Abstract
Objective
To explore the iodine status of lactating mother-newborn pairs, and whether neonatal serum thyroid-stimulating hormone (TSH) can be used for estimation of iodine status of the population.
Materials and Methods
A total of 334 mothers and their healthy neonates were included. Urine, serum, and breast milk samples were obtained at 4th and 6th days of delivery. Urinary iodine concentration (UIC) was measured in urine samples of mothers and their neonates, as well as breast milk iodine concentration (BMIC) and serum thyroid hormone levels of neonates, were measured from the samples taken between the 4th and 6th days after birth.
Results
Median age of the mothers was 27 years (23–30). The median UIC of mothers and their newborns were 125 μg/L and 142 μg/L, respectively. The median BMIC was 138,0 μg/L. There was a significant positive correlation between the BMIC and UIC of neonates (r=0.276, p<0.001). The prevalence of neonatal serum TSH >10 mIU/L, which is suggestive of mild iodine deficiency (i.e. 3.0–19.9%), was 19.0%. However, there were no participants with iodine deficiency in lactating mothers and neonates according to UIC.
Conclusion
By previous reports, Aydın is iodine sufficient. Although 19% of the neonates had serum TSH levels >10 mU/L, which is suggestive of a mild iodine deficiency, iodine deficiency was observed in none of the neonates and their mothers. Therefore, it will be appropriate to investigate the role of neonatal TSH levels in a larger sample to assess the iodine status of the population.
Keywords: Breast milk, neonate, thyroid function, urinary iodine
What is already known on this topic?
Iodine deficiency is an important public health problem in our country, iodine deficiency is common, especially in rural areas.
It is recommended to check the urinary iodine concentration to test the iodine status. Also, TSH levels of newborns are used as a marker to show iodine deficiency.
What this study adds on this topic?
Mothers and their newborns in Aydın province were found to be iodine-sufficient.
In the neonatal period, the TSH level is affected by many factors other than iodine deficiency, and its role in showing iodine deficiency should be investigated in larger studies.
Introduction
Iodine is an essential trace element that enters the structure of thyroid hormones and is necessary for thyroid hormone synthesis (1). Iodine deficiency diseases are disorders that can cause a series of developmental and functional diseases and can be prevented with iodine prophylaxis. Brain development is irreversibly affected in the case of iodine deficiency in the intrauterine period and within the first three months after birth (2). Iodine deficiency may cause an increase in endemic goiter, cretinism, mental retardation, infertility, congenital anomalies, perinatal and infant deaths due to thyroid hormone synthesis disorder (1, 2). Iodine deficiency diseases maintain their importance as an important public health problem in our country as well as in all over the world. Although the prevalence of iodine deficiency decreases as using iodized salt was made mandatory in our country, it continues to be a problem especially in rural areas (3).
The best indicator of iodine status in the community is the measurement of urinary iodine excretion (4). In the periods immediately after birth, when brain development is critical, breast milk is the only source of iodine for babies. Breast milk iodine concentration (BMIC) is another marker that can show the iodine status of society (5). Apart from urinary iodine concentration (UIC), goiter rate, thyroglobulin level in school-age children and thyroid-stimulating hormone (TSH) level in the neonatal period are also markers that can be used to evaluate the iodine status of the population (6). Since the iodine cycle in newborns is faster than in children and adults, it is known that TSH level in newborns may be a sensitive marker in reflecting the population’s iodine status (6).
In this study, it was aimed to evaluate the iodine status by examining the urine and breast milk iodine levels in the samples taken on the postnatal 4th–6th day from the breastfeeding mother and newborn couple and to investigate the role of serum TSH levels in newborn cases in predicting the population’s iodine status.
Materials and Methods
Approval for the study was obtained from Aydın Adnan Menderes University Clinical Research Ethics Committee (2006/00144). Participants in the study were informed about the study and the permission was obtained by signing an informed consent form. The study was conducted following the Helsinki declaration principles.
Participants
Mothers who gave birth in four major districts of Aydın (Efeler, Nazilli, Söke, Kuşadası) were included in the study and their newborn infants on the postnatal 4th–6th days were included. Inclusion criteria were determined as (1) the participants had no thyroid disease or a known chronic disease, (2) not using iodine-containing drugs during pregnancy, (3) being a single pregnancy, (4) the gestational age 37–42 weeks, (5) birth weight between 2,500 and 4,000 grams (6) babies are fed exclusively with breast milk.
