Abstract
Purpose of Review
Sexual well-being and intimacy are critical to overall quality of life and retain a high degree of significance for aging individuals, even though these considerations are often overlooked in older populations. Sexual health may be particularly impacted in older individuals living with HIV, especially women, as a result of both physical and psychosocial disease-specific factors. Despite this, sexuality research related to HIV has traditionally focused on risk reduction, rather than on other elements of sexual wellness. In this review, we examine several aspects of sexual well-being that may be important to older women living with HIV (OWLH).
Recent Findings
This review summarizes existing literature on sexuality in OWLH over the age of 50 and explores five themes related to sexual health: physical and emotional intimacy, desire/interest, satisfaction/pleasure, frequency of sexual activity, and abstinence. Reduced intimacy among OWLH was reported across most studies, due to stigma and disclosure concerns, lack of opportunity for relationships, and difficulty communicating sexual preferences. Data on sexual desire/interest and satisfaction/pleasure among OWLH were mixed. Frequency of sexual activity varied widely across studies, and abstinence emerged as both an intentional and inadvertent decision for OWLH. Factors related to menopause as it relates to sexuality and HIV are also discussed.
Summary
Sexual health and well-being are important to women living with HIV over 50, though key components such as intimacy, desire, and pleasure remain poorly understood. As this population continues to grow, comprehensive and age-specific interventions are needed to examine positive aspects of sexuality and promote sexual wellness among OWLH.
Keywords: Sexuality, Intimacy, Sexual function, Older women, HIV
Introduction
Sexual health is an important component of quality of life across the lifespan. Intimate partner relationships are also widely viewed as critical aspects of quality of life and emotional well-being [1, 2]. Although the importance of sexuality, sexual activity, and intimacy among older persons (aged 50 and older) who are now living longer, healthier lives has been increasingly recognized in the literature [3–5], the sexuality of older people is often neglected in other domains. Many major health surveys only collect data for individuals of reproductive age, i.e., from 15 to 49 [6], and providers often fail to address sexual health proactively for older people [7–9]. Yet, it is evident that older adults continue to desire romantic relationships, intimacy, and sexual activity as they age [10–12], which suggests that sexual health is a priority for this population.
Living with HIV may compromise sexual health, for older persons and specifically for women. In the USA, the Centers for Disease Control and Prevention estimate that older adults will comprise 70% of HIV/AIDS cases by 2020 [13], and older adults account for 17% of new cases [14]. With early and sustained use of antiretroviral therapies, all persons living with HIV are living longer and healthier lives [15–17]: as of 2013, an estimated 91,492 women living with HIV were aged 50 and older [18]. For these women, maintaining sexual health may prove difficult for a number of reasons, including compromised physical and mental health, menopause, and disability [19•, 20•, 21•, 22•]. In addition, older women living with HIV (OWLH) face psychosocial challenges that impact sexual well-being and affect safer sex practices, such as changes in relationship status (from married/partnered to separated, divorced, or widowed), social losses and stigma, diminished social support (along with grief, isolation, and loneliness), and limited opportunities for intimacy [23, 24].
Navigating the dual stigmas of age and HIV status may also negatively affect the sexual health of OWLH. When OWLH discuss or attempt to discuss aspects of their sexuality with medical providers, friends, and family members, they may be met with the belief that older women are not and should not be sexually active [12]. Providers may also believe that women living with HIV should not be sexually active. Fear of discrimination, stigma, and disclosure could result in self-imposed restrictions on expressions of sexuality, further compromising sexual health in this population [25].
OWLH may find that the few providers who do initiate conversations about sexual health in the exam room focus on the reduction of HIV transmission risk to the exclusion of sexual wellness or well-being. Research on sexual health among individuals living with HIV most often assesses the likelihood of sexual risk-taking or tests the efficacy of different risk reduction strategies rather than examining interventions that target intimacy, satisfaction, or pleasure [26••, 27]. Risk reduction strategies are certainly relevant to OWLH, and they should be discussed with patients. Indeed, a recent study demonstrated that condomless sex and other risky behaviors may be more common in OWLH because condom use negotiation is difficult with older male partners who have issues with sexual dysfunction, the likelihood of which increases with age [28]. Other psychosocial issues that may decrease the likelihood of safe sex behaviors among older women include partner trust, relationship imbalance, and traditional gender roles, among others [29, 30••]. However, although sexual risk certainly warrants continued attention, intimacy, and sexual well-being should also be addressed, if only to increase engagement in HIV-related care.
To date, there are no published reviews that examine other aspects of sexual health that are important to OWLH, such as desire, satisfaction, and intimacy. Examining the literature on the sexual well-being of these women is a crucial first step in developing comprehensive, generationally specific HIV-related interventions that attend to both risk reduction and sexual pleasure. In this review, we identify and review several aspects of sexual health and well-being that may be important to women aged 50 and older who are living with HIV. At this age, OWLH are also navigating the complexities of the menopausal transition, during which a range of physiological, psychosocial, and sexual symptoms may further compromise sexual intimacy and overall quality of life. Though we did not specifically focus on the effects of menopause on sexual health among OWLH, the menopausal transition provides an important context for these findings.
Methods
Information sources
We conducted a comprehensive search of PubMed, PsycINFO, PsycNET, and CINAHL for papers focusing on sexuality in older women living with HIV. To identify relevant studies, the following keyword search terms were used: “sexual satisfaction,” “sexuality NOT risk,” “sexual function,” “sexual disclosure,” “sexual desire,” “sexual communication,” and “intimacy.” All searches included the terms “HIV” and “older women.” Database results were combined with results from relevant literature reference lists, and duplicates were removed.
The first two authors independently reviewed article titles and abstracts, discussed and resolved discrepancies, and agreed on a final set of articles for a thorough review. The authors read the full texts of all remaining articles to assess eligibility for inclusion. Eligible articles were (1) published in peer-reviewed journals, (2) published in English, and (3) included women ages 50 and older who were living with HIV. No date nor geographical restrictions were used, and studies could be quantitative or qualitative. Clinical interventions were also included. Ineligible articles (1) did not include women in our target age range, (2) focused only on sexual or HIV risk, (3) did not cover sexual behavior, (4) did not cover HIV, or (5) did not constitute research studies (i.e., reviews or meta-analyses).
