Abstract
Background:
The 2019 coronavirus (COVID-19) pandemic has brought unprecedented challenges to the health sector nationwide and internationally. Across all disciplines, unique and novel modes of presentation with substantial morbidity and mortality are being encountered, and growing evidence suggests that psychiatric comorbidity is likely among COVID-19 patients.
Objective:
This article aims to broaden the current discussion on the psychiatric sequalae of COVID-19, which has largely focused on anxiety, and examine the recently documented psychiatric sequelae of COVID-19 infection, the secondary effects of the pandemic on public mental health, and future psychiatric conditions that may arise due to COVID-19.
Methods:
We conducted an in-depth review of the current global psychiatric literature and describe the wide range of psychopathological presentations reported among past COVID-19 patients worldwide and those that are expected to emerge.
Results:
Current discussions in the psychiatric literature on COVID-19 report anxiety and anxiety disorders as a predominant set of clinical presentations during the pandemic. The impacts of direct COVID-19 infection, associated psychopathological sequelae, and drastic lifestyle changes due to the COVID-19 pandemic in South Africa, are associated with a broad range of psychopathologies and other neuropsychiatric presentations. Pre-existing societal conditions and burdens on the health system in South Africa prompt healthcare providers and public health planners to accordingly prepare for the expected rise in new psychiatric presentations.
Conclusion:
Greater awareness of the various psychiatric conditions attributed to COVID-19 infection may allow for earlier screening, more effective treatment, and greater positive health outcomes and better prepare health systems to address the growing pandemic in South Africa.
Keywords: COVID-19, psychopathology, mental health, stress, South Africa
INTRODUCTION
Numerous countries worldwide have reported widespread elevations in psychiatric morbidity, increased risk for mental distress and illness and novel psychopathological presentations among afflicted patients and communities exposed to the 2019 coronavirus (COVID-19) pandemic. (1,2) Similar to the conditions faced in South Africa, the novel and dramatic societal shifts brought by the national and international social policies aimed at mitigating the spread of COVID-19, including forced isolation and confinement, limited physical mobility, fears of infection, emotional distress, and for some, extreme threats to survival, are understood to underlie these psychiatric presentations and exacerbate the existing clinical conditions.(2,3) The rapid, ongoing review of initial mental health research on COVID-19 has shared vital insights into the possible psychological impact of the pandemic and highlights the prevalent presentation of anxiety and fear among affected patients and communities. Yet, evidence from the past viral epidemics and broader knowledge on the clinical, social and environmental determinants of mental illness emphasises that the psychiatric sequelae of COVID-19 are likely much broader than what the current, initial literature presents.(3) In this rapid review, we move beyond the primary focus on anxiety to describe the wider psychological sequelae and psychopathological risks due to the COVID-19 pandemic in South Africa. The following areas of psychopathologies are reviewed in this article: neuropsychiatric sequelae, anxiety and anxiety disorders, obsessive compulsive disorder, mood disorders, psychotic disorders, child and adolescent mental health and specific threats to healthcare workers.
Neuropsychiatric sequelae
The neuropsychiatric sequelae of COVID-19 include a range of mental conditions that may occur due to brain damage or other physiological damage resulting from infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), either due to the direct effects of infection of the central nervous system (CNS) or through indirect mechanisms such as the body’s immune response to the infection.(2) Due to the lack of data on the manifestations of the COVID-19, researchers have drawn upon the epidemiology and findings from studies on two similar strains of coronaviruses, which also caused widespread respiratory disease across the world, for additional insights: (1) severe acute respiratory syndrome coronavirus (SARS-CoV), initially encountered in 2002 and responsible for severe acute respiratory syndrome (SARS), and (2) Middle East respiratory syndrome coronavirus (MERS-CoV), first identified in 2012 and responsible for Middle East respiratory syndrome (MERS).(2,3) These comparisons have been on the basis that the three coronaviruses are structurally and genetically highly homologous and hence are largely comparable.(3)
