Abstract
Context:
Onychomycosis (OM) accounts for 20%–40% of all nail disorders. Slow growth of nails, resistance to antifungal drugs, their side effects, and drug interactions limit treatment options. Q-switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser is approved for nail clearance of OM, however conflicting reports exist in literature about its efficacy. This study was conducted to compare the efficacy of Q-switched Nd:YAG laser.
Aim:
The aim of this study was to find the efficacy of Q-switched Nd:YAG laser (1064 nm) management of OM as monotherapy in comparison to itraconazole.
Settings and Design:
A randomized parallel group, outcome assessor trial was conducted over 18 months from July 1, 2015 to December 31, 2016, at skin center of a tertiary care hospital.
Subjects and Methods:
In the first group, patients of OM were administered 12 weekly sessions of the laser. Second group was administered itraconazole 200 mg twice a day for 1 week per month for the 3 months. Confirmed cases of OM, who had not received treatment 6 months before presentation, were selected and randomly allocated to two groups of 50 each. Onychomycosis severity index (OSI) and visual analog scale (VAS) score were used to assess nail involvement at the start of study, 3 months and 1 year after enrollment.
Statistical Analysis:
Clinical profile of patients was analyzed by chi-square test for qualitative variables. For comparison of quantitative variables, Student t test was performed. A 5% probability level was considered as statistically significant (P < 0.05).
Results:
VAS and OSI showed statistically significant improvement at 3 and 12 months in Group I, while resulting in faster clearance with laser; OSI was comparable in both groups at 12 months. Mycological cure was significantly higher in Group I. Both dermatophytes as well as non-dermatophytes responded well to laser treatment, whereas non-dermatophytes responded better to laser.
Conclusions:
Q-switched Nd:YAG laser is effective in inducing nail clearance in OM and is better than itraconazole in managing non-dermatophyte OM.
Keywords: Itraconazole, nail clearance, onychomycosis, Q-switched Nd, YAG laser
Key messages: Q-switched Nd:YAG laser is an effective treatment modality in the management of onychomycosis. It is better than itraconazole in non-dermatophyte onychomycosis.
INTRODUCTION
Onychomycosis (OM), worldwide in distribution accounts for approximately 20%–40% of all onychopathies.[1] Dermatophytes traditionally are reported as the most common cause of OM in 85%–90% followed by non-dermatophyte fungi.[2] Prolonged wearing of shoes in case of toenails and immunosuppression in general, predisposes to OM.[3,4,5,6]
Treatment of OM is challenging. Options include debridement of nail, mechanical and chemical palliative care, oral and topical antifungal drugs, and their various combinations with cure rates of 40%–80% despite several months use of potent systemic antifungals.[7,8] Oral antifungals may be associated with side effects, and topical therapy and lotions are seldom effective as monotherapy.
Non pharmacological treatment modalities such as photodynamic therapy, infradiode lasers, long pulse and Q switched Neodymium-doped Yttrium Aluminium Garnet (Nd-YAG) laser and Fractional CO2 lasers have hence emerged as an alternative treatment modality.[9,10] The therapeutic effect to laser is due to photothermal, thermomechanical, photo-acoustic, photochemical effects, and selective photothermolysis toward cell wall components chitin, xanthomegnin, and melanin.[11] Temperatures more than 50°C have been shown to have a direct thermal killing effect on fungal mycelia.[12] Chitin surrounding the fungal mycelium is slow to dissipate heat, resulting in heat buildup and rising temperature, which results in fungicidal effect. Lasers have now been approved for increasing the nail clearance in OM.[13]
This study was hence conducted with the aim to study the efficacy of Q-switched Nd:YAG laser management of OM as monotherapy in comparison to itraconazole, which is approved for dermatophyte OM and is used as an off-label indication for non-dermatophyte OM.
