Abstract
Background
Patients with obesity are at increased risk of developing severe COVID-19. The pandemic has caused delays in preoperative preparation, progression, and completion of bariatric surgeries.
Objectives
The aim of this study was to evaluate the impact of COVID-19 restrictions on bariatric surgery patients and assess their concern of COVID-19 as they continue the preoperative process.
Setting
Philadelphia, Pennsylvania
Methods
A questionnaire was administered to patients to assess the impact of COVID-19 on their weight loss goals, physical activity, and diet. Time points assessed were initial bariatric consultation (T1), as well as the beginning (T2), and the end (T3) of lockdown restrictions in the region.
Results
Seventy-four participants were invited and 50 completed the survey, for a response rate of 67.6%. The average age of participants was 44.1 years. Two-thirds of patients reported significant concern that COVID-19 would affect their weight loss goals. Patients reported significant improvements in their diet from T1 to T2 (P < .01). However, at T3, some patients returned to behaviors held at T1, with snacking behaviors significantly increasing between T2 and T3 (P < .01). Physical activity decreased in 60% of patients between T2 to T3. The vast majority (90%) wanted to have their surgery as soon as possible; 56% reported low levels of concern for COVID-19 infection.
Conclusion
Bariatric patients were highly motivated to proceed with bariatric surgery despite the risks imposed by the pandemic.
Key words: Bariatric surgery, Obesity, COVID-19, SARS-CoV-2, Elective surgery
Healthcare systems world-wide responded to the rising rates of COVID-19–related hospital admissions and resulting burden on hospital infrastructure by reorganizing daily operations. By mid-March 2020, many hospitals throughout the United States enacted policy to postpone procedures deemed elective, including bariatric procedures, to liberate in-patient beds and reduce nosocomial spread of the virus among patients and staff. These and other strategies also were enacted to reduce the overall admission rate and decrease length of stay for patients at greatest risk for severe COVID-19. This included patients with obesity, who are at greater risk of developing severe manifestations of COVID-19 and experience higher mortality rates [1].
Since the initial postponement of bariatric procedures in the spring of 2020, programs have used several strategies to care for the resulting backlog of patients [2]. Telemedicine has been used to help patients complete their preoperative consultations with good success [3]. While telemedicine is a viable alternative to in-person visits for the preoperative psychological evaluation or medical weight management sessions, other assessments are procedurally based and require in-person visits. In many hospitals, patients have been required to receive a negative COVID test before these procedures are undertaken. Patients who test positive for COVID-19 are often delayed from surgery until they have fully recovered from the virus, creating a further backlog of patients. Others appear to be reluctant to present for these assessments and enter an environment that may increase their risk of exposure to the virus. Both scenarios further challenge the return to normal operations of a bariatric program.
With these observations as a framework, the present study was undertaken to investigate patients’ perceptions of the effects of the COVID-19 pandemic on their progress during the preoperative period as well as their willingness to return to the hospital for surgery.
Methods
A questionnaire was administered to candidates for bariatric surgery who had their surgical procedures or care rescheduled or canceled due to the COVID-19 pandemic (Supplementary Table 1). Patients who were in the process of undergoing bariatric care between March 1, 2020, and June 15, 2020, were included. This period marked the timeframe of local lockdown measures and suspension of elective surgeries at our institution. Eligible patients were contacted for a single phone interview between July 20 and August 6, 2020. Informed consent was obtained, and the survey administered. The study was approved by our institutional review board (protocol 27374). Data were collected and managed using the REDCap data collection tool (Research Electronic Data Capture, Nashville, TN) [4,5].
