Abstract
Background
Coronavirus disease 2019 (COVID‐19) is a rapidly emerging disease classified as a pandemic by the World Health Organization (WHO). To support the WHO with their recommendations on quarantine, we conducted a rapid review on the effectiveness of quarantine during severe coronavirus outbreaks.
Objectives
To assess the effects of quarantine (alone or in combination with other measures) of individuals who had contact with confirmed or suspected cases of COVID‐19, who travelled from countries with a declared outbreak, or who live in regions with high disease transmission.
Search methods
An information specialist searched the Cochrane COVID‐19 Study Register, and updated the search in PubMed, Ovid MEDLINE, WHO Global Index Medicus, Embase, and CINAHL on 23 June 2020.
Selection criteria
Cohort studies, case‐control studies, time series, interrupted time series, case series, and mathematical modelling studies that assessed the effect of any type of quarantine to control COVID‐19. We also included studies on SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome) as indirect evidence for the current coronavirus outbreak.
Data collection and analysis
Two review authors independently screened abstracts and titles in duplicate. Two review authors then independently screened all potentially relevant full‐text publications. One review author extracted data, assessed the risk of bias and assessed the certainty of evidence with GRADE and a second review author checked the assessment. We used three different tools to assess risk of bias, depending on the study design: ROBINS‐I for non‐randomised studies of interventions, a tool provided by Cochrane Childhood Cancer for non‐randomised, non‐controlled studies, and recommendations from the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) for modelling studies. We rated the certainty of evidence for the four primary outcomes: incidence, onward transmission, mortality, and costs.
Main results
We included 51 studies; 4 observational studies and 28 modelling studies on COVID‐19, one observational and one modelling study on MERS, three observational and 11 modelling studies on SARS, and three modelling studies on SARS and other infectious diseases. Because of the diverse methods of measurement and analysis across the outcomes of interest, we could not conduct a meta‐analysis and undertook a narrative synthesis. We judged risk of bias to be moderate for 2/3 non‐randomized studies of interventions (NRSIs) and serious for 1/3 NRSI. We rated risk of bias moderate for 4/5 non‐controlled cohort studies, and serious for 1/5. We rated modelling studies as having no concerns for 13 studies, moderate concerns for 17 studies and major concerns for 13 studies.
Quarantine for individuals who were in contact with a confirmed/suspected COVID‐19 case in comparison to no quarantine
Modelling studies consistently reported a benefit of the simulated quarantine measures, for example, quarantine of people exposed to confirmed or suspected cases may have averted 44% to 96% of incident cases and 31% to 76% of deaths compared to no measures based on different scenarios (incident cases: 6 modelling studies on COVID‐19, 1 on SARS; mortality: 2 modelling studies on COVID‐19, 1 on SARS, low‐certainty evidence). Studies also indicated that there may be a reduction in the basic reproduction number ranging from 37% to 88% due to the implementation of quarantine (5 modelling studies on COVID‐19, low‐certainty evidence). Very low‐certainty evidence suggests that the earlier quarantine measures are implemented, the greater the cost savings may be (2 modelling studies on SARS).
Quarantine in combination with other measures to contain COVID‐19 in comparison to other measures without quarantine or no measures
When the models combined quarantine with other prevention and control measures, such as school closures, travel restrictions and social distancing, the models demonstrated that there may be a larger effect on the reduction of new cases, transmissions and deaths than measures without quarantine or no interventions (incident cases: 9 modelling studies on COVID‐19; onward transmission: 5 modelling studies on COVID‐19; mortality: 5 modelling studies on COVID‐19, low‐certainty evidence). Studies on SARS and MERS were consistent with findings from the studies on COVID‐19.
Quarantine for individuals travelling from a country with a declared COVID‐19 outbreak compared to no quarantine
Very low‐certainty evidence indicated that the effect of quarantine of travellers from a country with a declared outbreak on reducing incidence and deaths may be small for SARS, but might be larger for COVID‐19 (2 observational studies on COVID‐19 and 2 observational studies on SARS).
Authors' conclusions
The current evidence is limited because most studies on COVID‐19 are mathematical modelling studies that make different assumptions on important model parameters. Findings consistently indicate that quarantine is important in reducing incidence and mortality during the COVID‐19 pandemic, although there is uncertainty over the magnitude of the effect. Early implementation of quarantine and combining quarantine with other public health measures is important to ensure effectiveness. In order to maintain the best possible balance of measures, decision makers must constantly monitor the outbreak and the impact of the measures implemented.
This review was originally commissioned by the WHO and supported by Danube‐University‐Krems. The update was self‐initiated by the review authors.
Plain language summary
Does quarantine, alone or in combination with other public health measures, control coronavirus (COVID‐19)?
Background Coronavirus disease 2019 (COVID‐19) is caused by a new virus that has spread quickly throughout the world. Most infected people either experience no symptoms or suffer mild, flu‐like symptoms, but some become seriously ill, and may die. There is no vaccine (a medicine that stops people catching a specific disease) for COVID‐19, so other ways of slowing its spread are needed. One way of controlling the disease is quarantine. This means separating healthy people from other healthy people, who may have the virus after being in close contact with an infected person, or because they have returned from an area with high infection rates. Similar recommendations include isolation (like quarantine, but for people who tested positive for COVID‐19) and physical distancing (people without symptoms keep a distance from each other). What did we want to find out? We wanted to find out whether and how effectively quarantine stops COVID‐19 spreading and if it prevents death. We wanted to know if it was more effective when combined with other measures, and how much it costs. Study characteristics COVID‐19 is spreading rapidly, so we needed to answer these questions as quickly as possible. This meant we shortened some steps of the normal Cochrane Review process. Nevertheless, we are confident that these changes do not affect our overall conclusions. We looked for studies that assessed the effect of any type of quarantine, anywhere, on the spread and severity of COVID‐19. We also looked for studies that assessed quarantine alongside other measures, such as isolation, physical distancing or school closures. COVID‐19 is a new disease, so, to find as much evidence as possible, we also looked for studies on similar viruses, such as SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome). Studies measured the number of COVID‐19, SARS or MERS cases, how many people were infected, how quickly the virus spread, how many people died, and the costs of quarantine. Key results We included 51 studies. Thirty‐two studies focused on COVID‐19, 14 on SARS, three on SARS plus other viruses, and two on MERS. Most studies combined existing data from multiple sources and assumptions to create a model (a simulation) for predicting how events might occur over time, for people in different situations (called modelling studies). Four COVID‐19 studies observed the effects of quarantine (observational studies) on 6064 individuals in China, Greece and Singapore. Twenty‐eight COVID‐19 studies simulated outbreaks in Algeria, China, Canada, Italy, Kazakhstan, Nepal, UK, USA, Singapore, South Korea, on the cruise ship Diamond Princess, and in a general population. Four studies looked back on the effect of quarantine on 178,122 people involved in SARS and MERS outbreaks. The remaining 15 studies modelled SARS and MERS outbreaks.
The modelling studies all found that simulated quarantine measures reduce the number of people with COVID‐19 and the number of deaths. With quarantine, estimates showed a minimum reduction in the number of people with COVID‐19 of 44%, and a maximum reduction of 96%. Similarly, with quarantine, estimates of the number of deaths showed a minimum reduction of 31%, and a maximum reduction of 76%. Combining quarantine with other measures, such as closing schools or physical distancing, may be more effective at reducing the spread of COVID‐19 than quarantine alone. The SARS and MERS studies agreed with the studies on COVID‐19. Two SARS modelling studies assessed costs. They found that the costs may be lower when quarantine measures start earlier. Reliability of the evidence We are uncertain about the evidence we found for several reasons. The observational studies on COVID‐19 did not include a comparison group without quarantine. The COVID‐19 studies based their models on limited data and made different assumptions about the virus (e.g. how quickly it would spread). The other studies investigated SARS and MERS so they only provide indirect evidence. Conclusion Despite limited evidence, all the studies found quarantine to be important in reducing the number of people infected and the number of deaths. Results suggest that quarantine was most effective, and cost less, when it started earlier. Combining quarantine with other prevention and control measures may have a greater effect than quarantine alone. This review includes evidence published up to 23 June 2020.
Background
Coronavirus disease 2019 (COVID‐19) is a new, rapidly emerging zoonotic infectious disease (WHO 2020a). The first case was reported from Wuhan (Hubei province, China) on 31 December 2019. On 30 January 2020, the World Health Organization (WHO) declared the outbreak a global health emergency, on 11 March 2020, a pandemic (WHO 2020b).
COVID‐19 is caused by a novel coronavirus, SARS‐CoV‐2 (severe acute respiratory syndrome coronavirus 2), which is transmitted via droplets during close unprotected contact with an infector and fomites (WHO 2020a). The virus is genetically similar to the coronaviruses that caused severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), but SARS‐CoV‐2 appears to have greater transmissibility and lower pathogenicity than the aforementioned viruses. Estimates of the basic reproduction number (R0) of SARS‐CoV‐2, as a metric for transmissibility, depend on the estimation method, and range from 1.5 to 6.49, in the absence of intense quarantine and physical distancing measures (Liu 2020a). A recent systematic review found the average R0 to be 3.28 and the median to be 2.79 (Liu 2020a). In comparison, the R0 for SARS was estimated at 3.0 (Bauch 2005), and at less than 1.0 for MERS in most regions (Park 2018). The average reproduction number for seasonal influenza viruses is about 1.8 (Biggerstaff 2014).
The pathogenicity of SARS‐CoV‐2 appears to be substantially lower than that of SARS and MERS. The majority (81%) of symptomatic COVID‐19 patients develop a mild form of the disease with dry cough, fever, or unspecific symptoms such as headache, myalgia, or fatigue. More severe cases suffer from dyspnoea and pneumonia, and about 5.0% to 6.0% of COVID‐19 patients are critically ill with respiratory failure, sepsis, or multi‐organ failure (WHO 2020a; Wu 2020a). The case‐fatality rate for COVID‐19 was high at the beginning of the outbreak in Wuhan, but in China the overall case‐fatality rate has declined over time to 0.7% for patients with symptom onset after 1 February 2020 (WHO 2020a). On the cruise ship Diamond Princess, where all passengers were tested, the case‐fatality rate for COVID‐19 was 0.99% (Rajgor 2020). This is substantially lower than the case‐fatality rate for SARS (9.6%; WHO 2020c), and MERS (34.4%; WHO 2020d), but higher than that for seasonal influenza pandemics (0.01%; Taubenberger 2006). The case‐fatality rate, especially at the beginning of an outbreak, has to be interpreted with caution since the denominator (number of infected people) is often not yet well known. In addition case‐fatality rates differ by location, time, and specific demographics like age or pre‐existing health conditions. Data, based on confirmed COVID‐19 cases in Mainland China from 11 February 2020 showed that while the case‐fatality rate for people aged 40 to 49 years was 0.4% it was 8.0% for those aged 70 to 79 years, and 14.8% for infected people of 80 years or older (China CDC 2020).
Currently, no effective pharmacological interventions or vaccines are available to treat or prevent COVID‐19. For this reason, non‐pharmacological public health measures such as isolation, physical distancing, and quarantine are the only effective ways to respond to the outbreak. Isolation refers to the separation of COVID‐19 cases whereas quarantine is the restriction of asymptomatic healthy people who have had contact with confirmed or suspected cases. Quarantine can be implemented on a voluntary basis or can be legally enforced by authorities and may be applied at an individual, group, or community level (community containment (Cetron 2005)). A recent rapid review reported that quarantine can have negative psychological effects such as post‐traumatic stress symptoms, confusion and anger, which can lead to adverse long‐term psychological effects (Brooks 2020). The WHO and the US Center for Disease Control and Prevention (CDC) recommend 14 days of quarantine for individuals who were in close contact with a confirmed case, based on the estimated incubation period of SARS‐CoV‐2 (Jernigan 2020b; WHO 2020e).
According to the International Health Regulations 2005 (WHO 2005), that govern the management of disease outbreaks in 196 countries, any public health measures must be based on scientific evidence and recommendations from the WHO (Habibi 2020). At the beginning of February 2020, the WHO requested the review authors to conduct a rapid review on the effectiveness of quarantine during serious coronavirus outbreaks to support recommendations on quarantine. We updated the rapid review in March 2020 and published it in April 2020 (Nussbaumer‐Streit 2020). Because the body of evidence on COVID‐19 is growing very quickly, we self‐initiated an update of the rapid review in June 2020.
Objectives
To support the WHO for their recommendations on quarantine, we conducted a rapid review on the effectiveness of quarantine during COVID‐19 outbreaks. We aimed to answer the following key questions (KQs).
-
KQ1: Is quarantine of asymptomatic individuals who were in contact with a confirmed or suspected case of COVID‐19, effective to control the COVID‐19 outbreak?
KQ1a: Are there differences in the effectiveness of quarantine in different settings?
KQ1b: How effective is quarantine when combined with other interventions such as case isolation or school closures in reducing transmission, incidence of diseases, and mortality?
-
KQ2: Is quarantine of individuals coming from a country with a declared COVID‐19 outbreak, effective in controlling the COVID‐19 outbreak?
KQ2a: Are there differences in the effectiveness of quarantine in different settings?
Methods
To conduct this rapid review, we employed abbreviated systematic review methods. Compared with the methods of a systematic review, the review team applied the following methodological shortcuts for this rapid review.
No specific searches of grey literature, except for contacting experts in the field.
Abstract screening with support from Cochrane Crowd: all abstracts identified by the updated search were screened with support from Cochrane Crowd (crowd.cochrane.org). Cochrane Crowd is Cochrane's crowdsourcing platform that hosts tasks aimed at identifying health research. For this task we created an interactive training module made up of practice records. The Crowd contributor had to achieve 80% on the training module to be able to progress to the live task. A selected Crowd, those who had participated and performed well in another COVID‐19 related tasks on Cochrane Crowd, were invited to participate in this task. When three members of the Crowd agreed, independently, that a study was not relevant, one person of the author team reviewed the abstract. When three members of the Crowd agreed that a study was relevant, again only one author reviewed the abstract. In cases where the Crowd was not sure about eligibility, then we dually screened the abstracts.
No dual independent 'Risk of bias' assessment and rating of the certainty of evidence; one review author conducted the ratings, a second review author checked the plausibility and correctness. We adhered to PRISMA throughout this manuscript (Moher 2009).
For modelling studies we used an abbreviated tool to assess the quality of the studies.
Criteria for considering studies for this review
See Table 1 for the inclusion and exclusion criteria in this rapid review.
1. Inclusion and exclusion criteria of the rapid review.
| Inclusion | Exclusion | |
| Participants |
KQ1
KQ2
|
|
| Intervention |
KQ1 and KQ2 Different types and locations of quarantinec of individuals
KQ1b
|
|
| Control |
|
|
| Outcomes |
|
|
| Study designs |
|
|
| Languages |
|
|
| COVID‐19: coronavirus disease 2019; KQ: key question; MERS: Middle East respiratory syndrome; SARS: severe acute respiratory syndrome; WHO: World Health Organization | ||
aIn the original review we also included studies on SARS and MERS, due to the limited evidence on COVID‐19. For this update we identified more evidence on COVID‐19, therefore we decided against including additional SARS and MERS studies and included only COVID‐19 studies. We decided to retain the SARS and MERS studies included in the previous version, but we differentiate between evidence directly relevant to COVID‐19 and indirect evidence from SARS and MERS in the results section.
bDefined by WHO as an "occurrence of disease cases in excess of normal expectancy. The number of cases varies according to the disease‐causing agent, and the size and type of previous and existing exposure to the agent" (WHO 2020f). cWe included studies combining isolation with quarantine because isolation of confirmed cases is a prerequisite for quarantine of individuals who were in contact with these cases
The WHO expert panel selected four outcomes that they deemed relevant for their decision‐making process: incident cases, onward transmission, mortality, and costs. This rapid review did not examine the psychological impact of quarantine.
Types of studies
As randomization of quarantine is unethical and not feasible for the diseases in question, we considered non‐randomized studies of interventions to be the best potentially available empirical evidence. In addition, we also included modelling studies, because, especially for COVID‐19, we did not yet expect empirical studies to be available.
Cohort studies
Case‐control studies
Time series
Interrupted time series
Case series
Mathematical modelling studies
We excluded:
case reports
systematic reviews (used for reference list checking)
Language
We did not apply any language restrictions to this update. The previous, original version of this review was limited to Chinese and English.
Types of participants
We included:
(KQ1) contacts of a confirmed or suspected case of COVID‐19 or individuals who live in areas with high‐transmission rates;
(KQ2) individuals returning from countries with a declared outbreak of COVID‐19, defined by the WHO as an "occurrence of disease cases in excess of normal expectancy. The number of cases varies according to the disease‐causing agent, and the size and type of previous and existing exposure to the agent" (WHO 2020f).
We excluded:
symptomatic individuals of COVID‐19 infections;
asymptomatic individuals exposed to other pathogens that can cause respiratory infections.
For the original review published in April we also included studies on SARS and MERS, due to the limited evidence on COVID‐19. For this update we identified more evidence on COVID‐19, so we refrained from including additional SARS and MERS studies in the update. We decided to retain the SARS and MERS studies included in the previous version of this review, but we differentiate between evidence directly relevant to COVID‐19 and indirect evidence from SARS and MERS in the Results section.
Types of interventions
Different types and locations of quarantine of individuals. We included studies combining isolation with quarantine because isolation of confirmed cases is a prerequisite for quarantine of individuals who were in contact with these cases.
(KQ1 and KQ2)
-
Quarantine
voluntary
mandatory
-
Quarantine
individual level
group level
community level
-
Quarantine in
private residence
hospital
public institution
others (cruise ships, etc.)
-
(KQ1b) Quarantine of individuals or a community in combination with other measures:
avoiding crowding
hand hygiene
isolation
personal protective equipment
school measures/closures
physical distancing (also called social distancing)
workplace measures/closures
Control measures included the following.
No quarantine
Different types and locations of quarantine
Public health measures without quarantine to reduce the spread of the virus, such as isolation, physical distancing, personal protective equipment, hand hygiene, others
We excluded environmental measures and travel‐related measures (e.g. travel bans) as either an intervention or control measure (in case it was the only control measure).
Types of outcome measures
Incident cases (as reported by authors ‐ clinical diagnosis and/or laboratory confirmation)
Onward transmission
Mortality
-
Costs
costs of implementation (direct costs)
costs of lost productivity (indirect costs)
cost‐effectiveness
We focused on time points that studies reported for primary outcomes but also included time points that facilitated comparisons of effects across studies.
Search methods for identification of studies
In the following, we describe the search of this update. For detailed information on the search strategy used in the original review, please see the original publication (Nussbaumer‐Streit 2020).
For this update an Information Specialist conducted an update search between 23 and 24 June 2020. Search results were limited to references published since 2002, because the search strategy changed from the original search and it was not sufficient to search back to the date of the last search. No language or publication type limits were applied. We managed search results and removed duplicates in EndNote X9 (Clarivate). We uploaded references to the Cochrane Register of Studies for primary (title and abstract) screening via Cochrane Crowd. See Appendix 1 for the complete strategies.
Search sources
MEDLINE Ovid (1946 to 22 June 2020)
Embase Ovid (1996 to 2020, week 25)
CINAHL Ebsco (1981 to 24 June 2020)
Cochrane COVID‐19 Study Register (covid-19.cochrane.org; searched 21 June 21 via the Cochrane Register of Studies crsweb.cochrane.org)
WHO COVID‐19 Global literature on coronavirus disease (search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov; search 21 June 2020)
Google Scholar to identify citing studies of doi.org/10.1002/14651858.CD013574
Search summary
| Source | Results (with duplicates) | Results (unique) |
| MEDLINE | 2323 | 1728 |
| Embase | 2490 | 744 |
| CINAHL | 729 | 154 |
| Cochrane COVID‐19 Study Register | 1102 | 503 |
| WHO COVID‐19 Global literature on coronavirus disease | 3358 | 1473 |
| Google Scholar (for citing references) | 71 | 58 |
| Total: | 10,073 | 4660 |
Search results
We retrieved 10,073 references in the search and after removing duplicates there were 4660 references (including references previously screened by the original search and the update conducted in April).
Note on revisions from the last update (April 2020)
We included new information sources on COVID‐19 that did not exist in April 2020 (Cochrane COVID‐19 Study Register, and the WHO COVID‐19 Global literature on coronavirus disease). We removed the WHO Global Index Medicus from our source list as its contents on COVID‐19 are contained in the WHO COVID‐19 Global literature on coronavirus disease. We added new terminology to the search strategies for COVID‐19/SARS‐CoV‐2 and removed a language limit for English and German publications.
In addition, review authors screened reference lists of systematic reviews on quarantine in general, and included studies for additional relevant citations. We also contacted experts for additional studies.
Data collection and analysis
Selection of studies
A team of experienced review authors screened all titles and abstracts based on predefined inclusion and exclusion criteria (Table 1), with support from Cochrane Crowd (crowd.cochrane.org). When three members of the Crowd agreed, independently, that a study was not relevant, one person of the author team reviewed the abstract. When three members of the Crowd agreed that a study was relevant, again only one author reviewed the abstract. In cases where the Crowd was not sure about eligibility, then we dually screened the abstracts. While we did not do specific searches of grey literature, we contacted experts in the field for additional studies.
The review author team retrieved the full texts of all included abstracts. Two review authors screened all full‐text publications independently. We resolved disagreements by consensus or by involving a third, senior review author. The team conducted literature screening using Covidence.
Data extraction and management
One experienced review author extracted data from the included studies into standardized tables; a second review author checked the data extraction for completeness and correctness. The data items for observational studies included: author, publication year, country, study design, objective, characteristics of the study participants, description of the intervention, co‐interventions and comparison, and results. For the modelling studies, the data items were: author, year, type of model and model parameters, setting, time, data source and participants, interventions, and results. As different classifications for model types exist, we listed the model type as described by the study authors.
Assessment of risk of bias in included studies
The review author team assessed the risk of bias of the included controlled non‐randomized studies of interventions based on the Risk Of Bias In Non‐randomized Studies ‐ of Interventions (ROBINS‐I) tool (Sterne 2016). ROBINS‐I is a results‐based tool; we have applied the tool at the study level in this review, but we will apply it at the results level for the next update. For single‐arm observational studies of interventions we adapted the 'Risk of bias' assessment criteria for observational studies tool provided by Cochrane Childhood Cancer (Mulder 2019; Table 2). One review author rated the risk of bias for each study; a second review author checked the ratings. The risk of bias could be rated as low, moderate, serious, or critical. Due to time constraints, we omitted an independent, dual 'Risk of bias' assessment. As no validated 'Risk of bias' checklist for mathematical transmission models was available, we assessed whether the modelling and reporting followed the best practice recommendations of the International Society for Pharmacoeconomics and Outcomes (ISPOR) and the Society for Medical Decision making (SMDM) for dynamic mathematical transmission models. Dynamic transmission models allow for risk changes over time and can estimate direct and indirect effects of prevention and control measures on an infectious disease (Pitman 2012). We assessed whether the model was dynamic, whether the study authors conducted uncertainty analyses on key model parameters and assumptions, and whether the results provided estimates of the change in the burden of infection due to the intervention. We selected these three criteria because they best reflected methodological decisions that have an impact on results and conclusions. For modelling studies fulfilling all three criteria we had 'no concerns to minor concerns' regarding their quality; if one or more categories were unclear (e.g. because of incomplete reporting) we had 'moderate concerns', if one or more categories were not fulfilled we had 'major concerns'. We operationalized burden of infection as a quantitative outcome measure reflecting final outcomes affecting peoples' health status (www.who.int/healthinfo/indicators/2018). This includes final outcomes, such as mortality and morbidity (e.g. symptoms, complications, disability, hospitalisation, health‐related quality of life), as well as unintended health‐related harms of interventions. Although mere infection may not affect tangible health in all infected individuals, we included cases of infected individuals and the reproduction number as health outcomes too. Two review authors rated the quality of modelling studies, a senior review author checked the ratings.
