Abstract
Background
High uptake of Covid-19 vaccination is required to reach herd immunity.
Methods
A representative sample of 2,060 Belgians were surveyed in October 2020. Regression analyses identified the predictors associated with willingness to get vaccinated against Covid-19, and attitudes toward vaccination in general.
Results
34% of the participants reported that they will definitely get vaccinated against Covid-19 and 39% that they would “probably”. Intended uptake was strongly associated with age, opinion on the government’s dealing with the Covid-19 pandemic, medical risk, spoken language, gender, and to a lesser extent with having known someone who was hospitalised because of Covid-19. Similar predictors were identified for attitudes to vaccination in general. Covid-19 vaccine hesitancy was more marked in age groups below 54 years old. We further analysed a sample of 17% (N = 349) found favourable to vaccination in general but not willing to be vaccinated against Covid-19. They were mainly female, young, French speaking, slightly less educated, working, and did not belong to a Covid-19 risk group. They were very dissatisfied with the government’s dealing with the pandemic, and did not know someone who was hospitalised because of Covid-19.
Conclusions
Vaccine hesitancy was higher for Covid-19 vaccines than for other vaccines. The part of the population being convinced of the utility of vaccination in general but hesitant about the Covid-19 vaccine is a primary interest group for tailored communication campaigns in order to reach the vaccine coverage needed for herd immunity.
Keywords: Belgium, Covid-19, Hesitancy, Immunisation, Vaccination
1. Introduction
After months of a global public health crisis that has paralysed our societies, safe and effective vaccines that protect against Covid-19 are becoming available [1], [2]. The next crucial challenge will be to deploy these vaccines with sufficiently high vaccination coverage rates in the population so that thresholds required for herd immunity can be reached. For vaccine efficacies of approximately 80%, it has been estimated that herd immunity requires that minimally 60% but possibly up to 90% of the population become vaccinated [3], [4]. Herd immunity will not just be a bonus that comes on top of individual vaccine protection; it will be an essential layer of Covid-19 prevention on which many people will depend as it remains to be seen whether Covid-19 vaccines will be equally effective in all individuals and whether some population subgroups won’t be able to receive vaccination for medical reasons.
To rapidly achieve herd immunity, mass vaccination will be required. However, apart from the logistic challenge of reaching sufficient numbers of individuals, there is an even bigger challenge in convincing vaccine hesitant individuals to become vaccinated [5]. Vaccination has always been controversial and throughout history a part of the population has always resisted it [6]. Over the past years, researchers have observed substantial and increasing levels of vaccine hesitancy in the population, often linked to the fact that infectious diseases and their consequences are fading from public memory but also in part through misinformation propagated on the internet [7], [8]. The World Health Organization (WHO) labelled vaccine hesitancy one of the top ten threats to global health in 2019, next to e.g. antimicrobial resistance or air pollution and climate change [9]. In the context of the Covid-19 vaccine, policy makers dealing with vaccine hesitancy and scepticism will be a critical success factor. Therefore, it is important that policy makers have a good view on the people profiles who are likely to refuse or delay vaccination. This will enable them to target communication campaigns and to devise vaccination strategies that take into account the clustering of susceptibility in profiles that are likely to refuse. Several population surveys have identified predictors associated with Covid-19 vaccine hesitancy. It is more likely to occur in individuals of younger age, women as well as people with lower income, lower education, lower perceived severity of Covid-19, lower Covid-19 exposure, lower trust in government, living in more disadvantaged areas or people adhering to more right-wing political views [10], [11], [12], [13], [14].
This paper aims to identify among a representative sample of the Belgian population the predictors associated with the willingness to become vaccinated against Covid-19 and investigate whether these coincide with predictors of attitudes toward vaccination in general.