A series of neuropsychiatric presentations have been previously reported in cases of MERS, SARS and COVID-19. Research suggests that delirium is a common presentation in the acute stage of COVID-19 – especially in the severely ill.(2) Early studies show that 20%–30% of patients with COVID-19 will either present with or develop delirium; this is much higher in cases of severe illness, where 60%–70% of patients have presented with delirium.(4) In older patients with COVID-19, the presentation of the disease may be quite atypical as delirium presents in the absence of other related signs and symptoms, such as fever or dyspnoea.(4) Preliminary evidence on the elderly MERS patients also reports that delirium is associated with raised mortality.(2) A recent study also reported acute new-on-set psychosis among COVID-19 patients with no prior history of psychosis. Patients in this study exhibited presentations of agitation, disorganisation, paranoid ideation and auditory hallucinations.(5) Additionally, among severe COVID-19 patients requiring intensive care unit admission, neurocognitive impairment (e.g. dysexecutive syndrome) may be a feature in the longer term (e.g. months to years) after recovery from COVID-19.(2) For SARS and MERS, there is evidence for depression, anxiety, fatigue, impaired memory, insomnia and post-traumatic stress disorder (PTSD) occurring in the post-illness period (i.e. in the following months to years), but it is yet unknown whether this is also the case with COVID-19.(2,3)
Growing evidence illustrates the role of psychoneuroinflammatory pathways in precipitating a wide range of psychiatric conditions (e.g. depression, anxiety, schizophrenia) as well as the neuropsychiatric conditions associated with human immunodeficiency virus (HIV) infection. Similar mechanisms may underlie the neuropsychiatric presentations of COVID-19. In addition to acute stress from COVID-19, infection with SARS-CoV-2 may lead to a hyperinflammatory state and a heightened, sustained inflammatory response to the infection, which has been described as a ‘cytokine storm’ (also a feature of SARS and MERS).(2,5,7) In a case report of three COVID-19 patients with psychosis, patients exhibited elevated levels of systemic inflammation a few days prior to a positive COVID-19 diagnosis.(5) These patients were otherwise asymptomatic (e.g. normal vitals, no delirium, no other physical illness).(5,6) Even with no infiltration of the virus into the CNS, peripheral cytokines involved in the anti-viral response may give rise to neuropsychiatric manifestations by precipitating neuroinflammatory responses and/or compromising blood–brain interface integrity, leading to peripheral immune cell transmigration into the CNS and disruption of neurotransmission.(7) Overall, the aetiology of neuropsychiatric manifestations of COVID-19 is likely multifactorial and may be affected by a variety of influences, including the current state of immune function, direct effects of the viral infection (e.g. infection of the CNS), the degree of physiological compromise (e.g. hypoxia), pre-existing cerebrovascular disease, in addition to the availability and quality of medical interventions and the larger psychosocial experience of COVID-19.(1)
Anxiety and anxiety disorders
Anxiety symptoms may range from a wide variety of concerns around contracting or spreading the virus, inability to regulate uncertainty, limited social interactions, unsafe living conditions and economic fallout, among others.(8,9) While these symptoms might not constitute an anxiety disorder per se, they are currently among the most common symptoms emerging during the COVID-19 pandemic.(2,3) A possible worsening of symptomatology in the pre-existing cases is described in the literature.(9)
Generalised anxiety disorder is among the most frequently described presentations among the COVID-19 patients. A meta-analysis of SARS, MERS and COVID-19 studies reported that anxiety was common in the post-illness phase up to three years after infection.(2) A cross-sectional survey performed in China reported a relatively high prevalence of generalised anxiety disorder of 35.1%, particularly among patients below the age of 35 years and those who reported excessive rumination (≥3 h a day) about the pandemic.(11) In one recent study on the mental health impact of COVID-19 in Soweto, while a majority of adults perceived that COVID-19 did not affect their mental health, a variety of stressors that caused deep worry, anxiety and rumination (‘thinking too much’) were reported in approximately 20% of adults.(8) These concerns during the lockdown were driven and exacerbated by the inability to care for themselves and their families, crippling economic struggles, personal vulnerability due to illness, the invisible nature of COVID-19 transmission and a lack of awareness on the disease.
As described above, health anxiety is another common presentation seen during the pandemic (9) and may result in individuals seeking medical assistance repeatedly, or conversely, avoiding help-seeking behaviour even when unwell. Health anxiety may also result in a mistrust of or reluctance towards engaging health authorities.(10) These anxiety-related behaviours may be erroneously attributed to an anxiety disorder and impart an added pressure on the already overburdened mental health system in South Africa.
Panic attacks may also occur as a distinct disorder or in combination with other psychiatric disorders. There is a paucity of literature regarding this in relation to COVID-19. However, panic attack symptoms such as shortness of breath, chills or heat sensations and chest pain or discomfort may overlap with symptoms of COVID-19 infection. Individuals with pre-existing panic disorder or who experience panic attacks from any other medical or psychiatric disorder might experience panic attacks more frequently. New onset of panic attacks in individuals with other psychiatric diagnoses is also possible.
