Abstract
Background
Pain from episiotomy or tearing of perineal tissues during childbirth is often poorly treated and may be severe. This randomized double-blind controlled trial was performed to compare the effectiveness, side effects and cost of, and patient preference for, 2 analgesics for the management of postpartum perineal pain.
Methods
A total of 237 women who gave birth vaginally with episiotomy or a third- or fourth-degree tear between August 1995 and November 1996 at a tertiary-level teaching and referral centre for obstetric care in Vancouver were randomly assigned to receive either ibuprofen (400 mg) (n = 127) or acetaminophen (600 mg) with codeine (60 mg) and caffeine (15 mg) (Tylenol No. 3) (n = 110), both given orally every 4 hours as necessary. Pain ratings were recorded before the first dose and at 1, 2, 3, 4, 12 and 24 hours after the first dose on a 10-cm visual analogue scale. Side effects and overall opinion were assessed at 24 hours.
Results
Ibuprofen and acetaminophen with codeine had similar analgesic properties in the first 24 hours post partum (mean pain rating 3.4 and 3.3, mean number of doses in 24 hours 3.4 and 3.3, and proportion of treatment failures 13.8% [16/116] and 16.0% [16/100] respectively). Significantly fewer subjects in the ibuprofen group than in the acetaminophen with codeine group experienced side effects (52.4% v. 71.7%) (p = 0.006). There were no significant differences in overall patient satisfaction between the 2 groups. The major determinant of pain intensity was forceps-assisted delivery. Overall, 78% of the treatment failures were in women with forceps-assisted deliveries.
Interpretation
Since the 2 analgesics were rated similarly, ibuprofen may be the preferred choice because it is less expensive and requires less nursing time to dispense. Further studies need to address improved analgesia for women with forceps-assisted deliveries.
Episiotomy or tearing of perineal tissues during childbirth is associated with significant pain, infection and loss of mobility during the immediate postpartum period.1 Although the use of episiotomy is often debated, it remains a common surgical procedure in North America.2 Third- and fourth-degree tears, although less frequent than episiotomy, are a significant cause of morbidity during the postpartum period.1 Pain from perineal injury is often poorly treated and may be severe.3,4 Nonpharmacological methods of pain management (e.g., application of heat or cold, or sitz baths) are often inadequate. Codeine, alone or in combination with acetaminophen, is frequently used, but side effects, such as constipation, nausea, stomach pain and dizziness, limit its appeal. In addition, codeine alone has been shown to be no more effective for pain relief than placebo.5,6,7
NSAIDs, such as ibuprofen, have been found to be effective in the management of pain after episiotomy, without associated illness from side effects.8,9,10 Studies comparing various NSAIDs with opioid-containing compounds have, however, been limited by small samples,7,8,9,11,12 observation periods of less than 6 hours,5,6,8,9,10,12 lack of standardized or validated pain assessment,5,8,10,13 and omission of measurement of side effects5,9 and of patient preference.5,6,7,8,9,10,11,12,13
In our institution, standing orders for the management of postpartum pain include acetaminophen (300 mg) with codeine (30 mg) and caffeine (15 mg) (Tylenol No. 3), 1 or 2 tablets every 4 hours, or 400 mg of ibuprofen every 4 hours. These particular choices for analgesia have not been rigorously studied. Currently, nurses may choose to dispense either ibuprofen or acetaminophen with codeine, but there is no evidence on which to base their decision. Both analgesics are considered by the American Academy of Pediatrics to be compatible with breastfeeding.14 Because codeine is centrally acting, it has been combined with peripherally acting nonnarcotic analgesics to improve effectiveness.8 Compared with other NSAIDs, ibuprofen has a similar efficacy and fewer adverse side effects.15 Ibuprofen inhibits prostaglandin synthesis, which in turn is thought to sensitize pain receptors to the effects of pain mediators, such as bradykinin, acetylcholine and histamine.16
The purpose of this study was to compare in a randomized blinded design an NSAID, ibuprofen, with a narcotic analgesic, acetaminophen with codeine, over an observation period of 24 hours. We measured pain and side effects in addition to cost to compare the 2 agents. We also incorporated 2 measures of patient satisfaction, 1 simple and 1 complex. Measuring the woman's satisfaction by more than 1 means recognizes that satisfaction is a complex psychologic response to childbirth.17
Methods
We conducted a randomized double-blinded controlled clinical trial comparing ibuprofen and acetaminophen with codeine for the treatment of pain from perineal injury in childbirth. The study was conducted at British Columbia's Women's Hospital and Health Centre, Vancouver, a tertiary-level teaching and referral centre for obstetric care in British Columbia. Recruitment occurred from August 1995 to November 1996 during the 12-hour day shift. Ethical approval for the study was obtained from the University of British Columbia's Clinical Screening Committee for Research Involving Human Subjects.
