity checks of data collected within HS RIOTM have routinely found sensitivity, specificity, and positive predictive and negative predictive values above 90%.24
Statistical Analysis
Data were analyzed to examine the proportion of SRCs presenting with each reported symptom, the number of concussion symptoms reported per SRC, and distributions of SRT and RTP. For SRT and RTP, we were interested in the proportions of SRCs with SRT <7 and >21 d, and the proportions of SRCs with RTP <7 and >21 d (this included SRCs that resulted in a season or career medical disqualification). The cut-points for SRT and RTP were established based on the recorded categorizations of both variables within HS RIOTM (Table 1), as well as clinical indications of atypical recovery times in this population.
After descriptive analyses of all outcomes, we compared SRCs by event type (practice vs competition- including cheer performance); injury mechanism (person contact (contact with another person) vs nonperson contact (surface or equipment contact)); and injury history (new vs recurrent). We also examined sex and contact level concurrently through stratum-specific analyses that compared boys vs girls SRCs in high contact sports (ie, boys’ soccer, basketball; girls’ soccer, basketball, field hockey, lacrosse); boys vs girls SRCs in low/no contact sports (ie, boys’ baseball, swimming, cross country, track; and girls’ volleyball, softball, swimming, cross country, track); and collision sports (ie, boy's football, wrestling, ice hockey, lacrosse) vs all other sports SRCs, among boys. We excluded SRCs with other/missing mechanisms (n = 424) and missing injury history (n = 79).
Chi-square tests (or Fisher's exact tests when χ2 assumptions were violated) were used to examine differential symptom prevalence, and differential proportions of SRT and RTP outcomes. Wilcoxon rank-sum tests were used to examine differential symptom counts. Statistical significance was evaluated at the 0.001 level, accounting for the multiple comparisons involved. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
Overall, 9542 SRCs were reported during the 2013/14-2017/18 academic years. On average, 4.7 ± 2.4 (median = 4.0, interquartile range [IQR] = 3.0-6.0) symptoms were reported per SRC. The most commonly reported symptoms were headache (94.5%), dizziness (73.8%), difficulty concentrating (56.0%), and light sensitivity (52.6%) (Table 2). These symptoms were also commonly reported within each of the 20 sports examined (see Table, Supplemental Digital Content, for further details).
TABLE 2.
Comparisons of Concussion Symptom Prevalence, Symptom Resolution Time, Return-to-Play Time, and Symptom Counts Between Practice and Competition-Related SRCs Among High School Athletes in 20 Sports, 2013/14-2017/18 Academic Years
| Event | ||||
|---|---|---|---|---|
| Symptom prevalence, % (95% CI) | Overall | Practice | Competition | P valuea |
| Amnesia | 11.5 (10.8,12.1) | 8.8 (7.8,9.7) | 13.0 (12.1,13.8) | <.001 |
| Confusion/disorientation | 37.2 (36.2,38.1) | 36.4 (34.8,38.0) | 37.6 (36.4,38.8) | .25 |
| Difficulty concentrating | 56.0 (55.0,57.0) | 56.0 (54.3,57.6) | 56.0 (54.7, 57.2) | .98 |
| Dizziness/unsteadiness | 73.8 (72.9,74.7) | 74.8 (73.3,76.2) | 73.2 (72.1,74.3) | .10 |
| Drowsiness | 32.7 (31.8,33.7) | 34.6 (33.0,36.2) | 31.6 (30.5,32.8) | .003 |
| Foggy | 19.2 (33.8,35.7) | 18.6 (17.3,19.9) | 19.5 (18.5,20.5) | .27 |
| Headache | 94.5 (94.1,95.0) | 95.4 (94.7,96.1) | 94.0 (93.4,94.6) | .003 |
| Hyperexcitability | 2.1 (1.8,2.4) | 1.5 (1.1,1.9) | 2.5 (2.1,2.9) | .001 |
| Irritability | 13.3 (12.6,14.0) | 13.3 (12.1,14.4) | 13.3 (12.5,14.2) | .92 |
| Light sensitivity | 52.6 (51.6,53.6) | 52.9 (51.3,54.6) | 52.5 (51.2,53.7) | .66 |
| Loss of consciousness | 2.5 (2.2,2.8) | 1.3 (0.9,1.7) | 3.2 (2.7,3.6) | <.001 |
| Nausea | 28.3 (27.4,29.2) | 29.8 (28.2,31.3) | 27.4 (26.3,28.6) | .02 |
| Noise sensitivity | 34.7 (33.8,35.7) | 33.4 (31.8,34.9) | 35.5 (34.3,36.7) | .03 |
| Tinnitus | 6.4 (5.9,6.9) | 6.6 (5.8,7.5) | 6.3 (5.7,6.9) | .51 |
| Other | 8.3 (7.7,8.8) | 8.1 (7.2,9.0) | 8.4 (7.7,9.1) | .64 |
| Symptom resolution time, % | ||||
| <7 d | 51.3 (50.3,52.3) | 49.8 (48.2,51.5) | 52.1 (50.8,53.3) | .04 |
| >21 d | 6.3 (5.8,6.8) | 7.1 (6.2,7.9) | 5.8 (5.2,6.4) | .02 |
| Return-to-play time, % | ||||
| <7 d | 7.9 (7.4,8.4) | 7.3 (6.4,8.1) | 8.2 (7.6,8.9) | .09 |
| >21 db | 9.9 (9.3,10.5) | 11.5 (10.5,12.6) | 9.0 (8.2,9.7) | <.001 |
| Symptom mean | 4.7 | 4.7 | 4.7 | |
| ±SD | 2.4 | 2.3 | 2.4 | |
| Median | 4.0 | 4.0 | 4.0 | .72 |
| IQR | 3.0-6.0 | 3.0-6.0 | 3.0-6.0 | |
| Total (n) | 9542 | 3463 | 6079 | n/a |
aP-values correspond to χ2 tests (or Fisher's exact tests when χ2 assumptions were violated) for comparing (practice vs competition) symptom prevalences and proportions for symptom resolution time and return-to-play time; and Wilcoxon rank-sum tests comparing symptom counts.
bIncludes SRCs resulting in medical disqualification for the season or career.