2. Risk of bias criteria for single‐arm observational studies of interventions.
| Internal validity | External validity | |
| Study group | Selection bias (representative: yes/no) if the described study group consisted of more than 90% of eligible individuals |
Reporting bias (well defined: yes/no) if the intervention and number of participants was defined |
| Follow‐up | Attrition bias (adequate: yes/no) if the outcome was assessed for more than 90% of the study group of interest (++) or if the outcome was assessed for 60% to 90% of the study group of interest (+) |
Reporting bias (well defined: yes/no) if the length of follow‐up was mentioned |
| Outcome | Detection bias (blind: yes/no) if the outcome assessors were blinded to the investigated determinant |
Reporting bias (well‐defined: yes/no) if the outcome definition was objective and precise |
| Risk estimation | Confounding (adjustment for other factors: yes/no) if important prognostic factors (i.e. age, gender) or follow‐up were taken adequately into account |
Analyses (well‐defined: yes/no) If the method of analysis was described and the effect of the intervention was quantified |
Data synthesis
We synthesized results narratively and in tabular form. Because of the heterogeneity of available primary studies, we did not consider quantitative analyses.
Assessment of the certainty of the evidence
One experienced review author assigned certainty of evidence ratings based on an approach developed by the GRADE Working Group (Guyatt 2008; Schünemann 2013; Schünemann 2019). For observational studies we started at low‐certainty evidence. Newer GRADE guidelines state that observational studies can also start as high certainty if the 'Risk of bias' assessment tool used was ROBINS‐I (Schünemann 2019). However, for most observational studies we did not use ROBINS‐I, so we considered the approach of starting at 'low certainty' as more suitable. For grading the certainty of evidence of modelling studies we followed the recent guidance from the GRADE Working Group (Brozek 2020). Modelling studies start at high‐certainty evidence and are downgraded according to assessments of risk of bias, indirectness, inconsistency, imprecision, and publication bias. GRADE uses four categories to classify the certainty of evidence. A high‐certainty rating of a body of evidence means that we were very confident that the estimated effect lies close to the true effect; a moderate‐certainty rating means we assume the estimated effect is probably close to the true effect; a low‐certainty rating suggests that the estimated effect might substantially differ from the true effect; and a very low‐certainty rating means that the estimated effect is probably markedly different from the true effect. We assessed the certainty of evidence for the four main outcomes. We have reported other patient‐relevant outcomes in the Results section, but we did not grade the certainty of evidence.
Table 3 summarizes the certainty of evidence for KQ1; Table 4 summarizes the certainty of evidence for KQ1b; and Table 5 presents the certainty of evidence ratings for KQ2.
3. GRADE evidence profile for the effectiveness of quarantine for individuals who were in contact with a confirmed/suspected COVID‐19 case in comparison to no quarantine.
|
Patient or population: individuals who were in contact with a confirmed or suspected COVID‐19 case Settings: Canada, China, generic population, UK, Republic of Kazakhstan, Singapore, Taiwan, cruise ship Intervention: quarantine Comparison: no quarantine | ||||||||
| Outcome | Number of studies | Risk of bias | Indirectness | Imprecision | Inconsistency | Other considerations | Summary effect size/outcome | Certainty of the evidence |
| Incidence | 7 modelling studies (Cao 2020; Hsieh 2007; Koo 2020; Rocklöv 2020; Semenova 2020; Su 2020; Tang 2020a) |
Very seriousa | Direct | Precise | Consistent | None |
COVID‐19
Cao 2020 simulated the effect of loosening quarantine measures that are already in place. They concluded that if 40% fewer people were quarantined (e.g. because of less strict follow‐ups of contacts), the peak number of cases would increase two‐fold compared to keeping a full quarantine in place. Koo 2020 stated that under the assumption of R0 1.5, at day 80, isolation of infected persons and quarantine of family members reduced the number of infected individuals compared with the baseline scenario by 95.8%. Semenova 2020 simulated that quarantine reduced the number of infected individuals compared with the baseline scenario by 95.8% (2,038,000 versus 84,920). Su 2020 simulated that reducing the quarantine rate for Beijing to 0.8 would lead to 100 more infected cases after 50 days. Decreasing it to 0.6 would lead to approximately 300 more cases. Doubling the quarantine rate would half the number of infected cases. Rocklöv 2020 estimated that isolation and quarantine prevented 2307 (67%) cases during the COVID‐19 outbreak on the Diamond Princess cruise ship. Tang 2020a estimated that without any measures, the number of confirmed COVID‐19 cases in Wuhan would be 7723 by the end of January 2020. They estimated that reduced contact by 50% could reduce the number of confirmed COVID‐19 cases from 7723 to 4335 (44% reduction); reduced contact by 90% could reduce the number of confirmed COVID‐19 cases to 2731 (65% reduction). SARS Hsieh 2007 state that quarantine is effective to reduce incident cases (461 SARS cases (81%) averted, with a low quarantine rate of 0.05 that equals quarantining 1 out of 21 people that should be quarantined) |
Low |
| Onward transmission | 5 modelling studies (Kucharski 2020; Liu 2020b; Madubueze 2020; Peak 2020; Rocklöv 2020) | Very seriousa | Direct | Precise | Consistent | None |
COVID‐19 Kucharski 2020 estimated that case isolation and quarantine could reduce the effective reproduction number by 37%. Liu 2020b estimated that after implementing quarantine on the Diamond Princess cruise ship the R0 dropped from 6.94 to 0.2 and the transmission rate from 0.026 to 0.0007. Madubueze 2020 estimated R0 to be 1.51 when none of the exposed individuals are quarantined and 0.76 when all exposed individuals are quarantined. Peak 2020 estimated that in a high‐feasibility setting quarantine of individuals can reduce the effective R0 to 0.57 (95% CI 0.32 to 1.05), while monitoring of potentially infected people reduced R0 to 1.55 (95% CI 0.65 to 2.7) assuming a larger fraction of presymptomatic infections. In a low‐feasibility setting, both individual quarantine and active control monitoring alone could not reduce the R0 below 1 for both serial interval scenarios. Rocklöv 2020 estimated that isolation and quarantine lowered the R0 from 14.8 to 1.78 during the COVID‐19 outbreak on the Diamond Princess cruise ship. |
Low |
| Mortality | 3 modelling studies (Ferguson 2020; Hsieh 2007; Semenova 2020) | Very seriousa | Direct | Precise | Consistent | None |
COVID‐19
Ferguson 2020 estimated that for a timeframe of 3 months, case isolation and household quarantine would reduce deaths in the UK by 31% to 34%. Semenova 2020 simulated that quarantine reduced the number of deaths compared with the baseline scenario by 75.8% (15,470 versus 3750). SARS Quarantine was effective in reducing mortality (62 SARS (63%) deaths averted, with a low quarantine rate of 0.05 in Taiwan (Hsieh 2007)) |
Low |
| Costs | 3 modelling studies (Gupta 2005; Mubayi 2010; Semenova 2020) | Very seriousa | Indirectb | Precise | Consistent | None |
COVID‐19 Semenova 2020 states that the introduction of quarantine may potentially reduce the number of ICU doctors and nurses needed to 500 (from 12,026 without quarantine) and 2420 (from 58,144) meaning fewer resources required and lower costs in the healthcare sector. SARS Gupta 2005 stated that at a transmission rate of 8%, the total savings of quarantine over isolation alone varies between CAD 279 million to 232 million (reference year 2003). The earlier that effective quarantine measures are implemented, the greater are the savings. Mubayi 2010 came to similar conclusions and stated that increasing the quarantine effort results in lower overall costs over the entire outbreak in all 3 assessed quarantine strategies. |
Very low |
| CAD: Canadian Dollar; COVID‐19: coronavirus disease 2019;ICU: intensive care unit; R0: basic reproduction number; SARS: severe acute respiratory syndrome | ||||||||
aDowngraded two steps for risk of bias: one because we had moderate to minor concerns regarding quality and one because model parameters are accompanied by uncertainties. bDowngraded one step for indirectness because studies were on SARS or (in COVID‐19 study) only one aspect of resource use (health care personnel) was mentioned, without mentioning costs of quarantine measures.
4. GRADE evidence profile for the effectiveness of quarantine in combination with other measures to contain a COVID‐19 outbreak in comparison to no prevention and control measures or combined measures without quarantine.
|
Patient or population: individuals who were in contact with a confirmed or suspected COVID‐19 case or who live in an area with high‐transmission rates Settings: Algeria, China, Italy, Korea, Nepal, UK, USA, Singapore Intervention: quarantine (individual, community) in combination with other prevention and control measures Comparison: no prevention and control measures, combined measures without quarantine | ||||||||
| Outcome | Number of studies | Risk of bias | Indirectness | Imprecision | Inconsistency | Other considerations | Summary effect size/outcome | Certainty of the evidence |
| Incidence | 9 modelling studies (Choi 2020; Ferguson 2020; Hamidouche 2020; Hoertel 2020; Koo 2020; Shen 2020; Wang 2020; Wu 2020b; Zhao 2020a) | Very seriousa | Direct | Precise | Consistent | None |
COVID‐19
Choi 2020 stated that by reducing the transmission rate by 90% or 99% by implementing prevention and control measures (not specified) the proportion of COVID‐19 cases would only be 0.05% or 0.04% of the 5 million cases predicted for South Korea without any measures taken. Ferguson 2020 stated: "Reduction of cases that require critical care beds compared with unmitigated COVID‐19 epidemicb: Case isolation + home quarantine + physical distancing of those over 70 years of age: 67%" Hamidouche 2020 estimated that the implemented strategy (isolation of cases and 14‐day quarantine of contacts and travellers, physical distancing, movement restriction, and lockdown) has avoided 2993 COVID‐19 cases in the country(1914 instead of 4907 cases) within 7 days. Hoertel 2020 focused on the lifting of community quarantine. They estimated that a 2‐step quarantine lifting according to age, (i.e. a 3‐week quarantine for all individuals aged < 70 years and an additional 8‐week quarantine period for people aged > 70 years), would lower the cumulative incidence by 23%, compared to a 16‐week quarantine followed by a lifting for all individuals. Koo 2020 reported isolation of infected persons and quarantine of family members reduced the number of infected individuals compared with the baseline scenario by 95.8%, quarantine plus school closure and workplace distancing reduced the median cumulative number of infections 96.4% and 98.57%, respectively. The combination of all interventions reduced the median cumulative infection count by 99.3% from the baseline scenario (assuming R0 1.5, at day 80) Shen 2020 estimated that without the metropolitan‐wide quarantine, the epidemic would result in 491,320 (331,470 to 651,180) infected cases. Community quarantine could prevent 87.1% (95% CI: 84.7% to 89.5%) and 71.8% (95% CI: 66.4% to 77.3%) of infections in public spaces and households. Wang 2020 showed that without quarantine 10,111,537 individuals in Wuhan would have been infected (91%) by the end of one year, but with the control measures in place the number of infected individuals is 32,582 (0.3% of the Wuhan population). In Italy, a quarantine policy with an effective quarantine rate of 12% and lockdown would reduce the incidence of new infections exponentially, reaching ≤ 100 in just 26 days and zero in 62 days. In the UK, an effective quarantine rate of 20% would bring the incidence of new infections to under 100 in 35 days and to zero in 70 days. In the USA, a quarantine effective rate of 9% would bring the incidence of new infections to under 100 in 152 days; a rate of 20% in 65 days. Wu 2020b stated that stronger control measures (combination of multiple measures, such as isolation and quarantine, physical distancing, school closures) are more effective than single measures or no interventions. By reducing the contact rate and infection efficiency by > 50% they predicted 3088 COVID‐19 cases within 3 months in Wuhan. By reducing it only by < 45% they predicted 4719 cases. Zhao 2020a predicted more than 800 million COVID‐19 cases for China (without Hubei) without the implementation of any measures and an epidemic duration of 477 days. With prevention and control measures (e.g. isolation, quarantine, travel restrictions) the number of cases could be only 13,322 and the duration could be only 45 days. |
Low |
| Onward transmission | 5 modelling studies (Fang 2020; Geng 2020; Hamidouche 2020; Kucharski 2020; Sjödin 2020) | Very seriousa | Direct | Precise | Consistent | None |
COVID‐19
Fang 2020 stated that implementing a combination of containment measures including quarantine, school closures, travel restrictions, cancellation of mass gatherings, and strict exit screening reduced R0 from 2.9 to 2.3 starting at 2 weeks after implementation. Geng 2020 stated that quarantine and school closures in Wuhan reduced the peak of transmissions by 45.7% and 29.9%, respectively. Hamidouche 2020 calculated the average R0 over the first 42 days of the epidemic to be 2.28 (95% CI 1.85 to 2.71) and Rt after preventive measures implemented to be 1.25 (95% CI 1.19 to 1.31). Kucharski 2020 predicted that the combination of self‐isolation + household quarantine + manual tracing of acquaintances + limit to four daily contacts with other individuals + app‐based tracing could reduce the effective R0 by 66% (compared to isolation + quarantine: 37%). Sjödin 2020 focused on the situation in Italy and modelled the effectiveness of community quarantine by degree of compliance and household sizes. For a six‐person household and no quarantine adherence, the model predicted 43 new cases over 14 days. While for a single household with full adherence no secondary cases were predicted. This means that higher adherence and smaller quarantine units help to minimise the number of secondary cases over the 14‐day period. |
Low |
| Mortality | 5 modelling studies(Ferguson 2020; Hoertel 2020; Pandey 2020; Shen 2020; Wu 2020b) | Very seriousa | Direct | Precise | Consistent | None |
COVID‐19
Ferguson 2020: "Reduction of deaths compared with unmitigated COVID‐19 epidemicb:
Case isolation + home quarantine + physical distancing of those over 70 years of age: 49%" Hoertel 2020 focused on the lifting of community quarantine. They estimated that a 2‐step quarantine lifting according to age, (i.e. a 3‐week quarantine for all individuals aged < 70 years and an additional 8‐week quarantine period for people aged > 70 years), would lower cumulative mortality by 68%, compared to a 16‐week quarantine followed by a lifting for all individuals. Pandey 2020 Physical distancing for one year after a one‐month lockdown that reduces contact rates by 35% would reduce mortality by 33%. Control strategies that are focused on active case finding and isolating/quarantining (exposed and infectious) individuals after one month of lockdown would decrease mortality by 27%. Most efficient would be the combination of physical distancing and casefinding + isolation/quarantine after one month of lockdown, decreasing the number of projected deaths by 99.6%. Shen 2020 estimated that without the metropolitan‐wide quarantine, the epidemic would result in 15,907 (10,950 to 20,865) deaths. Community quarantine could prevent 79.27% (75.10 to 83.45) of deaths. Wu 2020b stated that stronger control measures reduce mortality of COVID‐19. By reducing the contact rate and infection efficiency by > 50% they predicted 443 deaths out of 11.5 million inhabitants in Wuhan within 3 months, by reducing it only to < 45% they predicted 739 deaths. |
Low |
| Costs | No evidence | |||||||
| CI: confidence interval; COVID‐19: coronavirus disease 2019; R0: basic reproduction number; Rt: current reproduction number | ||||||||
aDowngraded two steps for risk of bias: one because we had moderate to minor concerns regarding quality and one because model parameters are accompanied by uncertainties. bNumbers based on unpublished manuscript, pre‐peer review; numbers of other combination strategies do not seem plausible (potential mislabelling of table); we contacted study authors but did not receive a response.
5. GRADE evidence profile for the effectiveness of quarantine for individuals travelling from a country with a declared COVID‐19 outbreak compared to no quarantine.
|
Patient or population: individuals travelling from regions with a declared COVID‐19 outbreak Settings: travellers from China, UK, Spain, Turkey Intervention: quarantine of travellers Comparison: no quarantine of travellers | ||||||||
| Outcome | Number of studies | Risk of bias | Indirectness | Imprecision | Inconsistency | Other considerations | Summary effect size/outcome | Certainty of the evidence |
| Incidence | 4 observational studies (Arima 2020; Hsieh 2005; ; Lytras 2020; Wang 2007) | Seriousa | Indirectb | Precise | Inconsistentc | None |
COVID‐19 Arima 2020: from 566 travellers arriving in Japan from Hubei Province, 12 had COVID‐19 (2.1%). Seven of them were identified upon arrival by entry screening, but five were identified during 14‐day quarantine. Lytras 2020: from 357 travellers from the UK, 13 were SARS‐CoV‐2 positive (3.6%, 95% CI 2.0 to 6.1). From 394 travellers from Spain, 25 were positive (6.3, 95% CI 4.1 to 9.2), and two of 32 returnees from Turkey (6.3, 0.9 to 20.8). SARS Wang 2007 reported that 56 of 95,271 quarantined travellers developed SARS (0.0006%). Hsieh 2005 reported that 0 out of 95,828 quarantined travellers developed SARS (0%). |
Very low |
| 1 modelling study (Hsieh 2007) | Very seriousd | Indirecte | N/A | Inconsistentc | None | Hsieh 2007: if all 17 unquarantined imported cases had been quarantined, 280 SARS cases could have been averted. Based on their data source, out of the more than 95,000 quarantined people, only two developed SARS. If these two individuals had not been quarantined, 29 additional cases would have occurred. | Very low | |
| Onward transmission | No evidence | |||||||
| Mortality | 1 modelling study (Hsieh 2007) | Seriousd | Indirecte | N/A | Inconsistentc | None | Hsieh 2007: if all 17 unquarantined imported cases had been quarantine, 48 deaths could have been averted. Two people under quarantine developed SARS. By placing them under quarantine 5 additional deaths could be averted. | Very low |
| Costs | No evidence | |||||||
| CI: confidence interval; COVID‐19: coronavirus disease 2019; N/A: not applicable; SARS‐CoV‐2: severe acute respiratory syndrome coronavirus 2 | ||||||||
aDowngraded one step for risk of bias because three of the observational studies had a moderate risk of bias. bDowngraded one step for indirectness because observational studies did not report incidence of new cases or new cases averted but number of quarantined travellers who developed COVID‐19; two studies provided indirect evidence on SARS. cDowngraded one step because a retrospective study (Hsieh 2005), not specifically reporting incidence of new cases but number of quarantined travellers who developed SARS, reported 0 SARS cases within more than 95,000 quarantined travellers. This differs slightly from the data used by Hsieh 2007: 2 SARS cases out of more than 95,000 quarantined travellers. dDowngraded two steps for risk of bias: one because we had moderate concerns regarding quality and one because model parameters are accompanied by uncertainties. eDowngraded one step for indirectness because the study used SARS data, which does not reflect the presymptomatic infectiousness of COVID‐19.
Results
Description of studies
The PRISMA flow diagram in Figure 1 provides an overview of the study selection process; the characteristics of the included observational and modelling studies are in Characteristics of included studies tables. Table 6 presents the results of each individual study.
1.
