Abstract
Background:
Numerous diagnostic imaging measurements related to patellar instability have been evaluated in the literature; however, little has been done to compare these findings across multiple studies.
Purpose:
To review the different imaging measurements used to evaluate patellar instability and to assess the prevalence of each measure and its utility in predicting instability. We focused on reliability across imaging modalities and between patients with and without patellar instability.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
We performed a systematic review of the literature using the PubMed, SCOPUS, and Cochrane databases. Each database was searched for variations of the terms “patellar instability,” “patellar dislocation,” “trochlear dysplasia,” “radiographic measures,” “computed tomography,” and “magnetic resonance imaging.” Studies were included if they were published after May 1, 2009, and before May 1, 2019. A meta-analysis using a random effects model was performed on several measurements, comparing instability and control groups to generate pooled values.
Results:
A total of 813 articles were identified, and 96 articles comprising 7912 patients and 106 unique metrics were included in the analysis. The mean patient age was 23.1 years (95% CI, 21.1-24.5), and 41% were male. The tibial tubercle–trochlear groove (TT-TG) distance was the most frequently included metric (59 studies), followed by the Insall-Salvati ratio and Caton-Deschamps index (both 26 studies). The interobserver intraclass correlation coefficients were excellent or good for the TT-TG distance and Insall-Salvati ratio in 100% of studies reporting them; however, for the Caton-Deschamps index and Blackburne-Peel ratio, they were excellent or good in only 43% and 40% of studies. Pooled magnetic resonance imaging values for TT-TG distance (P < .01), Insall-Salvati ratio (P = .01), and femoral sulcus angle (P = .02) were significantly different between the instability and control groups. Values for tibial tubercle–posterior cruciate ligament distance (P = .36) and Caton-Deschamps index (P = .09) were not significantly different between groups.
Conclusion:
The most commonly reported measurements for evaluating patellar instability assessed patellar tracking and trochlear morphology. The TT-TG distance was the most common measurement and was greater in the patellar instability group as compared with the control group. In addition, the TT-TG, tibial tubercle–posterior cruciate ligament, and patellar tendon–trochlear groove distances were highly reproducible measurements for patellar tracking, and the Insall-Salvati ratio had superior reproducibility for assessing patellar height.
Keywords: patellar instability, radiologic measurements, TT-TG distance
Patellar instability is a common yet complex knee condition, with the highest incidence reported in 14- to 18-year-old patients.92 Sanders et al92 reported the annual incidence of first-time patellar dislocations to be 23.2 per 100,000 person-years. In addition to clinical examination findings, numerous anatomic variables identified through diagnostic imaging have been shown in the literature to contribute to patellar instability.105,121 These imaging criteria have been utilized to characterize trochlear morphology, patellar tracking, patellar morphology, and patellar height—major interdependent variables implicated in patellar instability. In addition to their diagnostic utility, measurements such as the tibial tubercle–trochlear groove (TT-TG) distance, sulcus angle, Insall-Salvati ratio, Blackburne-Peel ratio, and trochlear morphology classifications help guide clinical and surgical decision making.9,57,87,101,108 Researchers have continued to search for accurate and reliable measurements of various radiographic features of the knee in determining the underlying cause of patellar instability and planning possible surgical intervention.
While some measurements are used more commonly than are others, there has been a recent surge in new measurements and modifications of traditional measurements reported in the literature.13,15,18,19,22,26,32 Additionally, the imaging modality and technique of choice for several of these measurements remain to be determined.1,17,20 Furthermore, there is little consensus on the reliability and reproducibility of these various imaging metrics. For instance, Hinckel et al55 noted a difference in TT-TG distances when comparing magnetic resonance imaging (MRI) with computed tomography (CT) imaging. Smith et al102 also demonstrated generally poor inter- and intrarater reliability for several common radiologic measurements for patellar height.
The purpose of this study, therefore, was to provide a thorough review of the radiographic imaging measurements in the evaluation of patellar instability. We focused on the frequency of citation for these measurements, their reliability and reproducibility, and the numeric values of the various measurements across different imaging modalities and between patients with patellar instability and controls. The purpose was not to find a singular best study but rather to identify commonly reported and reliable measures of patellofemoral anatomy with regard to patellar instability.
Methods
Search Criteria
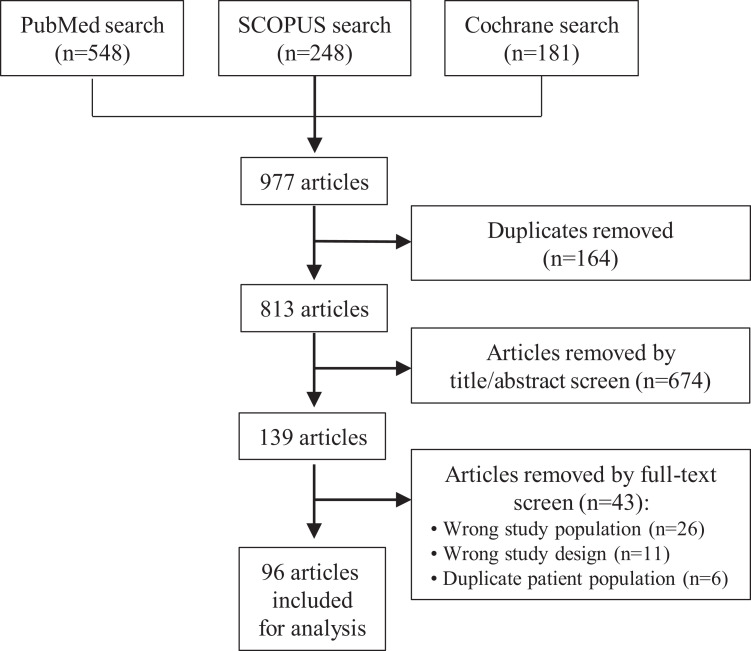
We performed a systematic review of the literature on diagnostic and predictive imaging measurements for patellar instability using the PubMed, SCOPUS, and Cochrane databases. Each database was searched for several variations of the terms “patellar instability,” “patellar dislocation,” “trochlear dysplasia,” “imaging measurement,” “radiographic measures,” “computed tomography,” and “magnetic resonance imaging.” Article screening was completed by 2 independent reviewers (D.B.C. and D.P.H.). PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria were followed throughout the systematic review process (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Duplicate studies were removed, and cohorts were assessed to ensure that patients were not included more than once for the same radiologic measurement in the analysis. All articles that remained were screened by title and abstract, followed by a full-text analysis as indicated.
Study inclusion criteria were level 4 evidence or greater and assessment of imaging measurements related to patellar instability in humans. Studies were included if they were published in English after May 1, 2009, but before May 1, 2019, and had a mean patient population age between 16 and 50 years. Studies were excluded if they included animal subjects, cadaveric specimens or skeletally immature patients; assessed measurements not related to patellar instability; or included patients who underwent previous surgery to the knee being studied. Systematic reviews, simple operative technique reports, and any studies with level 5 evidence were excluded. If a study reported only postoperative measurements, it was excluded. After the initial screening process, the references of the included articles were reviewed to evaluate for potentially missed articles.
Data Extraction
Demographic data and the types of imaging modalities were recorded for each study. The names of all imaging measurements were recorded, and their values were extracted for quantitative analysis. Reporting of means and SDs was required for individual study data to be included in the quantitative analysis. Additionally, surgical studies that limited inclusion of patients based on predetermined measurement cutoffs, such as TT-TG >20 mm and Insall-Salvati ratio >1.2, were excluded from the quantitative analysis to prevent skewing of the results. However, these studies were still included in the qualitative section of the article. Imaging reliability data were extracted in the form of inter- and intrarater intraclass correlation coefficients (ICCs). Inter- and intraobserver ICC values were classified according to the guidelines established by Koo and Li,63 who described ICC values ≥0.9 as excellent, between 0.75 and 0.89 as good, between 0.5 and 0.74 as moderate, and <0.5 as poor. Additionally, the primary findings from each study were collected and summarized and appear in Appendix 1 (available online as Supplemental Material). The number of times that each measurement was utilized was tallied, and each measurement was assigned to 1 of the following categories: patellar tracking, trochlear morphology, patellar height, patellar morphology, patellar inclination, or soft tissue description. Two independent reviewers (D.B.C. and D.P.H.) assessed risk of bias using the Cochrane tool for randomized controlled trials, the Newcastle-Ottawa quality assessment scale for cohort and case-control studies, and the Joanna Briggs critical appraisal tool for case series.60
Statistical Analysis
For quantitative analysis, baseline demographics and imaging measurements were stratified by instability and control groups. If data from instability and control groups were presented in at least 3 studies for a given instability measurement, the measurement was included for further quantitative analysis. A meta-analysis using a random effects model was then performed on these subgroups to generate a pooled value with 95% CI. Heterogeneity was assessed using the I 2 test. Data analysis and forest plot generation were completed using R Version 3.4.2 (R Foundation for Statistical Computing). The meta-analysis in R was completed using the meta package, with a P value <.05 considered statistically significant.