2. Methods
2.1. Survey
We used a nationally representative panel of the market research agency Dynata to complete a survey between 6 and 16 October 2020‡ . A sample of 2,698 respondents drawn from a panel of 5,500 selected members who mirror the Belgian population (aged 18–80 years) as well as possible§ , were invited to participate in the survey. Of these, 494 did not complete the survey and 144 were excluded because they did not meet the company’s internal quality controls (e.g., they completed the survey unreasonably fast (below a third of the median time to completion)). This left us with a sample of 2,060 responses, which fulfilled pre-determined Belgium quota for age, gender and province (Appendix A). The main objective of the survey was to carry out an experiment to elicit individual preferences on who should get vaccinated first in the population; the results of the experiment are reported elsewhere [15]. In this paper we focus on two specific questions about attitudes toward vaccination. Before participants took the experiment, we asked them to answer the question “Would you say that vaccination for infectious disease is… very useful, rather useful, rather useless, very useless”. Then, at the end of the experiment, we asked the question “Once there is a safe and effective Covid-19 vaccine, will you get vaccinated?” and the four response items were “definitely”, “probably”, “probably not”, “definitely not”. The survey started by asking respondents for a range of sociodemographic characteristics along with their attitudes toward the government’s dealing with the corona crisis, whether they had had Covid-19, whether someone they knew had had it, was hospitalised because of it and had died because of it. Respondents were also asked whether their profession was among the “essential professions” (i.e., those that were obliged to keep working during the first “lockdown” in March/April 2020) and whether they considered themselves to be part of a risk group for Covid-19 and if so, which group they belonged to (old age, chronic illness, obesity, or other). Finally, respondents were asked about whom should decide who gets the Covid-19 vaccine first (government, scientists or the population) and whether they would choose to be vaccinated themselves once a vaccine becomes available.
2.2. Data analysis
We considered willingness to get Covid-19 vaccinated as a binary variable grouping the answers “definitely” against “probably”, “probably not” and “definitely not”. We determined the factors significantly associated to this response using a multivariate logistic regression model with as dependent variable whether an individual intends to become vaccinated or still doubts or refuses to become vaccinated. We estimated adjusted and unadjusted odds ratios of willingness to be Covid-19 vaccinated using all the variables that showed significance (p < 0.05) in a univariate analysis. We repeated the same analysis for attitudes toward infectious disease vaccination grouping “very useful” against “rather useful”, “rather useless” and “very useless”.
We then studied the sub-sample of people who exhibited a seemingly inconsistent opinion of being pro-vaccination in general but being unwilling to take the Covid-19 vaccine once available. We used basic descriptive statistics and frequencies to describe all variables, comparing the full sample of survey data with the smaller sample of inconsistent individuals. We used chi-square tests to indicate significant differences in proportions between the two samples. We performed all analyses using the JMP Pro 16 statistical software.
3. Results
A total of N = 2,060 surveys were completed and checked for quality based on respondents’ answers to several comment boxes. None were excluded. Overall, 34% (N = 651) indicated that they would “definitely” become vaccinated with a Covid-19 vaccine and 39% (N = 742) stated that they would “probably” become vaccinated with a Covid-19 vaccine, 18% (N = 346) said “probably not” and 9% (N = 165) said “definitely not”. The numbers of sceptical answers to Covid-19 vaccination were substantially higher than the sceptical answers to the usefulness of vaccination in general. Whereas 73% stated to be willing to become vaccinated with the Covid-19 vaccine, 90% stated to think that vaccination is useful to protect against infectious diseases. 49% (N = 1,002) stated that vaccination is “very useful” and 41% (N = 848) stated it to be “rather useful”. 7% (N = 153) said “rather useless” and 3% (N = 57) said “very useless”.
