Abstract
Transitions from one level of care to another are complex processes that pose medical and organizational risks and depend on care integration between different providers. This qualitative study investigated user experiences with an existing digital system for care integration between hospitals and nursing homes, and the potential of artificial intelligence to contribute to its optimization. The findings reveal challenges regarding (a) untimely information, (b) irrelevant information, (c) confusing information, (d) missing information, (e) information overload, and (f) information multiplicity. Artificial intelligence could address these by (i) identifying and verifying low-quality information, (ii) targeting information for different user groups, (iii) visually summarizing relevant information, and (iv) jointly presenting multiple versions. The implications of these findings extend beyond the context of care integration, presenting empirical evidence for the importance of qualitative health research in, and a model for, determining the scope and design of future artificial intelligence solutions to optimize (health)care processes.
Keywords: artificial intelligence, care integration, hospital discharge summary, nursing care plan, transitional care, user perspective, nursing home, qualitative health research
What do we already know about this topic?
Transitions from one level of care to another are complex processes that pose medical and organizational risks and depend on care integration between different providers.
How does your research contribute to the field?
This qualitative study investigated user experiences with an existing digital system for care integration between hospitals and nursing homes, and the potential of artificial intelligence to contribute to its optimization.
What are your research’s implications toward theory, practice, or policy?
This research presents empirical evidence for the importance of qualitative health research in, and a model for, determining the scope and design of future artificial intelligence solutions to optimize (health)care processes.
Introduction
Care for the aging population presents one of the major societal challenges of the 21st century.1 In particular, elderly citizens residing in nursing homes are prone to frequent hospitalizations, changing their care contexts from nursing homes to hospitals and back in a cycle of readmissions and discharges.2 While hospitalization is typically urgent and unplanned, the discharge from hospital to nursing homes represents a complex process, requiring careful planning in order to achieve successful care integration.
In their qualitative metastudy, Allen et al3 identify discharge and transitional care as social processes based on interrogative strategies, which they pose as a foundation for optimizing user experiences in interventions and models for such processes. Canary and Wilkins4 uncovered practical issues and negative emotional experiences encountered in the discharge process, advocating improvements in communication as a primary strategy of improving it. However, already Colón-Emeric et al5 identified the complexity of medical and nursing staff communication within the context of nursing homes. Adding the interorganizational setting between hospitals and nursing homes can be assumed to further complexify the communication.
Naylor et al6 studied how interventions can improve transitional care, finding the use of health IT to be a promising vector of ensuring care integration. And indeed, care integration is increasingly supported by digital health information exchange systems, with countries such as Canada, Denmark, Israel, and Sweden taking the lead.7 In theory, digital care integration systems should be able to provide all the necessary information to the care professionals in nursing homes to ensure an optimal transition of care. However, it is well-known that policy and what actually happens are often at a clash in care contexts such as nursing homes,8 particularly given the high workload of the care professionals involved.
This article investigates user experiences with an existing digital system for care integration between hospitals and nursing homes in Denmark with the aim of understanding the potential of artificial intelligence (AI) to contribute to its optimization. The qualitative study reported upon was conducted under the umbrella of a collaborative research project regarding the user-driven co-development of this care integration system in an interdisciplinary setting between (qualitative) health researchers, AI researchers, and software engineers.
This article unfolds as follows. First, it briefly reflects on the use of AI for optimizing healthcare processes. Then, it describes the context of the study and the methods used for collecting and analyzing data. Then, the findings are presented, revealing 6 challenges of the existing system and suggesting 4 AI solutions that could address these. The article goes on to discuss how this empirical evidence highlights the importance of qualitative health research in determining the scope and design of future AI solutions. Finally, these insights are distilled into a model for the user-driven co-development of AI for the optimization of (health)care processes.
AI for Optimizing Healthcare Processes
AI has a large potential to improve healthcare through improved diagnosis and treatment, improved patient engagement and adherence, and improved administrative processes.9 AI has entered a productive state in diagnostics, routinely outperforming human specialists in tasks such as identifying breast cancer10 and holds great promise in effecting lifestyle changes through health coaching.11
In the face of increasing workloads and stagnating resources, burnout presents a major threat to care professionals’ health and patients’ quality of care.12 Clearly, the use of AI has great potential in optimizing care processes to address this problem, for example, by automating routine parts of administrative processes and by validating information quality.9
Applying AI methods to the optimization of care processes is typically more challenging than improving diagnostics, though. In diagnostics, there is typically a clearly delineated problem (eg, predict breast cancer) on a clearly delineated data set (eg, x-ray images). In contrast, care processes typically involve a number of human actors and the tasks amenable to be optimized by AI and the data available to that end are typically complex and less clearly delineated. Here, AI has the potential to disrupt care processes, both positively by supporting care professionals’ work but also negatively through the “4d-risks” depersonalization, discrimination, dehumanization, and disciplination.13
Davenport and Kalakota9 (p. 97) pose that “the greatest challenge to AI in these healthcare domains is not whether the technologies will be capable enough to be useful, but rather ensuring their adoption in daily clinical practice.” So, arguably, for AI to unleash its potential also for optimizing care processes, a deep understanding of the practices of the actors and the processes they are involved in is needed. AI experts need to closely collaborate with qualitative health researchers to determine the scope and design of AI solutions that could positively disrupt the care processes instead of presenting another item on care professionals’ workload balance.
