SUMMARY
Precise perforator mapping of the epifascial and subcutaneous course of the perforator flaps, including the precise detection of the skin point, is mandatory for successful preoperative flap design and planning of supramicrosurgery. We investigated the effectiveness of contrast-enhanced B-flow (BCEUS) imaging for perforator mapping and preoperative perforator flap planning and compared it with B-flow ultrasound, contrast-enhanced ultrasound, and color Doppler ultrasound. Sixteen patients who received an individualized perforator flap reconstruction were included in the study. Preoperative perforator mapping includes the following structures: subfascial course of the pedicle, fascial penetration point, subcutaneous course (epifascial and subcutaneous), and perforator skin point. The precision of the preoperative perforator mapping was analyzed for color Doppler ultrasound, contrast-enhanced ultrasound, B-flow ultrasound, and BCEUS. Each technique was able to precisely display the subfascial course of the vascular pedicle, including the fascial penetration point. However, only BCEUS enabled precise mapping of the epifascial and subcutaneous (suprafascial) course, including the skin point of the perforators with a clear delineation. Precise knowledge of the suprafascial course of the perforators is mandatory for successful supermicrosurgery and perforator flap planning. BCEUS imaging facilitates full perforator mapping, which improves the safety of flap harvesting. However, BCEUS is technically demanding and requires an experienced sonographer.
INTRODUCTION
According to the major dogma of plastic surgery referred to as “form, function, and aesthetics,” the introduction of perforator flaps and supermicroscopy represents a significant development; they simplify reconstructive concepts, reduce donor site morbidity, and no major vessels have to be harvested.1 Furthermore, most reconstructions require a thin adipocutaneous paddle; therefore, prefabricated perforator flaps harvested in the superficial fascial plane have been proposed.2
Reliable perforator mapping, including a detailed knowledge of the epi- and subcutaneous course, including its penetration through the fascia and skin, is required to enable proper preoperative flap design and planning.3–5 Debelmas5 introduced a color Doppler imaging protocol (CDUS) for prefabricated flap planning. They found an accuracy of 5 mm for the fascial penetration point with a sensitivity of 90%. This technique seemed to be more reliable than the hand-held Doppler,4 whereas the computer tomographic angiography6 is still the gold standard for most authors. Furthermore, CDUS does not utilize x-rays and provides dynamic information about perforator perfusion (velocity and diameter). However, the epifascial course of the perforators and the penetration point to the skin (SP) cannot be determined.7 Su1 introduced contrast-enhanced ultrasound imaging (CEUS) for perforator mapping. The injection of ultrasound contrast agents provides additional reflectors, increases the sensitivity for perforator mapping, and can be used in patients with renal insufficiency.3 However, the precise detection of the epifascial and subcutaneous course, including the entrance into the skin, is challenging.4
To overcome this, we evaluated the potential of contrast-enhanced B-flow-imaging (BCEUS) for perforator mapping. The B-flow technique for subcutaneous blood flow visualization (perforator mapping) is independent of the Doppler effect. It relies on a subtraction algorithm and provides spatial resolution similar to B-mode imaging.8 Artifacts, such as aliasing or blooming, are avoided with this technique. The sensitivity for small vessels can be enhanced in B-flow imaging by intravenous contrast agents,9,10 which may enable perforator mapping on a suprafascial level.7,8 This study investigated the potential of BCEUS in comparison with B-flow ultrasound (BUS), CEUS, and CDUS for perforator mapping and flap planning.
MATERIALS AND METHODS
A total of 16 patients who underwent flap graft reconstruction were included in the study (Table 2). Preoperative ultrasound was performed with a LOGIQ E9 scanner (GE Healthcare, Chicago, Ill.) equipped with a linear [2–8 MHz (9L-D)] and a matrix probe [4–15 MHz (ML6-15)].7,8 Perforator mapping included the subfascial course (l), the fascial point (F), the subcutaneous course (epifascial and subcutaneous), and the SP. (See figure, Supplemental Digital Content 1, which illustrates the perforator flaps and their ultrasound imaging. http://links.lww.com/PRSGO/B643.) (See Video [online], which displays the dynamic perforator mapping using contrast-enhanced B-flow. The subcutaneous course of the perforators is clearly visible up to the skin point.)
Table 2.
Perforator Flaps
| No. | Reconstruction Site | Donor Site Morbidity | Flap Size | No. Perforators | Flap Survival, Revision |
|---|---|---|---|---|---|
| Anterolateral thigh flap (ALTP) donor site | |||||
| 1 | Elbow | — | 11 × 19 cm | 1 | +, no revision |
| 2 | Forearm | — | 22 × 8 cm | 2 | + |
| 3 | Hand | — | 9 × 6 cm | 1 | + |
| 4 | Skull | — | 25 × 9 cm | 2 | + |
| 5 | Skull | Dehiscence | 21 × 8 cm | 2 | + |
| 6 | Face/maxilla | — | 18 × 6 cm | 2 | +, revision vein |
| 7 | Foot | — | 14 × 5 cm | 2 | + |
| 8 | Lower leg | — | 30 × 8 cm | 3 | + |
| 9 | Lower leg | Dehiscence | 21 × 8 cm | 2 | + |
| Thoracodorsal artery perforator flap (TDAP) donor site | |||||
| 10 | Lower leg | Dehiscence | 22 × 8 cm | 2 | + |
| 11 | Groin | — | 19 × 7 cm | 1 | +, revision vein |
| 12 | Groin | — | 17 × 6 cm | 1 | + |
| 13 | Tigh | Hypertrophic scar | 19 × 7 cm | 1 | + |
| 14 | Skull | — | 24 × 7 cm | 2 | + |
| Scapular, parascapular flap donor site | |||||
| 15 | Lower leg | Seroma | 15 × 6 cm | — | + |
| 16 | Lower leg | — | 14 × 5 cm | — | + |
Video 1. Video 1 from ”An innovative approach for preoperative perforator flap planning using contrast-enhanced B-Flow imaging”.