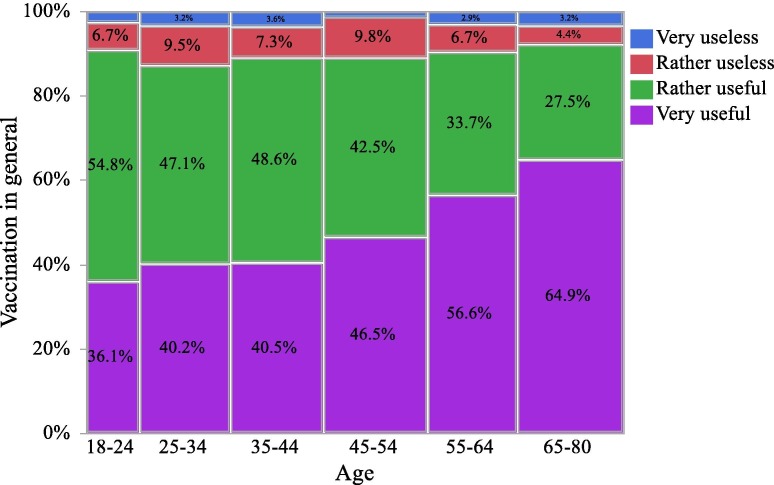
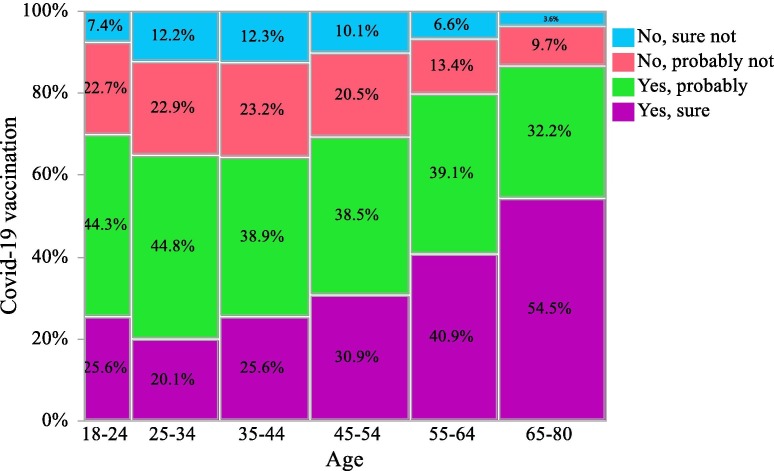
When carrying out univariate analyses, we found larger discrepancies in different age groups’ willingness to be Covid-19 vaccinated compared to their attitude toward vaccination in general. While at most 12.7% of the population across all age groups found vaccination rather or very useless (See Fig. 1 ), Covid-19 vaccine scepticism represented between 30% and 36% among people younger than 54 years old with the largest share of sceptics in the 25–34 and 35–44 age groups (See Fig. 2 ). While there were fewer Covid-19 vaccine sceptics in the older age groups (20% in 55–64 and 13.3% in people above 65), these shares were still larger than the shares of people reporting vaccination in general to be useless across any age groups.
Fig. 1.
Distribution of the attitudes toward the usefulness of infectious disease vaccination according to age groups.
Fig. 2.
Distribution of the willingness to be Covid-19 vaccinated according to age groups.
The multivariate logistic regression analyses (Table 1 ) revealed that factors predicting willingness to vaccinate against Covid-19 were being male (Odds Ratio (OR) = 1.53, (95% confidence interval 1.25–1.89), p < 0.0001), being Dutch-speaker (OR = 2.37 (1.89–2.95), p < 0.0001), knowing someone who was hospitalised for Covid-19 (OR = 1.78 (1.16–2.71), p = 0.0083), and belonging to a medically vulnerable group (OR = 1.71 (1.35–2.17), p < 0.0001). The willingness to get Covid-19 vaccinated also gradually increased with age groups from age 45 when compared to the younger age category of 18–24 (45–54 OR = 1.16 (0.75–1.77), 55–64 OR = 1.72 (1.11–2.66), 65 and above OR = 2.26 (1.45–3.53), p < 0.0001) and with satisfaction toward the government’s response to the health crisis (satisfied OR = 2.94 (1.61–5.37), rather satisfied OR = 1.55 (1.15–2.10), rather dissatisfied OR = 1.17 (0.87–1.58), p = 0.0003). When asked about who should decide about priority access to the Covid-19 vaccine, people willing to get vaccinated were more likely to reply government or scientists (respectively OR = 1.58 (1.00–2.51), OR = 2.14 (1.50–3.06), p < 0.0001) versus the population.
Table 1.
Unadjusted and adjusted odds ratios of willingness to get Covid-19 vaccinated and of having a non-hesitant attitude toward vaccination in general.
