Abstract
Objective
To quantify the environmental impact of personal protective equipment (PPE) distributed for use by the health and social care system to control the spread of SARS-CoV-2 in England, and model strategies for mitigating the environmental impact.
Design
Life cycle assessment was used to determine environmental impacts of PPE distributed to health and social care in England during the first six months of the COVID-19 pandemic. The base scenario assumed all products were single-use and disposed of via clinical waste. Scenario modelling was used to determine the effect of environmental mitigation strategies: (1) eliminating international travel during supply; (2) eliminating glove use; (3) reusing gowns and face shields; and (4) maximal recycling.
Setting
Royal Sussex County Hospital, Brighton, UK.
Main outcome measures
The carbon footprint of PPE distributed during the study period totalled 106,478 tonnes CO2e, with greatest contributions from gloves, aprons, face shields and Type IIR surgical masks. The estimated damage to human health was 239 DALYs (disability-adjusted life years), impact on ecosystems was 0.47 species.year (loss of local species per year), and impact on resource depletion was costed at US $12.7m (GBP £9.3m). Scenario modelling indicated UK manufacture would have reduced the carbon footprint by 12%, eliminating gloves by 45%, reusing gowns and gloves by 10% and maximal recycling by 35%.
Results
A combination of strategies may have reduced the carbon footprint by 75% compared with the base scenario, and saved an estimated 183 DALYS, 0.34 species.year and US $7.4m (GBP £5.4m) due to resource depletion.
Conclusion
The environmental impact of PPE is large and could be reduced through domestic manufacture, rationalising glove use, using reusables where possible and optimising waste management.
Keywords: Environmental issues, health policy, public health
Introduction
The use of personal protective equipment (PPE) has been a central behavioural and policy response to control the spread of the SARS-CoV-2 virus during the global COVID-19 pandemic. In particular, masks, and sometimes gloves, aprons, gowns and face/eye protection, have been recommended or used in high-risk situations such as healthcare settings or enclosed public spaces. The resultant surge in demand for PPE has required an increase in PPE production, including an estimated 11% increase in global production of gloves in 2020.1
While there is evidence that PPE is effective in limiting transmission of the SARS-CoV-2 virus, the necessity and extent of PPE for use in different circumstances is still subject to debate.2 Excessive use of PPE risks generating unnecessary financial cost: for example, the UK government budgeted GBP £15bn of funds for purchasing PPE for public sector workers in 2020–2021.3 In addition, the use of PPE generates a cost to the environment (which in turn impacts on human health), but to date that risk has not been quantified.
Here, we used the approach of life cycle assessment to estimate emissions and resulting environmental impact from the most common PPE items prescribed and used in the National Health Service (NHS) and public social care sector in England: masks, gloves, aprons, gowns and face/eye protection.4 We equated this with data on the volumes of these products distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic, to estimate the overall environmental impact of PPE over this period.5 We evaluated the associated damage to human health (measured in disability-adjusted life years [DALYs]), ecosystems (loss of local species) and resource scarcity (financial cost involved in future mineral and fossil resource extraction). We model a number of approaches which could mitigate such impact, and which could inform future policy on use and supply of PPE.
Methods
Selection of representative PPE items and determination of material composition
We based our analysis on products in use at our hospital (Royal Sussex County Hospital, Brighton, UK), which is a typical acute tertiary teaching hospital, to represent commonly used PPE. Specifically, we evaluated nitrile gloves, polyethylene aprons, plastic face shields (to represent all eye/face protection), polypropylene fluid-repellent gowns, polypropylene filtering face piece (FFP) respirator masks (both cup fit and duckbill style), Type II polypropylene surgical masks and Type IIR polypropylene fluid-resistant surgical masks. Type II surgical masks were not available in our hospital setting and so an example was sourced elsewhere, with packaging assumed to be the same as the Type IIR surgical masks.
For each item, we used manufacturer information to determine the raw material composition, or expert knowledge where such information was not available. Each component of the item was weighed using Fisherbrand FPRS4202 Precision balance scales (Fisher Scientific, Loughborough, UK). We included associated primary and secondary packaging up to the packing unit supplied to the hospital.
Parameters for life cycle assessment
A life cycle assessment was conducted in accordance with International Organization for Standardization 14044 Guidelines,6 and modelled using SimaPro Version 9.10 (PRé Sustainability, Amersfort, Netherlands), with additional analysis using Microsoft Excel for Mac Version 16.25 (Microsoft Corp., Redmond, WA, USA). We performed a ‘cradle to grave’ life cycle assessment including raw material extraction, manufacture, transport and disposal (system boundary outlined in Supplementary Figure 1).
The previously determined composition and weight of materials in each item and packaging was matched with closest materials within the Ecoinvent database Version 3.6 (within SimaPro), to determine material-specific global average impacts of raw material extraction, production and transport to the ‘end user’ (in this case the manufacturer).
For manufacturing, the country of origin was modelled based on those reported by the NHS PPE Dedicated Supply Channel.7 Where a type of product was procured from more than one country, a weighted average was applied to our calculations on the assumption that equal numbers of the product were distributed from each listed supplier.7 A list of suppliers awarded UK contracts for PPE is available in a UK National Audit Office report, but this does not provide data on volumes supplied or distributed, or country of origin3 and our model was based on best available information on the country of origin of products.7 Electricity consumption during the manufacturing process was modelled on best available secondary data for comparable products,8–11 and electricity inventory processes chosen and weighted based on country of origin(s). We excluded water and fuel during manufacture because such data were not available and were unlikely to materially affect results.