Protocol
Women who had given birth vaginally and had had an episiotomy or a third- or fourth-degree tear were included in the study. The main languages spoken by our clients are English (45%) and Cantonese or Mandarin (35%). Consent forms and data forms were written in English and Chinese script. The Chinese-language versions were translated by a bilingual nurse, and the translations were checked for content and cultural accuracy by a bilingual delivery suite nurse and an obstetric anesthesiologist. Exclusion criteria included allergy to either study drug, a history of drug dependence, regular use of analgesic drugs before or during pregnancy, and any medical condition known to be potentially exacerbated by opioids or NSAIDS, including a history of gastrointestinal ulcer or bleeding, significant renal or liver impairment and asthma. Women with postpartum hemorrhage or any other major postpartum complication were excluded.
After assessment for eligibility, subjects were recruited in the delivery suite by a research assistant (obstetric nurse) or one of the investigators. Written consent was obtained within 1 hour after delivery. Randomization occurred when the patient first indicated she had pain. Patients who did not request postpartum analgesia were therefore not assigned to either group. Randomization was done by the Pharmacy Department in blocks of 20. To minimize differences between the treatment groups in the proportion of women having forceps-assisted births, which we postulated might be associated with increased pain, the randomization was stratified on use of forceps. Subject assignment was concealed in opaque envelopes. The Pharmacy Department maintained the study code to facilitate accessibility in case of an adverse reaction.
The hospital pharmacy prepared the study medications in dark green gelatinous capsules in order to make them similar in appearance and taste. The dosing schedule for the study medications was ibuprofen (400 mg), or acetaminophen (600 mg) with codeine (60 mg) and caffeine (30 mg), both given orally every 4 hours as necessary for 24 hours after birth. The patients and their caregivers (nurses and investigators) were blinded as to group allocation. After the 24-hour period, patients received analgesic according to their individual physician's preferences.
Outcomes
The primary outcome for the study was severity of pain, rated on a 10-cm visual analogue scale from 0 (“no pain”) to 10 (“worst pain ever”).18 An initial rating was recorded before the subject took the first dose of analgesia and at 1, 2, 3, 4, 12 and 24 hours after the first dose. Study forms with the visual analogue scale on them were left at the bedside, and the subjects were reminded to complete them at the appropriate time by their postpartum nurse.
Secondary outcomes relating to pain were evaluated. The number of doses of medication, dosing intervals and treatment failures, if any, were retrieved from the patients' charts 24 hours after childbirth. If the patient indicated that analgesia was inadequate during the first 24 hours, the treatment was considered a failure, and the patient was given a synthetic opioid as “rescue” medication (anileridine, 25 to 50 mg administered orally). Patients were monitored thereafter to ensure that the rescue medication was effective.
As a secondary outcome, we also evaluated side effects, including nausea, vomiting, stomach pain, indigestion, disorientation and dizziness. The subjects completed a written questionnaire about side effects 24 hours after childbirth.
The subjects were asked to indicate their overall level of satisfaction with their study drug on a 10-cm visual analogue scale ranging from 0 (“very dissatisfied”) to 10 (“very satisfied”).