SUBJECTS AND METHODS
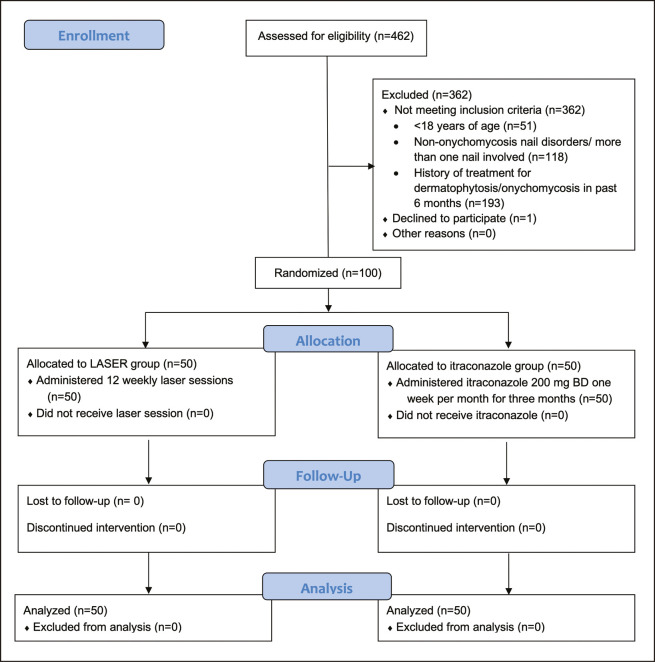
A total of 462 patients over 18 years of age, presenting with nail dystrophy for treatment to the dermatology department of a tertiary care hospital, were evaluated for inclusion to this study [Figure 1]. Those over 18 years of age, with single nail involvement, with no evidence of other disorders affecting nails, such as periungual bacterial infections, subungual hematoma, psoriasis, pityriasis rubra pilaris, atopic dermatitis, and lichen planus, and demonstrable fungus on KOH mount and/or fungal culture positive were included. Molds were only considered pathogenic if these cases showed nail abnormalities consistent with diagnosis, with demonstrated growth on culture of more than five colonies of the same mold in the absence of dermatophyte growth in at least two consecutive nail samplings.[4] Pregnant women and those with deranged liver functions on screening were excluded from the study.
Figure 1.
Consort flow diagram of the study
Selected cases were randomly divided into two groups on a draw of cards with 50 patients each. The study was conducted over a period of one and a half years: July 2015 to December 31, 2016, including a follow-up of 9 months at a tertiary hospital skin center.
Each patient of laser group, irrespective of finger or toenail involvement for consistency of methodology, was administered 12 weekly sessions of (three passes each with a 30-s gap between passes) Q-switched Nd:YAG laser (Neosys, FineMEC, Seoul, Korea), 1064 nm, energy of 350 mJ with a spot size of 1 mm.
Each patient in itraconazole group was administered capsule itraconazole in the dose of 200 mg twice daily for 1 week per month, for 3 months after a baseline screening of complete blood count, liver, and renal function tests. These were repeated after a week and at 3 months. Patients were alerted and advised to watch for side effects.[15]
Photographic record, Onychomycosis severity index (OSI), and visual analog scale (VAS) were maintained at the start of the study and at reassessment at the end of 3 months and at the end of 1 year from the date of enrollment, clinically by OSI[14] and photographs along with repeat cultures and direct microscopy. VAS was taken for the comparison of the result at similar time intervals.
Data were maintained prospectively in a computerized data base. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 20.0. The clinical profile of patients was analyzed by chi-square test for qualitative variables. For comparison of quantitative variables, Student t test was performed. A 5% probability level was considered as statistically significant (P < 0.05).
Endpoints during the study were appearance of any of the following, monitored every week for 12 weeks: Clear nail growth defined by at least 3 mm growth in 12 weeks, mycological clearance, adverse events in the form of redness, skin irritation adjacent to the treated nails or nail beds, intolerance to laser treatment in the form of intractable painful erythema, intractable pain, onychoschizia, onycholysis, or intolerance to oral itraconazole.
RESULTS
The two groups were well matched with no significant statistical difference in age and gender between the two groups. Males were 35 (70%) in Group I and 37 (74%) in Group II. All our patients were between 20 and 45 years of age.
