Summary
Purpose
Breast-conservation surgery (BCS) has become a standard treatment option for invasive breast carcinoma (IBC) and ductal carcinoma in situ (DCIS). The strongest predictor of local recurrence remains the surgical margin status. We evaluated the margin positivity by quantifying the tumor on positive margins and analyzing the histologic factors including type and extent in determining the likelihood of residual disease upon re-excision.
Method
Retrospective analysis of 210 BCS performed at Mount Sinai Medical Center from the period of January 2011 - December 2017 revealed that 58 had IBC, DCIS, or both, with positive margins that were followed by re-excision.
Result
The margins had IBC in 18 (31%), DCIS in 32 (55.2%) and both in 8 (13%) cases. Thirty-eight cases (65.5%) were free of carcinoma on re-excision. Of 40 cases with margins positive for DCIS, 16 (40%) had residual DCIS. Of 26 cases with IBC at the margins, and 5 had residual disease (19%). This difference was statistically significant (p = 0.002). Of 21 cases with extensive DCIS, 12 had residual disease (p = 0.02) as compared to only 4 out of 19 without extensive DCIS. None of the cases with clinging/micro-papillary DCIS had residual disease, while 51% of the other types (solid, cribriform, come-do) had residual disease (p = 0.02). The area of DCIS as measured on the involved margin correlated with the amount of residual disease on re-excision (p = 0.03).
Conclusion
Margins positive for DCIS are more likely to have residual disease on re-excision in comparison to margins positive for only IBC. The type and extent of DCIS appears to influence the likelihood of residual disease.
Key words: Early breast cancer, Invasive breast cancer, DCIS, Re-excision, Breast conservation surgery
Introduction
Invasive breast carcinoma (IBC) is the most common cancer affecting women and is a leading cause of death in the United States 1.
Ductal carcinoma in-situ (DCIS) is composed of heterogeneous lesions which exhibit differing clinical behaviors. In DCIS, the cancerous cells arise from the milk ducts of the breast and spread via the duct system. Breast conserving surgery (BCS) aiming at complete removal of DCIS and IBC is an acceptable treatment modality for selected patients 2-4. The advent of screening mammography has led to tumors, both IBC and DCIS, being diagnosed earlier, at sizes that are amenable to BCS 5. Large prospective trials have shown that long term survival rates after BCS are comparable to those of radical mastectomy 3.
However, BCS exposes the patient to a life-long risk of local recurrence 6. This risk can be reduced by wider excision, but extensive resections result in worse cosmetic results. Evaluation of the resection margins is frequently utilized to achieve an optimal balance between adequate local control and cosmetic results.
Local recurrence following BCS has been shown to be influenced by a number of factors which include patient demographics, such as age and tumor characteristics such as size, grade, and multifocality or multicentricity. However, the surgical margin still is the strongest predictor for possible local recurrence 6. According to different studies, the percentage of patients with positive margins ranges from 20 to 40% after partial mastectomy. These patients often undergo a revisit surgery for clear margins 7.
For BCS, the ideal negative margin width above which a re-excision should be advised has been extensively debated over the years. A meta-analysis concluded that increasing the tumor-free margin width did not significantly reduce the odds of local recurrence 8. Since a tumor-positive margin significantly increased the odds of local recurrence, the Society of Surgical Oncology and the American Society for Radiation Oncology (SSO-ASTRO) and European Society for Medical Oncology (ESMO) recently published guidelines recommending no ink on tumor as an adequate margin for IBC and 2 mm from inked margin as adequate margin for DCIS 9,10. Re-excision is advised in cases of positive resection margins. However, the guidelines do not distinguish between focally and extensively positive margins.
Margins in lumpectomy specimens can be evaluated using a radial/perpendicular method or a shaved/en-face method. The recommended method for margin assessment on breast specimens is the perpendicular technique, which allows for the exact measurement of the distance between tumor and the inked margin. This technique allows the pathologist to report the precise distance of the tumor from each margin and distinguishes a truly positive margin (tumor at ink) from a close margin. Running ink, imperfect orientation and surface irregularity of the breast specimen are disadvantages that hinder the effective examination of margins by this method.