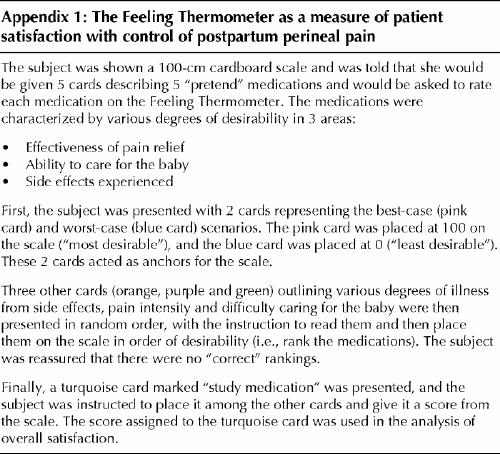
The subjects also ranked their study medication in comparison with other, theoretical analgesics using a tool from the health economics literature called the Feeling Thermometer.19 In the context of our study, the Feeling Thermometer was used for a global assessment of satisfaction (Appendix 1). We used it to combine patients' rankings of analgesic effectiveness (considering the side effects) with their evaluation of personal ability to care for the newborn.
We compared the cost of the 2 treatment regimens using direct costs of the drugs from the hospital pharmacy. The difference in nursing time needed to dispense a narcotic versus a nonnarcotic analgesic was arrived at by consensus among delivery suite nurses.20
Sociodemographic information was provided by the patients on a data form completed after childbirth. The type and dosage of analgesia used during labour and of nonpharmacologic analgesia used during the postpartum period were obtained from the patients' records. We compared the 2 groups in terms of these demographic and pregnancy- and labour-related factors.
Power analysis indicated that a sample of 104 subjects per study arm was required to achieve 80% power with a type I error set at 0.05 to determine a 30% difference in pain severity. In a pilot analysis, a sample of women who received acetaminophen with codeine for perineal pain had a mean pain rating on the visual analogue scale 3 cm lower after than before taking the medication. An additional decrease of 1 cm was considered clinically important, representing a relative difference of 30%.
Analysis proceeded according to intention to treat. We compared categorical variables, such as presence of side effects, using the χ2 test and compared continuous variables, such as overall satisfaction as measured on the visual analogue scale, using Student's t-test. Sequential measures on visual analogue pain scales were compared between groups with the use of a general linear model for repeated measures. The initial pain rating before the patient received the first dose of medication was included as a covariate in the model.
Results
During the study period 1575 women gave birth with or without forceps assistance and had either episiotomy or third- or fourth-degree tears. Most were not considered for participation in the study because of logistical reasons (e.g., delivery at night or on weekends, when an investigator was not on site). Of the remaining 297 women, 60 were excluded for the following reasons: maternal exhaustion, language barrier and lack of sufficient nursing staff during the evening and at night. Of the remaining 237 participants, 127 received ibuprofen, and 110 received acetaminophen with codeine (Fig. 1). Errors were made in the dosing interval when administering the study drug to 3 subjects in the ibuprofen group, and 1 subject in the acetaminophen with codeine group was withdrawn from the study because of a postpartum hemorrhage. The results for these subjects were retained in the analysis. There were no suggestions from patients or nurses that allocation was known for any patient. The study code was broken twice. A subject who received acetaminophen with codeine informed her nurse that she was allergic to codeine, but no adverse effects were observed. One subject who received ibuprofen reported hallucinations, which ceased when treatment with the medication was stopped.
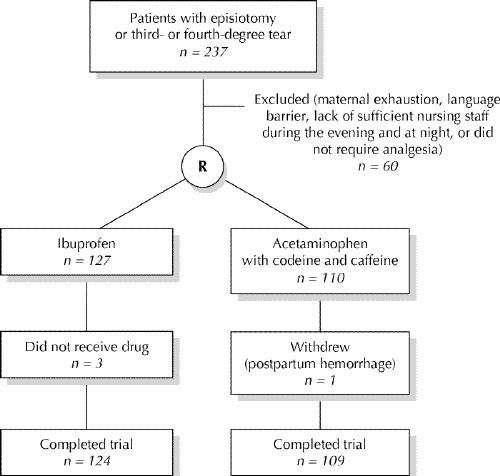
Fig. 1: Profile of trial. R = randomization.