Quality assessment
All included studies were independently assessed for quality by the first two authors. Quantitative studies were rated using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [31], which establishes guidelines for conducting quality assessments of observational research. The STROBE statement consists of a 22-item scoring checklist, with each item worth one point. Articles are rated across a number of domains pertaining to the abstract, method, results, and discussion sections, respectively; item scores are totaled for an overall quality rating. Articles with scores between 17 and 22 are considered to be of high quality, those between 11 and 16 of moderate quality, and those 10 and under of low quality.
Qualitative studies were assessed using the Evidence-Based Nursing Guide for evaluating qualitative research [32]. There are nine criteria, each worth one point, which include appraisals of the appropriateness of the research question, design, and sampling method, as well as the thoroughness of the analysis, description of findings, and relevance for clinical practice. High-quality articles are those scoring 50% or more of the maximum score (i.e., nine points), and low-quality articles are those with scores below 50% of the maximum score. All quality ratings, for both qualitative and quantitative studies, are displayed in Table 1.
Table 1.
Summary of overall themes for all studies
| Reference | Intimacy | Desire/interest | Satisfaction/pleasure | Frequency of sexual activity | Abstinence | Quality of evidence | Score |
|---|---|---|---|---|---|---|---|
| Boonyanurak et al. [33]a | X | X | X | High | 17 | ||
| Chirinda and Zungu [34]a | X | High | 18 | ||||
| Denis and Hong [35]a | X | X | X | X | Moderate | 16 | |
| Grodensky etal. [36•]b | X | X | X | High | 8 | ||
| Kaida et al. [37•]a | X | X | X | High | 20 | ||
| Lovejoy et al. [38]a | X | High | 22 | ||||
| Negin et al. [39]a | X | X | High | 18 | |||
| Nevedal and Sankar [40]b | X | X | High | 9 | |||
| Psaros et al. [41]b | X | X | High | 8 | |||
| Siegel and Schrimshaw [42]b | X | High | 8 | ||||
| Taylor et al. [43•]b | X | X | X | High | 8 | ||
| Whyte et al. [44]b | X | High | 7 |
Quantitative studies (maximum score 22)
Qualitative studies (maximum score 9)
Results
A flow chart of the literature search and article review process is shown in Fig. 1. A total of 483 citations were identified across all databases and reviews of reference lists in the literature. Following the removal of duplicates, 351 papers remained. The authors screened titles and abstracts of the 351 articles for eligibility. Following this process, 336 articles were removed; excluded articles were not about sex (n = 96) or HIV (n = 88), focused primarily on sexual risk (n = 83), did not include any participants in the target age range (n = 47), did not include women (n = 14), or were review articles (n = 14). Full texts of the remaining 15 papers were read to evaluate eligibility. Following this review, three additional articles were removed; one was outside the age range (n = 1), one was not about sex (n = 1), and one was a review article (n = 1). Thus, a total of 12 articles (six quantitative and six qualitative) met eligibility criteria and were included in this review.
Fig. 1.
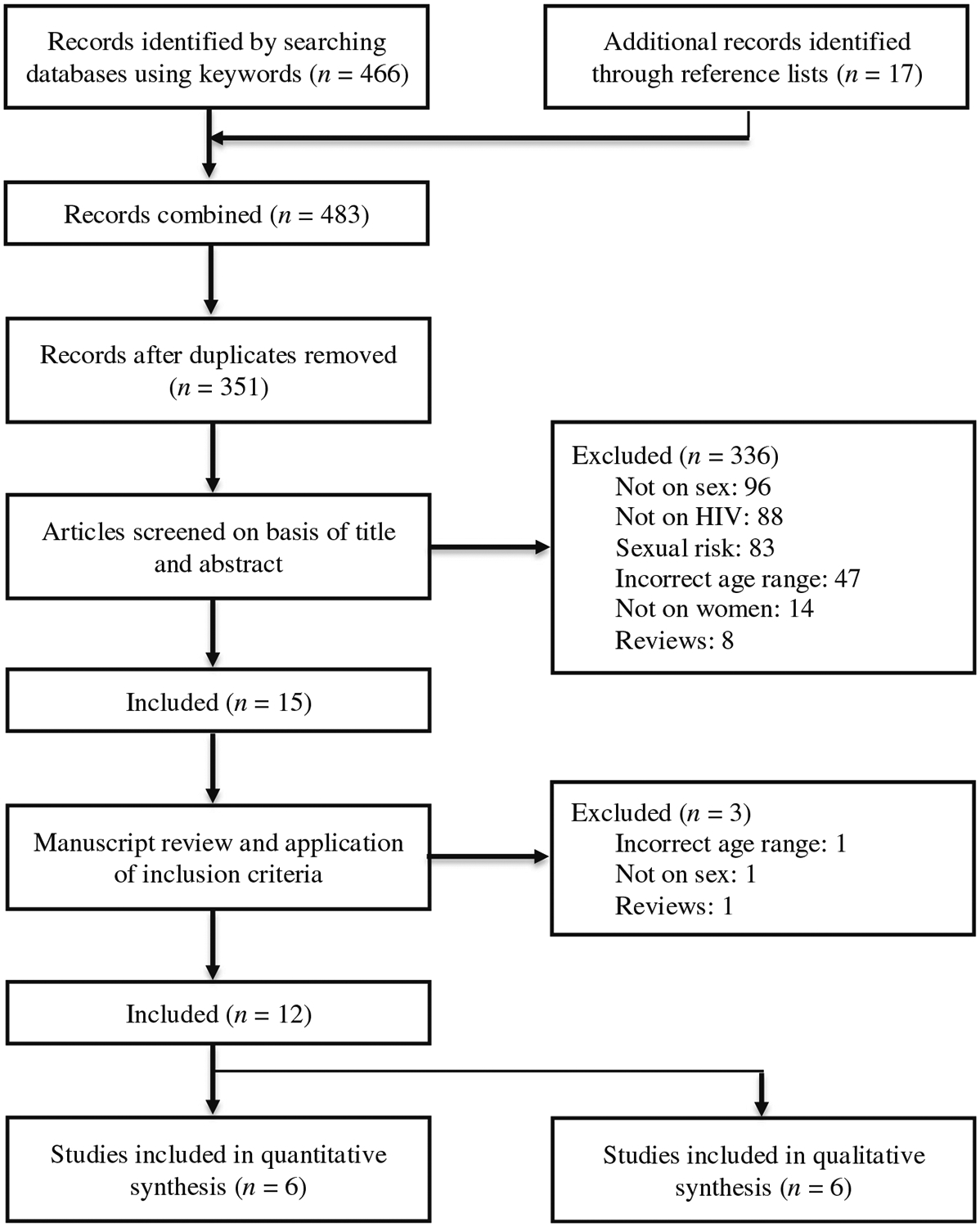
Flow diagram on identifying literature
Characteristics of the selected studies
All 12 studies included in this systematic review were published in peer-reviewed journals. The six quantitative papers were cross-sectional studies. Six different countries are represented in the selected studies, with one conducted in Thailand, one in South Africa, one in Australia, one in Canada, one in Uganda, and seven in the USA. There were 13,768 total participants, combined across all studies (9122 females). Sample sizes ranged from 11 to 11,642. The samples of five studies included both men and women, while seven studies included only women. The age ranges of participants, as well as the time since HIV diagnosis, varied across studies; these are displayed in Table 2. Given the small number of studies that examined these topics in older women, we opted to include studies that included both younger and older women, focusing specifically on data from women aged 50 and over.