The survey consisted of 3 main sections: (1) how patients felt about COVID-19 as it relates to their bariatric care; (2) how their physical exercise habits have changed during the pandemic; and (3) how their dietary habits have changed during the pandemic. Questions assessing the impact of the pandemic on patients’ weight loss efforts, their concern with the impact of the pandemic, and their opinion of how soon they wanted to have surgery were answered on a 5-point Likert scale [6]. Participants reported their weight, current level of physical activity, and diet/eating behaviors. To assess physical activity, respondents reported on the frequency and duration of exercise in the past week. Diet and eating behaviors were assessed by the self-reported engagement in relevant habits determined by our bariatric diet and nutrition team to be of particular relevance. These included the number of meals consumed each day, meals skipped, snacking, eating sweets/dessert, eating fast food, consumption of liquid calories, consumption of soda, consumption of coffee, episodes of emotional eating, and eating past fullness. Participants were asked to answer these questions with 3 different time points in mind: initial visit to the bariatric surgery program (T1); prior to the onset of COVID-19 restrictions (March 1; T2); and the end of the lockdown period (June 15; T3).
Categorical data were expressed as absolute and relative frequency. Categorical variables were compared with the use of the Pearson’s χ2 test. Nonnormally distributed variables were compared using Kruskal-Wallis test. Pairwise analysis was conducted through a Wilcoxon signed-rank test using Bonferroni correction. All statistical tests were 2-tailed and P < .05 were considered statistically significant. All statistical analyses were performed using R with the tidyverse and stats packages [7,8].
Results
We contacted 74 eligible patients and 50 completed the survey (67.6% response rate). The majority (88%) were female and mean age of participants was 44.1 years. As shown in Table 1 , 50% of respondents were Black, non-Hispanic; 42% Hispanic; and 6% White, non-Hispanic. The most common co-morbidities were obstructive sleep apnea (54%), hypertension (50%), diabetes (48%), asthma (34%), and gastroesophageal reflux (GERD) (34%). Osteoarthritis, hyperlipidemia, and depression were seen in smaller percentages of respondents.
Table 1.
Demographics and co-morbidities of study participants
| Black, non-Hispanic (n = 28) | Hispanic (n = 18) | White, non-Hispanic (n = 3) | Other (n = 1) | Total (n = 50) | |
|---|---|---|---|---|---|
| Age, yr, mean (SD) | 45.0 (12.3) | 43.4 (9.4) | 44.3 (9.6) | 38 (-) | 44.1 (10.7) |
| Sex | |||||
| Female | 27 (62.7) | 12 (66.7) | 3 (100.0) | 1 (100.0) | 43 (86.0) |
| Male | 1 (14.3) | 6 (33.3) | 7 (14.0) | ||
| Baseline BMI, kg/m2, mean (SD) | 51.6 (10.5) | 45.9 (6.7) | 46.7 (1.6) | 47.0 (-) | 48.8 (9.0) |
| Baseline weight, kg, mean (SD) | 138.6 (29.1) | 124.6 (16.0) | 123.8 (12.5) | 114.5 (-) | 131.3 (24.1) |
| Co-morbidities | |||||
| Obstructive sleep apnea | 16 (57.1) | 11 (61.1) | 27 (54.0) | ||
| Hypertension | 17 (60.7) | 8 (44.4) | 2 (66.7) | 27 (54.0) | |
| Diabetes | 13 (46.4 | 9 (50.0) | 2 (66.7) | 24 (48.0) | |
| Osteoarthritis | 7 (25.0) | 3 (16.7) | 10 (20.0) | ||
| Hyperlipidemia | 9 (32.1) | 3 (16.7) | 2 (66.7) | 14 (28.0) | |
| Cardiovascular disease | 3 (10.7) | 2 (11.1) | 5 (1.0) | ||
| Asthma | 11 (39.3) | 6 (33.3) | 17 (34.0) | ||
| Depression | 7 (25.0) | 3 (16.7) | 1 (33.3) | 11 (22.0) | |
| GERD | 14 (50.0) | 3 (16.7) | 1 (33.3) | 18 (36.0) | |
| Hyperthyroidism | 2 (11.1) | 2 (4.0) | |||
| Hypothyroidism | 4 (22.2) | 4 (8.0) | |||
| Crohn's disease | 1 (3.5) | 1 (2.0) | |||
| Irritable bowel syndrome | 1 (3.5) | 1 (2.0) | |||
| Iron deficiency anemia | 3 (10.7) | 1 (5.6) | 4 (8.0) | ||
| Hiatal hernia | 2 (7.1) | 1 (33.3) | 3 (6.0) | ||
| Umbilical hernia | 1 (3.5) | 1 (2.0) |
BMI = body mass index; GERD = gastroesophageal disease.
