Summary
Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disorder worldwide. This historical narrative traces the evolution from basic descriptions of fatty liver in the nineteenth century to our contemporary understanding of NAFLD in the twentieth and twenty-first centuries. A detailed historiographic review of fatty liver from 1800s onwards was performed alongside a brief review of contemporary associations. Archived published literature dating back to the 1800s describe clinicopathological features of fatty liver. In the nineteenth century, doyens of medicine associated fatty liver with alcohol, malnutrition or wasting conditions, and subsequently adiposity, unhealthy diets and sedentary lifestyle. Microscopically, fatty liver was described when 5% or more hepatocytes were distended with fat. Recommendations to reverse fatty liver included reducing consumption of fat, sugar, starchy carbohydrates and alcohol, plus increasing physical exercise. Fatty liver was associated with liver fibrosis and cirrhosis in the late 1800s, and with diabetes in the early 1900s. The diagnostic labels NAFLD and non-alcoholic steatohepatitis (NASH) were introduced in the late 1900s. Metabolic dysfunction-associated fatty liver disease (MAFLD) was recently proposed to update the nosology of fatty liver, recognising the similar metabolic pathogenesis evident in individuals with typical NAFLD and those with heterogenous “secondary” co-factors including alcohol and other aetiologies. Fatty liver has emerged from being considered a disorder of nutritional extremes or alcohol excess to contemporary recognition as a complex metabolic disorder that risks progression to cirrhosis and hepatocellular carcinoma. The increasing prevalence of NAFLD and our growing understanding of its lifestyle and metabolic determinants justify the current exercise of re-examining the evolution of this common metabolic disorder.
Keywords: Non-alcoholic fatty liver disease, metabolic dysfunction-associated fatty liver disease, MAFLD, non-alcoholic steatohepatitis, NASH, alcohol, diet, metabolic, liver fibrosis, obesity, diabetes, cirrhosis
Abbreviations: HCC, hepatocellular carcinoma; MAFLD, Metabolic dysfunction-associated fatty liver disease; NAFL, Non-alcoholic fatty liver; NAFLD, Non-alcoholic fatty liver disease; NAS, NAFLD activity score; T2DM, Type 2 diabetes mellitus
Key points.
-
•
Doyens of medicine described fatty liver related to diet, physical inactivity, obesity, and/or alcohol in the 1800s.
-
•
Treatment of fatty liver in the 1800s was increased exercise plus reduction of fatty food, starch, sugar and alcohol.
-
•
Fatty liver had been identified in overfed children as early as 1849.
-
•
Diabetes was linked with fatty liver and liver fibrosis in the early-mid 1900s.
-
•
The term non-alcoholic fatty liver disease (NAFLD) was proposed in 1986 and non-alcoholic steatohepatitis (NASH) in 1980.
Introduction
Fatty liver is a common finding in humans. The most common form of fatty liver worldwide is non-alcoholic fatty liver disease (NAFLD), occurring when there is fat accumulation in the liver unrelated to excessive alcohol consumption. NAFLD has unexpectedly become an increasing cause of cirrhosis and hepatocellular carcinoma (HCC), which frequently lead to orthotopic liver transplantation or death.[1], [2], [3], [4] The spectrum of NAFLD includes isolated steatosis or non-alcoholic fatty liver (NAFL), through to non-alcoholic steatohepatitis (NASH) or cirrhosis.5 As the prevalence of NAFLD achieves epidemic proportions, it is time to retrace the historical genesis of contemporary knowledge about fatty liver.
In this historical narrative, the descriptions of fatty liver from archived primary sources are cited using the parlance of the period, that often expressed lifestyle and clinical risk factors in less compassionate terms compared to contemporary reports. Current knowledge has shown that – beyond lifestyle factors – sex, genetic, epigenetic and racial differences may influence the phenotypic expression of NAFLD.
Search strategy
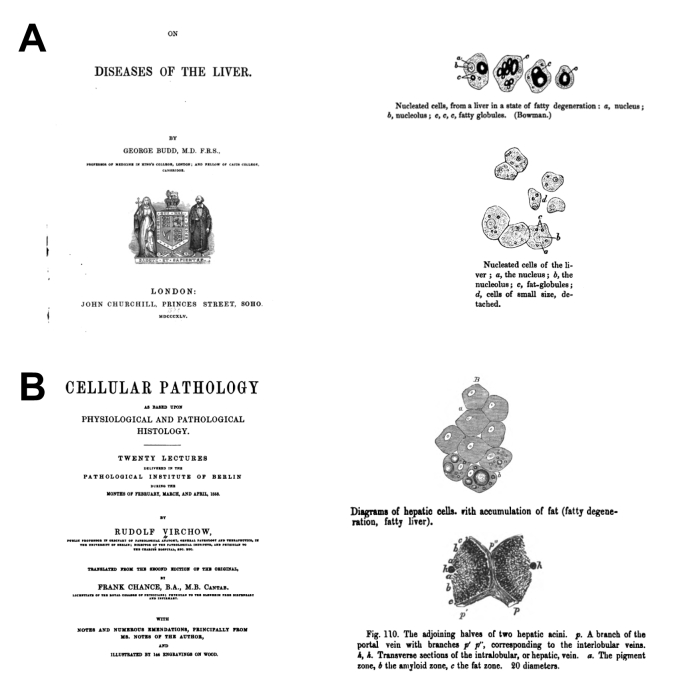
Historical records were identified from various databases, including Medline, Web of Science and Google books, using the medical subject heading (MeSH) key words ‘fatty liver’, ‘nonalcoholic fatty liver’, ‘nonalcoholic fatty liver disease’ or ‘NAFLD’, and from related cited references. Published books and academic journal articles from the nineteenth and twentieth centuries, in the English language or with full English language translations, were sourced, the text content checked for relevance and directly cited wherever possible. A brief contemporary history is included to provide context regarding more recent developments. Due to the exponentially increasing annual number of publications regarding “fatty liver” (Fig. 1) and “NAFLD” (Fig. 2), many worthy contributions to the literature could not be included. Fig. 3A and 3B are excerpts from microscopy from the 1800s.
Fig 1.
Trend of annual fatty liver publications (1910–2019).
After a slow rise in fatty liver publications from the mid-1960s onwards, there was an exponential rise from 1991, i.e. after introduction of the terms NASH and NAFLD and comparisons with alcohol-related liver disease.
Fig 2.
Trend of annual NAFLD publications (1986–2019).
Though the term ‘NAFLD’ was introduced in 1986, the exponential rise in NAFLD publications was most notable from 2000 onwards.
Fig 3.
Excerpts from books depicting fatty liver from the 1800s.
(A) George Budd. On diseases of the liver (1857). (B) Virchow R, Chance F. Cellular Pathology as based upon physiological and pathological histology. Twenty lectures delivered in the pathologic institute of Berlin (1858).