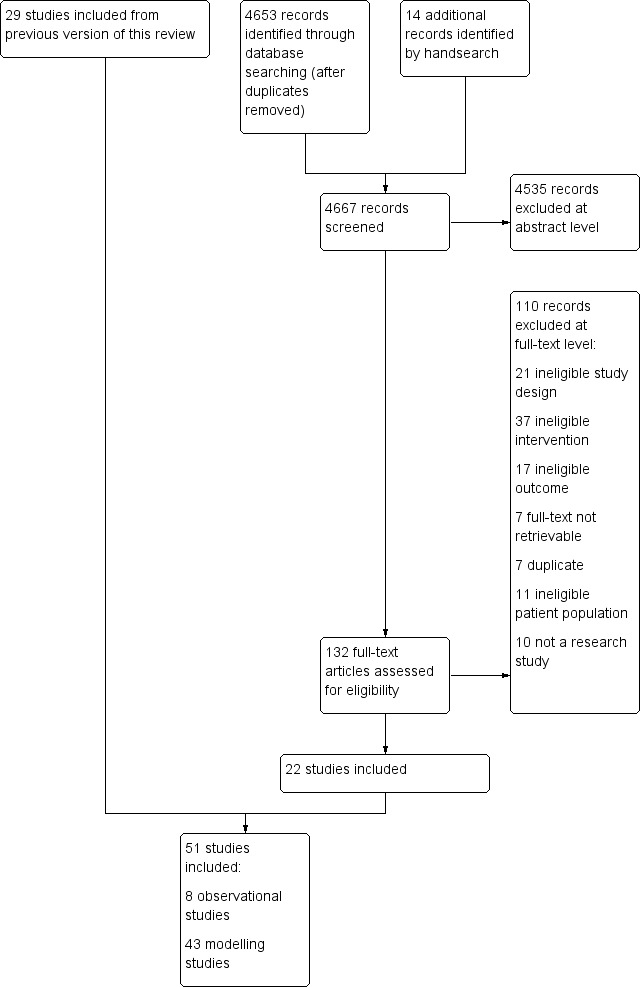
Study flow diagram
6. Results reported in individual studies.
| Study | Study design, publication type | Results |
| Arima 2020 | Cohort study (single‐arm, non‐controlled), journal publication | Among 566 travellers returning from China, 12 cases of SARS‐CoV‐2 infection were detected. Only 7 of these 12 were detected by entry screening (screening of symptomatic travellers only detected 2 cases), the other 5 travellers developed the disease during the 14‐day quarantine. Without quarantine of travellers, 5 cases would have been missed. |
| Cowling 2020 | Cohort study (single‐arm, non‐controlled), journal publication | "As of March 31, 2020, Hong Kong had confirmed 715 cases of SARS‐CoV‐2 infection", (386 imported cases, 142 unlinked local cases, and 187 secondary cases). 621 infections were symptomatic and 94 asymptomatic. "Transmissibility (Rt) remains around the critical threshold of 1." The combination of public health measures (quarantine of travellers, isolation of cases and quarantine of their contacts, population behaviour changes, such as physical distancing, personal protective measures and travel restrictions) was associated with reduced spread of COVID‐19. The authors were not able to disentangle the specific effects of each measure. |
| Hsieh 2005 | Cohort study (non‐randomized controlled study of intervention), journal publication | Level A (quarantine of close contacts): out of 55,632 quarantined individuals, 24 confirmed SARS cases Level B (quarantine of travellers): out of 95,828 quarantined individuals, 0 confirmed SARS cases Onset‐to‐diagnosis: significantly shorter in quarantined individuals (1.20 versus 2.89 days, P = 0.006) Diagnosis‐to‐classification: numerically shorter in quarantined individuals (6.21 versus 7.34 days, P = 0.7864) Onset‐to‐diagnosis time from period 1 to periods 2 and 3: significantly longer for period 1 (no intervention measures implemented) than period 2 (interventions include the implementation of a level B quarantine) (3.64 versus 2.10 days, P < 0.0001); no significant difference between periods 2 and 3 (expedited classification procedures in place) (2.10 versus 2.60 days, P = 0.072) Diagnosis‐to‐classification time from period 1 to periods 2 and 3: no statistically significant difference between periods 1 and 2 (9.18 versus 8.24 days); the time from period 2 to period 3 was significantly shortened (8.24 versus 5.65 days, P < 0.001) |
| Lee 2020 | Cohort study (single‐arm, non‐controlled), journal publication | "As of 10 March 2020, > 4000 close contacts had been placed under quarantine in Singapore, and eight cases developed symptoms while under quarantine and tested positive." |
| Lytras 2020 | Cohort study (single‐arm, non‐controlled), journal publication | Travellers arriving in Greece from countries with widespread SARS‐CoV‐2 (UK, Spain, Turkey) were screened between 20 and 25 March 2020. All but one traveller had no symptoms on arrival. Nevertheless prevalence was high in these cohorts: Travellers from UK: 3.6% from 357 (95% CI 2.0 to 6.1%), Spain: 6.3% from 394 (95% CI 4.1 to 9.2%), Turkey: 6.3% from 32 (95% CI 0.8 to 20.8%). Overall 5.1% (40 of 783) tested positive for SARS‐CoV‐2 on arrival, during quarantine another four tested positive for SARS‐CoV‐2. |
| Pang 2003 | Cohort study (single‐arm, non‐controlled), journal publication | Overall attack rate for becoming a probable case among close contacts: 6.3% (95% CI 5.3 to 7.3) Attack rate by demographics in % (95% CI)
Among 206 close contacts (whose last contact was a patient with SARS), 4 (1.9%) developed SARS. Some interventions, such as quarantine of low‐risk contacts and fever checks at transportation sites, seemed to have less direct impact in curbing the outbreak. |
| Park 2020 | Cohort study (non‐randomized controlled study of intervention), journal publication | Of all 116 quarantined people, 0% became confirmed cases during average quarantine duration of 15 days Overall survival rate: 104/116 (90% survived 2 years); no statistically significant difference between groups (P = 0.849) |
| Wang 2007 | Cohort study (non‐randomized controlled study of intervention), journal publication | Level A (quarantine of close contacts): out of 52,255 quarantined individuals: 102 probable/suspected/laboratory‐confirmed SARS cases Level B (quarantine of travellers): out of 95,271 quarantined individuals: 56 probable/suspected/laboratory‐confirmed SARS cases Advanced age (> 60 years) was identified as a risk factor for SARS in both level A and level B quarantine. For level A quarantine, the odds ratio for developing SARS in this age group was 2.7; for level B quarantine, the odds ratio was 10.5. The probabilities for contracting SARS for the referent group (age < 20 years) were different (0.09% versus 0.02% for level A versus level B quarantine). Quarantining only those with known SARS exposure could have reduced the number of people quarantined by approximately 64% |
| Study | Typeof model used, publication type | Results |
| Becker 2005 | Transmission model, journal publication | Quarantine of households of a confirmed case is more efficient if transmission rate is high and time to diagnosis is long. It reduces the R0 below 1 if every case is diagnosed within 8.8 days. Quarantine of households combined with contact tracing and quarantining of contacts of confirmed cases reduces the R0 from its base value of 6 to below 1 when cases are diagnosed within about 5 days of the onset of infectivity. |
| Cao 2020 | SEIR model, journal publication | With a combination of strict prevention and control measures (cancelling events, quarantine, physical distancing) the peak in Hubei was modelled to be at about 50,000 cases on 19 February 2020. Without prevention and control measures, twice as many people would be infected; the peak would be earlier and higher, resulting in greater loss of life. Assuming the quarantine ratio drops to 0.6, the peak number of cases will double compared to keeping full prevention and control measures in place. |
| Chau 2003 | Back‐projection method, journal publication | Quarantining the contacts of confirmed and suspected SARS cases seems to be more effective than quarantining only the contacts of confirmed cases due to the diagnosis time lag. Infections within hospitals can be reduced by better isolation measures and protective equipment. |
| Choi 2020 | Susceptible‐exposed‐infected‐hospitalized‐recovered model, journal publication | Assuming that the effect of the epidemic prevention measures starts on 5 March, when the transmission rate is reduced by 90% or 99%, the epidemic peak will be advanced to 7 March and 6 March. The total number of patients will be reduced to 26,634 and 19,426 instead of 4,992,000 without any measures. With the decrease in transmission rate, the total epidemic time, the size of the epidemic focus, and the total number of patients will all be reduced. If the transmission time of infection is reduced from 4 days to 2 days, the total epidemic time will be reduced, but the size of the epidemic point will be larger. Specific effect of quarantine = NR |
| Day 2006 | Probabilistic models, journal publication | When isolation is ineffective, the use of quarantine will be most beneficial when there is significant asymptomatic transmission, and if the asymptomatic period is neither very long nor very short. Provided that isolation is effective, the number of infections averted through the use of quarantine is expected to be very low. |
| Fang 2020 | SEIR model, journal publication | The declines in the dynamic trend of the effective R0 indicated the effectiveness of stringent government measures (early detection, isolation and quarantine, enough medical supplies, patients admitted to hospitals, therapeutic strategies). More rigorous government control policies are associated with a slower increase of the infected population. Quarantine and protective procedures are less effective as more cases accrue, so the optimization of a treatment plan and the development of specific drugs is of more importance. Specific effect of quarantine = NR |
| Ferguson 2020 | Modified, individual‐based simulation model, report on website of the Imperial College | Without doing anything, the model predicts 510,000 deaths in the UK For a timeframe of 3 months, home isolation and household quarantine would reduce the death rate by 31% to 34%. However, most effective is the combination of interventions (case isolation + home quarantine + physical distancing). This combination reduces the critical care demand by two‐thirds and halves the number of deaths. |
| Fraser 2004 | Model of infectious disease outbreak dynamics of several pathogens, journal publication | SARS and smallpox are easier to control than pandemic influenza and HIV using simple public health measures (i.e. isolation and quarantine). Influenza is very difficult to control even with 90% quarantining and contact tracing because of the high level of presymptomatic transmission and very short incubation (2 days) and infectious (3‐4 days) periods. |
| Geng 2020 | SEIR model, journal publication | The model shows that a further reducing of the number of susceptible people in contact with exposed and sick people by travel restriction (= community quarantine ‐ people only allowed to be in certain area) and work/school closure will slow down the development of the epidemic and reduce the peak of exposed and infected people by 45.71% and 29.90%, respectively. |
| Gumel 2004 | Deterministic model, journal publication | Both isolation and quarantine seem to be effective means for controlling the spread of SARS. Reduction of the time to quarantine or isolation resulted in the greatest reduction of cumulative deaths. If limited resources are available, the study authors recommend investing all resources in one intervention rather than partially investing in both. |
| Gupta 2005 | Mathematical and health economic model, journal publication | The results indicate that quarantine is effective in containing newly‐emerging infectious diseases and is also a cost saving when compared to not implementing a widespread containment mechanism. Primary wave: infected = 1, quarantined = 100, averted infections = 4672 Secondary wave: infected = 8, quarantined = 900, averted infections = 4608 Tertiary wave: infected = 64, quarantined = 7400, averted infections = 4096 |
| Hamidouche 2020 | Alg‐COVID‐19 model, pre‐print | The implemented preventive strategy (isolation of cases and 14‐day quarantine of contacts and travellers, physical distancing, movement restriction, and lockdown) has avoided 2993 COVID‐19 cases in the country (1914 instead of 4907 cases) within 7 days. The average R0 over the first 42 days of the epidemic was 2.28 (95% CI 1.85 to 2.71) and Rt after preventive measures implemented was 1.25 (95% CI 1.19 to 1.31). Specific effect of quarantine = NR |
| Hoertel 2020 | Stochastic agent‐based microsimulation model, pre‐print | Quarantine of all New Yorkers (community quarantine) was very efficient to contain the viral spread, but it is insufficient to prevent a second epidemic peak once lifted. The duration of quarantine (4 to 16 weeks) had no effects on the endpoints. A 2‐step quarantine lifting according to age, (i.e. 3‐week quarantine for all individuals aged < 70 years and an additional 8‐week quarantine period for people aged > 70 years), lower the cumulative incidence by 23% and the cumulative mortality by 68%, compared to a 16‐week quarantine followed by a lifting for all individuals. If no quarantine would have been in place the model estimated about 30,000 deaths in New York. |
| Hou 2020 | A well‐mixed SEIR compartmental model, journal publication | "Interventions, such as isolation and quarantine, can effectively reduce the peak number of COVID‐19 infections and delay the peak time of infections" by reducing the contact rate. |
| Hsieh 2007 | Susceptible‐infected‐recovered model with additional compartments for Level A and Level B quarantine, journal publication | Level A quarantine prevented approximately 461 additional SARS cases and 62 additional deaths. The effect of a Level B quarantine was comparatively minor; quarantined cases prevented 29 additional cases and 5 deaths. The combined impact of the 2 quarantine levels reduced the case number and deaths by almost one‐half. |
| Hu 2020 | SEIRQ model, journal publication | "No quarantine or very weak quarantine on the susceptible individuals and exposed individuals before the days of the peak values of the confirmed cases may lead to the disease outbreak again. The weaker quarantine rates together with the more input population resulted in the more infected individuals and increased" the maximum values of cumulative confirmed cases. |
| Koo 2020 | Agent‐based influenza epidemic simulation model (FluTE, stochastic), journal publication | R0 1.5, at day 80: isolation of infected persons and quarantine of family members reduced the number of infected individuals compared with the baseline scenario by 95.8%*, quarantine plus school closure and workplace distancing reduced the median cumulative number of infections 96.4% and 98.57%*, respectively. The combination of all interventions reduced the median cumulative infection count by 99.3%* from the baseline scenario. "The combined intervention had a smaller effect when R0 was 2.0 or 2.5." *self‐calculated percentages by review authors |
| Kucharski 2020 | Model of individual‐level transmission stratified by setting (household, work, school, or other), journal publication |
Mean transmission reduction:
|
| Liu 2020b | Contact‐network model, journal publication | "During the early epidemic with intensive social contacts", R0 was 6.94 and transmission rate was 0.026 (based on data from the cruise ship Diamond Princess". After implementing quarantine R0 dropped to 0.2 and the transmission rate to 0.0007. If no quarantine was in place, all people on board would have been infected within a month according to their model. |
| Lloyd‐Smith 2003 | Stochastic model, journal publication | Contact tracing and quarantine can, to some extent, compensate for inadequate isolation facilities, making an increasingly significant contribution as the basic R0 rises. If contact tracing is delayed, such that no individuals are quarantined until 5 days following exposure, the quarantine’s contribution is considerably reduced. Delays in initiating quarantine or isolation undermine the effectiveness of other control measures, particularly in high‐transmission settings. Healthcare workers are exposed to a prevalence much higher than that in the community at large. Measures that reduce transmission within hospitals have the greatest impact on the epidemic’s R0. Combined strategy of contact tracing and case‐management measures (quarantine and isolation) led to rapid containment of the outbreak in 85% of simulations. |
| Madubueze 2020 | Compartment model, pre‐print | With the combination of interventions, "the number of exposed and infected individuals will reduce drastically within a short time but not to zero, leaving a residue of infected individuals with the potential to cause a further outbreak. R0 = 1.51 when none of the exposed individuals are quarantined R0 = 0.76 when all exposed individuals are quarantined." |
| Mubayi 2010 | Dynamic model, cost‐effectiveness model, journal publication | The effect of the combination of quarantine and contact tracing depends on infectiousness of the virus, susceptibility of the population and resource availability. The study authors concluded that increases in the quarantine rates have the same qualitative effect (but different quantitative effects) on each random tracing strategy, and that the total numbers of new cases, deaths, and time to extinction decrease monotonically. Results suggest that the greatest reduction in cases, deaths and isolated individuals can be obtained by the use of the control policy when the contact‐tracing rate assumes a maximum effort independent of the outbreak size. |
| Nishiura 2004 | Deterministic mathematical model, journal publication | The possible trajectories of a SARS epidemic depend on the levels of public health interventions, as quarantine and precautionary measures greatly affect transmissibility. It is shown that either 100% effective precautionary public health measures or quarantine would lead to a decline in incidence, but the combination of them reduces the R0 in a linear way unlike the practice of isolation. In the absence of precautionary public health measures, at least 66.7% of susceptible people, traced latent or traced uninfected contacts, should be quarantined to suppress the epidemic. Precautionary public measures should be undertaken by a high proportion of susceptible people (75% or 90%) to reduce the number of newly‐infected cases when no quarantine was carried out. |
| Pandey 2020 | Age‐structured SEIR model, pre‐print | Without any intervention, the epidemic would peak at 100 days from 24 March. Demand for ICU beds would exceed the supply in Kathmandu, Nepal by a factor of 25. A lockdown will delay the peak but not make any difference to the number of deaths or ICU beds needed. Physical distancing for one year after a one‐month lockdown that reduces contact rates by 35% would reduce mortality by 33% and need for ICU beds by 63%. "Control strategies that are focused on active case finding and isolating infected (exposed and infectious) individuals" for one year after one month of lockdown would decrease mortality by 27% and demand for healthcare by 50%. Combining physical distancing and casefinding + isolation/quarantine after one month of lockdown, the total projected deaths would be decreased by 99.6%, healthcare demand would drop similarly. |
| Peak 2017 | Agent‐based branching model, journal publication | The interventions are not equivalent, and the choice of which intervention to implement to achieve optimal control depends on the infectious disease's natural history, its inherent transmissibility, and the intervention feasibility in the particular healthcare setting. The benefit of quarantine over symptom monitoring is maximized for fast‐course diseases (short duration of infectiousness and a short latent period compared with the incubation period) and in settings where isolation is highly effective, a large proportion of contacts is traced, or there is a long delay between symptom onset and isolation. |
| Peak 2020 | Stochastic SEIR model, journal publication | High‐feasibility setting: shorter serial interval (4.8 days): median effective R0 was 0.57 (95% CI 0.32 to 1.05) under individual quarantine and 1.55 (0.65 to 2.7) under active monitoring with the longer serial interval (7.5 days): median effective R0 was 0.49 (95% CI 0.34 to 0.97) under individual quarantine and 0.54 (0.32 to 0.98) under active monitoring. Low‐feasibility setting: R0 under individual quarantine and active control monitoring remained above 1 for both serial interval scenarios, even when R0 was 1.5. "Individual quarantine could contain an outbreak of COVID‐19 with a short serial interval (4.8 days), but only in settings with high intervention performance where at least 75% of infected contacts are individually quarantined. Assuming a mean serial interval of 4.8 days, the incremental benefit of individual quarantine over active monitoring was substantial as a result of the shorter time from infection to onward transmission and more presymptomatic transmission. However, using a mean serial interval of 7.5 days, individual quarantine and active monitoring are similarly effective at controlling onward transmission in a high‐feasibility setting." |
| Pourbohloul 2005 | Urban contact‐network model, journal publication | For a mildly contagious disease, an outbreak can be controlled with a combination of isolation, which reduces the infectious period by 25%, and quarantine, which successfully sequesters 30% of all case‐patient contacts. Much more rigorous isolation and quarantine are required for a more contagious disease. |
| Rocklöv 2020 | SEIR model, journal publication | The R0 on board (the Diamond Princess cruise ship) was initially 4 times higher compared to the R0 in Wuhan, but the countermeasures lowered it substantially. Based on the modelled initial R0 of 14.8, it was estimated that without any interventions 2920 out of 3700 people (79%) would have been infected from 21 January to 19 February 2020. Isolation and quarantine therefore prevented 2307 cases and lowered the R0 to 1.78. |
| Ryu 2020 | SEIRQ model, journal publication | Without any interventions the total number of infected individuals would reach 184 to 277 from 13 March to 26 March with the arrival of 0.1%, 0.2%, or 1% of pre‐infectious students from China in Seoul, assuming students would arrive in the 15 days before and after 1 March 2020. The number of infected and isolated individuals increases with higher proportions of subclinical COVID‐19 cases. The number of infected and isolated individuals was smaller due to a higher compliance of the quarantine programme. The study suggests that most of the infected individuals arriving in Seoul could be isolated from the home‐quarantine programme under a compliance rate of 70% to 100%, so an epidemic caused by incoming international students from Chinare is deemed unlikely to occur in Seoul, Korea. |
| Semenova 2020 | SEIR model, journal publication | Without containment measures, there will be 2.04 million infected individuals, 15,470 people will die, and 156,000 patients will require hospitalisation in Kazachstan. Under quarantine measures, reduction of all exposed and infected individuals will result in a total of 188,983 cases at the peak. There will be a total reduction of 3750 deaths at the peak and a reduction of 931,000 hospitalized patients at the peak. Introduction of quarantine may potentially reduce the number of ICU doctors and nurses needed to between 500 (from 12,026 without quarantine) and 2420 (from 58,144) |
| Shen 2020 | Dynamic compartmental model, journal publication | In the presence of the community quarantine, 100,610 (95% CI 82,326 to 118,900) infections may have occurred and among which 68,975 (56,621 to 81,330) would be diagnosed (68.58%), and 3252 (2667 to 3837) would have died. Without quarantine, the epidemic would result in 491,320 (331,470 to 651,180) infections and 15,907 (10,950 to 20,865) deaths. The "quarantine would prevent 79.27% (75.10–83.45%) of deaths, 87.08% (84.68–89.49%) and 71.84% (66.39–77.29%) of infections in public space and households." |
| Sjödin 2020 | Markov process for SEIR model, journal publication | "Higher adherence and smaller quarantine units help to minimise the number of secondary cases over the 14 days period, as well as latent and infectious cases at the end of a lockdown. Less strict quarantine will result in much longer lockdown periods. For an average household size of two persons with complete, near‐complete, medium and no community quarantine (i.e. 0, 1, 5, and 10 hours respectively in the community), we predict 3, 4, 7 and 11 secondary infections during the lockdown. With an average three‐person household size, 7, 8, 12 and 20 secondary infections are predicted, respectively. Transmission will continue to occur unless the most stringent community quarantine measures are being taken in a lockdown setting, which means near‐complete reduction of all activities in the community. Smaller household sizes, or quarantine group sizes, are associated with fewer secondary cases." |
| Su 2020 | SEIR model, journal publication | "Reducing the quarantined proportion of exposed individuals (0.8q, 0.6q) led to an increase in the peak value and delayed the peak time. Conversely, the peak value decreased and an earlier peak time occurred with a higher quarantined proportion of exposed individuals (2q, 1.5q)." Beijing: normal quarantine rate: 400 cases after 50 days 0.8 quarantine rate: 500 cases after 50 days 0.6 quarantine rate: 700 cases after 50 days 1.5 quarantine rate: 280 cases after 50 days 2 quarantine rate: 200 cases after 50 days (numbers estimated from figure 6 in Nussbaumer‐Streit 2020). The effects of quarantine rate were very similar for Shanghai, Guangzhou, Shenzhen. |
| Tang 2020a | Deterministic, compartmental SEIR model, journal publication | Reducing the contact rate persistently by isolation and quarantine decreases the peak value but may either delay or accelerate the peak. Increasing the quarantine rate by 10 or 20 times will accelerate the peak by 6.5 or 9 days and will lead to a reduction of the peak value by 87% or 93% in terms of the number of infected individuals. This indicates that enhancing quarantine and isolation following contact tracing and reducing the contact rate can significantly lower the peak and reduce the cumulative number of predicted reported cases. With travel restrictions in Wuhan, in 7 days the number of infected individuals in Beijing would decrease by 91.1%. Without travel restrictions, in 7 days, the number of infected individuals in Beijing would decrease by 88.9% only if the quarantine rate is increased by 100,000 times. This means that the effect of a travel restriction in Wuhan on the infection in Beijing is almost equivalent to increasing quarantine by a baseline value of 100,000. |
| Tang 2020b | Deterministic SEIR model, journal publication | "The predicted cumulative numbers of quarantined and suspected cases seems to be stable indicating that the epidemic's peak coming soon (February)." The trends of COVID‐19 in Hubei and China depend strongly on the ratio of suspected cases identified and quarantined. |
| Tuite 2020 | Age‐structured compartmental model, journal publication | "In the model base case, 56% (95% credible interval 42%–63%) of the Ontario population would be infected." Individuals aged 5–14 years (77%, 95% credible interval 63% to 83%) and 15–49 years (63%, 95% credible interval 48% to 71%) will be the most affected. For fixed‐duration interventions, quarantine of exposed people, enhanced case detection and less aggressive physical distancing reduce the proportion of infected population at two years. Implemented dynamically, 13 months of physical distancing, cycled on and off, reduced the median overall attack rate to 2%. |
| Wang 2004 | General, deterministic model simplified to a 2‐compartment suspect‐probable model and a single‐compartment probable model, journal publication | The incidence rate is characterized by 2 stages. The first stage is the process of developing protection measures and quarantine policy, and the second stage coincides with the process of maintaining control measures. The study showed the necessity of implementing maximal control measures in the second stage for a certain period to eradicate the disease. Furthermore, the control measures in the second stage should be implemented before a threshold for the number of probable cases is reached. When protection measures are taken, and the maximal control measures are maintained (quarantine, isolation, and various protection measures), the study authors predicted there will be 41 infected individuals if 1 infected person is introduced into a susceptible population, and the number of infective individuals returns to 1 after 61 days and dies out as time evolves thereafter. If the maximal control measures are not maintained, the disease will be persistent at a level of 688 infective individuals, and there will be 1000 infective individuals on the 43rd day. |
| Wang 2020 | Susceptible‐quarantined‐infected‐removed model, journal publication | If no quarantine was taken, 10,111,537 individuals (91.1% of the Wuhan population) would be infected. Under quarantine and case isolation, social distance and use of face masks, 32,583 individuals (0.3% of the population) were infected. Reducing the duration and the start date of quarantine measures (assuming 80% quarantine rate) from 9 to 7 weeks reduced the overall attack rate from 0.3% to 0.3%. If quarantine measures started after 11 weeks, these measures would not control the outbreak. According to this model, in Italy, a quarantine policy with an effective quarantine rate of 12% and lockdown would reduce the incidence of new infections exponentially, reaching ≤ 100 in just 26 days and zero in 62days. In the UK, an effective quarantine rate of 20% would bring the incidence of new infections to under 100 in 35 days and to zero in 70 days. In the USA, a quarantine effective rate of 9% would bring the incidence of new infections to under 100 in 152 days; a rate of 20% in 65 days. |
| Wu 2020b | Susceptible‐infected‐recovered model, journal publication | Predicted infection numbers without control measures compared to actual infection numbers with control measures (timeframe 23 January to 31 January 2020): 23 January: 952 versus 495 to 31 January: 9801 versus 3215) Under weak prevention and control measures that only succeed in reducing the contact rate and infection efficiency by ≤ 45%, the study authors predict 4719 cases with 739 deaths within 3 months out of 11.5 million inhabitants in Wuhan. Under strong prevention and control measures (defined as measures that succeed to reduce the contact rate and infection efficiency by ≥ 50%) the number of infected people would be about 3088 and the death toll about 443. |
| Yip 2007 | Back‐projection method, journal publication | The overall downward trend of the infection curve corresponds well to the date when changes in the review and classification procedure were implemented by the SARS Prevention and Extrication Committee. The start of large‐scale border control and home quarantine turned out to be the major turning point for ending the outbreak in Taiwan. |
| Yue 2020 | Dynamic infectious disease model, journal publication | The study authors assume a worsening of the epidemic’s severity if the government relaxes control measures (e.g. allows travelling), while the situation can be controlled by putting strict control measures in place such as the close‐down in Wuhan. |
| Zhang 2017 | Transmission dynamics model, journal publication | Quarantining close contacts and informing the public of the actual outbreak situation could be the main countermeasures. The most effective combination of interventions is characterized by the increased quarantine in designated hospitals, self‐protection of the public to reduce the contact rate, and the quick response to symptom onset for confirmation test with implementation of appropriate isolation procedures. |
| Zhao 2020a | Susceptible‐unquarantined infected‐quarantined infected‐confirmed infected model, journal publication | Without any prevention and control measures the model predicts 802,606,289 cases in China (without Hubei) and a duration of 477 days of the epidemic. With prevention and control measures (e.g. quarantine, travel restrictions), the number of cases can decrease to 13,322 and the duration to 45 days. |
| CI: confidence interval; COVID‐19: coronavirus disease 2019; ICU: intensive care unit; MERS: Middle East respiratory syndrome; n: number of participants; NR: not reported; R0: basic reproduction number; Rt: current reproduction number; SARS: severe acute respiratory syndrome; SARS‐CoV‐2: severe acute respiratory syndrome coronavirus 2; SEIR: susceptible‐exposed‐infected‐recovered; SEIRQ: susceptible‐exposed‐infected‐recovered‐quarantined; vs: versus | ||
Overall, we identified 51 relevant studies (Arima 2020; Becker 2005; Cao 2020; Chau 2003; Choi 2020; Cowling 2020; Day 2006; Fang 2020; Ferguson 2020; Fraser 2004; Geng 2020; Gumel 2004; Gupta 2005; Hamidouche 2020; Hoertel 2020; Hou 2020; Hsieh 2005; Hsieh 2007; Hu 2020; Koo 2020; Kucharski 2020; Lee 2020; Liu 2020b; Lloyd‐Smith 2003; Lytras 2020; Madubueze 2020; Mubayi 2010; Nishiura 2004; Pandey 2020; Pang 2003; Park 2020; Peak 2017; Peak 2020; Pourbohloul 2005; Rocklöv 2020; Ryu 2020; Semenova 2020; Shen 2020; Sjödin 2020; Su 2020; Tang 2020a; Tang 2020b; Tuite 2020; Wang 2004; Wang 2007; Wang 2020; Wu 2020b; Yip 2007; Yue 2020; Zhang 2017; Zhao 2020a). Of these, 32 focused on COVID‐19 (Arima 2020; Cao 2020; Choi 2020; Fang 2020; Ferguson 2020; Geng 2020; Hamidouche 2020; Hoertel 2020; Hou 2020; Hu 2020; Koo 2020; Kucharski 2020; Lee 2020; Liu 2020b; Lytras 2020; Madubueze 2020; Pandey 2020; Peak 2020; Rocklöv 2020; Ryu 2020; Semenova 2020; Shen 2020; Sjödin 2020; Su 2020; Tang 2020a; Tang 2020b; Tuite 2020; Wang 2020; Wu 2020b; Yue 2020; Wu 2020b; Zhao 2020), 14 focused on SARS (Becker 2005; Chau 2003; Day 2006; Gumel 2004; Gupta 2005; Hsieh 2005; Hsieh 2007; Lloyd‐Smith 2003; Mubayi 2010; Nishiura 2004; Pang 2003; Wang 2004; Wang 2007; Yip 2007), three focused on SARS and other infectious diseases caused by other viruses (e.g. influenza) (Fraser 2004; Peak 2017; Pourbohloul 2005), and two focused on MERS (Park 2020; Zhang 2017).