Data are represented as no. (%) unless otherwise specified.
BMI and weight
BMI and weight were evaluated at 3 different time points: T1 (initial visit), T2 (March 1), and T3 (June 15). The mean duration between T1 (initial visit) and T2 (June 15) was 292.14 (SD 251.32) days, and the duration between T2 (March 1) and T3 (June 15) was 107 days. Between T1 (initial visit) and T2 (March 1), patients experienced a decrease in BMI from 48.82 ± 8.95 at T1 (initial visit) to 47.32 ± 8.75 at T2 (March 1) with a 6.25% ± 9.82 excess weight loss (EWL) during that time. From T2 (March 1) to T3 (June 15), mean BMI increased to 48.04 ± 8.85 (−3.51% ± 8.10 EWL). Between T1 (initial visit) and T3 (June 15th), the overall mean %EWL was 2.74% ± 10.03. None of the changes were statistically significant.
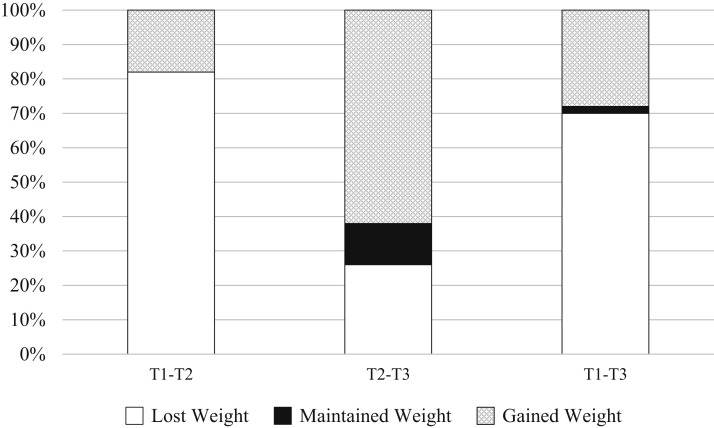
Fig. 1 displays the percentage of patients that lost weight, maintained weight, and gained weight at each time point. Between T1 (initial visit) and T2 (March 1), 42 patients (84%) reported weight loss, while 9 patients (18%) reported weight gain. Between T2 (March 1) and T3 (June 15), 13 patients (26%) reported weight loss, 6 patients (12%) reported maintenance of weight, and 31 patients (62%) reported weight gain.
Fig. 1.
Weight change from initial bariatric visit to end of shelter-in-place restrictions.
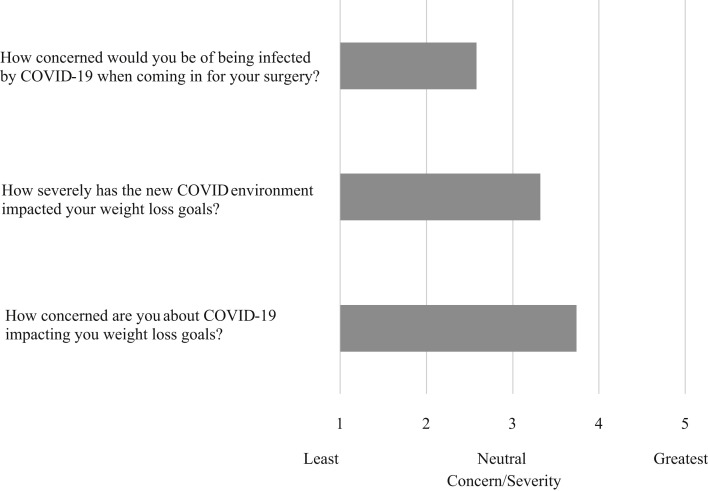
COVID-19
Fig. 2 presents the mean response to 3 of the questions assessing the effects of COVID-19 on change in weight. The following were assessed: level of concern of contracting COVID-19 when presenting for surgery, perceived severity of the impact of the new COVID-19 environment on weight loss goals, and level of concern about COVID-19 impacting weight loss goals. Responses were assessed on a 5-point Likert scale with 1 representing least concern/severity and 5 representing greatest concern/severity. When asked how the COVID-19 environment impacted their current weight loss goals, 48% of respondents reported a score ≥4 indicating substantial impact on their ability to achieve their goals. When asked about the level of concern regarding the COVID-19 pandemic impacting their future weight loss goals, 66% of participants reported a score ≥4, indicating great concern in their abilities to achieve their weight loss goals.
