Abstract
Evidence is still limited for the role of long-term PM2.5 exposure in cerebrovascular diseases among residents in high pollution regions. The study is aimed to investigate the long-term effects of PM2.5 exposure on stroke mortality, and further explore the effect modification of temperature variation on the PM2.5-mortality association in northern China. Based on a cohort data with an average follow-up of 9.8 years among 38,435 urban adults, high-resolution estimates of PM2.5 derived from a satellite-based model were assigned to each participant. A Cox regression model with time-varying exposures and strata of geographic regions was employed to assess the risks of stroke mortality associated with PM2.5, after adjusting for individual risk factors. The cross-product term of PM2.5 exposure and annual temperature range was further added into the regression model to test whether the long-term temperature variation would modify the association of PM2.5 with stroke mortality. Among the study participants, the annual mean level of PM2.5 concentration was 66.3 μg/m3 ranging from 39.0 μg/m3 to 100.6 μg/m3. For each 10 μg/m3 increment in PM2.5, the hazard ratio (HR) was 1.31 (95% CI: 1.04–1.65) for stroke mortality after multivariable adjustment. In addition, the HRs of PM2.5 decreased gradually as the increase of annual temperature range with the HRs of 1.95 (95% CI: 1.36–2.81), 1.53 (95% CI: 1.06–2.22), and 1.11 (95% CI: 0.75–1.63) in the low, middle, and high group of annual temperature range, respectively. The findings provided further evidence of long-term PM2.5 exposure on stroke mortality in high-exposure settings such as northern China, and also highlighted the view that assessing the adverse health effects of air pollution might not ignore the role of temperature variations in the context of climate change.
Keywords: Satellite-based model, Population-based cohort, Stroke mortality, Long-term exposure, Temperature variation
1. Introduction
Stroke is one of great threats to global health, contributing to approximate 6.2 million deaths worldwide and 2.1 million deaths in China (GBD 2017 Causes of Death Collaborators, 2018; Institute for Health Metrics and Evaluation, 2020). Also the modifiable risk factors such as hypertension, obesity and physical inactivity, which were closely related to risk of stroke, have not been well controlled during the past decades (GBD 2015 Risk Factors Collaborators, 2016). In addition to these well-known risk factors, increasing observational and experimental studies found that pollution of fine particulate matter (particulate matter with aerodynamic diameter ≤ 2.5 μm, PM2.5) might serve as a novel risk factor for stroke and other cardiovascular diseases (Brook et al., 2010; Rajagopalan et al., 2018). Most of population-based studies documented risks of hospital admission or mortality of stroke associated with short-term ambient PM2.5 exposure (Tian et al., 2018, 2019b; Shah et al., 2015). However, the evidence on cerebrovascular damage linked to long-term PM2.5 exposure was still limited. Based on the literature review of two meta-analysis studies (Yuan et al., 2019; Chen and Hoek, 2020), six epidemiology studies were conducted in Asian regions, and others mainly derived from European and North American countries where annual concentrations of ambient PM2.5 were usually not over 35 μg/m3 (Yuan et al., 2019; Chen and Hoek, 2020). Considering the uncertainties and heterogeneities of current findings (Yuan et al., 2019; Chen and Hoek, 2020), the exposure-response relationships derived from studies with relatively low levels of PM2.5 might not directly extended to those in high pollution regions. In addition, several studies conducted in the concentration range of 50–100 μg/m3 showed inconsistent results between long-term PM2.5 exposure and stroke risks (Huang et al., 2019; Chen et al., 2019; Yang et al., 2018). Thus research evidence focusing on the chronic effect of PM2.5 exposure on stroke need further accumulated, especially among people living in high pollution settings, which is important to obtain accurate estimations in cerebrovascular disease burden attributable to global exposure range of PM2.5.
In China, ambient air pollution has emerged as one of top risk factors contributing to cardiovascular disease burdens in 2017 (Institute for Health Metrics and Evaluation, 2020). Recently, two studies in mainland China observed long-term exposure to PM2.5 significantly associated with incidence and/or mortality of stroke (Huang et al., 2019; Chen et al., 2019), although one of the studies was conducted among ischemic stroke patients with only 1-year follow-up (Chen et al., 2019). Another publication conducted in Hong Kong, China, reported non-significant association of long-term PM2.5 exposure with cerebrovascular mortality in an elderly cohort (Yang et al., 2018). To illustrate the PM2.5-stroke relationship accurately, these research evidence still need validated independently from longitudinal cohort data with wide range of PM2.5 exposure. In addition, a few studies illustrated that effects of short-term PM2.5 exposure on cardiovascular events could be modified by ambient temperature (Chen et al., 2018; Qian et al., 2008; Yitshak-Sade et al., 2018), while two studies both reported increased effects of long-term PM2.5 pollution on natural-cause mortality were modified by an increase in annual or seasonal average temperature (Kioumourtzoglou et al., 2016; Wang et al., 2016). However, few studies have examined the role of annual temperature variation in effect modification for the association of long-term PM2.5 exposure with stroke mortality, considering potential interaction roles of air pollution and temperature.
In this study, combining the satellite-based PM2.5 exposure estimates with a cohort data among urban adults, we aimed to investigate the relationship between stroke mortality and long-term exposure to ambient PM2.5 in northern China, and examined the potential effect modification of annual temperature range in the context of global climate change.
2. Materials and methods
2.1. Study design and participants
The cohort study is proposed to investigate the relationship between long-term exposure to air pollution and health among adults who lived in northern China (Zhang et al., 2014; Chen et al., 2016; Shan et al., 2020). Details of the study population have been described in Supplemental Methods. In this study, 113 deceased participants before 2000 were excluded because the satellite-based estimation of ambient PM2.5 data in China was available after 2000. Furthermore, 506 participants with stroke or cancer at baseline were excluded, and 295 were excluded due to covariates data missing, finally leaving 38,140 participants for the analysis. A flow chart showed the inclusion and exclusion of the study population (Supplemental Fig. 1).
The study has been approved by the ethics committee of the coordinating center of Tianjin Medical University. Written informed consent was signed by each participant before surveys conducted.