From the 32 studies addressing COVID‐19, four were observational studies that included data on 6064 individuals and were conducted in China (Wuhan, Hong Kong), Singapore, and Greece (Arima 2020; Cowling 2020; Lee 2020; Lytras 2020). The other 28 were all modelling studies simulating outbreak scenarios for Algeria, China, Canada, Italy, Kazakhstan, Nepal, UK, USA, Singapore, South Korea, the cruise ship Diamond Princess, or for a generic population (Cao 2020; Choi 2020; Fang 2020; Ferguson 2020; Geng 2020; Hamidouche 2020; Hoertel 2020; Hou 2020; Hu 2020; Koo 2020; Kucharski 2020; Liu 2020b; Madubueze 2020; Pandey 2020; Peak 2020; Rocklöv 2020; Ryu 2020; Semenova 2020; Shen 2020; Sjödin 2020; Su 2020; Tang 2020a; Tang 2020b; Tuite 2020; Wang 2020; Wu 2020b; Yue 2020; Zhao 2020a). From the studies focusing on SARS or MERS, four were observational studies from China, South Korea, and Taiwan that included data on 178,122 individuals (Hsieh 2005; Pang 2003; Park 2020; Wang 2007). The other 15 studies on SARS or MERS were modelling studies using data from outbreaks in Canada, China, Hong Kong, Japan, South Korea, Singapore, and Taiwan (Becker 2005; Chau 2003; Day 2006; Fraser 2004; Gumel 2004; Gupta 2005; Hsieh 2007; Lloyd‐Smith 2003; Mubayi 2010; Nishiura 2004; Peak 2017; Pourbohloul 2005; Wang 2004; Yip 2007; Zhang 2017).
We judged risk of bias to be moderate for 2/3 non‐randomized studies of interventions (NRSIs) and serious for 1/3 NRSIs. We rated risk of bias moderate for 4/5 non‐controlled observational studies, and serious for 1/5. We rated modelling studies as having no concerns for 13 studies, moderate concerns for 17 studies, and major concerns for 13 studies.
Risk of bias in included studies
Of the observational studies, we rated six as having moderate risk of bias (Arima 2020; Lee 2020; Lytras 2020; Pang 2003;Wang 2007;Hsieh 2005), and two as having serious risk of bias (Cowling 2020; Park 2020). Regarding quality for 13 of the modelling studies we had no concerns to minor concerns (Day 2006; Ferguson 2020; Hoertel 2020; Gumel 2004; Koo 2020; Kucharski 2020; Mubayi 2010; Nishiura 2004; Pandey 2020; Peak 2020; Rocklöv 2020; Tang 2020a; Zhang 2017), for 18 modelling studies we had moderate concerns (Becker 2005; Cao 2020; Fang 2020; Fraser 2004; Gupta 2005; Hsieh 2007; Lloyd‐Smith 2003; Madubueze 2020; Peak 2017; Pourbohloul 2005; Semenova 2020; Shen 2020; Sjödin 2020; Su 2020; Tang 2020b; Tuite 2020; Wang 2020; Zhao 2020a), and for 12 modelling studies we had major concerns (Chau 2003; Choi 2020; Geng 2020; Hamidouche 2020; Hou 2020; Hu 2020; Liu 2020b; Ryu 2020; Wang 2004; Wu 2020b; Yip 2007; Yue 2020).
Appendix 2 and Appendix 3 present the assessment of risk of bias for the eight observational studies and Appendix 4 presents the quality rating of the 43 modelling studies.
Effects of interventions
1. Effectiveness of quarantine for individuals who were in contact with a confirmed/suspected COVID‐19 case in comparison to no quarantine (KQ1)
Direct evidence: COVID‐19
We identified one retrospective observational study assessing quarantine of individuals in Singapore (Lee 2020), and 14 modelling studies that addressed the effectiveness of quarantine for individuals who were in close contact with a COVID‐19 case (in combination with isolation of cases) for China, Singapore, South Korea, UK, the cruise ship Diamond Princess, or a generic population (Cao 2020; Ferguson 2020; Hu 2020; Hou 2020; Koo 2020; Kucharski 2020; Liu 2020b; Madubueze 2020; Peak 2020; Rocklöv 2020; Semenova 2020; Su 2020; Tang 2020a; Tang 2020b). One study used a modified individual‐based model (Ferguson 2020), one a model of individual‐level transmission stratified by setting (household, work, school, or other) (Kucharski 2020), one a contact‐network model (Liu 2020b), one a compartment model (Madubueze 2020), eight employed a susceptible–exposed–infected–recovered (SEIR) model (Cao 2020; Hou 2020; Rocklöv 2020; Peak 2020; Semenova 2020; Su 2020; Tang 2020a; Tang 2020b), one a susceptible–exposed–infected–recovered‐quarantined (SEIRQ) model (Hu 2020), and one an agent‐based influenza epidemic simulation model (Koo 2020). We report the evidence narratively.
Effectiveness
The only observational study showed that from more than 4000 close contacts that had been placed under mandatory quarantine for 14‐days up to 10 March 2020 in Singapore, eight people developed COVID‐19 (0.2%) (Lee 2020).
Semenova 2020 simulated the effect of isolation of infected people and quarantine of their family members in Kazakhstan assuming a reproduction number of 2.5. If no measures were implemented according to their model there would be 2,038,000 infected cases, 156,000 hospitalized patients, and 15,470 deaths at the peak of the outbreak. A 50% quarantine compliance could reduce the number of cases to 84,920, the number of hospitalized patients to 9310, and the number of deaths to 3750 at the peak (Semenova 2020). Koo 2020 modelled the effect of quarantine and other control strategies for Singapore and estimated that with a R0 (reproduction number) of 1.5, at day 80, isolation of infected persons and quarantine of family members reduced the number of infected individuals compared with the baseline scenario by 95.8% (Koo 2020).
The main objective of Ferguson 2020 was to compare two strategies intended to reduce transmission by limiting contacts in the general population (a mitigation versus suppression strategy) in the UK. For each strategy, the study modelled a range of non‐pharmaceutical interventions in different combinations and assessed their impacts on mortality and critical care bed requirements. The results showed that with an assumed R0 of 2.4, a combination of case isolation and voluntary quarantine for three months could prevent 31% of deaths compared with a scenario without any control measures for the epidemic (Ferguson 2020). A more recent study by Kucharski 2020 also modelled different non‐pharmacological strategies for controlling COVID‐19 in the UK assuming R0 of 2.6. The combination of case isolation and household quarantine would reduce the effective R0 by 37% (Kucharski 2020).
Six modelling studies simulated the situation in China (Cao 2020; Hou 2020; Hu 2020; Su 2020; Tang 2020a; Tang 2020b). Cao 2020 used data from the Hubei Province collected from 23 January to 24 February 2020 to build a SEIR model. The study authors did not explicitly assess the effectiveness of quarantine alone, but the impact of loosening quarantine measures that had already been in place. They concluded that if 40% fewer people were quarantined (e.g. because of less strict contact tracing), the peak number of cases would have increased two‐fold compared to keeping a full quarantine in place. Su 2020 also used data from 24 January to 23 February 2020 to simulate an adjusted SEIR model and also stated that reducing the proportion of quarantined exposed people would lead to an increase in the peak value and delay of peak time, and vice versa. Identifying contacts of cases and placing them under quarantine can greatly prevent the spread of COVID‐19 (Su 2020). The simulation by Tang 2020a aimed to estimate the basic reproduction number of SARS‐CoV‐2 and infer the required effectiveness of isolation and quarantine to contain the outbreak. Their SEIR model was based on data of confirmed cases from Wuhan collected from 10 to 20 January 2020, before the community quarantine in Wuhan. They calculated a basic R0 of 6.47 and estimated that without action the number of confirmed cases in Wuhan would be at 7723 by the end of January 2020. They calculated that a 50% reduced contact rate (achieved by isolation and quarantine) would reduce confirmed cases by 44%; reducing contacts by 90% would reduce the number of cases by 65%. Retrospectively, we know that by the end of January 2020, there were about 9000 cases, despite the community quarantine in place that started on 23 January 2020 (WHO 2020g). Tang 2020b extended their former model and predicted that numbers of quarantined and suspected cases seemed to be stable in February. The trends of COVID‐19 in Hubei and China depend strongly on the ratio of suspected cases identified and quarantined (Tang 2020b). Hu 2020 also used data from China and concluded that isolation and quarantine can effectively reduce the peak number of infected cases and delay the peak time (Hou 2020), and weaker or no quarantine may lead to an outbreak again (Hu 2020).
Madubueze 2020 and Peak 2020 simulated the effect of quarantine measures for a generic population. Madubueze 2020 simulated that without quarantine in place R0 would be 1.51, and with quarantine it would be reduced to 0.76. Also, these authors emphasize the essence of time and recommend implementing isolation, quarantine and education of the population within the first two to 10 days of the outbreak (Madubueze 2020). Peak 2020 compared quarantine of individuals with active monitoring of contacts for the mitigation of COVID‐19. They considered two settings: 1) a high‐feasibility setting with 90% contacts traced and a half‐day delay in identifying contacts and 90% effective isolation; and 2) a low‐feasibility setting with 50% of contacts traced, and on average a two‐day delay to identify contacts, and 50% effective isolation. Their simulation showed that in a high‐feasibility setting, quarantine of individuals can reduce the effective R0 to 0.57 (95% confidence interval (CI) 0.32 to 1.05), while monitoring of potentially infected people reduced R0 to 1.55 (95% CI 0.65 to 2.7), assuming a shorter serial interval of 4.8 days, hence more presymptomatic infections. With the longer time serial interval of 7.5 days (and less presymptomatic transmissions) both approaches could reduce the median effective R0 below 1 (quarantine: R0 0.49 (95% CI 0.34 to 0.97); active monitoring: R00.54 (95% CI 0.32 to 0.98). In a low‐feasibility setting, both individual quarantine and active control monitoring could not reduce the R0 below 1 for both serial interval scenarios. Individual quarantine could contain an outbreak of COVID‐19 with a short serial interval (4.8 days), but only in settings with high intervention performance, where at least 75% of infected contacts are individually quarantined. This requires that the number of cases is still traceable and resources for contact tracing are available (Peak 2020).
In their modelling study, Rocklöv 2020 used data from the Diamond Princess cruise ship. Due to the very dense population on board, the basic R0 was four times higher than in Wuhan. Isolation (i.e. removal of confirmed cases from the ship to hospitals) and quarantine of passengers that needed to stay in their cabins prevented 2307 (67%) cases, and lowered the basic R0 from 14.8 to 1.78. However, the study authors also state that early evacuation of all passengers and crew members would have prevented most infections. Liu 2020b also based their model on data from the Diamond Princess cruise ship and came to the conclusion that if no quarantine was in place all passengers would have been infected after one month. Although their calculated basic R0 differed from Rocklöv 2020, they also showed that implementing quarantine could reduce transmission from R0 6.94 to R0 0.2 (Liu 2020b).
Indirect evidence: MERS, SARS
Overall, we included three retrospective cohort studies for this question (Hsieh 2005; Pang 2003; Wang 2007), and 15 modelling studies that provided indirect evidence for KQ1 (Becker 2005; Chau 2003; Day 2006; Fraser 2004; Gumel 2004; Gupta 2005; Hsieh 2007; Lloyd‐Smith 2003; Mubayi 2010; Nishiura 2004; Peak 2017; Pourbohloul 2005; Wang 2004; Yip 2007; Zhang 2017). The cohort studies used data from Beijing and Taiwan during the SARS outbreaks in 2003. The modelling studies relied on data from SARS and MERS outbreaks in Canada, China, Hong Kong, Japan, Korea, Singapore, and Taiwan.
Effectiveness
One retrospective analysis of the SARS outbreak in Taiwan showed that out of 55,632 individuals quarantined due to contact with confirmed or probable cases, only 24 (0.04%) developed confirmed SARS (Hsieh 2005). The time from symptom onset to diagnosis was statistically significantly shorter in quarantined than in non‐quarantined people (1.20 versus 2.89 days, P = 0.0061; Hsieh 2005).
The other two retrospective data analyses from the SARS outbreaks in Beijing (Pang 2003), and Taiwan (Wang 2007), analysed the risk of actually developing a SARS infection for different subgroups who were quarantined because they had close contact with confirmed or suspected SARS cases. In Beijing, more than 30,000 close contacts were quarantined for 14 days. The majority were quarantined at home (60%), the rest at designated sites. In this cohort of quarantined individuals, the overall attack rate was 6.3%. The attack rates were highest among spouses (15.4%), other household members (8.8%), and non‐household relatives (11.6%). In these groups, the attack rates increased with the age of the close contact individual. Children younger than 10 years had an attack rate of 5.0%; adults aged 60 to 90 years had an attack rate of 27.6%. The attack rates among work and school contacts were low (0.36%; Pang 2003). The Taiwanese study confirmed the results of the analyses of the Beijing data. Among more than 55,000 quarantined people who had close contact with a SARS case, advanced age (> 60: adjusted odds ratio (aOR) 2.7, 95% CI 1.2 to 5.9) or being a family member or relative (aOR 4.7, 95% CI 2.0 to 11.0) were the main risk factors for developing SARS. Unprotected healthcare workers had the highest risk among all groups (aOR 17.5, 95% CI 6.9 to 44.1). By comparison, classmates, teachers, coworkers, and friends had no significant increase in the risk of developing SARS (aOR, 1.0 for all groups) (Wang 2007). The modelling studies combined epidemiological data from SARS and MERS outbreaks with different community characteristics. Continuous‐time or discrete‐time compartmental models were used in addition to back‐projection models and contact‐network models. Some studies considered multiple aspects of transmissibility, such as presymptomatic transmission, the contact intensity between individual people and households, the duration of infectiousness, and the host’s susceptibility to the infectious disease. Overall, the modelling studies consistently reported that quarantine was an effective measure to control SARS and MERS outbreaks. One study provided estimates of the impact of quarantine based on data from the 2003 SARS outbreak in Taiwan, where more than 55,000 individuals were quarantined because of contact with confirmed SARS cases (Hsieh 2007). The average quarantine rate in Taiwan during the outbreak, however, was estimated to be only 0.047. In other words, only one out of 21 asymptomatic individuals who should have been quarantined was indeed quarantined. Based on the study authors’ model, an increase of the quarantine rate to 0.1 would have averted 214 SARS cases and 33 deaths; an increase to 0.6 would have averted 477 SARS cases and 80 deaths. Nevertheless, even the low quarantine rate of 0.047 prevented 461 cases and 62 deaths (Hsieh 2007). Only three of these studies considered the effectiveness of quarantine in hypothetical examples that also modelled presymptomatic infectiousness (Day 2006; Fraser 2004; Peak 2017). Day 2006 used probabilistic models to determine the conditions under which quarantine is most useful. Their results indicated that the effectiveness of quarantine to reduce the number of infections depends on three main requirements: 1) that despite the implementation of isolation, a large disease R0 persists; 2) that a large proportion of infections generated by an individual could be prevented by quarantine; and 3) that there is a high probability (with a process in place, such as contact tracing) that an asymptomatic individual will be quarantined before they develop symptoms.
In the second study considering presymptomatic infectiousness, Peak 2017 found that the effectiveness of quarantine critically depends on the infectious disease’s biological dynamics (e.g. latent and infectious periods) and transmissibility. When the transmissibility is relatively low (R0 < 2.5), quarantine can control a disease, even when infectiousness precedes symptoms by several days. When transmissibility is high, and symptoms emerge long after infectiousness, quarantine will be insufficient. Using a different transmission model, Fraser 2004 reported findings consistent with those of Day 2006 and Peak 2017.
Costs
Two modelling studies assessed the costs associated with quarantine during SARS outbreaks (Gupta 2005; Mubayi 2010). Gupta 2005 compared the costs of two scenarios. In scenario A, SARS could be transmitted throughout the population without major public health interventions in place (only infected people are isolated). In scenario B, the early quarantine of first‐degree contacts of the index case was implemented to contain the virus. The model used data from the SARS outbreak in Toronto, Canada. To assess the economic impact of both scenarios, they considered direct costs (e.g. hospitalisation, administrative effort) and indirect costs (e.g. lost productivity). Depending on the transmission rate (8% to 25%), the costs of an epidemic without implementing quarantine vary. A transmission rate of 8% means that out of 100 contacts, eight get the infection; a transmission rate of 25% means that 25 contacts are infected. Aggregating primary, secondary, tertiary, and quaternary infections results in 4681 (with an 8% rate) to 406,901 infections (with a 25% rate). The direct and indirect costs of the disease would then range from CAD 72.0 to 25.4 million (reference year 2003). The study authors concluded that at a transmission rate of 8%, the quarantine costs would range between CAD 12.2 to 17.0 million, depending on the timing with which the quarantine measurements were effectively implemented. The total savings varied between CAD 279 to 232 million. The earlier effective quarantine measures are implemented, the greater the savings are.
Mubayi 2010 developed a general contact‐tracing model for the transmission of an infectious disease similar to SARS. They performed a cost‐analysis for various quarantine strategies combined with a fixed isolation strategy. They focused on direct costs allocated by public health authorities and present their analysis as incremental costs per infection prevented and lives saved. In strategy 1, a maximum quarantine effort at a per‐capita rate independent of the number of infected cases is in place. In strategy 2, the quarantine effort was proportional to the outbreak size, while in strategy 3, the quarantine process depended on the outbreak size, but was constrained by resource limitations. Contact tracing is assumed to happen randomly in the model, while in reality, this would depend on having contact with confirmed or suspected cases, so the model might overestimate the quarantine costs.
The study authors recommend using a combination of quarantine and isolation. Although isolation alone might be sufficient to control a SARS outbreak, it is too expensive and resource‐intensive, as isolation costs more than quarantine and it takes time to build isolation facilities. Therefore, a combination of quarantine and isolation is more beneficial than a single control measure. The optimal approach depends on available resources and the ability to quickly identify epidemiological factors, such as infectiousness or susceptibility during an outbreak to determine what quarantine and isolation combination is the best. Quarantine becomes less important the faster infectious patients are detected and isolated. Conversely, simulations show that the total cost is dominated by quarantine costs for a low contact‐tracing efficiency and by isolation at a high contact‐tracing efficiency. This means increasing the quarantine effort always results in lower overall costs over the entire outbreak. Strategy 1 was the most effective in decreasing the time to extinction but led to more cases, deaths, and people being isolated, though fewer were quarantined. Strategy 2 was the most cost‐effective strategy when comparing the cost of achieving a unit of health benefit (e.g. reduction of a case) and the cost of the quarantine/isolation strategies. The study authors stress that the greatest need for resources is early in the outbreak.
Table 3 summarizes the certainty of evidence for KQ1.