| Characteristic |
Covid-19 vaccine acceptance |
General vaccine acceptance |
||||
|---|---|---|---|---|---|---|
| Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) | P-value (adjusted) | Unadjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) | P-value (adjusted) | |
| Gender | ||||||
| Male | 1.55 (1.28–1.87) | 1.53 (1.25–1.89) | <0.0001 | 1.26 (1.06–1.50) | 1.32 (1.08–1.61) | 0.0058 |
| Language | ||||||
| Dutch | 2.33 (1.90–2.85) | 2.37 (1.89–2.95) | <0.0001 | 1.68 (1.41–2.00) | 1.54 (1.25–1.90) | <0.0001 |
| Age | ||||||
| 18–24 | 1.00 (reference) | 1.00 (reference) | <0.0001 | 1.00 (reference) | 1.00 (reference) | <0.0001 |
| 25–34 | 0.73 (0.47–1.13) | 0.69 (0.44–1.09) | 1.19 (0.83–1.70) | 1.28 (0.86–1.91) | ||
| 35–44 | 1.00 (0.66–1.52) | 0.95 (0.61–1.47) | 1.21 (0.85–1.72) | 1.29 (0.86–1.93) | ||
| 45–54 | 1.30 (0.87–1.95) | 1.16 (0.75–1.77) | 1.54 (1.09–2.18) | 1.59 (1.07–2.36) | ||
| 55–64 | 2.02 (1.35–3.03) | 1.72 (1.11–2.66) | 2.31 (1.62–3.30) | 2.31 (1.53–3.49) | ||
| 65–80 | 3.48 (2.35–5.16) | 2.26 (1.45–3.53) | 3.27 (2.31–4.64) | 2.45 (1.59–3.76) | ||
| Education | ||||||
| Basic | 1.00 (reference) | 1.00 (reference) | 0.1705 | 1.00 (reference) | 1.00 (reference) | 0.0002 |
| Third degree sec school | 1.18 (0.93–1.51) | 1.11 (0.84–1.45) | 1.31 (1.05–1.64) | 1.35 (1.04–1.75) | ||
| Higher | 1.09 (0.85–1.38) | 1.28 (0.98–1.68) | 1.52 (1.22–1.90) | 1.71 (1.32–2.22) | ||
| Have children | ||||||
| Yes | 1.22 (1.00–1.49) | NS | 1.30 (1.09–1.56) | NS | ||
| Profession | ||||||
| Working | 1.00 (reference) | NS | 1.00 (reference) | NS | ||
| Homemaker | 0.97 (0.58–1.62) | 1.05 (0.68–1.63) | ||||
| Student | 0.98 (0.66–1.46) | 0.76 (0.54–1.06) | ||||
| Unemployed | 1.02 (0.68–1.54) | 1.01 (0.70–1.44) | ||||
| Disabled | 1.87 (1.27–2.76) | 1.04 (0.72–1.50) | ||||
| Retired | 2.93 (2.33–3.69) | 2.06 (1.66–2.57) | ||||
| Profession is not 'essential' | ||||||
| Yes | 1.40 (1.09–1.81) | NS | 1.24 (1.00–1.55) | NS | ||
| Financial difficulties | ||||||
| Never | 1.41 (1.08–1.86) | NS | 1.84 (1.43–2.36) | 1.33 (1.00–1.79) | 0.1095 | |
| Once a year | 1.04 (0.77–1.42) | 1.27 (0.96–1.69) | 1.09 (0.79–1.50) | |||
| Once every three months | 0.89 (0.65–1.23) | 1.08 (0.81–1.44) | 1.01 (0.73–1.39) | |||
| Every month | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
| Satisfaction with government’s approach to Covid-19 pandemic | ||||||
| Very satisfied | 3.69 (2.12–6.43) | 2.94 (1.61–5.37) | 0.0003 | 5.28 (2.87–9.71) | 4.14 (2.13–8.04) | <0.0001 |
| Rather satisfied | 1.66 (1.26–2.19) | 1.55 (1.15–2.10) | 1.74 (1.36–2.23) | 1.53 (1.16–2.04) | ||
| Rather dissatisfied | 1.23 (0.94–1.63) | 1.17 (0.87–1.58) | 1.37 (1.07–1.75) | 1.24 (0.94–1.64) | ||
| Very dissatisfied | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||
| Has had a Covid-19 infection | ||||||
| Yes, confirmed with a test | 1.34 (0.70–2.54) | NS | 1.60 (0.90–2.86) | 1.07 (0.56–2.05) | 0.1145 | |
| Probably, but not confirmed | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
| with a test No |
1.43 (0.99–2.06) | 1.47 (1.07–2.02) | 1.45 (1.00–2.12) | |||
| Know personally someone who has had Covid-19 | ||||||
| Yes, confirmed with a test | 1.35 (0.90–2.04) | NS | 1.31 (0.91–1.88) | 1.13 (0.74–1.71) | 0.0036 | |
| Probably, but not confirmed with a test | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||
|
No |
1.28 (0.90–1.82) | 1.06 (0.78–1.44) | 0.71 (0.49–1.04) | |||
| Know personally someone who was hospitalised for Covid-19 | ||||||