Historical aspects of fatty liver in adults (nineteenth – twentieth centuries)
Clinicopathological records of fatty liver associated with malnutrition, excessive alcohol, obesity, physical inactivity, or excessive consumption of fatty food or carbohydrates are described dating back to the early-mid nineteenth century.[6], [7], [8], [9], [10], [11], [12], [13] Table 1 summarises reports of fatty liver and NAFLD from the nineteenth and twentieth centuries.
Table 1.
Relationship between historical fatty liver knowledge and contemporary NAFLD/MAFLD knowledge (nineteenth and twentieth centuries).
| Author | Year | Medical specialty | Country | Diagnostic modality | Comment | |
|---|---|---|---|---|---|---|
| 1 | Thomas Addison | 1836 | Physician | England | Clinical | Fatty liver was associated with alcohol or tuberculosis. |
| 2 | Cecil Watson | 1842 | Physician | USA | Clinical and gross anatomy | Hepatomegaly with smooth-surfaced liver full of grease. |
| 3 | Carl von Rokitansky | 1849 | Pathologist | Austria | Clinical and gross anatomy | Fatty liver was associated with tuberculosis, alcohol, or in children with excessive food consumption. Early published record of childhood NAFLD. Fatty liver was associated with visceral adiposity. |
| 4 | George Budd | 1857 | Physician | England | Clinical, gross anatomy and microscopy | Fatty liver was associated with sedentary lifestyle and excessive fatty food. Features were hepatomegaly with excess liver fat in asymptomatic adults with unhealthy diet. Diagnosed if there was excess fat in ≥5% of hepatocytes. Recommended lean meat, abstinence from fatty food, starch, sugar and alcohol and increased exercise. |
| 5 | Rudolf Virchow | 1858 | Physician and pathologist | Germany | Gross anatomy and microscopy | Excessive fat in the hepatic acinus, initially peri-portal. Fat granules coalesce in hepatocyte, resembling subcutaneous adipocyte. Cured by freeing hepatocytes from fat. |
| 6 | Friedrich von Frerichs | 1860 | Physician and pathologist | Germany | Clinical and gross anatomy | Not only fatty food, but also excessive amounts of any food, particularly carbohydrates, causes fatty liver. More prevalent in females than in males. |
| 7 | Charles Murchison | 1867 | Physician | England | Clinical, gross anatomy and physiology | Painless hepatomegaly without jaundice. Excessive food intake and sedentary lifestyle. Associated with subcutaneous fat accumulation and cardiac involvement. Fat was described as being produced in, or transported to, the liver. More prevalent in females than in males. |
| 8 | Austin Flint | 1867 | Physician | USA | Clinical | Fatty liver increases with age from young to older age, fatty diet and obesity. Fat-filled hepatocytes and hepatomegaly is seen. Precedes cirrhosis. Recommended treatment was exercise, avoiding fatty food, + abstinence from alcohol. |
| 9 | Charles Connor | 1938 | Pathologist | USA | Clinical, gross anatomy and physiology | Diabetes and reduced oxidation of liver fat cause fatty liver and liver fibrosis. Can cause cirrhosis similar to alcoholic cirrhosis. |
| 10 | Harold Himsworth | 1947, 1949 | Physician | England | Clinical, gross anatomy and physiology | Severity and duration of fatty liver correlates with liver fibrosis. Caused by dietary fat, choline or methionine deficiency. Emphasised that fatty liver is not innocuous. |
| 10 | Charles Best | 1949 | Physiologist | Canada | Physiology and microscopy | Concluded from animal studies that fatty and fibrotic changes in the liver resulting from alcohol or sucrose are due to a deficiency of lipotropic factors. Rats given alcohol or fed high sugar diet with inadequate lipotropic factors developed similar degrees of fatty liver and fibrosis. These were prevented by dietary choline, methionine or casein. |
| 11 | James Dible | 1951 | Pathologist | England | Clinical, microscopy and physiology | Described fatty liver as arising from fat produced in the liver or mobilized from peripheral sites and transported to the liver via the circulation. This is akin to contemporary fatty liver secondary to lipodystrophy and wasting disorders. He did not believe humans could have sufficient fat for long enough to result in fibrosis. Fatty liver was linked with obesity and diabetes. More prevalent in females than in males. |
| 12 | Carroll Leevy | 1962 | Physician | USA | Clinical and microscopy | Fatty liver was seen in 5% of liver biopsies. It was seen in all ages, from childhood to old age. Associated with diabetes, heart disease, obesity or gall bladder disease. 5 stages of severity of hepatic steatosis graded (none, abnormal but not clinically significant, mild, moderate, severe). |
| 13 | Heribert Thaler | 1962 | Physician | Austria | Clinical and microscopy | Fatty liver was further associated with development of cirrhosis. |
| 14 | Mario Dianzani | 1964 | Pathologist | Italy | Physiology | Described the pathogenesis of fat accumulation in the liver. |
| 15 | Michael Adler | 1979 | Physician | USA | Clinical and microscopy | Reported fatty liver with inflammation, fibrosis or cirrhosis unrelated to alcohol in diabetic or obese people |
| 16 | Jurgen Ludwig | 1980 | Pathologist | USA | Clinical and microscopy | Coined nonalcoholic steatohepatitis (NASH) as fatty liver with inflammation + variable fibrosis. Linked with obesity, diabetes, hepatomegaly or cholelithiasis. Predominantly seen in females. |
| 17 | Fenton Schaffner | 1986 | Physician and pathologist | USA | Clinical and microscopy | Introduced the term nonalcoholic fatty liver disease. |
| 18 | Heribert Thaler | 1988 | Physician | USA | Clinical and physiology | Described contemporary pathogenesis of fatty change in the liver as arising from:
|
| 19 | Randall Lee | 1989 | Pathologist | USA | Longitudinal study showing progression from NASH to cirrhosis in predominantly middle-aged, obese or diabetic females with raised liver enzymes or hepatomegaly. | |
| 20 | Amedeo Lonardo | 1997 | Physician | Italy | Clinical and sonography | The bright liver detected by ultrasound i.e. fatty liver was associated with increasing age and features of the metabolic syndrome. |
| 21 | Christi Matteoni | 1999 | Physician | USA | Clinical and microscopy | Described the spectrum of NAFLD severity. AST correlates with increasing NASH or fibrosis severity. |
| 22 | Elizabeth Brunt | 1999 | Pathologist | USA | Clinical and microscopy | Described histological grading and staging system for NASH. AST correlates with increasing NASH or fibrosis severity. |
| 23 | Giulio Marchesini | 1999 | Physician | Italy | Clinical and physiology | Linked NAFLD with insulin resistance. Observed NAFLD in lean people (lean NAFLD). |
Nineteenth century
Physicians and pathologists described clinical, morphometric and pathological features of fatty liver. Unhealthy dietary macronutrient or alcohol consumption and sedentary habits were associated with fatty liver. Clinical observations included hepatomegaly, visceral and subcutaneous adiposity, and cardiac comorbidity. Initial pathology reports depicted gross anatomical appearances and subsequently microscopy of the fatty liver.