Before the study, the mothers of the newborns were given detailed information about the study, a written informed consent text was presented about the study, and the informed consent form with written consent was read and signed. The age, educational status, number of pregnancies, number of births, miscarriage and stillbirth history, consanguinity, drug use, topical iodine exposure, salt-restricted diet use, history of goiter and thyroid disease, smoking, goitrogen food intake, the quality of the salt used in the diet, the way of storing the salt, the way of using it in meals, the frequency of seafood consumption, the week of gestation, the type of delivery and the gender, birth weight and height of the newborns, the diet and how the umbilical cord care is performed were questioned.
Time of Collection of Urine, Blood, and Breast Milk Samples and Storage Conditions
All samples (urine, blood, and breast milk) of mothers and newborns were collected between the 4th and 6th days of postpartum period.
Serum samples were taken from the veins on the dorsum of the newborns’ hands after cleaning the area where blood will be taken, with 70% alcohol cotton. After centrifugation at 4000 rpm for seven minutes, the separated maternal serum samples were stored at −80 °C until the analysis day, newborn serum samples were stored at −20 °C to be studied in the same week.
Urine samples were taken from the mothers and their newborns as the first urine in the morning. Urine samples obtained from mothers by mid-stream urine method and from newborns with urine bags suitable for their gender were placed in deiodinated Eppendorf tubes and all samples were stored at −80 C until the day of analysis.
The breast milk samples were taken into deiodinated Eppendorf tubes by hand milking from the mothers simultaneously with the urine and blood samples and stored at −80 ºC until the day of analysis.
Laboratory Measurements
UIC and BMIC were measured with the Sandell-Kolthoff reaction using the colorimetric ceric arsenic acid solution recommended by the World Health Organization (WHO) and the results were obtained as μg/L (7). Free T4 (FT4), total T4 (TT4), total T3 (TT3), and TSH levels were analyzed by electrochemiluminescence immunoassay (ECLIA) method (Roche Elecsys E170, USA). Normal ranges for newborns were taken as; 0.9–2.2 ng/dL for serum FT4, 0.4–10.0 mIU/L for TSH, 6.5–16.3 μg/dL for TT4, 100–300 ng/dL for TT3.
Definitions
According to the recommendations of WHO/International Council for the Control of Iodine Deficiency Disorders (ICCIDD)/UNICEF criteria, median UIC of <100 μg/L for breastfeeding mothers and newborn babies was accepted as deficiency and >100 μg/L as normal; Similarly, BMIC IC<100 μg/L was accepted as deficiency and >100 μg/L as normal (8).
A threshold value of 10 mIU/L was taken for serum TSH level for newborns and <3% of babies with a WHO-recommended TSH value >10 mIU/L (equivalent to capillary TSH> 5 mIU/L) was accepted as iodine adequacy (9, 10). Babies above this threshold were recalled and their thyroid hormone levels were re-studied one week later, and those with serum TSH levels >20 mIU/L were diagnosed with congenital hypothyroidism, and treatment was initiated (11).
Statistical Analysis
Statistical analysis of the data was performed using the Statistical Package for the Social Sciences (SPSS) version 25.0 (IBM SPSS Corp.; Armonk, NY, USA) package program. Descriptive and frequency analyzes were made. The normal distribution of the data was determined according to the Kolmogorov-Smirnov test, histogram, Q-Q plot, skewness, and kurtosis coefficients. Chi-square test was used for comparison of group proportions, and the Mann-Whitney U test was used to compare data of two independent groups that did not have a normal distribution. The relationship of the data with each other was analyzed by the Spearman correlation test. In the evaluation of the relationship, the correlation coefficient was classified as “0–0.24: poor”, “0.25–0.49: medium”, “0.50–0.74: strong “, “0.75–1.00: very strong”. Normally distributed data were given as mean ± standard deviation (SD), non-normally distributed data were given as median (25p–75p). Values of p<0.05 were considered significant.