| Yes | 1.60 (1.09–2.35) | 1.78 (1.16–2.71) | 0.0083 | 1.04 (0.73–1.49) | NS | |
| Know personally someone who died of Covid-19 | ||||||
| Yes | 1.31 (0.85–2.04) | NS | 1.21 (0.80–1.85) | NS | ||
| Belong to a medically vulnerable group | ||||||
| Yes | 2.61 (2.15–3.18) | 1.71 (1.35–2.17) | <0.0001 | 2.34 (1.95–2.81) | 1.83 (1.45–2.30) | <0.0001 |
| Determination vaccine prioritisation | ||||||
| Population | 1.00 (reference) | 1.00 (reference) | <0.0001 | 1.00 (reference) | 1.00 (reference) | <0.0001 |
| Government | 2.35 (1.53–3.60) | 1.58 (1.00–2.51) | 2.84 (1.90–4.23) | 1.94 (1.26–2.97) | ||
| Scientists | 2.30 (1.64–3.20) | 2.14 (1.50–3.06) | 2.84 (2.10–3.85) | 2.57 (1.86–3.55) | ||
| Covid-19 vaccine acceptance | ||||||
| Yes, sure | 16.44 (12.72–21.24) | |||||
| General vaccine acceptance | ||||||
| Very useful | 16.44 (12.72–21.24) | |||||
Note: NS stands for “highly non-significant” (p-value > 0.2).
The predicting factors of the willingness to get vaccinated against Covid-19 were mostly similar to the predicting factors of reporting that infectious disease vaccination is very useful as illustrated by the strong correlation with the very high odds ratio of being both willing to take the Covid-19 vaccine and finding infectious disease vaccination very useful (OR = 16.44 (12.72–21.24)). While socioeconomic characteristics were not identified as predictors of the willingness to vaccinate against Covid-19, educational attainment is significantly and increasingly associated with positive opinion about vaccination in general (compared to basic education, secondary school OR = 1.35 (1.04–1.75), higher education OR = 1.71 (1.32–2.22), p = 0.0002).
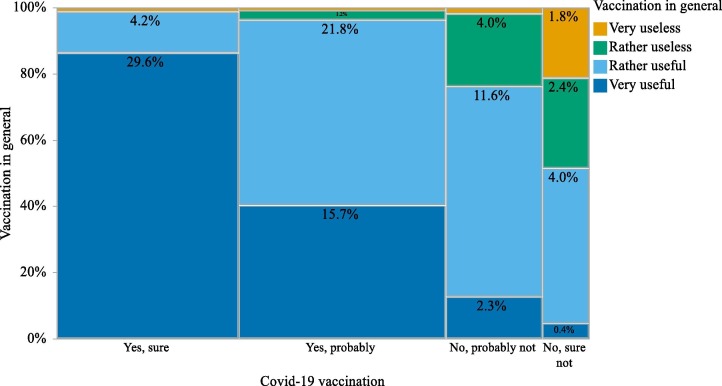
While most respondents finding vaccination very or rather useful were favourable to Covid-19 vaccination (71.3%), a sample of N = 349 individuals (18.3%) exhibited a remarkable opinion toward vaccination ( Fig. 3 ). They considered vaccination against infectious diseases very useful (15%, N = 52) or rather useful (85%, N = 297), but reported they would definitely not (24%, N = 85) or rather not (76%, N = 264) vaccinate against Covid-19. As these are likely to be the people in which communication campaigns about safety and effectiveness of Covid-19 vaccines are most effective, we investigated further who those people were (Table 2 ). Compared to the main sample, they were more likely to be women (p = 0.0067), younger than 54 years old (p < 0.0001), French speaking (p < 0.0001), with first or second degree secondary school (p = 0.0714), and working (p < 0.0001). They were also less likely to belong to a Covid-19 risk group (p < 0.0001), to have known someone who was hospitalised because of Covid-19 (p = 0.0314), and they were rather or very dissatisfied with the government’s dealing with the Covid-19 crisis (p < 0.0001). A sample of N = 36 individuals (1.9%) presented however negative attitudes toward vaccination in general but were willing to get vaccinated against Covid-19. They would get the Covid-19 vaccine for sure (0.4%, N = 8) or probably (1.5%, N = 28), but reported they find vaccination against infectious diseases very useless (0.7%, N = 13) or rather useless (1.2%, N = 23). Compared to the main sample, they were more likely to be men (p = 0.0046) who had not had a Covid-19 infection (p = 0.0546) or had not known someone with a Covid-19 infection (p = 0.0463), neither had they known someone who had been hospitalised (p = 0.0331) or had died (p = 0.0710) because of Covid-19.