2.2. Exposure and health data collection
The ambient PM2.5 levels in China were estimated using a satellite-based spatiotemporal model, and the detailed methodology of the model has been published elsewhere (Xiao et al., 2018; Liang et al., 2020b).
The demographic, socio-economic, and lifestyle information at baseline were collected by trained interviewers using standardized questionnaires. For death cases, local investigators used questionnaires to record the date, location and cause of death provided by next of kin. All mortality information was also crosschecked based on death certificates from the databases in local Centers for Disease Control and Prevention (CDCs). The causes of death were coded based on the International Classification of Diseases, tenth revision (I60–I69 for stroke).
Description for the features of modeling, estimations of individual exposure to ambient PM2.5, and health data collection could be found in Supplemental Methods.
2.3. Statistical analysis
Baseline characteristics of study populations were presented as percentages for categorical variables or mean ± standard derivation for continuous variables. The association between long-term exposure to PM2.5 and stroke mortality was assessed using a Cox proportional hazards model with time-varying exposure of PM2.5 on 1-year scale, considering changes of annual average PM2.5 levels during the follow-up period (Andersen and Gill, 1982). In addition, the Cox regression analysis was performed with a stratum variable of four residential cities as the indicator addressing potential variations due to geographic regions, and used time-on-study as the time scale (i.e., time since baseline to follow-up). The other covariates were included gradually in the following multi-variable adjustment models: Model 1 adjusting for age and sex; Model 2 further adjusting for education level and personal income; Model 3 additionally adjusting for BMI, smoke, drink, and exercise; and Model 4 additionally adjusting for medical history of hypertension and diabetes. The association estimate from Model 4 was reported as the main result after fully adjusting for individual cardiovascular covariates, based on recommendations from previous works (Yuan et al., 2019; Huang et al., 2019; Miller et al., 2007).
Subgroup analyses were performed based on Model 4, and stratified by age, sex, education, personal monthly income, smoking and alcohol drinking status. We further examined the multiplicative interactions of PM2.5 exposure and each characteristic factor by introducing a cross-product term in the Cox model. In addition, several sensitivity analyses were performed to test robustness of results. First, to minimize the potential bias, we excluded individuals with cardiovascular diseases at baseline, and repeated the Cox regression analysis. Second, the hazard ratios (HRs) were re-calculated after excluding participants who reported occupational exposure with particulate matter at baseline. Third, based on the Model 4, we additionally adjusted covariates of dietary frequencies, including seafood, red meat, poultry, vegetable, and fruit consumption at baseline which were classified into three groups: low (no more than once a week), moderate (two or three times per week), and high (equal to or more than four times a week).
Last, we examined whether the annual range of ambient temperature would modify the effect estimation for the association between long-term exposure to PM2.5 and stroke mortality. The annual temperature range was classified into low (24.6 °C–28.5 °C), middle (28.5 °C–30.6 °C), and high (30.6 °C–40.0 °C) groups, according to the cutoff points of tertiles. Based on the Model 4, main effects of PM2.5 and tertiles of annual temperature range were both included along with other covariates, and the multiplicative interaction term of annual PM2.5 exposure and annual temperature range was tested for the significance of effect modification.
All of the analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC) and R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria). The tests of significance were two sided with P-value < 0.05.
3. Results
3.1. Descriptive analysis of the study participants
During the average follow-up of 9.8 years, 254 deaths of stroke were observed among the eligible 38,140 Chinese participants. The study participants were on average 44.0 years of age, and 50.2% were women. In addition, over 50% and 38% of men were smokers and alcohol drinkers, respectively, which were much higher than those proportions of women. The detailed baseline characteristics of the study participants were shown in Table 1, and descriptions of city-specific characteristics in Supplemental Table 1.
Table 1.
Baseline characteristics of 38,140 participants in the cohort study.
| Characteristics | Total | Male | Female |
|---|---|---|---|
| Participants (n) | 38,140 | 18,990 | 19,150 |
| Age, y | 43.96 ± 13.68 | 43.74 ± 13.66 | 44.18 ± 13.69 |
| Education (%) | |||
| ≥ high school level | 16,434 (43.09) | 8749 (46.07) | 7685 (40.13) |
| Personal monthly income (%) | |||
| ≥ 500 Yuan | 20,927 (54.87) | 12,406 (65.33) | 8521 (44.50) |
| BMI, kg/m2 | 22.63 ± 2.95 | 22.66 ± 2.79 | 22.60 ± 3.11 |
| Physical activity (%) | 19,102 (50.08) | 9214 (48.52) | 9888 (51.63) |
| Occupational exposure (%) | 2746 (7.20) | 1694 (8.92) | 1052 (5.49) |
| Smokers (%) | 10,629 (27.87) | 9580 (50.45) | 1049 (5.48) |
| Alcohol drinkers (%) | 7718 (20.24) | 7221 (38.03) | 497 (2.60) |
| Hypertension (%) | 3942 (10.34) | 1827 (9.62) | 2115 (11.04) |
| Diabetes (%) | 1620 (4.25) | 737 (3.88) | 883 (4.61) |
3.2. Associations between long-term exposure to PM2.5 and stroke mortality
The average level of annual exposure to PM2.5 was 66.3 μg/m3 with the range from 39.0 μg/m3 to 100.6 μg/m3. The temporal trends of annual PM2.5 levels and annual temperature ranges by city and calendar year were shown in Supplemental Fig. 2. Based on the Cox regression models with various multivariable adjustments, Table 2 represented the hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the association of long-term PM2.5 exposure with stroke mortality. In the Model 4, the risk of stroke death was significantly elevated with a HR of 1.31 (95% CI, 1.04–1.65) per 10 μg/m3 increase of PM2.5 concentration after adjusting for age, sex, education level, personal income, BMI, smoke, drink, physical activity, and medical history of hypertension and diabetes at baseline. In addition, when the PM2.5 concentrations were categorized using the quartile cutoff points of 58.5 μg/m3, 63.6 μg/m3, and 75.1 μg/m3, higher risks of stroke mortality were also observed with HRs of 1.38 (95% CI, 0.91–2.10), 1.42 (95% CI, 0.96–2.10), and 1.60 (95% CI, 1.08–2.35) for the second, third, and fourth quarter group, respectively, compared with the first quarter as reference (Supplemental Table 2). The trend testing of HRs across the quarters was significant (P = 0.020).