Obsessive compulsive disorder
Another prominent presentation in the COVID-19 environment, by virtue of the clinical symptoms of distinct thoughts and often linked behaviours, is obsessive-compulsive disorder (OCD). This disorder was previously categorised under anxiety disorders and now exists as a separate category (OCD and related disorders) in the DSM-5 and can lead to significant functional impairment.(1) Numerous countries (e.g. China, the United States, the United Kingdom, Italy, India) have shown a recent increase in outpatients presenting with OCD symptoms, with exacerbation of symptoms such as hoarding and washing compulsions in already diagnosed OCD patients in response to stressors in the environment.(11,12) Lockdown measures may lead to panic buying and hoarding items such as hygiene products, flu medication and groceries.(11) Patients may struggle to determine what constitutes excessive behaviour under these extraordinary circumstances and normalise their compulsions as a precautionary response to the global pandemic. Proper hand-washing techniques recommended may also reinforce ritualistic behaviours, another clinical feature of OCD. The influx of information from TV, newspapers and social media sites regarding the virus can add to obsessions about the contamination.(12) During the previous epidemics such as SARS, MERS and influenza, researchers reported a worsening of OCD in patients up to 1 year later.(12)
Mood disorders
Direct infection of COVID-19 and the collateral impacts of the pandemic place many at risk for a variety of mood disorders. Seropositivity for viral illnesses linked to Influenza A and B and coronaviruses were shown to be associated with having a history of mood disorders, including depressive disorders, and increased suicide attempts.(13) One cross-sectional survey conducted in China during the COVID-19 outbreak found a prevalence of depressive symptoms of 20.1% and sleep disturbances of 18.2%.(10) Another Chinese study conducted during the early stages of the outbreak found that 16.5% of the sample reported moderate to severe depressive symptoms.(14) As noted with the HIV/AIDS epidemic in South Africa, depression can increase the risk of acquiring the virus, and the presence of mental illnesses can also be a stand-alone risk factor for acquiring the virus.(14) Human herpesvirus 6 has been also implicated in the development of bipolar disorder and depressive disorders, due to direct invasion of the CNS by the virus.(15) It has been hypothesised that coronaviruses typically invade the nervous system via the olfactory nerve. Thus, mood disorders can result directly from the virus, or secondarily through the resulting immunological response.(16,17) In persons with pre-existing mood disorders, infection with COVID-19 may result in a relapse of symptoms.
Patients with mood disorders often display cognitive changes that might affect their ability to rationalise the recommended measures of maintaining social distancing, regular washing of hands and surfaces and the use of a face-mask. Symptoms of acute mania include elevated mood, impulsivity, increased goal-directed activity and often, psychosis.(1) Acutely manic patients might be unable to appreciate the importance of these preventative measures, and hence be at higher risk of contracting and spreading the virus.
The numerous and ongoing psychosocial consequences of the pandemic can also result in the relapse of depressive disorders, bipolar disorder and suicidal thoughts,(17) particularly due to the widespread economic shocks due to COVID-19. The United Nations Development Programme has estimated an income loss of more than $220 billion in developing countries such as South Africa due to the pandemic.(18) Recessions inevitably leading to job losses and unemployment is an independent risk factor for the development of depressive disorders. A systematic review found a positive association between recession and higher suicide rates (19) with increases in global suicide rates of 20%–30% during the 2008 recession.(20)
Social isolation is also a risk factor for depressive disorders. One study, concerning patients and staff who were placed in an isolation dialysis unit during the MERS outbreak in 2015 in South Korea, found that isolation increased stress markers in both staff and patients.(21) Quarantine and social distancing measures, which limit the social interactions and communal gatherings (e.g. schools, work, churches and mosques, parks and other community facilities) during the lockdown, have removed vital social support systems for many patients. The lockdown also poses major barriers to accessing care. Some clinics, including in South Africa, are only allowing the patient to enter healthcare facilities, which is challenging in a discipline where collateral information is often imperative to assessing a patient’s progress. Restrictions on the availability of transport may also lead to decreased follow-up at clinics, non-adherence and subsequent relapses.
While studies on the psychological impact of COVID-19 in South Africa are limited, one recent study evaluated the mental health impacts of COVID-19 during the first 6 weeks of lockdown in Soweto.(8) In this community-based sample, 14.5% of adults displayed significant depressive symptoms, and greater knowledge of COVID-19 corresponded with lower perceived risk of COVID-19 infection but greater depressive symptoms.(8) Researchers also found that higher perceived risk of COVID-19 infection was associated with greater depressive symptoms, particularly among individuals with histories of childhood trauma (Figures 1 and 2).(8) An online survey conducted by the South African Depression and Anxiety Group found 65% of people felt stressed or very stressed about the imposed lockdown.(22) A majority of the respondents were from Gauteng (60%), and 59% had prior mental health disorders, and depression was the most common condition (46%). A portion of respondents reported a prior diagnosis with anxiety (30%) and bipolar disorder (12%). The main challenges faced during the lockdown included anxiety and panic (55%), financial stress and pressure (46%), depression (40%), poor family relations (30%), feelings of suicide (12%) and substance abuse (6%).
Fig 1: Predicted depression scores by the perceived COVID-19 risk group.