Note: Statistical significance was evaluated at the .001 level, accounting for the multiple comparisons involved. Also, as clinicians were presented with a subset of options for symptom selection, all reported concussions were retained for analysis even if no associated symptoms were reported.
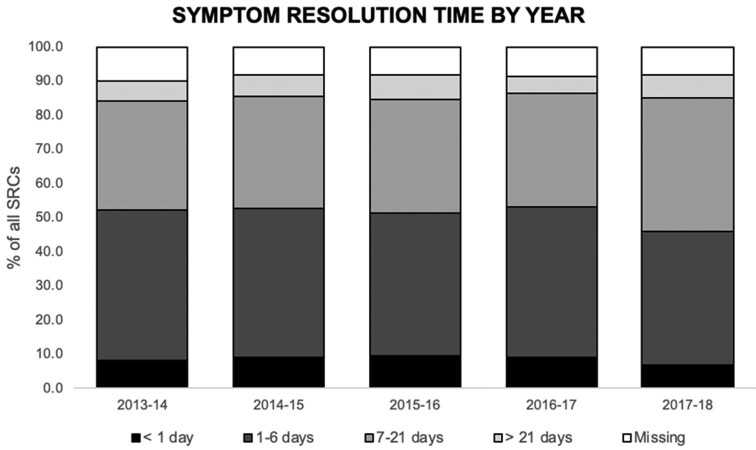
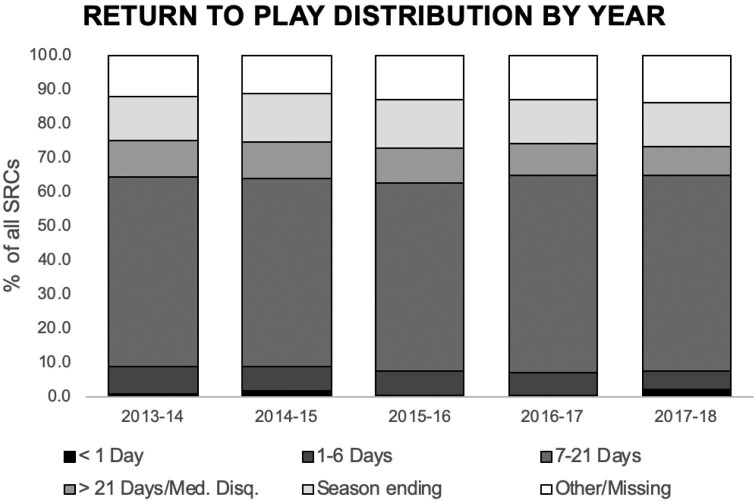
Most SRCs had SRT < 7 d (51.3%); 6.3% had SRT > 21 d. Conversely, 7.9% of SRCs had RTP < 7 d; 9.9% had RTP > 21 d. We observed no temporal trends in SRT and RTP, and distributions of both remained relatively constant over the study period (Figures 1 and 2).
FIGURE 1.
Temporal trends in concussion symptom resolution time among high school athletes.
FIGURE 2.
Temporal trends in return-to-play time following SRCs among high school athletes. Season ending refers to cases when the competitive season ended before the athlete returned to activity.
Comparisons by event type, injury mechanism, concussion history, and sex/contact level are only presented below if findings were statistically significant (details are presented in Tables 2-5).
TABLE 5.
Comparisons of Concussion Symptom Prevalence, Symptom Resolution Time, Return-to-Play Time, and Symptom Counts by Sex, and Sport Type Among High School Athletes in 20 Sports, 2013/14-2017/18 Academic Years
| High contact sportsa | Low/no contact sportsb | Boysc | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Symptom prevalence, % (95% CI) | Girls | Boys | P valued | Girls | Boys | P valued | Collision | All other | P valued |
| Amnesia | 8.5 (7.2,9.7) | 11.1 (9.0,13.1) | .03 | 5.8 (4.1,7.5) | 17.5 (12.0,23.0) | <.001 | 13.4 (12.5,14.4) | 12.1 (10.2,14.1) | .25 |
| Confusion/disorientation | 32.6 (30.6,34.7) | 34.7 (31.6,37.8) | .26 | 33.6 (30.1,37.0) | 42.6 (35.5,49.8) | .02 | 40.0 (38.6,41.3) | 36.1 (33.2,38.9) | .02 |
| Difficulty concentrating | 54.6 (52.4,56.7) | 53.4 (50.2,56.7) | .57 | 53.9 (50.3,57.5) | 53.0 (45.8,60.2) | .82 | 57.8 (56.4,59.1) | 53.4 (50.4,56.3) | .008 |
| Dizziness/unsteadiness | 74.0 (72.1,75.9) | 72.7 (69.8,75.6) | .45 | 77.4 (74.4,80.5) | 78.7 (72.8,84.6) | .72 | 73.0 (71.8,74.2) | 73.7 (71.1,76.3) | .66 |
| Drowsiness | 34.5 (32.5,36.6) | 32.9 (29.8,35.9) | .37 | 34.5 (31.1,38.0) | 30.1 (23.4,36.7) | .25 | 32.1 (30.9,33.4) | 32.4 (29.6,35.2) | .88 |
| Foggy | 18.2 (16.5,19.9) | 18.5 (15.9,21.0) | .87 | 19.0 (16.1,21.8) | 18.6 (12.9,24.2) | .90 | 19.6 (18.5,20.7) | 18.5 (16.2,20.8) | .41 |
| Headache | 96.2 (95.4,97.1) | 95.5 (94.1,96.8) | .34 | 96.7 (95.4,98.0) | 95.1 (91.9,98.2) | .30 | 93.3 (92.7,94.0) | 95.4 (94.2,96.6) | .01 |
| Hyperexcitability | 1.6 (1.1,2.2) | 1.8 (0.9,2.6) | .81 | 1.0 (0.3,1.7) | 2.7 (0.4,5.1) | .07 | 2.5 (2.1,2.9) | 1.9 (1.1,2.8) | .25 |
| Irritability | 15.3 (13.7,16.9) | 9.7 (7.8,11.7) | <.001 | 11.8 (9.5,14.2) | 13.1 (8.2,18.0) | .63 | 13.5 (12.6,14.5) | 10.3 (8.5,12.1) | .004 |
| Light sensitivity | 56.3 (54.1,58.5) | 52.1 (48.8,55.4) | .04 | 52.8 (49.2,56.4) | 53.0 (45.8,60.2) | .96 | 51.2 (49.8,52.5) | 52.3 (49.3,55.2) | .52 |
| Loss of consciousness | 1.2 (0.7,1.7) | 4.0 (2.7,5.3) | <.001 | 1.2 (0.4,2.0) | 5.5 (2.2,8.8) | .002 | 3.0 (2.5,3.4) | 4.2 (3.0,5.4) | .03 |