2. Comparative effectiveness of different types of quarantine (KQ1a)
A prospective cohort study from Korea followed 116 haemodialysis patients who had to be quarantined because they were exposed to individuals with confirmed MERS infections (Park 2020). For a mean of 15 days, they underwent different types of quarantine: single‐room quarantine (n = 54), cohort quarantine (n = 46), and self‐imposed quarantine (n = 16). None of the patients developed MERS symptoms, and no secondary transmission occurred. Because of the study’s small sample size, we are unable to draw any conclusions about the comparative effectiveness of the different quarantine types.
3. Effectiveness of quarantine in combination with other measures to contain a COVID‐19 outbreak in comparison to no prevention and control measures or other measures without quarantine (KQ1b)
Direct evidence: COVID‐19
Effectiveness
One observational study (Cowling 2020), and 15 modelling studies addressed the effectiveness of quarantine in combination with other measures to contain the COVID‐19 outbreak (Choi 2020; Fang 2020; Ferguson 2020; Geng 2020; Hamidouche 2020; Hoertel 2020; Koo 2020; Pandey 2020; Shen 2020; Sjödin 2020; Tuite 2020; Wang 2020; Wu 2020b; Yue 2020; Zhao 2020a; see Table 6). One study used an individual‐based transmission model developed for pandemic influenza to explore the effectiveness of different physical distancing measures for the UK (Ferguson 2020), one study used a susceptible‐exposed‐infected‐hospitalized‐recovered model to simulate the situation for South Korea (Choi 2020). One study used the Alg‐COVID‐19 model and focused on Algeria (Hamidouche 2020), one used a stochastic agent‐based microsimulation model to simulate the situation for New York (USA) (Hoertel 2020), Sjödin 2020 used a SEIR model for Italy. Pandey 2020 used an age‐structured SEIR model for Nepal, Koo 2020 used an agent‐based influenza epidemic simulation model for Singapore, and Tuite 2020 used an age‐structured compartmental model to simulate the situation in Canada. The other modelling studies were based on data from China: one study used a susceptible, unquarantined infected, quarantined infected, confirmed infected model (Zhao 2020a), one used a dynamic disease model (Yue 2020), one used a dynamic compartmental model (Shen 2020), one a susceptible‐infected‐quarantined‐recovered (SIQR) model (Wang 2020), the other three studies used SEIR models (Fang 2020; Geng 2020; Wu 2020b).
The only observational study looking at quarantine in combination with other measures reported that as of 31 March 2020, 715 cases of SARS‐CoV‐2 infection were confirmed in Hong Kong, of which 621 infections were symptomatic and 94 asymptomatic. The combination of public health measures (isolation of cases and quarantine of their contacts, quarantine of travellers, population behaviour changes, such as physical distancing, personal protective measures and travel restrictions) was associated with reduced spread of COVID‐19. However, the authors were not able to disentangle the specific effects of each measure (Cowling 2020).
Overall, the modelling studies conclude that quarantine in combination with other non‐pharmaceutical methods is more effective than no interventions and also than quarantine alone.
Tuite 2020 aimed to analyse how different non‐pharmaceutical control measures can contribute to control COVID‐19 and reduce burden on the healthcare system. They employed an age‐structured compartmental model of COVID‐19 transmission suited for the population in Ontario, Canada. In their base case scenario (limited testing, isolation, quarantine) 56% (95% credible interval 42% to 63%) of the Ontario population would be infected within two years. At the epidemic peak they estimate 107,000 cases in hospitals and 55,500 additional cases in intensive care units (ICUs). For fixed‐duration interventions, quarantine of exposed people, enhanced case detection and less aggressive physical distancing reduce the proportion of the infected population at two years. Implemented dynamically, 13 months of physical distancing, cycled on and off, reduced the median overall attack rate to 2%. The authors emphasize the important role of physical distancing and conclude that a dynamic approach that is turned on and off, depending on a threshold of current cases, could be sufficient to keep ICU resources from being overwhelmed compared to fixed‐duration interventions (Tuite 2020). Koo 2020 compared quarantine in combination with other control measures with quarantine alone using an agent‐based influenza epidemic simulation model for Singapore. While isolation of infected persons and quarantine of family members reduced the number of infected individuals compared with the baseline scenario by 95.8%*, quarantine plus school closure and workplace distancing reduced the median cumulative number of infections 96.4% and 98.57%*, respectively (*self‐calculated percentages by review authors). The combination of all interventions reduced the median cumulative infection count by 99.3%* from the baseline scenario (assuming R0 1.5, at day 80) (Koo 2020). Pandey 2020 used an age‐structured SEIR model to simulate the outbreak situation for Nepal. They estimated the peak at 100 days without any interventions and the demand for ICU beds to exceed supply in Kathmandu by a factor of 25. A lockdown would delay the peak but not make any difference to the number of deaths or ICU beds needed. Control strategies that are focused on active case findings and isolating/quarantining (exposed and infectious) individuals for one year after one month of lockdown would reduce mortality by 27% and demand for health care by 50%. Physical distancing for one year after a one‐month lockdown that reduces contact rates by 35%, would reduce mortality by 33% and the need for ICU beds by 63%. The most efficient measure would be the combination of physical distancing and casefinding + isolation/quarantine after one month of lockdown, reducing the number of projected deaths by 99.6%, healthcare demand would drop similarly (Pandey 2020).
Ferguson 2020 showed that with an assumed R0 of 2.4, a combination of case isolation and voluntary quarantine for three months, and physical distancing of people 70 years or older for four months, could prevent 49% of deaths. The need for critical care beds could be reduced by 67% with a combination of case isolation, voluntary quarantine, and physical distancing of people 70 years or older. The combination of case isolation, household quarantine, physical distancing of the entire population, and school and university closures would achieve the greatest effect (data in the pre‐report not plausible) and could reduce the R0 close to 1. Effects would become apparent approximately three weeks after implementation, and as long as measures are in place. The study authors point out, however, that the more successful a strategy is at temporary suppression, the larger the later epidemic is predicted to be because of the lower build‐up of herd immunity (Ferguson 2020). Kucharski 2020 also modelled different strategies to control COVID‐19 in the UK and found that the combination of self‐isolation of cases, household quarantine of contacts, manual and app‐based contact tracing of all contacts and limiting contacts to four people a day seemed to be most efficient, and reduced the effective R0 by 66%. Combining case isolation, quarantine, and manual contact tracing (without limiting contacts and app‐based contact tracing) was also effective and reduced the effective R0 by 64% (instead of a 37% reduction with isolation + quarantine alone). The authors emphasize that physical distancing does not only reduce the number of transmissions but also the number of unknown contacts, making contact tracing more feasible. A strategy that was not considerably less effective was mass testing of 5% of the population per week. This only resulted in reducing the effective R0 by 2%. For contact tracing the authors recommend tracing and testing of contacts of suspected cases, not only confirmed cases, due to the pre‐symptomatic transmission for SARS‐CoV‐2 (Kucharski 2020).
Wang 2020 created a SIQR model based on data from Wuhan. They simulated the effect of contact tracing and quarantine on top of physical distancing and compulsory face masks. While face masks and physical distancing capped the growth rate of infections per day, only adding contact tracing and quarantine could completely stop the outbreak. The model showed that without quarantine 10,111,537 individuals in Wuhan would have been infected (91%), but with the control measures in place the number of infected individuals was 32,582 (0.3% of the Wuhan population). Essential for effective quarantine is early implementation. Implementing quarantine 11 weeks after the outbreak started, it would not be able to control the outbreak. According to this model, in Italy a quarantine policy with an effective quarantine rate of 12% and lockdown would reduce the incidence of new infections exponentially, reaching ≤ 100 in just 26 days and zero in 62 days. In the UK, an effective quarantine rate of 20% would bring the incidence of new infections to under 100 in 35 days and to zero in 70 days. In the USA, an effective quarantine rate of 20% would reduce the incidence of new infections to around 100 in 65 days. When comparing diverse lockdown exit strategies the authors conclude that at a low level of cases, contact tracing and quarantine could be as effective as a lockdown and compulsory face masks.
One study simulated the outbreak for South Korea and estimated that there would be nearly 5 million COVID‐19 cases without any measures. By implementing prevention and control measures (not further specified) that are able to reduce the transmission rate by 90% or 99%, the number of COVID‐19 cases would be only a fraction, at 0.5% or 0.4%, respectively (Choi 2020). Another study focused on the outbreak in Algeria in their simulation, and postulated that implementing the strategy (isolation of cases and 14‐day quarantine of contacts and travellers, physical distancing, movement restriction, and lockdown) has prevented 2993 COVID‐19 cases (1914 instead of 4907 cases) within 7 days. The average R0 over the first 42 days of the epidemic was 2.28 (95% CI 1.85 to 2.71) and the current reproduction number (Rt) after implementing preventive measures was 1.25 (95% CI 1.19 to 1.31) (Hamidouche 2020). The five Chinese modelling studies concluded that the key to controlling COVID‐19 is to focus on early and strict prevention and control measures. According to the studies, only comprehensive measures can achieve a reduction in transmission of SARS‐CoV‐2 (Fang 2020; Geng 2020; Yue 2020; Wu 2020b; Zhao 2020a). One of these studies predicted that without implementation of any measures, China (without Hubei) would have had more than 800 million COVID‐19 cases and an epidemic duration of 477 days. With prevention and control measures, such as isolation, quarantine, and travel restrictions in place, not only could the number of cases be reduced, but the duration of the outbreak could also be reduced (Zhao 2020a).
Community quarantine
Four studies specifically assessed the effects of community quarantine which is usually accompanied by other non‐pharmaceutical measures (Geng 2020; Hoertel 2020; Shen 2020; Sjödin 2020). We defined community quarantine as placing individuals in a defined region under quarantine and not allowing people to leave this area or external people to enter this area. This is similar to a lockdown, while as lockdown we defined "stay‐at‐home" orders for whole countries, not just specific regions or cities.
Hoertel 2020 simulated the impact of community quarantine for New York. Without community quarantine in place the model estimated about 30,000 deaths in New York. Quarantine of all New Yorkers was very efficient to contain the viral spread, but it is probably insufficient to prevent a second epidemic peak once lifted. Different durations of quarantine (4 to 16 weeks) had no effects on the endpoints (cumulative incidence, mortality, ICU beds needed). The authors state that a two‐step quarantine lifting according to age, (i.e. a three‐week quarantine for all individuals aged < 70 years and an additional eight‐week quarantine period for people aged > 70 years), would lower the cumulative incidence by 23% and the cumulative mortality by 68%, compared to a 16‐week quarantine followed by a lifting for all individuals. Lowering the age cut‐off to 60 years would additionally reduce mortality by 3%; the cumulative incidence would be similar, but even fewer ICU beds would be needed (Hoertel 2020). Sjödin 2020 focused on the situation in Italy and modelled the effectiveness of community quarantine in North Italy by degree of compliance and household size. For a six‐person household and no quarantine adherence, the model predicted 43 new cases over 14 days. While for a single household with full adherence, no secondary cases were predicted. This means that higher adherence and smaller quarantine units help to minimise the number of secondary cases over the 14‐day period (Sjödin 2020).
Shen 2020 estimated in their model for Hubei province (China) that without the metropolitan‐wide quarantine, the epidemic would result in 491,320 (331,470 to 651,180) infected cases and 15,907 (10,950 to 20,865) deaths. Community quarantine could prevent 79.3% (75.1% to 83.45%) of deaths, and 87.1% (84.7% to 89.5%) of infections in public spaces and 71.8% (66.4 to 77.3%) of infections in households. Geng 2020 also based their analysis on data from Wuhan and reported that community quarantine and school closures reduced the peak of transmissions by 45.7% and 29.9%, respectively.
Costs
We did not identify any studies assessing any costs of quarantine in combination with other measures to control a COVID‐19 outbreak.
Indirect evidence: SARS
modelling studies also combined epidemiological data from MERS or SARS outbreaks with different community characteristics. Mostly, they used static models that assumed a constant risk of infection and did not consider the effects of disease control programmes. Some studies considered multiple aspects of transmissibility, such as presymptomatic transmission, the contact intensity between individual people and households, the duration of infectiousness, and the host’s susceptibility to the infection. In general, they confirmed that a combination of quarantine with other interventions is effective to reduce the transmission of MERS and SARS.
Table 4 summarizes the certainty of evidence for KQ1b.
4. Effectiveness of quarantine for individuals travelling from a country with a declared COVID‐19 outbreak compared to no quarantine (KQ2)
Direct evidence: COVID‐19
Effectiveness
We identified two observational studies on quarantine for individuals travelling from a country with a declared COVID‐19 outbreak and one modelling study. Arima 2020 assessed repatriates from China (Hubei Province), Lytras 2020 observed travellers from the UK, Spain, and Turkey.
The repatriates from Hubei Province arrived in Japan at the end of January 2020 (Arima 2020). At that time, the outbreak was largely centred around Hubei Province, with about 1300 newly‐reported cases per day (WHO 2020h). From 566 travellers arriving in Japan, 12 had COVID‐19 (2.1%). Seven of them were identified by entry screening upon arrival, but five were missed; only by placing them under quarantine could the infection chain be stopped (Arima 2020).
The prevalence of SARS‐CoV‐2 cases was higher in travellers from the UK, Spain, and Turkey (Lytras 2020). Between 20 to 25 March, flights from London, Barcelona, Madrid, and Istanbul arrived in Greece. All but one person from Spain were free of symptoms at arrival and placed under 14‐day quarantine. From 357 travellers from the UK, 13 were Sars‐CoV‐2 positive (3.6%, 95% CI 2.0 to 6.1). From 394 travellers from Spain, 25 were positive (6.3%, 95% CI 4.1 to 9.2), as were two of 32 returnees from Turkey (6.3%, 0.9 to 20.8). On 20 March 2020, the UK reported about 700 new cases per day, Spain 2800 new cases per day, and Turkey nearly 500 new cases per day (WHO 2020i). Overall, 52 out of 1349 travellers were positive in the identified observational studies (Arima 2020; Lytras 2020).
Ryu 2020 modelled how cases imported by students from China might effect South Korea. They used a SEIRQ model for the epidemic and assessed the impact of compliance with home quarantine among students arriving from China to South Korea. They estimated that the number of infected individuals would be 184 to 277 from 13 March to 26 March with the arrival of 0.1%, 0.2%, and 1% of pre‐infectious students in South Korea. They also estimated that at that time 184 to 248 of students would be under quarantine. The higher the compliance of quarantine, the smaller the number of infected individuals. The authors concluded that epidemics by incoming international students from China are unlikely to occur in South Korea, if the quarantine programme is in place and compliance is between 70% to 100% (Ryu 2020).
Costs
We did not identify any studies assessing any costs of quarantine for travellers from regions with high SARS‐CoV‐2 transmission rates.
Indirect evidence: SARS
We identified two observational studies (Hsieh 2005; Wang 2007), and two modelling studies (Hsieh 2007; Yip 2007), assessing the effectiveness of quarantine for people travelling from countries with a declared SARS outbreak.
Effectiveness
Two retrospective analyses (Hsieh 2005; Wang 2007), and two modelling studies (Hsieh 2007; Yip 2007), addressed the effectiveness of quarantine to reduce transmissions from individuals who travelled from regions with a declared outbreak. Hsieh 2005, Hsieh 2007 and Wang 2007 used data from the 2003 SARS outbreak in Taiwan during which the Taiwanese government home quarantined more than 95,000 travellers arriving at the borders from affected regions. Most quarantined people were confined to their homes for 10 to 14 days. While Wang 2007 reported that 56 of 95,271 quarantined people developed SARS, Hsieh 2005 reported that 0 out of 95,828 quarantined travellers developed SARS, indicating some inconsistency in the used data. Hsieh 2007 employed a susceptible‐infected‐recovered model with an estimated case‐fatality rate of 14.1%; the mean time of symptom onset to diagnosis were 1.20 days for the quarantined individuals and 2.89 days for those unquarantined. The results of the model showed that in the hypothetical scenario in which no one had been quarantined after arrival from a high‐transmission region, 511 additional SARS cases with 70 additional deaths would have occurred in Taiwan. In the database, 17 unquarantined imported cases could be traced (missed cases and cases before the quarantine was implemented). If all 17 unquarantined imported cases had been quarantined, 280 SARS cases and 48 deaths could have been averted. Based on their data source, out of the more than 95,000 quarantined people, only two developed SARS. If these two individuals had not been quarantined, 29 additional cases and five deaths would have occurred. The study authors acknowledge that caution should be exercised when viewing the numbers because the model did not account for the super‐spreading events that occurred in Taiwan.
Using data from Taiwan, Yip 2007 employed a back‐projection model without providing effect estimates for quarantine. The study authors state that the model confirms the effectiveness of quarantine measures in Taiwan, including the implementation of quarantine for travellers from regions with a declared outbreak.
Costs
We did not identify any studies assessing any costs of quarantine for travellers from regions with a declared outbreak.
Table 5 presents the certainty of evidence ratings for KQ2.
5. Comparative effectiveness of quarantine of travellers (KQ2a)
We did not identify any studies assessing comparative effectiveness of diverse types of quarantine for travellers from regions with a declared outbreak.
Discussion
This is an update of a recent rapid systematic evidence synthesis on the effectiveness of quarantine measures for COVID‐19. Within only two months, 22 additional studies on quarantine for COVID‐19 have been made publicly available (as journal papers or pre‐prints). Although the evidence base has doubled, it is still limited because most studies on COVID‐19 are mathematical modelling studies that make different assumptions on important model parameters. None of the observational studies on COVID‐19 have a control group and the risk of bias for these studies is moderate to serious. The other 19 included studies are on SARS and MERS and contribute only indirect evidence.
Nevertheless, modelling studies on COVID‐19 consistently reported a benefit of the simulated quarantine measures. For example, quarantine of people exposed to confirmed cases averted a high proportion of infections and deaths compared to no measures (low‐certainty evidence). Very low‐certainty of evidence indicated that the earlier that quarantine measures are implemented, the greater are the cost savings; however, this evidence is based on the SARS outbreak. Recent studies on quarantine of travellers showed that the proportion of travellers developing COVID‐19 while placed under quarantine was higher than in the SARS studies (Arima 2020; Hsieh 2005; Lytras 2020; Wang 2007). Considering that quarantine of travellers already showed a small positive effect during SARS, the higher prevalence of COVID‐19 among quarantined travellers from countries with a declared outbreak and high community transmission rates indicates that this strategy can be helpful in stopping the further spread of COVID‐19 in a country with low community transmission rates (very low‐certainty evidence). In general, the combination of quarantine with other prevention and control measures, such as physical distancing, face masks and others had a greater effect on the reduction of transmissions, cases, and deaths than individual measures (low‐certainty evidence). Studies on SARS and MERS are consistent with findings from the studies on COVID‐19.
A recently published pre‐print analysed 4579 non‐pharmaceutical interventions implemented in 76 territories (Haug 2020). Researchers showed that the effectiveness of interventions varies across countries, depending on the economic status and government dimensions, indicating that there is no "one size fits all" strategy, and a combination of non‐pharmaceutical interventions is more effective than single measures to control COVID‐19. In their analysis, quarantining people was relatively ineffective, but they used data from March to April 2020 when most countries had transmission rates that were too high to be able to identify all contacts and implement effective quarantine (Haug 2020).
Although more comprehensive and strict prevention and control measures are more effective in containing the COVID‐19 outbreak, at some point the incremental effect of adding another restrictive measure is only minimal and must be weighed up against the unintended negative effects that accompany it, such as the social and economic consequences on communities that have been subject to extended periods of physical distancing, and other prevention and control measures, that might lead to an increase in the burden on health overall. In order to maintain the best possible balance of measures, decision makers must constantly monitor the outbreak situation and the impact of the measures implemented.
Quarantine alone is an important component of outbreak control but seems not to be enough to contain COVID‐19. Preliminary estimates of the basic reproduction number (R0) of SARS‐CoV‐2 range from 2.8 to 5.5 (Read 2020; Zhao 2020; Zhou 2020b). Models have shown that the effectiveness of quarantining individuals during outbreaks of diseases with presymptomatic infectiousness and a basic reproduction number of greater than 2.5 is limited. Based on estimates of a basic R0 of 3.11 (95% CI 2.39 to 4.13), Read 2020 state in their pre‐print, that to stop the increase of COVID‐19 infections, 58% to 76% of the transmissions must be averted by control measures. In a situation with pre‐ or even asymptomatic infectiousness it is difficult to identify and isolate all cases and to place contacts of cases under quarantine early enough to reduce transmission markedly. So to some extent the effectiveness of quarantine is closely linked to effective contact tracing and adherence of the population to quarantine.
Limitations in the body of evidence
The best available direct evidence at the present time is from four observational studies that assessed how many people under quarantine developed COVID‐19 and 28 mathematical modelling studies that used current, but still variable estimates of the transmissibility, incubation period, and pathogenicity of SARS‐CoV‐2 to simulate the epidemic, and determine the transmission dynamics and the effects of various interventions to control the outbreak. The basic R0 in these models, for example, ranged from 0.5 to 7.2. Important parameters that are still largely unknown but have a substantial impact on results of models, are the time of asymptomatic infectiousness and the proportion of unidentified infected individuals. Ferguson 2020, for example, assumed that infectiousness occurs only 12 hours prior to the onset of symptoms and that two‐thirds of cases are symptomatic. In other models, study author assumptions were substantially different. For example, Cao 2020 assumed no asymptomatic infectiousness at all before onset of symptoms, Sjödin 2020 and Tuite 2020 assumed infectiousness 24 to 36 hours before symptom onset.
The majority of included studies on quarantine in combination with other non‐pharmaceutical interventions does not allow us to disentangle the effect of quarantine or the other specific measures. This makes it difficult to conclude what combination of methods is the best to reduce the number of cases and deaths and delay the outbreak. What most studies agree on is that it is essential to start with control measures early in the pandemic when numbers of cases are still low, to keep the outbreak under control. Many countries had implemented lockdowns within the lasts months, substantially reducing the number of cases. This gives countries the opportunity to find cases and their contacts and place them under quarantine in a timely manner. However, these measures are resource‐intensive and not feasible for all countries (Peak 2020).
Limitations of the review
Because of time constraints, we conducted a rapid review and abbreviated certain methodological steps of the review process. We used Cochrane Crowd to screen abstracts. This approach is still experimental, but the author team verified the decisions of the Crowd, therefore we are very confident that we did not miss important studies. In addition, single review authors rated risk of bias, conducted data extraction and rated certainty of evidence. A second review author checked the plausibility of decisions and the correctness of data. Because these steps were not conducted dually and independently, we introduced some risk of error to this rapid review. Nevertheless, we are confident that none of these methodological limitations would change the overall conclusions of this review. As no validated 'Risk of bias' checklist for mathematical transmission models was available, we only assessed whether the model was dynamic, whether the study authors conducted uncertainty analyses on key model parameters and assumptions, and whether the results provided estimates of the change in the burden of infection due to the intervention. We selected these three criteria because they best reflected methodological decisions that have an impact on results and conclusions. Although we are confident that the use of a more comprehensive tool would not affect our quality ratings markedly, we recommend to use a more formal and comprehensive tool for the next update of this review.