Context
The context of this study was the public healthcare system in Denmark. In this context, hospitals are operated by the 5 Danish regions while nursing homes are operated by the 98 Danish municipalities. The municipality where a citizen resides before hospitalization is responsible for transitional care after discharge from the hospital. Denmark exhibits high levels of data governance, as well as technical and operational readiness, and has developed one of the most advanced national health information exchange systems.14 The transition of care from the hospital to the municipal setting is supported by this system, which functions as a digital care integration system by allowing hospital staff to provide information to be used by municipal staff in post-discharge care.
The information is sent in the form of 2 types of semi-structured digital reports. The nursing care plan contains information about observed, expected, and potential changes in the citizen’s physical and mental function and care needs. One or several nursing care plans are sent from the hospital to the municipality where the citizen had been registered ahead of the discharge in order to function as a planning tool for municipal care. The hospital discharge summary describes the hospitalization from admission to discharge, including current function and health status, future treatment, and care needs. The hospital discharge summary is sent from the hospital to the municipality at the time of discharge of the citizen.
Both nursing care plans and hospital discharge summaries are created by hospital nursing staff and fulfill different, though related purposes for the 3 types of municipal users relevant in the context of care transition from hospitals to nursing homes: nurses affiliated with the municipal care needs assessment, nurses affiliated with nursing homes, and social care assistants affiliated with nursing homes. Nurses working as municipal assessors are expected to translate nursing care plans into action plans for the changed care needs of citizens returning to their homes or nursing homes. Nurses affiliated with nursing homes are expected to monitor the citizens’ health status and control their medication. The social care assistants perform the bulk of daily health and social care for the citizens.
Methods
The author had extensive experience with qualitative health research, mostly in the form of ethnographic studies with the aim of uncovering patient perspectives and had previously worked in close collaboration with general practitioners and care professionals, also in the context of nursing homes. The focus in these lines of research was not on the experiences of (health)care professionals but typically on those of patients. Accordingly, the researcher approached the study neither as a naive outsider nor as an informed insider but as an insider-outsider occupying the space in between.15
A combination of individual in-depth interviews and thematic focus groups was used to investigate the experiences of nurses and social care assistants as participants of the discharge process and as users of the care integration system. The conversational in-depth interviews allowed for deep reflections on the subject of the study while the focus groups helped participants to articulate their experiences through a facilitated dialog with colleagues that they were well-acquainted with. These conversational methods were complemented by the author immersing themselves in the field in order to observe how the care professionals interacted with both the existing digital care integration system and an early prototype of the AI solution. Here, the researcher filled an observer-as-participant role,16 with care professionals aware of but mostly ignoring the presence of the researcher.
Participants
The project and the associated care professionals constituted an intrinsic serviceable sampling frame. The participants of the study, nurses and social care assistants, were sampled purposively through typical instance sampling17 while ensuring roughly equal distribution of professions. Professionals without sufficient recent experience of using the existing digital care integration system were excluded.
The recruited sample consisted of 11 nurses and 16 social care assistants, aged between 28 and 57. The gender distribution was skewed at 25 females and 2 males, which closely reflects the gender distributions in nursing (3.5%) and social care (7%) professions in the Danish context.
Data Collection
The data were collected during the runtime of the collaborative project in 2018 and 2019 in 3 stages. In the first stage, data on experiences with the discharge process and the use of the existing digital care integration system were collected. In the second stage, the idea of an AI-enhanced care integration system was presented and user expectations to such a system were the primal focus points. In the third and last stage, user feedback, reflections, and experiences with an early prototype of the AI solution were collected. The later stages were designed after careful pre-analysis of the completed stages, allowing early insights to inform the further data collection process.
The researcher conducted the interviews and moderated the focus groups, all of which were audio recorded and transcribed. Fieldnotes with reflections were written immediately afterwards as well as during the observations of user interactions. The shortest interview was just under 60 min while the longest focus group was longer than 180 min. The fieldnotes on the observations were rather extensive, including details such as the areas of the screen that the care professionals focused on.
Ethics and Data Management
The collection and processing of the data were reported to the Danish Data Protection Agency as part of the collaborative research project. Ethical clearing by the Danish National Committee on Health Research Ethics is not required for this type of study. Participants were well-informed about the purpose of the study and consented and volunteered to participate in writing. Care processes and nursing homes represent a sensitive research context.18 Thus, ensuring participant anonymity was a priority. To avoid reidentification of participants by their employers, Saunders et al’s19 best practice recommendations regarding participant anonymity were adapted by only referring to professional roles, by merging related accounts, and by splitting unrelated accounts.
Data Analysis
The open coding20 of the data resulted in an extensive set of codes that were consecutively grouped into higher-order codes,21 giving rise to themes of “challenges” with sub-themes “information quality” and “information amount” as well as “solutions” with sub-themes “organizational” and “AI.” The categories of codes comprising these themes resulted in the identification of the 6 challenges and the 4 suggested AI solutions outlined in the following section.