| Nausea | 28.8 (26.8,30.8) | 23.5 (20.7,26.2) | .003 | 29.8 (26.5,33.2) | 29.5 (22.9,36.1) | .93 | 28.7 (27.4,29.9) | 24.5 (21.9,27.0) | .005 |
| Noise sensitivity | 38.0 (35.9,40.2) | 35.7 (32.6,38.9) | .24 | 40.3 (36.7,43.9) | 29.5 (22.9,36.1) | .007 | 32.7 (31.4,33.9) | 34.7 (31.9,37.5) | .20 |
| Tinnitus | 5.6 (4.6,6.6) | 7.2 (5.5,8.9) | .10 | 5.0 (3.4,6.5) | 8.7 (4.7,12.8) | .05 | 6.9 (6.2,7.6) | 7.5 (5.9,9.0) | .50 |
| Other | 7.7 (6.5,8.9) | 8.1 (6.3,9.9) | .74 | 8.4 (6.4,10.4) | 7.7 (3.8,11.5) | .75 | 8.5 (7.8,9.3) | 8.0 (6.4,9.6) | .57 |
| Symptom resolution time, % | |||||||||
| <7 d | 47.7 (45.6,49.9) | 58.5 (55.3,61.7) | <.001 | 50.9 (47.3,54.5) | 62.3 (55.3,69.3) | .006 | 51.7 (50.4,53.1) | 59.2 (56.2,62.1) | <.001 |
| >21 d | 7.3 (6.1,8.4) | 3.7 (2.4,4.9) | <.001 | 8.4 (6.4,10.4) | 2.7 (0.4,5.1) | .008 | 6.1 (5.4,6.7) | 3.5 (2.4,4.6) | <.001 |
| Return-to-play time, % | |||||||||
| <7 d | 7.8 (6.6,8.9) | 9.9 (7.9,11.8) | .06 | 9.5 (7.4,11.6) | 7.7 (3.8,11.5) | .44 | 7.6 (6.9,8.3) | 9.5 (7.7,11.2) | .03 |
| >21 de | 9.8 (8.5,11.1) | 6.0 (4.4,7.5) | <.001 | 10.5 (8.2,12.7) | 7.7 (3.8,11.5) | .26 | 10.2 (9.4,11.0) | 6.3 (4.8,7.7) | <.001 |
| Symptom mean | 4.7 | 4.6 | 4.7 | 4.9 | 4.8 | 4.6 | |||
| ±SD | 2.4 | 2.3 | 2.3 | 2.4 | 2.4 | 2.4 | |||
| Median | 4.0 | 4.0 | .11 | 4.0 | 5.0 | .58 | 5.0 | 4.0 | .07 |
| IQR | 3.0-6.0 | 3.0-6.0 | 3.0-6.0 | 3.0-7.0 | 3.0-6.0 | 3.0-6.0 | |||
| Total (n) | 2009 | 904 | n/a | 727 | 183 | n/a | 5279 | 1087 | n/a |
aCorresponds to comparisons of male and female SRCs in high contact sports (high contact: boys/girls—soccer and basketball, girls—field hockey and lacrosse).
bCorresponds to comparisons of male and female SRCs in low/no contact sports (low contact: boys/girls—swim & dive, track & field, and cross country, boys—baseball, girls—volleyball and softball).
cCorresponds to comparisons between SRCs in collision (collision: boys—football, wrestling, ice hockey, and lacrosse) and noncollision sports among boys.
dP-values correspond to χ2 tests (or Fisher's exact tests when χ2 assumptions were violated) for comparing symptom prevalences and proportions for symptom resolution time and return-to-play time; and Wilcoxon rank-sum tests comparing symptom counts.
eIncludes SRCs resulting in medical disqualification for the season or career.
Note: Statistical significance was evaluated at the 0.001 level, accounting for the multiple comparisons involved. Also, as clinicians were presented with a subset of options for symptom selection, all reported concussions were retained for analysis even if no associated symptoms were reported.
Symptoms by Event Type
Most SRCs were reported during competition (63.7%) (Table 2). Compared to practice-related SRCs, higher proportions of competition-related SRCs had reported amnesia (13.0% vs 8.8%; P < .001) and loss of consciousness (LOC) (3.2% vs 1.3%; P < .001). Also, the proportion of SRCs resulting in RTP > 21 d was higher in practice than that in competitions (11.5% vs 9.0%; P < .001).
Symptoms by Injury Mechanism
Among all SRCs reported, most were due to person-contact mechanisms (62.2%) (Table 3). Compared to nonperson-contact SRCs, a higher proportion of person-contact SRCs had reported amnesia (12.7% vs 9.3%; P < .001) and confusion/disorientation (38.7% vs 34.4%; P < .001).
TABLE 3.