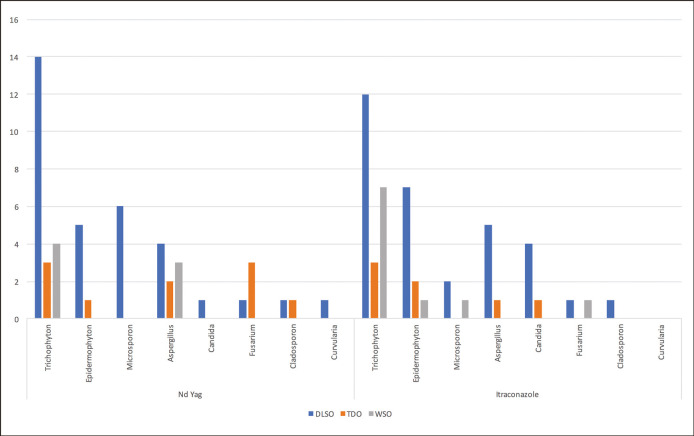
Dermatophyte infection accounted for the majority, 66% in Group I and 72% in Group II with most common species as Trichophyton species [Figure 2]. Coexistent dermatophytosis was observed in 18 cases in Group I and 21 cases in Group II.
Figure 2.
Fungal culture results in both groups at 0, 3, and 12 months of treatment (DLSO = Disto-lateral subungual onychomycosis, TDO = Total dystrophic onychomycosis, WSO = White superficial onychomycosis)
Disto-lateral subungual OM was the most common pattern (33 in both groups); however, there was a statistically significant difference (P < 0.05) in overall pattern occurrence between the two groups [Figure 2].
Fingernail infection was seen in 28 patients in case group and 23 in controls. Response of fingernails and toenails was comparable in both the groups with no statistical difference (P = 0.317).
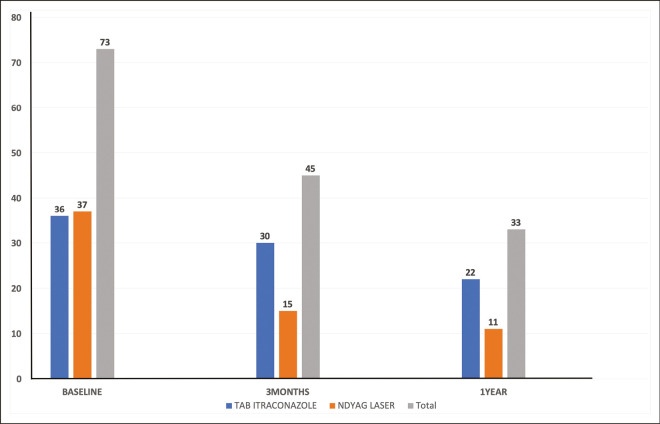
Baseline KOH mount positivity was comparable in both the groups, 37 in case group and 36 in control group. Fungal culture was positive in all at the start of the study. Both KOH mount and fungal culture revealed a statistically significant reduction in Group I compared to Group II at 3 months and 1 year [Figures 3 and 4]. At the end of 3 months, 58% of Group I were culture negative, whereas only 12% of Group II showed mycological cure. At 12 months, this rose to 68% and 32% in Group I and Group II, respectively, which was highly significant (P < 0.001) in both cases. There was no treatment failure in the form of proximal extension of the lesion or increase in the infection during treatment.
Figure 3.
KOH mount status in both groups at 0, 3, and 12 months of treatment
Figure 4.