Several strategies to ensure internal validity and trustworthiness were employed,22 including the determination of sample size through data saturation23 and methods and data triangulation,24 among others making use of fieldnotes from observations in the interpretation of interview and focus group transcriptions. Furthermore, the three-stage research design allowed to validate insights from the pre-analysis of previous stages during following interviews and focus groups.
Findings
To begin with, the analysis revealed that users of the existing care integration system indeed experience challenges with it. The main problem seemed to be that users experienced reading the nursing care plans (abbreviated as NCPs in the remainder of this section) and hospital discharge summaries (abbreviated as HDSs) as time-consuming:
Social care assistant: I find it hard to read all the information the hospital sends. We have many residents here that come back from the hospital. I simply don’t have enough time to sit down and read up in detail on each of them!
This experience is shared by both nurses and social care assistants, who are experiencing increasing workloads and, in particular, increasing requirements regarding documentation of their work processes:
Nurse: Now, we are using a lot more time to find out where do we need to write what, where do we find the relevant information, who do we need to communicate to? It is quite challenging for us.
Furthermore, different users were found to use the information provided by the care integration system differently. Nurses working as municipal assessors were indeed focusing primarily on NCPs while those affiliated with nursing homes were reading both types of reports, spending a large amount of time doing so. Social care assistants used NCPs to prepare for the arrival of discharged citizens:
Social care assistant: The NCP also helps us to find out what information we are missing and ask the hospital staff to elaborate on certain points.
The social care assistants valued also the HDSs in the creation of action plans for individual citizens:
Social care assistant: In the HDS, there is a section called “future agreements”, which is not part of the NCPs. This is very practical to have and avoids duplicating work.
The participants largely agreed on 2 points: reading thoroughly through all NCPs and HDSs is challenging and time-consuming but necessary as it provides valuable information essential for them to perform their job functions as part of the care processes for the elderly citizens.
The following subsections outline the 6 themes regarding the challenges participants experienced with the existing care integration system as well as how the introduction of artificial intelligence might address these challenges and which data would be required to that end (see Table 1 for a summary). First, the 6 challenges of the existing care integration system as experienced by users are presented grouped into 2 categories regarding the quality of the information and its amount. Then, possible AI solutions and how they have the potential to address these challenges are introduced.
Table 1.
Summary of Challenges and AI Solutions Identified, with Connections Indicated.
| Challenges identified | Information quality | Information amount | ||||
| (a) Untimely information | (b) Irrelevant information | (c) Confusing information | (d) Missing information | (e) Information overload | (f) Information multiplicity | |
| Information is outdated or not yet relevant | Information is not relevant at all or only to a group of users | Information misplaced or insufficiently structured | Relevant information has not been provided | There is more information than users can process | There are multiple versions of the information | |
| ||||||
| Potential AI solutions | (i) Identify and verify low-quality information | (ii) Targeted information for different user groups | (iii) Visually summarize relevant information | (iv) Jointly present multiple versions | ||
| Identify outdated, irrelevant, confusing or missing information using AI, visualize it to users, and recommend information creators to amend, move, or verify low-quality information | Identify the varying informational needs of different user groups and intelligently adapt the ordering, selection, and presentation of the information to the identified varied needs | Select a certain number of most relevant topics, fully-automatically identify those parts of the information that contribute most to these topics, and visualize them to the users | Compute the differences between multiple concomitant versions, evaluate them in relation to significance, and present them in reverse-chronological order to the users | |||
| Required data | Unlabeled NCPs and HDSs, preferably with only high-quality reports having been selected by care professionals | NCPs and HDSs where each section is labeled with its relevance, manually labeled by care professionals | Excerpts from NCPs and HDSs relevant to the topics selected and manually labeled by care professionals | Semantic text similarity scores for pairs of texts, reusing existing clinical data sets extracted from electronic health records | ||
Challenges Regarding the Quality of the Information
The quality of the information is an important contributor to the value of the care integration system. The other way around, low-quality information leads to suboptimal care processes through ill-informed action plans as well as extra time consumption due to increased needs for communication with hospital staff outside of the care integration system. The analysis identified many concerns regarding quality, which have been grouped into the 3 themes presented in this subsection.
(a) Untimely information
Outdated information is a typical case of low-quality information that imposes additional workload on care professionals:
Nurse: Once, an old remark had been copied into the HDS. It said that the citizen was unable to receive nourishment orally. The social care assistants came to me and were worried how they should handle that? We had to create an emergency plan. But then I saw a new correspondence with an update on the functionality of the elderly citizen, stating that the problem had been resolved.
While this situation was resolved rather quickly thanks to information external to the care integration system, in some cases the outdated information disturbs care professionals’ work until after the citizen has been discharged. A citizen was flagged as currently undergoing severe hallucinations in the HDS, where apparently information from a previous NCP had been copied into the category of “psychosocial conditions.” This outdated information caused extra preparations for the citizen’s arrival, which turned out to be entirely unnecessary:
Social care assistant: I was prepared to receive a citizen who sees flying elephants, green pigs, and dead people. Then, he arrived and presented himself calmly and absolutely sane.
Due to confidentiality concerns, no cases with directly detrimental effects on the care outcomes were related. Nevertheless, even in these 2 more harmless cases, outdated information resulted in care processes for other citizens being degraded as working time was spent on unnecessary emergency plans and preparations instead of actual care.