In 1836, the English physician and scientist, Thomas Addison described cases of fatty degeneration of the liver, or fatty liver, related to excessive alcohol intake.6
In 1842, the American physician, Cecil Watson described the gross anatomy of the fatty liver as “inordinately large, of a smooth, uniform color and appearance”.7 “This liver is full of fat, or grease”.
Clinicopathological records by Carl von Rokitansky (an Austrian pathologist) in 1849 described fatty liver as adipose metamorphosis, with morbid accumulation of fat in the liver.8 Though fatty liver was commonly associated with tuberculosis, it also “developed in consequence of a luxurious and indolent regimen, in children who have been gorged with food, and especially as a result of dram-drinking”. It was accompanied by “accumulations of fat in the omentum, the mesenteries, the pericardium, the heart and the subcutaneous cellular tissue…”.
In 1857, George Budd (a British physician) produced a detailed record of the clinical, gross anatomy and microscopy of ‘fatty liver’ or ‘fatty degeneration of the liver’.9 “In every human liver there is some uncombined oil or fat, which, in healthy grown-up persons, amounts, perhaps, on an average, to three or four per cent, of the whole mass”. “In the fatty liver the quantity of fatty matter is enormously increased. The hepatic cells are gorged with large globules, which greatly distend them”. “In many of the cells thus gorged with oil the nuclei have disappeared or are rendered invisible by the oil globules”. Budd noted the absence of symptoms. “An accumulation of fatty matter in the lobular substance of the liver, …causes no obvious derangement of health”. “The liver becomes fatty in very different states of the body. 1st.—It is often fatty in persons who lead indolent lives, and are at the same time gross feeders—eating largely of fatty substances, and drinking freely of porter and other heavy malt liquors; and in such persons there is generally with the fatty liver an excess of fat under the skin, and in other parts of the body in which fat is usually deposited”. The liver is sometimes “extremely fatty in men who take little exercise, and drink immoderately of ardent spirits”. Lifestyle management was recommended – “If he will rise early, take active exercise, live chiefly on lean meat, with plenty of salt, and drink water, and will abstain from butter, bacon, oil, beer and other fermented drinks, and not eat too largely of sugar and starch”.9
In 1858, Rudolf Virchow, a German polymath (physician and pathologist) described the microscopic appearance of the fatty liver.10 “Upon studying a fatty liver, it is generally seen that the fat is first deposited in that zone of the acini which is immediately contiguous to the capillaries into which the branches of the portal vein break up”. “The more abundant the infiltration, the broader does the fatty zone become, and there are cases in which the fat fills the whole of the acini up the central (intralobular) hepatic vein and every single cell is crammed full of fat. In rare cases it certainly happens, that we find just the reverse, and that the fat lies around the central vein”. Fat-filled liver cells “present the same appearance as those of adipose tissue; scarcely any membrane, and scarcely ever a nucleus is seen, nevertheless they both still continue to exist”. “Hence it follows, that a fatty condition of the liver may be removed, that it is curable...” “The only requisite is, that the causes of the retention be removed, and the hepatic cells be freed from fat”.10
In 1860, the German physician and pathologist, Friedrich von Frerichs11 expatiated on the link between dietary habits and fatty liver, stating “It is not only food unusually rich in fat that gives rise to these deposits in the liver, but, under certain circumstances, every kind of food, when in too great quantity, has the same effect, even when it is free from fat, and only contains a large quantity of the carbohydrogens”. “…a fatty liver is not unfrequently found in individuals who have died suddenly in the bloom of good health…however, in improper food, the deposit increases more and more, and gradually exceeds the boundaries of health”. Fatty liver was more common in females than in males.
The British physician Charles Murchison, in 1867,12 reported clinical associations of fatty liver - “Fatty enlargement of the liver is painless, from first to last”. “The constitutional symptoms of fatty liver are few and not characteristic, and those which have been noted are often due for the most part to coexisting fatty degeneration of other organs, and more especially of the heart”. “Although fatty liver can coexist with cirrhosis, the liver under such circumstances is reduced in size”. “Jaundice, is not a feature of the fatty liver.” Conditions associated with fatty liver included “large accumulation of fat beneath the skin and throughout the body in people who are gross feeders and lead indolent lives”. “Persons who drink immoderately of ardent spirits, particularly if they take little exercise, are very subject to fatty liver”. “Fatty liver is met with under two opposite conditions: one, in which there is an increased amount of material capable of being converted into oil, and where fat often accumulates in all the tissues of the body; the other in which there is a rapid absorption of fat from all the tissues, with consequent emaciation”.
In 1867, Austin Flint, an American physician, described fatty liver with hepatomegaly in healthy, mostly female individuals.13 According to Flint, “The liver is to be considered as morbidly fatty, when the accumulation of fat is sufficient to increase the size of the organ”. For diagnosis - “… the readiest and most reliable test is the appearance of the hepatic cells under the microscope. Oil drops are found, larger and more numerous than in health…”. “Fatty articles of food entering largely into the diet, conjoined with indolent habits, conduce to the accumulation of fat in the liver, the mechanism being the same as in the production of the foie gras of geese”. Fatty liver was also related to alcohol. “Fatty liver and fatty kidney are sometimes observed in young subjects”. “The fatty liver and cirrhosis, however, may be combined…”. Proposed treatment of fatty liver was “by a reformation of the habits of living, viz., by temperance, or total abstinence, in respect of the use of alcoholic beverages, by restricting the diet, in a great measure, to articles not abounding in fat, and, if the strength will permit, by more muscular exercise”.13
Twentieth century
Notwithstanding controversy regarding the natural history of fatty liver, the understanding of its pathogenesis improved throughout the twentieth century. Nutritional deficiencies in lipotropic factors, micronutrients, amino acids and proteins were associated with fatty liver, while diabetes and chronic hepatic steatosis increased the risk of liver fibrosis and cirrhosis. The contribution of women to the field of fatty liver research became more prominent in the late-twentieth century, reflecting improving equity and inclusivity in medicine at the time. Fatty liver was recognised as a heterogenous disorder of metabolism and the microscopy of alcohol-related and non-alcoholic fatty liver were noted to be similar. Finally, the histologic spectrum of NAFLD severity was described in adults and children, the diagnostic terms NAFLD and NASH were introduced and NAFLD was associated with insulin resistance.
Pre-NAFLD and NASH years
In 1938, fatty liver and cirrhosis associated with diabetes were reported by Charles Connor (American pathologist),14 describing “in man, the decreased oxidation of liver fat associated with diabetes results in a chronic fatty infiltration, and this prolonged infiltration may lead to a cirrhosis of the liver that is indistinguishable from alcoholic cirrhosis”. He asserted that “long continued fatty infiltration of the liver is a mechanical factor of great importance in the development of a fibrous tissue-retaining wall around distended lobules”.