For transportation, we assumed all items were shipped from the country of origin to the UK, because this method of transport was most commonly used (>80%) for PPE from new suppliers to the UK during the period included in the study.3 We included 160 km of travel by road via heavy goods vehicles both within the country of origin and in the UK, with an additional 8 km at either end of each journey via courier. All transportation distances were estimated using the online Pier2Pier tool (Supplementary Table 1).12
The processes in relation to raw material extraction, manufacture, transport and disposal selected for the life cycle assessment inventory within SimaPro are shown in Supplementary Table 2. We modelled life cycles on the basis that all items were used only once, and (in accordance with UK guidance) disposed of as clinical waste13 via high-temperature hazardous incineration.14
Impact assessment methodologies
Following the development of the life cycle assessment inventory within SimaPro, we used the ReCiPe Midpoint Hierarchist method Version 1.1 (integrated within SimaPro) to characterise emissions from the lifecycle inventory assessment and to combine these into environmental impacts. ReCiPe is a widely used impact assessment method, chosen because it considers a broad range of global environmental impacts (unlike others which are regional), and because it considers impacts at two levels; midpoint and endpoint. Eighteen midpoint impact categories (considering single environmental problems) are evaluated using this method: global warming; stratospheric ozone depletion; ionising radiation; ozone formation (on human health and terrestrial ecosystems); fine particulate matter formation; terrestrial acidification; eutrophication (freshwater and marine); ecotoxicity (terrestrial, freshwater, marine); toxicity to humans (relating to chemicals with reported carcinogenic [cancer] effects such as polyaromatic hydrocarbons and chemicals with non-carcinogenic effects [non-cancer diseases] such as lead, which is associated with learning disabilities at high blood levels), land use; resource scarcity (mineral and fossil); and water consumption. Global warming was the primary impact evaluated, with greenhouse gases summated and expressed as carbon dioxide equivalents (CO2e), providing a ‘carbon footprint’. We also aggregated midpoint impact categories to calculate endpoint factors for damage to human health, the natural environment and resource scarcity, as per the ReCiPe Endpoint Hierarchist method, Version 1.1.
We calculated environmental impact values per item, and then multiplied it by the total number of PPE items supplied to health and social care services in England between 25 February and 23 August 2020, using publicly available volumes data.5 For respirator masks, we combined volumes of FFP2 and FFP3 masks and assumed an equal split between cup fit and duckbill styles. Table 1 details extracted parameters on electricity in manufacture, and on country of origin and volumes of PPE distributed for use by health and social care services in England. We used ReCiPe Hierarchist method normalisation factors to compare our calculated total midpoint and endpoint impacts to the mean average contributions to each of those impacts from a global average person’s daily routine activities over a six-month period.
Table 1.
Model parameters for manufacture and supply of PPE items.
| Product | Manufacturing electricity (kWh/kg product) | Country of origin7 (ratio) | Number distributed February–August 20205 |
|---|---|---|---|
| Apron | 0.49010 | China, Thailand (9:1) | 441,061,000 |
| Face shield | 0.367= mean810,11 | China (1) | 45,326,000 |
| FFP respirator (any type) | 0.29611 | China, UK, France (1:1:1) | 37,212,000 |
| Gloves (single) | 2.7909 | Malaysia (1) | 1,839,235,000 |
| Single-use gown | 0.3168 | China, Egypt, Germany (9:4:3) | 5,985,000 |
| Surgical mask (Type II) | 0.29611 | China, UK, Mexico (11:2:1) | 6,623,000 |
| Surgical mask (Type IIR) | 479,341,000 | ||
| Disinfectant wipe | 0.29611 | China (1) | – |
| Reusable gown | 0.3168 | China, UK (3:1) | – |
Note: Model parameters and source of data on electricity within manufacture (not including production of material), country of origin, and number distributed to health and social care services in England (25 February–23 August 2020).
FFP: filtering facepiece; PPE, personal protective equipment.
Scenario modelling
We modelled the effect of four approaches that could mitigate the environmental impact of PPE manufacture, supply and disposal.
First, we modelled the impact of domestic (UK) manufacture of products, effectively eliminating international transport (shipping) but using the same road travel assumptions, with UK electricity grid inventory process data for manufacture.
Second, we modelled reducing glove use by replacing use of gloves (with subsequent hand washing), with hand washing alone (which can effectively destroy the virus).15 It was not necessary to calculate the environmental impact of hand washing itself, because hand washing is common to both scenarios, and so not relevant to comparative analysis.
Third, we modelled the impact of using reusable gowns and reusing face shields. Reusable gowns were assumed to be laundered and re-used 75 times before disposal (based upon direct correspondence with the manufacturer). We extracted energy, water and detergent requirements, based upon previously published studies and reports.8,16 Detergent chemical composition was included where known, and where the chemical constituted ≥1% of the detergent composition (Supplementary Table 3). The transportation of linen from the user site to a laundering facility was assumed to be 160 km (round trip) via heavy goods vehicles by road. Face shields were assumed to be reused five times, with cleaning by a disinfectant wipe between uses – an accepted practice in the UK.17 To inform this model, we calculated the environmental impacts of reusable gowns and disinfectant wipes, using the same approach detailed earlier for other PPE (except that secondary packaging of reusable gowns was excluded, as this was likely to reach the insignificance threshold of contributing <1% to the impact).18 The country of origin of the reusable gown and disinfectant wipes in use at our hospital were assumed to be representative, and determined using either the packaging or direct contact with the manufacturer.
Fourth, we modelled the environmental impact of maximal recycling of products, assuming it was possible to recycle all items and their components. We used the open-loop ‘recycled content method’, which allocates subsequent emissions and environmental impacts of the recycling process, and net reduction of virgin material acquisition, to the production of the recycled goods.18
Finally, we modelled the environmental impact of combining these mitigation measures.
We also modelled the effect of changes that could increase the environmental impact, specifically a change of overseas transportation to air freight. Air freight was employed for rapid delivery of PPE supplies to the UK early in the COVID-19 pandemic because of insufficient stock.19
Results
The composition and weight of materials for each item of PPE and associated packaging are detailed in Table 2.