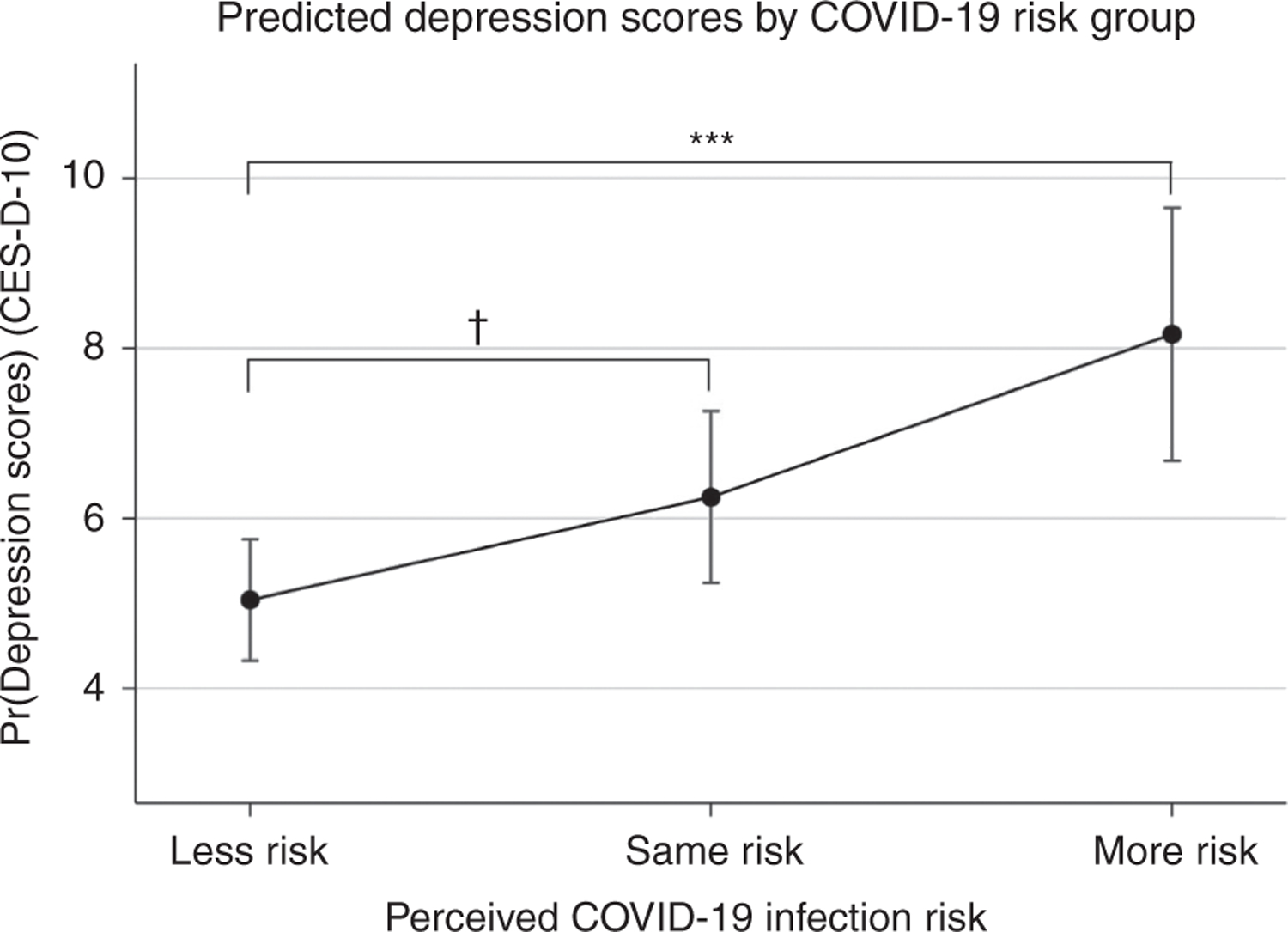
Note: Greater perceived risk of COVID-19 infection corresponds with greater depression symptomatology in adults living in Soweto. The effect of being in the ‘More risk’ group is highly significant (p ≤ 0.001) relative to being at ‘Less risk’, while the effect of perceiving that one is at the ‘Same risk’ of COVID-19 infection relative to other individuals living in Soweto on depression symptoms is marginally significant (p = 0.095). The respective predicted depression scores (assessed using the 10-item Centre for Epidemiologic Studies Depression Scale, CES-D-10) for each group are as provided: Less risk = 5.04, Same risk = 6.25, More risk = 8.17.(8)
Fig 2: Childhood trauma (ACES) and depression scores (CESD) by the COVID-19 risk group.