Despite reports linking fatty liver, diabetes and cirrhosis, in the 1940s–1950s, there was ongoing controversy about whether fatty liver actually resulted in liver fibrosis or cirrhosis.[15], [16], [17], [18] Sir Harold Himsworth, a British physician, believed that the severity and duration of chronic fatty infiltration correlated with liver fibrosis.15 He concurred with the view that fatty infiltration arose from an excess of dietary fat or a deficiency of lipotropic factors such as choline or methionine that prevent fat from accumulating in the liver.16 To the chagrin of some of his contemporaries, Himsworth declared that fatty infiltration was not just an innocuous condition but could progress to diffuse liver fibrosis.
Based on studies in rats, the American-Canadian physiologist and co-discoverer of insulin, Charles Best concluded in 1949 that diets with an imbalance of calories and nutrients, particularly diets deficient in lipotropic factors relative to caloric intake, increased the risk of fatty liver or liver fibrosis.17 Best found that choline, methionine and casein protected the liver, therefore suggesting that “choline and other essentials should be supplied as naturally occurring components of a well-balanced diet, but the dietary faddist, alcoholic, or "soft-drink" addict does not consume this normal diet”.
In 1951, the British pathologist, James Dible accepted Virchov’s theory that fatty liver resulted from either fatty degeneration, in which hepatocyte protein was transformed into fat, or fatty infiltration, characterised by the accumulation of fat delivered to the liver via the circulation. Although acknowledging a quantitative relationship between the amount of fat available for transport and the degree to which it infiltrates the liver, Dible did not accept that humans could have abundant liver fat for long enough durations to develop liver fibrosis.18 He believed that in contrast with animal models, a human liver was unlikely to accumulate more than 30% fat for the equivalent of 7–8 years or 15% fat for up to 20 years, sufficient to cause liver fibrosis. Interestingly, Dible’s pathological series of fatty cirrhosis comprised predominantly obese, middle-aged diabetic females.18
In 1950, the African-American physician Carroll Leevy, conducted one of the first serial liver biopsy studies involving diabetic adolescents and adults biopsied after 1.5–16–year intervals. Leevy observed progression to cirrhosis in the majority of patients with a poor diet and alcoholism, but not in those who discontinued alcohol and had a good diet.19 He reported that a healthy, protein-adequate diet, weight loss, and control of diabetes resulted in mobilisation of liver fat and an associated improvement of hepatomegaly and liver transaminases in patients with uncomplicated hepatic steatosis. He estimated the cost of care for pre-cirrhotic alcohol-associated fatty liver was less than one-tenth of the cost of treating cirrhosis and its complications. In 1962, Leevy also described histological fatty liver in 5% of patients from a series of 5,000 percutaneous liver biopsies including children and adults.20 Amongst patients with fatty liver, one-quarter had ‘nonalcoholic fatty liver’ and the remainder ‘alcoholic fatty liver’. Both groups shared comorbidities of heart disease, diabetes, obesity and gallbladder disease. Leevy noted “the degree of steatosis and obesity showed a good correlation in nonalcoholic patients”. Expanding on the fatty liver threshold reported by Budd9 a century earlier, Leevy stratified steatosis severity into the following categories: total liver fat <5% (normal), 5–9% (abnormal but not clinically significant), 10–30% (mild), 30–70% (moderate), and >70% (severe fatty liver).20
Heribert Thaler (Austrian physician) further highlighted associations between fatty liver and cirrhosis in 1962,21 while Mario Dianzani (Italian pathologist) expatiated on the pathogenesis of fat accumulation in the liver in 1964.22
In 1973, Hans Popper (American pathologist) and colleagues described fatty liver as a potentially reversible “acquired disorder of intermediary metabolism of multiple etiologies resulting in the deposition of triglycerides in the liver”. It could result from alcohol, medications, toxins, starvation, protein-calorie malnutrition, after small bowel bypass, cholesteryl ester storage disease, and acutely during late stages of pregnancy.23 Macroscopically, the liver was enlarged, smooth and pale and microscopically fat was distributed throughout the whole lobule (although it sometimes affected central areas in early stages).
NAFLD, NASH and beyond
Fatty liver with inflammation, fibrosis or cirrhosis, unrelated to alcohol but associated with diabetes or obesity, was reported by Michael Adler and Fenton Schaffner (American physicians) in 1979.24 Subsequently, in 1980, Jurgen Ludwig (American pathologist) and colleagues introduced the term non-alcoholic steatohepatitis (NASH) based on a case series of predominantly female patients with obesity and diabetes, hepatomegaly or cholelithiasis, plus non-alcoholic fatty liver with lobular hepatitis, inflammatory infiltrates, Mallory bodies and variable severity of liver fibrosis.25 Mallory bodies (also termed Mallory-Denk bodies) were initially reported in 1911 in human alcohol-related liver disease by Frank Mallory (American pathologist);26 its description was refined in 1975 by Helmut Denk (Austrian pathologist) who also confirmed their presence in non-alcoholic liver disorders.27
NASH progressing through fibrosis to cirrhosis was reported by Randall Lee (American pathologist) in 1989.28 The term non-alcoholic fatty liver disease entered the hepatology lexicon in 1986, introduced by Fenton Schaffner (American physician and pathologist).29 In 1988, Anna Mae Diehl (American physician) described alcohol-like histologic features in middle-aged patients with NASH who differed from those with alcohol-related liver disease by being predominantly female, asymptomatic, obese, diabetic, hypertensive, and having cardiovascular disease, more severe steatosis and advanced fibrosis or cirrhosis (in over one-third of cases).30
In 1999, Christi Matteoni (American physician) described a histological spectrum of NAFLD severity including grading of steatosis, lobular inflammation, ballooning degeneration and Mallory hyaline or fibrosis.31 A histological grading and staging system to create uniformity in the description of NASH features was also proposed by Elizabeth Brunt (American pathologist).32 Further, Giulio Marchesini (Italian physician) and colleagues associated NAFLD with insulin resistance, an observation that included lean people.33 Concomitantly, studies by Portugese physician Helena Cortez-Pinto34 and Canadian scientist Picard Marceau35 linked NAFL with the metabolic syndrome. Hilla Knobler (Israeli physician)36 found that dietary interventions improve features of the metabolic syndrome and liver enzymes.