Fig. 2.
Participant survey responses regarding concern raised by COVID-19 on bariatric program progression.
When asked how soon patients wanted to schedule their surgery, 90% reported a preference to schedule their surgery as soon as possible. Only 9% preferred to wait an additional 3–6 months due to fears related to COVID-19. Moreover, of those who did not want to delay surgery (n = 45), the majority (53%) cited health reasons (related to their obesity) and 36% reported an urgency to be done with surgery. When asked about the level of concern about contracting COVID-19 when coming in for surgery, 25 out of 45 (56%) reported a score ≤2, suggesting low levels of concern. The great majority (90%) stated that they would return to the healthcare setting even prior to receiving the COVID-19 vaccination. At the time of the survey, no study participants had tested positive for COVID-19.
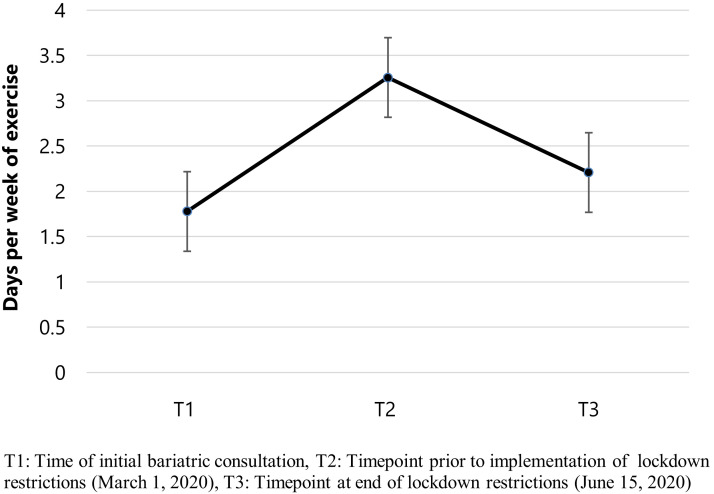
Physical activity
The plurality (60%) of patients reported that they were exercising less than they had been prior to lockdown; 22% reported that they were exercising the same amount and 18% reporting that they were exercising more. Fig. 3 shows the mean frequency per week that patients reported exercising at T1 (initial visit), T2 (March 1), and T3 (June 15). Patients exercised 1.78 ± 1.41 times a week at T1 (initial visit), 3.26 ± 1.33 times at T2 (March 1), and 2.21 ± 1.61 times at T3 (June 15) (P < .01). In addition to frequency of exercise, length of exercise sessions also was assessed. A similar pattern was observed, with patients having shorter sessions at T1 (initial visit), longer sessions at T2 (March 1), and reverting to shorter sessions at T3 (June 15) during lockdown restrictions. At T1 (initial visit), 66% of patients reported exercise sessions <30 minutes, 26% reported sessions between 30–60 minutes, and 8% reported sessions >60 minutes. At T2 (March 1), 40% of patients reported sessions <30 minutes long, while 36% reported sessions between 30–60 minutes, and 24% reported sessions >60 minutes. At T3 (June 15), 60% of patients reported exercise sessions <30 minutes in length, 28% reported sessions between 30–60 minutes, and 12% reported exercise sessions l>60 minutes.
Fig. 3.
Mean days per week of exercising at T1, T2, and T3 time points by study participants.
Diet and eating behaviors
Table 2 displays questions related to diet and eating behaviors. The frequency per day of the following were assessed: number of meals consumed each day, meals skipped, snacking, eating sweets/dessert, eating fast food, consumption of liquid calories, consumption of soda, consumption of coffee, episodes of emotional eating, and eating past fullness. The mean response for each category was calculated for each time point. For all categories, with the exception of number of meals per day, there was a significant decline in frequency between T1 (initial visit) and T2 (March 1) (P < .01). Between T2 (March 1) and T3 (June 15) there was an increase in all the variables but only snacking was significant (P < .01).