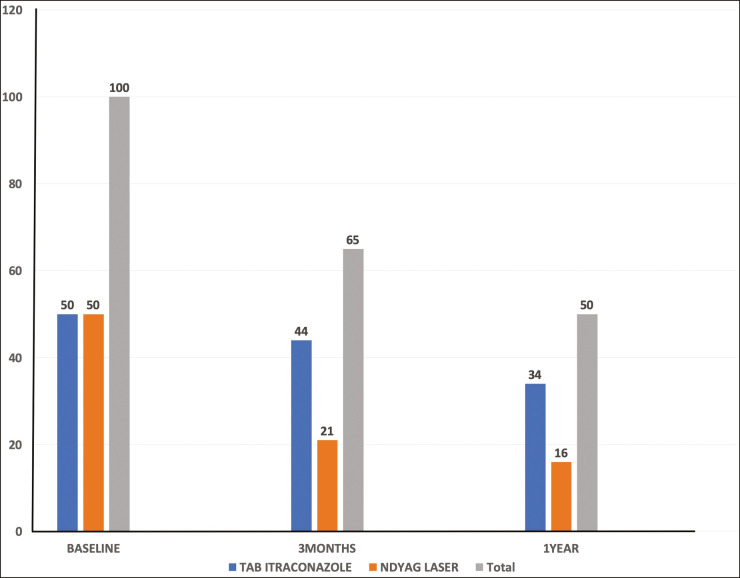
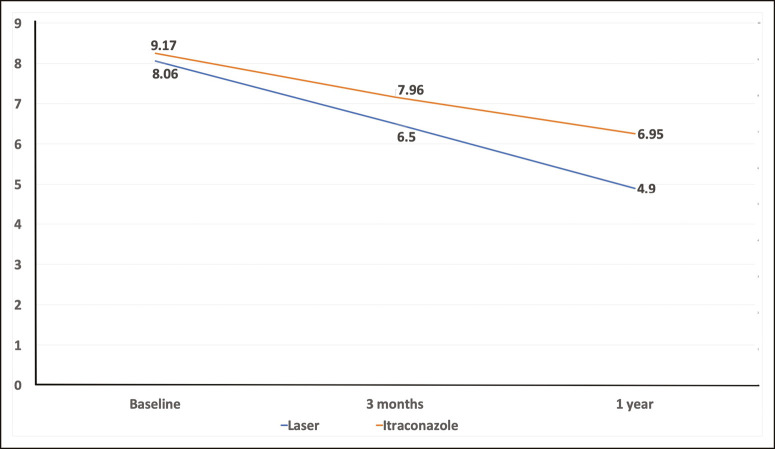
OSI in both groups at 0, 3, and 12 months of treatment
OSI measurement observed a mean fall of 3.16 after 1 year of treatment in Group I and 1.20 in Group II [Figure 5]. In Group I, mean VAS at the end of 1 year was 2.60 as compared to Group II in which mean VAS was 1.1 [Figure 6]. Comparison of the OSI revealed a highly significant improvement in both groups at 1 year; however, the VAS score revealed highly significant improvement (P < 0.001) in the laser group as compared to significant improvement in the itraconazole group when it was compared between 3 months and 1-year follow-up. There was statistically no difference in mean OSI between the two groups at start of the study. A comparison of mean OSI response between dermatopyte and non-dermatophytes revealed a similar response to laser treatment (P = 0.07), while dermatophytes responded better to itraconazole (P = 0.018).
Figure 5.
OSI change on treatment and follow-up
Figure 6.
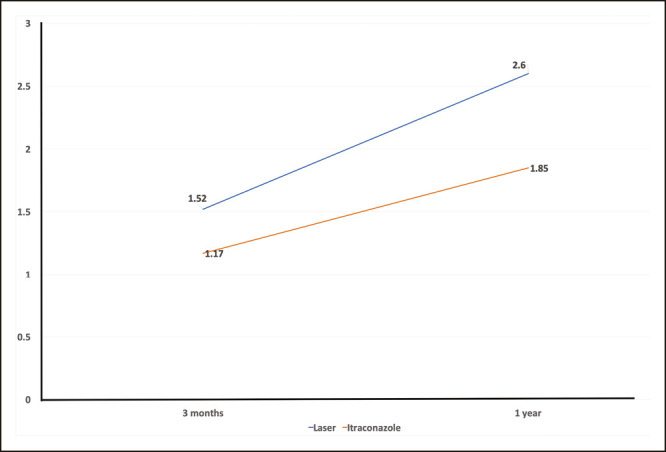
VAS change on treatment and follow-up
Three patients in Group I had mild dryness of the lateral nail folds. Brittleness of nail in three cases in Group I led to distal crumbling of the diseased nail in the first month. It was not progressive and did not interfere with treatment. No other side effects were noted in either group.
DISCUSSION
Treatment options of OM are limited by issues of incomplete cure, poor treatment adherence, and high reinfection rates. Itraconazole is used in weekly pulses to treat OM caused by both dermatophyte and non-dermatophytes.[4] Increasing resistance to antifungals is now presenting as widespread persistent infection.[16]
Long-pulse Nd:YAG laser is the most common device used among lasers in the management of OM. Q-switched Nd:YAG laser as compared to other laser devices, delivers higher energy in short pulses, thus causing a rapid elevation in temperature and photomechanical disruption in the target area, along with immunological stimulation.[17] Our use of a small spot size of 1 mm despite reported literature of 1.5-10 mm spot size was based on this premise and to reduce pain due to lesser depth, and hence three passes were given to induce the aforementioned changes.[18] Reduced penetration due to the small spot size, hence, may not affect the outcome as was seen in our observations.