Results
A total of 813 articles was identified in the literature after removal of duplicates. After appropriate screening, 96 articles comprising 7912 patients were included for analysis (Figure 1).∥ The mean age was 23.1 years (95% CI, 21.1-24.5), and 41% of the sample was male (Table 1). There was no difference in age, height, and body mass index between the instability and control groups (P ≥ .2). However, differences in sex were statistically significant, as female patients composed 63% and 51% of the instability and control groups, respectively (P < .01). A total of 89 studies examined 6573 patients with instability, which included patients with first-time and multiple episodes of patellar dislocation. Of these articles, 55 examined a subgroup of control patients (n = 1349), defined as asymptomatic patients with no history of patellofemoral dislocation or patients with alternative knee pathology. After consolidation of synonymous terms and like measurements, there were 106 unique measurements: 39 were categorized as patellar tracking; 38, as trochlear morphology; 11, as patellar height; 10, as soft tissue description; and 4 each, as patellar morphology and patellar inclination. The most common measurements are presented by category in Table 2. The full list of measurements, ranked by number of studies with their assigned category, and the individual forest plots from our statistical analysis are provided in Appendix 2 (available online as Supplemental Material). The definitions of common measurements are provided by diagram and mathematical description in Figure 2.
Table 1.
Pooled Demographic Data Between the Instability and Control Groupsa
| Patellar Instability Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|
| No. of Studies | No. of Patients | Pooled Value (95% CI) | No. of Studies | No. of Patients | Pooled Value (95% CI) | P Value | |
| Male, % | 73 | 1502 | 37 (34-40) | 39 | 1129 | 49 (44-55) | <.01 |
| Age, y | 43 | 2471 | 22.56 (20.91-24.21) | 23 | 1343 | 24.62 (21.95-27.29) | .2 |
| BMI | 10 | 476 | 23.97 (22.04-25.9) | 6 | 264 | 23.49 (20.50-26.48) | .79 |
| Height, cm | 3 | 139 | 167.93 (157.38-178.48) | 2 | 68 | 166.13 (153.02-179.24) | .83 |
a556 males and 946 females in the patellar instability group; 553 males and 576 females in the control group. BMI, body mass index.
Table 2.
Most Commonly Reported Measurements by Category for the Assessment of Patellar Instabilitya
| Measurement | No. of Studies |
|---|---|
| Patellar tracking | |
| TT-TG distance | 59 |
| Congruence/Merchant angle | 13 |
| Patellar lateral displacement shift | 9 |
| TT-PCL distance | 9 |
| 2-/3-dimensional knee rotation angle | 6 |
| Tibial/tibial tubercle torsion | 6 |
| Trochlear morphology | |
| Femoral/trochlear sulcus angle | 19 |
| Dejour classification | 12 |
| Trochlear groove depth | 10 |
| Lateral trochlear or facet inclination / tilt angle | 9 |
| Patellar height | |
| Insall-Salvati/modified Insall-Salvati ratio | 26 |
| Caton-Deschamps index | 26 |
| Blackburne-Peel ratio | 5 |
| Patellar trochlear index | 5 |
| Patellar inclination | |
| Patellar tilt, inclination angle, lateral patellofemoral angle | 22 |
| Lateral patellofemoral angle | 6 |
| Soft tissue description | |
| MPFL thickness | 5 |
| VMO morphology | 3 |
| Patellar morphology | |
| Patellofemoral contacting surface ratio | 2 |
| Wiberg classification | 2 |
| Patellar length | 2 |
aMPFL, medial patellofemoral ligament; TT-PCL, tibial tubercle–posterior cruciate ligament; TT-TG, tibial tubercle–trochlear groove; VMO, vastus medialis obliquus.
Figure 2.
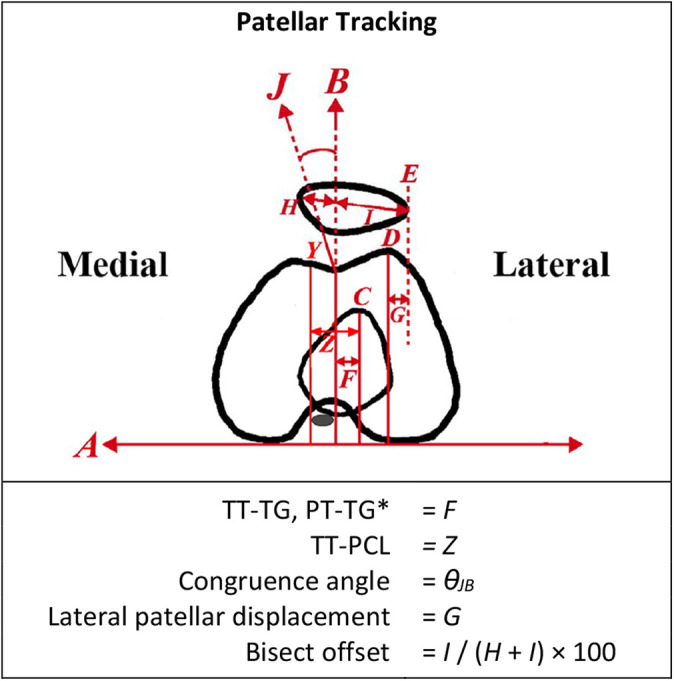
Axial diagram of the knee describing common parameters used to assess patellar tracking. A is drawn horizontally across the posterior femoral condyles. B is drawn perpendicular to A, passing through the deepest point of the femoral sulcus. C is drawn on an inferior cut from line A to the most anterior portion of the tibial tubercle. Y is a line drawn parallel to C alongside the medial border of the PCL. Z is the distance between C and Y. D is the height of the lateral femoral condyle, drawn perpendicular to A. E is drawn perpendicular to A, crossing the most lateral aspect of the patella. F is the distance between B and C; G is the distance between D and E. H and I form a line bisecting the patella. H is the distance from B to the most medial aspect of the patella; I is the distance from B to the most lateral aspect of the patella. J is a reference line drawn from the deepest point of the femoral sulcus, passing through the inferior patellar pole. *TT-TG and PT-TG are measured in a similar manner. The PT-TG measurement is from the center of the patellar tendon to the center of the trochlear groove. The TT-TG measurement is from the center of the tibial tubercle to the center of the trochlear groove. For the purposes of this diagram, they are the same measurement. PCL, posterior cruciate ligament; PT-TG, patellar tendon–trochlear groove; TT-PCL, tibial tubercle–posterior cruciate ligament; TT-TG, tibial tubercle–trochlear groove.
Patellar Tracking
Patellar tracking was the most commonly studied category, with 39 unique measures cited in the literature. A total of 59 studies examined TT-TG distance in some manner, and it was the most cited measurement in the patellar tracking category and overall. The second-most reported measurement in the patellar tracking category was the congruence or Merchant angle (13 studies).¶ Five of 6 studies (83%) that measured TT-TG distance using CT22,44,55,77,106,112 and 9 of 15 study populations (13 studies)# (60%) that measured TT-TG distance using MRI reported interobserver ICCs >0.9.** However, all studies reported interobserver ICCs >0.75 for TT-TG distance, regardless of imaging modality. Three of 4 studies (75%) reported ICCs >0.9 for the tibial tubercle–posterior cruciate ligament (TT-PCL) measurement,19,31,51 and 1 of 4 studies reported an ICC between 0.75 and 0.9.98 Pooled TT-TG measurements are depicted in Table 3. The pooled mean TT-TG distance for patients with instability was 13.61 mm (95% CI, 12.24-14.97) as measured using MRI and 15.89 mm (95% CI, 14.08-17.70) as measured using CT, whereas the pooled mean TT-TG distance for the control group was 10.24 mm (95% CI, 8.45-12.02) using MRI and 12.61 mm (95% CI, 10.47-14.74) using CT. Among patients with instability, the TT-TG distance as measured using CT was just shy of statistical significance when compared to MRI (P = .05).