While outdated information was the main concern regarding timeliness, premature information also presented a challenge:
Social care assistant 1: You can see that this HDS was sent on the 14th and the elderly citizen was discharged on the 16th.
Social care assistant 2: It is a bit too early because a lot of things can change in two days.
Information that arrives before time has low relevance and is, consequently, obstructing rather than assisting care processes.
(b) Irrelevant information
Unlike outdated information, irrelevant information poses no direct harm to the care process. But like premature information, it obstructs care processes as it consumes time and hinders access to relevant information:
Nurse: I don’t care how many children the elderly citizen has at home. I want to know when the hospital has taken a blood sample, what the current dose of the medication is, when to take another blood sample. It takes a very long time to figure this out.
Finding the relevant information in an extensive report is a time-consuming process, as much of the provided information is deemed irrelevant.
In addition to irrelevant contents of the sections of the reports, some sections are considered irrelevant in their entirety:
Social care assistant: The field “sexual activity” often is filled by stating that it is not relevant. Why is it included if it rarely is relevant, and I anyway don’t have to do anything with its contents?
Irrelevant information also induces processes of reflection, as they often pose more questions than they provide answers:
Social care assistant: Here from the report: “Before hospitalization, the patient experienced that his home was invaded.” Ok, but what should I do with this information? Does it somehow affect the current state of the citizen?
This type of irrelevant information is more confusing than supporting care professionals’ preparations for the discharge of the elderly citizen.
(c) Confusing information
The existing care integration system does not have the possibility to analyze the contents of the sections and ensure their consistency. Thus, different sections of a report can and do contain contradictory information:
Nurse: The citizen needs help with medication? Ok. It says so here, but further up it said they didn’t.
In this case, the nurse had to clarify the situation by contacting the hospital staff outside of the care integration system, delaying the processing of the NCP and using valuable time. Another source of confusion stems from misplaced bits of information that end up in sections where they do not belong while they are missing in those, where they do. During observation of a social care assistant reading through an HDS, the social care assistant suddenly seemed a bit tense. Asked about what was going on, she explained that information was misplaced:
Social care assistant: Here under “Living situation” it says: “Patient eats well in company of others.” This says nothing about who he lives with. That’s not how this section is supposed to be filled. That information belongs under “Nutrition” or maybe “Psychosocial conditions”.
The fieldnotes specify that she feels that the careless filling of the reports is “disrespectful” and “devaluates her work.” Her emotional response seems to be based on experiencing confusing information as increasing the already high workload of care professionals:
Social care assistant: The information is quite mixed up. We’re not able to easily find what we need, what is relevant for us, we have to filter through a lot.
Filtering through the rather long reports presents a challenge, as it means that other tasks will have less time allocated to them. This leaves many of the participants with a feeling of performing their job inadequately.
Challenges Regarding the Amount of Information
The right amount of information requires a precarious balance between the need for succinctly summarized presentations of the most important aspects and the need to include all potentially relevant information. The analysis identified many concerns regarding quality, which have been grouped into the 3 themes presented in this subsection.
(d) Missing information
Incomplete information can obstruct care processes through the same mechanism of posing more questions than providing answers described above for (b) irrelevant information:
Social care assistant: This section says that the need for assistive devices has to be evaluated. Who has to evaluate this? Me?
Here, the information is missing regarding who the recipient of this request is. The field notes specify that the “social care assistant looks puzzled; she feels ill-equipped to evaluate this.” In further discussion, it became apparent that the social care assistant would feel irresponsible if she just ignored this request.
The matter is further aggravated when important information is obviously missing, as was observed in a nurse’s interaction with an HDS in the care integration system:
Nurse: Eating, drinking – ok, he got a stoma. But what about urination? That information is missing.
Here, the presence of newly established stoma indicated in the HDS necessitates information about urination that was blatantly absent.
(e) Information overload
Both the NCP and the HDS contain many sections to fill, with the HDS allowing even more information to be included:
Nurse: The NCP contains a lot of data, but it only provides a here-and-now picture. The HDS is a little more complex than the NCP. It contains additional sections such as “diagnosis” and “future agreements”. You can go into more depth regarding the description of how the patient is.
The extensive information contained in NCPs and HDSs satisfies the users need to understand the citizen’s state and care needs after the hospital discharge. But the sheer amount of information is overloading the care professionals, both with regard to time consumption and ensuring that relevant information is not overlooked:
Social care assistant: First, I look at the discharge date to figure out how much time we have to make the arrangements for receiving the soon-to-be discharged citizen. Further down it gets messier, look how much text there is! And look, there are three NCPs regarding this hospitalization!
Not only is the amount of information contained in a single report overwhelming, but there are typically also multiple such reports, multiplying the amount of information that has to be processed by care professionals.
(f) Information multiplicity
The existence of several versions of closely related information such as several NCPs and an HDS for the same hospitalization often give rise to information multiplicity, where the same bits of information occur in several versions. To create a new version of an NCP or an HDS, hospital staff often start from copying the entire contents from a previous NCP, often without verifying whether all duplicated information is still relevant. This challenge is related by 2 nurses functioning as municipal assessors when discussing multiple NCPs:
Nurse 1: What is the new information? That’s hard to figure out and identify. The hospital staff don’t have time to delete the old information from the NCP.