Table 2.
Adjusted hazard ratio (95% CI) of stroke mortality associated with each 10 μg/m3 increase in PM2.5 levels.
| Items | Number | Hazard Ratio (95%CI) | p-value |
|---|---|---|---|
| Death cases of stroke | 254 | ||
| Follow-up (person-years) | 375,876 | ||
| Model 1a | 1.27 (1.01–1.60) | 0.044 | |
| Model 2b | 1.29 (1.02–1.63) | 0.031 | |
| Model 3c | 1.31 (1.04–1.64) | 0.023 | |
| Model 4d | 1.31 (1.04–1.65) | 0.020 |
Model 1: adjusted for age and sex.
Model 2: Model 1 + adjusted for education and personal monthly income (< 500 Yuan vs ≥ 500 Yuan).
Model 3: Model 2 + adjusted for BMI, smoke (yes vs no), drink (yes vs no), and physical activity (inactive vs active).
Model 4: Model 3 + adjusted for history of hypertension (yes vs no) and diabetes (yes vs no).
3.3. Subgroup and sensitivity analyses
The associations between long-term exposure to PM2.5 and stroke mortality across different subgroups were displayed stratified by age, sex and education levels in Table 3. The risk of stroke mortality linked to long-term PM2.5 exposure seemed higher among elder, women, and people with low level of education. The estimates of HRs were similar among other subgroups categorized by personal income, smoking, and alcohol drinking. However, we did not observed significant interactions between PM2.5 exposure and those individual factors of demographic or behavior characteristics (P-value for interaction ≥0.05).
Table 3.
Subgroup analyses for hazard ratios (95% CIs) of stroke mortality associated with each 10 μg/m3 increase in PM2.5 levels.
| Subgroup | No. of deaths | Person-years of follow-up | Hazard ratio (95%CI)a | p-value for interaction |
|---|---|---|---|---|
| Age | ||||
| < 65 | 101 | 339,598 | 1.00 (0.68–1.47) | |
| ≥ 65 | 153 | 35,750 | 1.58 (1.17–2.13) | 0.716 |
| Sex | ||||
| Men | 163 | 186,434 | 1.24 (0.93–1.66) | |
| Women | 91 | 189,442 | 1.48 (1.01–2.19) | 0.143 |
| Education | ||||
| < high school level | 209 | 212,962 | 1.36 (1.05–1.75) | |
| ≥ high school level | 45 | 162,913 | 1.18 (0.68–2.05) | 0.639 |
Covariates in the multivariable-adjusted models included age, sex, education, personal monthly income, BMI, smoke, alcohol drink, physical activity, history of hypertension and diabetes.
In the sensitivity analysis, the HRs for the PM2.5-stroke mortality associations were 1.29 (95%CI, 1.02–1.64) and 1.32 (95%CI, 1.04–1.68) after removing participants with cardiovascular disease at baseline and those with self-reported occupational particulate exposure, respectively (Table 4). When dietary factors were further adjusted in the multivariate regression model (Model 5), the result kept consistent with the main analysis (Model 4). Moreover, we removed the strata of cities and directly added an indicator variable of four residential cities as a covariate into the Cox model, which showed little change with HR of 1.31 (95%CI, 1.04–1.65). In addition, residents within the same neighborhoods may share similar socioeconomic status and environmental factors. Thus, we used a shared frailty model by which cluster effect of residential neighborhoods were incorporated into the Cox regression analysis, and the HR of association was 1.31 (95%CI, 1.04–1.66) which was close to the main result. Overall, the results of sensitivity analyses did not show substantial changes in association estimations of long-term PM2.5 exposure with stroke mortality.
Table 4.
Sensitivity analyses for associations of stroke mortality with 10 μg/m3 increase in PM2.5.
| Sensitivity analysis | No. of Deaths | Person-years of follow-up | Hazard ratio (95% CI) | p-value |
|---|---|---|---|---|
| Excluding 2118 participants with CVD at baseline | ||||
| Cox Regression Model 4a | 244 | 355,178 | 1.29 (1.02–1.64) | 0.032 |
| Excluding 2746 participants with occupational particulate matter exposure at baseline | ||||
| Cox Regression Model 4a | 235 | 348,854 | 1.32 (1.04–1.68) | 0.022 |
| Adjusting for dietary factors in addition to the covariates of Model 4 | ||||
| Cox Regression Model 5b | 254 | 375,876 | 1.31 (1.04–1.66) | 0.022 |
Model 4: adjusted for age, sex, education, personal monthly income (< 500 Yuan vs ≥ 500 Yuan), BMI, smoke (yes vs no), drink (yes vs no), physical activity (inactive vs active), history of hypertension (yes vs no) and diabetes (yes vs no).
Model 5: Model 4 + dietary frequency per week (i.e., low, moderate, or high) for red meat, poultry, seafood, vegetable, and fruit.
3.4. Effect modification of annual temperature range for the association between PM2.5 and stroke mortality
The mean level for annual range of temperature exposure among the study participants were 30.4 °C (minimum to maximum: 24.6–40.0 °C). After adding the annual range of temperature as a continuous covariate into the Cox regression model, the risk of stroke mortality was still associated significantly with each 10 μg/m3 increase of PM2.5, and the HR (95% CI) slightly increased to 1.35 (95% CI, 1.04–1.77). The participants were further categorized into three subgroups according to the tertiles of annual temperature range. Fig. 1 illustrated that HRs for the associations of long-term PM2.5 exposure with stroke mortality decreased gradually as the increment of annual temperature range. The effect modification of annual temperature range was significant by testing the cross-product term of annual PM2.5 exposure and tertiles of annual temperature range (P = 0.048).
Fig. 1.