Table 3.
Pooled Quantitative Data for the Most Common Measurements Comparing the Instability and Control Groupsa
| Patellar Instability Group | Control Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | No. of Knees | Pooled Value (95% CI) | I 2, % | No. of Studies | No. of Knees | Pooled Value (95% CI) | I 2, % | P Value | |
| TT-TG: MRI | 29 | 2110 | 13.61 mm (12.24-14.97) mm | 0 | 17 | 1109 | 10.24 mm (8.45-12.02) mm | 0 | <.01 |
| TT-TG: CT | 12 | 729 | 15.89 mm (14.08-17.70) mm | 0 | 7 | 392 | 12.61 mm (10.47-14.74) mm | 0 | .02 |
| Insall-Salvati ratio | 10 | 815 | 1.31 (1.21-1.41) | 0 | 8 | 503 | 1.14 (1.05-1.23) | 4 | .01 |
| Caton-Deschamps index | 10 | 947 | 1.16 (1.05-1.26) | 0 | 6 | 478 | 1.02 (0.90-1.14) | 0 | .09 |
| Femoral sulcus angle | 5 | 387 | 158.46° (145.84°-171.08°) | 93 | 3 | 139 | 142.09° (135.36°-148.82°) | 0 | .02 |
| TT-PCL | 6 | 381 | 21.38 (17.88-24.88) | 0 | 5 | 342 | 19.18 (16.04-22.33) | 0 | .36 |
aAll measurements were compared using MRI measurements, with the exception of TT-TG, which also compared CT measurements separately. CT, computed tomography; MRI, magnetic resonance imaging; TT-PCL, tibial tubercle–posterior cruciate ligament; TT-TG, tibial tubercle–trochlear groove.
Trochlear Morphology
The second-most encountered measurement category was trochlear morphology with 38 unique measurements. The most cited measures included trochlear or femoral sulcus angle (19 studies),†† the Dejour classification (12 studies),‡‡ trochlear groove depth (10 studies),§§ and lateral trochlear or facet inclination/tilt angle (9 studies).3,5,12,25,30,35,62,68,81 Three studies reported 4 unique interobserver ICCs for sulcus angle, and all of these values were between 0.75 and 0.9.46,48,69 The pooled mean sulcus angle among patients with instability was 158.5° (95% CI, 145.8°-171.08°) and among controls was 142.1° (95% CI, 135.4°-148.8°) (P = .02) (Figure 3).
Figure 3.
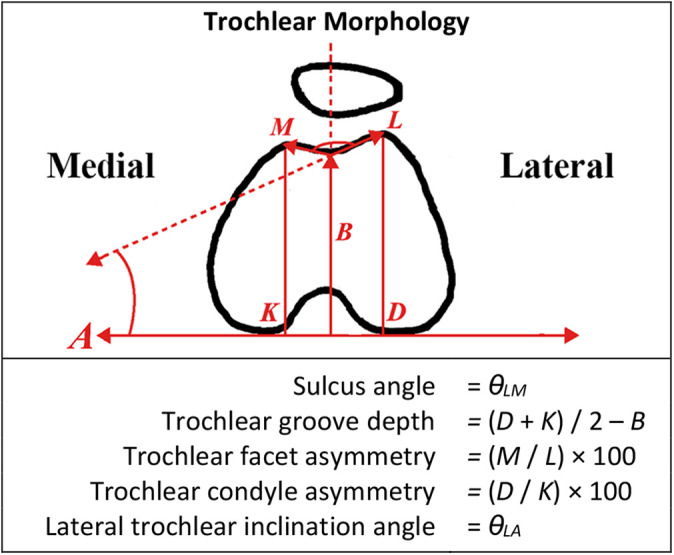
Axial diagram of the knee describing common parameters used to assess trochlear morphology. A is drawn horizontally across the posterior femoral condyles. B is drawn perpendicular to A, passing through the deepest point of the femoral sulcus. D and K are the lengths of the lateral and medial femoral condyles, respectively. L and M are the lengths of the lateral and medial trochlear facets, respectively.
Patellar Height
There were 11 unique metrics related to patellar height. The most commonly encountered measurements were the Caton-Deschamps index (26 studies)∥∥ and Insall-Salvati ratio (26 studies).¶¶ Five studies reported the Blackburne-Peel ratio.7,48,78,89,116 Three of 8 studies reported 4 separate interobserver ICC values >0.9 for the Insall-Salvati ratio,13,68,69 while zero of 7 studies reported an interobserver ICC >0.9 for the Caton-Deschamps index. The Caton-Deschamps index and Blackburne-Peel ratio interobserver ICC’s were excellent or good in just 43% and 40% of studies, respectively. The pooled mean Insall-Salvati ratios for the instability and control groups were 1.31 (95% CI, 1.21-1.41) and 1.14 (95% CI, 1.05-1.23), respectively. The pooled mean Caton-Deschamps values for the instability and control groups were 1.16 (95% CI, 1.05-1.26) and 1.02 (95% CI, 0.90-1.14). The difference between the instability and control groups for the Insall-Salvati ratio was statistically significant (P = .01) but was not different for the Caton-Deschamps index (P = .09) (Figure 4).
Figure 4.
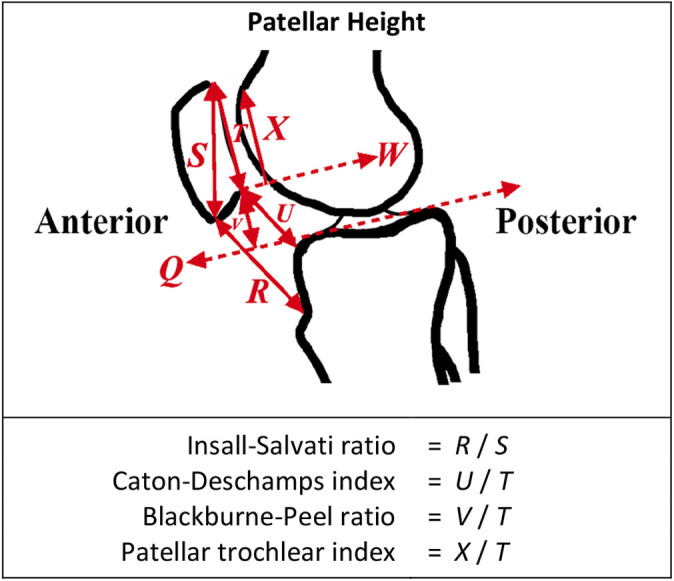
Sagittal diagram of the knee describing common parameters used to assess patellar height. Q is drawn tangent to the tibial plateau articular surface in the sagittal plane. R is the patellar tendon length. S is the patellar length, from superior pole to inferior. T is the length of the patellar articular surface. U is drawn from the inferior margin of the patella to the anterior superior tibial joint surface. V is a line drawn perpendicularly from a horizontal reference line across the tibial plateau to the inferior articular surface of the patella. X is the distance from the superior aspect of the femoral articular cartilage to line W, which is a horizontal reference line perpendicular to the inferior margin of the patellar articular surface.
Other Categories
Of the 4 unique measurements in the patellar inclination category, the patellar tilt angle was the most common (22 studies)## (Figure 5). There were 10 unique measurements in the category of soft tissue description, including medial patellofemoral ligament thickness, vastus medialis obliquus morphology, medial patellofemoral ligament length, and stress shift ratios. Four unique measurements were cited that fit into the category of patellar morphology (Appendix 2, available online as Supplemental Material).
Figure 5.
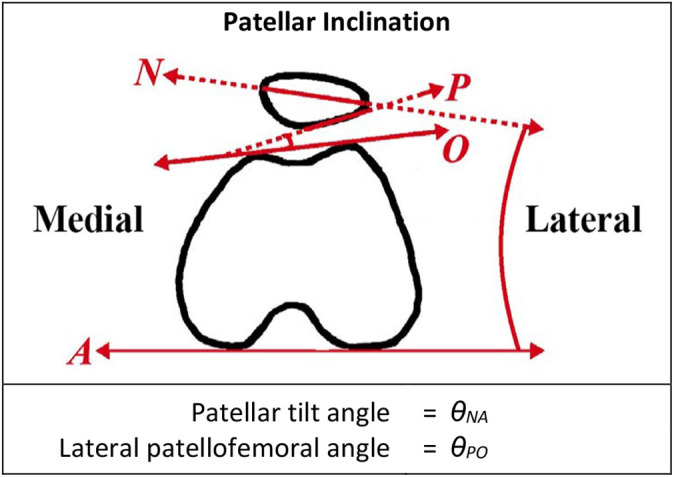
Axial diagram of the knee describing common parameters used to assess patellar inclination. A is drawn horizontally across the posterior femoral condyles. O is a line drawn across the anterior surface of the femoral condyles. P is a line intersecting O and passing along the lateral articular surface of the patella. N is a line passing through the medial and lateral poles of the patella.