Comparisons of Concussion Symptom Prevalence, Symptom Resolution Time, Return-to-Play Time, and Symptom Counts Between Nonperson-Contact and Person-Contact-Resultant SRCs Among High School Athletes in 20 Sports, 2013/14-2017/18 Academic Years
| Mechanism | |||
|---|---|---|---|
| Symptom prevalence, % (95% CI) | Nonperson contacta | Person contact | P valueb |
| Amnesia | 9.3 (8.3,10.3) | 12.7 (11.9,13.6) | <.001 |
| Confusion/disorientation | 34.4 (32.7,36.0) | 38.7 (37.5,40.0) | <.001 |
| Difficulty concentrating | 54.1 (52.4,55.9) | 57.0 (55.7,58.2) | .009 |
| Dizziness/unsteadiness | 74.7 (73.2,76.2) | 74.0 (72.9,75.1) | .47 |
| Drowsiness | 32.8 (31.2,34.5) | 32.7 (31.5,33.9) | .88 |
| Foggy | 19.6 (18.2,21.0) | 18.9 (17.9,19.9) | .39 |
| Headache | 95.4 (94.6,96.1) | 94.7 (94.2,95.3) | .18 |
| Hyperexcitability | 1.7 (1.3,2.1) | 2.4 (2.0,2.8) | .03 |
| Irritability | 13.4 (12.2,14.6) | 13.2 (12.3,14.0) | .76 |
| Light sensitivity | 53.2 (51.5,55.0) | 52.8 (51.5,54.1) | .71 |
| Loss of consciousness | 2.5 (1.9,3.0) | 2.5 (2.1,2.9) | .80 |
| Nausea | 28.6 (27.0,30.2) | 28.3 (27.1,29.4) | .72 |
| Noise sensitivity | 35.9 (34.3,37.6) | 34.1 (32.9,35.3) | .08 |
| Tinnitus | 5.6 (4.8,6.4) | 7.0 (6.3,7.6) | .01 |
| Other | 7.3 (6.4,8.2) | 8.6 (7.9,9.3) | .03 |
| Symptom resolution time, % | |||
| <7 d | 49.9 (48.2,51.7) | 52.4 (51.2,53.7) | .02 |
| >21 d | 6.7(5.8,7.5) | 5.9 (5.3,6.5) | .15 |
| Return-to-play time, % | |||
| <7 d | 8.2 (7.3,9.2) | 7.8 (7.1,8.5) | .48 |
| >21 dc | 10.2 (9.1,11.2) | 9.7 (9.0,10.5) | .50 |
| Symptom mean | 4.7 | 4.8 | |
| ±SD | 2.4 | 2.4 | |
| Median | 4.0 | 4.0 | .09 |
| IQR | 3.0-6.0 | 3.0-6.0 | |
| Total (n) | 3177 | 5941 | n/a |
aNonperson contact includes SRCs due to surface contact or equipment contact.
bP-values correspond to χ2 tests (or Fisher's exact tests when χ2 assumptions were violated) for comparing symptom prevalences and proportions for symptom resolution time and return-to-play time; and Wilcoxon rank-sum tests comparing symptom counts.
cIncludes SRCs resulting in medical disqualification for the season or career.
Note: Statistical significance was evaluated at the 0.001 level, accounting for the multiple comparisons involved. Also, as clinicians were presented with a subset of options for symptom selection, all reported concussions were retained for analysis even if no associated symptoms were reported.
Symptoms by Concussion History
Overall, 8.3% of SRCs reported were recurrent (Table 4). Compared to new SRCs, a higher proportion of recurrent SRCs had SRT > 21 d (12.0% vs 5.8%; P < .001). Similarly, a higher proportion of recurrent SRCs had RTP > 21 d (15.9% vs 9.4%; P < .001).
TABLE 4.
Comparisons of Concussion Symptom Prevalence, Symptom Resolution Time, Return-to-Play Time, and Symptom Counts Between New and Recurrent SRCs Among High School Athletes in 20 Sports, 2013/14-2017/18 Academic Years
| History | |||
|---|---|---|---|
| Symptom prevalence, % (95% CI) | Recurrent | New | P valuea |
| Amnesia | 11.6 (9.3,13.8) | 11.5 (10.8,12.2) | .95 |
| Confusion/disorientation | 36.6 (33.3,40.0) | 37.2 (36.2,38.2) | .74 |
| Difficulty concentrating | 54.1 (50.6,57.6) | 56.2 (55.2,57.3) | .25 |
| Dizziness/unsteadiness | 73.8 (70.8,76.9) | 73.9 (72.9,74.8) | .99 |
| Drowsiness | 30.9 (27.7,34.2) | 32.9 (31.9,33.9) | .26 |
| Foggy | 18.9 (16.1,21.6) | 19.2 (18.4,20.1) | .80 |
| Headache | 95.4 (93.9,96.8) | 94.5 (94.0,94.9) | .29 |
| Hyperexcitability | 1.9 (0.9,2.8) | 2.2 (1.8,2.5) | .63 |
| Irritability | 14.5 (12.0,16.9) | 13.2 (12.5,13.9) | .31 |
| Light sensitivity | 53.3 (49.9,56.8) | 52.6 (51.5,53.6) | .68 |
| Loss of consciousness | 2.3 (1.2,3.3) | 2.5 (2.2,2.8) | .66 |
| Nausea | 29.8 (26.6,33.0) | 28.1 (27.2,29.1) | .31 |
| Noise sensitivity | 36.9 (33.5,40.2) | 34.6 (33.6,35.6) | .19 |
| Tinnitus | 6.2 (4.5,7.8) | 6.4 (5.9,7.0) | .76 |
| Other | 9.3 (7.3,11.3) | 8.2 (7.6,8.8) | .27 |
| Symptom resolution time, % | |||
| <7 d | 47.4 (44.0,50.9) | 51.6 (50.6,52.7) | .02 |
| >21 d | 12.0 (9.7,14.2) | 5.8 (5.3,6.2) | <.001 |
| Return-to-play time, % | |||
| <7 d | 7.6 (5.7,9.4) | 7.9 (7.3,8.5) | .72 |
| >21 db | 15.9 (13.3,18.4) | 9.4 (8.7,10.0) | <.001 |
| Symptom mean | 4.8 | 4.7 | |
| ±SD | 2.3 | 2.4 | |
| Median | 4.0 | 4.0 | .69 |
| IQR | 3.0-6.0 | 3.0-6.0 | |
| Total (n) | 795 | 8668 | n/a |
aP-values correspond to χ2 tests (or Fisher's exact tests when χ2 assumptions were violated) for comparing symptom prevalences and proportions for symptom resolution time and return-to-play time; and Wilcoxon rank-sum tests comparing symptom counts.
bIncludes SRCs resulting in medical disqualification for the season or career.