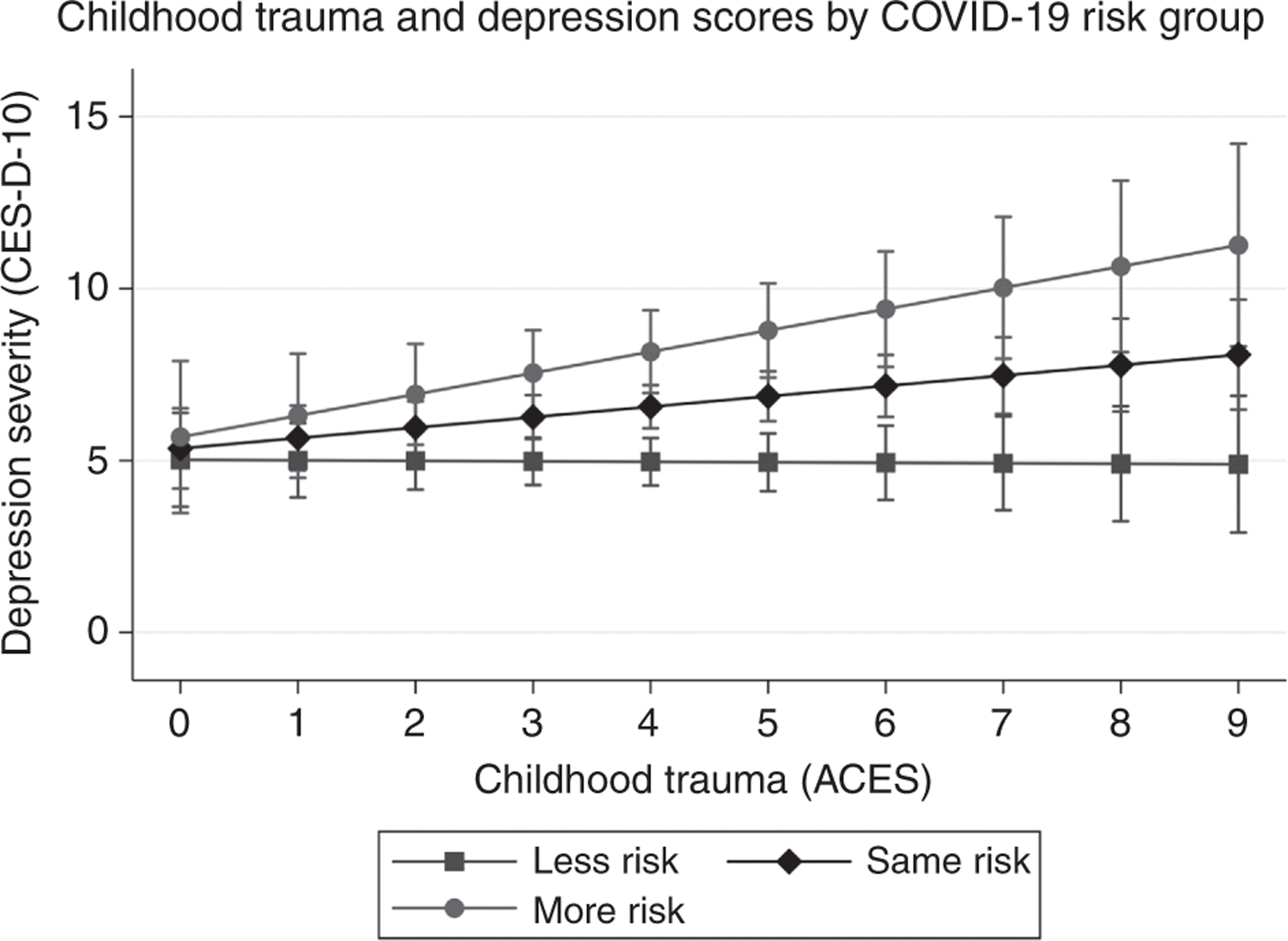
Note: Greater childhood trauma (ACES) potentiates the positive relationship between greater perceived COVID-19 risk and the severity of depressive symptomatology. The effect of the interaction between childhood trauma and perceived COVID-19 risk on depression is marginally significant (F[1, 206] = 3.53, p = 0.0617).(8)
Psychotic disorders
It has been postulated that exposure to a virus in utero increases the risk of developing schizophrenia later in life, with data from research conducted in the aftermath of the great Spanish influenza of 1918 demonstrating an association between exposure to general respiratory viruses such as influenza and subsequent psychotic episodes.(23,24) The response of immunoglobulin G was investigated against four human coronavirus strains that were prevalent at the time. Evidence showed that in approximately 90% of adults diagnosed with psychosis, elevated levels of antibodies to one or more viruses were found. Pandemics such as the Spanish flu demonstrated that these viruses can have a more immediate effect, resulting in cases of acute psychosis soon after or at the time of infection. Further research is, however, required, as it remains unclear whether this is due to the direct effects of the virus on the brain, systemic inflammation due to infection or perhaps a post-viral immune activation.(24)
Stress related to a pandemic may precipitate, exacerbate or impact the content of the psychotic symptoms(25,26). Patients presenting with psychosomatic delusions may experience intense paranoia.(25) A 43-year-old male patient in Germany with psychiatric illness presented with auditory hallucinations commenting that he has not cared for his parents who could have died of COVID-19, paranoid delusions that his parents and neighbours had contracted COVID-19, as well as delusions that he had immunity from the virus after contracting the virus from a Chinese message on a WhatsApp message.(26) In another case, a 38-year-old married woman with secondary-level education, good premorbid functioning and no prior psychiatric history believed she was potentially infected with the virus after a visit to her dentist (who had recently vacationed in France and was not donning a mask). Within four days, she became anxious with malaise and fever, developed command auditory hallucinations to go to multiple health centres for testing and began to feel ‘an evil demonic force which would take her soul in order to possess her.’ She also had visual hallucinations of shadows, delusions of reference and a formal thought disorder. The voice ultimately ordered her to kill her family. She was diagnosed with an acute psychotic disorder and was treated effectively with antipsychotic therapy.(27)
Anxiety is a common symptom in psychotic disorders as well and can interfere with rational decision-making, which could engender maladaptive behaviours such as excessive health-seeking, disproportionate hand-washing or purchasing protective gear.(27) Media coverage during pandemics or crises will unduly influence psychotic manifestations.(26) These case studies emphasise the profound impact that a global pandemic can have on patients with established psychopathology, as well as those without prior history. Difficulties in distinguishing ‘normal paranoia’ around the illness and psychosis are best managed by a mental healthcare practitioner.