Assessment of Risk of Bias
The Cochrane tool identified risk of bias for each of the 3 randomized controlled trials as having “some concerns.”43,61,70 The Newcastle-Ottawa quality assessment scale for cohort and case-control studies was a mean of 7.17 of 9, denoting a fair quality of studies. Finally, the Joanna Briggs critical appraisal tool for case series identified just 2 of 33 studies as being at a high risk for bias,12,13 with the remaining 31 being low risk.a The assessments of risk of bias for the included studies are presented in Appendix 3 (available online as Supplemental Material).
Discussion
The primary findings of this study are multifold. For one, the most commonly reported measurements in the literature for evaluating instability assessed patellar tracking and trochlear morphology, with the most common individual measurement being the TT-TG distance. Additionally, TT-TG, TT-PCL, and patellar tendon–trochlear groove (PT-TG) distances were highly reproducible metrics in the assessment of patellar tracking. For patellar height, the Insall-Salvati ratio had superior imaging reproducibility relative to the Caton-Deschamps index and Blackburne-Peel ratio. Finally, the TT-TG distance, Insall-Salvati ratio, and femoral sulcus angle were significantly greater in patients with instability as compared with controls, while the Caton-Deschamps index and TT-PCL distance were not significantly different between groups.
There is a large breadth of literature on patellofemoral imaging for diagnostic, predictive, and surgical planning purposes. Presumably, this expanse of research is related to the wide spectrum of anatomic factors related to the pathology of lateral patellar instability. In an MRI study of patients with primary patellar dislocation, Arendt et al3 found patellar height and trochlear dysplasia to be the most common risk factors; however, they found no predominant pattern in their population. Furthermore, a systematic review on the evaluation of trochlear dysplasia found 33 unique measurements in the literature, recommending 6 of them based on an assessment of their reliability.86 The surplus of unreliable metrics on the topic proves just how little consensus there is surrounding diagnostic imaging measurements. Likewise, planning for bony realignment procedures involving tibial tubercle osteotomy has found good utility in patellar tracking measurements, including the TT-TG distance.44 It should be noted, however, that the predictability of the static TT-TG measurement related to dynamic patellar tracking has been brought into question.24 The present study sought to categorize the 106 unique measurements identified in the literature as a way to qualitatively organize this information for clinicians. Six broad categories were established: patellar morphology, patellar height, patellar inclination, patellar tracking, trochlear morphology, and soft tissue description. Although these categories were not mutually exclusive, they served to organize the various measurements. The most commonly represented categories were patellar tracking and trochlear morphology or dysplasia, with 39 and 38 unique measurements, respectively.
Merchant et al76 described the use of radiography in 1974 to assess for instability using Insall-Salvati ratio, sulcus angle, and congruence angle with the knee flexed to 45°. Kujala et al64,65 expanded outside of static imaging, noting the importance in evaluating the first 30° of flexion for determining instability. CT soon became preferred to radiography, as it provided more detail. Using CT, quantitative values for patellar tracking, patellar height, patellar tilt, and others were established.93,96 Certain measurements, such as those involving the trochlea, rely on the evaluation of articular cartilage, resulting in different values on MRI and CT scans.91,113 However, controversy remains regarding the preferential use of CT or MRI for several measurements, such as TT-TG distance. Schoettle et al94 demonstrated differences in CT and MRI measurements when the authors used soft tissue landmarks to determine TT-TG distance. Our study demonstrated that there was a statistically significant difference in the TT-TG measurements of patients with instability when made on MRI scans (13.61 mm) as compared with CT scans (15.89 mm). This is in accordance with Schoettle et al, who reported a TT-TG distance of 13.5 and 15.3 mm on MRI and CT scans, respectively.94
Two of the more common measures cited in the literature to evaluate patellar tracking are TT-TG and TT-PCL distance. Several sources consider TT-TG or TT-PCL distances >20 mm to be pathologic.31,33,98 The present study did not aim to identify a pathologic threshold but determined a pooled mean TT-TG measurement on MRI scans of 13.61 mm for patients with instability, as compared with 10.24 mm for controls. Given that many surgeons use a 20-mm threshold for TT-TG distance in their decision to perform a tibial tubercle osteotomy,71 our findings highlight the need to consider multiple patient and anatomic characteristics in surgical planning.
In determining if preference should be given to using CT or MRI in the workup of a patient with patellar instability, our findings are inconclusive. In general, MRI scans have the benefit of demonstrating soft tissue anatomy, including any contribution of the articular cartilage to the stability of the patellofemoral joint, while CT scans show greater bony detail. Notably, the CT values for TT-TG distance in the present study were roughly 2 mm greater than those of the MRI values for the instability and control groups, which the surgeon needs to consider when determining if a patient is a candidate for tibial tubercle osteotomy. CT measurements for TT-TG distance did have a greater portion of inter- and intrarater ICCs deemed excellent when compared with MRI measurements. Given this, CT may be most useful in cases of abnormal bony anatomy and should be considered if TT-TG distance is difficult to determine on MRI scans.
Use of the TT-PCL measurement on MRI scans has also gained popularity in the assessment of patellar instability and the need to perform tibial tubercle osteotomy.14,31,98 Proponents of using the TT-PCL measurement have argued its favorability over the TT-TG measurement, as it eliminates the confounding variable of knee flexion with both points of measurement on the tibia.15 However, the current study did not detect a statistically significant difference for TT-PCL distance between instability and control groups. Additionally, the pooled average TT-PCL measurement for the control group was just shy of the 20-mm pathologic cutoff that surgeons often cite to indicate a patient for tubercle transfer.33 Additionally, current literature has cited that a femoral sulcus angle >150° indicates pathology.38 The findings of the present study align with this convention, as the mean femoral sulcus angle in the instability group was 158.46°—significantly greater than that of the control group measurement of 142.09°.
Patellar height is another common measure in the evaluation of patellar instability. The most ubiquitous metrics cited in the literature include the Insall-Salvati ratio, Caton-Deschamps index, and Blackburne-Peel ratio. Values >1.2 are considered pathologic for all 3 of these metrics measured on radiographs.33,59 The current study suggests that the Insall-Salvati ratio and the Caton-Deschamps index are cited at equal rates in the literature. The Blackburne-Peel ratio and patellar trochlear index are somewhat distant thirds. The pooled data showing a significantly different Insall-Salvati ratio of 1.31 in patients with instability as compared with 1.14 in controls is consistent with the previously defined cutoff of 1.2 used to determine presence of pathology. This solidifies the Insall-Salvati ratio as a good predictive measure for patellar instability. In contrast, the Caton-Deschamps index failed to show a statistical difference between the instability and control groups and had a pooled instability group value <1.2 (1.16). Pooled values could not be determined for the Blackburne-Peel ratio. These data suggest that the Insall-Salvati ratio may be more valuable in predicting instability; however, the Caton-Deschamps index maintains utility in its ability to assess postoperative changes after tibial tubercle distal advancement procedures.
Several studies have performed dedicated analyses on the reliability of the various measurements for patellar instability. One review of MRI, CT, and radiographic measurements in trochlear dysplasia deemed only 6 of 33 measurements reliable enough for recommendation.86 The recommended measurements included lateral trochlear inclination, the crossing sign, the trochlear bump, TT-TG distance, the trochlear depth, and the ventral trochlear prominence.86 Smith et al102 evaluated 10 radiographic measurements of patellar height, patellar tracking, and trochlear morphology and found that the reliability of these radiologic measurements was “cautiously low.”102 Our systematic review produced enough imaging reliability results to allow for the analysis of 7 measurements. Patellar height measurements for reliability analysis included the Insall-Salvati ratio, Caton-Deschamps index, and Blackburne-Peel ratio. Of these, the Insall-Salvati ratio demonstrated superior interobserver reliability, with 100% of ICCs >0.75. Intraobserver reliability for these 3 measures was less frequently reported but was lowest for the Caton-Deschamps index. Three patellar tracking measurements had ample reliability data for analysis: TT-TG, TT-PCL, and PT-TG distances. All intra- and interobserver ICCs for these measures were >0.75; interestingly however, the PT-TG measurement had the greatest percentage of intraobserver ICCs >0.9, and the TT-TG measurement was the only measure with <100% of intraobserver ICCs >0.9. Sulcus angle was the lone trochlear morphology measure with reliability data, and all ICCs for intra- and interobserver reliability were >0.75.