Table 2.
Material composition of PPE.
| Product | Example manufacturer and model | Item |
Packaging |
|||
|---|---|---|---|---|---|---|
| Material | Weight (g) (number of uses when > 1) | Material | Weight (g) | Number of items/ package | ||
| Apron | Trans-Continental Marketing TCMAPR200W | LDPE film | 9.86 | LDPE film Corrugated cardboard | 6.36 365.67 | 200 1000 |
| Face shield | Miers Mio-shield | LDPE film Polyurethane foam Synthetic rubber | 18.53 5.44 4.95 | LDPE film Corrugated cardboard | 8.48 683.57 | 1 200 |
| FFP respirator (cup fit) | 3M FFP3 8833 | Non-woven polypropylene Melt-blown polypropylene Polypropylene injection moulded Polyurethane foam Synthetic rubber Aluminium Steel | 5.98 2.99 3.93 2.54 2.55 1.13 0.32 | Boxboard Corrugated cardboard | 88.32 350.40 | 20 120 |
| FFP respirator (duckbill) | 3M FFP3 1863 | Non-woven polypropylene Melt-blown polypropylene Polyurethane foam Synthetic rubber Steel | 5.52 2.76 0.85 0.77 0.48 | LDPE film Boxboard Corrugated cardboard | 1.25 88.32 350.40 | 1 20 120 |
| Gloves (single) | Schottlander Soft touch flexible nitrile | Synthetic rubber | 3.23 | Boxboard Corrugated cardboard | 64 382.55 | 200 1000 |
| Single-use gown | YADU Medical surgical gown reinforced | Non-woven polypropylene Synthetic rubber | 134.74 7.72 | LDPE film Paper Corrugated cardboard | 4.43 6.46 911.22 | 1 1 50 |
| Surgical mask (Type II) | Genmed Surgical face mask Type II elastic strap | Non-woven polypropylene Melt-blown polypropylene Synthetic rubber Aluminium | 1.00 0.50 0.28 0.23 | Boxboard Corrugated cardboard | 41.75 843.30 | 2000 50 |
| Surgical mask (Type IIR) | Arma Pennine Disposable medical face mask 3-ply with earloops | Non-woven polypropylene Melt-blown polypropylene Synthetic rubber Aluminium | 1.63 0.82 0.45 0.20 | Boxboard Corrugated cardboard | 41.75 843.30 | 50 2000 |
| Disinfectant wipe | Clinell Universal Wipe | Non-woven polyester Quaternary ammonium compounds and polymeric biguanide hydrochloride | 2.28 0.02* | Polypropylene, oriented film Polypropylene, injection moulding Corrugated cardboard | 13.28 10.90 406.47 | 200 200 1200 |
| Reusable gown | Elis Standard protection reusable gown | Polyester microfibre Synthetic rubber Tissue paper | 301.37(75) 18.31(75) 13.41 | LDPE film Paper | 6.42 19.90 | 1 1 |
Note: All items single-use aside from components of reusable gown.
FFP: filtering facepiece; PPE: personal protective equipment.
aAssumed proportion.
Impact assessment: The environmental impact of PPE
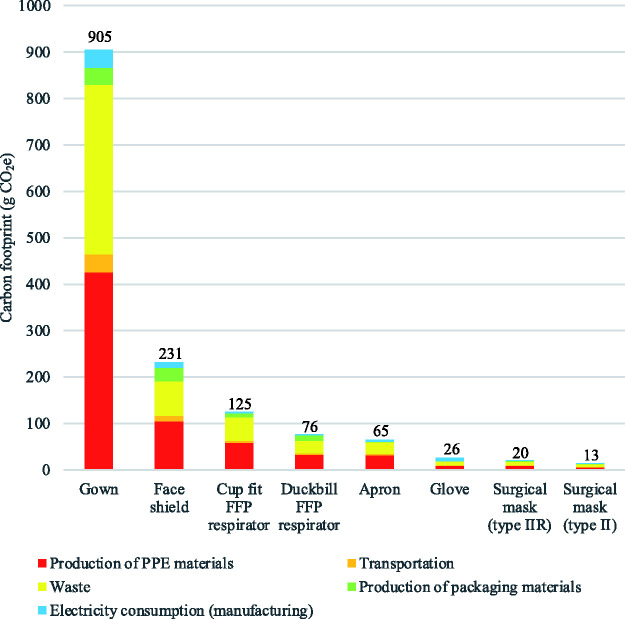
The carbon footprints of individual items were estimated as follows: single-use gowns 905 g CO2e; face shield 231 g CO2e; cup fit FFP respirator 125 g CO2e; duckbill FFP respirator 76 g CO2e; apron 65 g CO2e; single glove 26 g CO2e; Type IIR surgical mask 20 g CO2e; and Type II surgical mask 13 g CO2e. The mean contribution of production of materials to the overall carbon footprint of items was 46% (range: 35%–49%), 39% from clinical waste (range: 32%–40%), 6% from production of packaging materials (range: 0.5%–16%), 5% from electricity used within manufacturing (range: 2%–29%) and 4% from transportation (range: 3%–6%) (Figure 1). Supplementary Tables 4 to 11 show contributions per item across all environmental impacts, with further breakdown of processes. Supplementary Figures 2 to 9 provide network diagrams visualising the process drivers of global warming impact.
Figure 1.
Carbon footprint of individual PPE items. Carbon footprint of individual single-use PPE items, with breakdown of process contributions. Production of PPE materials includes the raw material extraction, production and transport to the PPE manufacturer.
CO2e: carbon dioxide equivalents; FFP: filtering facepiece; PPE, personal protective equipment.