Children and COVID-19
Children’s mental health has been overshadowed by the drastic and necessary measures taken to curb the spread of infection. The first onset of mental disorders typically occur in childhood or adolescence.(28) It is therefore of concern that in a recent survey conducted on primary school children in Hubei Province in China to evaluate the impact of home confinement on the mental health of children, increased rates of depressive and anxiety symptoms were found, and the authors concluded that “serious infectious diseases may influence the mental health of children as other traumatic experiences do.”(29) The direct impact on a child may be related to: anxiety and uncertainty about an unfamiliar infectious condition, contraction of the virus (with the potential for self-isolation, quarantine in hospital, and separation from family), having vulnerabilities to contracting the illness (e.g. being immunocompromised or respiratory disease), or having a loved one experience or die from COVID-19.(30) A child’s reaction to novel situations depends on various factors (summarised in Table 1).
Table 1:
Determinants of children’s reactions to novel situations
| Individual | Family | Environmental |
|---|---|---|
| • Developmental stage | • Communication styles | • Peer relationships |
| • Temperament | • Parental psychopathology | • Social support systems |
| • Coping strategies | • Home stability | • Early adversity |
| • Pre-existing illness | • Interpersonal relationships | • Substance use |
| • Resilience | • Modelled behaviour | • Social media |
| • School |
Social interactions are an important component of a child’s emotional development and their capacity for social competence.(31) School closure has resulted in academic and social losses, but in South Africa there are further challenges due to limited access to online education, malnutrition (with the suspension of school feeding programmes), and the lack of provision of school-based therapeutic interventions for children with disabilities (e.g. occupational therapy). The implementation of home confinement has also resulted in social isolation, school closure, play restrictions and a major lifestyle and routine adjustment. Parents staying at home may not always translate into more child-focused interactions. Additionally, lockdown restrictions limit the potential psychological benefits of exercise and physical activity for children. Many South African children live in overcrowded, confined spaces and do not have access to private outdoor areas. Financial strain is a potent parental stressor and may have an impact on family stability. Co-parenting, custody arrangements, and movement of children between households during lockdown might also lead to added stress in children. National epidemiological data is guiding the proposed re-opening of schools but there are legitimate concerns about the sector’s ability to implement measures to limit transmission (e.g. maintenance of social distancing in the classroom and the playground, provision of adequate protective apparel and sanitisation, conduction of screening protocols, psychological first aid training, etc.).
Healthcare workers
Healthcare workers are employed in environments that regularly present them with often unique and hazardous challenges, many of which are seen as an inherent part of work responsibilities. COVID-19 pandemic introduced additional work hazards in the healthcare environment.(31) Globally, various difficulties have been exacerbated due to the pandemic and newer challenges have emerged. These include the requirement for much stricter biosecurity measures, the constant risk of contracting the disease, increased workloads, concerns about putting family members at risk and the stigma faced by healthcare workers.(1) The World Health Organisation (WHO) has acknowledged an increased risk of anxiety amongst healthcare workers and a possible increase in burnout and PTSD. (32–34) Healthcare workers have also been faced with significant shortages of personal protective equipment, the lack of specific treatments, constant media coverage and a sense of not being supported adequately.(2) Additionally, reasons for psychological distress include fears of contracting the virus, passing on the virus to families, increased patient load and staff shortages.(35,36)
One cross-sectional study of healthcare workers in multiple hospitals in China between 29 January and 3 February 2020 assessed the mental health outcomes and associated factors among healthcare workers who were involved in managing COVID-19 patients.(35) In this study, 50.4% of participants reported symptoms of depression, 44.6% anxiety, 34.0% insomnia and 71.5% distress. Symptoms were more severe across all measurements among nurses, women, frontline workers and those working in Wuhan, the epicentre of the epidemic. There have also been reports of medical personnel succumbing to suicide during the COVID-pandemic. Even during non-pandemic circumstances, physicians and healthcare workers face elevated risks for suicide.(37)
A significant number of healthcare workers have been infected and succumbed to the disease internationally. This places an added burden on an already-constrained workforce, thereby increasing the workload and risks faced in the workplace, particularly as the number of admitted cases exponentially increase during peaks of the pandemic.(38) This may create a sense of powerlessness among healthcare workers and thus increase their vulnerability to adverse mental health outcomes. One of the most important factors that may have a detrimental effect on mental health outcomes is the assembly line conditions that may exist in the healthcare system,(3) which have become increasingly prevalent in the current pandemic.
The COVID-19 pandemic and the severe constraints on resources have thrown to the fore certain serious ethical dilemmas faced by frontline workers.(39,40) One of the most important of these has been patients’ access to life-saving interventions such as critical care beds and ventilation. Healthcare workers often have to make decisions on who these are allocated to. This responsibility can have negative effects on healthcare workers’ mental health outcomes. Specific interventions designed to meet the concerns and challenges faced by healthcare workers during the pandemic must include the availability and accessibility of mental health services to healthcare workers within the workplace to enable early detection and management of mental health issues.