Fig. 3.
Attitudes toward the usefulness of infectious disease vaccination and the willingness to be Covid-19 vaccinated.
Table 2.
Descriptive statistics of the full sample and the subsample of contradictory respondents who believe vaccination is useful, but who do not wish to become vaccinated against Covid-19.
| Characteristic | Responseitem |
Full sample (N = 2,060) |
Subsample (N = 349) |
P-value of difference$ | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Respondents’ general background | ||||||
| Gender | Female | 1055 | 51% | 206 | 59% | p = 0.0067 |
| Male | 1005 | 49% | 143 | 41% | ||
| Age | 18–24 | 208 | 10% | 41 | 12% | p < 0.0001 |
| 25–34 | 346 | 17% | 76 | 22% | ||
| 35–44 | 358 | 17% | 83 | 24% | ||
| 45–54 | 400 | 19% | 79 | 22% | ||
| 55–64 | 341 | 17% | 38 | 11% | ||
| 65–80 | 407 | 20% | 32 | 9% | ||
| Language | Dutch | 1174 | 57% | 156 | 45% | p < 0.0001 |
| French | 886 | 43% | 193 | 55% | ||
| Education | None | 8 | 0% | 0 | 0% | p = 0.0714 |
| Primary school | 65 | 3% | 6 | 2% | ||
| First degree secondary school | 208 | 10% | 43 | 12% | ||
| Second degree secondary school | 262 | 13% | 53 | 15% | ||
| Third degree secondary school | 715 | 35% | 120 | 35% | ||
| Higher education (non-university) | 495 | 24% | 81 | 23% | ||
| University or post-university education | 278 | 14% | 45 | 13% | ||
| PhD | 21 | 1% | 0 | 0% | ||
| Other | 8 | 0% | 1 | 0% | ||
| Have children | Yes | 1283 | 62% | 208 | 60% | p = 0.3414 |
| No | 777 | 38% | 141 | 40% | ||
| Profession | Working | 1039 | 51% | 216 | 62% | p < 0.0001 |
| Homemaker | 87 | 4% | 14 | 4% | ||
| Student | 168 | 8% | 28 | 8% | ||
| Unemployed | 138 | 7% | 30 | 8% | ||
| Disabled | 131 | 6% | 20 | 6% | ||
| Retired | 497 | 24% | 41 | 12% | ||
| Difficulties with monthly expenses | Never | 847 | 41% | 124 | 35% | p = 0.2371 |
| Once a year | 447 | 22% | 79 | 23% | ||
| Once every three months | 413 | 20% | 77 | 22% | ||
| Every month | 353 | 17% | 69 | 20% | ||
| Respondents’ Covid-19 related background | ||||||
| Self-reported membership of a Covid-19 risk group | No | 1261 | 61% | 265 | 76% | p < 0.0001 |
| Yes, elderly | 384 | 19% | 28 | 8% | ||
| Yes, chronically ill | 424 | 21% | 52 | 15% | ||
| Yes, severe obesity | 133 | 6% | 14 | 4% | ||
| Yes, other | 69 | 3% | 6 | 2% | ||
| Self-reported profession is labelled as 'essential' | Yes | 393 | 19% | 74 | 21% | p = 0.3575 |
| No | 1667 | 81% | 275 | 79% | ||
| Has had a Covid-19 infection | Yes, confirmed with a test | 64 | 3% | 8 | 2% | p = 0.4110 |
| Probably, but not confirmed with a test | 173 | 8% | 24 | 7% | ||
| No | 1823 | 89% | 317 | 91% | ||
| Know personally someone who has had Covid-19 | Yes, confirmed with a test | 314 | 15% | 49 | 14% | p = 0.7480 |
| Probably, but not confirmed with a test | 187 | 9% | 35 | 10% | ||
| No | 1559 | 76% | 265 | 76% | ||
| Know personally someone who was hospitalised for Covid-19 | Yes | 127 | 6% | 12 | 3% | p = 0.0314 |
| No | 1933 | 94% | 337 | 97% | ||
| Know personally someone who died of Covid-19 | Yes | 92 | 4% | 13 | 4% | p = 0.5222 |
| No | 1968 | 96% | 336 | 96% | ||
| Satisfaction with government’s approach to Covid-19 pandemic | Very satisfied | 66 | 3% | 2 | 1% | p < 0.0001 |
| Rather satisfied | 774 | 38% | 92 | 26% | ||
| Rather dissatisfied | 827 | 40% | 158 | 45% | ||
| Very dissatisfied | 393 | 19% | 97 | 28% | ||
| Determination of the vaccine prioritization strategy | Population | 242 | 13% | 58 | 17% | p = 0.1030 |
| Government | 196 | 10% | 29 | 8% | ||
| Scientists | 1466 | 77% | 262 | 75% | ||
Chi-square test to indicate significant differences in proportions between the two samples.