This review focused on transmission, mortality reduction and costs of quarantine, because the WHO expert panel selected these outcomes. We did not include the psychological impact of quarantine on individuals, because this was addressed recently in a rapid review (Brooks 2020). However, we focused on studies available in databases, so government papers and other potentially relevant grey literature are not included in this review. While we believe this has no impact on outcomes of effectiveness, this might have led to not finding all available relevant information on costs of quarantine. In addition, there may be other health and economic adverse effects resulting from quarantine that have not been assessed by this review (e.g. quality of life, healthcare demand, number of people placed unnecessarily under quarantine, unemployment, domestic violence). For these reasons, our review is unable to address the question of when quarantining and other public health measures aiming to reduce the spread of COVID‐19 should be relaxed or lifted. It is also important to highlight that we did not subject the two modelling studies reporting on costs to specific critical appraisal for economic evaluations, and we did not attempt to draw conclusions regarding the relative costs or efficiency of quarantine alone or in combination with other public health measures compared to no such interventions or single public health measures. For future updates, we will critically appraise studies on resource use for economic evaluations.
Due to the urgency of the topic we decided to include pre‐prints. These publications have not yet undergone peer review. However, since we assessed the risk of bias of these studies we feel that the benefits of including the data from these pre‐prints in our review outweighs the risks.
Authors' conclusions
Implications for practice
Despite the limited evidence on quarantine to control COVID‐19, studies consistently concluded that quarantine is an important public health measure to reduce the number of people infected and the number of deaths. For both effectiveness and costs, early and efficient implementation of quarantine seems to be key. The combination of quarantine with other prevention and control measures showed the greatest effect in reducing transmissions, incident cases, and mortality. In order to maintain the best possible balance of measures, decision makers must constantly monitor the outbreak situation and the impact of the measures implemented.
Implications for research
Further research on important disease dynamics of COVID‐19, such as prevalence, or case‐fatality rate are crucial. Testing in representative samples in different settings could help assess the true prevalence of infection, which would greatly reduce uncertainty of model simulations. Consequently, modelling studies simulating the effectiveness of control measures to contain COVID‐19 could be updated as soon as new knowledge on important parameters is available. More non‐randomized studies of interventions that assess the effectiveness of quarantine alone or in combination with other public health measures to control COVID‐19 are also needed. Comparing the effectiveness of diverse strategies will help us gain more evidence for future pandemics. Essential for future research is to disentangle the effects of diverse prevention and control measures to know which interventions or combinations work best and cost less in terms of the economic and health burden on society. Therefore non‐randomized studies with robust quasi‐experimental designs are preferred to observational studies, since the former (but not the latter) can in principle enable causal inferences to be drawn about effects of quarantine measures and other prevention and control measures (Rockers 2015).
What's new
| Date | Event | Description |
|---|---|---|
| 15 September 2020 | Amended | Cochrane Crowd added to Acknowledgements |
History
Review first published: Issue 4, 2020
| Date | Event | Description |
|---|---|---|
| 27 August 2020 | New citation required and conclusions have changed | Review updated from original review published on 8 April 2020. 22 new studies included. |
| 27 August 2020 | New search has been performed | Updated search identified 22 new included studies. |
| 29 June 2020 | Amended | Amended funding statement and added disclaimer statement to the Acknowledgements section |
| 29 June 2020 | Amended | Corrected funding source name to University for Continuing Education Krems ‐ Danube University Krems |
| 7 May 2020 | Amended | Minor typographical amendments. Addition of affiliation to Acknowledgements |
Acknowledgements
We would like to thank Susan Norris from the World Health Organization (WHO) for valuable feedback on the original manuscript. Furthermore, we would like to thank Helen Wakeford and Toby Lasserson for editing the review, Sarah Hodgkinson and Tess Moore for methodological feedback, Robin Featherstone for peer review of the original search and for conducting the updated search, Denise Mitchell for transferring the document from Word to Review Manager 5, drafting a Plain Language Summary, and copyediting the original review, and Clare Dooley for copyediting the updated review. We would also like to thank Beate Jahn, and Gaby Sroczynski from UMIT ‐ University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria for advice on how to classify modelling studies, Petra Wellemsen for administrative support throughout this project, and Genevieve Iseult Eldredge and Dawn Gartlehner for editing and proofreading the original manuscript. We also want to thank Xuan Yu of the Evidence‐based Medicine Centre, Lanzhou University, China, for translating the Chinese language studies into English. In addition, we would like to thank Cochrane Editors Sarah Hodgkinson and Lisa Bero, and peer referees Ian Shemilt, Nathan Kapata, Dale Fisher and Doug Salzwedel for their valuable comments. We would also like to thank Claudia Christof who participated in the original review, but not in this update.
We would like to acknowledge and thank the following people for their help in assessing the search results for this review via Cochrane Crowd: Sunday Onagbiye, Marlon L. Bayot MPH RMT, Ya‐Ying Wang, Caroline Meijdam, Susanna Wisniewski, Dorothy Halfhide, Hariklia Nguyen, Ana‐Marija Ljubenković, Sarah Barter Godfrey, Stella Le, Dulce Estêvão, Mohammad Aloulou, Constantine Ezeme, Chloe Thomson, Sarah Moore, Bert Dhondt, Elizabeth Stovold, Nuno Fernandes, Shireen Rafeeq, Danielle Johnson, Joanna Thompson‐Coon, Kit Byatt, Pedro Lobos, Nikolaos Sideris, Renato Brandi Pereira Carneiro, Vinayak Mishra, Sayel Albasha, Nandini Suresh Theodoros Aslanidis, Carrie Dickson, Basavaraj Poojar, Louise Murphy, Neelakanta Reddy Buchireddygari, Therese Dalsbø, Ursula Ellis, Bernardo Costa, Jade Scott, Brian Duncan, Andrew Ying, Emmy Ingle, Iltimass Gouazar, Julia Robertson, Patrick Wilson and Irena Ilic.
This rapid review was undertaken by the Department for Evidence‐based Medicine and Evaluation at University for Continuing Education Krems ‐ Danube University Krems, which is a WHO Collaborating Centre, and it is not a publication of the WHO. The review authors are responsible for the views expressed in this publication, and they do not necessarily represent the decisions or policies of the WHO.
The editorial base of the Cochrane Infectious Diseases Group is funded by UK aid from the UK government for the benefit of low‐ and middle‐income countries (project number 300342‐104). The views expressed do not necessarily reflect the UK government's official policies.
Appendices
Appendix 1. Search strategy for the update
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) 1946 to June 22, 2020
Date search conducted: June 23, 2020
Strategy:
1 exp Coronavirus/ (17477)
2 exp Coronavirus Infections/ (16923)
3 COVID‐19.rs. (7278)
4 severe acute respiratory syndrome coronavirus 2.os. (6086)
5 (2019 nCoV or 2019nCoV or 2019‐novel CoV).ti,ab,kf. (892)
6 (Coronavir* or corona virus* or Middle East Respiratory Syndrome or MERS or Severe Acute Respiratory Syndrome or SARS).ti,ab,kf. (34149)
7 COVID 19.mp. (24452)
8 (COVID19 or COVID 2019).ti,ab,kf. (426)
9 (nCov 2019 or nCov 19).ti,ab,kf. (54)
10 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").mp. (7844)
11 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").mp. (7757)
12 or/1‐11 [Set 1: COVID‐19] (51237)
13 quarantine/ (2334)
14 patient isolation/ (3881)
15 Hospitals, Isolation/ (104)
16 quarantin*.ti,ab,kf. (5305)
17 (isolat* adj2 (exposed or contact? or suspected or healthy or human? or people or person? or men or man or wom?n or child* or community or case? or infected or patient?)).ti,ab,kf. (80858)
18 (isolation adj2 (ward? or unit? or hospital? or room? or cohort or facilit* or area? or practice? or strateg* or procedure? or precaution?)).ti,ab,kf. (8281)
19 (lockdown? or lock‐down?).mp. (806)
20 ((travel* or mobility or movement) adj2 restrict*).mp. (3800)
21 travel ban?.mp. (55)
22 cordon? sanitaire?.mp. (24)
23 sanitary barrier?.mp. (21)
24 (contain* adj3 (communit* or geograph* or area* or local* or urban or region*)).mp. (39155)
25 or/13‐24 [Set 2: Quarantine] (140865)
26 and/12,25 [Sets 1 and 2] (2551)
27 limit 26 to "humans only (removes records about animals)" (2450)
28 limit 27 to yr="2002 ‐Current" (2416)
29 remove duplicates from 28 (2323)
Database: Ovid Embase 1996 to 2020 Week 25
Date search conducted: June 23, 2020
Strategy:
1 coronaviridae/ (942)
2 exp coronavirinae/ (14305)
3 exp coronavirus/ (14305)
4 exp coronavirus infection/ (14690)
5 (2019 nCoV or 2019nCoV or 2019‐novel CoV).ti,ab,kw. (771)
6 (coronavir* or corona virus* or 'middle east respiratory syndrome' or mers or 'severe acute respiratory syndrome' or sars).ti,ab,kw. (32068)
7 COVID 19.af. (21139)
8 (COVID19 or COVID 2019).ti,ab,kw. (359)
9 (nCov 2019 or nCov 19).ti,ab,kw. (25)
10 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").af. (6308)
11 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").af. (5590)
12 or/1‐11 [Set 1: COVID‐19] (50483)
13 exp quarantine/ (1718)
14 exp isolation/ (1919)
15 quarantin*.ti,ab,kw. (4701)
16 (isolat* adj2 (exposed or contact or suspected or healthy or human* or people or person* or men or man or wom#n or child* or community or case* or infected or patient*)).ti,ab,kw. (84798)
17 (isolation adj2 (ward* or unit* or hospital* or room* or cohort or facilit* or area* or practice* or strateg* or procedure* or precaution*)).ti,ab,kw. (7442)
18 (lockdown or lock down).ti,ab,kw. (584)
19 ((travel* or mobility or movement) adj2 restrict*).ti,ab,kw. (4143)
20 travel ban*.ti,ab,kw. (54)
21 cordon* sanitaire*.ti,ab,kw. (17)
22 sanitary barrier*.ti,ab,kw. (27)
23 (contain* adj3 (communit* or geograph* or area* or local* or urban or region*)).ti,ab,kw. (31962)
24 or/13‐23 [Set 2: Quarantine] (134106)
25 and/12,24 [Sets 1 and 2] (2688)
26 (animal experiment/ or exp animal/) not exp human/ (3152639)
27 25 not 26 (2609)
28 27 not conference abstract.pt. (2550)
29 limit 28 to yr="2002‐current" (2520)
30 remove duplicates from 29 (2490)
Database: CINAHL (Ebsco) 1981 to Jun 24, 2020
Date search conducted: June 24, 2020
Strategy:
| S1 | (MH "Coronavirus+") | Search modes ‐ Boolean/Phrase | (1,042) |
| S2 | (MH "Coronavirus Infections+") | Search modes ‐ Boolean/Phrase | (4,339) |
| S3 | TI ("2019 nCoV" OR "2019nCoV" OR "2019‐novel CoV") OR AB ("2019 nCoV" OR "2019nCoV" OR "2019‐novel CoV") | Search modes ‐ Boolean/Phrase | (7) |
| S4 | TI (Coronavir* OR "corona virus*" OR "Middle East Respiratory Syndrome" OR MERS OR "Severe Acute Respiratory Syndrome" OR SARS) OR AB (Coronavir* OR "corona virus*" OR "Middle East Respiratory Syndrome" OR MERS OR "Severe Acute Respiratory Syndrome" OR SARS) | Search modes ‐ Boolean/Phrase | (6,543) |
| S5 | TI ("COVID 19" OR COVID19 OR "COVID 2019") OR AB ("COVID 19" OR COVID19 OR "COVID 2019") | Search modes ‐ Boolean/Phrase | (119) |
| S6 | TI ("nCov 2019" OR "nCov 19") OR AB ("nCov 2019" OR "nCov 19") | Search modes ‐ Boolean/Phrase | (1) |
| S7 | TI ("SARS‐CoV‐2" OR "SARS‐CoV2" OR SARSCoV2 OR "SARSCoV‐2") OR AB ("SARS‐CoV‐2" OR "SARS‐CoV2" OR SARSCoV2 OR "SARSCoV‐2") | Search modes ‐ Boolean/Phrase | (740) |
| S8 | TI ("SARS coronavirus 2" OR "SARS‐like coronavirus" OR "Severe Acute Respiratory Syndrome Coronavirus‐2") | Search modes ‐ Boolean/Phrase | (8) |
| S9 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 | Search modes ‐ Boolean/Phrase | (8,367) |
| S10 | (MH "Patient Isolation") | Search modes ‐ Boolean/Phrase | (2,644) |
| S11 | (MH "Quarantine") | Search modes ‐ Boolean/Phrase | (680) |
| S12 | TI quarantin* OR AB quarantin* | Search modes ‐ Boolean/Phrase | (688) |
| S13 | TI isolation OR AB isolation | Search modes ‐ Boolean/Phrase | (24,699) |
| S14 | TI (isolat* N1 (exposed OR contact OR suspected OR healthy OR human# OR people OR person# OR men OR man OR wom#n OR child* OR community OR case# OR infected OR patient#)) OR AB (isolat* N1 (exposed OR contact OR suspected OR healthy OR human# OR people OR person# OR men OR man OR wom#n OR child* OR community OR case# OR infected OR patient#)) | Search modes ‐ Boolean/Phrase | (10,101) |
| S15 | TI (lockdown OR "lock down") OR AB (lockdown OR "lock down") | Search modes ‐ Boolean/Phrase | (252) |
| S16 | TI ((travel* OR mobility OR movement) N1 restrict*) OR AB ((travel* OR mobility OR movement) N1 restrict*) | Search modes ‐ Boolean/Phrase | (1,064) |
| S17 | TI "travel ban#" OR AB "travel ban#" | Search modes ‐ Boolean/Phrase | (36) |
| S18 | TI cordon# sanitaire# OR AB cordon# sanitaire# | Search modes ‐ Boolean/Phrase | (6) |
| S19 | TI "sanitary barrier#" OR AB "sanitary barrier#" | Search modes ‐ Boolean/Phrase | (0) |
| S20 | TI (contain* N2 (communit* OR geograph* OR area* OR local* OR urban OR region*)) OR AB (contain* N2 (communit* OR geograph* OR area* OR local* OR urban OR region*)) | Search modes ‐ Boolean/Phrase | (1,233) |
| S21 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 | Search modes ‐ Boolean/Phrase | (37,904) |
| S22 | S9 AND S21 | Search modes ‐ Boolean/Phrase | (731) |
| S23 | S9 AND S21 |
Limiters ‐ Published Date: 20000101‐20201231 Search modes ‐ Boolean/Phrase |
(729) |
Database: Cochrane COVID‐19 Study Register
URL:https://covid-19.cochrane.org/ (searched via the Cochrane Register of Studies: https://crsweb.cochrane.org/)
Date search conducted: June 24, 2020
Strategy:
(quarantin* OR isolat* OR cordon* OR lockdown OR "lock down" OR cordon* OR "community containment" OR "containment area"):TI,AB (1102)
RMF note: Content: The Cochrane COVID‐19 Study Register contains study references from ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), PubMed, medRxiv and other hand‐search articles from publishers' websites.
Database: WHO COVID‐19 Global literature on coronavirus disease
URL:https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/
Date search conducted: June 21, 2020
Strategy:
quarantin* OR isolat* OR cordon* OR lockdown OR "lock down" OR cordon* OR "community containment" OR "containment area" (3358)
RMF note: Content: The WHO Global COVID‐19 Health literature database contains primarily research (published AND/OR pre‐publication) journal articles from PubMed, Web of Science, Global Index Medicus, Embase. In addition, Lanzhou University submits on a daily basis citations from CNKI as well as a number of Chinese journal publishers.
Source: Google Scholar
URL: https://scholar.google.com/
Date search conducted: June 24, 2020
Strategy:
10.1002/14651858.CD013574
> Cited by 73 (unique 71)
For details on the original search strategy see Nussbaumer‐Streit 2020.
Appendix 2. Risk of bias assessment of non‐randomized observational studies of interventions based on ROBINS‐I
| Author and year | Bias due to confounding | Bias in selection of participants into the study | Bias in classification of interventions | Bias due to deviations from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported result | Overall risk of bias |
| Hsieh 2005 | Moderate | Low | Low | Low | Moderate | Moderate | Low | Moderate |
| Park 2020 | Serious | Low | Low | Low | Moderate | Moderate | Low | Serious |
| Wang 2007 | Moderate | Low | Low | Low | Moderate | Moderate | Low | Moderate |
Appendix 3. Risk of bias assessment of single‐arm observational studies of interventions
| Internal validity | External validity | ||||||||
| Author and year | Selection bias (representative: yes/no) | Attrition bias (adequate: yes/no) | Detection bias (blind: yes/no) | Confounding (adjustment for other factors: yes/no | Reporting bias (well defined: yes/no) [study group] | Reporting bias (well defined: yes/no) [follow‐up] | Reporting bias (well defined: yes/no) [outcome] | Analyses (well defined: yes/no) | Overall risk of bias |
| Arima 2020 | yes | yes | unclear | unclear | yes | yes | yes | yes | Moderate |
| Cowling 2020 | yes | yes | unclear | unclear | yes | yes | yes | no | Serious |
| Lee 2020 | yes | yes | unclear | unclear | yes | yes | yes | yes | Moderate |
| Lytras 2020 | yes | yes | unclear | unclear | yes | yes | yes | yes | Moderate |
| Pang 2003 | yes | yes | unclear | yes | yes | yes | yes | yes | Moderate |
Appendix 4. Quality rating of the modelling studies based on three best practice recommendations from ISPOR
| Author and year | Was the model a dynamic (transmission) model? | Did the authors conduct uncertainty analyses on key assumptions that may have had an impact of the conclusions? | Do the results provide estimates of the change in the burden of infection due to the intervention? | Quality |
| Becker 2005 | Yes | Unclear | Unclear | Moderate concerns |
| Cao 2020 | Yes | Unclear | Unclear | Moderate concerns |
| Chau 2003 | Yes | No | Unclear | Major concerns |
| Choi 2020 | Unclear | No | Unclear | Major concerns |
| Day 2006 | Yes | Yes | Yes | No concerns to minor concerns |
| Fang 2020 | Yes | Yes | Unclear | Moderate concerns |
| Ferguson 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Fraser 2004 | Yes | Unclear | Unclear | Moderate concerns |
| Geng 2020 | Yes | No | Yes | Major concerns |
| Gumel 2004 | Yes | Yes | Yes | No concerns to minor concerns |
| Gupta 2005 | Unclear | Yes | Yes | Moderate concerns |
| Hamidouche 2020 | Unclear | Yes | No (only very limited) | Major concerns |
| Hoertel 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Hou 2020 | Yes | Yes | No | Major concerns |
| Hsieh 2007 | Yes | Unclear | Yes | Moderate concerns |
| Hu 2020 | Yes | Yes | No (only very limited) | Major concerns |
| Koo 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Kucharski 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Liu 2020b | Yes | Yes | No (only very limited) | Major concerns |
| Lloyd‐Smith 2003 | Yes | Yes | Unclear | Moderate concerns |
| Madubueze 2020 | Yes | Yes | Unclear | Moderate concerns |
| Mubayi 2010 | Yes | Yes | Yes | No concerns to minor concerns |
| Nishiura 2004 | Yes | Yes | Yes | No concerns to minor concerns |
| Pandey 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Peak 2017 | Yes | Unclear | Yes | Moderate concerns |
| Peak 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Pourbohloul 2005 | Yes | Yes | Unclear | Moderate concerns |
| Rocklöv 2020 | Yes | Yes | Yes | No concerns to minor concerns |
| Ryu 2020 | Yes | Unclear | No (only very limited) | Major concerns |
| Semenova 2020 | Yes | No | Yes | Major concerns |
| Shen 2020 | Yes | Unclear | Yes | Moderate concerns |
| Sjödin 2020 | Yes | Unclear | Yes | Moderate concerns |
| Su 2020 | Yes | Unclear | Yes | Moderate concerns |
| Tang 2020a | Yes | Yes | Yes | No concerns to minor concerns |
| Tang 2020b | Yes | Unclear | Yes | Moderate concerns |
| Tuite 2020 | Yes | Unclear | Yes | Moderate concerns |
| Wang 2004 | Yes | Unclear | No | Major concerns |
| Wang 2020 | Unclear (but missing compartment E is an issue) | Yes | Yes | Moderate concerns |
| Wu 2020b | Yes | No | Yes | Major concerns |
| Yip 2007 | Yes | No | Unclear | Major concerns |
| Yue 2020 | Yes | No | Yes | Major concerns |
| Zhang 2017 | Yes | Yes | Yes | No concerns to minor concerns |
| Zhao 2020a | Yes | Yes | Unclear | Moderate concerns |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arima 2020.
| Study characteristics | ||
| Study design | Cohort study (single‐arm, not controlled) | |
| Objectives | To review the screening and quarantine measures of returnees from Wuhan (China) | |
| Study details | Japan, n = 566 returnees from Wuhan | |
| Interventions | Entry screening (n = 566):
|
|
| Notes | ||
Becker 2005.
| Study characteristics | ||
| Study design | Modelling study Transmission model R0 = 6; infectious period 9 days; incubation period 6.5 days |
|
| Objectives | To determine to which extent the interventions reduce the effective reproduction number and which intervention requirements are necessary to achieve elimination of the disease | |
| Study details | Data from SARS outbreak 2003 in Singapore and Hong Kong and the Australian census 2001 n = NR | |
| Interventions |
|
|
| Notes | ||
Cao 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model R0 = 2; considers transmission risk during incubation period; does not consider asymptomatic patients |
|
| Objectives | To simulate the effect of the decrease in the proportion of follow‐up quarantine on the development of the epidemic after governmental prevention and control measures have been in place | |
| Study details | Data from COVID‐19 outbreak in the Hubei Province from 23 January 2020 to 24 February 2020 n = 59.17 million | |
| Interventions |
|
|
| Notes | ||
Chau 2003.
| Study characteristics | ||
| Study design | Modelling study Back‐projection method R0 = NR; incubation period 6.37 days (SD 4.09), time from onset of clinical symptoms to admission to hospital differs from time to time (3.67 to 4.85 days) |
|
| Objectives | To estimate the SARS infection curve and assess the effectiveness of interventions | |
| Study details | Data from the SARS outbreak in Hong Kong, 1 March 2003 to 24 June 2003 n = NR | |
| Interventions |
|
|
| Notes | ||
Choi 2020.
| Study characteristics | ||
| Study design | Modelling study Susceptible‐exposed‐infected‐hospitalized‐recovered model R0 = 3.48 to 3.54; transmission period 2 to 4 days |
|
| Objectives | To estimate and evaluate the effectiveness of preventive measures using mathematical modelling | |
| Study details | Data from COVID‐19 outbreak in South Korea (Daegu and North Gyeongsang) between 20 January and 4 March 2020 n = NR | |
| Interventions |
|
|
| Notes | ||
Cowling 2020.