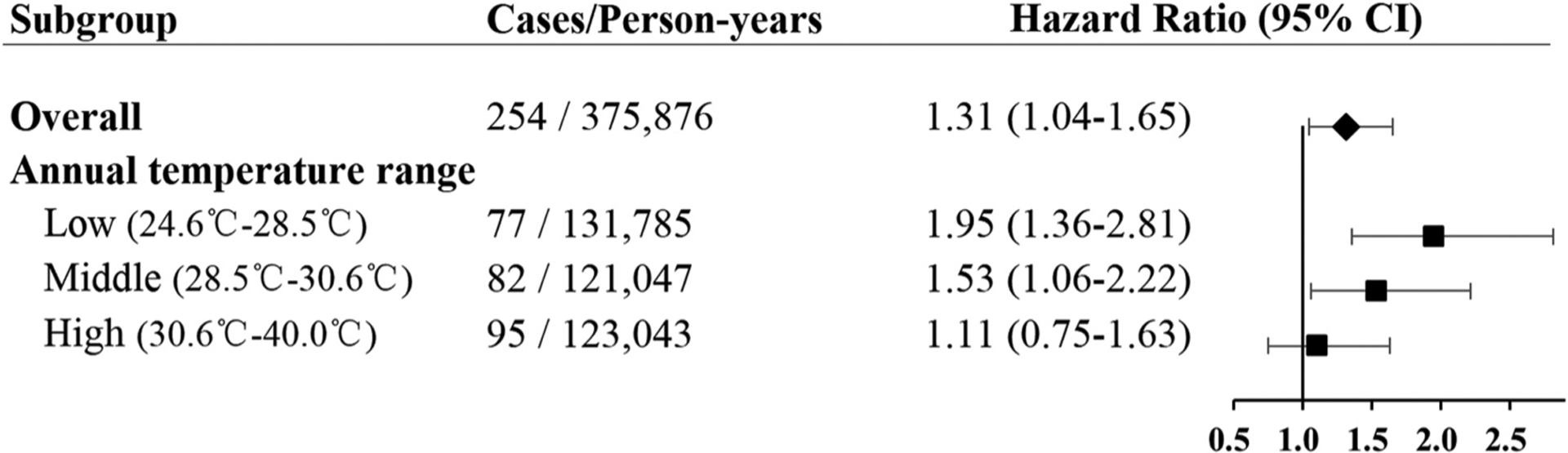
Adjusted hazard ratio (95% CI) of stroke mortality per 10 μg/m3 increase of PM2.5 across different groups of annual temperature range. The annual temperature range was classified into the Low, Middle, and High groups using tertiles as cutoff points. The rhombus and square markers represent the point estimations of hazard ratios, and the black bars represent 95% CIs.
4. Discussion
Using the cohort data collected from 2000 to 2009 among 38,140 participants, a significant association of long-term exposure to PM2.5 with stroke mortality was observed in northern China, where the urban residents had been living in high-polluted environments with the annual average level of PM2.5 ranging from 39.0 μg/m3 to 100.6 μg/m3. In addition, the study observed that the effect estimation for the PM2.5-stroke mortality association was strengthened when the annual range of ambient temperature kept at low level. These findings highlighted the importance of assessing the health effects attributable to air pollution and climate change jointly in future research works.
Air pollution has been considered as a great threat to global public health, and particulate matter pollution has exhibited extensive adverse effects to cardiovascular and cerebrovascular functions (Manisalidis et al., 2020; Burnett et al., 2018). Many studies have documented the short-term exposure to particulate matter was significantly associated with elevated risks of stroke mortality (Shah et al., 2015), but the evidence of long-term exposure to PM2.5 was still limited, especially in high pollution settings. One recent meta-analysis pooled 16 cohort studies to obtain an overall association between stroke mortality and long-term exposure to PM2.5 with the HR of 1.11(95% CI: 1.04, 1.18) per 10 μg/m3 increase of PM2.5 (Chen and Hoek, 2020). However, 13 of those studies have been conducted in North American or European countries, where the annual mean levels of PM2.5 exposure were often less than 35 μg/m3. In addition, only 5 original studies of the 16 cohorts included in the meta-analysis showed significant positive associations along with substantial heterogeneities of the pooled result (I2 = 84.7%). To the best of our knowledge, effect estimations of associations between stroke mortality and long-term exposure to PM2.5 were inadequate among populations exposed to high-polluted settings such as in mainland China. Two population-based prospective cohort studies in mainland China have examined the risks of stroke deaths associated with long-term PM2.5 exposure, the mean levels of which reached to 43.7 μg/m3 (range: 4.2 μg/m3 – 83.8 μg/m3) for the Chinese Male Cohort and 67.4 μg/m3 (range: 25.5 μg/m3–114.0 μg/m3) for the study of Prediction for Atherosclerotic Cardiovascular Disease Risk in China (China-PAR) (Liang et al., 2020a; Yin et al., 2017). The Chinese Male Cohort observed risk of stroke mortality elevated for a 10 μg/m3 increase with a HR of 1.14 (95% CI, 1.13–1.16) (Yin et al., 2017), but the study was only recruited male participants (Niu et al., 1998). The China-PAR study covered 15 provinces across China with an average follow-up of 7.6 years among 116,792 participants, which reported the HR of stroke mortality was 1.10 (95% CI, 1.05–1.18) for a 10 μg/m3 increase of PM2.5 (Liang et al., 2020a). The two works did not report the specific HRs of stroke mortality stratified by regions (northern vs southern China), while it is known that average PM2.5 concentrations were much higher in the northern than other regions in China (He et al., 2017). Our study was conducted in four northern cities of China among over 38,000 urban participants, and observed a relative higher HR of 1.31 (95% CI, 1.04–1.65) for the association of long-term PM2.5 exposure with stroke mortality. To diminish potential confounding maximally, we have adjusted demographics, BMI, smoke, drink, physical activity, and medical history in Model 4 (Table 2) and available dietary information in Model 5 (Table 4). The association results were robust in the multivariate analyses. We also used the stratified Cox regression model with a stratum variable of the four cities, which allowed us to control potential heterogeneities of study regions assuming distinct baseline hazard function for each stratum (Kleinbaum, 1996). As one of sensitivity analyses, if the variable of four cities was added as a covariate into the Cox model without the strata, the result was almost the same to the primary analysis with the HR of 1.31 (95% CI, 1.04–1.65).