Results
Three-hundred thirty-four mothers and their newborn babies were included in the study. It was determined that 81.6% of mothers with a median age of 27 years were housewives, 59% were multiparous, 41.6% were primary school graduates, 40% had consanguineous marriages and 97% used table salt containing iodine. Most of the mothers consumed seafood less than once a week consumed more than 1 teaspoon of salt and added salt when the meal was close to being cooked. The median birth height and weight of newborn babies (53.3% girls, 46.7% boys) were 49 cm (48–50) and 3340 g (3050–3600), respectively. Umbilical cord care was performed with a topical disinfectant containing iodine in 20.4% of the babies. The main characteristics of the mothers and their babies included in the study are given in Table 1.
Table 1.
Demographic and nutritional characteristics of the mother and newborn
| Characteristics | n | % |
|---|---|---|
| Mothers | ||
| Age (year) | 27 (23–30) | |
| Median (25p–75p) | ||
| Type of Delivery | ||
| Normal | 193 | 57.8 |
| Cesarean | 141 | 42.2 |
| Parity | ||
| Primipara | 137 | 41 |
| Multipara | 197 | 59 |
| Education Status | ||
| Illiterate | 25 | 7.5 |
| Literate | 6 | 1.8 |
| Primary School | 139 | 41.6 |
| Secondary School | 52 | 15.6 |
| High School | 76 | 22.8 |
| University | 36 | 10.8 |
| Occupation | ||
| Housewife | 273 | 81.7 |
| Worker/officer | 45 | 13.5 |
| Self-employment | 12 | 3.6 |
| Other | 4 | 1.2 |
| Consanguinity | 40 | 12 |
| Daily salt consumption | ||
| Teaspoon | 84 | 25.1 |
| Dessert spoon | 163 | 48.8 |
| Tablespoon | 77 | 23.1 |
| No | 10 | 3.0 |
| How to use salt | ||
| Before cooking | 133 | 39.8 |
| Close to cooking | 173 | 51.8 |
| After cooking | 29 | 8.4 |
| Seafood consumption | ||
| Once a week | 101 | 30.2 |
| Biweekly | 86 | 25.7 |
| Once in a month | 61 | 18.3 |
| Less | 86 | 25.8 |
| Thyroid disease in the family | 100 | 29.9 |
| Newborns | ||
| Birth weight (g) | 3340 (3050–3600) | |
| Median (25p–75p) | ||
| Birth Height (cm) | 49 (48–50) | |
| Median (25p–75p) | ||
| Gender | ||
| Female | 178 | 53.3 |
| Male | 156 | 46.7 |
| Umbilical cord care with iodine | ||
| Yes | 68 | 20.4 |
| No | 266 | 79.6 |
Median UIC value of mothers was found as 125 μg/L (118.0–141.0) BMIC was 138.0 μg/L (132.0–143.0) UIC value of neonates was 142.0 μg/L (132.0–151.0) in urine of neonates. Iodine deficiency was not found in any mother and newborn baby included in the study (Table 2).
Table 2.
Iodine levels and serum thyroid hormone levels of the participants
| Characteristics | Median | 25p–75p | %95 CI |
|---|---|---|---|
| Mothers | |||
| Urinary iodine concentration (μg/L) | 125.0 | 118.0–141.0 | 126.9–129.6 |
| Breast milk iodine concentration (μg/L) | 138 | 132.0–143.0 | 136.6–138.3 |
| Newborns | |||
| Free T4 (ng/dL) | 1.67 | 1.49–1.91 | 1.66–1.72 |
| Total T4 (μg/dl) | 13.7 | 11.4–16.2 | 13.7–14.4 |
| Total T3 (ng/dl) | 178.5 | 148.0–223.3 | 183.6–196.9 |
| TSH (mIU/L) | 4.6 | 2.8–8.5 | 6.3–7.9 |
| Urinary iodine concentration (μg/L) | 142.0 | 132.0–151.0 | 14.05–143.5 |
CI: confidence interval
There were 66 newborns (19.7%) with serum TSH levels >10 mIU/L. Twenty of these babies had iodine-containing antiseptic exposure for umbilical cord care. When newborns with serum TSH levels >10 mIU/L and <10 mIU/L were compared, no significant difference was found between the two groups in terms of UIC and BMIC (Table 3). Four (6%) of these recalled babies were diagnosed with congenital hypothyroidism and thyroxine treatment was started for these babies.