| Study characteristics | ||
| Study design | Cohort study (single‐arm, not controlled) | |
| Objectives | To examine the effect of non‐pharmaceutical interventions and behavioral changes of the public on the incidence of COVID‐19 and influenza virus infections | |
| Study details | Hong Kong, n = 715 | |
| Interventions |
|
|
| Notes | ||
Day 2006.
| Study characteristics | ||
| Study design | Modelling study Probabilistic model R0 = 3; infectious period 8 days; latent period 6.4 days; transmission rate 0.375 |
|
| Objectives | To determine factors that make quarantine an effective control measure for some diseases but not for others | |
| Study details | Data based on other mathematical models and epidemiological studies of SARS n = NR | |
| Interventions |
|
|
| Notes | ||
Fang 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model R0 = NR; probability of infection per exposure 10%; frequency of exposure 10; incubation period 7 days; average recovery time 10.25 days |
|
| Objectives | To simulate the spread dynamics of a COVID‐19 outbreak and the impact of different control measures, to conduct a sensitivity analysis to identify the key factor(s), to plot the trend curve of the effective reproduction number, and to perform data fitting after the simulation | |
| Study details | Data from COVID‐19 outbreak in China and former studies concerning COVID‐19 n = 1,000,000 Population consistent with the size of Wuhan city | |
| Interventions |
|
|
| Notes | ||
Ferguson 2020.
| Study characteristics | ||
| Study design | Modelling study Modified, individual‐based simulation model R0 = 2 to 2.6 (2.4 at baseline); incubation period 5.1 days; mean infectious period 6.5 days; symptomatic individuals are 50% more infectious than asymptomatic individuals |
|
| Objectives | To assess the impact of nonpharmaceutical interventions on the death rate and the peak healthcare demand during a COVID‐19 epidemic | |
| Study details | Setting: UK Data based on census data to define age and household distribution size, data on average class sizes and staff‐student ratios, data on the distribution of workplace size n = NR |
|
| Interventions |
|
|
| Notes | ||
Fraser 2004.
| Study characteristics | ||
| Study design | Modelling study Model of infectious disease outbreak dynamics of several pathogens Various R0 and incubation period depending on the pathogen |
|
| Objectives | To identify the general properties of emerging infectious agents that determine the likely success of isolating symptomatic individuals and tracing and quarantining their contacts | |
| Study details | Data based on other mathematical models, the analysis of clinical patient records and case studies of 4 known pathogens: SARS, HIV, pandemic influenza, smallpox n = NR | |
| Interventions |
|
|
| Notes | ||
Geng 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model R0 ≈ 2.38 to 2.72 |
|
| Objectives | To model the transmission process of SARS‐CoV‐2 | |
| Study details | Data from National Bureau of Statistics of the People’s Republic of China (population of Wuhan at the end of 2018) n = 8.8 million | |
| Interventions |
|
|
| Notes | ||
Gumel 2004.
| Study characteristics | ||
| Study design | Modelling study Deterministic model R0 = 4.8, 3.6, 5.04, and 4.91; rate of development of clinical symptoms 0.1 and 0.125 |
|
| Objectives | To examine the impact of isolation and quarantine on the control of SARS and cumulative deaths | |
| Study details | Data from WHO and epidemiological studies (outbreaks in Toronto, Beijing, Hong Kong, Singapore) n = NR | |
| Interventions |
|
|
| Notes | ||
Gupta 2005.
| Study characteristics | ||
| Study design | Modelling study Mathematic and health economic model R0 = NR; transmission rate of infection 0.08, 0.15 and 0.25; incubation period 10 days |
|
| Objectives | To estimate the economic effects of an epidemic, the number of averted infections, the direct and indirect costs of quarantine, and the total savings | |
| Study details | Data from other researchers, the popular press, and interviews about the SARS outbreak in Toronto 2003 n = NR | |
| Interventions |
|
|
| Notes | ||
Hamidouche 2020.
| Study characteristics | ||
| Study design | Modelling study Alg‐COVID‐19 model based on three parameters: average R0 = 2.55 (95% CI 2.17 to 2.92), serial interval (SI = 4.4) and the prediction time (t) |
|
| Objectives | To assess the preventive strategy adopted in Algeria and to estimate the number of COVID‐19 cases avoided by these measures | |
| Study details | Algerian Ministry of Health 2020 and official media in (APS), Algeria 25 February to 19 April 2020, n = NR | |
| Interventions |
|
|
| Notes | ||
Hoertel 2020.
| Study characteristics | ||
| Study design | Modelling study Stochastic agent‐based microsimulation model R0 = 2.79 |
|
| Objectives | To evaluate the potential impact of conditions of quarantine measures against COVID‐19 on disease’s cumulative incidence and mortality, and on ICU‐bed occupancy | |
| Study details | Based data from the US Census Bureau and from the Department of Health of the New York State; New York City, n = 500,000 (extrapolated to 8.5 million) | |
| Interventions |
|
|
| Notes | ||
Hou 2020.
| Study characteristics | ||
| Study design | Modelling study A well‐mixed SEIR compartmental model, assumption: contact rate of latent individuals is between 6 and 18 |
|
| Objectives | To explore the effectiveness of the quarantine of Wuhan city against the COVID‐19 epidemic | |
| Study details | Data of the Health Commission of Wuhan City, the Health Commission of Hubei Province, the National Health Commission of the People's Republic of China, and the WHO situation reports; Wuhan city, n = 11,081,000 | |
| Interventions |
|
|
| Notes | ||
Hsieh 2005.
| Study characteristics | ||
| Study design | Cohort study (non‐randomized controlled study of intervention) | |
| Objectives | To evaluate the effectiveness of quarantine in reducing the time from onset to diagnosis and the time from diagnosis to classification | |
| Study details | SARS‐positive patients, previously quarantined or not quarantined during the 2003 outbreak Setting: Taiwan n = 480 | |
| Interventions |
|
|
| Notes | Case definition: confirmed cases had clinical diagnosis and positive laboratory test for SARS‐CoV‐2 | |
Hsieh 2007.
| Study characteristics | ||
| Study design | Modelling study SEIR model with additional compartments R0 = NR; daily infection rate 0.347 (95% CI 0.31 to 0.38) |
|
| Objectives | To assess the impact of quarantine on preventing additional SARS cases and additional deaths | |
| Study details | Data from Taiwan Center for Disease Control, SARS database (SARS outbreak in Taiwan 2003) n = 151,460 | |
| Interventions |
|
|
| Notes | ||
Hu 2020.
| Study characteristics | ||
| Study design | Modelling study Susceptible, exposed, infectious, removed, quarantined susceptible, quarantined exposed, quarantined infectious model (SEIRQ) R0 = NR |
|
| Objectives | To evaluate the effect of input population and quarantine strategies on the disease variations, including peak values of cumulative confirmed cases, daily new increased confirmed cases and confirmed cases of COVID‐19, and corresponding times | |
| Study details | The Health Commission of Guangdong Province, the Health Commission of Hubei Province, the National Health Commission of the People’s Republic of China; January 27 to February 20, 2020; n = 113,460,000 |
|
| Interventions |
|
|
| Notes | ||
Koo 2020.
| Study characteristics | ||
| Study design | Modelling study Agent‐based influenza epidemic simulation model (FluTE, stochastic), parameters: 7.5% asymptomatic infected people, incubation period 5.3 days, asymptomatic individuals were 50% less infectious then symptomatic patients R0 = 1.5, R0 = 2.0, R0 = 2.5 |
|
| Objectives | To investigate options for early intervention in Singapore if local containment measures are unsuccessful | |
| Study details | Data of Singapore Census of Population 2010 and several public sources (e.g. Report on registration of births and deaths 2010); Singapore, n = 3,770,000 | |
| Interventions | Quarantine is defined as quarantine of family members of infected persons; four intervention scenarios:
|
|
| Notes | ||
Kucharski 2020.
| Study characteristics | ||
| Study design | Modelling study individual‐level transmission model stratified by setting (household, work, school, or other), secondary attack rate of 20% for households and 6% for all contacts Overall R = 2.6 in the baseline scenario |
|
| Objectives | To estimate reduction in transmission under different control measures across settings and how many contacts would be quarantined per day in different strategies for a given level of symptomatic case incidence | |
| Study details | Data of the BBC Pandemic Dataset 2018 UK, n= 40,162 | |
| Interventions | Quarantine of exposed individuals (within the household or via other contact) Interventions:
|
|
| Notes | ||
Lee 2020.
| Study characteristics | ||
| Study design | Cohort study (single‐arm, not controlled) | |
| Objectives | To show that Singapore’s strategy of using a comprehensive surveillance system has been effective in containing spread of COVID‐19 | |
| Study details | Singapore, n = 4000 | |
| Interventions |
|
|
| Notes | ||
Liu 2020b.
| Study characteristics | ||
| Study design | Modelling study Contact network mode Stage 1: unprotected contact: average transmissibility t = 0.026, R0 = 6.94 Stage 2a: protected contact for the crew Stage 2b: airborne spread for passengers |
|
| Objectives | To reconstruct unprotected, protected contact, and airborne spread to simulate the two‐stages outbreak of COVID‐19 on the 'Diamond Princess' cruise ship | |
| Study details | Data of National Institute of Infectious Diseases of Japan and indirect information of the SARS outbreak in Amoy Gardens of Hong Kong; cruise ship, stage 1: 20 January to 4 February; stage 2: 5 to 19 February n = 3711 | |
| Interventions |
|
|
| Notes | ||
Lloyd‐Smith 2003.
| Study characteristics | ||
| Study design | Modelling study Stochastic model R0 ranging from 1.5 to 5; mean incubation period 4.5 days; mean symptomatic period 16.3 days (SD 7.3 days) |
|
| Objectives | To address the relative benefits of case isolation, quarantine, hospital‐wide contact precautions and reduced HCW‐community mixing for SARS | |
| Study details | Data source = NR n = 100,000 individuals and a hospital of 3000 individuals | |
| Interventions |
|
|
| Notes | ||
Lytras 2020.
| Study characteristics | ||
| Study design | Cohort study (single‐arm, not controlled) | |
| Objectives | To review the screening and quarantine of repatriated persons from European countries to Greece | |
| Study details | Greece, repatriated travellers from the UK, Spain and Turkey, n = 783 | |
| Interventions |
|
|
| Notes | ||
Madubueze 2020.
| Study characteristics | ||
| Study design | Modelling study Compartment model, Compartments: susceptible, exposed, quarantined, infectious not hospitalized, hospitalized/isolated infectious and recovered |
|
| Objectives | To study the effect of different control strategies as time‐dependent interventions | |
| Study details | Parameter values and initial conditions from the literature on COVID‐19, SARS and MERS, n = 12,000,000 | |
| Interventions |
|
|
| Notes | ||
Mubayi 2010.
| Study characteristics | ||
| Study design | Modelling study Dynamical model, cost‐effectiveness model R0 = 3.22; mean infectious period 28.4 days; mean incubation period 6.37 days |
|
| Objectives | To compare three different quarantine strategies implemented alongside a single isolation strategy, with resource allocation modelled in terms of simple cost functions | |
| Study details | Data from SARS outbreaks in Hong Kong (census data from 2001 to 2004 in Hong Kong City) and related studies n = NR | |
| Interventions |
|
|
| Notes | ||
Nishiura 2004.
| Study characteristics | ||
| Study design | Modelling study Deterministic mathematical model R0 = 3; in sensitivity analysis various R0 (depending on the effectiveness of the quarantine and of the precautionary measures) |
|
| Objectives | To predict the epidemiological outcomes and assess the effect of any specified control strategy on SARS | |
| Study details | Data from SARS outbreak in Hong Kong and epidemiological data from other countries n = NR | |
| Interventions |
|
|
| Notes | ||
Pandey 2020.
| Study characteristics | ||
| Study design | Modelling study Age‐structured SEIR model with heterogeneous mixing to estimate epidemic burden due to COVID‐19 in Kathmandu Model was parameterized using published estimates of COVID‐19 epidemic dynamics; R0 = 2.4, incubation period 3 days; infectious duration 7 days |
|
| Objectives | To assess the potential effects of implementing control interventions: a lockdown, physical distancing, or aggressive testing and contact tracing with quarantine | |
| Study details | Limited resource settings, hypothetical COVID‐19 epidemic in Kathmandu (population 2.6 million), Nepal | |
| Interventions |
|
|
| Notes | ||
Pang 2003.
| Study characteristics | ||
| Study design | Cohort study (single‐arm, not controlled) | |
| Objectives | To describe and evaluate measures undertaken to control the SARS outbreak: quarantine among other things | |
| Study details | Individuals with close contact to SARS patients who were quarantined Setting: Beijing n = 30,000 | |
| Interventions | Quarantine of individuals who were in close contact with infected people | |
| Notes | Case definition ‐ cases had to meet one of the three following categories:
|
|
Park 2020.
| Study characteristics | ||
| Study design | Cohort study (non‐randomized controlled study of intervention) | |
| Objectives | To evaluate the effects of different quarantine strategies on the prevention and rate of secondary viral transmission | |
| Study details | Patients from 3 haemodialysis units exposed to MERS during the 2015 outbreak Setting: Korea n = 116 | |
| Interventions |
|
|
| Notes | Case definition: to confirm cases serologic analysis were performed Potential bias: allocation to type of quarantine was based on disease severity |
|
Peak 2017.
| Study characteristics | ||
| Study design | Modelling study Agent‐based branching model of several pathogens Parameters depend on the type of disease, e.g. SARS: R0 = 2.9 (95% CI 2.2 to 3.6) Incubation period 4.01 days Maximum duration of infectiousness 21.6 days |
|
| Objectives | To identify which disease characteristics and intervention attributes are most critical in deciding between quarantine and symptom monitoring and to provide a general framework for understanding the consequences of isolation policies during emerging epidemics | |
| Study details | Data from other case studies of 7 known pathogens (Ebola, hepatitis A, influenza A, MERS, pertussis, SARS, smallpox) n = NR | |
| Interventions |
|
|
| Notes | ||
Peak 2020.
| Study characteristics | ||
| Study design | Modelling study Stochastic SEIR model, sequential Monte Carlo algorithm R0 = 2.20 Incubation periode 4.14 days; serial interval distribution: 4.8 days and 7.5 days |
|
| Objectives | To evaluate the comparative efficacy of individual quarantine and active monitoring of contacts to control SARS‐CoV‐2 |
|
| Study details | NR | |
| Interventions |
|
|
| Notes | ||
Pourbohloul 2005.
| Study characteristics | ||
| Study design | Modelling study Urban contact network model Mildly contagious disease R0 = 1.545 Moderately contagious disease R0 = 5.047 |
|
| Objectives | To assess a population’s vulnerability to an infectious disease based on the structure of the network and on the average transmissibility of the disease | |
| Study details | Publicly available data from sources such as Statistics Canada n = 10,308 (2000 households) | |
| Interventions |
|
|
| Notes | ||
Rocklöv 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model Initial R0 = 14.8; infectious period 10 days; incubation period 5 days |
|
| Objectives | To estimate the basic reproduction number under cruise ship conditions and the response effectiveness of the quarantine and removal interventions, and to compare scenarios of an earlier and later evacuation of the ship | |
| Study details | Based on confirmed cases of COVID‐19 on the Diamond Princess cruise ship 21 January 2020 to 20 February 2020 n = 3700 | |
| Interventions |
|
|
| Notes | ||
Ryu 2020.
| Study characteristics | ||
| Study design | Modelling study SEIRQ model, R0 = 2.68, 0.1%, 0.2%, or 1% were in the preinfectious period of COVID‐19 infection, latent period 6.5 days |
|
| Objectives | To estimate the number of infected persons in Seoul based on incoming international students from China (no COVID‐19 transmission within the community of Seoul) | |
| Study details | Data source NR, Seoul (South Korea), n = 9,740,000 | |
| Interventions |
|
|
| Notes | ||
Semenova 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model R0 = 2.5 Incubation period 5 days, maximum time of forecast: 200 days; mild infection duration 4 days, critical infection duration 15 days |
|
| Objectives | To report on the rates of COVID‐19 in the Republic of Kazakhstan and to predict the effect of quarantine on cases, deaths, and recoveries, as well as to forecast the demand on HCWs | |
| Study details | Website of Republican Center for Health Development; 13 March 2020 to 28 May 28 2020, n = 18,654,000 | |
| Interventions | Quarantine measures:
|
|
| Notes | ||
Shen 2020.
| Study characteristics | ||
| Study design | Modelling study Dynamic compartmental model R0 = NR |
|
| Objectives | To evaluate the impact of the metropolitan‐wide quarantine on the trend and transmission route of the SARS‐CoV‐2 epidemic | |
| Study details | The Health Commission of Hubei Province 15 January 2020 to 8 April 2020 n = NR | |
| Interventions |
|
|
| Notes | ||
Sjödin 2020.
| Study characteristics | ||
| Study design | Modelling study SEIR model Standard reproductive rate was set within a houshold to 2.1 and public locations in the community to 0.27. Incubation period: 5 days, latent period: 4 days, infectious period 2 days |
|
| Objectives | To investigate the extent of physical distancing needed to effectively control the outbreak in a lockdown situation in a small size town setting typical of Italy | |
| Study details | The model was parameterized to COVID‐19 based on published data on incubation time and infectious period. City with a population of 5000, Italy | |
| Interventions |
|
|
| Notes | ||
Su 2020.
| Study characteristics | ||
| Study design | Modelling study Adjusted SEIR model R0 = 1.75 to 2.91 |
|
| Objectives | To estimate COVID‐19 development in four high‐risk metropolitan areas of China: Beijing, Shanghai, Guangzhou, and Shenzhen | |
| Study details | Data of cases reported in Beijing, Shanghai, Guangzho and Shenzhen from 24 January 2020 to 23 February 2020 to estimate the likely number of infections | |
| Interventions |
|
|
| Notes | ||
Tang 2020a.
| Study characteristics | ||
| Study design | Modelling study Deterministic, compartmental SEIR model R0 = 6.47; incubation period 7 days |
|
| Objectives | To estimate the basic reproduction number of SARS‐CoV‐2 and infer the required effectiveness of isolation and quarantine to prevent an outbreak | |
| Study details | Based on confirmed COVID‐19 cases in Wuhan, China from 10 January 2020 to 22 January 2020 n = 11,081,000 | |
| Interventions |
|
|
| Notes | ||
Tang 2020b.
| Study characteristics | ||
| Study design | Modelling study (extension of the model developed in Tang 2020a by new compartments, more data on quarantined and suspected cases) Deterministic SEIR model based on the clinical progression of the disease, epidemiological status of the individuals, and intervention measure estimates based on transmission dynamics models |
|
| Objectives | To evaluate a dynamic model with suspected compartments incorporating prevention and control strategies to predict the trend of the COVID‐19 epidemic based on multiple data sources and assess the efficacy of control strategies | |
| Study details | Data of laboratory‐cofirmed COVID‐19 cases in China from the National Health Commission of the People's Republic of China and the Hubei's Health Commission n = NR | |
| Interventions |
|
|
| Notes | ||
Tuite 2020.
| Study characteristics | ||
| Study design | Modelling study Age‐structured compartmental model R0 = 2.3, latent period 2.5 days, presymptomatic period 1 day |
|
| Objectives | To evaluate the applicability of different nonpharmaceutical interventions to control COVID‐19 pandemic and reduce the burden on the healthcare system | |
| Study details | Ottawa: Statistics Canada; 2019 (2019 population estimates) n = NR | |
| Interventions |
|
|
| Notes | ||
Wang 2004.
| Study characteristics | ||
| Study design | Modelling study General, deterministic model, simplified to a 2‐compartment suspect‐probable model and a single‐compartment probable model R0 = varies from 1.1 to 3.3 |
|
| Objectives | To predict future incidence and simulate the impact of additional control strategies by studying the transmission dynamics of the spread of SARS in Beijing | |
| Study details | Daily reported cases by the Ministry of Health of the People's Republic of China n = NR | |
| Interventions |
|
|
| Notes | ||
Wang 2007.
| Study characteristics | ||
| Study design | Cohort study (non‐randomized controlled study of intervention) | |
| Objectives | To identify risk factors for the development of SARS among quarantined people | |
| Study details | Individuals with known or suspected (travellers coming from SARS‐affected areas) exposure to infected people during the 2003 outbreak Setting: Taiwan n = 147,526 | |
| Interventions |
|
|
| Notes | Case definition: cases were classified according to the WHO case definition in suspected, probable, and laboratory‐confirmed cases | |
Wang 2020.
| Study characteristics | ||
| Study design | Modelling study Susceptible‐quarantined‐infected‐removed model R0 = NR, social transmissibility factor 5.8 (under normal social circumstance), and 1.4 (after lockdown), incubation period 5 days |
|
| Objectives | To analyse the impact and repercussions of the surge in healthcare demand in response to the COVID‐19 pandemic, assess the potential effectiveness of various infection/disease control measures, and make projections on the best approach to exit from the current lockdown | |
| Study details | Demographic and COVID‐19 epidemiological data in Wuhan; 8 December 2019 to 8 March 2020 n = 11.10 million | |
| Interventions |
|
|
| Notes | ||
Wu 2020b.
| Study characteristics | ||
| Study design | Modelling study Susceptible–infected–recovered model R0 = 2.9 and 3.6; infectious period 14 days |
|
| Objectives | To predict the outcome of prevention and control measures of diverse intensity in Wuhan | |
| Study details | Official data from COVID‐19 outbreak in Wuhan n = 1,500,000 (inhabitants of Wuhan) | |
| Interventions | Combination and different intensity of:
|
|
| Notes | ||
Yip 2007.
| Study characteristics | ||
| Study design | Modelling study Back‐projection method R0 = 2.9 and 3.6; infectious period 14 days |
|
| Objectives | To reconstruct the infection curve for the 2003 SARS epidemic in Taiwan and to ascertain the temporal changes in the mean daily number of infections that occurred during the course of the outbreak | |
| Study details | Taiwan Center for Disease Control and the WHO n = NR | |
| Interventions |
|
|
| Notes | ||
Yue 2020.
| Study characteristics | ||
| Study design | Modelling study Dynamic infectious disease model R0 = NR |
|
| Objectives | To develop a model to predict the future trend of the epidemic, introducing a quarantine rate parameter to the model | |
| Study details | Numbers of confirmed cases and cures published by the Chinese National Health Committee n = NR | |
| Interventions |
|
|
| Notes | ||
Zhang 2017.
| Study characteristics | ||
| Study design | Modelling study Transmission dynamics model R0 ranged from 2.5 to 7.2; incubation period 7.5 days; no asymptomatic transmission |
|
| Objectives | To estimate the transmissibility of MERS and identify the effective countermeasures that stopped its spread | |
| Study details | Outbreak data released by Korea Centers for Disease Control and Prevention n = NR | |
| Interventions |
|
|
| Notes | ||
Zhao 2020a.
| Study characteristics | ||
| Study design | Modelling study Susceptible, unquarantined infected, quarantined infected, confirmed infected model R0 ranged between 0.48 and 5.93 |
|
| Objectives | To characterise the dynamics of COVID‐19 in China and whether control and prevention measures are effective | |
| Study details | Model uses data on COVID‐19 confirmed cases from China, 20 January to 21 February 2020 n = 187,009 | |
| Interventions |
|
|
| Notes | ||
CI: confidence interval; COVID‐19: coronavirus disease 2019; HCW: healthcare workers; ICU: intensive care unit; MERS: Middle East respiratory syndrome; NR: not reported; PCR: polymerase chain reaction; RT‐PCR: reverse transcription polymerase chain reaction; SARS: severe acute respiratory syndrome; SARS‐CoV‐2: severe acute respiratory syndrome coronavirus 2; SD: standard deviation; SEIR: susceptible‐exposed‐infected‐recovered; SEIRQ: susceptible‐exposed‐infected‐recovered‐quarantined; WHO: World Health Organization
Differences between protocol and review
In the original version of this rapid review (Nussbaumer‐Streit 2020), we limited searches to English and Chinese only. Because COVID‐19 is now affecting the whole world, we did not apply any language restrictions when updating the review.