In addition, after a series of sensitive analyses, the estimations for HRs seemed no substantial changes in our data (Table 4), although a slight overestimation for the association might exist considering the relatively narrow range of PM2.5 exposure (39.0 μg/m3–100.6 μg/m3) in this study, compared with aforementioned studies of the Chinese Male Cohort and the China-PAR cohort. More evidence derived from high polluted regions will be warranted in future to obtain robust estimations for the stroke mortality-PM2.5 associations.
In the subgroup analysis, we did not find significant differences in the association estimations between PM2.5 concentrations and stroke mortality stratified by either demographic factors (e.g., age and sex) or individual behavior characteristics (e.g., smoke and drink). Interestingly, it is observed that the annual temperature range significantly modified the effect of stroke mortality- PM2.5 association. Numerous studies highlighted the impacts of climate change on human health (Bernard et al., 2001), and pervious researches mainly focused on the short-term temperature change related to stroke events (Takumi et al., 2015; Tian et al., 2019a; Pan et al., 1995; Vered et al., 2020). Impacts of long-term temperature change on stroke mortality have not been fully understood yet. For the health effects of long-term temperature change, several researches documented increases in annual temperature were significantly associated with elevated fasting blood glucose and obesity (Wallwork et al., 2017; Yang et al., 2015; Valdes et al., 2014), which were metabolic risk factors for stroke. A few studies also suggested that higher temperature standard deviation was associated with increased natural-cause mortality (Shi et al., 2015, 2016). Some plausible mechanisms explaining these associations included direct effects of temperature variability on cardiovascular systems, and changes in population behavior such as more time spent indoor. Additionally, several case-crossover or time-series studies observed the short-term temperature change could modify the acute effects of particulate matter on cardiovascular events (Chen et al., 2015; Huang et al., 2016; Li et al., 2015; Sun et al., 2015), but less is known about the role of long-term temperature variation in the association between PM2.5 and stroke. Based on the cohort data, this study found that the annual temperature range also affected the health effects of PM2.5 in long run, and the association between PM2.5 and stroke mortality was enhanced when the annual range of temperature was relatively low (< 28.5 °C) among the study participants. Although evidence is still limited in the interactions of temperature variability and air pollution on long-term health outcomes, the findings suggested that assessing chronic health effects linked to air pollution might not ignore the role of long-term temperature change. Further studies need more concerns on the disease burdens attributable to ambient air pollution and temperature jointly in the context of global climate change.
The understanding of biological mechanisms underlying PM2.5-mediated cerebrovascular risk is still evolving. In general, inhaled PM2.5 may stimulate mediators of oxidative stress, or initiating inflammatory responses, while some ultrafine particles may penetrate into the circulatory system leading to direct deleterious effects (Rajagopalan et al., 2018). Animal toxicological and human epidemiological studies also suggested that fine particulate pollutants could provoke vascular endothelial dysfunction, enhance blood coagulation, and promote artery calcification (Franchini and Mannucci, 2011; Kaufman et al., 2016; Tornqvist et al., 2007). These pathophysiologic pathways may be related to the development of stroke and increased risk of stroke mortality associated with long-term PM2.5 exposure. In addition, extreme temperature variations plausibly contributed to cardiovascular damages by increasing amount of free radicals, inducing neuronal apoptotic signal transduction, and even elevating blood pressure and heart rate (Gostimirovic et al., 2020). In future, we still need bio-molecular evidence supporting the specific and joint influences of long-term PM2.5 pollution and temperature variation in cerebrovascular functions.
One of strengths in the current study is that the cohort data were collected from general Chinese participants with a long period of follow-up. Uniformed protocols and questionnaires with strict training for interviewers with strict quality control guaranteed the data quality from multiple survey centers, where the residents had a relatively high exposure of PM2.5. In addition, the high-resolution (1-km) PM2.5 estimates we used were derived from an ensemble machine-learning spatiotemporal model, which had improved the accuracy of ambient PM2.5 exposure estimation (Xiao et al., 2018; Liang et al., 2020b).
Despite the strengths above, several limitations should be addressed. First, the particulate matter is a complex mixture and chemical compositions of PM2.5 may vary in different regions of China (Wang et al., 2014; Zhu et al., 2018), nevertheless we did not collect the detailed composition data of PM2.5 among the study participants. Although all of the study participants were from four northern cities of China, it still needs cautions with effect estimations in the current study, and specific cerebrovascular damages related to different particulate compositions need investigations in future. Second, some known confounders such as fasting lipids and glucose were not available in the baseline survey, although the covariates of demographics, lifestyle, and medical history had been adjusted in regression models stepwise and the results seemed robust for the PM2.5-stroke mortality relationship. Third, the analysis did not consider the indoor air pollutants, such as solid fuel use, which may also contribute to long-term health effects (Arku et al., 2018; Yu et al., 2018, 2020). Fourth, the mechanism for the interaction of long-term exposure to PM2.5 pollution and temperature range is still unclear. It is inferred that a larger annual temperature range might be a marker for a more severe winter with heavier indoor air pollution due to solid fuel use, or a marker for more time spent indoors with less physical activity. More validated studies are expected with more careful and accurate measurements for exposure and potential confounders. Last, the results of subgroup analyses should be cautiously treated, especially in the subgroups of age and education level due to some unbalanced distributions across the four study cities. Independent multi-center studies with uniformed participants’ characteristics should be conducted in the future to obtain robust subgroup-specific associations and to identify people more susceptible to long-term air pollution.
5. Conclusion
In sum, this extended follow-up study provided direct evidence that long-term exposure to PM2.5 will significantly increase stroke mortality under the high concentrations of PM2.5 pollution in northern China. The findings also supported that the strength of association between stroke mortality and air pollution could be modified by annual temperature range. Despite of existed uncertainties, these new findings expand our understanding in the excess mortality linked to long-term PM2.5 exposure and temperature variations. More solid evidence on the adverse health effects related to air pollution and climate change will promote us to take more targeted and efficient reactions to issues of environment and health, especially in those fast industrializing countries such as China.
