Abstract
Dual left anterior descending artery (LAD) is a rare phenomenon that occurs in less than one percent of the population. To date, 12 variants have been identified. Proper identification of coronary vessels is crucial in emergent situations that require prompt action, such as percutaneous coronary intervention (PCI). We propose that our case highlights a novel 13th (type XIII) variant. We present the case of a 57-year-old African American woman with a past medical history of hypertension, glaucoma, cerebral vascular accident, dyslipidemia who presented to the ED complaining of atypical chest pain for one day duration. Electrocardiography showed normal sinus rhythm at 60 beats per minute (bpm), normal axis, normal intervals, no acute ischemic changes, and an isolated T wave inversion in DIII. Cardiac markers were within normal limits. The patient was started on aspirin 81mg, atorvastatin 40mg, and restarted on amlodipine 5mg. Echocardiography showed a left ventricular ejection fraction (LVEF): 65%, normal right ventricular size and systolic function, mild mitral valve regurgitation, and mild aortic regurgitation. Computed tomographic (CT) angiography showed a novel subtype of dual LAD, the left circumflex and right coronary arteries were patent. The patient was discharged once stabilized and advised to follow up with cardiology. Dual LAD describes a rare anatomic variant in which two coronary branches, known as short and long LAD arteries, supply the territory normally supplied by the solitary LAD artery. To date, 12 variants of dual LAD, classified by origin and course of the short and long LAD arteries, have been described in the literature. To the best of our knowledge, the current case describes a novel subtype of dual LAD, variant XIII. The LAD originates as usual from the left main coronary artery (LMCA) and initially runs in the anterior interventricular groove for a short course before bifurcating into two long LADs which both leave the interventricular groove and course out to the apex. One of the vessels courses laterally and the other courses medially of the interventricular groove. It is pertinent to identify the coronary vessels accurately before certain interventions are taken. Acknowledgement of this phenomenon can help guide accurate management in the future for patients with this condition.
Keywords: ct coronary angiography, dual lad, acs, atypical chest pain, anatomical variant, lad variant, cardiac anatomy
Introduction
Dual left anterior descending artery (LAD) is a rare phenomenon that occurs in less than one percent of the population [1]. To date, 12 variants have been identified [2]. Proper identification of coronary vessels is crucial in emergent situations that require prompt action, such as percutaneous coronary intervention (PCI). We propose that our case highlights a novel 13th (type XIII) variant. We present the case of a middle-aged black female who presented to the ED complaining of substernal non-radiating atypical chest pain after witnessing an altercation. Upon admission cardiac imaging revealed a novel subtype of dual LAD. The patient was discharged once stabilized and advised to follow up with cardiology. It is pertinent to identify the coronary vessels accurately before certain interventions are taken. Acknowledgement of this phenomenon can help guide accurate management in the future for patients with this condition.
Case presentation
The patient is a 57-year-old African American woman with a past medical history of hypertension, glaucoma, cerebral vascular accident (two times, once in 2014 and once in 2016, with no residual deficits), and dyslipidemia who presented to the emergency department (ED) complaining of atypical chest pain for one day’s duration. The patient stated that her chest pain started after she witnessed an altercation. She mentioned the pain was substernal, tight/pressure-like in nature, non-radiating, worse with anxiety, and 6/10 in intensity. Her new pain came in the setting of vertigo (for the past four months), lightheadedness, and difficulty ambulating. She denied any alleviating symptoms and the rest of the review of systems was non-pertinent.