Nurse 2: Yes, it’s easy to miss something important.
The information duplicated from previous versions makes it hard to compare the contents of the 2 versions and determine what has changed from 1 version to another, requiring a full manual comparison of 2 versions.
The same problem is related by a nurse affiliated with a nursing home regarding HDSs:
Nurse: I can only see the differences between the NCP and the HDS when I remember that a certain piece of information wasn’t there the day before. Otherwise, I have to read it as a whole every time.
Obviously, the care professionals’ ability to memorize the NCPs for multiple patients is limited. The practice of generating new NCPs and HDSs from previous NCPs is, thus, creating a significant amount of potentially avoidable workload.
Potential AI Solutions
Based on the challenges identified from user experiences with the existing care integration system and user expectations to an ideal system, a number of potential AI solutions were devised and qualified with the help of feedback from AI experts that were part of the collaborative project. Depending on feasibility and available project resources, these solutions were partly implemented in an early-stage prototype of an AI-improved care integration system. User feedback on the prototype was analyzed to further qualify and revise the AI solutions, arriving at the 4 presented in this subsection.
(i) Identify and verify low-quality information
A first type of AI model could be trained with existing NCPs and HDSs in order to learn which information is expected to be placed in which section. The trained model could be used to predict the most likely section for some bit of information together with a confidence score. If the predicted most likely section is different from the section the information was filled in, the system could indicate this to users. More fruitful, the system could give real-time feedback during the creation of the report, suggesting that the content be moved to another section. If the confidence score for the information in a given section is low, this could indicate that the information is incomplete, and the system could suggest amending the information. This model would, thus, contribute to identifying and correcting misplaced and missing information.
A second type of model could be trained in order to learn which bits of information are expected to be in a report given the type of the report (NCP or HDS) and the other bits of information occurring in the report. By learning the co-occurrence relation between bits of information, the system would contribute to identifying untimely, irrelevant, and missing information: if a bit of information is present but unexpected, this could indicate irrelevant or untimely information, and if a bit of information is expected but absent, this could indicate missing information. Like with the first model, the results could be indicated to users or, preferably, lead to suggestions for the creators to improve the report.
In both cases, the main benefit would be to providing hospital staff with real-time feedback during the creation of NCPs and HDSs. As this was out of scope for the collaborative project framing this study, this solution was not included in the early-stage prototype. Instead, the focus was on integration with the Danish joint medicine card, a database holding past and current medication information from hospitals and general practitioners:
Social care assistant: Sometimes I think it would be nice to know what medicine has been administered. For example, what type of painkillers were given? If the citizen had a lot of pain, did the hospital staff reduce the dose quickly? Maybe there is some medication that they got but which stopped before the report was filled.
Verifying and amending the information about medication needs in the reports would improve the information quality for the users without the need to change the creation process.
(ii) Targeted information for different user groups
A system that targets information to different user groups (eg, municipal assessors, nursing home nurses, and social care assistants) would contribute to increasing information relevance and alleviate information overload. Such targeting requires an assessment of the varying informational needs of different user groups and could be used to adapt the ordering, selection, and presentation of the information accordingly.
A simple solution not relying on AI could be to use a different but fixed order, selection, and presentation of the sections for the 2 user groups. Such a static solution is unlikely to meet the informational needs of the care professionals, though, as these needs are dynamic and not necessarily directly linked to particular sections:
Social care assistant: For me, most important is knowing what they have been hospitalized for. How was their status before? What is their status now? Why are they here at the nursing home? What is the purpose of staying here? How long are they staying here? Is there anything we need to pay particular attention to? Any specific medical issues?
Ideally, an AI-solution would have to dynamically order, select, and present information from the reports, taking their content into account. To train such an AI model, labeled data would have to be collected from many interactions with concrete NCPs and HDSs, where the care professionals would have to indicate how relevant particular sections were for a given report by assigning labels (eg, 0 for irrelevant, 1 for nice-to-know, 2 for need-to-know) to all its sections. Such a labeling function in the system could also be used to personalize the AI solution at the individual or institutional level.
(iii) Visually summarize relevant information
The insights from the qualitative study indicate that there are certain areas that are of particular interest to care professionals, including medication needs, nutrition and hydration, bowel and bladder management, and functional mobility. These areas could be represented as immediately recognizable pictograms and color-coded according to the degree to which citizens need care in these areas according to the information in the report.
An AI-model could be trained to perform this color coding based on scores and descriptions from the reports. The first AI model from (i) could be adapted to identify all the bits of information that are relevant to each of the areas. The care professionals as users would then assist in the generation of labels for these sets of information by providing their assessment on a three-color scale (green for no-assistance-needed, yellow for some-assistance-needed, and red for full-assistance-needed) after the patient has successfully been (re)integrated in the nursing home. An AI model trained on such a labeled data set could be chained with the adapted AI model from (i) with the purpose of identifying relevant information from the reports and color-code the areas of interest accordingly in the visualization of the report.