Examination of margins by the en-face method allows the oriented specimen to be inked entirely in a single color, thus eliminating the problems caused by running ink. The margins are shaved off parallel to the surface of the specimen at a depth of approximately 0.3 cm. The sections are embedded en-face with the inked surface facing down. The presence of tumor cells anywhere in the section is reported as a positive margin. Unfortunately, the above method precludes the exact measurement of the distance of the tumor from the inked margin. Also many experts argue that this method precludes the examination of the true margin as the true margin is actually lost during processing. The advantages of this method include easier and faster examination, no ink problems and the examination of a larger surface area with fewer histologic sections. This technique is believed to over-call positive margins as demonstrated in prior studies 11.
The aim of this study is to evaluate the margin positivity by quantifying the tumor on the positive margin and analyzing the histologic factors including type of cancer and extent of DCIS in determining the likelihood of residual disease on re-excision.
Materials and methods
This was a retrospective analysis. The case search was performed using “CoPath”, the pathology computerized database application at the Mount Sinai Medical Center, Department of Pathology. The search included all breast excisions (lumpectomy) with positive margins and followed by subsequent re-excisions submitted for evaluation for the period from January 1, 2011 - December 31, 2017.
Cases reported to contain DCIS or invasive breast carcinoma with positive margins followed by re-excision and the subsequent surgical re-excision specimens were included for the study.
The margin closest to the tumor or biopsy site was examined by the perpendicular technique. The margins away from the tumor or biopsy site were shaved off parallel to the surface of the inked specimen at a tissue depth of 0.2-0.3 cm. The sections were then embedded en-face with the inked surface facing down.
Quantification of tumor at the margin was assessed using the software ImageJ 1.51t (National Institutes of Health, USA) on captured and scaled images. For perpendicular margins, the total length of inked margin involvement was measured. In cases with discontinuous involvement, separate lengths were summed. For en-face margins, the total area of involvement and the largest individual linear dimension were measured. The total area of involvement included the neoplasm and its stroma. Measurements of cancerization of lobules by DCIS also included the area occupied by non-neoplastic tissue within the terminal duct lobular unit. Multiple foci, when present, were summed for calculation of the total area. In re-excisions, the largest individual linear dimension of residual tumor was recorded. Additionally DCIS was defined as extensive if greater than 25% of the ducts were involved by DCIS on a single slide.
Statistical analysis was performed using SPSS 22.0. The data was analyzed and found to be non-parametric. Fischer exact, Chi-square, Mann Whitney U test were performed to analyze the data. Correlation using the Spearmann coefficient and ROC curves were also plotted.
Results
A total of 210 cases underwent BCS for invasive and/or DCIS from January 2011 to December 2017 at Mount Sinai Medical Center. Of these 58 cases (27.6%) underwent re-excision for positive margins (Tab. I).
Tab. I.
Baseline characteristics of the study subjects.
| Age (mean ± standard deviation) | 64 ± 13 | |
| Invasive carcinoma only | Ductal | 4 |
| Lobular | 7 | |
| DCIS only | 22 | |
| Invasive carcinoma + DCIS | Ductal | 24 |
| Lobular | 0 | |
| Indeterminate | 1 | |
Of the 58 cases, the positive margins were 45 en-face (77.6%), 9 perpendicular (15.5%) and both in 4 cases (6.9%).The margins were involved by invasive carcinoma in 18 (31%), DCIS in 32 (55.2%) and both in 8 (13%) cases. 20 cases (34.5%) had residual disease on re-excision. Of the en-face margins that were called positive, 37.5 % cases had residual disease on re-excision. Of the perpendicular margins that were positive, 16.6 % had residual disease on re-excision. The rate of residual disease in cases of positive margins for DCIS was 40% (16/40), while the rate was 19% (5/26) for invasive carcinoma. This difference was statistically significant (p = 0.002) (Tab. II).
Tab. II.