Table 2.
Age and other demographic information from reviewed studies
| Reference | Sex of sample | Age at time of data collection (years) | Time since diagnosis |
|---|---|---|---|
| Boonyanurak et al. [33] | Women only | 40+ (full sample)a | Median = 11.1 years (full sample) |
| Chirinda and Zungu [34] | Men and women | 50–80+ (full sample) | Not reported |
| Denis and Hong [35] | Women only | Under 20–59 (full sample)a | Not reported |
| Grodensky et al. [36•] | Women only | 50–79 | Not reported |
| Kaida et al [37•] | Women only | 16–50+a | Median = 10.8 years |
| Lovejoy et al. [38] | Men and women | 50+ (full sample) | Mean = 11.9 years (abstinent women) Mean = 12.4 years (sexually active women) |
| Negin et al. [39] | Men and women | 50–83 (full sample) | Mean = 9 years (full sample) |
| Nevedal and Sankar [40] | Men and women | 51–78 (full sample); 51–69 (women only) |
Mean = 11.1 years (full sample) |
| Psaros et al. [41] | Women only | 50+ | Mean = 16.32 years (full sample) |
| Siegel and Schrimshaw, 2003 [42] | Men and women | 50–68 (full sample) | Mean = 6.29 years (full sample) |
| Taylor et al. [43•] | Women only | 50–69 | Not reported |
| Whyte et al. [44] | Women only | 49–67 | Mean = 1.6 years (full sample) |
For studies including younger women as well as older women, we focused on women over the age of 50
Five themes of sexual health were identified across the 12 studies: intimacy, desire/interest, satisfaction/pleasure, frequency of sexual activity, and abstinence. The findings of the studies that addressed these themes are reviewed below:
Intimacy
Intimacy referred to any discussion of emotional or physical engagement in sexual relationships and activities [40]. Six of the 12 studies addressed intimacy in the context of romantic relationships. Many women reported challenges initiating and maintaining intimate relationships. In one study, postmenopausal women living with HIV were significantly more likely to avoid intimacy than non-postmenopausal women living with HIV [33], suggesting that age does impact intimacy and relationship building. Compared to women who did not have HIV, OWLH had significantly lower scores on the relationship subscale of the Sexual Health Questionnaire (SHQ [45]), which approximates intimacy by measuring the combination of conflict in the relationship, ability to communicate sexual desires and preferences, and overall satisfaction [35]. Among older women who contracted the virus from long-term male partners who also have sex with men, maintaining an intimate relationship in the face of anger at that partner and a sense of betrayal required a strong history of previous intimacy and joint investment in the physical health of both partners [44]. After they were diagnosed, some women chose to leave their partners. OWLH describe the importance of companionship [44]; it is evident that intimacy with a partner is difficult to achieve for these women.
In a study that examined the role of intimacy among African American OWLH, some participants distinguished between sexual intimacy and emotional intimacy [40]. For these women, the loss of emotional intimacy at the end of a relationship was the greater burden; they reported that sexual relationships were sometimes not worth the risk of rejection and humiliation, whereas emotional closeness was highly valued. Similar sentiments were also expressed in other studies [41]. Fears associated with disclosure compromised both emotional and sexual intimacy, leading some women to pursue or maintain seroconcordant relationships. Only two of the 13 women described overcoming the barriers to establishing an intimate relationship and ultimately revealing their HIV status to their partners. Disclosure challenges may be heightened among African American women, as HIV-related stigma is reportedly higher in this group compared to other populations of older adults living with HIV [46].
Specific barriers to intimacy, such as fear associated with disclosure, HIV-related stigma, and limited sexual opportunities, were also addressed. In a small qualitative study of OWLH in the southern region of the USA, all participants reported limiting social and intimate interactions because they feared that others would learn of their HIV status [36•]. In this same sample, only three of 15 women reported having a committed romantic partner with whom they were sexually active, and just one woman reported having occasional sex with a male friend. In another qualitative study, fears related to the process of disclosure also affected intimacy; OWLH felt a sense of obligation to disclose their HIV status to potential partners, but they also feared their reactions [41]. This type of HIV-related stigma led to profound hopelessness about ever finding intimacy with a partner. In the same sample, body image was also a significant barrier to intimacy. Participants reported significant body dissatisfaction (due in part to long-term use of antiretroviral medications and/or menopausal status), which left them feeling undesirable to current or potential intimate partners [41].
Desire/interest
Five studies examined the sexual desire of OWLH. Sexual desire is typically defined as the motivation to engage in or be receptive to a sexual event, whether partnered or alone. Other words used to describe desire include interest, drive, or libido [47]. Most of the studies reviewed here demonstrated decreased desire among OWLH compared to both older women without HIVand pre-menopausal women, though it is challenging to disentangle the effects of menopause from those of the virus. Compared to women who were not living with HIV, OWLH had significantly lower scores on the sexual interest subscale of the SHQ [45], which measures the frequency of sexual thoughts, urges, or fantasies as well as the desire to engage in fantasy, foreplay, or sexual activity [35]. Among older adults living with HIV in Uganda, a quantitative measure of sexual desire was lower in women than in men [39]. When asked what interfered with their ability to be sexually active, women reported that low levels of desire and HIV status limited their sexual engagement.