The carbon footprint of all PPE supplied to health and social care services in England between 25 February and 23 August totalled 106,478 tonnes CO2e. This equated to 26,662 times the global average person’s carbon footprint during a six-month time period (normalised results Table 3). The proportional contribution for each type of item was primarily determined by the volumes distributed of that item, and was greatest for gloves, followed by aprons, face shields and Type IIR surgical masks. The relative impact of PPE distributed during this period on the carbon footprint and other midpoint environmental measures are detailed in Table 3. Endpoint impact results estimated that the total damage to human health during this period was 239 DALYs, equating to 20,126 times the average person’s contribution to DALYs over a similar period. The impact on ecosystems was 0.47 species.year (loss of local species per year), equivalent to 1,300 times a person’s impact in this category over the study period. The impact on resource depletion equated to US $12.7m (GBP £9.3m) involved in future mineral and fossil resource extraction, equal to 907 times a person’s average contributions to resource depletion over six months.
Table 3.
Environmental impact of PPE distributed to health and social care services in England February–August 2020. Environmental impacts (midpoint categories) measured using life cycle assessment and modelled on total volumes of core PPE distributed to health and social care services in England between 25 February and 23 August 2020.
| Impact category | Unit | Apron | Face shield | FFP respirator | Gloves | Gown | Surgical mask (Type II) | Surgical mask (Type IIR) | Total (Normalised results: 6 months) |
|---|---|---|---|---|---|---|---|---|---|
| Global warming | kg CO2e | 28,792,521 | 10,487,030 | 3,749,353 | 48,261,870 | 5,419,004 | 89,353 | 9,678,860 | 106,477,990 (26,662) |
| Stratospheric ozone depletion | kg CFC11 eq | 9 | 3 | 1 | 21 | 2 | 0 | 4 | 41 (1,354) |
| Ionising radiation | kBq Co-60 eq | 1,110,473 | 373,453 | 166,612 | 1,635,054 | 206,718 | 3,608 | 386,809 | 3,882,727 (16,152) |
| Ozone formation, Human health | kg NOx eq | 69,028 | 26,751 | 8445 | 103,536 | 12,212 | 233 | 24,148 | 244,353 (23,751) |
| Fine particulate matter formation | kg PM2.5 eq | 35,895 | 13,990 | 4664 | 83,617 | 6569 | 123 | 12,839 | 157,696 (12,332) |
| Ozone formation, Terrestrial ecosystems | kg NOx eq | 72,203 | 27,939 | 8726 | 108,003 | 12,611 | 239 | 24,863 | 254,584 (28,666) |
| Terrestrial acidification | kg SO2 eq | 86,847 | 34,296 | 11,342 | 161,236 | 15,825 | 298 | 31,178 | 341,022 (16,642) |
| Freshwater eutrophication | kg P eq | 8446 | 2791 | 1052 | 16,963 | 1627 | 27 | 2882 | 33,786 (104,062) |
| Marine eutrophication | kg N eq | 770 | 509 | 164 | 1179 | 135 | 3 | 258 | 3017 (1310) |
| Terrestrial ecotoxicity | kg 1,4-DCB | 51,133,924 | 19,578,216 | 7,632,980 | 100,702,920 | 11,071,880 | 195,488 | 20,672,169 | 210,987,577 (407,206) |
| Freshwater ecotoxicity | kg 1,4-DCB | 759,210 | 286,495 | 110,292 | 1,730,262 | 168,812 | 2782 | 303,240 | 3,361,094 (5,478,583) |
| Marine ecotoxicity | kg 1,4-DCB | 1,011,748 | 381,554 | 146,223 | 2,308,253 | 222,862 | 3686 | 401,385 | 4,475,710 (8,673,927) |
| Human carcinogenic toxicity | kg 1,4-DCB | 1,735,767 | 582,944 | 228,986 | 2,860,153 | 336,096 | 5431 | 595,737 | 6,345,112 (4,581,171) |
| Human non-carcinogenic toxicity | kg 1,4-DCB | 17,603,872 | 6,489,782 | 2,396,602 | 42,327,720 | 3,491,487 | 60,950 | 6,533,952 | 78,904,366 (1,058,897) |
| Land use | m2a crop eq | 635,797 | 239,803 | 157,939 | 1,070,855 | 145,353 | 4681 | 379,597 | 2,634,025 (853) |
| Mineral resource scarcity | kg Cu eq | 44,167 | 33,459 | 11,536 | 528,975 | 13,753 | 315 | 34,988 | 667,193 (11) |
| Fossil resource scarcity | kg oil eq | 10,131,513 | 3,790,965 | 1,290,985 | 15,959,889 | 2,007,022 | 30,317 | 3,382,452 | 36,593,143 (74,650) |
| Water consumption | m3 | 285,962 | 122,024 | 32,176 | 427,167 | 37,714 | 633 | 67,654 | 973,331 (7,300) |
Normalised results: environmental impact relative to the global average person’s contribution to the impact category over six months. For example, a normalised figure of 26,662 for the global warming category indicates that the greenhouse gas emissions relating to the total volume of PPE supplied during the study period equates to the total amount of greenhouse gases expected to be generated by the activities of 26,662 average people over the course of six months.
FFP: filtering facepiece; 1,4-DCB: dichlorobenzene; CFC11: trichlorofluoromethane; CO2e: carbon dioxide equivalents; Cu: copper; eq: equivalents; kBq Co-60 eq: kilobecquerel Cobalt-60; m2a: square meter years, N: nitrogen, NOx: nitrous oxides; P: phosphate; PM2.5: particulate matter < 2.5 micrometers; PPE: personal protective equipment; SO2: sulphur dioxide.