4. Discussion
A majority of Belgians (73%) report that they will definitely or probably get vaccinated against Covid-19, though uptake is predicted to be lower among younger individuals, people at lower risk of severe forms of Covid-19, women, those with lower education, and those with lower trust in authorities. These characteristics have also been identified as predictors of Covid-19 vaccine hesitancy in similar studies in other countries [10], [11], [12], [13], [14].
According to Anderson et al. (2020) [3], if a vaccine has approximately 80% efficacy, it is between 70% and 90% of the population who needs to be vaccinated. If this is the case, the observed share of the population willing to get Covid-19 vaccinated in this representative sample may not be sufficient. However, a sample of 17% of the population was found to be in favour of vaccination in general but hesitant toward Covid-19 vaccination and so, this hesitant group may be a key factor in whether herd immunity against the coronavirus can be achieved within the population. Our study suggests that, rather than focussing on vaccine sceptics or antivaxxers who will be harder to convince that Covid-19 vaccination is necessary, communication and educational efforts should be mainly targeted at the group we identified as being pro-vaccines but doubtful about the specific Covid-19 vaccine.
A limitation of this survey is that it did not collect reasons for Covid-19 vaccine hesitancy to study further the sample of contradictory individuals who consider vaccination useful, but do not wish to get vaccinated against Covid-19. Why are people hesitant? Some of the many reasons behind vaccine hesitancy are related to the success of vaccines to eradicate diseases that used to be deathly and as a result, people focus on the perceived risks of vaccination because they are less aware of the consequences of not vaccinating [5], [16]. In the context of Covid-19, we show that vaccine hesitancy may also be caused by individuals having no personal experience with people in their proximity having been critically ill or passing away as a result of Covid-19 [17] because the willingness to get vaccinated is almost twice higher when knowing someone who has been hospitalised because of Covid-19. However, there is hesitancy toward the Covid-19 vaccine beyond a clear support for the usefulness of vaccination against infectious diseases. This Covid-19 hesitant group differs from anti-vax profiles. Their hesitancy might therefore be explained by particular concerns about the Covid-19 vaccine, e.g., that it has been developed too fast, that the full safety profile of the vaccine is not (yet) entirely understood or where it was manufactured as shown in other studies [12], [13], [14], [18], [19].
To conclude, our study found that a larger than usual share of the general public may prefer not to vaccinate against Covid-19 and this suggests that many feel they cannot make a fully informed vaccination decision. This calls for communication campaigns that comfort people on the safety and efficacy of Covid-19 vaccination, particularly in the hesitant subgroup that is nonetheless pro-vaccination in general.
5. Ethics committee approval
This study did not fall under the Belgian law on experiments as anonymised data collected by a third party were analysed and therefore the Social and Societal Ethics Committee (SMEC) of KU Leuven decided that no approval was needed.
Role of funding source
No funding sources to declare. Roselinde Kessels acknowledges her Elinor Ostrom research grant from Maastricht University which was used to collect part of the data. Also, she thanks the JMP Division of SAS Institute for further financial support.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The authors are grateful to Xan Gregg for providing assistance with the data visualizations in JMP.
Footnotes
Our survey was carried out almost one month before the press release from Pfizer-BioNTech successfully completing their phase III trials for a Covid-19 vaccine (9 November, 2020).