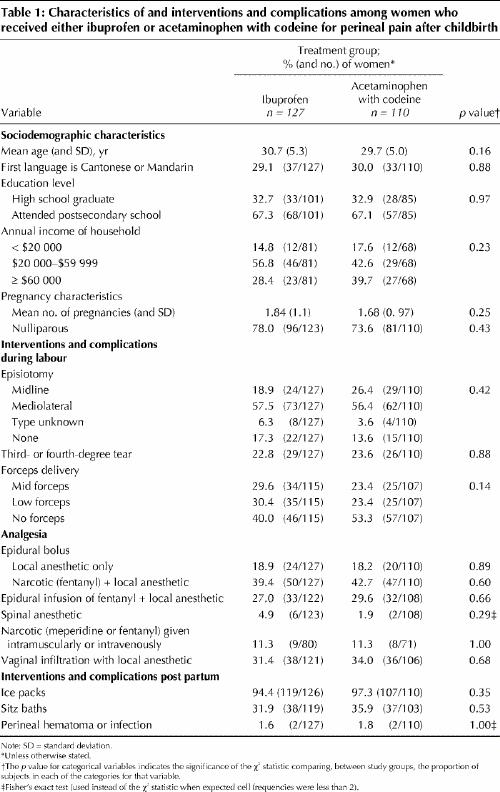
The 2 groups were comparable in sociodemographic characteristics and in gravidity and parity (Table 1). There was no difference in the use of episiotomy or in the incidence of third- and fourth-degree tears between the groups. Although the analysis was stratified for use of forceps, there were more forceps-assisted births in the ibuprofen group than in the acetaminophen with codeine group. Infant birth weights were similar between the groups, as were analgesic methods used in labour and use of ice packs and sitz baths post partum (Table 1).
Table 1
The severity of perineal pain did not differ at any of the time intervals between the ibuprofen and acetaminophen with codeine groups (Table 2). The mean ratings of pain intensity were 3.4 and 3.3 respectively. In a general linear model, using a repeated-measures analysis, in addition to including pain rating before the first request for analgesia, we included use of forceps as a covariate, given the uneven distribution between groups. Pain levels did not differ between the groups when pain level before receiving the first dose of study drug and use of forceps were controlled for. The main determinant of pain intensity was use of forceps. When we combined the data for the 2 groups, the women who had forceps-assisted births rated their pain significantly higher than those without forceps-assisted births at 1 hour (3.7 v. 2.8), 3 hours (4.1 v. 2.6) and 4 hours (4.5 v. 3.0) (p = 0.02, < 0.001 and < 0.001 respectively). A total of 78% of the treatment failures occurred in women with forceps-assisted deliveries.
Table 2
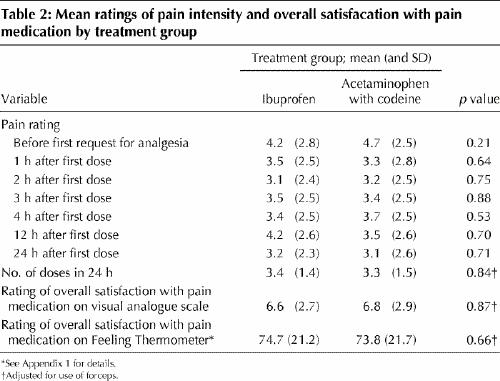
Similarly, the secondary indicators of pain did not differ between the groups. The mean number of doses in 24 hours was 3.4 for the ibuprofen group and 3.3 for the acetaminophen with codeine group (p = 0.84). The proportion of treatment failures in the 2 groups was 13.8% (16/116) and 16.0 (16/100) respectively (p = 0.46, adjusted for use of forceps).
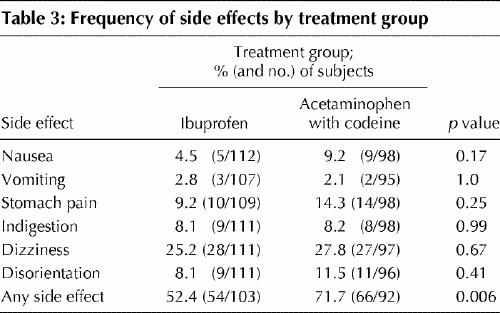
Significantly fewer subjects in the ibuprofen group than in the acetaminophen with codeine group experienced side effects (52.4% v. 71.7%) (p = 0.006) (Table 3). The difference was mostly due to fewer subjects with nausea, stomach pain and disorientation in the ibuprofen group.