Importantly, sexual desire was not dampened for all participants in the studies reviewed; some women reported an increase in sexual desire as they aged, and a subset of women who were currently in relationships did not report any decreases in sexual interest. One participant explained, “I feel like I am at my peak. I’m in the prime of my life…that I want to be sexually aroused. I want my husband to make love to me because I feel that as I was growing up I really didn’t care about sex” [43•, p. 1140–1141]. In a separate study, OWLH who were in an intimate relationship did not report a lack of or diminished sexual desire, whereas OWLH who were not in relationships either did not want to have sex, did not care either way, or reported that sex was not important to them [36•]. It may be that relationship status and partner availability play an important role in the maintenance of sexual desire among OWLH.
Satisfaction/pleasure
Sexual satisfaction and pleasure were discussed in three studies, and the findings were relatively mixed. Compared to women who were not living with HIV, OWLH had significantly lower sexual satisfaction in one study [35]. Yet, most women surveyed in a separate study reported being satisfied with their current sex lives (64% [37•]). As in other research on women without HIV, sexual satisfaction was lower among sexually inactive OWLH than among sexually active women (49% vs. 79% [37•]). Demographic factors may account for this difference; OWLH in the first study were slightly older than their comparison group. Similarly, the sexually inactive group was significantly older and less likely to be in a committed relationship than the women who were sexually active [37•]. Of the 12 studies included in this analysis, Taylor and colleagues’ [43•] qualitative interviews and focus groups with older African American and Latina OWLH most thoroughly addressed the changes in sexual pleasure and satisfaction that were associated with HIV and aging. Many participants reported that sex became more satisfying after age 50 due to both increased comfort with experimentation and greater awareness of pleasurable sensations in the body, which may also have been associated with increased desire. One participant reported that, as she aged, she derived more enjoyment from the non-penetrative aspects of sexual activity, such as touching, kissing, and caressing. Though sexual satisfaction increased across the lifespan for several women, others were dissatisfied by their partners’ inability to perform sexually, often due to physical ailments and/or sexual dysfunction. Participants’ own physical limitations and HIV-related health conditions (e.g., diabetes, hypertension, neuropathy) also created barriers to their own pleasure and associated frustration. Despite these challenges, most participants had a strong desire to maintain sexual pleasure as they aged, in part because it was perceived to be a fundamentally important aspect of womanhood.
Frequency of sexual activity
Seven studies addressed the frequency of sexual activity and factors associated with reduced activity among OWLH, and three studies compared the experiences of older women with those of older men. Compared to women who were not living with HIV, OWLH engaged in sexual activity significantly less frequently over the past month [35]; activities assessed in this study included vaginal intercourse as well as kissing, touching, hugging, and holding a partner. Consistent with the literature on younger individuals with and without HIV, older men living with HIV were significantly more sexually active than OWLH [34, 38, 39]. In one study, only 21% of heterosexual women were sexually active in the past month, compared to 36% of gay or bisexual men and 72% of heterosexual men [38]. In a sample of older men and women living with HIV in Uganda, 14% of women were currently sexually active with one partner, whereas 39% of men reported having one sexual partner, and 10% of men had more than one [39]. In South Africa, older men living with HIV were more likely to report sexual activity within the past year than older women [34]; however, the prevalence of sexual activity among older women increased over time, from 28.8% in 2005 to 33.8% in 2012. Across the seven studies, the highest percentage of sexually active OWLH was 82%, reported by Taylor and colleagues [43•]; this study reported a variety of sexual behaviors as well as concurrent sexual partnerships.
Several factors, ranging from income level to HIV-related stigma, were associated with sexual activity frequency among OWLH. Women who reported being in a relationship had higher annual incomes and had greater perceived physical well-being were likely to be sexually active [38], whereas symptoms of menopause were related to lack of sexual activity in the past month [33]. Factors associated with reduced sexual activity in older South African women included HIV and increasing age [34]. In a hierarchical regression model of sexual activity among older adults living with HIV in Uganda, the odds of sexual activity in the past year significantly increased with the availability of a partner (married or cohabitating), better physical functioning, and male gender [39]. In a separate logistic regression model, sexual inactive OWLH in Canada had significantly higher adjusted odds of being older, not being in a relationship, having low household income, and reporting high HIV-related stigma [37•]. The authors of this study noted that sexual inactivity was not associated with ART use or viral suppression, suggesting that strong HIV-related treatment outcomes alone do not lead to healthy and satisfying sex for OWLH.
Abstinence
Five studies included some evidence of OWLH choosing to remain abstinent from sexual activity for a variety of reasons, including fear of HIV transmission, stigma, and lack of trust. Some women refrained from sexual activity as a means of preventing transmission to others and avoiding prosecution for doing so. For example, one woman explained, “Where I moved from, on the table in the clinic was a brochure, a Xeroxed page reminding us that it’s a felony—you can be arrested—if you, for example, have a sexual relationship and you do not disclose it…Lots of worries about abstinence. Or if you’re not abstinent” [41]. Among several older African American women living with HIV, fear of rejection was a significant contributing factor associated with abstinence [40]. In this study, six of 13 participants refused any involvement in sexual or intimate relationships; some of these women described privileging their concerns about rejection over the pain caused by a lack of intimacy, whereas others noted a loss of self-esteem and poor body image as factors driving their abstinence. Fear of rejection as well as negative expectations and risks associated with disclosure were linked to abstinence in several other studies [37•, 41].
In a study that specifically examined reasons for celibacy among older adults following an HIV diagnosis, women were more likely than men to abstain from sexual activity (78% vs. 36%; [42]). The authors defined celibacy as abstinence from sexual intercourse and other sexual activity with another person for at least 2 months following a diagnosis. Some reasons for celibacy were shared between men and women (e.g., fear of transmitting the virus); others were specific to women, such as a loss of interest in sex or anger and distrust of men. Though both men and women reported changes in their sexual activity post-diagnosis, women often chose to remain abstinent out of anger and a strong sense of victimization, especially when they acquired the virus through a trusted partner.