Note: Statistical significance was evaluated at the 0.001 level, accounting for the multiple comparisons involved. Also, as clinicians were presented with a subset of options for symptom selection, all reported concussions were retained for analysis even if no associated symptoms were reported.
Symptoms by Sex and Contact Level
Most SRCs originated from boys’ collision sports (n = 5279), followed by girls’ high contact sports (n = 2009), and boys’ high contact sports (n = 904) (Table 5).
Sex Differences Among High Contact Sports
Among high contact sports, a higher proportion of female SRCs than male SRCs had reported irritability (15.3% vs 9.7%; P < .001) (Table 5); in contrast, a higher proportion of male SRCs than female SRCs had reported LOC (4.0% vs 1.2%; P < .001). Also, a higher proportion of male SRCs than female SRCs had SRT < 7 d (58.5% vs 47.7%; P < .001); in contrast, a higher proportion of female SRCs than male SRCs had SRT > 21 d (7.3% vs 3.7%; P < .001). Similarly, a higher proportion of female SRCs than male SRCs had RTP > 21 d (9.8% vs 6.0%; P < .001).
Sex Differences Among Low/No Contact Sports
Among low/no contact sports, a higher proportion of male SRCs than female SRCs had reported amnesia (17.5% vs 5.8%; P < .001) (Table 5).
Comparing Collision Sports to All Other Sports Among Boys
Compared to SRCs in collision sports, a higher proportion of SRCs in noncollision sports had SRT < 7 d (59.2% vs 51.7%; P < .001); in contrast, compared to SRCs in noncollision sports, a higher proportion of SRCs in collision sports had SRT > 21 d (6.1% vs 3.5%; P < .001). Similarly, a higher proportion of SRCs in collision sports, as compared with SRCs in noncollision sports, had RTP > 21 d (10.2% vs 6.3%; P < .001).
DISCUSSION
In this sample of HS SRCs, we observed that headaches, dizziness, and difficulty concentrating were the most commonly reported symptoms. This is consistent with the existing SRC literature in this,17,25 as well as other age cohorts.26 In half of all reported SRCs, symptoms resolved in <7 d; however, only 8% of SRCs resulted in RTP of <7 d. This potentially indicates a cautious, multifactorial approach to RTP and a clinical propensity for completing RTP protocols, even after symptoms have dissipated. Given that RTP protocols are typically initiated 5 to 7 d after symptom resolution, greater alignment between SRT and RTP would be particularly unexpected within the <7 d category. No temporal trends in RTP were seen, which may indicate stabilizing clinical practice. This may be due to the fact that by 2014 (start of the study period), every US state had adopted some legislation addressing concussion management.27 Differential symptom prevalence was most notable for amnesia and LOC, and group differences in SRT and RTP were also most often observed for the longer SRT and RTP categories. We observed statistically significant differences in the prevalence of the aforementioned symptoms by event type, injury mechanism, and sex. We observed differential proportions of longer SRT by injury history, sex, and sport type, as well as differential proportions of longer RTP by event type, injury history, sex, and sport type. Considering the potential implications of these symptoms and outcomes, the observed group differences warrant further attention and discussion.
Differential Prevalence of Amnesia and LOC
Amnesia and LOC are 2 severe SRC symptoms. They require immediate referral for further care, and have been associated with prolonged recovery.28 Therefore, it is important to closely examine the prevalence of, and group differences associated with these symptoms. We observed differential proportions of amnesia by event type (higher in competition-related SRCs), injury mechanism (higher in person-contact SRCs), and sex in low/no contact sports (higher in male SRCs). These results suggest that intrinsic factors, extrinsic factors, and inciting mechanisms are associated with the presentation of these symptoms. The prevalence of amnesia observed within male SRCs in low/no contact sports is particularly noteworthy and may suggest a differential role of injury mechanism in determining SRC presentations between sport classes. Admittedly, such inferences are limited by the nature of surveillance data. However, it is important to examine the interaction between sport type and injury mechanism in driving SRC symptom presentations in this population.
We also observed differential proportions of LOC by event type (higher in competition-related SRCs), and sex in high contact sports (higher in male SRCs). The higher prevalence of LOC in competition-related and male SRCs mirrors the results observed for amnesia. While it may be important to temper etiological inferences given the available data, the higher prevalence of one or both of these symptoms in SRCs occurring during competition, from person contact, and in male sports suggest that symptoms of greater severity may be observed more commonly in these contexts. Although significant progress has been made in mitigating practice-related concussions, the potential severity of competition-related concussions may warrant further examination. Albeit with mixed results, there already exist examples of policies implemented to restrict player contact in different sports (such as limited checking in hockey and safer tackling in football).29,30 Future interventions motivated by reducing the apparent severity of competition-related and person contact-resultant SRCs could target coaching and refereeing education in HS sports, wherein both parties can maintain high vigilance during potential player-to-player collisions. Further research into these observed patterns may be used to inform the development of such interventions.
Differential Proportions of Longer SRT
Determinants of longer SRT require careful examination considering the risk of postconcussion syndrome, where symptoms last greater than 1 mo.31,32 We observed differential proportions of longer SRT by injury history (higher in recurrent SRCs), by sex in high contact sports (higher in female SRCs), and by sport type in boys (higher in collision sport SRCs). Longer SRT following recurrent concussions in comparison with new concussions is unsurprising given the existing literature.2 While the observed sex differences are also consistent with the existing literature,33,34 the etiology of these sex differences remains to be reconciled. As lower SRC self-reporting intentions have been previously observed in male athletes,35-37 it is yet reasonable to suggest that this result is at least partially attributable to sex differences in reporting behaviors. Differences in longer SRT between collision and other sports among male SRCs may be indicative of the role of sport-specific exposures on injury prognosis. Further research on context-specific exposures is required to understand this paradigm.