In the original review we only screened 30% of abstracts dually. For the update we screened abstracts with support from Cochrane Crowd. Records where three independent Crowd members agreed on, were only screened by one review author, others were screened dually.
In the original review we searched different databases and the World Health Organization (WHO) conducted a search in Chinese databases. Since new COVID‐19 specific registries have emerged, we adapted the sources searched for this update. We also contacted experts to identify additional studies this time.
We included studies on SARS and MERS, due to the limited evidence on COVID‐19. For this update we included only studies on COVID‐19. We retained the SARS and MERS studies from the former version of the review and differentiated between COVID‐19 and non‐COVID‐19 evidence in our results section.
The WHO supported the original review financially. This update was funded by internal funds of the Department of Evidence‐based Medicine and Evaluation at the Danube‐University Krems.
Contributions of authors
Study design: BN, GG, IK Literature search: IK Study selection, data collection: AD, AC, BN, CZ, DL, EP, GG, GW, VM Quality assessment of studies: AD, AC, BN, CZ, DL, EP, GG, GW, US, VM GRADEing the certainty of evidence: GG, BN, VM Narrative synthesis and data interpretation: BN, GG Figures and tables: AD, AC, BN, CL, CZ, EP, GG, GW, US, VM Writing the manuscript: BN Supervision: GG Critical revision and feedback on the manuscript: AD, AC, CZ, DL, EP, GG, GW, IK, US, VM
Sources of support
Internal sources
Liverpool School of Tropical Medicine (LSTM), UK
External sources
-
University for Continuing Education Krems ‐ Danube University Krems, Austria
This review was performed by the Department for Evidence‐based Medicine and Evaluation, University for Continuing Education Krems ‐ Danube University Krems in its capacity as a WHO Collaborating Center for evidence‐based medicine
Foreign, Commonwealth and Development Office (FCDO) Project number 300342‐104, UK
Declarations of interest
Barbara Nussbaumer‐Streit: no conflicts of interest with respect to the topic of this manuscript Verena Mayr: consultancy (Borealis AG) concerning how to deal with the current SARS‐CoV‐2 situation at work ‐ no competing interest with the review Andreea Iulia Dobrescu: no conflicts of interest with respect to the topic of this manuscript Andrea Chapman: no conflicts of interest with respect to the topic of this manuscript Emma Persad: no conflicts of interest with respect to the topic of this manuscript Irma Klerings: no conflicts of interest with respect to the topic of this manuscript Gernot Wagner: no conflicts of interest with respect to the topic of this manuscript Uwe Siebert: no conflicts of interest with respect to the topic of this manuscript Dominic Ledigner: no conflicts of interest with respect to the topic of this manuscript Casey Zachariah: no conflicts of interest with respect to the topic of this manuscript Gerald Gartlehner: no conflicts of interest with respect to the topic of this manuscript
Edited (no change to conclusions)
References
References to studies included in this review
Arima 2020 {published data only}
- Arima Y, Shimada T, Suzuki M, Suzuki T, Kobayashi Y, Tsuchihashi Y, et al. Severe acute respiratory syndrome coronavirus 2 infection among returnees to Japan from Wuhan, China, 2020. Emerging Infectious Diseases 2020;26(7):1596-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Becker 2005 {published data only}
- Becker NG, Glass K, Li Z, Aldis GK. Controlling emerging infectious diseases like SARS. Mathematical Biosciences 2005;193(2):205-21. [DOI] [PubMed] [Google Scholar]
Cao 2020 {published data only}
- Cao S, Feng P, Shi P. Study on the epidemic development of coronavirus disease-19 (COVID-19) in Hubei Province by a modified SEIR model. Journal of Zhejiang University (Medical Sciences) 2020;49(2):178-84. [DOI: 10.3785/j.issn.1008-9292.2020.02.05] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chau 2003 {published data only}
- Chau PH, Yip PS. Monitoring the severe acute respiratory syndrome epidemic and assessing effectiveness of interventions in Hong Kong Special Administrative Region. Journal of Epidemiology and Community Health 2003;57(10):766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2020 {published data only}
- Choi SC, Ki M. Estimating the reproductive number and the outbreak size of novel coronavirus disease (COVID-19) using mathematical model in Republic of Korea. Epidemiology and Health 2020;42:e2020011. [DOI: 10.4178/epih.e2020011] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cowling 2020 {published data only}
- Cowling BJ, Ali ST, Ng TW, Tsang TK, Li JC, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health 2020;5(5):279-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Day 2006 {published data only}
- Day T, Park A, Madras N, Gumel A, Wu J. When is quarantine a useful control strategy for emerging infectious diseases? American Journal of Epidemiology 2006;163(5):479-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fang 2020 {published data only}
- Fang Y, Nie Y, Penny M. Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: a data-driven analysis. Journal of Medical Virology 2020;06:06. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferguson 2020 {published data only}
- Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf (accessed prior to 1 September 2020).
Fraser 2004 {published data only}
- Fraser C, Riley S, Anderson RM, Ferguson NM. Factors that make an infectious disease outbreak controllable. Proceedings of the National Academy of Sciences of the United States of America 2004;101(16):6146-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Geng 2020 {published data only}
- Geng H, Xu A, Wang X, Zhang Y, Yin X, Mao MA, et al. Analysis of the role of current prevention and control measures in the epidemic of new coronavirus based on SEIR model. Journal of Jinan University (Natural Science & Medicine Edition) 2020.
Gumel 2004 {published data only}
- Gumel AB, Ruan S, Day T, Watmough J, Brauer F, Van den Driessche P, et al. Modelling strategies for controlling SARS outbreaks. Proceedings of the Royal Society of London. Series B, Containing Papers of a Biological Character. Royal Society (Great Britain) 2004;271(1554):2223-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gupta 2005 {published data only}
- Gupta AG, Moyer CA, Stern DT. The economic impact of quarantine: SARS in Toronto as a case study. Journal of Infection 2005;50(5):386-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamidouche 2020 {published data only}
- Hamidouche M. COVID-19 epidemic in Algeria: assessment of the implemented preventive strategy. medRxiv 2020. [DOI: 10.1101/2020.04.21.20074443] [DOI] [Google Scholar]
Hoertel 2020 {published data only}
- Hoertel N, Blachier M, Blanco C, Olfson M, Massetti M, Limosin F, Leleu H. Facing the COVID-19 epidemic in NYC: a stochastic agent-based model of various intervention strategies. medRxiv 2020. [DOI: 10.1101/2020.04.23.20076885] [DOI] [Google Scholar]
Hou 2020 {published data only}
- Hou C, Chen J, Zhou Y, Hua L, Yuan J, He S, et al. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID‐19): A well‐mixed SEIR model analysis. Journal of Medical Virology 2020;92:841-48. [DOI] [PubMed] [Google Scholar]
Hsieh 2005 {published data only}
- Hsieh YH, King CC, Chen CW, Ho MS, Lee JY, Liu FC, et al. Quarantine for SARS, Taiwan. Emerging Infectious Diseases 2005;11(2):278-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsieh 2007 {published data only}
- Hsieh YH, King CC, Chen CW, Ho MS, Hsu SB, Wu YC. Impact of quarantine on the 2003 SARS outbreak: a retrospective modeling study. Journal of Theoretical Biology 2007;244(4):729-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hu 2020 {published data only}
- Hu Z, Cui Q, Han J, Wang X, Sha WEI, Teng Z. Evaluation and prediction of the COVID-19 variations at different input population and quarantine strategies, a case study in Guangdong province, China. International Journal of Infectious Diseases 2020;95:231-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koo 2020 {published data only}
- Koo JR, Cook AR, Park M, Sun Y, Sun H, Lim JT, et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infectious Diseases 2020;20(6):678-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kucharski 2020 {published data only}
- Kucharski AJ, Klepac P, Conlan AJ, Kissler SM, Tang ML, Fry H, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infectious Diseases 2020 June 15 [Epub ahead of print ]. [10.1016/S1473-3099(20)30457-6] [DOI] [PMC free article] [PubMed]
Lee 2020 {published data only}
- Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. Journal of Travel Medicine 2020;27(3):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2020b {published data only}
- Liu F, Li X, Zhu G. Using the contact network model and Metropolis-Hastings sampling to reconstruct the COVID-19 spread on the “Diamond Princess”. Science Bulletin 2020;65(15):1297-1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lloyd‐Smith 2003 {published data only}
- Lloyd-Smith JO, Galvani AP, Getz WM. Curtailing transmission of severe acute respiratory syndrome within a community and its hospital. Proceedings of the Royal Society of London. Series B, Containing Papers of a Biological Character. Royal Society (Great Britain) 2003;270(1528):1979-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lytras 2020 {published data only}
- Lytras T, Dellis G, Flountzi A, Hatzianastasiou S, Nikolopoulou G, Tsekou K, et al. High prevalence of SARS-CoV-2 infection in repatriation flights to Greece from three European countries. Journal of Travel Medicine 2020;27(3):1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Madubueze 2020 {published data only}
- Madubueze CE, Dachollom S, Onwubuya O. Controlling the spread of COVID-19: optimal control analysis. medRxiv 2020. [DOI: 10.1101/2020.06.08.20125393] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mubayi 2010 {published data only}
- Mubayi A, Zaleta CK, Martcheva M, Castillo-Chavez C. A cost-based comparison of quarantine strategies for new emerging diseases. Mathematical Biosciences and Engineering: MBE 2010;7(3):687-717. [DOI] [PubMed] [Google Scholar]
Nishiura 2004 {published data only}
- Nishiura H, Patanarapelert K, Sriprom M, Sarakorn W, Sriyab S, Ming Tang I. Modelling potential responses to severe acute respiratory syndrome in Japan: the role of initial attack size, precaution, and quarantine. Journal of Epidemiology and Community Health 2004;58(3):186-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pandey 2020 {published data only}
- Pandey KR, Subedee A, Khanal B, Koirala B. COVID-19 control strategies and intervention effects in resource limited settings: a modeling study. medRxiv 2020. [DOI: 10.1101/2020.04.26.20079673] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pang 2003 {published data only}
- Pang X, Zhu Z, Xu F, Guo J, Gong X, Liu D, et al. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA 2003;290(24):3215-21. [DOI] [PubMed] [Google Scholar]
Park 2020 {published data only}
- Park HC, Lee SH, Kim J, Kim DH, Cho A, Jeon HJ, et al. Effect of isolation practice on the transmission of Middle East respiratory syndrome coronavirus among hemodialysis patients: a 2-year prospective cohort study. Medicine 2020;99(3):e18782. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peak 2017 {published data only}
- Peak CM, Childs LM, Grad YH, Buckee CO. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proceedings of the National Academy of Sciences of the United States of America 2017;114(15):4023-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peak 2020 {published data only}
- Peak CM, Kahn R, Grad YH, Childs LM, Li R, Lipsitch M, Buckee CO. Individual quarantine versus active monitoring of contacts for the mitigation of COVID-19: a modelling study. Lancet Infectious Diseases 2020 May 20 [Epub ahead of print]. [DOI: 10.1016/S1473-3099(20)30361-3] [DOI] [PMC free article] [PubMed]
Pourbohloul 2005 {published data only}
- Pourbohloul B, Meyers LA, Skowronski DM, Krajden M, Patrick DM, Brunham RC. Modeling control strategies of respiratory pathogens. Emerging Infectious Diseases 2005;11(8):1249-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rocklöv 2020 {published data only}
- Rocklöv J, Sjodin H, Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. Journal of Travel Medicine 2020;28:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryu 2020 {published data only}
- Ryu S, Ali ST, Lim JS, Chun BC. Estimation of the excess COVID-19 cases in Seoul, South Korea by the students arriving from China. International Journal of Environmental Research and Public Health 2020;17(9):3113. [DOI: 10.3390/ijerph17093113] [DOI] [PMC free article] [PubMed] [Google Scholar]
Semenova 2020 {published data only}
- Semenova Y, Glushkova N, Pivina L, Khismetova Z, Zhunussov Y, Sandybaev M, et al. Epidemiological characteristics and forecast of COVID-19 outbreak in the Republic of Kazakhstan. Journal of Korean Medical Science 2020;35(24):e227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shen 2020 {published data only}
- Shen M, Peng Z, Guo Y, Rong L, Li Y, Xiao Y, et al. Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households. International Journal of Infectious Diseases 2020;96:503-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sjödin 2020 {published data only}
- Sjödin H, Wilder-Smith A, Osman S, Farooq Z, Rocklov J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. European Surveillance 2020;25(13):2000280. [DOI: 10.2807/1560-7917.ES.2020.25.13.2000280] [DOI] [PMC free article] [PubMed] [Google Scholar]
Su 2020 {published data only}
- Su L, Hong N, Zhou X, He J, Ma Y, Jiang H, et al. Evaluation of the secondary transmission pattern and epidemic prediction of COVID-19 in the four metropolitan areas of China. Frontiers in Medicine 2020;7:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tang 2020a {published data only}
- Tang B, Wang X, Li Q, Bragazzi NL, Tang S, Xiao Y, et al. Estimation of the transmission risk of the 2019-nCoV and its implication for public health interventions. Journal of Clinical Medicine 2020;9(2):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tang 2020b {published data only}
- Tang B, Xia F, Tang S, Bragazzi NL, Li Q, Sun X, et al. The effectiveness of quarantine and isolation determine the trend of the COVID-19 epidemic in the final phase of the current outbreak in China. International Journal of Infectious Diseases 2020;96:636-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tuite 2020 {published data only}
- Tuite AR, Fisman DN, Greer AL. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. Canadian Medical Association Journal 2020;192(19):e497-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2004 {published data only}
- Wang W, Ruan S. Simulating the SARS outbreak in Beijing with limited data. Journal of Theoretical Biology 2004;227(3):369-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2007 {published data only}
- Wang TH, Wei KC, Hsiung CA, Maloney SA, Eidex RB, Posey DL, et al. Optimizing severe acute respiratory syndrome response strategies: lessons learned from quarantine. American Journal of Public Health 2007;97 Suppl 1:S98-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2020 {published data only}
- Wang T, Wu Y, Lau JY, Yu Y, Liu L, Zhang K, et al. A four-compartment model for the COVID-19 infection—implications on infection kinetics, control measures, and lockdown exit strategies. Precision Clinical Medicine 2020;3(2):104-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2020b {published data only}
- Wu W-T, Li D-N, Li L. Analysis of the role of different intensity prevention and control measures in the current epidemic of novel coronavirus (2019-nCoV) infected pneumonia in Wuhan based on SIR model. New Medicine 2020;30(1):78-82. [Google Scholar]
Yip 2007 {published data only}
- Yip PS, Hsieh YH, Xu Y, Lam KF, King CC, Chang HL. Assessment of intervention measures for the 2003 SARS epidemic in Taiwan by use of a back-projection method. Infection Control and Hospital Epidemiology 2007;28(5):525-30. [DOI] [PubMed] [Google Scholar]
Yue 2020 {published data only}
- Yue Y, Chen Y, Liu K, Luo X, Xu B, Jiang Y, et al. Modeling and prediction of new coronavirus pneumonia based time-delay dynamic system. Scientia Sinica Mathematica 2020;50(3):1-8.
Zhang 2017 {published data only}
- Zhang XS, Pebody R, Charlett A, Angelis D, Birrell P, Kang H, et al. Estimating and modelling the transmissibility of Middle East respiratory syndrome coronavirus during the 2015 outbreak in the Republic of Korea. Influenza and Other Respiratory Viruses 2017;11(5):434-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhao 2020a {published data only}
- Zhao S, Chen H. Modeling the epidemic dynamics and control of COVID-19 outbreak in China. Quantitative Biology 2020 Mar 11 [Epub ahead of print]. [DOI: 10.1007/s40484-020-0199-0] [DOI] [PMC free article] [PubMed]
Additional references
Bauch 2005
- Bauch CT, Lloyd-Smith JO, Coffee MP, Galvani AP. Dynamically modeling SARS and other newly emerging respiratory illnesses: past, present, and future. Epidemiology 2005;16(6):791-801. [DOI] [PubMed] [Google Scholar]
Biggerstaff 2014
- Biggerstaff M, Cauchemez S, Reed C, Gambhir M, Finelli L. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infectious Diseases 2014;14(1):480. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks 2020
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395(10227):912-20. [DOI] [PMC free article] [PubMed]
Brozek 2020
- Canelo-Aybar C, Akl EA, Bowen JM, Butcher J, Chiu WA, Cronin M. GRADE Guidelines 30: the GRADE approach to assessing the certainty of modelled evidence - an overview in the context of health decision-making. Draft article. [DOI] [PMC free article] [PubMed]
Cetron 2005
- Cetron M, Landwirth J. Public health and ethical considerations in planning for quarantine. Yale Journal of Biology and Medicine 2005;78(5):329-34. [PMC free article] [PubMed] [Google Scholar]
China CDC 2020
- Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese Journal of Epidemiology 2020;41(2):145-51. [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed March 2020. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical Research Ed.) 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Habibi 2020
- Habibi R, Burci GL, Campos TC, Chirwa D, Cinà M, Dagron S, et al. Do not violate the International Health Regulations during the COVID-19 outbreak. Lancet 2020;395(10225):664-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haug 2020
- Haug N, Geyrhofer L, Londey A, Dervic E, Desvars-Larrive A, Loreto V, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. medRxiv 2020. [DOI: 10.1101/2020.07.06.20147199] [DOI] [PubMed] [Google Scholar]
Jernigan 2020b
- Jernigan DB. Update: Public Health response to the coronavirus disease 2019 outbreak — United States. MMWR. Morbidity and Mortality Weekly Report 2020;69:216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2020a
- Liu Ying, Gayle AA, Wilder-Smith A, Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. Journal of Travel Medicine 2020;27(2):taaa021. [DOI: 10.1093/jtm/taaa021] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Journal of Clinical Epidemiology 2009;62(10):1006-12. [DOI] [PubMed] [Google Scholar]
Mulder 2019
- Mulder RL, Bresters D, Van den Hof M, Koot BG, Castellino SM, Loke YK, et al. Hepatic late adverse effects after antineoplastic treatment for childhood cancer. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No: CD008205. [DOI: 10.1002/14651858.CD008205.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2018
- Park J-E, Jung S, Kim A. MERS transmission and risk factors: a systematic review. BMC Public Health 2018;18(1):574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pitman 2012
- Pitman R, Fisman D, Zaric GS, Postma M, Kretzschmar M, Edmunds J, et al. Dynamic transmission modeling: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group–5. Medical Decision Making 2012;32(5):712-21. [DOI] [PubMed] [Google Scholar]
Rajgor 2020
- Rajgor DD, Lee MH, Archuleta S, Bagdasarian N. The many estimates of the COVID-19 case fatality rate. Lancet infection 2020;20:776-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Read 2020
- Read JM, Bridgen JR, Cummings DA, Ho A, Jewell CP. Novel coronavirus 2019-nCoV: early estimation of epidemiological parameters and epidemic predictions. medRxiv 2020. [DOI: 10.1101/2020.01.23.20018549] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rockers 2015
- Rockers PC, Røttingen JA, Shemilt I, Tugwell P, Bärnighausen T. Inclusion of quasi-experimental studies in systematic reviews of health systems research. Health Policy 2015;119(4):511-21. [DOI] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Schünemann 2019
- Schünemann HJ, Cuello C, Akl EA, Mustafa RA, Meerpohl JJ, Thayer K. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Journal of Clinical Epidemiology 2019;111:105-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taubenberger 2006
- Taubenberger JK, Morens DM. 1918 influenza: the mother of all pandemics. Emerging Infectious Diseases 2006;12(1):15-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2005
- World Health Organization (WHO). International Health Regulations - third edition. apps.who.int/iris/bitstream/handle/10665/246107/9789241580496-eng.pdf;jsessionid=8E87192BD7F98D81317FD117AC6B43E4?sequence=1 (accessed prior to 1 September 2020).
WHO 2020a
- World Health Organization (WHO). Report of the WHO-China Joint Mission on coronavirus disease 2019 (COVID-19). www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (accessed 29 February 2020).
WHO 2020b
- World Health Organization (WHO). Rolling updates on coronavirus diseases (COVID-19). www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 3 April 2020).
WHO 2020c
- World Health Organization (WHO). Cumulative number of reported probable cases of severe acute respiratory syndrome (SARS). www.who.int/csr/sars/country/en/ (accessed 28 February 2020).
WHO 2020d
- World Health Organization (WHO). Middle East respiratory syndrome coronavirus (MERS-CoV). www.who.int/emergencies/mers-cov/en/ (accessed 28 February 2020).
WHO 2020e
- World Health Organization (WHO). Considerations for quarantine of individuals in the context of containment for coronavirus disease (COVID-19). www.who.int/internal-publications-detail/considerations-for-quarantine-of-individuals-in-the-context-of-containment-for-coronavirus-disease-(covid-19) (accessed 29 February 2020).
WHO 2020f
- World Health Organization (WHO). Environmental health in emergencies. www.who.int/environmental_health_emergencies/disease_outbreaks/en/ (accessed 12 February 2020).
WHO 2020g
- World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Report-11. www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4 (accessed 2 April 2020).
WHO 2020h
- World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Report-12. www.who.int/docs/default-source/coronaviruse/situation-reports/20200201-sitrep-12-ncov.pdf?sfvrsn=273c5d35_2 (accessed 3 August 2020).
WHO 2020i
- World Health Organization (WHO). Novel Coronavirus (2019-nCoV) Situation Report-61. www.who.int/docs/default-source/coronaviruse/situation-reports/20200321-sitrep-61-covid-19.pdf?sfvrsn=ce5ca11c_2 (accessed 3 August 2020).
Wu 2020a
Zhao 2020
- Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. International Journal of Infectious Diseases 2020;92:214-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 2020b
- Zhou T, Liu QH, Yang ZM, Liao J, Yang K, Bai W, et al. Preliminary prediction of the basic reproduction number of the Wuhan novel coronavirus 2019-nCoV. Journal of Evidence-based Medicine 2020;13(1):3-7. [DOI: 10.1111/jebm.12376] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Nussbaumer‐Streit 2020
- Nussbaumer‐Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID‐19: a rapid review. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD013574. [DOI: 10.1002/14651858.CD013574] [DOI] [PMC free article] [PubMed] [Google Scholar]