Abstinence was also envisioned by some as an opportunity to focus on personal issues rather than a means of coping with fear or avoiding potential rejection. Some women viewed abstinence as a permanent choice (e.g., “I don’t do that anymore”), whereas others considered their abstinence to be temporary [36•, 41]. Permanent or temporary abstinence could either be deliberate (e.g., “I am comfortable focusing on myself”) or unintentional (e.g., “My partner died”, or “I desire a partner but there are none available”). In a separate study, some women who chose abstinence reported feeling emotionally satisfied with their individual relationships with God and therefore had little or no need for romantic partnerships [36•]. Though most OWLH associated negative experiences or emotions with abstinence, some women chose not to engage in sexual activity because they felt comfortable focusing on themselves and maintaining other important relationships.
Discussion
This review explored the sexual well-being of OWLH, focusing on aspects of sexual health that are often overlooked both in this population and in general, including pleasure, desire, and satisfaction. In 12 studies that included or specifically recruited only OWLH, five areas of sexuality and sexual wellness were addressed: intimacy, desire/interest, satisfaction/pleasure, frequency of sexual activity, and abstinence. Most studies found intimacy to be reduced among OWLH, due to limited opportunities for intimate relationships, concerns about stigma and rejection after disclosure, difficulties communicating sexual desires and preferences to partners, body dissatisfaction, and a general sense of hopelessness [33, 35, 36•, 40, 41]. The data on satisfaction and pleasure among OWLH were mixed, with some studies reporting significantly lower satisfaction, others suggesting sufficient satisfaction, and still others indicating an increase in sexual pleasure with age; such findings are not uncommon in the sexual health literature, especially among older women. With respect to sexual activity, the percentage of sexually active OWLH ranged from 14% [39] to 82% [43•], though sexual activity was measured over different periods of time, from within the past month to over the past year. Older women with HIV were significantly less likely than older men with HIV to be sexually active [34, 38, 39], and sexually inactive women were more likely to be older, not in a relationship, have low household income, and have high HIV stigma [37•]. Finally, some OWLH intend to abstain from all sexual activity, whereas others inadvertently stop having sex due to partner death or abandonment. Avoidance-based reasons for abstinence include fear of rejection following disclosure, fear of HIV transmission, and HIV-related stigma; low self-esteem, loss of interest, and distrust of men also factored into the decision-making process [37•, 40–42].
It is important to consider and address the influence of menopause on the sexual health of OWLH. Studies have reported decreases in the frequency of sexual activity in postmenopausal women [48], as declines in estrogen and testosterone are known to affect sexual desire, sexual activity frequency, and overall urogenital health. Several studies have demonstrated that natural menopause occurs earlier in women living with HIV, at approximately 46–49 years of age [33, 49•, 50]. The menopausal transition, and particularly early menopause, can have multi-dimensional effects on the health and well-being of women living with HIV. In addition to its impacts on sexual function and sexual activity, early menopause is associated with a number of negative health outcomes, including cardiovascular disease [51], stroke [52], and bone fracture [53] among women in the general population. Older women living with HIV are more vulnerable to these comorbidities [54–56], and therefore, they may face additional challenges during the transition to menopause. For example, OWLH in the UK described several menopause-related concerns that were associated with their HIV status, including difficulties distinguishing menopausal symptoms from HIV symptoms, difficulties accessing appropriate menopause care, and challenges navigating the impact of menopausal symptoms on antiretroviral therapy adherence [57]. In this large, UK-based sample (10,000+ OWLH), very few participants were using menopausal hormone therapy, which is considered to be the most effective treatment for vasomotor symptoms associated with menopause at any age [58]. It is evident that OWLH may require additional support throughout the menopausal transition to maintain both physical health and sexual well-being.
Another crucial aspect of sexual health for OWLH is sexual risk reduction, which we purposefully did not address in this review given the fairly robust body of extant literature on that topic. Indeed, condomless sex may be common among sexually active OWLH, due in part to a low perceived risk of HIV transmission [43•]. Power dynamics and relationship factors affect condom use, as men continue to play the leading role in condom use decision making; reduced pregnancy concerns and higher rates of age-related erectile dysfunction also contribute to increased risk for transmission of HIV and STIs [11, 59]. Though OWLH may be interested in maintaining safer sex practices, partner attitudes and beliefs around condom use, their own misperceptions about transmission, and the prevalence of sexual dysfunction compromise those efforts.
With these associated risks in mind, focusing on pleasure and sexual wellness in both research and clinical practice may have positive implications for maintaining safe sex practices in this population. Safety and satisfaction can go hand in hand if both sexual health interventions developed for OWLH and conversations between providers and patients address risk reduction and pleasure simultaneously. Interventions may include dyadic elements (e.g., sexual communication tools that have been associated with increased sexual satisfaction), mindfulness-based exercises that have been demonstrated to increase sexual desire [60], or psychoeducation on the relationship between menopause and HIV. Providers should consider initiating conversations about sexual pleasure and satisfaction by first asking patients if they are comfortable answering some questions related to their sexual activity and then directly probing about pleasure, satisfaction, and desire. Risk-related messaging that does not incorporate these additional strategies or fails to acknowledge the many positive aspects of sexual health may alienate patients from their providers and ultimately be less efficacious.
Sexual health programs or antiretroviral medication adherence interventions that incorporate both risk and intimacy will also need to be tailored to the unique needs and social norms of OWLH in resource-limited settings. Only three studies in this review examined the sexual wellness of OWLH in these settings, though evidence from cohorts in South Africa, Uganda, Malawi, and Zimbabwe indicates that men and women remain sexually active well past their 50s [61–64]. In a population-based survey of South Africans aged 15–80, Houle and colleagues [63••] found that around 20% of women aged 60 and over have had sex in the past 2 years; 20% is far from negligible.