Table 2.
Mean frequency per day of participation in dietary habits of interest
| T1 | T2 | T3 | P value∗ | |
|---|---|---|---|---|
| Meals per day | 2.66 | 2.76 | 2.80 | .38 |
| Skipping meals | .13† | .00 | .06 | <.01 |
| Snacking | 1.84† | .27‡ | .94§ | <.01 |
| Eating sweets | .91† | .13 | .34§ | <.01 |
| Eating fast food | .53† | .05 | .19§ | <.01 |
| Drinking liquid calories | 1.72† | .27 | .35§ | <.01 |
| Drinking soda | 1.5† | .13 | .2§ | <.01 |
| Drinking coffee | 1.02† | .38 | .4§ | .10 |
| Emotionally eating | 1.06† | .11 | .41§ | <.01 |
| Eating past fullness | 1.05† | .18 | .47¶ | <.01 |
T1 = time of initial bariatric consultation; T2 = timepoint prior to implementation of lockdown restrictions (March 1, 2020); T3 = timepoint at end of lockdown restrictions (June 15, 2020).
Post hoc pairwise comparisons using Wilcoxon rank sum test performed between T1 and T2, T2 and T3, and T1 and T3.
Kruskal-Wallis H Test performed on all time points.
T1 versus T2, P < .01.
T2 versus T3, P < .01.
T1 versus T3, P < .01.
T1 versus T3, P < .05.
Discussion
In bariatric surgery patients who had their surgeries delayed by the pandemic, we observed self-reported weight loss in the first months, but weight gain as the delay moved into late spring. Prior to COVID-19 related restrictions, patients reported a mean BMI reduction of 1.5 kg/m2 (6.25% ± 9.82 EWL). However, once COVID-19 restrictions were enacted, 62% of participants reporting weight gain and the progress previously achieved in BMI reduction decreased by 52%. The reasons behind re-gaining of weight during this lockdown period are likely multifactorial. Respondents indicated that the COVID-19 restrictions negatively impacted their eating habits, physical activity levels, and psychological wellbeing. However, despite gaining weight, participants reported continuation of healthy lifestyle changes after their initial consultation.
Prior to surgery, patients are instructed on the dietary and behavioral changes believed to promote maximum weight loss, prevent nutritional deficiencies, and decrease unwanted gastrointestinal side effects. While most patients reported successful implementation of these behaviors after their initial consultation, there was an overall decline in adherence to these changes during the period of COVID-19 restrictions. They reported an increase in snacking, eating sweets, eating fast food, drinking liquid calories, drinking soda, drinking coffee, emotionally eating, and eating past fullness after the COVID-19 restrictions were implemented. They frequently cited confinement, boredom, and increased access to unhealthy food as potential reasons for not adhering to dietary recommendations. These observations are consistent with other studies which have reported reduced consumption of fruits and vegetables and an increased consumption of snacks, frozen or shelf-stable foods, and unhealthy foods during the pandemic [9,10].
Engagement in physical activity is an important part of long-term weight control. Patients who increase their physical activity prior to bariatric surgery have been found to experience larger postoperative weight losses [11]. Physical activity prior to surgery improves cardiopulmonary capacity, increases lean muscle mass, and improves cardiometabolic risk factors [12]. In this study, patients who initially reported significant increases in frequency and duration of physical activity in preparation for surgery reported a decrease in these behaviors during the early days of the lockdown. Patients attributed the decline in their physical activity to the inability to exercise outdoors, visit gym facilities, or exercise with others. Bariatric surgery patients often over report their physical activity levels compared with objective assessment [13]. It is possible that our patients’ self-reported physical activity also was an overestimation of their true activity. Objective assessment of activity levels during this time would have provided a more reliable assessment of how these behaviors changed in relationship to the pandemic.