The choice of a red-yellow-green tri-coloration was received favorably by the users interacting with the early-stage prototype. The main reasons are users’ familiarity with such scales and their ability to attract attention to the items marked in red:
Social care assistant: Yes, when something is marked red, I will click on it. When it says that there is something important regarding bowel and bladder management – is it because he is unable to urinate without assistance? Or does he have a catheter or stoma? It would be nice you could click on it and get to know what is going on.
The users expressed a desire for getting to know the reasons for the color-coded score. This desire could be satisfied by using techniques from the rapidly developing field of explainable AI.25 The early-stage prototype would need to be developed further to use an explainable AI model to color-code the areas of interest and comprehensibly visualize its explanation to the users.
Notably, the tri-coloration was not found to prevent the participants from reading yellow and green information. In the observations, they rather used it as a help to prioritize their attention and the order of their reading:
Nurse: The colours provide a quick overview. My focus quickly falls onto the items relevant for us nurses. Of course, I anyway skim through the other parts.
As a note of caution, it remains unclear whether this is due to the participants being observed and, consequently, whether users in everyday contexts would still opt to read through entire reports.
(iv) Jointly present multiple versions
The redundancy caused by information multiplicity between several versions of NCPs and an HDS for a single hospitalization is the foundation of a large amount of potentially avoidable workload for care professionals. To realize this potential, the improved care integration system needs to compute the differences between multiple concomitant versions of reports and present them understandably to the users.
The most recent information is usually perceived as the most relevant:
Nurse: My request would be that it is always the latest.
To this end, the early-stage prototype used reverse-chronological order for displaying multiple versions as 1 version with differences. This was generally received favorably by the participants.
The prototype worked fine without relying on AI as long as unchanged information was copied straight from previous versions. When the same information was supplied in different formulations, the system naturally failed to recognize this, presenting the same information as different. The field notes summarize that “users have to read the same information twice, believe there is a significant difference, puzzled because they cannot find the difference.”
The early-stage prototype could thus be improved by an AI solution that does not compute differences syntactically as changed characters in a text but considers the semantic similarity between the information contained in these texts.
As an example, consider the texts “the patient can stand up without help” and “the senior citizen does not need assistance to get up.” Syntactically, these are different and would be highlighted as a change to consider between different versions of reports by a simple solution based on syntactic text comparison. Semantically, the 2 sentences are all but indistinguishable and should not be highlighted as different. Existing AI models for semantic textual similarity26 could be fine-tuned on clinical semantic textual similarity data sets extracted from electronic health records27 to be able to assess the semantic similarity of such sentences. This could provide a more robust solution for handling information multiplicity that avoids falsely highlighting semantically inconsequential changes and, hence, reduce the workload of care professionals.
The integration of new technologies such as the suggested one is, of course, always a disruption of existing care processes, as users are initially not trained to understand the new way that for example, multiple reports are presented. To alleviate these disruptive effects, it is important that users feel that it is okay to be struggling at first and to know where they can obtain help in everyday interactions with the system:
Social care assistant: I’m not really yet a super user of this system, but when one of us can’t figure it out, we ask each other for help. And often that works well, as one of us has experienced something similar before.
The role of colleagues rather than formal technical support was a recurring topic in the interviews and focus groups and seems to be a sensible way of easing the adoption of AI solutions into care processes.
Discussion
The findings regarding the challenges with the existing digital care integration system all concern information quality or information amount. Thus, they support Colón-Emeric et al’s5 results on the complexity of the communication in nursing homes and extend them by providing empirical evidence for a further increase of complexity in an interorganizational setting with predominantly digital communication between the organizations. The potential AI solutions identified to address the challenges jointly aim at improving the communication efficiency and effectivity to solve both practical issues and improve the emotional experience of the staff, lending support to Canary and Wilkins4 recommendation to improve the discharge processes.
Given the nature of digital care integration systems, many communication aspects worth improving are inherently more amenable to AI solutions than to traditional measures of improving interpersonal communication. These solutions are supporting the interrogative strategies of the users by providing higher-quality information and assisting the process of seeking and assessing information, effectively supporting the negotiation and navigation of the transition of care from hospital to nursing home.3
The insights, challenges, and potential AI solutions gained from the co-development of a care integration system turned out to be rather general with no or only minor context dependency. It is thus not unreasonable to assume that they would be applicable beyond the context of care integration for discharge from hospital to nursing homes, allowing us to potentially transfer some of the results to different kinds of (health)care processes and the health information exchange systems7 supporting these.
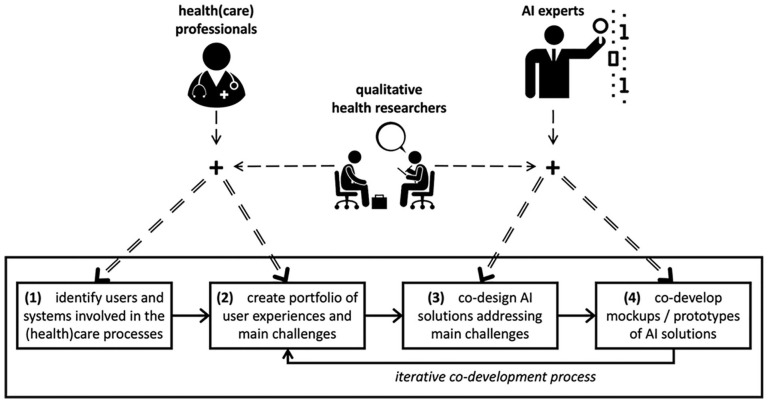
To aid this transfer, this article condenses the experiences and insights from this study into the User-driven Co-development of AI (UCAI) model for the optimization of (health)care processes presented in Figure 1. This model allows involving the experiences, expectations, and feedback of users into the process of determining the scope and design of AI solutions. Furthermore, as exemplified for AI solutions (ii) and (iii), the process suggested in the model has the potential to create valuable (labeled) training data for creating new and refining existing AI solutions based on user feedback.