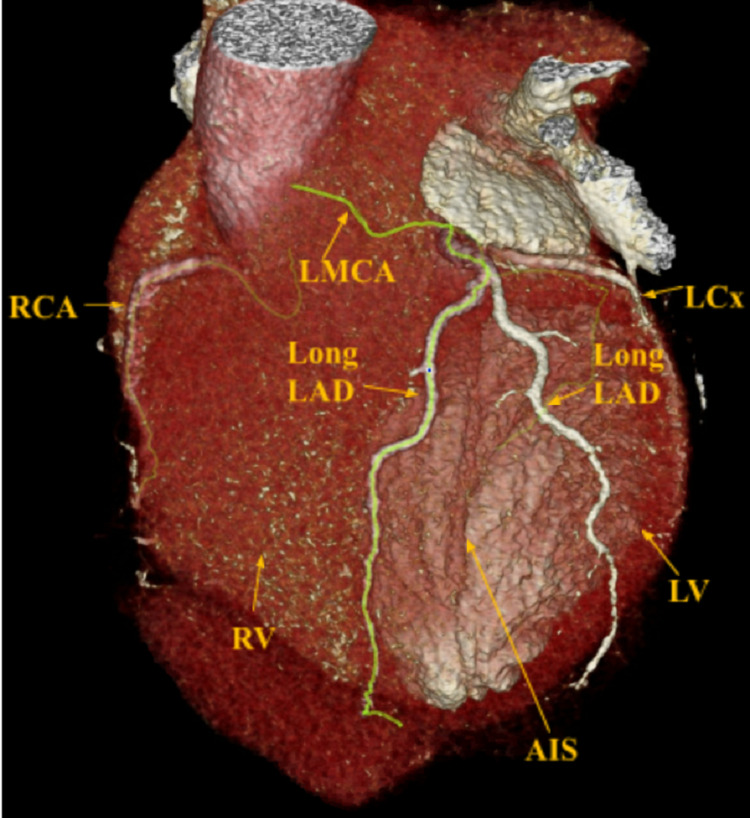
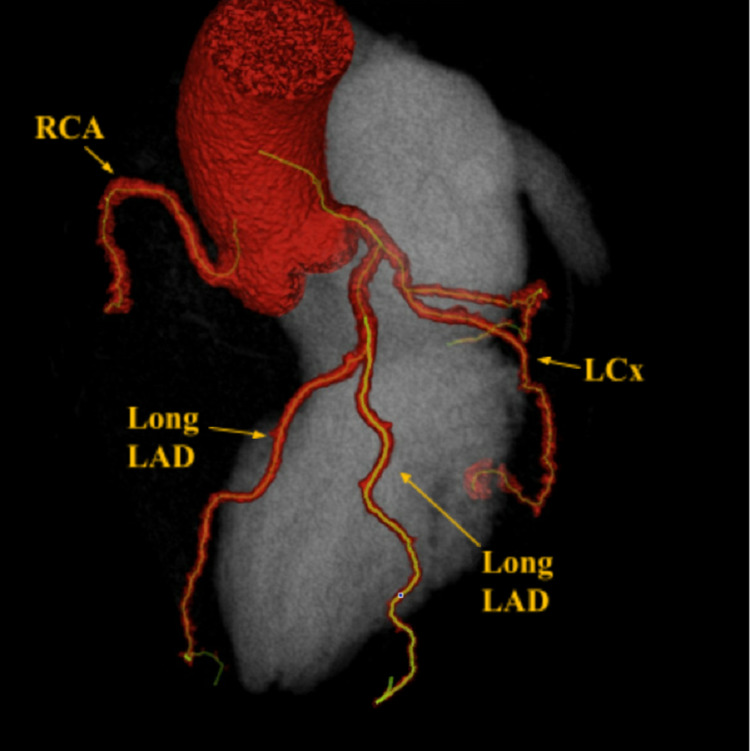
Physical exam was unremarkable, except for mild tenderness to palpation of the chest wall and anxiety. An electrocardiography (ECG) was performed and showed normal sinus rhythm at 60 beats per minute (bpm), normal axis, normal intervals, no acute ischemic changes, and an isolated T wave inversion in lead 3. Vitals in the ED were normal except for elevated blood pressure at 170/84. Cardiac markers were within normal limits. Echocardiography showed a left ventricular ejection fraction of 65%, normal right ventricular size and systolic function, mild mitral valve regurgitation, and mild aortic regurgitation. Coronary computed tomography (CCT) (Figures 1, 2) was performed to evaluate coronary artery anatomy and assess plaque burden.