Table 3.
Comparison of babies with serum TSH levels <10 mIU/L and >10 mU/mL
| Characteristics | Serum TSH <10 mIU/L (n=268) | Serum TSH >10 mIU/L (n=66) | P * |
|---|---|---|---|
| Gender | |||
| Female (%) | 149 (55.6) | 29 (43.9) | |
| Male (%) | 119 (44.4) | 37 (56.1) | 0.89 |
| Type of Delivery | |||
| Normal | 152 (56.7) | 41 (62.1) | |
| Cesarean | 116 (43.3) | 25 (37.9) | 0.426 |
| Birth weight (g) | 3300 (3000–3600) | 3430 (3140–3600) | 0.119 |
| Birth height (cm) | 49 (48–50) | 50 (49–51) | 0.123 |
| Maternal age (year) | 27 (22–30) | 26.5 (23–29) | 0.896 |
| Number of pregnancies | 2 (1–2) | 2 (1–3) | 0.206 |
| Free T4 (ng/dL) | 1.68 (1.52–1.91) | 1.59 (1.39–1.89) | 0.042 |
| Total T4 (μg/dL) | 13.9 (11.6–16.3) | 12.6 (10.9–15.6) | 0.066 |
| Total T3 (ng/dL) | 178.5 (148.3–222.8) | 178.5 (146.5–226.8) | 0.139 |
| TSH (mIU/L) | 3.89 (2.48–5.74) | 15.4 (12.10–22.30) | <0.001 |
| Neonatal urinary iodine concentration (μg/L) | 141.0 (131.0–150.0) | 145.0 (138,0–154,3) | 0.053 |
| Maternal urinary iodine concentration (μg/L) | 125.0 (118.0–140.0) | 129.0 (117–142) | 0.957 |
| Breast milk urinary iodine concentration (μg/L) | 138,0 (132.0–143.0) | 138.5 (130.8–143.0) | 0.720 |
Chi-square test and Mann-Whitney U test
Data are given as median value (25p–75p).
Infants who used iodine-containing antiseptic for umbilical cord care were found to have lower serum free and total T4 levels, and higher TSH and UIC levels compared to infants who did not use (P<0.005) (Table 4).
Table 4.
Characteristics of babies with and without topical iodine in umbilical cord care
| Characteristics | Iodine used (n=68) | Iodine not used (n=266) | P * |
|---|---|---|---|
| Gender | |||
| Female (%) | 35 (51.5) | 143 (53.8) | |
| Male (%) | 33 (48.5) | 123 (46.2) | 0.736 |
| Type of Delivery | |||
| Normal | 39 (57.4) | 154 (57.9) | |
| Cesarean | 29 (42.6) | 112 (42.1) | 0.936 |
| Birth weight (g) | 3500 (3062–3787) | 3300 (3048–3565) | 0.030 |
| Birth height (cm) | 50 (48–51) | 49 (48–50) | 0.139 |
| Maternal age (year) | 25.5 (22.0–29.8) | 27 (23–30) | 0.11 |
| Number of pregnancies | 2 (1–3) | 2 (1–2) | 0.879 |
| Free T4 (ng/dL) | 1.60 (1.36–1.82) | 1.70 (1.52–1.92) | 0.005 |
| Total T4 (μg/dL) | 12.55 (10.63–15.53) | 13,90 (11.68–16.40) | 0.005 |
| Total T3 (ng/dL) | 171.5 (144–225) | 180.0 (148.0–222.3) | 0.747 |
| TSH (mIU/L) | 6.53 (3.65–11.25) | 4.34 (2.66–7.32) | 0.002 |
| Newborn urinary iodine concentration (μg/L) | 150.5 (141.3–160.0) | 140.0 (130.0–149.0) | <0.001 |
Chi-square test and Mann-Whitney U test
Data are given as median value (25P–75P).
When the relationship between iodine levels was evaluated, there was a positive significant relationship between BMIC and newborn IC (r= 0.276, P<0.001), but no relationship was found between maternal UIC and newborn UIC.
While no relationship was observed between TSH levels of newborn cases and maternal UIC and BMIC, a positive significant correlation was found with UIC of newborn cases (r=0.120, P=0.028) (Table 5, Figure 1).