Scenario analysis: Mitigating the environmental impact of PPE
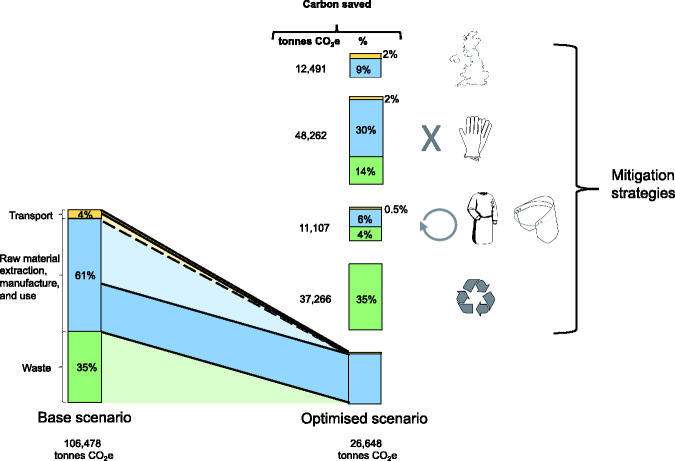
The carbon footprint of PPE was reduced by 12% through manufacturing PPE in the UK, saving 12,491 tonnes CO2e over the six-month study period. Reductions were due to the elimination of overseas travel (2.4%), alongside use of UK electricity (9.3%) (which has a higher proportion of renewables compared with the majority of countries of origin assumed in the base scenario).
Eliminating glove use would have reduced the carbon footprint by 45%, saving 48,262 tonnes CO2e over six months.
For reuse, the environmental impact of one use of a reusable gown was lower than that of a single-use gown across 16/18 environmental midpoint impact categories (with impact reductions of 17% to 86%) (Supplementary Figure 10). The impact of reusable gowns on marine eutrophication was 47% greater than single-use gowns, with 72% of this impact from wastewater generated during the laundering process (Supplementary Figure 11). The impact of reusable gowns on land use was more than double that of single-use gowns, with 86% of this effect due to single-use paper within the associated hand-towel and packaging (Supplementary Figure 12). Reusing face shields five times with disinfectant wipe between use showed 57% to 73% lower impact across all midpoint categories, when compared with single use (Supplementary Figure 13). Opting for reusable gowns and reusing face masks could have saved 11,107 tonnes of CO2e over the study period (10% of the total for all PPE distributed).
Maximal recycling reduced the carbon footprint of PPE by 35% (saving 37,266 tonnes CO2e).
A combination of UK manufacturing, eliminating glove use, reuse of gowns and face shields, and maximal recycling could have led to a 75% reduction (saving 79,830 tonnes CO2e) (Figure 2). Results of other midpoint impact categories are detailed in Supplementary Table 12.
Figure 2.
Mitigating the carbon footprint of personal protective equipment (PPE). Bar graph to left demonstrates the carbon footprint of the base scenario PPE use (modelled on total volumes of core PPE distributed to health and social care services in England between 25 February and 23 August 2020, and assuming shipping, single-use PPE and clinical waste), totaling 106,478 tonnes CO2e (carbon dioxide equivalents). Bar graph to right at base demonstrates mitigation of the carbon footprint (modelled through combining scenarios), totaling 26,648 tonnes CO2e. Bar graphs stacked above optimised scenario demonstrate the carbon savings from each mitigation strategy (reported in tonnes and as a percentage, compared with the base scenario). Scenarios from top to bottom: UK manufacture, eliminating glove use, reuse of gowns and face shields, recycling.
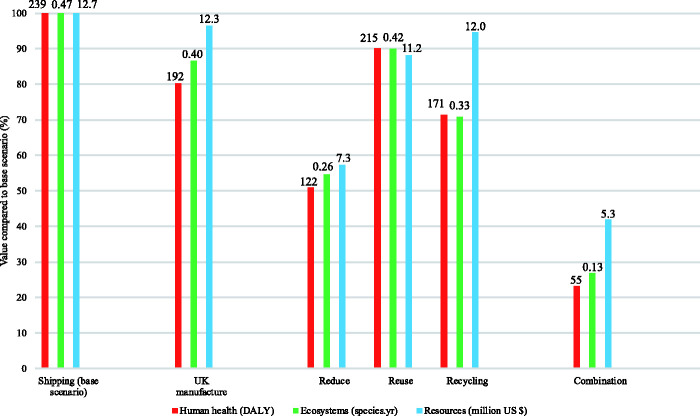
Endpoint category scenario modelling showed a similar pattern, with largest reductions seen through eliminating glove use (Figure 3, Supplementary Table 13). Maximum reductions through a combination of UK manufacture, eliminating glove use, reusable gowns and face shields, and maximal recycling would have saved an estimated 183 DALYS, 0.34 species.year, and US $7.4m (GBP £5.4m) due to resource depletion.
Figure 3.
Environmental impacts of alternative scenarios. Environmental impacts (endpoint categories) of alternative scenarios, modelled on total volumes of core personal protective equipment (PPE) distributed to health and social care services in England between 25 February and 23 August 2020, normalised to highest scenario for each impact factor, modelling base scenario (shipping, single-use PPE, clinical waste), use of UK manufacture, shipping, reduce (zero glove use), reuse (reusable gown, reuse of face shield, all other items single-use), recycling and combination of measures. Data labels above bars relate to absolute values, measured in disability-adjusted life years (DALYs), loss of local species per year (species.year) and extra costs involved for future mineral and fossil resource extraction (US $).
The effect of air freight on environmental impact
Use of air freight in place of shipping increased the carbon footprint of PPE by 50%. This would have increased the carbon footprint by 52,360 tonnes CO2e over the six-month study period, and resulted in an additional 75 DALYS, 0.20 species.year and US $7.7m (GBP £5.6m) due to resource depletion (compared with base scenario).