Table 3
Overall satisfaction with the study drug, as measured with the visual analogue scale, did not differ between the 2 groups (mean rating 6.6 for the ibuprofen group and 6.8 for the acetaminophen with codeine group) (p = 0.87). When we combined the results for the 2 groups, overall satisfaction was significantly lower for the women who had forceps-assisted births than for those who did not (6.2 v. 7.7) (p < 0.001).
A total of 131 subjects (55.3%) completed the Feeling Thermometer. Ranking scores on the Feeling Thermometer did not distinguish the groups (mean score 74.7 for the ibuprofen group and 73.8 for the acetaminophen with codeine group, out of a maximum possible score of 100) (p = 0.66) (Table 2).
At the time of the study, 1 tablet of ibuprofen cost $0.02, and 1 tablet of Tylenol No. 3 cost $0.05. Administration of a narcotic analgesic has previously been estimated by nursing staff to take 10 minutes longer than administration of ibuprofen, because self-administration of narcotics was not available at our institution at the time of the study. The 10 minutes would be spent obtaining keys to the narcotics cupboard, dispensing from the narcotics cupboard and signing the narcotics record. Ten minutes every 4 hours could make a difference in nursing time available for other tasks of 30 minutes in a 12-hour shift.
Interpretation
We were unable to demonstrate a difference in perineal pain ratings between women treated with ibuprofen and those treated with acetaminophen with codeine in a repeated-measures analysis controlling for use of forceps and initial expression of pain. Although significantly fewer subjects in the ibuprofen group than in the acetaminophen with codeine group experienced side effects, the women in the 2 groups did not differ in their expression of satisfaction or in their ranking of study medication. One subject who received ibuprofen experienced hallucinations. The incidence of hallucinations with ibuprofen has been reported to be 3% to 9%, but the relation is not known to be causal at this time.21 Our findings are consistent with those of Walters and colleagues,12 who compared suprofen (200 mg) and codeine (30 mg) for episiotomy pain and found that pain relief was similar with the 2 agents, although there was increased drowsiness with suprofen.
In contrast, Laska and Sunshine5 reported that fenoprofen (100 or 200 mg) was more effective than codeine (60 mg) for relief of episiotomy pain. Schachtel and associates9 found that ibuprofen (400 mg) was more effective than acetaminophen (1000 mg) for total pain relief and for reduction of pain by more than 50%, with faster onset and longer duration. Yonkeura and coworkers10 found meclofenamate at 2 dosage levels, 100 and 200 mg, to be superior to 60 mg of codeine. None of these investigators compared acetaminophen plus codeine with ibuprofen. The combination of acetaminophen and codeine may actually be more potent than either drug alone. McQuay and Moore22 derived a “number needed to treat” of 5.3 for paracetamol (acetaminophen) versus 3.1 for paracetamol with codeine. This means that for patients with moderate to severe pain, 1 in 3 will have a 50% reduction in pain with the combination of medications, compared with 1 in 5 with paracetamol alone.
None of these investigators measured the prevalence of forceps use in their samples. The overall rate of forceps-assisted births at our institution during the study period was 9.0%. The high prevalence of forceps use in our study (61.4% in the ibuprofen group and 47.7% in the acetaminophen with codeine group) may have masked the effectiveness of these agents because of an increased requirement for analgesia. Pain intensity and duration increase with the degree of perineal injury.4 Maternal trauma is a recognized complication of forceps-assisted delivery, with significant soft-tissue injury, such as third- or fourth-degree tears or extensions of episiotomy, occurring in 17% to 49% of cases.23 When we disregarded treatment allocation, use of forceps was significantly related to overall satisfaction and pain intensity at 4 hours. Given this finding and the fact that neither treatment was rated very highly (mean rating 6.6 and 6.8 on a scale of 10), it would be prudent for clinicians to pursue a better method of pain management for women having forceps-assisted deliveries.