The perforators were mapped using each technique, CDUS, CEUS, BUS, and BCEUS, and were documented by cine loops and freeze frames, traced to the skin, and photographed (Table 1) (See figure, Supplemental Digital Content 1. http://links.lww.com/PRSGO/B643.). CEUS and BCEUS required an intravenous bolus injection of 2.5 mL of SonoVue10 (Bracco, Italy). According to the principles of supermicrosurgery, the customized size and geometry of the raised flaps were designed according to blood supply and number of perforators, including their central SP. Flap design was performed according to BCEUS mapping. In the operating room, all perforator flaps were dissected on an epi- and suprafascial plane initially, followed by subfascial dissection of the pedicle. (See figure, Supplemental Digital Content 1. http://links.lww.com/PRSGO/B643.) The accuracy for each technique was analyzed by calculating the metric deviations of its actual and preplanned course (SPSS 27.0, Table 1).
Table 1.
Precision of Perforator Mapping
| Perf. Imaging | Subfascial Course of Pedicle (l) and Fascial Point (F) | Subcutaneous Course of Perforators Epifascial Subcutaneous | SP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Δ l (mm) | D (mm) | F (Del.) | Δ l (mm) | D (mm) | Del | Δ l (mm) | D (mm) | Del | Δ l (mm) | D (mm) | Del. | Sens (%). | |
| CDUS | 6 | ±1.2 | + | – | – | – | – | – | – | – | – | – | – |
| CEUS | 6.5 | ±1.03 | ++ | – | – | +/– | – | – | – | – | – | – | – |
| BUS | 7 | ±1.55 | ++ | 6 | ±0.73 | +/– | – | – | – | – | – | +/– | 45% |
| BCEUS | 6 | ±0.73 | ++ | 4 | ±1.15 | ++ | 4 | ±0.98 | ++ | 3 | ±1.12 | ++ | 96% |
Data were analyzed using SPSS (27.0) statistical software. All variables were tested for normal distribution using the Shapiro−Wilk test. Differences in the subfascial, epifascial, and subcutaneous plane were compared using Kruskal-Wallis and Mann-Whitney test as it was appropriate. All tests were performed at a 5% level of significance. Bonferroni adjustment was used to counteract the problem of multiple comparisons; P values were adjusted accordingly. No significances were seen (P > 0.05).
Perf. = Perforator, Δ l = mean l imaging - l real, D = stand. Deviation, F = fascial penetration point, Sig. = Significance, Del. = Delineation, Sens. = Sensitivity
RESULTS
Sixteen perforator flaps were raised (Table 2), and the accuracy of the perforator mapping was recorded (Table 1, Fig. 1). Each ultrasound technique was able to precisely display the subfascial course of the vascular pedicle, including the fascial penetration point. However, only the BCEUS technique enabled precise mapping of the epifascial and subcutaneous course with a clear delineation and a precision of 4 mm, whereas BUS was able to show the entire subcutaneous course. The essential perforator SP, which should always be in the center of the flap harvest, could only be visualized using BCEUS. The precision was 3 mm (±1.12) with a sensitivity of 96%. The delineation using BUS was unreliable, with a sensitivity of only 45%. The other techniques could not reliably display the SP and the epifascial or subcutaneous course of the perforators (See figure, Supplemental Digital Content 1. http://links.lww.com/PRSGO/B643.)
Fig. 1.
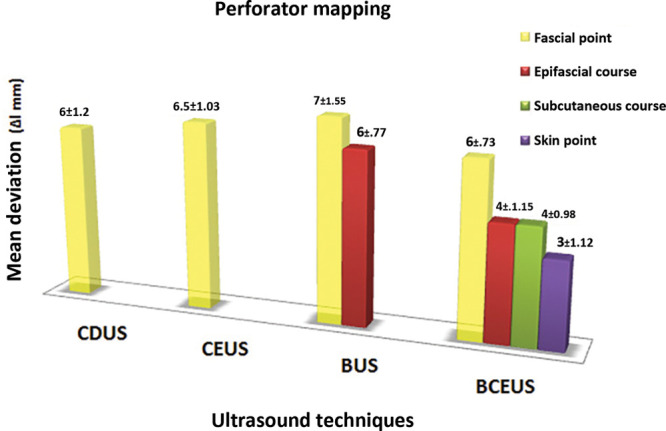
The bar graph displays the precision for each technique. Only BCEUS enabled entire perforator mapping, including the subcutaneous course, the fascial point, and the perforator skin point. The BUS was clearly able to delineate the epifascial and subfascial course, including the fascial point, in contrast to CDUS and CEUS only being able to delineate the subfascial course and fascial point.