Local lockdown measures also have had an impact on psychosocial well-being. Not surprisingly, persons with clinically severe obesity also have reported untoward effects on their psychosocial status [14]. Some of this may have been exacerbated by early, erroneous mass media reports that persons with obesity were more likely to contract COVID-19. These reports are largely now seen as yet another example of how persons with obesity are often stigmatized for their disease. Subsequent studies have indicated that excess weight does not leave individuals more susceptible to contracting the virus, but rather may contribute to more severe forms of the disease and increased risk of death [15]. Despite these risks, patients surveyed were willing and eager to return to a health care setting and have their care continued, with 90% indicating that they desired to undergo surgery as soon as possible and even if not vaccinated against the virus. For many of the participants, the potential risk of COVID infection did not outweigh the desire to have surgery as soon as possible. Fifty-three percent indicated that their obesity-related co-morbidities were significantly hindering their quality of life and that they were afraid of the continued decline in their health if they were not able to treat their obesity in a timely fashion. More than half of respondents reported low concern about being exposed to the virus in the hospital. Only 20% reported extreme levels of concern. Interestingly, patients voiced that their levels of stress surrounding their bariatric surgery were also related to the unknown timing of the continuation of their care. Many patients expressed worry that their weight gain during lockdown would disqualify them from surgery. As we continue to live with the threat of COVID-19, patients will rightfully feel concerned about possible infection. Articulation of clear and transparent protocols designed to minimize the risk of exposure during preoperative consultations, perioperative care, and postoperative follow-up will be key in assuring patient wellbeing and safety.
This study presents bariatric patients’ perspectives and difficulties with regard to COVID-19 and the associated lockdown. Providers need to be aware of these challenges to better serve their patients and provide optimal care. With the reduction of in-person bariatric clinic appointments, practices should encourage telehealth encounters, particularly with dieticians, to assist patients adapt to challenges specifically posed by COVID-19. In the face of restrictions to outdoor movement and need for social distancing, bariatric practices can provide patients with physical activity regimens that can be performed in or around the home. The increased risk of persons with obesity having severe disease from COVID-19 stresses the importance of prioritizing bariatric surgery, and ensuring that it is enacted with appropriate safety measures in place.
The COVID-19 pandemic has disproportionally impacted individuals from underserved communities [16,17]. The present study was undertaken in a health care system located in one of the most underserved areas of Philadelphia, where rates of obesity and its co-morbidities are among the highest, and life expectancy among the lowest, in the city. Close to 85% of patients served by our hospital system are covered by public insurance and 83% of our patients are Black, Hispanic, or from other minority groups. Those who are employed often held jobs that made them ‘essential workers’ who had to be physically present to allow for continuation of critical services. The impact of the interaction of obesity and COVID-19 in these communities, anecdotally seen at present and likely to be confirmed by epidemiologic studies on morbidity and mortality, is likely to be a sobering reminder of the need for novel public health strategies to protect the health and well-being of the most vulnerable of our population.
This survey has provided novel information on the impact of the pandemic on the delivery of preoperative bariatric care. The cohort we spoke to also represent a diverse population that were willing to offer a unique insight and a perspective of the challenges faced by patients from a dense, underserved urban area. However, the study has limitations. First, the reliance on both self-reported and in-clinic weights is a limitation. In addition, it is possible that more than 1 scale was used in the clinic. While in-clinic scales are calibrated to one another, they are not calibrated with personal scales. Second, as participants were asked to report their dietary and physical activity habits dating back to their initial bariatric evaluation, these responses are susceptible to recall bias. Furthermore, reliance on retrospective self-report, rather than objective measurement, raises the potential concern for response bias. Third, the survey questions investigating dietary habits were derived from questions used by our registered dieticians during clinical interactions with our patients and are not validated against patient-reported outcomes measures. Fourth, our results may be limited in generalizability as our study population is reflective of individuals living in an urban environment, with significant baseline disease burden, and who predominately identify as Black and Hispanic. Finally, the sample size was relatively small with 50 participants, which may have left us underpowered to detect statistically significant differences.