Discussion
We estimate the carbon footprint of PPE distributed for use by health and social care services in England during the first six months of the COVID-19 pandemic to be 106,478 tonnes CO2e, which is equivalent to 0.8% of the entire carbon footprint of health and social care in England during six months of normal activity (estimated at 27 million tonnes CO2e per annum in 2018).20 Per day, this equates to a mean of 591 tonnes CO2e, equivalent to 27,000 times the average individual’s carbon footprint, or around 244 return flights from London to New York.21
There are some caveats in the interpretation of these data. Around three billion items of PPE were used in the six-month period analysed, but data from 2019 (prior to the pandemic) suggest that around 1.2 billion items would normally be consumed in the NHS in a six-month period5; hence, the excess in this period was in fact 1.8 billion items. However, 70%–80% of elective care in the NHS stopped during the first few months of the pandemic, and emergency attendances decreased by 30%–40%,22 meaning PPE use related to normal (non-pandemic) NHS activity would have fallen by a comparable amount. The backlog of pending elective activity means that the PPE required to deliver elective care has been deferred rather than abolished, and as elective activity resumes, current requirements for enhanced protection mean that use of PPE will likely be even higher than before.
The large environmental impact of PPE, and the probability that we will continue to require and use high volumes of PPE for the foreseeable future, demands an urgent evaluation of approaches to reduce this impact.
Opportunities to mitigate the environmental harm of PPE
Strategies to mitigate environmental impact are often based on principles of reduce, reuse and recycle, and we believe this approach can also be applied to PPE, and without compromising safety.
In healthcare settings in England, the policy at the time of the study period mandated the use of gloves for close patient contact,4 although transmission of coronavirus is thought to occur mostly via airborne spread rather than direct transfer.23 Hand washing can destroy the SARS-CoV-2 virus,15 so may negate the need to wear gloves. In our six-month analysis period, nearly 1.8 billion gloves were distributed to health and social care services, and these volumes increased in July and August 20205 despite a reduction in the number of COVID-19 cases in the same time period. Gloves accounted for 45% of the total carbon footprint of PPE in our study, so a policy to rationalise glove use could have a large impact on environmental harm. Furthermore, aprons accounted for 27% of the carbon footprint of PPE, and there may be parallel opportunities for policy change to reduce use of aprons, again without compromising safety. Current UK guidance advises that gloves and aprons are no longer required where contact with patients is minimal, although the existence of contradictory local policy documents24 suggests that these may not have been universally adopted. The UK government also supports reducing glove use because of their association with contact dermatitis among healthcare staff.25
Where PPE is required, our data suggest use of domestic manufacture could reduce associated carbon footprint by 12%. Domestic PPE manufacture has been used in many countries in response to PPE shortages, including Germany, where the government introduced a scheme to support German manufacture of facemasks.26 The UK government has released a policy seeking to develop and maintain a domestic manufacturing base to improve resilience,3 with the ambition that this will meet the majority (70%) of PPE demands, although this target excludes gloves which are responsible for a large proportion of PPE.25 The policy also includes adequate stockpiling of PPE, and this, together with domestic manufacture, will mitigate the need to urgently air freight PPE from abroad with the associated 50% increase in carbon footprint.
Reuse of PPE is also feasible, and practised in some settings. Extended use of masks is supported by several guidelines27 and should be encouraged to reduce environmental impact. Reprocessing by sterilisation through chemical or physical means has also been explored,28 although not widely implemented. For users who wear a mask often, reusable passive or powered air purifiers may have a lower overall carbon footprint, although that was not formally evaluated here. Face shields are already reused in many settings, and our analysis suggests that cleaning with disinfectant wipes and reusing five times lowers carbon footprint by 70% compared to single use. Reusable gowns are already available and utilised in operating theatres, and we found use of reusable rather than disposable gowns would reduce carbon footprint by two-thirds (consistent with calculations by other authors).8 To provide reusable gowns to ward or outpatient settings would need an increase in stock, upscaling of laundering facilities, and ideally removal of the hand towels and inner wrap typically supplied with gowns used in operating theatres. The UK government has released policy supporting manufacture of reusable PPE alternatives where possible (including eye protection and gowns), and reprocessing of single-use PPE in emergency circumstances (for example moist heat treatment or hydrogen peroxide vapour for FFP3 masks).25
Maximal recycling reduced carbon footprint by 35% but is unrealistic because adequate infrastructure for waste segregation does not currently exist, particularly for multi-component products such as masks (which would require disassembly of potentially infected materials). However, if PPE in the NHS was disposed of via infectious waste streams rather than clinical waste streams (where it may be decontaminated prior to disposal through recycling, landfill or low temperature incineration with energy from waste),14 then the carbon footprint of disposal could be at least halved.29 A recent life cycle assessment study modelled alternative disposal of PPE, finding that decentralised (local) incineration was preferrable to centralised incineration or landfill across all environmental impacts assessed, and opportunities to reduce transportation of waste to such facilities should be explored.30
We recognise that a complete implementation of these strategies is not possible or practical, but the models we provide do suggest where policy changes could have impact. The extent to which each of the environmental mitigation strategies can be implemented in practice will be dynamically dependant on multiple factors including industry response to the call for greater domestic manufacture of PPE, availability of local facilities for recycling and local policies and attitudes. This warrants closer examination, but is beyond the scope of this paper.
Limitations to our dataset
Our calculations are based on a number of assumptions. We calculated the environmental impact on a single typical model of each type of PPE, but there will be other models and brands, with differences in environmental harm. However, the differences are likely small and unlikely to make substantive changes to the estimates of total environmental impact of the PPE distributed, relative contributions from different product types, or magnitude of mitigation strategies. We assumed all waste was disposed of via clinical waste as recommended, but in reality some PPE incorrectly enters other hospital waste streams (which have a lower environmental impact). We assumed shipping for all PPE from outside the UK, but we only included a single direction of transport via shipping and some PPE may have been transported via other means.