Table 5.
Correlation of TSH levels of newborns with clinical and laboratory findings
| Neonatal TSH | ||
|---|---|---|
| Spearman’s Rho | r | P |
| Birth Weight | 0.052 | 0.346 |
| Free T4 | −0.095 | 0.082 |
| Total T4 | −0.101 | 0.065 |
| Total T3 | 0.081 | 0.138 |
| Breast milk urinary iodine concentration | 0.025 | 0.646 |
| Maternal urinary iodine concentration | −0.049 | 0.371 |
| Newborn urinary iodine concentration | 0.120 | 0.028 |
Figure 1.
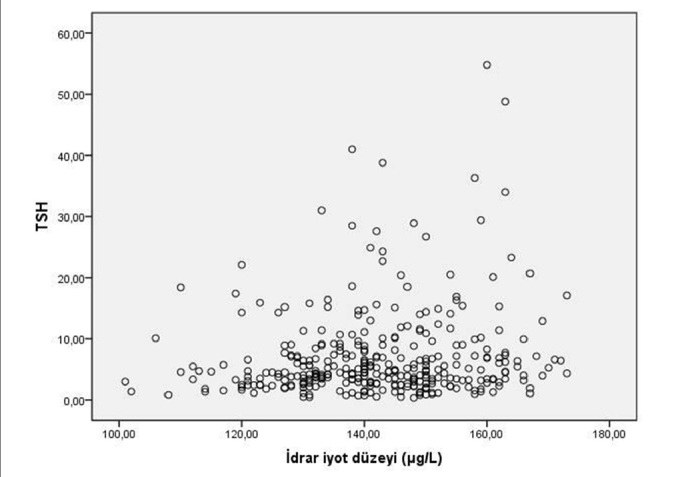
Correlation of urinary iodine concentration and serum TSH level of newborns
Discussion
Iodine intake should be sufficient for normal thyroid functions of mothers and newborn babies during pregnancy and breastfeeding (2). In this study, iodine levels were found to be >100 μg/L in mothers who gave birth in Aydın and their newborns according to the WHO definition, and the iodine status of the study population was found to be sufficient following previous studies (3).
Iodine deficiency continues to be an important public health problem worldwide (6). Since 1999, Turkey has mandated the enrichment of table salt with iodine (12). Although a dramatic decrease in the prevalence of iodine deficiency has been observed in our country with this policy, iodine deficiency is still common, especially in rural areas (3). Although there is more than one method for evaluating iodine status in a region, it has been recommended to check UIC since 2001 (4). A median UIC level of >100 g/L in children and breastfeeding women is considered as normal (8). In studies conducted in our country in recent years and investigating UIC in pregnant or breastfeeding mothers, median UIC has been reported in ranges between 80.5–222.0 μg/L (13–16). According to the data in 2007, the median UIC in Aydın is 140 μg/L and Aydın has been reported as an iodine sufficient region (3). In our study, the median UIC values of breastfeeding mothers and newborns were found to be 125 μg/L and 142 μg/L, respectively, which shows that iodine levels in our city are consistent with 2007 data. Also, the use of iodine-enriched table salt by 97% of mothers, most of whom are housewives and approximately half of them have only received primary education, indicates that iodized salt can be an effective method in preventing iodine deficiency and the target of 95% of the households’ iodized salt consumption rate of the Turkish Ministry of Health has been reached. However, considering that the daily iodine requirement (220 mcg) during pregnancy can be met with approximately one teaspoon of iodized salt, it is observed that the salt consumption of the mothers in our study was higher than the need (2).