In our study, male preponderance and age-group of 20–40 years affected, were possibly because of greater outdoor occupation and prolonged wearing of closed footwear. Both gender and age-group were consistent with literature.[19,20]
KOH mount was found positive in 74% for fungal elements, whereas fungal culture was positive in all, which is much higher than that reported[21] possibly because all our patients had received no treatment in the past 6 months. Culture also revealed higher incidence of non-dermatophytes than earlier reported, 34% in Group I and 28% in Group II, but consistent with emerging reports of higher non-dermatophyte nail infections.[4,22,23] A higher mycological cure at 12 months possibly occurred due to continued immunological stimulation in Group I and persistence of drug in nails in Group II, resulting in a better end result. Pattern of OM with a majority presenting as Disto-lateral onychomycosis (DLSO) in both groups is consistent with the known presentations. However, the pattern variation between the two groups was significant (P < 0.05) and was considered as a limitation of our study.
OSI, a validated tool, was used as a clinical tool to assess cases in both groups before and after treatment.[14] A lower OSI reflects a better response to treatment because of lesser severity of involvement. VAS score was also considered as an additional validation tool where a higher score reflected better treatment outcome. A statistically significant improvement in Group I as compared to Group II at 3 months meant a faster nail clearance with laser, whereas at 12 months, both groups showed a highly significant response (P < 0.001), which meant both modalities were ultimately effective. Gupta et al.[13] analyzed 10 trials of lasers in OM from 2010 to 2014, reviewing their different parameters and results. The studies claimed that Nd:YAG can achieve a success rate of 60%–95% in accelerating nail clearance of the fungus over a treatment period of 3–6 months. However, Karsai et al.[19] in a randomized controlled trial of short-pulsed Q-switched Nd:YAG laser concluded that it was not effective as monotherapy.[24]
Assessment by VAS also revealed that Group I had a better response than Group II. Our results are consistent with those of a study by Kalokasidis et al.,[25] which also showed excellent response in >75% of patient and very good response in 50%–74% of the patients.
Mycological cure reported after 3 months of Q-switched Nd:YAG laser treatment reportedly ranges from 82%–96%.[26] However, these studies did not follow up cases for a year after initiation of treatment as in our case. This may account for the lower culture negative (mycological cure) in this study at 1 year, possibly reflecting the longer term efficacy of the laser in OM.
Dermatophytes as well as non-dermatophytes responded to the laser treatment, whereas response to itraconazole was better by the dermatophytes than the non-dermatophytes [Figures 7 and 8]. Poor response of molds to itraconazole is well documented and is consistent with our findings.[27]
Figure 7.
Panel showing comparative pretreatment status (top row) and posttreatment status (bottom row) of dermatophytes and mold at 3 months; OSI change in (A): 15 (17 to 2) Aspergillus sp., (B): 3 (8 to 5) Epidermophyton sp., (C): 4 (6 to 2) Trichophyton sp., (D): 1 (19 to 18) Fusarium sp.
Figure 8.
Panel showing comparative pretreatment status (top row) and posttreatment status (bottom row) of dermatophytes and mold at 12 months; OSI change in (A): 5 (5 to 0) Aspergillus sp., (B): 8 (8 to 0) Trichophyton sp., (C): 4 (6 to 2) Trichophyton sp.
Three patients in Group II had mild side effects, which did not interfere with their management. No other side effects were noted in either groups.
This study had limitations that it was based on clinical findings, that is, clear nail growth and posttreatment KOH mount or fungal culture; however, nail growth rate was not measured. Thus, no quantifiable data regarding nail growth rate were obtained. A negative culture, that is, mycological cure does not always constitute proof of clinical cure due to well-known high rate of false-negative culture results. The authors acknowledge the high culture positive status of our study at baseline may not always ensure true positives in subsequent cultures.