Supplementary Material
Acknowledgment
This work was supported by the National Key Research and Development Program of China (2017YFC0211600, 2017YFC0211605 and 2017YFC0211704); and the Special Environmental Research Fund for Public Welfare (No. 200709048) from Ministry of Environmental Protection of the People’s Republic of China. The work of Yang Liu is supported by the Multi-Angle Imager for Aerosols Science Team at the Jet Propulsion Laboratory, California Institute of Technology (Subcontract No. 1588347) and the National Institute of Environmental Health Sciences of the National Institutes of Health (Grant No. 1R01ES032140). The content is solely the responsibility of the authors and does not necessarily represent the official views of NASA JPL or NIH.
Abbreviations list:
- PM2.5
particulate matter with aerodynamic diameter ≤ 2.5 μm
- HR
hazard ratio
- China-PAR
Prediction for Atherosclerotic Cardiovascular Disease Risk in China
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ecoenv.2021.112063.
References
- Andersen PK, Gill RD, 1982. Cox’s regression model for counting processes: a large sample study. Ann. Stat 10 (4), 1100–1120. [Google Scholar]
- Arku RE, Birch A, Shupler M, Yusuf S, Hystad P, Brauer M, 2018. Characterizing exposure to household air pollution within the prospective urban rural epidemiology (PURE) study. Environ. Int 114, 307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard SM, Samet JM, Grambsch A, Ebi KL, Romieu I, 2001. The potential impacts of climate variability and change on air pollution-related health effects in the United States. Environ. Health Perspect 109 (Suppl 2), 199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr., Whitsel L, Kaufman JD, American Heart Association Council on E, Prevention CotKiCD, Council on Nutrition PA, Metabolism, 2010. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121 (21), 2331–2378. [DOI] [PubMed] [Google Scholar]
- Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA 3rd, Apte JS, Brauer M, Cohen A, Weichenthal S, Coggins J, Di Q, Brunekreef B, Frostad J, Lim SS, Kan H, Walker KD, Thurston GD, Hayes RB, Lim CC, Turner MC, Jerrett M, Krewski D, Gapstur SM, Diver WR, Ostro B, Goldberg D, Crouse DL, Martin RV, Peters P, Pinault L, Tjepkema M, van Donkelaar A, Villeneuve PJ, Miller AB, Yin P, Zhou M, Wang L, Janssen NAH, Marra M, Atkinson RW, Tsang H, Quoc Thach T, Cannon JB, Allen RT, Hart JE, Laden F, Cesaroni G, Forastiere F, Weinmayr G, Jaensch A, Nagel G, Concin H, Spadaro JV, 2018. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci 115 (38), 9592–9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G, Wang A, Li S, Zhao X, Wang Y, Li H, Meng X, Knibbs LD, Bell ML, Abramson MJ, Wang Y, Guo Y, 2019. Long-term exposure to air pollution and survival after ischemic stroke. Stroke 50 (3), 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Hoek G, 2020. Long-term exposure to PM and all-cause and cause-specific mortality: a systematic review and meta-analysis. Environ. Int 143, 105974. [DOI] [PubMed] [Google Scholar]
- Chen K, Wolf K, Breitner S, Gasparrini A, Stafoggia M, Samoli E, Andersen ZJ, Bero-Bedada G, Bellander T, Hennig F, Jacquemin B, Pekkanen J, Hampel R, Cyrys J, Peters A, Schneider A, Uf, Group, H.S., 2018. Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ. Int 116, 186–196. [DOI] [PubMed] [Google Scholar]
- Chen X, Zhang LW, Huang JJ, Song FJ, Zhang LP, Qian ZM, Trevathan E, Mao HJ, Han B, Vaughn M, Chen KX, Liu YM, Chen J, Zhao BX, Jiang GH, Gu Q, Bai ZP, Dong GH, Tang NJ, 2016. Long-term exposure to urban air pollution and lung cancer mortality: a 12-year cohort study in Northern China. Sci. Total Environ 571, 855–861. [DOI] [PubMed] [Google Scholar]
- Chen YC, Weng YH, Chiu YW, Yang CY, 2015. Short-term effects of coarse particulate matter on hospital admissions for cardiovascular diseases: a case-crossover study in a tropical city. J. Toxicol. Environ. Health A 78 (19), 1241–1253. [DOI] [PubMed] [Google Scholar]
- Franchini M, Mannucci PM, 2011. Thrombogenicity and cardiovascular effects of ambient air pollution. Blood 118 (9), 2405–2412. [DOI] [PubMed] [Google Scholar]
- GBD 2015 Risk Factors Collaborators, 2016. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 388 (10053), 1659–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2017 Causes of Death Collaborators, 2018. Causes of death collaborators. global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392 (10159), 1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostimirovic M, Novakovic R, Rajkovic J, Djokic V, Terzic D, Putnik S, Gojkovic-Bukarica L, 2020. The influence of climate change on human cardiovascular function. Arch. Environ. Occup. Health 75, 406–414. [DOI] [PubMed] [Google Scholar]
- He MZ, Zeng X, Zhang K, Kinney PL, 2017. Fine particulate matter concentrations in urban Chinese cities, 2005–2016: a systematic review. Int. J. Environ. Res. Public Health 14 (2), 191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang F, Luo Y, Guo Y, Tao L, Xu Q, Wang C, Wang A, Li X, Guo J, Yan A, Guo X, 2016. PartIculate Matter And Hospital Admissions for Stroke in Beijing, China: Modification Effects by Ambient Temperature. In: J Am Heart Assoc, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang K, Liang F, Yang X, Liu F, Li J, Xiao Q, Chen J, Liu X, Cao J, Shen C, Yu L, Lu F, Wu X, Zhao L, Wu X, Li Y, Hu D, Huang J, Liu Y, Lu X, Gu D, 2019. Long term exposure to ambient fine particulate matter and incidence of stroke: prospective cohort study from the China-PAR project. BMJ 367, l6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation, 2020. Available from https://vizhub.healthdata.org/gbd-compare. (Accessed 24 August 2020).