CONCLUSION
This review highlights some of the possible psychiatric sequelae resulting from infection and experiences due to the recent COVID-19 pandemic. In addition to the focus on anxiety among afflicted patients, we expand the scope of COVID-19-related psychopathological presentations and disease trajectories that have been documented worldwide and that may arise in South Africa. Other important disorders such as trauma and stressor-related disorders and bereavement issues have not been included here. The global disruption in economies, health systems and daily life has inevitably made a comprehensive impact on the South African society. Future risks include limited allocation of funding to state and non-governmental mental health and social services, greater challenges to pre-existing service delivery limitations and threats to quality of care. We caution the extrapolation of current research findings on COVID-19 and encourage a critical appraisal of early studies on the disease. We offer this broader review of the psychopathological impacts due to and exacerbated by the COVID-19 pandemic and offer further insight into the possible psychiatric presentations that clinicians may face in the near future and to prepare health systems as the pandemic escalates in South Africa.
Table 2:
Considerations for special groups of children who are at elevated risk of psychiatric morbidity during COVID-19
| Special groups | |
|---|---|
| Pre-existing mental illness | • Specific concerns include the exacerbation of symptoms, non-compliance to treatment, and difficulties in adjusting to new routines. |
| • Children with autistic spectrum disorders do not adapt well to change, and the wearing of masks is sometimes problematic in those with tactile sensitivities. | |
| • Caregivers of children with OCD, who may have contamination obsessions or compulsive hand washing, find it challenging to navigate the need for sanitising. | |
| • Confinement and the lack of sufficient physical activity can worsen the low frustration tolerance of children with Attention Deficit Hyperactivity Disorder. | |
| Institution-based children | • Most of the emphasis on children housed in children’s homes, juvenile detention centres, child and youth care centres and ‘places of safety’, has been on curbing the transmission of COVID-19. |
| • The poor conditions of most facilities, potential exposure to violence, lack of contact with family, and the suspension of academic and therapeutic programmes magnifies the unmet medical, mental health and social needs of this vulnerable population. | |
| Child-headed households | • There is a dearth of information on the psychosocial impact of the pandemic on child-only households in South Africa. |
| Survivors of maltreatment | • COVID-19 has had a deleterious effect on the victims of abuse in terms of diminished access to support structures (shelters, police, extended family, support groups). |
| • Poverty, overcrowding and unemployment have further contributed to increases in domestic and gender-based violence. | |
| Children with limited access to medical care | • International data (30,31) suggest a decrease in clinic visits, vaccinations and treatment follow-ups, and delays in screenings, referrals and assessments for various medical conditions. |
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th ed. Arlington (VA): American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry Published online May 18, 2020. Available from: 10.1016/S2215-0366(20)30203-0 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 3.Sommer IE, Bakker PR. What can psychiatrists learn from SARS and MERS outbreaks? Lancet Psychiatry Available from: 10.1016/S2215-0366(20)30219-4 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 4.O’Hanlon Inouye SK. Delirium: a missing piece in the COVID-19 pandemic puzzle. Age Ageing 2020; 1–2. 10.1093/ageing/afaa094 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 5.Ferrando SJ, Klepacz L, Lynch S, et al. COVID-19 Psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? Psychosomatics 2020. Available from: 10.1016/j.psym.2020.05.012 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 6.Varatharaj A, Thomas N, Ellul M, et al. UK-wide surveillance of neurological and neuropsychiatric complications of COVID-19: the first 153 Patients 2020. Available from: 10.2139/ssrn.3601761 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 7.Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun 2020. Available from: 10.1016/j.bbi.2020.04.027 [Accessed 19.05.2020] [DOI] [PMC free article] [PubMed]
- 8.Kim AW, Nyengerai T, Mendenhall E Evaluating the mental health impacts of the COVID-19 pandemic: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Available at SSRN. medRxiv. 2020. [DOI] [PMC free article] [PubMed]
- 9.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psych 2020. doi: 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed]
- 10.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psych. Res 2020. doi: 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed]
- 11.Banerjee D The other side of COVID-19: impact on obsessive compulsive disorder (OCD) and hoarding. Psych. Res 2020. doi: 10.1016/j.psychres.2020.112966 [DOI] [PMC free article] [PubMed]
- 12.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed]