Rate of residual disease on re-excision.
| Residual disease on re-excision | No residual disease | P-value | ||
|---|---|---|---|---|
| Type of disease on margin | Invasive carcinoma | 4 | 14 | P > 0.05 |
| DCIS | 13 | 19 | ||
| Both | 3 | 5 | ||
| Extent of DCIS | Extensive | 12 | 9 | P = 0.02 |
| Non-extensive | 4 | 19 | ||
| Type of DCIS | Solid/Cribriform | 13 | 12 | P = 0.02 |
| Clinging/Micropapillary | 0 | 9 | ||
| Comedo | 3 | 3 | ||
Of 21 cases with extensive DCIS, 12 had residual disease as compared to only 4 out of 19 with non-extensive DCIS (p = 0.02). The DCIS was classified as solid/cribriform in 25 cases, clinging/micro-papillary in 9, and comedo in 6 cases. Of the 9 cases with clinging/ micro-papillary DCIS, none had residual disease, while 51% of the other types had disease on re-excision (p = 0.02). The grade of the DCIS did not influence the likelihood of residual disease on re-excision (p = 0.05).
The greatest linear dimension of disease on margin did not correlate with the presence of residual disease in any cohort. However the area of DCIS measured on en-face margins correlated with the residual disease on re-excision (p = 0.03) (Tab. III). ROC curves showed a fair correlation between area of disease measured on the margin and presence of residual DCIS (Fig. 1). The correlation improved from fair to good when the ROC curve was drawn for non-extensive DCIS (Fig. 2).
Tab. III.
Quantitation of tumor on positive margins.
| Residual disease | No residual disease | P-value | |
|---|---|---|---|
| Linear dimension (Perpendicular) |
4.800 (1.457-7.1370) |
2.993 (0.926-20) |
0.149 |
| Area (en-face) | 8.172 (0.7331-39.475) |
4.181 (0.207-33.545) |
0.059 |
Fig. 1.
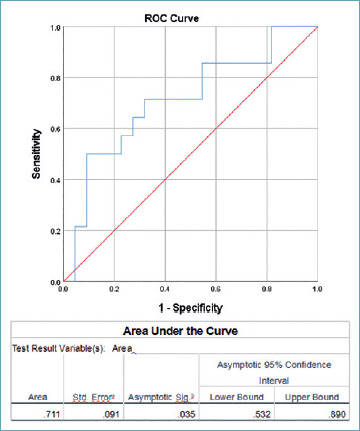
ROC curve showing correlation between area of disease measured on the margin and presence of residual DCIS.
Fig. 2.
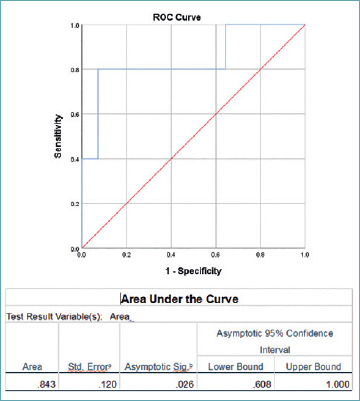
ROC curve showing correlation between area of disease measured on the margin and presence of residual DCIS for non-extensive DCIS.
Discussion
As per SSO-ASTRO Consensus Guidelines for Margins in Breast-Conserving Surgery, a positive margin, defined as tumor on ink for invasive carcinoma or tumor within 2 mm of inked margins in ductal carcinoma in situ (DCIS), is associated with at least a two-fold increase in ipsilateral breast tumor recurrence 9,10.
Optimal compliance with the CAP breast cancer protocols and SSO/ASTRO/ASCO guidelines requires the exclusive use of the perpendicular margin technique, because this is the only proven method that allows visualization of ‘‘tumor on ink’’ and a measurement of the distance between tumor and the inked margins of resection 10.
In a College of American Pathologists Survey that included 866 Laboratories, 76% of respondents reported examining perpendicular margins exclusively, while 23% reported examining en-face margins in at least some circumstances. Respondents who reported using both methods often stated that they evaluate perpendicular margins when grossly obvious tumor is close to the margins, and en-face margins when the tumor is away from margins 12.