- Kaufman JD, Adar SD, Barr RG, Budoff M, Burke GL, Curl CL, Daviglus ML, Roux AVD, Gassett AJ, Jacobs DR, Kronmal R, Larson TV, Navas-Acien A, Olives C, Sampson PD, Sheppard L, Siscovick DS, Stein JH, Szpiro AA, Watson KE, 2016. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the multi-ethnic study of atherosclerosis and air pollution): a longitudinal cohort study. Lancet 388 (10045), 696–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kioumourtzoglou MA, Schwartz J, James P, Dominici F, Zanobetti A, 2016. PM2.5 and mortality in 207 US cities: modification by temperature and city characteristics. Epidemiology 27 (2), 221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinbaum DG, 1996. Survival Analysis: A Self-Learning Test. Springer, New York, NY. [Google Scholar]
- Li Y, Ma Z, Zheng C, Shang Y, 2015. Ambient temperature enhanced acute cardiovascular-respiratory mortality effects of PM2.5 in Beijing, China. Int. J. Biometeorol 59 (12), 1761–1770. [DOI] [PubMed] [Google Scholar]
- Liang F, Liu F, Huang K, Yang X, Li J, Xiao Q, Chen J, Liu X, Cao J, Shen C, Yu L, Lu F, Wu X, Wu X, Li Y, Hu D, Huang J, Liu Y, Lu X, Gu D, 2020a. Long-term exposure to fine particulate matter and cardiovascular disease in China. J. Am. Coll. Cardiol 75 (7), 707–717. [DOI] [PubMed] [Google Scholar]
- Liang F, Xiao Q, Huang K, Yang X, Liu F, Li J, Lu X, Liu Y, Gu D, 2020b. The 17-y spatiotemporal trend of PM2.5 and its mortality burden in China. Proc. Natl. Acad. Sci. USA 117 (41), 25601–25608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E, 2020. Environmental and health impacts of air pollution: a review. Front. Public Health 8, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD, 2007. Long-term exposure to air pollution and incidence of cardiovascular events in women. New Engl. J. Med 356 (5), 447–458. [DOI] [PubMed] [Google Scholar]
- Niu SR, Yang GH, Chen ZM, Wang JL, Wang GH, He XZ, Schoepff H, Boreham J, Pan HC, Peto R, 1998. Emerging tobacco hazards in China: 2. Early mortality results from a prospective study. BMJ 317 (7170), 1423–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan WH, Li LA, Tsai MJ, 1995. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 345 (8946), 353–355. [DOI] [PubMed] [Google Scholar]
- Qian Z, He Q, Lin HM, Kong L, Bentley CM, Liu W, Zhou D, 2008. High temperatures enhanced acute mortality effects of ambient particle pollution in the “oven” city of Wuhan, China. Environ. Health Perspect 116 (9), 1172–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajagopalan S, Al-Kindi SG, Brook RD, 2018. Air pollution and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol 72 (17), 2054–2070. [DOI] [PubMed] [Google Scholar]
- Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Mills NL, 2015. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 350, h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shan A, Zhang Y, Zhang LW, Chen X, Li X, Wu H, Yan M, Li Y, Xian P, Ma Z, Li C, Guo P, Dong GH, Liu YM, Chen J, Wang T, Zhao BX, Tang NJ, 2020. Associations between the incidence and mortality rates of type 2 diabetes mellitus and long-term exposure to ambient air pollution: a 12-year cohort study in northern China. Environ. Res 186, 109551. [DOI] [PubMed] [Google Scholar]
- Shi L, Kloog I, Zanobetti A, Liu P, Schwartz JD, 2015. Impacts of temperature and its variability on mortality in New England. Nat. Clim. Chang 5, 988–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Liu P, Wang Y, Zanobetti A, Kosheleva A, Koutrakis P, Schwartz J, 2016. Chronic effects of temperature on mortality in the southeastern USA using satellite-based exposure metrics. Sci. Rep 6, 30161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Cao P, Chan KP, Tsang H, Wong CM, Thach TQ, 2015. Temperature as a modifier of the effects of fine particulate matter on acute mortality in Hong Kong. Environ. Pollut 205, 357–364. [DOI] [PubMed] [Google Scholar]
- Takumi I, Mishina M, Kominami S, Mizunari T, Kobayashi S, Teramoto A, Morita A, 2015. Ambient temperature change increases in stroke onset: analyses based on the Japanese regional metrological measurements. J. Nippon Med Sch 82 (6), 281–286. [DOI] [PubMed] [Google Scholar]
- Tian Y, Liu H, Zhao Z, Xiang X, Li M, Juan J, Song J, Cao Y, Wang X, Chen L, Wei C, Hu Y, Gao P, 2018. Association between ambient air pollution and daily hospital admissions for ischemic stroke: a nationwide time-series analysis. PLoS Med 15 (10), e1002668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian Y, Liu H, Si Y, Cao Y, Song J, Li M, Wu Y, Wang X, Xiang X, Juan J, Chen L, Wei C, Gao P, Hu Y, 2019a. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: a national time-series study. PLoS Med 16 (1), e1002738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian Y, Liu H, Wu Y, Si Y, Song J, Cao Y, Li M, Wu Y, Wang X, Chen L, Wei C, Gao P, Hu Y, 2019b. Association between ambient fine particulate pollution and hospital admissions for cause specific cardiovascular disease: time series study in 184 major Chinese cities. BMJ 367, l6572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tornqvist H, Mills NL, Gonzalez M, Miller MR, Robinson SD, Megson IL, Macnee W, Donaldson K, Soderberg S, Newby DE, Sandstrom T, Blomberg A, 2007. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med 176 (4), 395–400. [DOI] [PubMed] [Google Scholar]