Differential Proportions of Longer RTP
We observed differential proportions of longer RTP by event type (higher in practice), injury history (higher in recurrent), sex in high contact SRCs (higher in female SRCs), and sport type in boys SRCs (higher in collision sport SRCs). Akin to SRT, it is reasonable to suggest that longer RTP indicates an injury of greater severity. The differences by event type in proportions of longer RTP are noteworthy, and inconsistent with expectations considering the existing literature connecting competition-related injuries with longer RTP.38 These results indicate that while progress has been made in mitigating practice-related concussions, further monitoring and closer evaluation of SRCs in practice events may be needed. Sex differences in longer RTP following SRCs are consistent with expectations given the SRT results discussed above, as well as existing literature,39 and illustrate the need for further multifactorial examinations of RTP following concussions in order to reconcile mechanistic frameworks underpinning the observed results. In future studies, it is also important to consider the potential effects of differential reporting behaviors. Furthermore, the differences in longer RTP between collision and other sports among male SRCs may indicate that collision sports require a more cautious RTP approach, and that the relatively higher proportion of collision sport SRCs resulting in longer RTP reflect caution in clinical practice. Therefore, clinical decision making may warrant further attention in this regard.
Delving into the Explanatory Variables
These results form the basis for crafting etiological hypotheses and for future studies examining concussion etiology. We observed that mechanistic, intrinsic, and extrinsic factors were differently associated with concussion symptom presentations and outcomes. For example, sex differences in severe symptom presentations and outcomes highlight the need for examining their etiologic underpinnings. While cerebrovascular, hormonal, and musculoskeletal factors have been previously speculated to be responsible for sex differences in concussion outcomes,40-42 there is an urgent need for further research to verify these hypotheses. The higher severity of person-contact-resultant SRCs and SRCs in collision sports highlight the need to better understand the mechanisms influencing SRC presentations and outcomes. For instance, the impacts occurring in collision sports may be of greater force magnitudes, as compared with other sports. The idea that varying injury mechanisms pose differential mechanical loads is also intuitive, and may motivate further studies of head impact biomechanics in this population. While injury surveillance has been critical in identifying patterns of SRCs in large samples, the explanatory variables examined warrant further investigation.
Limitations and Related Considerations
We acknowledge several limitations to this analysis. Firstly, as only ATs with NATA affiliations contributed data into HS RIOTM, we note that the external validity of our findings is restricted. We also acknowledge the potential for misclassification of concussion due to between-clinician heterogeneity in diagnoses. We nonetheless anticipate minimal misclassification, as all diagnoses were made by trained clinicians. However, given that injury data were reported on a weekly basis, the potential for recall bias in reporting cannot be ruled out. Similarly, we acknowledge that the injury history data reported in this study are limited by the self-reported nature of this variable. We also note that surveillance mechanisms do not capture detailed data on intrinsic (athlete-specific) or mechanistic (impact location, impact force, etc) factors, which limits our ability to test etiologic hypotheses. Furthermore, as symptoms are captured dichotomously, we are also unable to discuss symptom burden. Also, as SRT and RTP are captured as ordinal variables in HS RIOTM, the precision in evaluating the time course of the injury is restricted. Given the nature of surveillance data, we are also unable to provide additional details on the RTP process, or to discuss the clinical decision-making surrounding RTP. Similarly, as SRT captured the time taken for all symptoms for a given SRC to resolve, we are unable to determine symptom-specific resolution time and identify patterns related to prolonged presentations of specific symptoms. We also note that we are unable to discuss instances where symptoms may have returned after having once resolved completely. Finally, we note that while our conservative threshold for evaluating statistical significance preserves the overall familywise error rate, we acknowledge that we resultantly are vulnerable to greater likelihoods of type II error on any given comparison. However, we maintain that our threshold helps ensure that statistically significant results observed here are also practically (or clinically) meaningful.
CONCLUSION
The most commonly observed SRC symptoms among HS athletes were headaches, dizziness, and light sensitivity. Differential symptom prevalence was most notably observed for amnesia and LOC. Differential proportions of SRC outcomes were most notably observed for SRT and RTP >21 d. In future studies, there is a need for targeted investigations of the group differences observed here.
Disclosures
We disclose the content of this report represents data collection from High School Reporting Information Online (HS RIOTM). These data were provided by Dr R. Dawn Comstock of the Colorado School of Public Health and University of Colorado School of Medicine. HS RIOTM was funded in part by the Centers for Disease Control and Prevention (grant nos. R49/CE000674-01 and R49/CE001172-01) and the National Center for Research Resources (award no. KL2 RR025754). The authors also acknowledge the research funding contributions of the NFHS, National Operating Committee on Standards for Athletic Equipment (NOCSAE), DonJoy Orthotics, and EyeBlack. The content of this report is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations.
Supplementary Material
Acknowledgments
We thank the many athletic trainers who have volunteered their time and efforts to submit data to HS RIOTM. Their efforts are greatly appreciated and have had a tremendously positive effect on the safety of high school student athletes.
Notes
A portion of the contents of this study was previously presented as a poster presentation at the 13th World Congress on Brain Injury on March 14, 2019 in Toronto, Canada.
Contributor Information
Avinash Chandran, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Matthew Gfeller Sport-Related Traumatic Brain Injury Research Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Datalys Center for Sports Injury Research and Prevention, Inc., Indianapolis, Indiana.
Zachary Y Kerr, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Matthew Gfeller Sport-Related Traumatic Brain Injury Research Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Patricia R Roby, Matthew Gfeller Sport-Related Traumatic Brain Injury Research Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Human Movement Science Curriculum, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Aliza K Nedimyer, Matthew Gfeller Sport-Related Traumatic Brain Injury Research Center, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Human Movement Science Curriculum, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Alan Arakkal, Department of Epidemiology, University of Colorado Anschutz, Aurora, Colorado.
Lauren A Pierpoint, Steadman Philippon Research Institute, Vail, Colorado.
Scott L Zuckerman, Vanderbilt Sports Concussion Center, Vanderbilt University School of Medicine, Nashville, Tennessee; Department of Neurological Surgery, Vanderbilt University School of Medicine, Nashville, Tennessee.
Neurosurgery Speaks! Audio abstracts available for this article at www.neurosurgery-online.com.
Supplemental Digital Content. Table. Symptom prevalence, symptom resolution time, return-to-play time, and symptom counts among high school athletes in 20 sports, 2013/14-2017/18 academic years.