Though this review did not explicitly examine the cultural factors that affect sexual well-being among OWLH, partnered relationships and reasons for sexual activity differ by region and by country. It is important to acknowledge that sexual health data from one resource-limited setting does not generalize to other resource-limited settings. For instance, marriage rates are lower and later in South Africa than in both Thailand and Uganda, and there is considerable variation in age at first sex, time spent single, and time spent sexually active in Eastern and Southern Africa [65] as well as across Southeast Asia [66, 67]. Moreover, in these contexts more so than in developed countries, women may engage in sexual activity for reasons other than wanting to do so. Given the now worldwide consensus that individuals living with HIV whose viral loads are stably suppressed cannot sexually transmit the virus [68••], OWLH in these settings may be more interested in building intimate relationships with partners, remaining sexually active, and increasing their sexual satisfaction. Providers and clinicians who work with OWLH should convey the message that undetectable=untransmittable (U=U) not only to increase motivation to adhere to antiretroviral regimens, but also to enable sex without fear [68••].
For the most part, the limitations of this review reflect the general limitations of the size and scope of this body of literature. Five of the included studies examined aspects of sexual health among both women and men living with HIV, and three studies included participants across a wide age range. Analyses were often not separated by gender or age, perhaps masking differences or nuances that may warrant further exploration. No studies currently exist that evaluate sex-positive interventions for older women living with HIV. In addition, the sexual health and well-being of OWLH in specific resource-limited settings or culturally similar regions should ideally be the subject of its own review. Unfortunately, data in this area are currently lacking, which impacts the generalizability of these findings.
Conclusions
Sexuality, intimacy, and sexual health are multifaceted and nuanced concepts. Models of sexual health highlight the importance of safe sex practices while also acknowledging other key components, like body image, culture, fantasy, and spirituality (see Sexual Health Model [69]). These models bring us closer to actualizing the positive health, dignity, and prevention goals that have been put forth by The Joint United Nations Program on HIV/AIDS [70], which place the person living with HIVat the center of her healthcare and well-being, but evidence-based, culturally specific interventions have yet to be developed. Sexuality and sexual wellness are a critical component of this care, especially for OWLH, who generally desire to maintain sexual satisfaction and intimacy but face numerous barriers in doing so.
Funding Information
This work was supported by a T32 training grant (5T32MH116140-02).
Dr. Robbins declares grants from Gilead, Emergent Solutions, Citius Pharmaceuticals, Inc., and Pfizer, outside of the submitted work.
Dr. Psaros reports personal fees in consultation with collaborators at Brown University. In this role, she supervises interventionists on an HIV medication adherence trial.
Footnotes
Conflict of Interest Dr. Stanton, Dr. Looby, and Dr. Goodman each declare no conflicts of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Bouman WP, Arcelus J, Benbow SM. Nottingham study of sexuality & ageing (NoSSA I). Attitudes regarding sexuality and older people: a review of the literature. Sex Relation Ther. 2006;21:149–61. [Google Scholar]
- 2.Lee D, Nazroo J, O’Connor D, et al. Sexual health and well-being among older men and women in England: findings from the English Longitudinal Study of Ageing. Arch Sex Behav. 2016;45: 133–44. [DOI] [PubMed] [Google Scholar]
- 3.Delamater J Sexual expression in later life: a review and synthesis. J Sex Res. 2012;49:125–41. [DOI] [PubMed] [Google Scholar]
- 4.Syme ML. The evolving concept of older adult sexual behaviour and its benefits. Generations. 2014;38:35–41. [Google Scholar]
- 5.Wang V, Depp CA, Ceglowski J, et al. Sexual health and function in later life: a population-based study of 606 older adults with a partner. Am J Geriatr Psychiatry. 2015;23:227–33. [DOI] [PubMed] [Google Scholar]
- 6.Negin J, Cumming R. HIV infection in older adults in sub-Saharan Africa: extrapolating prevalence from existing data. Bull World Health Organ. 2010;88:847–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gott M, Galena E, Hinchliff S, et al. ‘Opening a can of worms’: GP and practice nurse barriers to talking about sexual health in primary care. Fam Pract. 2004;21:528. [DOI] [PubMed] [Google Scholar]
- 8.Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58:2093–103. [DOI] [PubMed] [Google Scholar]
- 9.Politi M, Clark M, Armstrong G, McGarry K, Sciamanna CN. Patient-provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med. 2009;24: 511–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks JT, Buchacz K, Gebo KA, et al. HIV infection and older Americans: the public health perspective. (Author abstract). Am J Public Health. 2012;102:1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schick V, Herbenick D, Reece M, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: implications for sexual health promotion for older adults. J Sex Med. 2010;7:315–29. [DOI] [PubMed] [Google Scholar]
- 12.Taylor A, Gosney MA. Sexuality in older age: essential considerations for healthcare professionals. Age Ageing. 2011;40:538–43. [DOI] [PubMed] [Google Scholar]
- 13.Tietz D. Older Americans: the changing face of HIV/AIDS in America. 2013. https://www.aging.senate.gov/imo/media/doc/02_Tietz_9_18_13.pdf. Accesssed 01 Jul 2019.
- 14.Administration on Aging. HIV: know the RISKS. Get the FACTS. 2016. https://acl.gov/sites/default/files/programs/2016-11/HIVAIDS_Factsheet.pdf. Accesssed 01 Jul 2019.
- 15.Hogg RS, Yip B, Chan KJ, Wood E, Craib KJ, O’Shaughnessy MV, et al. Rates of disease progression by baseline CD4 cell count and viral load after initiating triple-drug therapy. JAMA. 2001;286: 2568–77. [DOI] [PubMed] [Google Scholar]
- 16.Patterson S, Cescon A, Samji H, Chan K, Zhang W, Raboud J, et al. Life expectancy of HIV-positive individuals on combination antiretroviral therapy in Canada. BMC Infect Dis. 2015;15:1–10. 10.1186/s12879-015-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.••.Samji H, Cescon A, Hogg RS, et al. Closing the gap: increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS ONE. 2013;8. 10.1371/journal.pone.0081355 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study estimates changes in life expectancy among individuals living with HIV and on antiretroviral therapies (ART) from 2000–2007. The authors determined that a 20-year-old individual on ART in the USA or Canada could expect to live into their early 70s, a life expectancy that approaches that of the general population in these two countries.
- 18.Centers for Disease Control and Prevention. HIV surveillance report. 2014. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf. Accesssed 01 Jul 2019.