The problem arises in cases of DCIS where the tumor is not grossly identifiable making it impossible to identify where the perpendicular section would have tumor closest to the resection margin. Taking one representative perpendicular section of margins located away from the biopsy clip or tumor may lead to under-calling of positive margins, exposing the patient to the risk of residual disease. An alternative is to “bread-loaf” and submit each margin entirely. However, this is time consuming increasing the technical burden, the cost and the turn-around time. En-face margins in this setting are helpful to examine larger surface areas 13.
Previous studies by Moo et al. concluded that the en-face method had a higher rate of positive margins at first excision than perpendicular and cavity-shave methods 14. In our study, 77.6% of the margins examined were taken en-face, only when these margins were located far away enough that the area or lesion of interest could not have been included in the block with a perpendicular orientation. Of the en-face margins that were called positive, 37.5% cases had residual disease on re-excision. This finding suggests that en face margins may actually be a comparable technique for evaluating margins in our institution.
Murphy et al. evaluated 382 patients who underwent lumpectomy for DCIS and invasive carcinoma. They found that the re-excision rate was higher in patients with DCIS than in those with invasive disease 15. Our findings are concordant with the aforementioned study, in the fact that positive margins are more frequently involved by DCIS than invasive carcinoma.
Findlay-Shiras et al. found 62.7% of lumpectomies for invasive carcinoma had residual disease on re-excisions 16. This study exclusively examined perpendicular margins of lumpectomies for invasive cancer. In our study, residual disease was present in 19% of re-excision subsequent to a positive lumpectomy margin for invasive carcinoma. Therefore, invasive carcinoma resections are more accurately evaluated using perpendicular margins exclusively. The use of en-face margins leads to over calling of positive margins and over-treatment for margin positivity.
Regarding margin assessment for DCIS using perpendicular technique, Sigal-Zafrani et al. reported residual tumor in 44% of close non-involved (> 1 mm width) margins 17. In DCIS, the growth of the tumor within the duct system leads to extensive spread and therefore difficulty in localization. This necessitates visualization of more ductal structures on the resection surface to ascertain the adequacy of excision. En-face margins allow for the evaluation of a greater surface area in relatively fewer histological sections. In our study, the use of en-face margins along with the closest margin perpendicular yielded 40% residual disease on re-excisions which is similar to the detection rate of the previous study. These findings further support that en-face margins are comparable to perpendicular margins in assessment of DCIS margins and perhaps better given that a greater surface area can be assessed on en-face margins.
Previous studies attempting to evaluate the tumor burden of DCIS concluded that the majority of extensive disease with positive margins had residual disease on subsequent re-excisions 18. However, the definition of extensive was limited to the disease present on margin. In our study, we classified extensive DCIS as DCIS involving at least 25% of the ducts on one slide. Cases of extensive DCIS according to this definition showed residual disease in 57% of the cases in comparison to only 21% of the cases with non-extensive DCIS whenever the margins had been reported positive.
In our attempt to quantify the disease burden on margins involved by DCIS, we found that an area of disease measuring more than 7.4 mm2 on en-face margins correlated with presence of residual disease on re-excision with a sensitivity and specificity of 64.3% and 72.7%, respectively. The correlation was stronger when only non-extensive DCIS cases were taken into account. In non-extensive DCIS, an area of disease greater than 9.9 mm2 was associated with residual disease on re-excision with a sensitivity and specificity of 80% and 92.9%, which is higher than seen in extensive DCIS. The extensiveness of DCIS reflects a greater burden of disease within the ductal system and thus is a stronger predictor of residual disease on re-excision. In cases where DCIS is not extensive, i.e., the burden of disease is limited, the area of disease on the positive margin is a better predictor of residual disease. This finding needs to be further investigated in a larger sample size in order to assess its effectiveness as a predictor of residual disease and therefore the need for re-excision.
Considering types of DCIS, the clinging/micro-papillary types was not associated with residual disease while other types (including solid, cribriform and comedo) were associated with residual disease in 51% of the cases. The clinging/micro-papillary type appears to be pauci-cellular as compared to the other types further supporting that the volume of the disease is a factor in predicting the presence of residual DCIS.