A total of 58.9% of the English-speaking subjects in our study experienced at least 1 side effect, as compared with 68.9% of the Chinese-speaking women. This difference was not significant. This analysis was done because of the potential for Chinese-speaking women to have higher serum levels of the drugs, given their smaller stature, with possible increased morbidity from side effects.
Since the experience and expression of pain may be culturally determined,24 we felt it was important to study the major cultural groups at our institution. The visual analogue scale for the rating of pain has been evaluated for the Chinese population and has been found to be accurate and reliable.25,26 Visual analogue scales have been found to correlate with verbal rating scales, global comparison scales and numerical scales.18 There were no differences in pain intensity at any of the time intervals between the English-speaking and Chinese-speaking women in our study. The latter indicated marginally higher levels of satisfaction on the visual analogue scale (7.3 [standard deviation 2.3] v. 6.5 [standard deviation 2.4]) (p = 0.06). Ranking scores on the Feeling Thermometer did not differ between the 2 cultural groups; however, only 24 Chinese-speaking subjects completed this instrument because of the difficulty getting an assistant who had the particular skills to administer this interactive tool and could speak Cantonese or Mandarin.
The strengths of our study include use of a randomized, blinded design, several measures of pain intensity, measurement of a variety of side effects and 2 separate methods of measuring overall patient satisfaction. The results were similar between 2 cultural groups in our setting. We were able to collect detailed demographic data not readily available from the medical chart, such as family income and woman's education level, in order to test comparability of the groups.
The study was limited by its small sample. Although the sample was larger than those in many studies published to date, the repeated-measures analysis included only 111 subjects at 24 hours. Many women chose to stop rating their pain when their pain management was satisfactory and they were no longer requesting analgesia. To permit repeated-measures analysis, all subjects have to complete the scale at each time interval. Analysis of shorter time intervals (4 and 12 hours) did not reveal any significant differences in perception of pain intensity between the treatment groups.
In conclusion, we found that ibuprofen and acetaminophen with codeine and caffeine were similar in efficacy for the treatment of postpartum pain from episiotomy or third- or fourth-degree tears. Neither method is ideal, and women, particularly those with forceps-assisted deliveries, remain underserved in the management of perineal pain.
Appendix 1.
Footnotes
This article has been peer reviewed.
Acknowledgements: This study was supported by the British Columbia Women's Foundation.
Competing interests: None declared.
Correspondence to: Dr. Elizabeth A. Peter, Department of Anaesthesia, Rm. 1Q72, British Columbia's Women's Hospital and Health Centre, 4500 Oak St., Vancouver BC V6H 3N1; fax 604 875-2733
References
- 1.Klein MC, Gauthier RJ, Robbins JM, Kaczorowski J, Jorgensen SH, Franco ED, et al. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol 1994; 171: 591-8. [DOI] [PubMed]
- 2.Levitt C, Hanvey L, Avard D, Chance G, Kaczorowski J. Survey of routine maternity care and practices in Canadian hospitals. Ottawa: Health Canada and Canadian Institute of Child Health; 1995. p. 60.
- 3.Reading AE, Sledmere CM, Cox DN, Campbell S. How women view post-episiotomy pain. BMJ 1982;284:243-6. [DOI] [PMC free article] [PubMed]
- 4.Macarthur A, Macarthur C. Perineal trauma and postpartum perineal pain [abstract]. Am J Obstet Gynecol 1997;176:S121.