In the evaluation of iodine deficiency diseases in a region, TSH levels of newborns are also used in addition to UIC (17). In newborns, more than 3% of cases with capillary TSH level >5 mIU/L and cord blood TSH level> 10 mIU/L indicates iodine deficiency (17, 18). In our study, this rate was found to be 19% and although it indicates a mild iodine deficiency according to this definition, no iodine deficiency was found according to UIC. There are studies in the literature that do not show a relationship between maternal UIC and neonatal capillary TSH levels (19, 20). In a recent study conducted with 399 German newborn cases where capillary TSH> 5 mIU/L frequency was found to be compatible with mild iodine deficiency with 14%, the median UIC was reported to be iodine sufficient with 150 μg/L (21). Researchers have reported that when iodine is sufficient, the mass and amount of thyroid cells decrease, so more TSH is needed to produce a sufficient amount of thyroid hormone, and consequently, the TSH threshold value should be taken higher (21). Apart from the mother’s iodine status, many factors such as prematurity, the time of blood collection for TSH determination, exposure of the mother or baby to antiseptics containing iodine, and the measurement method of TSH affect the TSH levels of newborns. In our study, it was shown that the main reason in cases with TSH level >10 mIU/L was not iodine deficiency, and the TSH level returned to the normal range in 94% of these babies who were recalled and evaluated. It is also known that the TSH measurement method can affect the results. In a study conducted in Buenos Aires, it was reported that the number of newborns with TSH >5 mIU/L with standard immunoflurometric measurement was 2.7%, while this rate was 10 times (30%) higher when measured by the immunoradiometric method (22). There are at least 13 analysis methods for TSH screening in the United States Centers for Disease Control and Prevention program. Considering that there is a difference of up to 15% between these methods, it is seen that TSH threshold values can be easily affected by the measurement method (23). The results of this study revealed that serum TSH levels in postnatal 4th–6th days in newborn cases are not suitable for evaluating the iodine status of mothers. In the study conducted on 42 newborns by Kurtoğlu et al. (24) in Kayseri, Turkey in 1995, they found no iodine deficiency in babies with high TSH levels in their cord blood. They emphasized that the high TSH detected in the cord blood in the moderate to severe iodine deficiency region may be associated with primary congenital hypothyroidism, maternal iodine overload at birth, or antithyroid drugs. In our study, 4 babies (1.2%) were diagnosed with congenital hypothyroidism, and the etiological cause of these babies was not revealed. It was thought that the transplacental passage of TSH receptor-blocking antibodies, exposure to environmental endocrine disruptors, or other reasons that were not included in the evaluation in this study, may have affected the TSH levels in neonatal cases (25, 26).
It is known that the use of iodine-containing antiseptics in the umbilical cord care of the newborn may affect the TSH level (27). Lin et al. (28) reported that false-positive high TSH levels were more common in newborns whose umbilical cord care was made with a povidone-iodine-containing antiseptic than babies whose care was with alcohol or triple dye (4.6% and 0%, respectively, 7). In our study, free T4 levels were found to be significantly lower, and TSH levels and urinary IC were found to be significantly higher in babies who underwent umbilical cord care with iodine-containing antiseptic compared to babies who did not. and findings were evaluated following the literature information.
There is very little iodine in the thyroid gland of newborn babies, so newborns need iodine in breast milk for normal physical and neurological development (5). The most important determinant of iodine in breast milk is the iodine intake of mothers, and the median BMIC gives an idea about the iodine status (5). Ordookhani et al. (29) found a significant positive relationship between breast milk and urine, between newborn urine and breast milk, and between maternal and newborn UIC in 48 healthy term newborns and their mothers. In our study, the median BMIC was 138 μg/L and UIC was similar, and there was a weak-moderate positive correlation between BMIC and neonatal UIC.
The most important limitation in our study is that while evaluating the iodine status of newborn babies, iodine antiseptics used during delivery were ignored. Although no participant with high iodine level was found in our study, no comment could be made on the elevation of TSH due to possible iodine overload at birth. The fact that other factors that may affect UIC were not evaluated (daily water consumption, drugs other than iodine, etc.) and the neonatal TSH level was determined in serum instead of capillary blood were considered as limitations since they create difficulties in interpreting the data. Also, the cross-sectional character of the study limits the cause-effect relationship.
In conclusion, UIC were found above 100 μg/L in all newborns and their mothers in this study. The ratio of babies with a TSH>10 mIU/L suggesting mild iodine deficiency is 19%, and this mentions that TSH levels are also affected by factors other than iodine, and the role of serum TSH level in evaluating iodine status in the newborn period should be investigated in larger series and in cases where iodine contact is completely stopped.
Footnotes
Ethical Committee Approval: Ethical committee approval was received from the Clinical Ethics Committee of Aydın Adnan Menderes University (Date: 2006, no: 00144).