Figure 1. CCT showing two long LADs, one coursing laterally and the other coursing medial to the AIS.
CCT: Coronary computed tomography; LAD: Left anterior descending artery; AIS: Anterior interventricular sulcus.
Figure 2. CCT showing two long LADs.
CCT: Coronary computed tomography; LAD: Left anterior descending artery.
Discussion
Differential diagnosis included acute coronary syndrome (ACS), musculoskeletal pain, and anxiety-induced chest pain. ACS was ruled out after cardiac markers were negative twice and ECG had no acute ischemic changes. Incidentally, the CCT results showed a left anterior descending artery (LAD) that originates from the left main coronary artery (LMCA) and initially runs in the anterior interventricular sulcus (AIS) for a short course before bifurcating into two long LADs which both leave the AIS and course out to supply the apex. While it may be considered that the second long LAD may represent a large first diagonal branch; that would assume that the patient has an LAD that resides in the expected anatomic position in the anterior interventricular groove, but in fact it does not, and instead another Long LAD, that runs medially to supply the septum and medial structures, is noted and does not run in the anterior interventricular groove [3]. One of the vessels was noted to course laterally and the other coursed medially of the AIS. The left circumflex (LCx) and right coronary arteries (RCA) were patent (Figures 1, 2).
The patient was continued on her home medications for hypertension - amlodipine 5mg oral daily. She was discharged once stabilized and advised to follow up as an outpatient. While dual LAD is rare (Sidhu and Wander found 0.68% prevalence for any type of dual LAD) and presumed benign, it presents various diagnoses and treatment challenges of which practitioners must be aware [4-6]. Prerequisite to successful surgical intervention, like revascularization, is the precise knowledge of the anatomical features to be evaluated. For example, if both the short and long LAD arteries are significantly stenosed in a patient, revascularization of both vessels may be necessary to restore blood supply to the septum and anterior wall. Additionally, as CCT has become the noninvasive imaging modality of choice for the diagnosis of cardiovascular coronary pathology, it is particularly imperative that clinicians be aware of these variants to allow for precise evaluation and management.
Typically, the LMCA gives rise to the LAD artery, which descends through the epicardial fat of the AIS. It then proceeds to give off septal and diagonal branches which supply the anteroseptal and anteroapical regions of the heart [1]. Dual LAD describes a rare anatomic variant in which two coronary branches, known as the “short” and “long” LAD arteries, supply the territory normally supplied by the solitary LAD artery.
Dual LAD was first reviewed and classified by Spindola-Franco et al. in 1983 when just three variants had been discovered [2]. To date, 12 variants of dual LAD, classified by origin and course of the short and long LAD arteries, have been described in the literature. Retrospective analyses have revealed that Type I dual LAD (in which the short LAD artery originates from the LAD proper and terminates in the AIS, while the long LAD artery originates from the LAD proper and descends to the left of the AIS before entering the AIS more distally) is the most common variant. Current classification of dual LAD can be seen in Table 1.
Table 1. Classification of dual LAD variants.