- 5.Laska E, Sunshine A. Fenoprofen and codeine analgesia. Clin Pharmacol Ther 1981; 29:606-16. [DOI] [PubMed]
- 6.Norman SL, Jeavons BI, O'Brien PMS, Johnson IR. A double-blind comparison of a new ibuprofen-codeine phosphate combination, codeine phosphate, and placebo in the relief of postepisiotomy pain. Clin Ther 1985;7:549-54. [PubMed]
- 7.Bloomfield S, Barden T, Mitchell J. Naproxen, aspirin, and codeine in postpartum uterine pain. Clin Pharmacol Ther 1983;34:414-21. [DOI] [PubMed]
- 8.Sunshine A, Roure C, Olson N, Laska E, Zorrilla C, Rivera J. Analgesic efficacy of two ibuprofen-codeine combinations for the treatment of postepisiotomy and postoperative pain. Clin Pharmacol Ther 1987;42:374-80. [DOI] [PubMed]
- 9.Schachtel B, Thoden W, Baybutt R. Ibuprofen and acetaminophen in the relief of postpartum episiotomy pain. J Clin Pharmacol 1989;29:550-3. [DOI] [PubMed]
- 10.Yonkeura M, Turner J, diZerega G. Double-blind comparison of meclofenamate sodium with codeine and placebo for the pain of episiotomy. Clin Ther 1987; 9:578-93. [PubMed]
- 11.Vangen O, Doessland S, Lindbaek E. Comparative study of ketorolac and paracetamol/codeine in alleviating pain following gynaecological surgery. J Int Med Res 1988;16:443-51. [DOI] [PubMed]
- 12.Walters B, Smith V, De Swiet M. Pain relief after episiotomy — a comparative study of suprofen and dihydrocodeine. Br J Obstet Gynaecol 1985;92:1160-3. [DOI] [PubMed]
- 13.Jacobson J, Bertilson S. Analgesic efficacy of paracetamol/codeine and paracetamol/dextropropoxyphene in pain after episiotomy and ruptures in connection with childbirth. J Int Med Res 1987;15:89-95. [DOI] [PubMed]
- 14.Committee on Drugs, American Academy of Pediatrics. The transfer of drugs and other chemicals into human breast milk. Pediatrics 1994;93:137-50. [PubMed]
- 15.Kaplan B, Farris KB, Kirking DM. Assessing physician choice of nonsteroidal antiinflammatory drugs in a health maintenance organization. Ann Pharmacother 1993;27(11):1393-9. [DOI] [PubMed]
- 16.Miller R. Evaluation of the analgesic efficacy of ibuprofen. Pharmacotherapy 1981;1:21-7. [DOI] [PubMed]
- 17.Robinson PN, Salmon P, Yentis SM. Maternal satisfaction. Int J Obstet Anesth 1998;7:32-7. [DOI] [PubMed]
- 18.Reading A. A comparison of pain rating scales. J Psychosom Res 1980;24:119-24. [DOI] [PubMed]
- 19.Furlong W, Feeny D, Torrance G, Barr R, Horsman J. Guide to design and development of health-state utility instrumentation. Hamilton (ON): Centre for Health Economics and Policy Analysis (CHEPA), McMaster University; 1990. CHEPA working paper no 9009.
- 20.Peter EA. A cost-utility evaluation of post-operative analgesia in the elderly in a community hospital using decision analysis [abstract]. Can J Anaesth 1994; 41: A22.
- 21.Compendium of pharmaceuticals and specialties. 35th ed. Ottawa: Canadian Pharmaceutical Association; 2000. p. 989.
- 22.McQuay H, Moore A. Paracetamol with and without codeine in acute pain. In: An evidence-based resource for pain relief. Oxford (UK): Oxford University Press; 1998. p. 60.
- 23.Johanson R, Rice C, Doyle M, Arthur J, Anyanwu L, Ibrahim J, et al. A randomised prospective study comparing the new vacuum extractor policy with forceps delivery. Br J Obstet Gynaecol 1993;100:524-30. [DOI] [PubMed]
- 24.Park KJY, Peterson LM. Beliefs, practices, and experiences of Korean women in relation to childbirth. Health Care Women Int 1991;12:261-9. [DOI] [PubMed]
- 25.Soh G, Ang HG. Comparison of two pain rating scales among Chinese patients. Chin Med J 1992;105:953-6. [PubMed]
- 26.Ann C, Lam YN, Collett B. Evaluation of the use of a visual analogue scale in a Chinese population. Pain 1986;25:215-21. [DOI] [PubMed]