The research company has a pool of 252,597 volunteers, from which it selected a standard panel of 5,500 individuals who resemble the Belgian citizens as well as possible. The company evaluates their pool of participants continuously, systematically eliminates low-quality responders and participation is rewarded with bonus points that lead to vouchers to buy certain products or make donations. Online panels are second-best in comparison with population surveys with randomly drawn participants from a census. However, we checked how our survey sample compared to national Belgium data (see Appendix A) and found that our sample was representative of Belgians for most comparable characteristics but higher educated respondents were overrepresented.
Appendix A. Study sample representativeness compared to overall Belgian population
| Variables | Categories | Study sample | Belgian population§ |
|---|---|---|---|
| Gender | Female | 51% | 51% |
| Male | 49% | 49% | |
| Age | 18–24 | 10% | 11% |
| 25–34 | 17% | 16% | |
| 35–44 | 17% | 17% | |
| 45–54 | 19% | 18% | |
| 55–64 | 17% | 16% | |
| 65–80 | 20% | 22% | |
| Language | Dutch | 57% | 60% |
| French | 43% | 40% | |
| Province | Vlaams-Brabant | 10% | 10% |
| Waals-Brabant | 7% | 3% | |
| Brussels Capital | 9% | 10% | |
| Antwerpen | 15% | 16% | |
| Limburg | 8% | 8% | |
| East Flanders | 13% | 13% | |
| West Flanders | 10% | 11% | |
| Hainaut | 6% | 12% | |
| Liège | 10% | 10% | |
| Luxembourg | 5% | 3% | |
| Namur | 8% | 4% | |
| Education | None or primary school | 26% | 34% |
| Secondary school | 35% | 37% | |
| Higher education | 39% | 29% |
§Source: Statbel
References
- 1.Voysey M., Clemens S.A.C., Madhi S.A., Weckx L.Y., Folegatti P.M., Aley P.K., et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2020;397(10269):99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396(10263):1614–1616. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altmann D.M., Douek D.C., Boyton R.J. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020;395(10236):1527–1529. doi: 10.1016/S0140-6736(20)30985-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAteer J., Yildirim I., Chahroudi A. for the Society for Pediatric Research Advocacy C. The VACCINES Act: Deciphering Vaccine Hesitancy in the Time of COVID-19. Clin Infect Dis. 2020;71(15):703–705. doi: 10.1093/cid/ciaa433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall G.S. Vaccine Hesitancy, History, and Human Nature: The 2018 Stanley A. Plotkin Lecture. J Pediatric Infect Dis Soc. 2019;8(1):1–8. doi: 10.1093/jpids/piy082. [DOI] [PubMed] [Google Scholar]
- 7.Horne Z., Powell D., Hummel J.E., Holyoak K.J. Countering antivaccination attitudes. Proc Natl Acad Sci. 2015;112(33):10321–10324. doi: 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luyten J., Bruyneel L., van Hoek A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine. 2019;37(18):2494–2501. doi: 10.1016/j.vaccine.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 9.WHO. Ten threats to global health in 2019; 2018 [
- 10.Edwards B., Biddle N., Gray M., Sollis K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE. 2021;16(3) doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020;1–15 doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Commun Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCabe S.D., Hammershaimb E.A., Cheng D., Shi A., Shyr D., Shen S., et al. Unraveling Attributes of COVID-19 Vaccine Hesitancy in the U.S.: A Large Nationwide Study. medRxiv. 2021 doi: 10.1038/s41598-023-34340-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luyten J., Tubeuf S., Kessels R. Who should get it first? Public preferences for distributing a COVID-19 vaccine. CEPR Covid Econ. 2020;57:1–19. [Google Scholar]
- 16.Luyten J., Desmet P., Dorgali V., Hens N., Beutels P. Kicking against the pricks: vaccine sceptics have a different social orientation. Eur J Public Health. 2014;24(2):310–314. doi: 10.1093/eurpub/ckt080. [DOI] [PubMed] [Google Scholar]
- 17.Davies C. Imperial Bioscience Review [Internet]. London; 2020. Available from: https://imperialbiosciencereview.com/2020/11/20/how-do-we-tackle-vaccine-hesitancy-and-effectively-communicate-vaccine-safety-to-the-general-public-in-the-covid-19-era/
- 18.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A., et al. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]