Contemporary aspects of fatty liver (twenty-first century)
Metabolic and histopathologic phenotype
NAFLD in non-diabetic, non-obese people with insulin resistance, was associated with metabolic features similar to those seen in diabetes or obesity, resulting in NAFLD being considered a feature of the metabolic syndrome.37 To improve uniformity of histologic reporting of NAFLD, Kleiner and the Pathology Committee of the NASH Clinical Research Network in the USA developed the NAFLD activity score (NAS), comprising scores for steatosis, lobular inflammation, hepatocellular ballooning, and fibrosis, for use in clinical trials.38 NAFLD is currently estimated to affect 25% of the global population and is associated with an increased risk of metabolic syndrome, T2DM, cirrhosis and hepatocellular cancer.39
Diet and adiposity
Associations between dietary composition, particularly fatty food, carbohydrates, sugar and soft-drinks, and fatty liver have been reported since the 1800s.9,11,13,17 The nutrition transition and increasing obesity over several decades40 have led to an increasing incidence of NAFLD.
Heritability, genetic and racial influences
NAFLD is now recognised as a complex disorder influenced by ethnicity,41 heritability within families,42 and genetic factors including the variants PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 and[43], [44], [45], [46], [47].
Other factors
Liver-related complications are most likely to occur in individuals with NASH and advanced fibrosis.48 The interplay of various factors determines the risk of NASH and liver fibrosis. A two-hit hypothesis – wherein chronic steatosis followed by oxidative stress result in NASH – provided a useful pathological explanation for NASH and the fibrosis seen in fatty livers.49 However, this concept has now been replaced by a multiple hit hypothesis involving complex simultaneous processes that contribute to hepatic steatosis, inflammation and fibrosis in genetically and epigenetically susceptible individuals.50 Insulin resistance was deemed a prerequisite for NAFLD.51 Both personal and family history of T2DM or insulin resistance are associated with increased risk of NASH and liver fibrosis in individuals with NAFLD.52,53
Fatty liver in children and adolescents
Nineteenth century
Fatty liver was observed by Rokitansky in overfed children as far back as 18498 and noted in young people by Flint in 1867.13
Twentieth century
Fatty liver in children can progress through liver fibrosis to cirrhosis. In the early-mid 1900s fatty liver in children was related to wasting disorders or chronic severe malnutrition such as kwashiorkor54 and subsequently with diabetes or obesity.19,20,55 Severe fatty liver with periportal fibrosis was observed in children with impaired brain development.56 The duration and severity of obesity has been associated with histologic NASH and NASH-related cirrhosis in children.57,58
Twenty-first century
Increasing rates of obesity-associated fatty liver in children and adolescents have been observed worldwide, such that in the USA there was a doubling of NAFLD prevalence over 20 years up to 2010.59 Obese children with NASH are at increased risk of developing cirrhosis.60 Schwimmer described the histopathologic differences between paediatric and adult NAFLD.61
Natural history studies of fatty liver (twentieth and twenty-first century)
Following Leevy’s biopsy series,19 other natural history studies have also shown progression of NAFLD to cirrhosis28 and identified liver histological characteristics associated with an increased likelihood of liver-related outcomes. Though NAFL has repeatedly been shown to portend a more benign liver-related course than fibrosing NASH,[62], [63], [64], [65], [66], [67] recent data have shown that with longer follow up, some individuals with isolated NAFL progress to end-stage liver disease.68
Lean NAFLD
Less than 20% of patients with NAFLD are lean and these individuals usually have features of metabolic dysfunction and visceral adiposity.69 Fibrosing NASH in non-obese, non-diabetic adults in the USA was described in 1994.70
Diagnosis
Beyond diet, physical inactivity, obesity and alcohol, fat accumulation in the liver may also result from the use of steatogenic medications, or from medical conditions including Wilson’s disease, chronic hepatitis C genotype 3, severe malnutrition, parenteral nutrition, lipodystrophy, abetalipoproteinaemia, and inborn errors of metabolism.71,72
For many decades the diagnosis of hepatic steatosis relied on liver histology, but nowadays it is usually based on liver ultrasound. Ultrasound-diagnosed fatty liver was proposed as the barometer of metabolic health.73 Fig 4, Fig 5B show microscopy from liver biopsies of NAFL, NASH with fibrosis, and NASH with cirrhosis, respectively. Liver biopsy is invasive and associated with sampling variability,20,74 hence there is a need for reliable and preferably non-invasive diagnostic tools to assess liver fibrosis. A discussion of these tests is beyond the scope of this review.
Fig 4.
Contemporary adult non-alcoholic fatty liver (NAFL or simple steatosis),
(H&E stain).
Fig 5.
Contemporary adult non-alcoholic steatohepatitis (NASH) with fibrosis (Masson’s trichrome stain).
(A) NASH with fibrosis (Masson’s trichrome stain). (B) NASH with cirrhosis (Masson’s trichrome stain).
Discussion
Fatty liver – the past vs. the present
Historical and contemporary records have reported fatty liver as a heterogenous, complex clinicopathological entity related to metabolic dysfunction. It is plausible that controversy regarding progression to liver fibrosis or cirrhosis18 and the historical association of fatty liver with alcohol resulted in a lag between early reports and acceptance of the potential seriousness of NAFLD.
Metabolic dysfunction-associated fatty liver disease (MAFLD)
Alcohol-associated and non-alcoholic fatty liver and cirrhosis share clinical, metabolic and histologic characteristics.14 Following the momentum to reform the diagnostic label NAFLD to a descriptive nomenclature better reflecting the pathophysiology of the disorder,75,76 the term metabolic dysfunction-associated fatty liver disease (MAFLD) was recently proposed by a group of international experts in the hope that an alternative name and definition will provide diagnostic clarity for clinical care, research and clinical trials.77 MAFLD is not simply a throwback to historical descriptions of fatty liver but an acceptance of the need for broader clinicopathological recognition of the metabolic basis and risk factors for fatty liver as observed over nearly two centuries. The definition of MAFLD requires evidence of hepatic steatosis plus metabolic syndrome, or at least two features of metabolic dysfunction (including overweight or obese BMI, obese waist circumference, systolic or diastolic arterial hypertension, hypertriglyceridaemia, low plasma high-density lipoprotein cholesterol, T2DM or prediabetes, homeostasis model assessment of insulin resistance score ≥2.5 or high-sensitivity C-reactive protein level >2 mg/L). Unlike NAFLD, the MAFLD definition does not exclude secondary factors such as alcohol or concomitant liver disease, or non-overweight BMI, as long as the other metabolic features are fulfilled. Consequently, a metabolic focus on people with so-called secondary causes of fatty liver is encouraged.77
Epidemiology and phenotype
The 5% threshold of steatotic hepatocytes, clinical phenotype, lifestyle factors and the relative absence of symptoms has been consistent with NAFLD over nearly two centuries. Historical data suggested a female preponderance, association with subcutaneous and visceral adiposity, and cardiac involvement8,9,12 with fatty liver. This contrasts with contemporary reports of NAFLD being more common in males and associating with visceral but not subcutaneous adiposity.71,72 The historical female preponderance of NAFLD might reflect type 1 NASH that is reportedly more common in White females, compared with contemporary type 2 NASH which is more common in males.61
Pathophysiology and histology
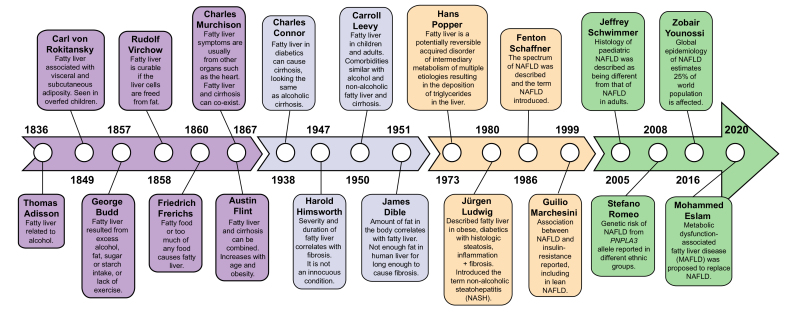
Contrasting with contemporary adult NAFLD histology, many cases of fatty liver described by Virchow10 had a zone 1 distribution of steatosis. Although there is no clear explanation for this discrepancy, Virchow’s description is not entirely inconsistent with the distribution of steatosis in up to 20% of liver biopsies from adults with NAFLD (from the original NAS dataset38) and in a series of children.78 The severity and durations of steatosis that Dible considered a prerequisite for developing liver fibrosis18 are now common. Further, the basic pathogenesis of fatty liver described by Virchow, Murchison, Dible, and Thaler (Fig. 6)10,12,18,21 has similarities to contemporary observations of NAFLD resulting from de novo lipogenesis and lipid influx from the circulation.79 Fig. 7 provides a timeline of our evolving understanding of fatty liver.