CONCLUSIONS
Our study revealed that Nd:YAG laser (1064 nm) can be used as a treatment modality in diagnosed cases of OM as an alternative to oral or topical antifungals. The findings indicate that using a Q-switched Nd:YAG laser (1064 nm) in patients of OM is more efficacious than itraconazole in nail clearance at 3 months of treatment, and both modalities are effective at 1-year follow-up. The procedure is quick, simple, and uncomplicated. The procedure is quick, simple, uncomplicated, safe and effective even at the small spot size of 1 mm for all OM irrespective of the species of fungi. It thus may help in turning the tide against this resurgent ‘menace’ of dermatophytosis[28] which in its due course results in resistant onychomycosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ghannoum MA, Hajjeh RA, Scher R, Konnikov N, Gupta AK, Summerbell R, et al. A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol. 2000;43:641–8. doi: 10.1067/mjd.2000.107754. [DOI] [PubMed] [Google Scholar]
- 2.Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther. 2010;35:497–519. doi: 10.1111/j.1365-2710.2009.01107.x. [DOI] [PubMed] [Google Scholar]
- 3.Pichardo-Geisinger R, Mora DC, Newman JC, Arcury TA, Feldman SR, Quandt SA. Comorbidity of tinea pedis and onychomycosis and evaluation of risk factors in Latino immigrant poultry processing and other manual laborers. South Med J. 2014;107:374–9. doi: 10.14423/01.SMJ.0000450705.67259.26. [DOI] [PubMed] [Google Scholar]
- 4.Singal A, Khanna D. Onychomycosis: diagnosis and management. Indian J Dermatol Venereol Leprol. 2011;77:659–72. doi: 10.4103/0378-6323.86475. [DOI] [PubMed] [Google Scholar]
- 5.Gupta AK, Gupta MA, Summerbell RC, Cooper EA, Konnikov N, Albreski D, et al. The epidemiology of onychomycosis: possible role of smoking and peripheral arterial disease. J Eur Acad Dermatol Venereol. 2014;14:466–9. doi: 10.1046/j.1468-3083.2000.00124.x. [DOI] [PubMed] [Google Scholar]
- 6.Baran R. The nail in the elderly. Clin Dermatol. 2011;29:54–60. doi: 10.1016/j.clindermatol.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Havu V, Brandt H, Heikkilä H, Hollmen A, Oksman R, Rantanen T, et al. A double-blind, randomized study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nail onychomycosis. Br J Dermatol. 1997;136:230–4. [PubMed] [Google Scholar]
- 8.Mahajan S, Tilak R, Kaushal SK, Mishra RN, Pandey SS. Clinico-mycological study of dermatophytic infections and their sensitivity to antifungal drugs in a tertiary care center. Indian J Dermatol Venereol Leprol. 2017;83:436–40. doi: 10.4103/ijdvl.IJDVL_519_16. [DOI] [PubMed] [Google Scholar]
- 9.Gupta AK, De Doncker P, Scher RK, Haneke E, Daniel CR, 3rd, André J, et al. Itraconazole for the treatment of onychomycosis. Int J Dermatol. 1998;37:303–8. doi: 10.1046/j.1365-4362.1998.00360.x. [DOI] [PubMed] [Google Scholar]
- 10.Gupta AK, Simpson FC. Medical devices for the treatment of onychomycosis. Dermatol Ther. 2012;25:574–81. doi: 10.1111/j.1529-8019.2012.01519.x. [DOI] [PubMed] [Google Scholar]
- 11.Vural E, Winfield HL, Shingleton AW, Horn TD, Shafirstein G. The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci. 2008;23:349–53. doi: 10.1007/s10103-007-0492-4. [DOI] [PubMed] [Google Scholar]
- 12.Paasch U, Mock A, Grunewald S, Bodendorf MO, Kendler M, Seitz AT, et al. Antifungal efficacy of lasers against dermatophytes and yeasts in vitro. Int J Hyperthermia. 2013;29:544–50. doi: 10.3109/02656736.2013.823672. [DOI] [PubMed] [Google Scholar]
- 13.Gupta AK, Foley KA, Versteeg SG. Lasers for onychomycosis. J Cutan Med Surg. 2017;21:114–6. doi: 10.1177/1203475416677722. [DOI] [PubMed] [Google Scholar]