The actual quantity (and so carbon footprint) of PPE used in health organisations in England during the pandemic is larger than we have included here. Our estimates do not include PPE procured outside of the government dedicated supply channel, including gloves or gowns for use in the operating theatre (which are procured through different channels), or PPE procured by private organisations. We found no publicly available data on PPE procured in other countries, although one supplier in the USA (Project N95) records over two million items of PPE supplied over six months from mid-May to November 2020.31
Looking beyond our dataset
Outside of the healthcare setting, other organisations and individuals will procure PPE, particularly following policy in countries such as the UK for the use of masks when indoors.32 In our data, the majority of PPE was manufactured partially or completely from plastics or petroleum-based synthetic rubbers, including for example nitrile for gloves, polypropylene for masks and gowns, and polyethylene for visors and aprons, which we estimated to have a mass of over 14,000 tonnes over the six-month period. Disposal of PPE outside of healthcare will mostly be in domestic waste streams which may enter landfill, risking plastic pollution. Discarded masks and gloves have been found polluting oceans.33
We are also aware of social (alongside environmental) harms from PPE. There have been longstanding concerns about abuse of workers manufacturing masks and gloves,34 and such concerns have continued or been exacerbated in recent months, with reports of forced labour to make masks in China,35 and abuse of migrant workers in factories producing gloves in Malaysia.36
Conclusion
The environmental impact of PPE is substantial and requires urgent review to mitigate effects on planetary health. The most opportune and impactful strategies may be through reduced use of gloves by using hand washing alone, domestic manufacture of PPE and extended use or reuse of PPE such as masks and gowns. These possibilities warrant further investigation and analysis of feasibility and safety, as well as engagement of policy makers around the globe.
Supplemental Material
Supplemental material, sj-pdf-1-jrs-10.1177_01410768211001583 for Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic by Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta in Journal of the Royal Society of Medicine
Supplemental material, sj-pdf-2-jrs-10.1177_01410768211001583 for Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic by Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta in Journal of the Royal Society of Medicine
Acknowledgements
None to declare.
Declarations:
Competing Interests: None declared.
Funding: None declared.
Ethics approval: Not required – this study did not involve any patients or healthcare staff.
Guarantor: CR.
Contributorship: CR led on life cycle assessment study design and analysis, and co-authored the first draft of the manuscript. MB initiated the article, sourced sample PPE materials, and co-authored the first draft of the manuscript. MR provided critical input to structure and content. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Provenance: Not commissioned; peer reviewed by Brett Duane, Wallace Hayes, and Julie Morris.
ORCID iDs
Chantelle Rizan https://orcid.org/0000-0002-9518-2948
Malcolm Reed https://orcid.org/0000-0001-7442-2132
References
- 1.Reuters. Top supplier Malaysia sees no quick end to shortages in $8 billion gloves Industry. See https://www.reuters.com/article/us-health-coronavirus-malaysia-gloves/top-supplier-malaysia-sees-no-quick-end-to-shortages-in-8-billion-gloves-industry-idUSKBN23B105 (2020, last checked 13 August 2020).
- 2.Karlsson U, Fraenkel CJ. Complete protection from covid-19 is possible for health workers. BMJ 2020; 370: m2641–m2641. [DOI] [PubMed] [Google Scholar]
- 3.UK Government Department of Health and Social Care. The supply of personal protective equipment (PPE) during the COVID-19 pandemic. See https://www.nao.org.uk/report/supplying-the-nhs-and-adult-social-care-sector-with-personal-protective-equipment-ppe/ (2020, last checked 3 December 2020).
- 4.Public Health England. Recommended PPE for healthcare workers by secondary care inpatient clinical setting, NHS and independent sector. See. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/886707/T1_poster_Recommended_PPE_for_healthcare_workers_by_secondary_care_clinical_context.pdf (2020, last checked 13 August 2020).
- 5.Department of Health and Social Care. Experimental statistics – personal protective equipment distributed for use by health and social care services in England: 25 Feb to 23 Aug 2020. See https://www.gov.uk/government/publications/ppe-deliveries-england-17-august-to-23-august-2020/experimental-statistics-personal-protective-equipment-distributed-for-use-by-health-and-social- care-services-in-england-17-august-to-23-august-202 (2020, last checked 2 September 2020).
- 6.International Standards Organisation. ISO 14044 Environmental management- Life cycle assessment- requirements and guidelines. See https://www.iso.org/standard/38498.html (2006, last checked 8 September 2020).
- 7.PPE Dedicated Supply Channel. PPE product listing. See https://www.ppe-dedicated-supply-channel.co.uk/ppe-product-listing/ (2020, last checked 13 August 2020).
- 8.Carre A. Life Cycle Assessment Comparing Laundered Surgical Gowns with Polypropylene Based Disposable Gowns, Melbourne, Australia: RMIT University, 2008. [Google Scholar]
- 9.Poh GKX, Chew IML, Tan J. Life cycle optimization for synthetic rubber glove manufacturing. Chem Eng Technol 2019; 42: 1771–1779. [Google Scholar]
- 10.Kimmel RM, Cooksey KD, Littman A. Life Cycle Assessment of Grocery Bags in Common Use in the United States, Clemson, SC: Clemson University, 2014. [Google Scholar]
- 11.Allison AL, Ambrose-Dempster E, Aparsi TD, Bawn M, Arredondo MC, Chau C, et al. The environmental dangers of employing single-use face masks as part of a COVID-19 exit strategy. UCL Open: Environment Preprint. See https://ucl.scienceopen.com/document?vid=6290e0d8-ff01-4c3e-9397-536b76481c50 (2020, last checked Aug 13 2020).
- 12.Pier2Pier. Pier2Pier. See http://www.pier2pier.com/Co2/ (2020, last checked 13 August 2020).
- 13.Public Health England. COVID-19 personal protective equipment (PPE). See https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe#ppe-guidance-by-healthcare-context (2020, last checked 13 August 2020).
- 14.Department of Health. Environment and sustainability health technical memorandum 07-01: safe management of healthcare waste. See https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data /file/167976/HTM_07-01_Final.pdf (2013, last checked 13 August 2020).