- 13.Okusaga O, Yolken RH, Langenberg P, et al. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disorders 2011; 130(1–2):220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Joska JA, Stein DJ, Grant I. HIV and psychiatry 1st ed. London, UK: John Wiley & Sons Limited. 2014; 84. [Google Scholar]
- 15.Prusty BK, Gulve N, Govind S, et al. Active HHV-6 infection of cerebellar Purkinje cells in mood disorders. Front Microbiol 2018; 9:1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brietzke E, Magee T, Freire RCR, Gomes FA, Milev R. Three insights on psychoneuroimmunology of mood disorders to be taken from the COVID-19 pandemic. Brain, Behavior, & Immunity – Health 2020. doi: 10.1016/j.bbih.2020.100076 [DOI] [PMC free article] [PubMed]
- 17.Regger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019 A perfect storm? JAMA Psychiatry doi: 10.1001/jamapsychiatry.2020.1060 [DOI] [PubMed]
- 18.United Nations Development Programme. COVID-19: Looming crisis in developing countries threatens to devastate economies and ramp up inequality Available: https://www.undp.org/content/undp/en/home/news-centre/news/2020/COVID19_Crisis_in_developing_countries_threatens_devastate_economies.html [Accessed: 15.05.2020]
- 19.Oyesanya M, Lopez-Morinigo J, Dutta R. Systematic review of suicide in economic recession. World J Psych 2015;5(2): 243–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nordt C, Warnke I, Seifritz E, Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries. The Lancet Psychiatry 2015; 2(3):239–245. [DOI] [PubMed] [Google Scholar]
- 21.Kim YG, Moon H, Kim S, et al. Inevitable isolation and the change of stress markers in hemodialysis patients during the 2015 MERS-CoV outbreak in Korea. Scientific Report 2019; 9:5676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.South African Depression and Anxiety Group. SADAG’s Online Survey Findings on COVID-19 and Mental Health (21 April 2020) [Accessed 01.05.2020] http://www.sadag.org/index.php?option=com_content&viewarticle&id=3092:sadag-s-online-survey-findings-on-covid-19-and-mental-health-21-april-2020&catid=149:press-releases&Itemid=226
- 23.Mednick SA, Machon RA, Huttunen MO, Bonett D. Adult schizophrenia following prenatal exposure to an influenza epidemic. Arch Gen Psych 1988; 45(2):189–192. [DOI] [PubMed] [Google Scholar]
- 24.Vlessides M COVID-19 and psychosis: is there a link? Medscape Cited 2020 May 8. Available: https://wwww.medscape.com/viewarticle/930224 [Accessed 14.05.2020]
- 25.Luming L Challenges and priorities in responding to COVID-19 in inpatient psychiatry American Psychiatric Association. Last Updated 2020 Apr 23. Available: 10.1176/appi.ps.202000166 [Accessed 14.05.2020] [DOI] [PubMed] [Google Scholar]
- 26.Fischer M, Coogan AN, Faltraco F, Thome J. COVID-19 paranoia in a patient suffering from schizophrenic psychosis – a case report. Psych Res 2020. doi: 10.1016/j.psychres.2020.113001 [DOI] [PMC free article] [PubMed]
- 27.Psychosis in a patient with anxiety related to COVID-19: a case report. Psych Res 2020. doi: 10.1016/j.psychres.2020.113052 [DOI] [PMC free article] [PubMed]
- 28.Mental Health Facts. National Alliance on Mental Illness Available: https://www.nami.org/NAMI/media/NAMI-Media/Infographics/Children-MH-Facts-NAMI.pdf. [Accessed 21.05.2020]
- 29.Xie X, Xue Q, Zhou Y, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei province, China. JAMA Pediatrics 2020. doi: 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed]
- 30.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. New Engl J Med 2020. April. doi: 10.1056/NEJMp2008017 [DOI] [PubMed]
- 31.Guidance on Providing Pediatric Well-Care during COVID-19. American Academy of Pediatrics: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/guidance-on-providing-pediatric-well-care-during-covid-19/. [Accessed 21.05.2020]
- 32.Cullen W, Gulati G, Kelly B. Mental health in the COVID-19 pandemic. QJM: Inter J Med 2020; 113:311–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. WHO Timeline – COVID-19 2020. Available: https://www.who.int/news-room/detail/27-04-2020-who-timeline—covid-19 [Accessed 27.04.2020]
- 34.China Global Television Network. Why are COVID-19 doctors committing suicide? Available: https://newsus.cgtn.com/news/2020-04-29/Why-are-COVID-19-doctors-committing-suicide--Q4yi8yhYB2/index.html [Accessed 18.05.2020]
- 35.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open 2020; 3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xiong Y, Peng L. Focusing on health-care providers’ experiences in the COVID-19 crisis. The Lancet Global Health April 2020. Available: 10.1016/S2214-109X(20)30214-X [DOI] [PMC free article] [PubMed]
- 37.Duthell F, Aubert C, Pereira B, et al. Suicide among physicians and health care workers: a systematic review and meta-analysis. PloS ONE 2019. 10.1371/journal.pone.0226361 [DOI] [PMC free article] [PubMed]
- 38.Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China American Psychiatric Association. Last Updated 2020 May 7. Available: 10.1176/appi.ajp.2020.20030304 [Accessed 14.05.2020] [DOI] [PubMed] [Google Scholar]
- 39.Ross F The cost of ignoring our doctors’ mental health. USA Mental Health First Aid 12 February 2018. Available: www.mentalhealthfirstaid.org/external/2018/02/cost-ignoring-doctors-mental-health/ [Accessed 13.05.2020]
- 40.Gostin LO, Friedman EA, Wetter SA. Responding to COVID-19: how to navigate a public health emergency legally and ethically. Wiley Online Library 26 March 2020. Available: 10.10.1002/hast.1090. [Accessed 13.05.2020] [DOI] [PMC free article] [PubMed]