The most significant limitation in this study was the heterogeneity of the data. Specifically, studies had various purposes for performing imaging, including surgical planning, assessing predictability, and diagnostic purposes, among others. Additionally, the control and instability groups were not uniform across studies. Instability as defined by the various studies ranged from a primary dislocation to recurrent dislocations, and control groups were either healthy volunteers or individuals with knee pathology unrelated to patellar instability. The heterogeneity of the data also limited the ability to perform statistical analysis and specifically prevented any such comparison to be done for the reliability of measurements. The present study also employed an imperfect system for categorizing measurements, as several measurements were intended to span multiple categories. In particular, it was often difficult to differentiate patellar tracking versus trochlear morphology measurements because the 2 categories are closely interrelated. Furthermore, given the immense number of publications, the present search was necessarily limited to a 10-year period; thus, it may have missed unique measurements reported in earlier literature regarding patellar instability and may have missed the opportunity to perform additional statistical analysis. Finally, the risk-of-bias assessment demonstrated additional heterogeneity in the quality of studies in this analysis, but study quality beyond sample size did not factor into our weighting for statistical purposes.
Conclusion
The most commonly reported measurements in the literature for evaluating patellar instability are those that assess patellar tracking and trochlear morphology. The TT-TG measurement is the most ubiquitous and appears to be significantly greater in patients with patellar instability as compared with controls. According to this review, the TT-TG, TT-PCL, and PT-TG distances are reproducible measurements for patellar tracking, and the Insall-Salvati ratio has superior reproducibility for assessing patellar height. Finally, this systematic review highlights the need for greater consolidation of the most reliable radiologic measurements and their roles in the assessment of patellar instability.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-2-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-3-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine
∥References 2 –8, 10 –13, 16, 17, 19, 21 –23, 25 –32, 34 –37, 39 –58, 61, 62, 66 –70, 72 –75, 77 –85, 88 –91, 95, 97 –100, 102 –104, 106, 107, 109 –112, 114 –122.
∥∥References 3, 5, 7, 12, 13, 25, 30, 32, 47, 50, 53, 62, 69, 70, 78, 80 –82, 84, 89, 102, 109, 116, 119, 121, 122.
¶¶References 3, 4, 7, 12, 13, 17, 25, 28, 45, 54, 61, 62, 68 –70, 78, 89, 95, 99, 102, 109, 110, 116, 118, 119, 121.
Footnotes
Final revision submitted October 10, 2020; accepted November 19, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.T.O. and W.D.E. have received education payments from Liberty Surgical. K.B.F. has received education payments from Liberty Surgical, honoraria from Vericel, consulting fees from DePuy/Medical Device Business Services, and nonconsulting fees from Aastrom and Vericel. F.P.T. has received consulting fees from Medical Device Business Services and nonconsulting fees from Smith & Nephew and Medtronic. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967121993179.
References
- 1. Aarvold A, Pope A, Sakthivel VK, Ayer RV. MRI performed on dedicated knee coils is inaccurate for the measurement of tibial tubercle trochlear groove distance. Skeletal Radiol. 2014;43(3):345–349. [DOI] [PubMed] [Google Scholar]
- 2. Arai Y, Nakagawa S, Higuchi T, et al. Comparative analysis of medial patellofemoral ligament length change pattern in patients with patellar dislocation using open-{MRI}. Knee Surg Sport Traumatol Arthrosc. 2017;25(8):2330–2336. [DOI] [PubMed] [Google Scholar]
- 3. Arendt EA, England K, Agel J, Tompkins MA. An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3099–3107. [DOI] [PubMed] [Google Scholar]
- 4. Balcarek P, Oberthür S, Frosch S, Schüttrumpf JP, Stürmer KM. Vastus medialis obliquus muscle morphology in primary and recurrent lateral patellar instability. Biomed Res Int. 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Balcarek P, Radebold T, Schulz X, Vogel D. Geometry of torsional malalignment syndrome: Trochlear dysplasia but not torsion predicts lateral patellar instability. Orthop J Sport Med. 2019;7(3):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Balcarek P, Terwey A, Jung K, et al. Influence of tibial slope asymmetry on femoral rotation in patients with lateral patellar instability. Knee Surg Sport Traumatol Arthrosc. 2013;21(9):2155–2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barnett AJ, Prentice M, Mandalia V, Wakeley CJ, Eldridge JDJ. Patellar height measurement in trochlear dysplasia. Knee Surg Sport Traumatol Arthrosc. 2009;17(12):1412–1415. [DOI] [PubMed] [Google Scholar]
- 8. Beckert MW, Albright JC, Zavala J, Chang J, Albright JP. Clinical accuracy of J-Sign measurement compared to magnetic resonance imaging. Iowa Orthop J. 2016;36:94–97. [PMC free article] [PubMed] [Google Scholar]
- 9. Berruto M, Ferrua P, Carimati G, Uboldi F, Gala L. Patellofemoral instability: classification and imaging. Joints. 2013;1(2):7–14. [PMC free article] [PubMed] [Google Scholar]
- 10. Biedert RM, Bachmann M. Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg Sport Traumatol Arthrosc. 2009;17(10):1225–1230. [DOI] [PubMed] [Google Scholar]
- 11. Biedert RM, Netzer P, Gal I, Sigg A, Tscholl PM. The lateral condyle index: A new index for assessing the length of the lateral articular trochlea as predisposing factor for patellar instability. Int Orthop. 2011;35(9):1327–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biyani R, Elias JJ, Saranathan A, et al. Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(10):2334–2341. [DOI] [PubMed] [Google Scholar]
- 13. Bonadio MB, Helito CP, do Prado Torres JA, et al. Plateau-patella angle: an option for the evaluation of patellar height in patients with patellar instability. Knee. 2017;24(2):340–344. [DOI] [PubMed] [Google Scholar]
- 14. Boutris N, Delgado DA, Labis JS, McCulloch PC, Lintner DM, Harris JD. Current evidence advocates use of a new pathologic tibial tubercle–posterior cruciate ligament distance threshold in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2733–2742. [DOI] [PubMed] [Google Scholar]
- 15. Brady JM, Rosencrans AS, Shubin Stein BE. Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med. 2018;11(2):261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brady JM, Sullivan JP, Nguyen J, et al. The tibial tubercle-to-trochlear groove distance is reliable in the setting of trochlear dysplasia, and superior to the tibial tubercle-to-posterior cruciate ligament distance when evaluating coronal malalignment. Arthroscopy. 2017;33(11):2026–2034. [DOI] [PubMed] [Google Scholar]
- 17. Burke CJ, Kaplan D, Block T, et al. Clinical utility of continuous radial magnetic resonance imaging acquisition at 3 T in real-time patellofemoral kinematic assessment: a feasibility study. Arthroscopy. 2018;34(3):726–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Camp CL, Heidenreich MJ, Dahm DL, Bond JR, Collins MS, Krych AJ. A simple method of measuring tibial tubercle to trochlear groove distance on MRI: description of a novel and reliable technique. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):879–884. [DOI] [PubMed] [Google Scholar]
- 19. Camp CL, Heidenreich MJ, Dahm DL, Stuart MJ, Levy BA, Krych AJ. Individualizing the tibial tubercle–trochlear groove distance: patellar instability ratios that predict recurrent instability. Am J Sports Med. 2016;44(2):393–399. [DOI] [PubMed] [Google Scholar]
- 20. Camp CL, Stuart MJ, Krych AJ, et al. CT and MRI measurements of tibial tubercle–trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835–1840. [DOI] [PubMed] [Google Scholar]