In conclusion, both the perpendicular and en-face methods for margin evaluation in conservative breast excisions have their advantages and demerits. While the perpendicular method allows for precise measurement of tumor distance from true margin, the en-face method permits faster evaluation of a larger resection surface area. Our study shows that margins positive for DCIS are more likely to have residual disease on re-excision as compared to margins positive for invasive carcinoma. Additionally, the extent and type of DCIS appear to influence the likelihood of residual disease. Extensive DCIS has a higher rate of residual disease as compared to non-extensive DCIS. Margins positive for the clinging/micro-papillary type of DCIS are less likely to have residual disease on re-excision when compared to other DCIS types. The area of DCIS as measured on the positive margin may be a predictor for residual disease. However, more extensive studies are needed to prove the hypothesis.
Figures and tables
Footnotes
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Cancer statistics review 1975-2015. Available at: https://seer.cancer.gov/statfacts/html/common.html [Accessed 2 Jul. 2018].
- 2.Fisher ER, Anderson S, Redmond C, et al. Ipsilateral breast tumor recurrence and survival following lumpectomy and irradiation: pathological findings from NSABP protocol B-06. Semin Surg Oncol 1992;8:161-6. [PubMed] [Google Scholar]
- 3.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [DOI] [PubMed] [Google Scholar]
- 4.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [DOI] [PubMed] [Google Scholar]
- 5.Cady B, Stone MD, Shuler JG, et al. The new era in breast cancer. Invasion, size, and nodal involvement dramatically decreasing as a result of mammographic screening. Arch Surg 1996;131:301. [DOI] [PubMed] [Google Scholar]
- 6.Schnitt SJ. Risk factors for local recurrence in patients with invasive breast cancer and negative surgical margins of excision. Where are we and where are we going? Am J Clin Pathol 2003;120:485-8. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez C, Brem R F, McSwain AP, et al. Factors associated with re-excision in patients with earlystage breast cancer treated with breast conservation therapy. Am Surg 2010;76:331-4. [PubMed] [Google Scholar]
- 8.Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Ann Surg Oncol 2014;21:704. [DOI] [PubMed] [Google Scholar]
- 9.Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Int J Radiat Oncol Biol Phys 2014;88:553-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morrow M, Van Zee KJ, Solin LJ, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology Consensus Guideline on Margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. Ann Surg Oncol 2016;23:3801-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidi AJ, Connolly JL, Harris JR, et al. The relationship between shaved margin and inked margin status in breast excision specimens. Cancer 1997;79:1568-73. [PubMed] [Google Scholar]
- 12.Guidi AJ, Tworek JA, Mais DD, et al. Breast specimen processing and reporting with an emphasis on margin evaluation: a college of american pathologists survey of 866 laboratories. Arch Pathol Lab Med 2018;142:496-506. [DOI] [PubMed] [Google Scholar]
- 13.Chiappa C, Rovera F, Corbenc AD, et al. Surgical margins in breast conservation. Int J Surg 2013;11:S69-72. [DOI] [PubMed] [Google Scholar]
- 14.Moo TA, Choi L, Culpepper C, et al. Impact of margin assessment method on positive margin rate and total volume excised. Ann Surg Oncol 2014;21:86-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murphy BL, Boughey JC, Keeney MG, et al. Factors associated with positive margins in women undergoing breast conservation surgery. Mayo Clin Proc 2018;93:429-35. [DOI] [PubMed] [Google Scholar]
- 16.Findlay-Shirras LJ, Outbih O, Muzyka CN, et al. Predictors of residual disease after breast conservation surgery. Ann Surg Oncol 2018;25:1936-42. [DOI] [PubMed] [Google Scholar]
- 17.Sigal-Zafrani B, Lewis JS, Clough KB, et al. Histological margin assessment for breast ductal carcinoma in situ: precision and implications. Mod Pathol 2004;17:81-8. [DOI] [PubMed] [Google Scholar]
- 18.Neuschatz AC, DiPetrillo T, Steinhoff M, et al. The value of breast lumpectomy margin assessment as a predictor of residual tumor burden in ductal carcinoma in situ of the breast. Cancer 2002;94:1917-24. [DOI] [PubMed] [Google Scholar]