Figure 1.
User-driven co-development of AI (UCAI) model.
The model comprises 3 main categories of actors:
The category of health(care) professionals includes the health and healthcare professionals affiliated with municipal, regional, and national organizations and institutions that are or will directly or indirectly fill the role of users of the system.
The category of qualitative health researchers covers both medical and organizational anthropologists as well as other health researchers working with qualitative methods.
The category of AI experts typically comprises experts in AI methods such as machine learning researchers and data scientists, software engineers and developers, as well as privacy experts and AI ethicists who play an increasingly significant role in the development of AI solutions.28
Scaffolding on the diverse but complementary practitioner and researcher skills of these actors, the UCAI model unfolds in 4 steps, possibly with iteration:
(1) The relevant users and health information exchange systems involved in the (health)care process to optimize are identified by the qualitative health researchers based on a first round of data collection involving (health)care professionals.
(2) The (health)care professionals’ user experiences with, expectations for, and feedback on the current state of the systems are investigated by the qualitative health researchers, resulting in a portfolio of the main challenges to be addressed.
(3) The qualitative health researchers communicate the challenges to the AI experts and jointly co-designs potential new or refined AI solutions that address one or multiple challenges identified in the previous step with them.
(4) The AI experts co-develop the AI solutions in close collaboration with the qualitative health researchers, yielding mockups, proof-of-concepts, or prototypes. These AI solutions are then iteratively investigated by returning to Step (2).
While the model to a certain degree hides the organizational complexity behind and the interrelation of the different types of health(care) professionals by grouping them in 1 actor category, the different perspectives of users at hospitals, municipalities, and nursing homes obviously constitute valuable sources of insights. Diligently uncovering and considering this multiplicity of users is one of the key tasks of the qualitative health researchers in Steps (1) and (2) of the model.
The user-driven co-development of AI solutions in close collaboration with qualitative health researchers has direct benefits for technical companies and research groups active in the field of AI in healthcare. By involving the users of the solutions from the onset of the development, it allows them to overcome the not-invented-here phenomenon29 and deliver solutions that are aligned with user needs and can be embedded organizationally. The UCAI model, thus, addresses Davenport and Kalakota’s9 main challenge of ensuring the adoption of AI solutions in daily clinical practice.
Finally, yet importantly, the findings and model can be viewed as supportive of addressing 2 of Rubeis’13 “4d-risks” of AI for care processes. The user-driven co-development of AI solutions to support rather than replace (health)care processes has the potential to avoid the pitfalls of depersonalization and, above all, dehumanization of care processes.
Conclusion
The integration of AI solutions into (health)care processes holds great potential but is inherently a complex process. This article has provided empirical evidence for the importance of qualitative health research in the process of determining the scope of future AI solutions for the optimization of (health)care processes and to aid in their design and specification. User-driven co-development of such AI solutions based on a close collaboration between technical experts and qualitative health researchers seems fruitful and can take its onset in the UCAI model presented in this article.
Further research is needed to determine the utility of the model in (health)care processes other than care integration. Last, but not least, future qualitative health research is needed to understand how to develop the field of AI in healthcare from a focus on full automation of human tasks toward the augmentation of human-delivered healthcare and, ultimately, toward the creation of hybrid intelligent systems comprising a true symbiosis of human and artificial intelligence.
Footnotes
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The data collection for this study was part of the collaborative research project VIND co-funded by the European Union (ERDF) and the Danish state (SVF).