- 21. Campos T, Soogumbur A, McNamara IR, Donell ST. The trochlear isometric point is different in patients with recurrent patellar instability compared to controls: a radiographical study. Knee Surg Sport Traumatol Arthrosc. 2018;26(9):2797–2803. doi:10.1007/s00167-017-4740-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cao P, Niu Y, Liu C, et al. Ratio of the tibial tuberosity–trochlear groove distance to the tibial maximal mediolateral axis: a more reliable and standardized way to measure the tibial tuberosity–trochlear groove distance. Knee. 2018;25(1):59–65. [DOI] [PubMed] [Google Scholar]
- 23. Caplan N, Lees D, Newby M, et al. Is tibial tuberosity–trochlear groove distance an appropriate measure for the identification of knees with patellar instability? Knee Surgery, Sport Traumatol Arthrosc. 2014;22(10):2377–2381. doi:10.1007/s00167-014-2954-0 [DOI] [PubMed] [Google Scholar]
- 24. Carlson V, Sheehan F, Shen A, Yao L, Jackson J, Boden B. The relationship of static tibial tubercle–trochlear groove measurement and dynamic patellar tracking. Am J Sports Med. 2017;45(8):1856–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Charles MD, Haloman S, Chen L, Ward SR, Fithian D, Afra R. Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am J Sports Med. 2013;41(2):374–384. [DOI] [PubMed] [Google Scholar]
- 26. Chassaing V, Zeitoun J-M, Camara M, Blin J-L, Marque S, Chancelier M-D. Tibial tubercle torsion, a new factor of patellar instability. Orthop Traumatol Surg Res. 2017;103(8):1173–1178. [DOI] [PubMed] [Google Scholar]
- 27. Chen S, Zhou Y, Qian Q, Wu Y, Fu P, Wu H. Arthroscopic lateral retinacular release, medial retinacular plication and partial medial tibial tubercle transfer for recurrent patellar dislocation. Int J Surg. 2017;44:43–48. [DOI] [PubMed] [Google Scholar]
- 28. Clark D, Stevens JM, Tortonese D, Whitehouse MR, Simpson D, Eldridge J. Mapping the contact area of the patellofemoral joint: the relationship between stability and joint congruence. Bone Jt J. 2019;101–B(5):552–558. [DOI] [PubMed] [Google Scholar]
- 29. Cooney AD, Kazi Z, Caplan N, Newby M, St Clair Gibson A, Kader DF. The relationship between quadriceps angle and tibial tuberosity-trochlear groove distance in patients with patellar instability. Knee Surgery, Sport Traumatol Arthrosc. 2012;20(12):2399–2404. [DOI] [PubMed] [Google Scholar]
- 30. Crebs DT, Anthony CA, McCunniff PT, Nieto MJ, Beckert MW, Albright JP. Effectiveness of fulkerson osteotomy with femoral nerve stimulation for patients with severe femoral trochlear dysplasia. Iowa Orthop J. 2015;35:34–41. [PMC free article] [PubMed] [Google Scholar]
- 31. Daynes J, Hinckel BB, Farr J. Tibial tuberosity–posterior cruciate ligament distance. J Knee Surg. 2016;29(6):471–477. [DOI] [PubMed] [Google Scholar]
- 32. Dejour D, Ferrua P, Ntagiopoulos PG, et al. The introduction of a new MRI index to evaluate sagittal patellofemoral engagement. Orthop Traumatol Surg Res. 2013;99(8):S391–S398. [DOI] [PubMed] [Google Scholar]
- 33. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 34. Demehri S, Thawait GK, Williams AA, et al. Imaging characteristics of contralateral asymptomatic patellofemoral joints in patients with unilateral instability. Radiology. 2014;273(3):821–830. [DOI] [PubMed] [Google Scholar]
- 35. De Oliveira V, de Souza V, Cury R, et al. Medial patellofemoral ligament anatomy: is it a predisposing factor for lateral patellar dislocation? Int Orthop. 2014;38(8):1633–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Deveci A, Cankaya D, Yilmaz S, Celen E, Sakman B, Bozkurt M. Are metric parameters sufficient alone in evaluation of the patellar instability? New angular measuring parameters: The trochlear groove-patellar tendon angle and the trochlear groove-dome angle. J Orthop Surg. 2017;25(1):1–6. [DOI] [PubMed] [Google Scholar]
- 37. Dickschas J, Harrer J, Bayer T, Schwitulla J, Strecker W. Correlation of the tibial tuberosity-trochlear groove distance with the {Q}-angle. Knee Surg Sport Traumatol Arthrosc. 2016;24(3):915–920. [DOI] [PubMed] [Google Scholar]
- 38. Diederichs G, Issever A, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics. 2010;30(4):961–981. [DOI] [PubMed] [Google Scholar]
- 39. Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med. 2013;41(1):51–57. [DOI] [PubMed] [Google Scholar]
- 40. Dong Z, Niu Y, Duan G, Song Y, Qi J, Wang F. Evaluation of trochlear dysplasia severity using trochlear angle: A retrospective study based on computed tomography (CT) scans. Med Sci Monit. 2018;24:5118–5122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dornacher D, Reichel H, Lippacher S. Measurement of tibial tuberosity-trochlear groove distance: Evaluation of inter- and intraobserver correlation dependent on the severity of trochlear dysplasia. Knee Surg Sport Traumatol Arthrosc. 2014;22(10):2382–2387. [DOI] [PubMed] [Google Scholar]
- 42. Dragoo JL, Nguyen M, Gatewood CT, Taunton JD, Young S. Medial patellofemoral ligament repair versus reconstruction for recurrent patellar instability: Two-year results of an algorithm-based approach. Orthop J Sport Med. 2017;5(3):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Du H, xiao Tian X, qi Guo F, et al. Evaluation of different surgical methods in treating recurrent patella dislocation after three-dimensional reconstruction. Int Orthop. 2017;41(12):2517–2524. [DOI] [PubMed] [Google Scholar]
- 44. Edwards A, Larson E, Beckert M, Sahai N, Albright JP. TT-TG vs modified lateral patellar edge for determination of tibial tubercle transfer distance in Fulkerson osteotomy procedures. Knee. 2016;23(4):712–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Falkowski AL, Camathias C, Jacobson JA, Magerkurth O. Increased magnetic resonance imaging signal of the lateral patellar facet cartilage: A functional marker for patellar instability? Am J Sports Med. 2017;45(10):2276–2283. [DOI] [PubMed] [Google Scholar]
- 46. Ferlic PW, Runer A, Dammerer D, Wansch J, Hackl W, Liebensteiner MC. Patella height correlates with trochlear dysplasia: A computed tomography image analysis. Arthrosc - J Arthrosc Relat Surg. 2018;34(6):1921–1928. [DOI] [PubMed] [Google Scholar]
- 47. Franciozi CE, Ambra LF, Albertoni LJB, et al. Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthrosc - J Arthrosc Relat Surg. 2017;33(3):633–640. [DOI] [PubMed] [Google Scholar]
- 48. Gillespie D, Mandziak D, Howie C. Influence of posterior lateral femoral condyle geometry on patellar dislocation. Arch Orthop Trauma Surg. 2015;135(11):1503–1509. [DOI] [PubMed] [Google Scholar]
- 49. Graf KH, Tompkins MA, Agel J, Arendt EA. Q-vector measurements: physical examination versus magnetic resonance imaging measurements and their relationship with tibial tubercle-trochlear groove distance. Knee Surg Sport Traumatol Arthrosc. 2018;26(3):697–704. [DOI] [PubMed] [Google Scholar]
- 50. Guilbert S, Chassaing V, Radier C, et al. Axial MRI index of patellar engagement: A new method to assess patellar instability. Orthop Traumatol Surg Res. 2013;99(8 S):S399–S405. [DOI] [PubMed] [Google Scholar]
- 51. Heidenreich MJ, Camp CL, Dahm DL, Stuart MJ, Levy BA, Krych AJ. The contribution of the tibial tubercle to patellar instability: analysis of tibial tubercle–trochlear groove (TT-TG) and tibial tubercle–posterior cruciate ligament (TT-PCL) distances. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(8):2347–2351. [DOI] [PubMed] [Google Scholar]
- 52. Heidenreich MJ, Sanders TL, Hevesi M, et al. Individualizing the tibial tubercle to trochlear groove distance to patient specific anatomy improves sensitivity for recurrent instability. Knee Surg Sport Traumatol Arthrosc. 2018;26(9):2858–2864. [DOI] [PubMed] [Google Scholar]
- 53. Hevesi M, Heidenreich MJ, Camp CL, et al. The recurrent instability of the patella score: A statistically based model for prediction of long-term recurrence risk after first-time dislocation. Arthrosc - J Arthrosc Relat Surg. 2019;35(2):537–543. [DOI] [PubMed] [Google Scholar]
