Epidemiology: Even though head-lice infestation is common, affecting about 10% of primary grade school children and their families each year, few people talk about it.1 The condition has been stigmatized by the false belief that lice are attracted to dirty scalps and unkempt hair. In fact, the lowly louse with the lofty name — Pediculus humanus capitus — does not discriminate on the basis of hygiene. The only essentials for this wingless parasite are hair to cling to and scalp blood to feed on.
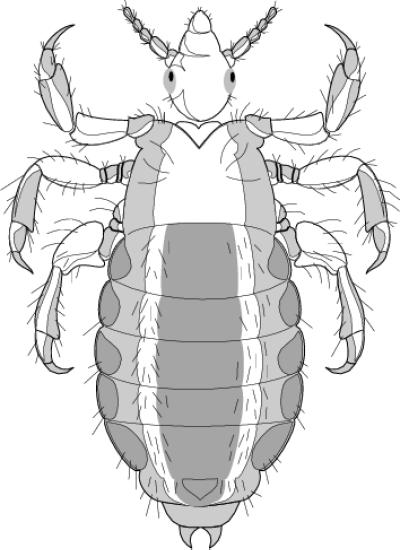
The adult louse is the size of a sesame seed, has 6 legs and assumes the shade of the hair it infests. The female lays yellow, shiny, oval eggs (nits) that cement firmly to the hair shaft near the scalp. Within a week the nits hatch into nymphs, which mature into adults about 7 days after hatching. Adults can live up to 30 days on a person's head.2
Transmission typically occurs between people who know each other well, and outbreaks are common when children return to school after summer holidays; it takes about 30 seconds for lice to move from one infested head to another, which means that prolonged head-to-head contact is usually required before they spread.3 Children aged 3 to 10 years and their families are infested most often, girls more so than boys. Infestations can also be started by wearing infested clothing, such as hats and scarves, by using infested combs or towels, or by lying on beds or pillows used by an infested person; however, lice found in the latter locations are mostly sick, elderly or dead and carry little capability of infecting a person.3 If a louse falls off a person, it dies within 1–2 days.
Clinical management: The main presenting complaint is a mildly itchy scalp, caused by an allergic reaction to lice saliva. This varies from no reaction to delayed and immediate reaction to tolerance. Occasionally, secondary bacterial dermal infections result from scratching.
Crawling head lice may be detected by close inspection of the hair or by the fine-tooth combing of wet hair. Nits are often seen in the hair behind the ears and at the nape of the neck. The mere presence of nits alone does not indicate infestation; the US Centers for Disease Control and Prevention recommend that only cases in which nits are located within 0.6 cm of the scalp, which means they are likely viable, should be treated as an infestation.2 A microscopic examination of specimens identified as lice or nits by health care professionals and lay personnel revealed that both groups tend to overdiagnose and mismanage infestations by failing to distinguish extinct from active infestations.4
Several products (pediculicides) are available to treat head lice, including lindane, pyrethrine and permethrin-based products. A recent Cochrane review of evidence on head-lice treatments5 identified only 3 trials of suitable quality. The review found no evidence that any product has greater curative effect than another, but it did find evidence that localized resistance to particular agents is starting to emerge. No major adverse effects were reported in the 43 trials that sought data on product safety; minor adverse effects (stinging, erythema, rash, slight edema) were reported in 4%–6% of users of each agent. The review identified no randomized controlled trials on the effectiveness of herbal treatments for head lice and only 1 trial that compared wet-combing to a pediculicide, which showed combing to be ineffective as a curative treatment.6 Details on alternative treatments are available in recent reviews.7
Time spent ridding an individual of lice is wasted unless close contacts, including adults, are also traced and treated if infested. All machine-washable clothing and bed linens that the infested person touched during the 2 days before treatment should be washed in hot water. Materials that cannot be washed (e.g., stuffed animals) should be sealed in a plastic bag for 2 weeks. Combs and brushes should be soaked in alcohol or Lysol for an hour, and carpets and furniture must be vacuumed. Fumigant sprays are not indicated.2
Prevention: Infestation can be prevented by avoiding head-to-head contact among children. Regular examination of the child's head using a louse comb is the best way to detect early infestation. Every Oct. 31, the United Kingdom marks a national “bug-busting day” to remind families to check for lice.
There are no regulations concerning school attendance if a child is infested. This is controversial: some parents demand the exclusion of children with dead nits after treatment, and some public health units have opted to appease these demands by adopting a “no-nits” policy.
Thanks to Dr. Erika Abraham, infection control consultant, Ontario Ministry of Health and Long-Term Care.
Signature
Erica Weir
CMAJ
Figure.
References
- 1.Scowan P. Head lice: a problem for 1 in 10 primary school children. Prof Care Mother Child 1996;6:139-40. [PubMed]
- 2.Division of Parasitic Diseases, US Centers for Disease Control and Prevention. Fact sheet: treating head lice. Available: www.cdc.gov/ncidod/dpd/parasites/headlice/factsht_head_lice_treating.htm (accessed 2001 Aug 20).
- 3.Burgess IF. Shampoos for head lice treatment – comparative in vitro tests. Pharm J 1996;257: 188-90.
- 4.Pollack RJ, Kiszewski A, Spielman A. Overdiagnosis and consequent mismanagement of head louse infestations in North America. Pediatr Infect Dis J 2000;19:689-93. [DOI] [PubMed]
- 5.Dodds CS. Interventions for treating head lice [Cochrane review]. In: The Cochrane Library; Issue 2, 2001. Oxford: Update Software. [DOI] [PubMed]
- 6.Roberts R, Caseu D, Morgan D, Petrovic M. Comparison of wet combing with malathion for treatment of head lice in the UK: a pragmatic randomised controlled trial. Lancet 2000;356:540-4. [DOI] [PubMed]
- 7.Pray WS. Head lice: perfectly adapted human predators. Am J Pharm Educ 1999;63:204-9.