Informed Consent: Written informed consent was obtained from all participants who participated in this study.
Peer-review: Externally peer-reviewed.
Conflict of interest: The authors have no conflicts of interest to declare.
Author Contributions: Concept-M.K.T., T.Ü.; Design - T.Ü., A.A., A.A..; Supervision - M.K.T., T.Ü., P.Ö.K.; Funding - M.K.T., T.Ü., P.Ö.K.; Materials - M.K.T., T.Ü., P.Ö.K.; Data Collection and/or Processing - A.A., A.A., P.Ö.K.; Analysis and/or Interpretation - A.A., A.A., P.Ö.K., M.K.T.; Literature Review - A.A., A.A., P.Ö.K.; Writing - A.A., A.A., P.Ö.K.; Critical Review - M.K.T., A.A.
Financial Disclosure: This study was supported by Adnan Menderes University Scientific Research Projects (TPF-07010).
References
- 1.Pearce EN. Iodine deficiency in children. Endocr Dev. 2014;26:130–8. doi: 10.1159/000363160. [DOI] [PubMed] [Google Scholar]
- 2.Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 2008;372:1251–62. doi: 10.1016/S0140-6736(08)61005-3. [DOI] [PubMed] [Google Scholar]
- 3.Erdogan MF, Agbaht K, Altunsu T, et al. Current iodine status in Turkey. J Endocrinol Invest. 2009;32:617–22. doi: 10.1007/BF03346519. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. Geneva: World Health Organization; 2001. [Google Scholar]
- 5.Dror DK, Allen LH. Iodine in Human Milk: A Systematic Review. Adv Nutr. 2018;9:347–57. doi: 10.1093/advances/nmy020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wainwright P, Cook P. The assessment of iodine status - populations, individuals, and limitations. Ann Clin Biochem. 2019;56:7–14. doi: 10.1177/0004563218774816. [DOI] [PubMed] [Google Scholar]
- 7.Hedayati M, Khazan M, Yaghmaee P, Yeghaneh MZ, Behdadfar L, Daneshpour MS. Rapid microwave digestion and microplate reading format method for urinary iodine determination. Clin Chem Lab Med. 2011;49:281–4. doi: 10.1515/CCLM.2011.053. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization United Nations Children’s Fund & International Council for the Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. 3rd ed. Geneva: World Health Organization; 2007. [Google Scholar]
- 9.Delange F. The disorders induced by iodine deficiency. Thyroid. 1994;4:107–28. doi: 10.1089/thy.1994.4.107. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of P; Rose SR, et al. Section on E. Update of newborn screening and therapy for congenital hypothyroidism. Pediatrics. 2006;117:2290–303. doi: 10.1542/peds.2006-0915. [DOI] [PubMed] [Google Scholar]
- 11.Leger J, Olivieri A, Donaldson M, et al. European Society for Paediatric Endocrinology consensus guidelines on screening, diagnosis, and management of congenital hypothyroidism. J Clin Endocrinol Metab. 2014;99:363–84. doi: 10.1210/jc.2013-1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erdogan G, Erdogan MF, Emral R, et al. Iodine status and goiter prevalence in Turkey before mandatory iodization. J Endocrinol Invest. 2002;25:224–8. doi: 10.1007/BF03343994. [DOI] [PubMed] [Google Scholar]
- 13.Oguz Kutlu A, Kara C. Iodine deficiency in pregnant women in the apparently iodine-sufficient capital city of Turkey. Clin Endocrinol (Oxf) 2012;77:615–20. doi: 10.1111/j.1365-2265.2012.04440.x. [DOI] [PubMed] [Google Scholar]
- 14.Isiklar Ozberk D, Kutlu R, Kilinc I, Kilicaslan AO. Effects of mandatory salt iodization on breast milk, urinary iodine concentrations, and thyroid hormones: is iodine deficiency still a continuing problem? J Endocrinol Invest. 2019;42:411–8. doi: 10.1007/s40618-018-0930-0. [DOI] [PubMed] [Google Scholar]