- 54. Higuchi T, Arai Y, Takamiya H, Miyamoto T, Tokunaga D, Kubo T. An analysis of the medial patellofemoral ligament length change pattern using open-{MRI}. Knee Surg Sport Traumatol Arthrosc. 2010;18(11):1470–1475. [DOI] [PubMed] [Google Scholar]
- 55. Hinckel BB, Gobbi RG, Filho ENK, et al. Are the osseous and tendinous-cartilaginous tibial tuberosity–trochlear groove distances the same on CT and MRI? Skeletal Radiol. 2015;44(8):1085–1093. [DOI] [PubMed] [Google Scholar]
- 56. Hinckel BB, Gobbi RG, Kihara Filho EN, et al. Why are bone and soft tissue measurements of the TT-TG distance on MRI different in patients with patellar instability? Knee Surg Sport Traumatol Arthrosc. 2017;25(10):3053–3060. [DOI] [PubMed] [Google Scholar]
- 57. Hinckel BB, Gobbi RG, Kihara Filho EN, Demange MK, Pécora JR, Camanho GL. Patellar tendon–trochlear groove angle measurement: a new method for patellofemoral rotational analyses. Orthop J Sports Med. 2015;3(9):2325967115601031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hingelbaum S, Best R, Huth J, Wagner D, Bauer G, Mauch F. The TT-TG index: a new knee size adjusted measure method to determine the TT-TG distance. Knee Surg Sport Traumatol Arthrosc. 2014;22(10):2388–2395. [DOI] [PubMed] [Google Scholar]
- 59. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. [DOI] [PubMed] [Google Scholar]
- 60. Joanna Briggs Institute. Checklist for case series: critical appraisal tools for use in JBI systematic reviews. Published 2020. https://joannabriggs.org/sites/default/files/2020-08/Checklist_for_Case_Series.pdf
- 61. Kang H, Cao J, Yu D, Zheng Z, Wang F. Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: A prospective randomized study. Am J Sports Med. 2013;41(5):1013–1021. [DOI] [PubMed] [Google Scholar]
- 62. Köhlitz T, Scheffler S, Jung T, et al. Prevalence and patterns of anatomical risk factors in patients after patellar dislocation: a case control study using {MRI}. Eur Radiol. 2013;23(4):1067–1074. [DOI] [PubMed] [Google Scholar]
- 63. Koo T, Li M. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kujala UM, Kormano M, Osterman K, et al. Magnetic resonance imaging analysis of patellofemoral congruity in females. Clin J Sport Med. 1992;2(1):21–26. [Google Scholar]
- 65. Kujala UM, Osterman K, Kormano M, Komu M, Schlenzka D. Patellar motion analyzed by magnetic resonance imaging. Acta Orthop Scand. 1989;60(1):13–16. [DOI] [PubMed] [Google Scholar]
- 66. Kulkarni S, Shetty AP, Alva KK, Talekar S, Shetty VD. Patellar instability in {Indian} population: relevance of tibial tuberosity and trochlear groove distance. SICOT J. 2016;2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kuroda R, Nagai K, Matsushita T, et al. A new quantitative radiographic measurement of patella for patellar instability using the lateral plain radiograph: ‘patellar width ratio’. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(1):123–128. [DOI] [PubMed] [Google Scholar]
- 68. Li J, Sheng B, Yu F, et al. Quantitative magnetic resonance imaging in patellar tendon-lateral femoral condyle friction syndrome: relationship with subtle patellofemoral instability. Skeletal Radiol. 2019;48(8):1251–1259. [DOI] [PubMed] [Google Scholar]
- 69. Lim WY, Lim M-H. Comparative study of magnetic resonance imaging (MRI) parameters in a Southeast Asian population with symptomatic patellofemoral instability. Knee. 2016;23(4):588–592. [DOI] [PubMed] [Google Scholar]
- 70. Liu C, Duan G, Niu Y, et al. Lateral retinaculum plasty instead of lateral retinacular release with concomitant medial patellofemoral ligament reconstruction can achieve better results for patellar dislocation. Knee Surgery, Sport Traumatol Arthrosc. 2018;26(10):2899–2905. [DOI] [PubMed] [Google Scholar]
- 71. Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar instability management: a survey of the International Patellofemoral Study Group. Am J Sports Med. 2018;46(13):3299-3306. [DOI] [PubMed] [Google Scholar]
- 72. Liu JN, Brady JM, Kalbian IL, et al. Clinical outcomes after isolated medial patellofemoral ligament reconstruction for patellar instability among patients with trochlear dysplasia. Am J Sports Med. 2018;46(4):883–889. [DOI] [PubMed] [Google Scholar]
- 73. Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: A randomized controlled trial. Arthrosc - J Arthrosc Relat Surg. 2013;29(5):891–897. [DOI] [PubMed] [Google Scholar]
- 74. Marzo J, Kluczynski M, Notino A, Bisson L. Comparison of a novel weightbearing cone beam computed tomography scanner versus a conventional computed tomography scanner for measuring patellar instability. Orthop J Sport Med. 2016;4(12):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. McDermott SE, Anthony CA, McCunniff P, Duchman K, Albright JP. A clinical and radiographic approach for establishing proper tibial tubercle transfer when using quad active femoral nerve stimulation. Iowa Orthop J. 2013;33:84–89. [PMC free article] [PubMed] [Google Scholar]
- 76. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56(7):1391–1396. [PubMed] [Google Scholar]
- 77. Mohammadinejad P, Shekarchi B. Value of CT scan-assessed tibial tuberosity–trochlear groove distance in identification of patellar instability. Radiol Medica. 2016;121(9):729–734. [DOI] [PubMed] [Google Scholar]
- 78. Munch JL, Sullivan JP, Nguyen JT, et al. Patellar articular overlap on MRI is a simple alternative to conventional measurements of patellar height. Orthop J Sport Med. 2016;4(7):2325967116656328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nelitz M, Lippacher S, Reichel H, Dornacher D. Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sport Traumatol Arthrosc. 2014;22(1):120–127. [DOI] [PubMed] [Google Scholar]
- 80. Neri T, Parker DA, Putnis S, et al. Clinical and radiological predictors of functional outcome after isolated medial patellofemoral ligament reconstruction at midterm follow-up. Am J Sports Med. 2019;47(6):1338–1345. [DOI] [PubMed] [Google Scholar]
- 81. Netto ADS, de Brito MBS, Severino FR, et al. Study on the patellofemoral joint using magnetic resonance imaging: Morphological variation of the medial patellofemoral ligament. Rev Bras Ortop. 2012;47(2):204–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Nha KW, Ha Y, Oh S, et al. Surgical treatment with closing-wedge distal femoral osteotomy for recurrent patellar dislocation with genu valgum. Am J Sports Med. 2018;46(7):1632–1640. [DOI] [PubMed] [Google Scholar]
- 83. Niimoto T, Deie M, Adachi N, Usman MA, Ochi M. Quantitative stress radiography of the patella and evaluation of patellar laxity before and after lateral release for recurrent dislocation patella. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(10):2408–2413. [DOI] [PubMed] [Google Scholar]
- 84. Noehren B, Duncan S, Lattermann C. Radiographic parameters associated with lateral patella degeneration in young patients. Knee Surgery, Sport Traumatol Arthrosc. 2012;20(12):2385–2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Ortug A, Ormeci T, Yuzbasioglu N, Albay S, Seker M. Evaluation of normal tibial tubercle to trochlear groove distance in adult Turkish population. Niger J Clin Pract. 2018;21(11):1403–1407. [DOI] [PubMed] [Google Scholar]
- 86. Paiva M, Blønd L, Hölmich P, et al. Quality assessment of radiological measurements of trochlear dysplasia: a literature review. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):746–755. [DOI] [PubMed] [Google Scholar]
- 87. Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133(2):209-213. [DOI] [PubMed] [Google Scholar]
- 88. Pozzi G, Al-Mnayyis A, Almolla J, et al. Middle patellar tendon to posterior cruciate ligament (PT–PCL) and normalized PT–PCL: New magnetic resonance indices for tibial tubercle position in patients with patellar instability. Knee. 2018;25(5):799–806. [DOI] [PubMed] [Google Scholar]
- 89. Roessler PP, Wimmer MD, Jacobs C, Bornemann R, Stein T, Lahner M. Medial patellofemoral ligament reconstruction fails to correct mild patella alta in cases of patellofemoral instability—a case-control study. Int Orthop. 2019;43(9):2071–2075. [DOI] [PubMed] [Google Scholar]