AIS: Anterior Interventricular Sulcus, LAD: Left Anterior Descending Artery, LMCA: Left Main Coronary Artery, LCS: Left Coronary Sinus, LV: Left Ventricle, RCA: Right Coronary Artery, RCS: Right Coronary Sinus, RVOT: Right Ventricle Outflow Tract, RV: Right Ventricle
| Type | Short LAD Origin | Long LAD Origin | Short LAD Course | Long LAD Course |
| I | LAD Proper | LAD Proper | Originates from the LAD proper and terminates in the proximal AIS | Descends on LV side of the proximal AIS and enters the distal anterior interventricular sulcus |
| II | LAD Proper | LAD Proper | Originates from the LAD proper and terminates in the proximal AIS | Descends on the RV side of the proximal AIS and reenters the distal AIS |
| III | LAD Proper | LAD Proper | Originates from the LAD proper and terminates in the proximal AIS | Courses through the intramyocardial septum proximally, and may emerge in the distal AIS or terminate in the apical septum |
| IV | LMCA | RCA | Originates from the LMCA and terminates in the proximal AIS | Courses along an anomalous prepulmonic course anterior to the right ventricular outflow tract (RVOT) and reenters the distal AIS |
| V | LCS | RCS | Originates from the left coronary sinus (LCS) and terminates in the proximal AIS | Courses along an anomalous intramyocardial course within the septal crest, emerges epicardially, to enter the distal AIS |
| VI | LMCA | RCA | Originates from the LMCA and terminates in the proximal AIS | Courses between the RVOT and the aortic root and emerges in distal AIS |
| VII | LAD Proper | LAD Proper | Originates from the LAD proper and terminates in the proximal AIS | Courses along the LV side of the proximal AIS and reenters the distal AIS |
| VIII | LMCA | Mid-RCA | Originates from the LMCA and terminates in the proximal AIS | Courses along the inferior wall of the RV and traverses the apex to terminate in the distal AIS |
| IX | LAD Proper | LAD Proper | Originates from the LAD proper and terminates in the proximal AIS | Courses along the LV side of the AIS, enters the distal AIS and terminates before the apex |
| X | LMCA | RCS | Originates from the LMCA and terminates in the proximal AIS | Courses along an anomalous prepulmonic course anterior to the RVOT and reenters the distal AIS |
| XI | RCS | RCS | Originates from the RCS, takes an intramyocardial course within proximal septum and emerges in the proximal AIS | Courses along an anomalous prepulmonic course anterior to the RVOT and reenters the distal AIS |
| XII | LMCA | RCS | Originates from LMCA that originates in the RCS and terminates in the proximal AIS | Courses anterior to the main pulmonary artery and terminates in the distal AIS |
| XIII | No Short LAD | LAD Proper LAD Proper | Not applicable | Two long LADs which both leave the AIS and course out to the apex. One of the vessels courses laterally and the other courses medially of the AIS |
Conclusions
To the best of our knowledge, the current case describes a novel subtype of dual LAD, which we propose to name variant XIII. In theory, mortality associated with LAD occlusion should be minimized if there are two LADs supplying the same territory as a single LAD. However, in patients with long-standing atherosclerosis, it is possible that both LADs may be occluded. Therefore, it is pertinent to identify the coronary vessels accurately before certain interventions are taken. Our case proposes a novel variant (Type XIII) of the dual LAD anatomic phenomenon never before described in the world literature. Acknowledgement of this phenomenon can help guide accurate management in the future for patients with this variant.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Coronary artery anatomy and variants. Malagò R, Pezzato A, Barbiani C, Alfonsi U, Nicolì L, Caliari G, Pozzi Mucelli R. Pediatr Radiol. 2011;41:1505–1515. doi: 10.1007/s00247-011-2218-9. [DOI] [PubMed] [Google Scholar]
- 2.Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Spindola-Franco H, Grose R, Solomon N. Am Heart J. 1983;105:445–455. doi: 10.1016/0002-8703(83)90363-0. [DOI] [PubMed] [Google Scholar]
- 3.Yet another novel variant of dual left anterior descending artery: type XII. Pandey NN, Shaw M, Sharma A, Ganga KP, Gulati GS. Heart Lung Circ. 2020;29:33–35. doi: 10.1016/j.hlc.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Prevalence and morphologic features of dual left anterior descending artery subtypes in coronary CT angiography. Şeker M. Radiol Med. 2020;125:247–256. doi: 10.1007/s11547-019-01124-7. [DOI] [PubMed] [Google Scholar]
- 5.Prevalence of dual left anterior descending artery variations in CT angiography. Bozlar U, Uğurel MŞ, Sarı S, Akgün V, Örs F, Taşar M. Diagn Interv Radiol. 2015;21:34–41. doi: 10.5152/dir.2014.14275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevalence and characteristics of dual left anterior descending artery in adult patients undergoing coronary angiography. Sidhu NS, Wander GS. Future Cardiol. 2019;15:425–435. doi: 10.2217/fca-2019-0052. [DOI] [PubMed] [Google Scholar]