- 14.Carney C, Tosti A, Daniel R, Scher R, Rich P, DeCoster J, et al. A new classification system for grading the severity of onychomycosis: onychomycosis severity index. Arch Dermatol. 2011;147:1277–82. doi: 10.1001/archdermatol.2011.267. [DOI] [PubMed] [Google Scholar]
- 15.Ashbee HR, Barnes RA, Johnson EM, Richardson MD, Gorton R, Hope WW. Therapeutic drug monitoring (TDM) of antifungal agents: guidelines from the British Society for Medical Mycology. J Antimicrob Chemother. 2014;69:1162–76. doi: 10.1093/jac/dkt508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perlin DS, Shor E, Zhao Y. Update on antifungal drug resistance. Curr Clin Microbiol Rep. 2015;2:84–95. doi: 10.1007/s40588-015-0015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhatta AK, Keyal U, Wang X, Gellén E. A review of the mechanism of action of lasers and photodynamic therapy for onychomycosis. Lasers Med Sci. 2017;32:469–74. doi: 10.1007/s10103-016-2110-9. [DOI] [PubMed] [Google Scholar]
- 18.Bhatta AK, Huang X, Keyal U, Zhao JJ. Laser treatment for onychomycosis: a review. Mycoses. 2014;57:734–40. doi: 10.1111/myc.12225. [DOI] [PubMed] [Google Scholar]
- 19.Karsai S, Jäger M, Oesterhelt A, Weiss C, Schneider SW, Jünger M, et al. Treating onychomycosis with the short-pulsed 1064-nm-Nd:YAG laser: results of a prospective randomized controlled trial. J Eur Acad Dermatol Venereol. 2017;31:175–80. doi: 10.1111/jdv.13798. [DOI] [PubMed] [Google Scholar]
- 20.Gupta M, Sharma NL, Kanga AK, Mahajan VK, Tegta GR. Onychomycosis: clinico-mycologic study of 130 patients from Himachal Pradesh, India. Indian J Dermatol Venereol Leprol. 2007;73:389–92. doi: 10.4103/0378-6323.37055. [DOI] [PubMed] [Google Scholar]
- 21.Shenoy MM, Teerthanath S, Karnaker VK, Girisha BS, Krishna Prasad MS, Pinto J. Comparison of potassium hydroxide mount and mycological culture with histopathologic examination using periodic acid-Schiff staining of the nail clippings in the diagnosis of onychomycosis. Indian J Dermatol Venereol Leprol. 2008;74:226–9. doi: 10.4103/0378-6323.39584. [DOI] [PubMed] [Google Scholar]
- 22.Raghavendra KR, Yadav D, Kumar A, Sharma M, Bhuria J, Chand AE. The nondermatophyte molds: emerging as leading cause of onychomycosis in South-East Rajasthan. Indian Dermatol Online J. 2015;6:92–7. doi: 10.4103/2229-5178.153010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asifa N, Farhath K. Current mycological profile of onychomycosis in Kashmir valley: a hospital-based study. J Lab Physicians. 2017;9:190–4. doi: 10.4103/JLP.JLP_131_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaiswal A, Sharma RP, Gupta K. Onychomycosis: a clinicomycological study from western Uttar Pradesh, India. Indian J Med Specialities. 2015;6:8–12. [Google Scholar]
- 25.Kalokasidis K, Onder M, Trakatelli M-G, Richert B, Fritz K. The effect of Q-Switched Nd:YAG 1064 nm/532 nm Laser in the Treatment of Onychomycosis in vivo. Dermatol Res Pract. [Internet]. 2013 [cited 2020 Jun 20];2013. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3875102/ [DOI] [PMC free article] [PubMed]
- 26.Kojarev J, Vizintin Z. Novel laser therapy in treatment of onychomycosis. J Laser Health Acad. 2010;1:1–8. [Google Scholar]
- 27.Piraccini BM, Alessandrini A. Onychomycosis: a review. J Fungi (Basel) 2015;1:30–43. doi: 10.3390/jof1010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panda S, Verma S. The menace of dermatophytosis in India: the evidence that we need. Indian J Dermatol Venereol Leprol. 2017;83:281–4. doi: 10.4103/ijdvl.IJDVL_224_17. [DOI] [PubMed] [Google Scholar]