Fig 6.
Pathogenesis of fatty liver as described between the 1850s and 1970.
Fatty liver was described as resulting from excessive fat delivery to the liver, increased hepatic lipogenesis, reduced hepatic fat excretion, or reduced hepatic fat oxidation.
Fig 7.
Timeline summarising the evolution of fatty liver knowledge.
Management
Recommended lifestyle changes over nearly two centuries have failed to arrest the rising tide of NAFLD, which has emerged as a growing topic of academic research. Indeed, numerous clinical trials are currently evaluating treatments for NASH, with the aim of fulfilling a major unmet need in those at the highest risk of progression to cirrhosis and its complications. At the time of completing this manuscript there is no approved treatment for NASH. Differences in NAFLD phenotypes and genotypes, alcohol consumption, diet, exercise, severity of metabolic comorbidity, use of concomitant medications and adverse events in clinical trial participants are likely to influence both treatment responses and interpretations of NASH clinical trial results.80
Limitations
The limitations of this review include (a) reliance on accessible historical records with variable clinical characterisation of patients and lifestyle interventions, and (b) only publications in English language or published translations in English were utilised to inform this narrative. Nevertheless, the reports describe the changing epidemiology and knowledge regarding fatty liver.
“Fatty infiltration is normally regarded, in itself, as an innocuous condition; but recent work indicates that it is not so” – Harold Himsworth (1949).
Conclusions
Historical records have depicted features of metabolic-associated fatty liver and fibrosis for over 150 years. Rising population-level trends in obesity, diabetes and other metabolic risk factors provide a prescient warning of a potential cascade of NAFLD, MAFLD, NASH, cirrhosis and HCC cases, as a silent but predictable epidemic. Therefore, there is a need for improved understanding and comprehensive management of metabolic features that place individuals at risk of NASH, cirrhosis, HCC, T2DM and cardiovascular disease.
The NAFLD crisis was a long time coming but now it is growing much faster than predicted.
Financial support
The authors received no financial support to produce this manuscript.
Conflict of interest
The authors declare no conflicts of interest that pertain to this work.
Please refer to the accompanying ICMJE disclosure forms for further details.
Acknowledgements
Associate Professor Leon Adams, Associate Professor Oyedeji Ayonrinde and Professor John Olynyk for critical review of the manuscript; Dr Bastiaan De Boer and Dr Dilini Gunawardena for the contemporary NAFLD histology images; Dr Derrick van Rooyen for illustrating Fig 6, Fig 7.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhepr.2021.100261.
Supplementary data
The following is the supplementary data to this article:
References
- 1.Farrell G.C., Larter C.Z. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43(2 Suppl 1):S99–S112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 2.Wong R.J., Aguilar M., Cheung R., Perumpail R.B., Harrison S.A., Younossi Z.M. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–555. doi: 10.1053/j.gastro.2014.11.039. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg D., Ditah I.C., Saeian K., Lalehzari M., Aronsohn A., Gorospe E.C. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152:1090–1099. doi: 10.1053/j.gastro.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belli L.S., Perricone G., Adam R., Cortesi P.A., Strazzabosco M., Facchetti R. Impact of DAAs on liver transplantation: major effects on the evolution of indications and results. An ELITA study based on the ELTR registry. J Hepatol. 2018;69:810–817. doi: 10.1016/j.jhep.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 6.Addison T. Observations on fatty degeneration of the liver. Guys Hosp Rep. 1836;1:476–485. [Google Scholar]
- 7.Watson Course of clinical lectures: delivered at the Middlesex Hospital. Prov Med J Retrosp Med Sci. 1842;5:103–108. doi: 10.1136/bmj.s1-5.110.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rokitansky C. vol. 2. Sydenham Society; London: 1849. (A Manual of Pathological Anatomy). Translated by William Edward Swaine, Edward Henry Sieveking, Charles Hewitt Moore, George Edward Day. [Google Scholar]
- 9.Budd G. 3rd ed. John Churchill; London: 1857. On diseases of the liver. [Google Scholar]
- 10.Virchow R., Chance F. John Churchill; London: 1860. Cellular Pathology as based upon physiological and pathological histology. Twenty lectures delivered in the pathologic institute of Berlin. 1858. Translated from the second edition of the original by F. Chance. With notes and numerous emendations principally from MS. notes of the author, and illustrated by 144 engravings on wood. [Google Scholar]
- 11.Frerichs F.T. New Sydenham society; 1860. A Clinical treatise on diseases of the liver. Translated from Volume 1 of the original by Charles Murchison. [Google Scholar]
- 12.Murchison C. Clinical Lectures on diseases of the liver. The Lancet. 1867;89:621–622. [Google Scholar]
- 13.Flint A. 2nd ed. Henry C Lea; Philadelphia: 1867. A treatise on the principles and practice of medicine: designed for the use of practitioners and students of medicine. revised and enlarged. [PMC free article] [PubMed] [Google Scholar]
- 14.Connor C.L. Fatty infiltration of the liver and the development of cirrhosis in diabetes and chronic alcoholism. Am J Pathol. 1938;14:347–364. PMID: 19970395. [PMC free article] [PubMed] [Google Scholar]
- 15.Himsworth H.P. Blackwell; Oxford: 1947. Lectures on the liver and its diseases. [Google Scholar]
- 16.Himsworth H.P., Steel J.D. Liver damage of metabolic origin. Proc R Soc Med. 1949;42:201–206. doi: 10.1177/003591574904200401. PMID: 18127908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Best C.H., Hartroft W.S., Lucas C.C., Ridout J.H. Liver damage produced by feeding alcohol or sugar and its prevention by choline. Br Med J. 1949;2(4635):1002–1006. doi: 10.1136/bmj.2.4635.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dible J.H. Degeneration, necrosis and fibrosis in the liver. Br Med J. 1951;1:833–841. doi: 10.1136/bmj.1.4711.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leevy C.M., Ryan C.M., Fineberg J.C. Diabetes mellitus and liver dysfunction; etiologic and therapeutic considerations. Am J Med. 1950;8:290–299. doi: 10.1016/0002-9343(50)90062-3. [DOI] [PubMed] [Google Scholar]