COMMENT
Concussion management has been an evolving landscape over the past two decades. Prior to the 2001 consensus guidelines on concussion,1 systematic protocols for concussion management were rarely used,2-3 and same day or next day return to play was commonplace.4-5 Since that time, several organizations have released guidelines advocating for a symptom-free waiting period and more gradual return to play guidelines.6-9 Following the implementation of these guidelines, symptom duration, length of the symptom-free waiting period, and days to return to play increased in collegiate athletes, suggesting more conservative concussion management.10 The authors provide updated data regarding patterns in symptom prevalence, symptom resolution time, and return-to-play time for sport-related concussions across 20 high school sports during the 2013/14-2017/18 seasons.
Jaclyn B. Caccese
Newark, Delaware
REFERENCES
- 1.Aubry M, Cantu R, Dvorak J, et al.. Summary and agreement statement of the first international conference on concussion in sport, vienna 2001. The Physician and sports medicine. 2002;30(2):57-63. [DOI] [PubMed] [Google Scholar]
- 2.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. Journal of Athletic Training. 2001;36(2):145. [PMC free article] [PubMed] [Google Scholar]
- 3.Notebaert AJ, Guskiewicz KM. Current trends in athletic training practice for concussion assessment and management. Journal of Athletic Training. 2005;40(4):320. [PMC free article] [PubMed] [Google Scholar]
- 4.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643-650. [DOI] [PubMed] [Google Scholar]
- 5.Pellman EJ, Powell JW, Viano DC, et al. Concussion in professional football: epidemiological features of game injuries and review of the literature—part 3. Neurosurgery. 2004;54(1):81-96. [DOI] [PubMed] [Google Scholar]
- 6.Harmon KG, Clugston JR, Dec K, et al. American medical society for sports medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213-225. [DOI] [PubMed] [Google Scholar]
- 7.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in berlin, october 2016. Br J Sports Med. 2017;51:838-847. [DOI] [PubMed] [Google Scholar]
- 8.Register-Mihalik JK, Sarmiento K, Vander Vegt CB, Guskiewicz KM. Considerations for athletic trainers: a review of guidance on mild traumatic brain injury among children from the centers for disease control and prevention and the national athletic trainers' association. Journal of Athletic Training. 2019;54(1):12-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weissman B, Joseph M, Gronseth G, Sarmiento K, Giza CC. CDC's guideline on pediatric mild traumatic brain injury: recommendations for neurologists. Neurology: Clinical Practice. 2019;9(3):241-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCrea M, Broglio S, McAllister T, et al. Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA concussion study (1999-2001) and CARE consortium (2014-2017). Br J Sports Med. 2019: bjsport-100579. [DOI] [PubMed] [Google Scholar]
Neurosurgery Speaks (Audio Abstracts)
Listen to audio translations of this paper's abstract into select languages by choosing from one of the selections below.
REFERENCES
- 1.Bryan MA, Rowhani-Rahbar A, Comstock RD, Rivara F. Sports- and recreation-related concussions in US youth. Pediatrics. 2016;138(1):e20154635. [DOI] [PubMed] [Google Scholar]
- 2.Guskiewicz K, Mccrea M, Marshall SWet al.. Cumulative effects associated with recurrent concussion in collegiate football players the NCAA concussion study. J Am Med Assoc. 2003;290(19):2549-2555. [DOI] [PubMed] [Google Scholar]
- 3.Guskiewicz KM, Marshall SW, Bailes Jet al.. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719-726. [DOI] [PubMed] [Google Scholar]
- 4.Guskiewicz KM, Marshall SW, Bailes Jet al.. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903-909. [DOI] [PubMed] [Google Scholar]
- 5.Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among united states high school athletes in 20 sports. Am J Sports Med. 2012;40(4):747-755. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor K, Baker M, Dalton S, Dompier T, Broglio S, Kerr Z. Epidemiology of sport-related concussions in high school athletes: National Athletic Treatment, Injury and Outcomes Network (NATION), 2011-2012 through 2013-2014. J Athl Train. 2017;52(3):175-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee Green J. Legal Perspectives, Recommendations on State Concussion Laws. https://www.nfhs.org/articles/legal-perspectives-recommendations-on-state-concussion-laws/. 2014. Accessed March 3, 2019. [Google Scholar]
- 8.van Mechelen W, Hlobil H, Kemper HCG. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sport Med. 1992;14(2):82-99. [DOI] [PubMed] [Google Scholar]
- 9.Howell DR, O’Brien MJ, Beasley MA, Mannix RC, Meehan WP. Initial somatic symptoms are associated with prolonged symptom duration following concussion in adolescents. Acta Paediatr Int J Paediatr. 2016;105(9):e426-e432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meehan WP, Mannix R, Monuteaux MC, Stein CJ, Bachur RG. Early symptom burden predicts recovery after sport-related concussion. Neurology. 2014;83(24):2204-2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCrory P, Meeuwisse W, Dvořák Jet al.. Consensus statement on concussion in sport—the 5th International Conference on Concussion in Sport Held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847. [DOI] [PubMed] [Google Scholar]
- 12.Broglio SP, Cantu RC, Gioia GAet al.. National athletic trainers’ association position statement: management of sport concussion. J Athl Train. 2014;49(2):245-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams RM, Puetz TW, Giza CC, Broglio SP. Concussion recovery time among high school and collegiate athletes: a systematic review and meta-analysis. Sport Med. 2015;45(6):893-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cancelliere C, Hincapié CA, Keightley Met al.. Systematic review of prognosis and return to play after sport concussion: results of the international collaboration on mild traumatic brain injury prognosis. Arch Phys Med Rehabil. 2014;95(3 suppl):S210-29. [DOI] [PubMed] [Google Scholar]