- 15.Kasap B, Akbaba G, Yeniceri EN, et al. Adequate iodine levels in healthy pregnant women. A cross-sectional survey of dietary intake in Turkey. Saudi Med J. 2016;37:698–702. doi: 10.15537/smj.2016.6.13887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anaforoglu I, Algun E, Incecayir O, Topbas M, Erdogan MF. Iodine status among pregnant women after mandatory salt iodisation. Br J Nutr. 2016;115:405–10. doi: 10.1017/S0007114515004559. [DOI] [PubMed] [Google Scholar]
- 17.Andersson M, de Benoist B, Rogers L. Epidemiology of iodine deficiency: Salt iodisation and iodine status. Best Pract Res Clin Endocrinol Metab. 2010;24:1–11. doi: 10.1016/j.beem.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Zimmermann MB, Aeberli I, Torresani T, Burgi H. Increasing the iodine concentration in the Swiss iodized salt program markedly improved iodine status in pregnant women and children: A 5-y prospective national study. Am J Clin Nutr. 2005;82:388–92. doi: 10.1093/ajcn/82.2.388. [DOI] [PubMed] [Google Scholar]
- 19.McElduff A, McElduff P, Gunton JE, Hams G, Wiley V, Wilcken BM. Neonatal thyroid-stimulating hormone concentrations in northern Sydney: Further indications of mild iodine deficiency? Med J Aust. 2002;176:317–20. doi: 10.5694/j.1326-5377.2002.tb04431.x. [DOI] [PubMed] [Google Scholar]
- 20.Rajatanavin R. Iodine deficiency in pregnant women and neonates in Thailand. Public Health Nutr. 2007;10:1602–5. doi: 10.1017/S1368980007360990. [DOI] [PubMed] [Google Scholar]
- 21.Ittermann T, Volzke H, Krey A, et al. Median urinary iodine concentration reflected sufficient iodine supply in neonates from Northeast Germany in 2005–2006. Eur J Nutr. 2019;58:1815–20. doi: 10.1007/s00394-018-1731-0. [DOI] [PubMed] [Google Scholar]
- 22.Gruneiro-Papendieck L, Chiesa A, Mendez V, Bengolea S, Prieto L. Neonatal TSH levels as an index of iodine sufficiency: differences related to time of screening sampling and methodology. Horm Res. 2004;62:272–6. doi: 10.1159/000081786. [DOI] [PubMed] [Google Scholar]
- 23.Li M, Eastman CJ. Neonatal TSH screening: is it a sensitive and reliable tool for monitoring iodine status in populations? Best Pract Res Clin Endocrinol Metab. 2010;24:63–75. doi: 10.1016/j.beem.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Kurtoğlu S, Akcakuş M, Güneş T, Kiriş A. Urinary iodine levels of the term newborns in Kayseri Province. Erciyes Med J. 2002;24:69–75. [Google Scholar]
- 25.de Cock M, de Boer MR, Govarts E, et al. Thyroid-stimulating hormone levels in newborns and early life exposure to endocrine-disrupting chemicals: Analysis of three European mother-child cohorts. Pediatr Res. 2017;82:429–37. doi: 10.1038/pr.2017.50. [DOI] [PubMed] [Google Scholar]
- 26.Bucci I, Giuliani C, Napolitano G. Thyroid-stimulating hormone receptor antibodies in pregnancy: Clinical relevance. Front Endocrinol (Lausanne) 2017;8:137. doi: 10.3389/fendo.2017.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Findik RB, Yilmaz G, Celik HT, Yilmaz FM, Hamurcu U, Karakaya J. Effect of povidone-iodine on thyroid functions and urine iodine levels in caesarean operations. J Matern Fetal Neonatal Med. 2014;27:1020–2. doi: 10.3109/14767058.2013.847417. [DOI] [PubMed] [Google Scholar]
- 28.Lin CP, Chen W, Wu KW. Povidone-iodine in umbilical cord care interferes with neonatal screening for hypothyroidism. Eur J Pediatr. 1994;153:756–8. doi: 10.1007/BF01954494. [DOI] [PubMed] [Google Scholar]
- 29.Ordookhani A, Pearce EN, Hedayati M, et al. Assessment of thyroid function and urinary and breast milk iodine concentrations in healthy newborns and their mothers in Tehran. Clin Endocrinol (Oxf) 2007;67:175–9. doi: 10.1111/j.1365-2265.2007.02857.x. [DOI] [PubMed] [Google Scholar]