- 15.World Health Organization. Coronavirus disease (COVID-19) advice for the public. See https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (2020, last checked 2 September 2020).
- 16.Vozzola E, Overcash M, Griffing E. Environmental considerations in the selection of isolation gowns: a life cycle assessment of reusable and disposable alternatives. Am J Infect Control 2018; 46: 881–886. [DOI] [PubMed] [Google Scholar]
- 17.Manchester Foundation Trust Infection Prevention Control Team. SOP Decontamination of disposable visors/goggles V3.0. See https://www.pat.nhs.uk/Coronavirus/North%20Manchester/SOP%20decontamination%20of%20visors%20and%20goggles.pdf (2020, last checked 13 August 2020).
- 18.Institute of World Resources, 2011 Greenhouse gas protocol, product life cycle accounting and reporting standard. See https://www.wri.org/publication/greenhouse-gas-protocol-product-life-cycle-accounting-and-reporting-standard (2011, last checked 27 December 2019).
- 19.NHS Supply Chain. Important COVID-19 Supplier Updates London, UK: NHS Supply Chain. See https://www.supplychain.nhs.uk/suppliers/ (2020, last checked 13 August 2020).
- 20.Sustainable Development Unit. Reducing the Use of Natural Resources in Health and Social Care. See https://www.sduhealth.org.uk/policy-strategy/reporting/natural-resource-footprint-2018.aspx (2018, last checked 13 August 2020).
- 21.Department for Environment, Food and Rural Affairs/Department for Business, Energy & Industrial Strategy. UK Government GHG Conversion Factors for Company Reporting. See https://www.gov.uk/government/publications/greenhouse-gas-reporting-conversion-factors-2019 (2019, last checked 13 August 2020).
- 22.British Medical Association. Pressure Points in the NHS. See https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressure-points-in-the-nhs (2020, last checked 2 September 2020).
- 23.Zhang R, Li Y, Zhang AL, et al. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci USA 2020; 117: 14857–14863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Public Health England. COVID-19: Guidance for the Remobilisation of Services Within Health and Care Settings. See https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/910885/COVID-19_Infection_prevention_and_control_guidance_FINAL_PDF_20082020.pdf (2020, last checked 18 November 2020).
- 25.UK Department of Health and Social Care. Personal Protective Equipment (PPE) Strategy: Stabilise and Build Resilience. See https://www.gov.uk/government/publications/personal-protective-equipment-ppe-strategy-stabilise-and-build-resilience/personal-protective-equipment-ppe-strategy-stabilise-and-build-resilience (2020, last checked 3 December 2020).
- 26.Wilson A. Robust Response to PPE Shortages in Germany. See https://www.innovationintextiles.com/robust-response-to-ppe-shortages-in-germany/ (2020, last checked 7 September 2020).
- 27.Toomey E, Conway Y, Burton C, Smith S, Smalle M, Chan XH, et al. Extended use or re-use of single-use surgical masks and filtering facepiece respirators: a rapid evidence review. Centre for Evidence Based Medicine. See https://www.cebm.net/covid-19/extended-use-or-re-use-of-single-use-surgical-masks-and-filtering-facepiece-respirators-a-rapid-evidence-review/ (2020, last checked 2 September 2020).
- 28.Rodriguez-Martinez CE, Sossa-Briceño MP and Cortés JA. Decontamination and reuse of N95 filtering facemask respirators: a systematic review of the literature. Am J Infect Control 2020; 48: 1520–1532. [DOI] [PMC free article] [PubMed]
- 29.Rizan C, Bhutta M, Reed M, Lillywhite R. The carbon footprint of waste streams in a UK hospital. J Clean Prod 2020; 286: 125446–125446. [Google Scholar]
- 30.Kumar H, Azad A, Gupta A, Sharma J, Bherwani H, Labhsetwar KN, et al. COVID-19 Creating another problem? Sustainable solution for PPE disposal through LCA approach. Environment, Development and Sustainability. (epub ahead of print). https://link.springer.com/article/10.1007/s10668-020-01033-0 (2020, last checked 18 November 2020). [DOI] [PMC free article] [PubMed]
- 31.Project N95. Project N95. See https://www.projectn95.org (2020, last checked 2 September 2020).
- 32.UK Department of Health and Social Care. Face Coverings: When to Wear One and How to Make Your Own. See https://www.gov.uk/government/publications/face-coverings-when-to-wear-one-and-how-to-make-your-own/face-coverings-when-to-wear-one-and-how-to-make-your-own (2020, last checked 2 September 2020).
- 33.Kassam A. ‘More masks than jellyfish': Coronavirus Waste Ends up in Ocean: The Guardian. See https://www.theguardian.com/environment/2020/jun/08/more-masks-than-jellyfish-coronavirus-waste-ends-up-in-ocean (2020, last checked 2 September 2020).
- 34.Bhutta MF. Time for a global response to labour rights violations in the manufacture of health-care goods. Bull World Health Organ 2017; 95:314-A. [DOI] [PMC free article] [PubMed]
- 35.Xiao M, Willis H, Koettl, et al. China Is Using Uighur Labor to Produce Face Masks. New York Times. See https://www.nytimes.com/2020/07/19/world/asia/china-mask-forced-labor.html (2020, last checked 7 September 2020).
- 36.Miller J. Revealed: Shocking conditions in PPE factories supplying UK. Channel 4. See https://www.channel4.com/news/revealed-shocking-conditions-in-ppe-factories-supplying-uk (2020, last checked 2 September 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jrs-10.1177_01410768211001583 for Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic by Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta in Journal of the Royal Society of Medicine
Supplemental material, sj-pdf-2-jrs-10.1177_01410768211001583 for Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic by Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta in Journal of the Royal Society of Medicine