- Valdes S, Maldonado-Araque C, Garcia-Torres F, Goday A, Bosch-Comas A, Bordiu E, Calle-Pascual A, Carmena R, Casamitjana R, Castano L, Castell C, Catala M, Delgado E, Franch J, Gaztambide S, Girbes J, Gomis R, Gutierrez G, Lopez-Alba A, Martinez-Larrad M, Menendez E, Mora-Peces I, Ortega E, Pascual-Manich G, Serrano-Rios M, Urrutia I, Vazquez JA, Vendrell J, Soriguer F, Rojo-Martinez G, 2014. Ambient temperature and prevalence of obesity in the Spanish population: the Di@bet.es study. Obes. (Silver Spring) 22 (11), 2328–2332. [DOI] [PubMed] [Google Scholar]
- Vered S, Paz S, Negev M, Tanne D, Zucker I, Weinstein G, 2020. High ambient temperature in summer and risk of stroke or transient ischemic attack: a national study in Israel. Environ. Res 187, 109678. [DOI] [PubMed] [Google Scholar]
- Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, Schwartz JD, Baccarelli AA, 2017. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am. J. Epidemiol 185 (1), 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Ying Q, Hu J, Zhang H, 2014. Spatial and temporal variations of six criteria air pollutants in 31 provincial capital cities in China during 2013–2014. Environ. Int 73, 413–422. [DOI] [PubMed] [Google Scholar]
- Wang Y, Kloog I, Coull BA, Kosheleva A, Zanobetti A, Schwartz JD, 2016. Estimating causal effects of long-term PM2.5 exposure on mortality in New Jersey. Environ. Health Perspect 124 (8), 1182–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Q, Chang HH, Geng G, Liu Y, 2018. An ensemble machine-learning model to predict historical PM2.5 concentrations in china from satellite data. Environ. Sci. Technol 52 (22), 13260–13269. [DOI] [PubMed] [Google Scholar]
- Yang HK, Han K, Cho JH, Yoon KH, Cha BY, Lee SH, 2015. Ambient temperature and prevalence of obesity: a nationwide population-based study in Korea. PLoS One 10 (11), e0141724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Tang R, Qiu H, Lai PC, Wong P, Thach TQ, Allen R, Brauer M, Tian L, Barratt B, 2018. Long term exposure to air pollution and mortality in an elderly cohort in Hong Kong. Environ. Int 117, 99–106. [DOI] [PubMed] [Google Scholar]
- Yin P, Brauer M, Cohen A, Burnett RT, Liu J, Liu Y, Liang R, Wang W, Qi J, Wang L, Zhou M, 2017. Long-term fine particulate matter exposure and nonaccidental and cause-specific mortality in a large national cohort of Chinese men. Environ. Health Perspect 125 (11), 117002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yitshak-Sade M, Bobb JF, Schwartz JD, Kloog I, Zanobetti A, 2018. The association between short and long-term exposure to PM2.5 and temperature and hospital admissions in New England and the synergistic effect of the short-term exposures. Sci. Total Environ 639, 868–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu K, Qiu G, Chan KH, Lam KH, Kurmi OP, Bennett DA, Yu C, Pan A, Lv J, Guo Y, Bian Z, Yang L, Chen Y, Hu FB, Chen Z, Li L, Wu T, 2018. Association of solid fuel use with risk of cardiovascular and all-cause mortality in rural China. JAMA 319 (13), 1351–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu K, Lv J, Qiu G, Yu C, Guo Y, Bian Z, Yang L, Chen Y, Wang C, Pan A, Liang L, Hu FB, Chen Z, Li L, Wu T, Chen J, Chen Z, Clarke R, Collins R, Guo Y, Li L, Lv J, Peto R, Walters R, Avery D, Boxall R, Chang Y, Chen Y, Chen Z, Clarke R, Du H, Gilbert S, Hacker A, Hill M, Holmes M, Iona A, Kartsonaki C, Kerosi R, Kong L, Kurmi O, Lancaster G, Lewington S, Lin K, McDonnell J, Millwood I, Nie Q, Radhakrishnan J, Ryder P, Sansome S, Schmidt D, Sherliker P, Sohoni R, Stevens B, Turnbull I, Walters R, Wang J, Wang L, Wright N, Yang L, Yang X, Bian Z, Guo Y, Han X, Hou C, Lv J, Pei P, Liu C, Tan Y, Yu C, Pang Z, Gao R, Li S, Wang S, Liu Y, Du R, Zang Y, Cheng L, Tian X, Zhang H, Zhai Y, Ning F, Sun X, Li F, Lv S, Wang J, Hou W, Zeng M, Jiang G, Zhou X, Yang L, He H, Yu B, Li Y, Xu Q, Kang Q, Guo Z, Wang D, Hu X, Wang H, Chen J, Fu Y, Fu Z, Wang X, Weng M, Guo Z, Wu S, Li Y, Li H, Fu Z, Wu M, Zhou Y, Zhou J, Tao R, Yang J, Su J, Liu F, Zhang J, Hu Y, Lu Y, Ma L, Tang A, Zhang S, Jin J, Liu J, Tang Z, Chen N, Huang Y, Li M, Meng J, Pan R, Jiang Q, Lan J, Liu Y, Wei L, Zhou L, Chen N, Wang P, Meng F, Qin Y, Wang S, Wu X, Zhang N, Chen X, Zhou W, Luo G, Li J, Chen X, Zhong X, Liu J, Sun Q, Ge P, Ren X, Dong C, Zhang H, Mao E, Wang X, Wang T, Zhang X, Zhang D, Zhou G, Feng S, Chang L, Fan L, Gao Y, He T, Sun H, He P, Hu C, Zhang X, Wu H, He P, Yu M, Hu R, Wang H, Qian Y, Wang C, Xie K, Chen L, Zhang Y, Pan D, Gu Q, Huang Y, Chen B, Yin L, Liu H, Fu Z, Xu Q, Xu X, Zhang H, Long H, Li X, Zhang L, Qiu Z, 2020. Cooking fuels and risk of all-cause and cardiopulmonary mortality in urban China: a prospective cohort study. Lancet Glob. Health 8 (3), e430–e439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S, Wang J, Jiang Q, He Z, Huang Y, Li Z, Cai L, Cao S, 2019. Long-term exposure to PM2.5 and stroke: a systematic review and meta-analysis of cohort studies. Environ. Res 177, 108587. [DOI] [PubMed] [Google Scholar]
- Zhang LW, Chen X, Xue XD, Sun M, Han B, Li CP, Ma J, Yu H, Sun ZR, Zhao LJ, Zhao BX, Liu YM, Chen J, Wang PP, Bai ZP, Tang NJ, 2014. Long-term exposure to high particulate matter pollution and cardiovascular mortality: a 12-year cohort study in four cities in northern China. Environ. Int 62, 41–47. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Huang L, Li J, Ying Q, Zhang H, Liu X, Liao H, Li N, Liu Z, Mao Y, Fang H, Hu J, 2018. Sources of particulate matter in China: insights from source apportionment studies published in 1987–2017. Environ. Int 115, 343–357. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