DISCUSSION
The advantages of perforator flaps are recognized globally, as the increased number of options regarding the harvest of fasciocutaneous flaps enables greater surgical variability and is associated with decreased donor site morbidity.9 However, due to anatomical variations, precise perforator mapping on a suprafascial level, including the skin point which should be in the exact center, is very helpful in complex cases for quick and successful perforator flap planning and harvest. Previous studies recommended CDUS5 and CEUS1 for perforator mapping; however, they cannot precisely and reliably visualize the full epifascial course or the skin point. Even special Doppler-based technologies with high sensitivities display interruptions in tortuous vessels due to unfavorable Doppler angles. This can be omitted by using non-Doppler algorithms such as BCEUS. Although computerized tomography and magnetic resonance imaging angiography are considered ideal for perforator mapping,5 they cannot provide hemodynamic information and its precise transformation to the body is difficult. Therefore, we recommend BCEUS for perforator mapping because the SP and the epifascial course can be visualized with a clear delineation. Besides these promising results, further challenges remain. Three-dimensional stacks cannot be obtained using BUS or BCEUS due to the large amount of data that requires processing. However, this may be solved with new rendering options. Thus, 4-dimensional BCEUS would be desirable. Additionally, Doppler-based technologies such as Superb Microvascular Imaging (Canon Medical), MicroFlow Imaging (Philips Healthcare), or optimized Power Doppler settings should be tested vigorously for perforator mapping. Indeed, further studies are required with larger numbers of subjects, including valuable hemodynamic parameters of the perforators such as peak velocity and resistance index for a quality assessment of the perforators.
CONCLUSIONS
Precise knowledge of the suprafascial course of perforators is mandatory for successful perforator flap planning. BCEUS requires an experienced sonographer, since the amplifying effect of the contrast medium is limited in time. BCEUS improves the safety of flap harvest.
ACKNOWLEDGMENT
The institutional review board approved this study, waiving written informed consent due to its retrospective nature.
Supplementary Material
Footnotes
Published online 21 May 2021.
Drs Heneweer and Zirk contributed equally to this work.
Presented at the German Radiology Congress, May 29–June 1, 2019, Leipzig, Germany.
Disclosure: All the authors have no financial interest in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Su W, Lu L, Lazzeri D, et al. Contrast-enhanced ultrasound combined with three-dimensional reconstruction in preoperative perforator flap planning. Plast Reconstr Surg. 2013; 131:80–93. [DOI] [PubMed] [Google Scholar]
- 2.Hong JP, Chung IW. The superficial fascia as a new plane of elevation for anterolateral thigh flaps. Ann Plast Surg. 2013; 70:192–195. [DOI] [PubMed] [Google Scholar]
- 3.Feng S, Min P, Grassetti L, et al. A prospective head-to-head comparison of color Doppler ultrasound and computed tomographic angiography in the preoperative planning of lower extremity perforator flaps. Plast Reconstr Surg. 2016; 137:335–347. [DOI] [PubMed] [Google Scholar]
- 4.Ono S, Hayashi H, Ohi H, et al. Imaging studies for preoperative planning of perforator flaps: an overview. Clin Plast Surg. 2017; 44:21–30. [DOI] [PubMed] [Google Scholar]
- 5.Debelmas A, Camuzard O, Aguilar P, et al. Reliability of color doppler ultrasound imaging for the assessment of anterolateral thigh flap perforators: a prospective study of 30 perforators. Plast Reconstr Surg. 2018; 141:762–766. [DOI] [PubMed] [Google Scholar]
- 6.Imai R, Matsumura H, Tanaka K, et al. Comparison of Doppler sonography and multidetector-row computed tomography in the imaging findings of the deep inferior epigastric perforator artery. Ann Plast Surg. 2008; 61:94–98. [DOI] [PubMed] [Google Scholar]
- 7.GE Healthcare. Flow Imaging, LOGIQ E10 Series. General Electric Company;2020. Available at: http://www.gehealthcare.com.au/Ijssmedia/fe8dObe639e544139fea346561401715.pdf?la=en-au. Accessed February 15, 2021.
- 8.Cosgrove D, Lassau N. Imaging of perfusion using ultrasound. Eur J Nucl Med Mol Imaging. 2010; 37(Suppl 1):S65–S85. [DOI] [PubMed] [Google Scholar]
- 9.Hong JP, Koshima I. Using perforators as recipient vessels (supermicrosurgery) for free flap reconstruction of the knee region. Ann Plast Surg. 2010; 64:291–293. [DOI] [PubMed] [Google Scholar]
- 10.International Contrast Ultrasound Society (ICUS). Video ceus watch CEUS demonstrations. Available at: http://icus-society.org/?s=video+ceus watch CEUS demonstrations. Accessed February 15, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