ORCID iD: Anna Schneider-Kamp  https://orcid.org/0000-0001-9822-6996
https://orcid.org/0000-0001-9822-6996
References
- 1. Conroy S, Dowsing T. What should we do about hospital readmissions? Age Ageing. 2012;41(6):702-704. doi: 10.1093/ageing/afs154 [DOI] [PubMed] [Google Scholar]
- 2. Dobrzanska L, Newell R. Readmissions: a primary care examination of reasons for readmission of older people and possible readmission risk factors. J Clin Nurs. 2006;15(5):599-606. doi: 10.1111/j.1365-2702.2006.01333.x [DOI] [PubMed] [Google Scholar]
- 3. Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care integration in transitional care for older people from hospital to home: a meta-synthesis. Qual Health Res. 2017;27(1):24-36. doi: 10.1177/1049732316658267 [DOI] [PubMed] [Google Scholar]
- 4. Canary HE, Wilkins V. Beyond hospital discharge mechanics: managing the discharge paradox and bridging the care chasm. Qual Health Res. 2017;27(8):1225-1235. doi: 10.1177/1049732316679811 [DOI] [PubMed] [Google Scholar]
- 5. Colón-Emeric CS, Ammarell N, Bailey D, et al. Patterns of medical and nursing staff communication in nursing homes: implications and insights from complexity science. Qual Health Res. 2006;16(2):173-188. doi: 10.1177/1049732305284734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30(4):746-754. doi: 10.1377/hlthaff.2011.0041 [DOI] [PubMed] [Google Scholar]
- 7. Zelmer J, Ronchi E, Hyppönen H, et al. International health IT benchmarking: learning from cross-country comparisons. J Am Med Inform Assoc. 2017;24(2):371-379. doi: 10.1093/jamia/ocw111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hyman RB, Bulkin W, Woog PC. The staff’s perception of a skilled nursing facility. Qual Health Res. 1993;3(2):209-235. doi: 10.1177/104973239300300205 [DOI] [Google Scholar]
- 9. Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94-98. doi: 10.7861/futurehosp.6-2-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McKinney SM, Sieniek M, Godbole V, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577(7788):89-94. doi: 10.1038/s41586-019-1799-6 [DOI] [PubMed] [Google Scholar]
- 11. Everett E, Kane B, Yoo A, Dobs A, Mathioudakis N. A novel approach for fully automated, personalized health coaching for adults with prediabetes: pilot clinical trial. J Med Internet Res. 2018;20(2):e72. doi: 10.2196/jmir.9723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cooper SL, Carleton HL, Chamberlain SA, Cummings GG, Bambrick W, Estabrooks CA. Burnout in the nursing home health care aide: a systematic review. Burn Res. 2016;3(3):76-87. doi: 10.1016/j.burn.2016.06.003 [DOI] [Google Scholar]
- 13. Rubeis G. The disruptive power of artificial intelligence. Ethical aspects of gerontechnology in elderly care. Arch Gerontol Geriatr. 2020;91:104186. doi: 10.1016/j.archger.2020.104186 [DOI] [PubMed] [Google Scholar]
- 14. Eichler H-G, Bloechl-Daum B, Broich K, et al. Data rich, information poor: can we use electronic health records to create a learning healthcare system for pharmaceuticals? Clin Pharmacol Ther. 2019;105(4):912-922. doi: 10.1002/cpt.1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dwyer SC, Buckle JL. The space between: on being an insider-outsider in qualitative research. Int J Qual Methods. 2009;8(1):54-63. doi: 10.1177/160940690900800105 [DOI] [Google Scholar]
- 16. Junker B. Some suggestions for the design of field work learning experiences. Cases Field Work Chic Univ Chic Part III-A. 1952. [Google Scholar]
- 17. Emmel N. Sampling and Choosing Cases in Qualitative Research. SAGE Publications; 2013. [Google Scholar]
- 18. Kayser-Jones J. Continuing to conduct research in nursing homes despite controversial findings: reflections by a research scientist. Qual Health Res. 2003;13(1):114-128. doi: 10.1177/1049732302239414 [DOI] [PubMed] [Google Scholar]
- 19. Saunders B, Kitzinger J, Kitzinger C. Participant anonymity in the internet age: from theory to practice. Qual Res Psychol. 2015;12(2):125-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. SAGE Publications; 2014. [Google Scholar]
- 21. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Transaction Publishers; 2009. [Google Scholar]
- 22. Hamilton JB. Rigor in qualitative methods: an evaluation of strategies among underrepresented rural communities. Qual Health Res. 2020;30(2):196-204. doi: 10.1177/1049732319860267 [DOI] [PubMed] [Google Scholar]
- 23. Rowlands T, Waddell N, McKenna B. Are we there yet? A technique to determine theoretical saturation. J Comput Inf Syst. 2016;56(1):40-47. [Google Scholar]
- 24. Denzin N. Sociological Methods: A Sourcebook. Aldine; 1970. [Google Scholar]
- 25. Reddy S, Allan S, Coghlan S, Cooper P. A governance model for the application of AI in health care. J Am Med Inform Assoc. 2020;27(3):491-497. doi: 10.1093/jamia/ocz192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yang Z, Dai Z, Yang Y, Carbonell J, Salakhutdinov RR, Le QV. XLNet: generalized autoregressive pretraining for language understanding. In: Wallach H, Larochelle H, Beygelzimer A, Alché-Buc F d’, Fox E, Garnett R, eds. Advances in Neural Information Processing Systems. Vol. 32. Curran Associates, Inc.; 2019. https://proceedings.neurips.cc/paper/2019/file/dc6a7e655d7e5840e66733e9ee67cc69-Paper.pdf [Google Scholar]
- 27. Wang Y, Afzal N, Fu S, et al. MedSTS: a resource for clinical semantic textual similarity. Lang Resour Eval. 2020;54(1):57-72. doi: 10.1007/s10579-018-9431-1 [DOI] [Google Scholar]
- 28. Borenstein J, Howard A. Emerging challenges in AI and the need for AI ethics education. AI Ethics. 2021;1(1):61-65. doi: 10.1007/s43681-020-00002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nissen HA, Evald MR, Clarke AH. Firms’ reshaping of commercialization practices to overcome the ‘not invented here’ phenomenon in public healthcare organizations. Innov J. 2015;20(3):1-27. [Google Scholar]