- 19.•.Brennan D, Emlet C, Eady A. HIV, sexual health, and psychosocial issues among older adults living with HIV in North America. Ageing Int. 2011;36:313–33 [Google Scholar]; This paper describes some of the epidemiological trends among older adults living with or at risk for HIV in North America. The authors also review the current and emerging sexual health needs of this population.
- 20.Grov C, Golub S, Parsons J, Brennan M, Karpiak SE. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care. 2010;22:630–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalichman SC, Heckman T, Kochman A, Sikkema K, Bergholte J. Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatr Serv. 2000;51:903–7. [DOI] [PubMed] [Google Scholar]
- 22.Shippy RA, Karpiak SE. The aging HIV/AIDS population: fragile social networks. Aging Ment Health. 2005;9:246–54. [DOI] [PubMed] [Google Scholar]
- 23.Dykstra PA, Fokkema T. Social and emotional loneliness among divorced and married men and women: comparing the deficit and cognitive perspectives. Basic Appl Soc Psych. 2007;29:1–12. [Google Scholar]
- 24.Pinquart M Loneliness in married, widowed, divorced, and never-married older adults. J Soc Pers Relat. 2003;20:31–53. [Google Scholar]
- 25.Gurevich M, Mathieson CM, Bower J, et al. Disciplining bodies, desires and subjectivities: sexuality and HIV-positive women. Fem Psychol. 2007;17:9–38. [Google Scholar]
- 26.••.Gay J, Hardee K, Croce-Galis M, et al. What works to meet the sexual and reproductive health needs of women living with HIV/AIDS. J Int AIDS Soc. 2011;14:56–56. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review identifies sexual and reproductive health interventions that have been effectively employed in resource-limited countries to address the needs of women living with HIV. The authors emphasize that there are a number of promising interventions, but they note that operationalizing these programs has been challenging.
- 27.Kennedy CE, Spaulding AB, Brickley DB, et al. Linking sexual and reproductive health and HIV interventions: a systematic review. J Int AIDS Soc. 2010;13:26–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nunes S, Azevedo F, Lisboa C. Sexually transmitted infections in older adults – raising awareness for better screening and prevention strategies. J Eur Acad Dermatol Venereol. 2016;30:1202–4. [DOI] [PubMed] [Google Scholar]
- 29.Jarman M, Walsh S, De Lacey G. Keeping safe, keeping connected: a qualitative study of HIV-positive women’s experiences of partner relationships. Psychol Health. 2005;20:533–51. [Google Scholar]
- 30.••.Stevens PE, Galvao L. ‘He won’t use condoms’: HIV-infected women’s struggles in primary relationships with serodiscordant partners. Am J Public Health. 2007, 97:1015–22 [DOI] [PMC free article] [PubMed] [Google Scholar]; In this longitudinal qualitative study, women living with HIV described their sexual behavior over time. Women who reported engaging in sexual activity without using a condom highlighted challenges negotiating condom use with their partners.
- 31.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453. [DOI] [PubMed] [Google Scholar]
- 32.Russell CK, Gregory DM. Evaluation of qualitative research studies. Evid Based Nurs. 2003;6:36–40. [DOI] [PubMed] [Google Scholar]
- 33.Boonyanurak P, Bunupuradah T, Wilawan K, Lueanyod A, Thongpaeng P, Chatvong D, et al. Age at menopause and menopause-related symptoms in human immunodeficiency virus–infected Thai women. Menopause. 2012;19:820–4. [DOI] [PubMed] [Google Scholar]
- 34.Chirinda W, Zungu N. Health status and years of sexually active life among older men and women in South Africa. Reprod Health Matters. 2016;24:14–24. [DOI] [PubMed] [Google Scholar]
- 35.Denis A, Hong S-M. Sexual functioning of women with HIV: a comparison with non-HIV women. Can J Hum Sex. 2003;12:97. [Google Scholar]
- 36.•.Grodensky C, Golin C, Jones C, et al. ‘I should know better’: the roles of relationships, spirituality, disclosure, stigma, and shame for older women living with HIV seeking support in the South. J Assoc Nurses AIDS Care. 2015;26:12. [DOI] [PMC free article] [PubMed] [Google Scholar]; This qualitative study examines the specific stressors faced by older women living with HIV in the Southeastern USA, where HIV-related stigma is particularly high. Some women reported that spirituality provided some support.
- 37.•.Kaida A, Carter A, De Pokomandy A, et al. Sexual inactivity and sexual satisfaction among women living with HIV in Canada in the context of growing social, legal and public health surveillance. J Int AIDS Soc. 2015; 18:n/a–n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study investigates the influence of legal and public health surveillance of HIVon the sexual activity and well-being of women living with HIV. The authors suggest that some women may be choosing to abstain from sexual activity to resist surveillance by the state and avoid criminalization for non-disclosure.
- 38.Lovejoy TI, Heckman TG, Sikkema KJ, Hansen NB, Kochman A, Suhr JA, et al. Patterns and correlates of sexual activity and condom use behavior in persons 50-plus years of age living with HIV/AIDS. AIDS Behav. 2008;12:943–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Negin J, Geddes L, Brennan-Ing M, Kuteesa M, Karpiak S, Seeley J. Sexual behavior of older adults living with HIV in Uganda. Arch Sex Behav. 2016;45:441–9. [DOI] [PubMed] [Google Scholar]
- 40.Nevedal A, Sankar A. The significance of sexuality and intimacy in the lives of older african americans with HIV/AIDS. Gerontologist. 2016;56:762–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Psaros C, Barinas J, Robbins GK, Bedoya CA, Safren SA, Park ER. Intimacy and sexual decision making: exploring the perspective of HIV positive women over 50. AIDS Patient Care STDS. 2012;26: 755–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siegel K, Schrimshaw EW. Reasons for the adoption of celibacy among older men and women living with HIV/AIDS. J Sex Res. 2003;40:189–200. [DOI] [PubMed] [Google Scholar]
- 43.•.Taylor TN, Munoz-Plaza CE, Goparaju L, et al. “The pleasure is better as I’ve gotten older”: sexual health, sexuality, and sexual risk behaviors among older women living with HIV. Arch Sex Behav. 2017;46:1137. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this qualitative study of older women living with HIV in three US cities, some participants reported an increase in sexual pleasure and sexual freedom with age.