- 90. Roger J, Lustig S, Cerciello S, Bruno CF, Neyret P, Servien E. Short lateral posterior condyle is associated with trochlea dysplasia and patellar dislocation. Knee Surgery, Sport Traumatol Arthrosc. 2019;27(3):731–739. [DOI] [PubMed] [Google Scholar]
- 91. Salzmann GM, Weber TS, Spang JT, Imhoff AB, Schöttle PB. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with trochlear dysplasia. Arch Orthop Trauma Surg. 2010;130(3):335–340. [DOI] [PubMed] [Google Scholar]
- 92. Sanders T, Pareek A, Hewett T, Stuart M, Dahm D, Krych A. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 2018;10(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Sasaki T, Yagi T. Subluxation of the patella: investigation by computerized tomography. Int Orthop. 1986;10(2):115–120. [PubMed] [Google Scholar]
- 94. Schoettle PB, Zanetti M, Seifert B, Pfirrmann CWA, Fucentese SF, Romero J. The tibial tuberosity–trochlear groove distance: a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. [DOI] [PubMed] [Google Scholar]
- 95. Schueda MA, Astur DC, Bier RS, Bier DS, Astur N, Cohen M. Use of computed tomography to determine the risk of patellar dislocation in 921 patients with patellar instability. Open Access J Sport Med. 2015;6:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Schutzer SF, Ramsby GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986;17(2):235–248. [PubMed] [Google Scholar]
- 97. Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. The position of the tibia tubercle in 0°–90° flexion: comparing patients with patella dislocation to healthy volunteers. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(10):2396–2400. [DOI] [PubMed] [Google Scholar]
- 98. Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle–posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40(5):1119–1125. [DOI] [PubMed] [Google Scholar]
- 99. Shimizu R, Sumen Y, Sakaridani K, Matsuura M, Adachi N. Middle-to long-term outcome after medial patellofemoral ligament reconstruction with Insall’s proximal realignment for patellar instability. Asia-Pacific J Sport Med Arthrosc Rehabil Technol. 2019;17:5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Skelley N, Friedman M, McGinnis M, Smith C, Hillen T, Matava M. Inter- and intraobserver reliability in the {MRI} measurement of the tibial tubercle-trochlear groove distance and trochlea dysplasia. Am J Sport Med. 2015;43(4):873–878. [DOI] [PubMed] [Google Scholar]
- 101. Smith BW, Millar EA, Jones KC, Elias JJ. Variations in tibial tuberosity to trochlear groove and posterior cruciate ligament distances due to tibial external and valgus rotations. J Knee Surg. 2018;31(6):557–561. [DOI] [PubMed] [Google Scholar]
- 102. Smith TO, Cogan A, Patel S, Shakokani M, Toms AP, Donell ST. The intra- and inter-rater reliability of x-ray radiological measurements for patellar instability. Knee. 2013;20(2):133–138. [DOI] [PubMed] [Google Scholar]
- 103. Swarup I, Elattar O, Rozbruch SR. Patellar instability treated with distal femoral osteotomy. Knee. 2017;24(3):608–614. [DOI] [PubMed] [Google Scholar]
- 104. Takagi S, Sato T, Watanabe S, et al. Alignment in the transverse plane, but not sagittal or coronal plane, affects the risk of recurrent patella dislocation. Knee Surg Sport Traumatol Arthrosc. 2018;26(10):2891–2898. [DOI] [PubMed] [Google Scholar]
- 105. Tan SHS, Ibrahim MM, Lee ZJ, Chee YKM, Hui JH. Patellar tracking should be taken into account when measuring radiographic parameters for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3593–3600. [DOI] [PubMed] [Google Scholar]
- 106. Tanaka MJ, Elias JJ, Williams AA, Carrino JA, Cosgarea AJ. Correlation between changes in tibial tuberosity-trochlear groove distance and patellar position during active knee extension on dynamic kinematic computed tomographic imaging. Arthrosc - J Arthrosc Relat Surg. 2015;31(9):1748–1755. [DOI] [PubMed] [Google Scholar]
- 107. Tensho K, Shimodaira H, Akaoka Y, et al. Lateralization of the tibial tubercle in recurrent patellar dislocation. J Bone Jt Surg. 2018;100(9):e58. [DOI] [PubMed] [Google Scholar]
- 108. Thakkar RS, Del Grande F, Wadhwa V, et al. Patellar instability: CT and MRI measurements and their correlation with internal derangement findings. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):3021–3028. [DOI] [PubMed] [Google Scholar]
- 109. Tscholl PM, Wanivenhaus F, Fucentese SF. Conventional radiographs and magnetic resonance imaging for the analysis of trochlear dysplasia: The influence of selected levels on magnetic resonance imaging. Am J Sport Med. 2017;45(5):1059–1065. [DOI] [PubMed] [Google Scholar]
- 110. Tsuda E, Ishibashi Y, Yamamoto Y, Maeda S. Incidence and radiologic predictor of postoperative patellar instability after {Fulkerson} procedure of the tibial tuberosity for recurrent patellar dislocation. Knee Surg Sport Traumatol Arthrosc. 2012;20(10):2062–2070. [DOI] [PubMed] [Google Scholar]
- 111. Urch SE, Tritle BA, Shelbourne KD, Gray T. Axial linear patellar displacement: a new measurement of patellofemoral congruence. Am J Sport Med. 2009;37(5):970–973. [DOI] [PubMed] [Google Scholar]
- 112. Urgery S, Ncorporated I, Tensho K, Akaoka Y, Shimodaira H, Takanashi S. What components comprise the measurement of the tibial tuberosity-trochlear groove distance. Published online. 2015:1441–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. van Huyssteen AL, Hendrix MRG, Barnett AJ, Wakeley CJ, Eldridge JDJ. Cartilage-bone mismatch in the dysplastic trochlea. J Bone Joint Surg Br. 2006;88-B(5):688–691. [DOI] [PubMed] [Google Scholar]
- 114. Voss A, Shin SR, Murakami AM, et al. Objective quantification of trochlear dysplasia: Assessment of the difference in morphology between control and chronic patellofemoral instability patients. Knee. 2017;24(5):1247–1255. [DOI] [PubMed] [Google Scholar]
- 115. Wind RJP, Heesterbeek PJC, Wymenga AB. A combined procedure with Bereiter-type trochleoplasty leads to a stable patellofemoral joint at 5-year follow-up. Knee Surgery, Sport Traumatol Arthrosc. 2019;27(3):716–723. [DOI] [PubMed] [Google Scholar]
- 116. Woodmass JM, Johnson NR, Cates RA, Krych AJ, Stuart MJ, Dahm DL. Medial patellofemoral ligament reconstruction reduces radiographic measures of patella alta in adults. Orthop J Sport Med. 2018;6(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Xue Z, Song G-Y, Liu X, et al. Excessive lateral patellar translation on axial computed tomography indicates positive patellar {J} sign. Knee Surg Sport Traumatol Arthrosc. 2018;26(12):3620–3625. [DOI] [PubMed] [Google Scholar]
- 118. Yamada Y, Toritsuka Y, Nakamura N, et al. Correlation of 3D shift and 3D tilt of the patella in patients with recurrent dislocation of the patella and healthy volunteers: An in vivo analysis based on 3-dimensional computer models. Am J Sport Med. 2017;45(13):3111–3118. [DOI] [PubMed] [Google Scholar]
- 119. Yang Y, Zhang Q. Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surgery, Sport Traumatol Arthrosc. 2019;27(8):2599–2607. [DOI] [PubMed] [Google Scholar]
- 120. Yi M, Hong SH, Choi J-Y, et al. Femoral trochlear groove morphometry assessed on oblique coronal MR images. AJR Am J Roentgenol. 2015;205(6):1260–1268. [DOI] [PubMed] [Google Scholar]
- 121. Yue RA, Arendt EA, Tompkins MA. Patellar height measurements on radiograph and magnetic resonance imaging in patellar instability and control patients. J Knee Surg. 2017;30(9):943–950. [DOI] [PubMed] [Google Scholar]
- 122. Zheng X, Hu Y, Xie P, et al. Surgical medial patellofemoral ligament reconstruction versus non-surgical treatment of acute primary patellar dislocation: a prospective controlled trial. Int Orthop. 2019;43(6):1495–1501. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-2-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-3-ojs-10.1177_2325967121993179 for Radiologic Measurements in the Assessment of Patellar Instability: A Systematic Review and Meta-analysis by Alex E. White, Peters T. Otlans, Dylan P. Horan, Daniel B. Calem, William D. Emper, Kevin B. Freedman and Fotios P. Tjoumakaris in Orthopaedic Journal of Sports Medicine