The COVID-19 pandemic continues to be an evolving situation with recurrent surges, emerging mutant strains, and varying public health responses world-wide. The effect of these factors on healthcare delivery to patients seeking bariatric surgery and care are difficult to anticipate. While these times prove challenging, more work is needed to assess and maintain the quality of the bariatric process in spite of the difficulties imposed by the pandemic.
Conclusion
Patients pursuing bariatric surgery have had their care postponed and rescheduled due to the risks and constraints presented by the COVID-19 pandemic. Those subject to lockdown restrictions during the pre-operative period have been challenged by difficulty in maintaining healthy nutritional habits as well as physical activity goals, resulting in weight gain – though not to pre-consultation levels. Despite the additional risks posed by the on-going COVID-19 pandemic, patients remain in favor of undergoing bariatric surgery during this period. To enable continued care for this population willing to undergo surgery, communication of risks as well as procedures that will be enacted to minimize their risk with respect to COVID-19 are critical.
Disclosures
Dr. Sarwer currently has grant funding from the National Institute of Diabetes, Digestive, and Kidney Disease (R01-DK-108628-01), National Institute of Dental and Craniofacial Research (R01 DE026603), Department of Defense, as well as the Commonwealth of Pennsylvania (PA CURE). He has consulting relationships with Ethicon and Novo Nordisk. All other authors report no relevant disclosures.
Footnotes
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.soard.2021.05.026.
Supplementary materials
References
- 1.Hussain A., Mahawar K., Xia Z., Yang W., EL-Hasani S. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020;14:295–300. doi: 10.1016/j.orcp.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Rubino F., Cohen R.V., Mingrone G., le Roux C.W. Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes Endocrinol. 2020;8(7):640–648. doi: 10.1016/S2213-8587(20)30157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarwer D.B. Mask wearing and interpersonal interactions. CommonHealth. 2020;1(3):153–156. https://tuljournals.temple.edu/index.php/commonhealth/article/view/422 Available from: [Google Scholar]
- 4.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22(140):55. [Google Scholar]
- 7.Wickham H., Averick M., Bryan J. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686. [Google Scholar]
- 8.Team R Development Core. R: A language and environment for statistical computing. R Found Stat Comput 2018;2. Available from: https://www.R-project.org. Accessed December 1, 2020.
- 9.Pellegrini M., Ponzo V., Rosato R. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7):2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jayawardena R., Misra A. Balanced diet is a major casualty in COVID-19. Diabetes Metab Syndr. 2020;14(5):1085–1086. doi: 10.1016/j.dsx.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baillot A., Vallée C.A., Mampuya W.M. Effects of a pre-surgery supervised exercise training 1 year after bariatric surgery: a randomized controlled study. Obes Surg. 2018;28(4):955–962. doi: 10.1007/s11695-017-2943-8. [DOI] [PubMed] [Google Scholar]
- 12.Tabesh M.R., Maleklou F., Ejtehadi F., Alizadeh Z. Nutrition, physical activity, and prescription of supplements in pre- and post-bariatric surgery patients: a practical guideline. Obes Surg. 2019;29(10):3385–3400. doi: 10.1007/s11695-019-04112-y. [DOI] [PubMed] [Google Scholar]
- 13.Possmark S., Sellberg F., Willmer M., Tynelius P., Persson M., Berglind D. Accelerometer-measured versus self-reported physical activity levels in women before and up to 48 months after Roux-en-Y gastric bypass. BMC Surg. 2020;20(1):1–10. doi: 10.1186/s12893-020-00699-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Youssef A., Cassin S.E., Wnuk S., Leung S., Jackson T., Sockalingam S. The impact of COVID-19 pandemic on bariatric patients’ self-management post-surgery. Appetite. 2021;162:105166. doi: 10.1016/j.appet.2021.105166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson K., Hollin I., Palumbo A., Spitzer J., Sarwer D.B. An ecologic analysis of comorbidities in patients with COVID-19 in Philadelphia and New York City. CommonHealth. 2020;1(3):85–92. [Google Scholar]
- 16.Azar K.M.J., Shen Z., Romanelli R.J. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 17.Millett G.A., Jones A.T., Benkeser D. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.