- 44.Whyte J, Whyte MD, Cormier E. Down low sex, older African American women, and HIV infection. J Assoc Nurses AIDS Care. 2008;19:423–31. [DOI] [PubMed] [Google Scholar]
- 45.Syrjala KL, Schroeder TC, Abrams JR, et al. Sexual function measurement and outcomes in cancer survivors and matched controls. J Sex Res. 2000;37:213–25. [Google Scholar]
- 46.Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. J Assoc Nurses AIDS Care. 2010;21:144–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Althof SE, Meston CM, Perelman MA, Handy AB, Kilimnik CD, Stanton AM. Opinion paper: on the diagnosis/classification of sexual arousal concerns in women. J Sex Med. 2017;14:1365–71. [DOI] [PubMed] [Google Scholar]
- 48.Addis IB, Van Den Eeden SK, Wassel-Fyr CL, et al. Sexual activity and function in middle-aged and older women. Obstet Gynecol. 2006;107:755–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.•.de Pommerol M, Hessamfar M, Lawson-Ayayi S, Neau D, Geffard S, Farbos S, et al. Menopause and HIV infection: age at onset and associated factors, ANRS CO3 Aquitaine cohort. Int J STD AIDS. 2011;22:67–72 [DOI] [PubMed] [Google Scholar]; This paper demonstrates increased risk of early menopause among women living with HIV.
- 50.Ferreira CE, Pinto-Neto AM, Conde DM, Costa-Paiva L, Morais SS, Magalhães J. Menopause symptoms in women infected with HIV: prevalence and associated factors. Gynecol Endocrinol. 2007;23:198–205. [DOI] [PubMed] [Google Scholar]
- 51.Melissa WJ, Pamela OM, Pamela SM, et al. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause. 2012;19:1081–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Walter RA, Brandon GR, Virginia MM, et al. Premature menopause or early menopause and risk of ischemic stroke. Menopause. 2012;19:272–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Svejme O, Ahlborg H, Nilsson J, Karlsson MK. Early menopause and risk of osteoporosis, fracture and mortality: a 34-year prospective observational study in 390 women. BJOG. 2012;119:810–6. [DOI] [PubMed] [Google Scholar]
- 54.Kanapathipillai R, Hickey M, Giles M. Human immunodeficiency virus and menopause. Menopause. 2013;20:983–90. [DOI] [PubMed] [Google Scholar]
- 55.Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab. 2007;92:2506–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Michael YT, Chiyuan ZA, Donald MJ, et al. Higher rates of bone loss in postmenopausal HIV-infected women: a longitudinal study. J Clin Endocrinol Metab. 2012;97:554–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tariq S, Burns FM, Gilson R, et al. PRIME (Positive Transitions Through the Menopause) Study: a protocol for a mixed-methods study investigating the impact of the menopause on the health and well-being of women living with HIV in England. BMJ Open. 2019, 9. 10.1136/bmjopen-2018-025497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.De Villiers TJ, Gass MLS, Haines CJ, et al. Global consensus statement on menopausal hormone therapy. Climacteric. 2013;16:203–4. [DOI] [PubMed] [Google Scholar]
- 59.Zona S, Guaraldi G, Luzi K, Beggi M, Santi D, Stentarelli C, et al. Erectile dysfunction is more common in young to middle-aged HIV-infected men than in HIV-uninfected men. J Sex Med. 2012;9:1923–30. [DOI] [PubMed] [Google Scholar]
- 60.Brotto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women. Behav Res Ther. 2014;57:43–54. [DOI] [PubMed] [Google Scholar]
- 61.Freeman E, Anglewicz P. HIV prevalence and sexual behaviour at older ages in rural Malawi. Int J STD AIDS. 2012;23:490–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Freeman EK, Coast E. Sex in older age in rural Malawi. Ageing Soc. 2014;34:1118–41. [Google Scholar]
- 63.••.Houle B, Mojola SA, Angotti N, Schatz E, Gómez-Olivé FX, Clark SJ, et al. Sexual behavior and HIV risk across the life course in rural South Africa: trends and comparisons. AIDS Care. 2018;30:1435–43 [DOI] [PMC free article] [PubMed] [Google Scholar]; This population-based survey reveals similarities and differences in sexual risk and protective behaviors among young, middle-aged, and older adults in South Africa. Notably, the findings demonstrate risk for acquiring HIV among older adults, stemming from cross-generational sex and low condom use.
- 64.Todd J, Cremin I, Mcgrath N, et al. Reported number of sexual partners: comparison of data from four African longitudinal studies. Sex Transm Infect. 2009;85. 10.1136/sti.2008.033985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marston M, Slaymaker E, Cremin I, et al. Trends in marriage and time spent single in sub-Saharan Africa: a comparative analysis of six population-based cohort studies and nine demographic and health surveys. Sex Transm Infect. 2009;85:1. i64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jones GW, Gubhaju B. Factors influencing changes in mean age at first marriage and proportions never marrying in the low-fertility countries of East and Southeast Asia. Asian Popul Stud. 2009;5: 237–65. [Google Scholar]
- 67.Techasrivichien T, Darawuttimaprakorn N, Punpuing S, Musumari PM, Lukhele BW, el-Saaidi C, et al. Changes in sexual behavior and attitudes across generations and gender among a population-based probability sample from an urbanizing province in Thailand. Arch Sex Behav. 2016;45:367–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.••.Calabrese SK, Mayer KH. Providers should discuss U=U with all patients living with HIV. Lancet HIV. 2019;6:e211–3 [DOI] [PubMed] [Google Scholar]; The authors of this paper call for providers to communicate to their patients that, if their HIV viral load is suppressed, they cannot transmit the virus sexually. Awareness of this relationship may contribute to improved sexual health and well-being.
- 69.Robinson B’B’ E, Bockting WO, Simon Rosser BR, et al. The Sexual Health Model: application of a sexological approach to HIV prevention. Health Educ Res. 2002;17:43–57. [DOI] [PubMed] [Google Scholar]
- 70.UNAIDS, Global Network of People Living with HIV. Positive health, digity, and prevention: a policy framework. 2011. https://www.unaids.org/sites/default/files/media_asset/20110701_PHDP_0.pdf. Accesssed 01 Jul 2019.