- 20.Leevy C.M. Fatty liver: a study of 270 patients with biopsy proven fatty liver and review of the literature. Medicine (Baltimore) 1962;41:249–276. doi: 10.1097/00005792-196209000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Thaler H. The fatty liver and its pathogenetic relation to liver cirrhosis. Virchows Arch Pathol Anat Physiol Klin Med. 1962;335:180–210. PMID: 13920484. [PubMed] [Google Scholar]
- 22.Dianzani M.U. Sulla patogenesi dell’accumulo del grasso nella steatosi epatica. Rass Med Sarda. 1964;66:67–90. [PubMed] [Google Scholar]
- 23.Popper Hans., John E., Fogarty International Center for Advanced Study in the Health Sciences. International Association for the Study of the Liver . The Center; Bethesda, Md: 1973. Nomenclature, diagnostic criteria, and diagnostic methodology for diseases of the liver and biliary tract. [Google Scholar]
- 24.Adler M., Schaffner F. Fatty liver hepatitis and cirrhosis in obese patients. Am J Med. 1979;67:811–816. doi: 10.1016/0002-9343(79)90740-x. [DOI] [PubMed] [Google Scholar]
- 25.Ludwig J., Viggiano T.R., McGill D.B., Oh B.J. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. PMID: 7382552. [PubMed] [Google Scholar]
- 26.Mallory F.B. Cirrhosis of the liver: five different lesions from which it may arise. Bull Johns Hopkins Hosp. 1911;22:69–75. [Google Scholar]
- 27.Denk H., Gschnait F., Wolff K. Hepatocellar hyalin (Mallory bodies) in long term griseofulvin-treated mice: a new experimental model for the study of hyalin formation. Lab Invest. 1975;32:773–776. PMID: 50498. [PubMed] [Google Scholar]
- 28.Lee R.G. Nonalcoholic steatohepatitis: a study of 49 patients. Hum Pathol. 1989;20:594–598. doi: 10.1016/0046-8177(89)90249-9. [DOI] [PubMed] [Google Scholar]
- 29.Schaffner F., Thaler H. Nonalcoholic fatty liver disease. Prog Liver Dis. 1986;8:283–298. PMID: 3086934. [PubMed] [Google Scholar]
- 30.Diehl A.M., Goodman Z., Ishak K.G. Alcohollike liver disease in nonalcoholics. A clinical and histologic comparison with alcohol-induced liver injury. Gastroenterology. 1988;95:1056–1062. PMID: 3410220. [PubMed] [Google Scholar]
- 31.Matteoni C.A., Younossi Z.M., Gramlich T., Boparai N., Liu Y.C., McCullough A.J. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 32.Brunt E.M., Janney C.G., Di Bisceglie A.M., Neuschwander-Tetri B.A., Bacon B.R. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 33.Marchesini G., Brizi M., Morselli-Labate A.M., Bianchi G., Bugianesi E., McCullough A.J. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med. 1999;107:450–455. doi: 10.1016/s0002-9343(99)00271-5. [DOI] [PubMed] [Google Scholar]
- 34.Cortez-Pinto H., Camilo M.E., Baptista A., De Oliveira A.G., De Moura M.C. Non-alcoholic fatty liver: another feature of the metabolic syndrome? Clin Nutr. 1999;18:353–358. doi: 10.1016/s0261-5614(99)80015-6. [DOI] [PubMed] [Google Scholar]
- 35.Marceau P., Biron S., Hould F.S., Marceau S., Simard S., Thung S.N. Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab. 1999;84:1513–1517. doi: 10.1210/jcem.84.5.5661. [DOI] [PubMed] [Google Scholar]
- 36.Knobler H., Schattner A., Zhornicki T., Malnick S.D., Keter D., Sokolovskaya N. Fatty liver--an additional and treatable feature of the insulin resistance syndrome. QJM. 1999;92:73–79. doi: 10.1093/qjmed/92.2.73. [DOI] [PubMed] [Google Scholar]
- 37.Marchesini G., Brizi M., Bianchi G., Tomassetti S., Bugianesi E., Lenzi M. Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes. 2001;50:1844–1850. doi: 10.2337/diabetes.50.8.1844. [DOI] [PubMed] [Google Scholar]
- 38.Kleiner D.E., Brunt E.M., Van Natta M., Behling C., Contos M.J., Cummings O.W. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 39.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 40.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bambha K., Belt P., Abraham M., Wilson L.A., Pabst M., Ferrell L. Ethnicity and nonalcoholic fatty liver disease. Hepatology. 2012;55:769–780. doi: 10.1002/hep.24726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwimmer J.B., Celedon M.A., Lavine J.E., Salem R., Campbell N., Schork N.J. Heritability of nonalcoholic fatty liver disease. Gastroenterology. 2009;136:1585–1592. doi: 10.1053/j.gastro.2009.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Romeo S., Kozlitina J., Xing C., Pertsemlidis A., Cox D., Pennacchio L.A. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Palmer N.D., Musani S.K., Yerges-Armstrong L.M., Feitosa M.F., Bielak L.F., Hernaez R. Characterization of European ancestry nonalcoholic fatty liver disease-associated variants in individuals of African and Hispanic descent. Hepatology. 2013;58:966–975. doi: 10.1002/hep.26440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krawczyk M., Rau M., Schattenberg J.M., Bantel H., Pathil A., Demir M. Combined effects of the PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 variants on NAFLD severity: a multicenter biopsy-based study. J Lipid Res. 2017;58:247–255. doi: 10.1194/jlr.P067454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu Y.L., Reeves H.L., Burt A.D., Tiniakos D., McPherson S., Leathart J.B. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat Commun. 2014;5:4309. doi: 10.1038/ncomms5309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anstee Q.M., Darlay R., Cockell S., Meroni M., Govaere O., Tiniakos D. Genome-wide association study of non-alcoholic fatty liver and steatohepatitis in a histologically characterised cohort. J Hepatol. 2020;73:505–515. doi: 10.1016/j.jhep.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 48.Angulo P., Kleiner D.E., Dam-Larsen S., Adams L.A., Bjornsson E.S., Charatcharoenwitthaya P. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397. doi: 10.1053/j.gastro.2015.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Day C.P., James O.F. Steatohepatitis: a tale of two “hitsˮ? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 50.Buzzetti E., Pinzani M., Tsochatzis E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD) Metabolism. 2016;65:1038–1048. doi: 10.1016/j.metabol.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 51.Chitturi S., Abeygunasekera S., Farrell G.C., Holmes-Walker J., Hui J.M., Fung C. NASH and insulin resistance: insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology. 2002;35:373–379. doi: 10.1053/jhep.2002.30692. [DOI] [PubMed] [Google Scholar]