- 15.Currie DW, Kraeutler MJ, Schrock JB, McCarty EC, Comstock RD. Time trends in concussion symptom presentation and assessment methods in high school athletes. Am J Sports Med. 2017;45(14):3368-3373. [DOI] [PubMed] [Google Scholar]
- 16.Giza CC, Brooks A, Mihalik JPet al.. Correlation of concussion symptom profile with head impact biomechanics: a case for individual-specific injury tolerance. J Neurotrauma. 2017;35(4):681-690. [DOI] [PubMed] [Google Scholar]
- 17.Chandran A, Elmi A, Young H, Dipietro L. Determinants of concussion diagnosis, symptomology, and resolution time in U.S. high school soccer players. Res Sport Med. 2020;28(1):42-54 [DOI] [PubMed] [Google Scholar]
- 18.McGuine TA, Pfaller A, Kliethermes Set al.. The effect of sport-related concussion injuries on concussion symptoms and health-related quality of life in male and female adolescent athletes: a prospective study. Am J Sports Med. published online: October 24, 2019 (doi:10.1177/0363546519880175). [DOI] [PubMed] [Google Scholar]
- 19.Neidecker JM, Gealt DB, Luksch JR, Weaver MD. First-time sports-related concussion recovery: the role of sex, age, and sport. J Am Osteopath Assoc. 2017;117(10):635-642. [DOI] [PubMed] [Google Scholar]
- 20.Kerr ZY, Comstock RD, Dompier TP, Marshall SW. The first decade of web-based sports injury surveillance (2004-2005 through 2013-2014): methods of the National Collegiate Athletic Association Injury Surveillance Program and High School Reporting Information Online. J Athl Train. 2018;53(8):729-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCrory P, Meeuwisse WH, Aubry Met al.. Consensus statement on concussion in sport—the 4th International Conference on Concussion in Sport Held in Zurich, November 2012. PM & R. 2013;5(4):255-279. [DOI] [PubMed] [Google Scholar]
- 22.Yard EE, Collins CL, Comstock RD. A comparison of high school sports injury surveillance data reporting by certified athletic trainers and coaches. J Athl Train. 2009;44(6):645-652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lombardi NJ, Tucker B, Freedman KBet al.. Accuracy of athletic trainer and physician diagnoses in sports medicine. Orthopedics. 2016;39(5):e944-949. [DOI] [PubMed] [Google Scholar]
- 24.Comstock RD, Pierpoint LA, Arakkal A, Bihl J. Convenience Sample Summary Report: National High School Sports-Related Injury Surveillance Study: 2017-2018 School Year. http://www.ucdenver.edu/academics/colleges/PublicHealth/research/ResearchProjects/piper/projects/RIO/Documents/2017-18Convenience Sample.pdf. 2018. Accessed May 14, 2019. [Google Scholar]
- 25.Lovell MR, Iverson GL, Collins MWet al.. Measurement of symptoms following sports-related concussion: reliability and normative data for the post-concussion scale. Appl Neuropsychol. 2006;13(3):166-174. [DOI] [PubMed] [Google Scholar]
- 26.Wasserman EB, Kerr ZY, Zuckerman SL, Covassin T. Epidemiology of sports-related concussions in National Collegiate Athletic Association athletes from 2009-2010 to 2013-2014. Am J Sports Med. 2016;44(1):226-233. [DOI] [PubMed] [Google Scholar]
- 27.Lowrey KM. State laws addressing youth sports-related. J Bus Law Technol. 2015;10(1):61-72. [Google Scholar]
- 28.Heyer GL, Schaffer CE, Rose SC, Young JA, McNally KA, Fischer AN. Specific factors influence postconcussion symptom duration among youth referred to a sports concussion clinic. J Pediatr. 2016;174:33-38.e2. [DOI] [PubMed] [Google Scholar]
- 29.Krolikowski MP, Black AM, Palacios-Derflingher L, Blake TA, Schneider KJ, Emery CA. The effect of the “zero tolerance for head contact” rule change on the risk of concussions in youth ice hockey players. Am J Sports Med. 2017;45(2):468-473. [DOI] [PubMed] [Google Scholar]
- 30.Wiebe DJ, D’Alonzo BA, Harris R, Putukian M, Campbell-McGovern C. Association between the experimental kickoff rule and concussion rates in ivy league football. JAMA J Am Med Assoc. 2018;320(19):2035-2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Inj. 2015;29(2):228-237. [DOI] [PubMed] [Google Scholar]
- 32.Rose SC, Fischer AN, Heyer GL. Physicians’ management practices and perceived health risks when postconcussion symptoms persist. Sports Health. 2016;8(1):37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hurtubise JM, Hughes CE, Sergio LE, Macpherson AK. Comparison of baseline and postconcussion SCAT3 scores and symptoms in varsity athletes: an investigation into differences by sex and history of concussion. BMJ Open Sport Exerc Med. 2018;4(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howell DR, Kriz P, Mannix RC, Kirchberg T, Master CL, Meehan WP. Concussion symptom profiles among child, adolescent, and young adult athletes. Clin J Sport Med. 2019;29(5):391-397. [DOI] [PubMed] [Google Scholar]
- 35.Wallace J, Covassin T, Beidler E. Sex differences in high school athletes’ knowledge of sport-related concussion symptoms and reporting behaviors. J Athl Train. 2017;52(7):1062-6050-52.3.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. 2015;134:66-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kroshus E, Baugh CM, Stein CJ, Austin SB, Calzo JP. Concussion reporting, sex, and conformity to traditional gender norms in young adults. J Adolesc. 2017;54:110-119. [DOI] [PubMed] [Google Scholar]
- 38.Yard EE, Schroeder MJ, Fields SK, Collins CL, Comstock RD. The epidemiology of United States high school soccer injuries, 2005-2007. Am J Sports Med. 2008;36(10):1930-1937. [DOI] [PubMed] [Google Scholar]
- 39.Chandran A, Barron MJ, Westerman BJ, DiPietro L. Multifactorial examination of sex-differences in head injuries and concussions among collegiate soccer players: NCAA ISS, 2004–2009. Inj Epidemiol. 2017;4(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Broshek DK, Kaushik T, Freeman JR, Erlanger D, Webbe F, Barth JT. Sex differences in outcome following sports-related concussion. J Neurosurg. 2005;102(5):856-863. [DOI] [PubMed] [Google Scholar]
- 41.Esposito G, Van Horn JD, Weinberger DR, Berman KF. Gender differences in cerebral blood flow as a function of cognitive state with PET. J Nucl Med. 1996;37(4):559-564. [PubMed] [Google Scholar]
- 42.De Courten-Myers G. The human cerebral cortex: gender differences in structure and function. J Neuropathol Exp Neurol. 1999;58(3):217-226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.