- 52.Loomba R., Abraham M., Unalp A., Wilson L., Lavine J., Doo E. Association between diabetes, family history of diabetes, and risk of nonalcoholic steatohepatitis and fibrosis. Hepatology. 2012;56:943–951. doi: 10.1002/hep.25772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abdelmalek M.F., Liu C., Shuster J., Nelson D.R., Asal N.R. Familial aggregation of insulin resistance in first-degree relatives of patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2006;4:1162–1169. doi: 10.1016/j.cgh.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 54.Frenk S., Gomez F., Ramos-Galvan R., Cravioto J. Fatty liver in children; kwashiorkor. Am J Clin Nutr. 1958;6:298–309. doi: 10.1093/ajcn/6.3.298. [DOI] [PubMed] [Google Scholar]
- 55.Marble A., White P., Bogan I.K., Smith R.M. Enlargement of the liver in diabetic children: I. Its incidence, etiology and nature. Arch Intern Med. 1938;62:740–750. doi: 10.1001/archinte.1938.00180160019002. [DOI] [Google Scholar]
- 56.Roosen-Runge E.C. Fatty infiltration of the liver in patients with mongolism and in children with hydrocephaly and microcephaly. Am J Pathol. 1947;23:79–91. PMID: 19970920. [PMC free article] [PubMed] [Google Scholar]
- 57.Moran J.R., Ghishan F.K., Halter S.A., Greene H.L. Steatohepatitis in obese children: a cause of chronic liver dysfunction. Am J Gastroenterol. 1983;78:374–377. PMID: 6859017. [PubMed] [Google Scholar]
- 58.Kinugasa A., Tsunamoto K., Furukawa N., Sawada T., Kusunoki T., Shimada N. Fatty liver and its fibrous changes found in simple obesity of children. J Pediatr Gastroenterol Nutr. 1984;3:408–414. doi: 10.1097/00005176-198406000-00018. [DOI] [PubMed] [Google Scholar]
- 59.Welsh J.A., Karpen S., Vos M.B. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988-1994 to 2007-2010. J Pediatr. 2013;162:496–500. doi: 10.1016/j.jpeds.2012.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Molleston J.P., White F., Teckman J., Fitzgerald J.F. Obese children with steatohepatitis can develop cirrhosis in childhood. Am J Gastroenterol. 2002;97:2460–2462. doi: 10.1111/j.1572-0241.2002.06003.x. [DOI] [PubMed] [Google Scholar]
- 61.Schwimmer J.B., Behling C., Newbury R., Deutsch R., Nievergelt C., Schork N.J. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42:641–649. doi: 10.1002/hep.20842. [DOI] [PubMed] [Google Scholar]
- 62.Teli M.R., James O.F.W., Burt A.D., Bennett M.K., Day C.P. The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology. 1995;22:1714–1719. PMID: 7489979. [PubMed] [Google Scholar]
- 63.Powell E.E., Cooksley W.G., Hanson R., Searle J., Halliday J.W., Powell L.W. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80. doi: 10.1002/hep.1840110114. [DOI] [PubMed] [Google Scholar]
- 64.Adams L.A., Lymp J.F., St Sauver J., Sanderson S.O., Lindor K.D., Feldstein A. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 65.Dam-Larsen S., Franzmann M., Andersen I.B., Christoffersen P., Jensen L.B., Sørensen T.I. Long term prognosis of fatty liver: risk of chronic liver disease and death. Gut. 2004;53:750–755. doi: 10.1136/gut.2003.019984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Adams L.A., Sanderson S., Lindor K.D., Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 67.Kleiner D.E., Brunt E.M., Wilson L.A., Behling C., Guy C., Contos M. Association of histologic disease activity with progression of nonalcoholic fatty liver disease. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.12565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nasr P., Ignatova S., Kechagias S., Ekstedt M. Natural history of nonalcoholic fatty liver disease: a prospective follow-up study with serial biopsies. Hepatol Commun. 2017;2:199–210. doi: 10.1002/hep4.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Younes R., Bugianesi E. NASH in lean individuals. Semin Liver Dis. 2019;39:86–95. doi: 10.1055/s-0038-1677517. [DOI] [PubMed] [Google Scholar]
- 70.Bacon B.R., Farahvash M.J., Janney C.G., Neuschwander-Tetri B.A. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107:1103–1109. doi: 10.1016/0016-5085(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 71.Chalasani N., Younossi Z., Lavine J.E., Charlton M., Cusi K., Rinella M. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 72.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 73.Chitturi S., Farrell G.C. Fatty liver now, diabetes and heart attack later? The liver as a barometer of metabolic health. J Gastroenterol Hepatol. 2007;22:967–969. doi: 10.1111/j.1440-1746.2007.04995.x. [DOI] [PubMed] [Google Scholar]
- 74.Ratziu V., Charlotte F., Heurtier A., Gombert S., Giral P., Bruckert E. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 75.Loria P., Lonardo A., Carulli N. Should nonalcoholic fatty liver disease be renamed? Dig Dis. 2005;23:72–82. doi: 10.1159/000084728. [DOI] [PubMed] [Google Scholar]
- 76.Eslam M., Sanyal A.J., George J. Toward more accurate nomenclature for fatty liver diseases. Gastroenterology. 2019;157:590–593. doi: 10.1053/j.gastro.2019.05.064. [DOI] [PubMed] [Google Scholar]
- 77.Eslam M., Newsome P.N., Sarin S.K., Anstee Q.M., Targher G., Romero-Gomez M. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 78.Africa J.A., Behling C.A., Brunt E.M., Zhang N., Luo Y., Wells A. In children with nonalcoholic fatty liver disease, zone 1 steatosis is associated with advanced fibrosis. Clin Gastroenterol Hepatol. 2018;16:438–446. doi: 10.1016/j.cgh.2017.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Donnelly K.L., Smith C.I., Schwarzenberg S.J., Jessurun J., Boldt M.D., Parks E.J. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115:1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ampuero J., Romero-Gomez M. Stratification of patients in NASH clinical trials: a pitfall for trial success. JHEP Rep. 2020;2:100148. doi: 10.1016/j.jhepr.2020.100148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.