Abstract
Purpose:
Given clinical activity of AR-42, an oral histone deacetylase inhibitor, in hematologic malignancies and preclinical activity in solid tumors, this phase 1 trial investigated the safety and tolerability of AR-42 in patients with advanced solid tumors, including neurofibromatosis type 2 associated meningiomas and schwannomas (NF2). The primary objective was to define the maximum tolerated dose (MTD) and dose-limiting toxicities (DLTs). Secondary objectives included determining pharmacokinetics and clinical activity.
Methods:
This phase I trial was an open-label, single-center, dose-escalation study of single-agent AR-42 in primary central nervous system and advanced solid tumors. The study followed a 3+3 design with an expansion cohort at the MTD.
Results:
Seventeen patients were enrolled with NF2 (n=5), urothelial carcinoma (n=3), breast cancer (n=2), non-NF2-related meningioma (n=2), carcinoma of unknown primary (n=2), small cell lung cancer (n=1), Sertoli cell carcinoma (n=1), and uveal melanoma (n=1). The recommended phase II dose is 60 mg three times weekly, for three weeks of a 28-day cycle. DLTs included grade 3 thrombocytopenia and grade 4 psychosis. The most common treatment-related adverse events were cytopenias, fatigue, and nausea. The best response was stable disease in 53% of patients (95%CI:26.6–78.7). Median progression-free survival (PFS) was 3.6 months (95%CI:1.2–9.1). Among evaluable patients with NF2 or meningioma (n=5), median PFS was 9.1 months (95%CI:1.9-not reached).
Conclusion:
Single-agent AR-42 is safe and well tolerated. Further studies may consider AR-42 in a larger cohort of patients with NF2 or in combination with other agents in advanced solid tumors.
NCT01129193 , registered 5/24/2010.
Keywords: histone deacetylase inhibitor, neurofibromatosis type 2, phase 1, pharmacokinetics, solid tumor
INTRODUCTION
Histone deacetylase (HDAC) enzymes catalyze removal of acetyl groups from lysine in proteins, including histone proteins, resulting in tight DNA interaction with the nucleosome, which regulates transcription.[1] This epigenetic regulation is performed by 18 HDAC proteins, that fall into four classes (I-IV).[2] HDACs have been implicated in hematologic and solid tumor malignancies through altered acetylation of histones and non-histone proteins involved in cell growth, differentiation, and apoptosis.[3–5] As a result, HDAC inhibitors have been developed as antineoplastic agents and have proven efficacy in some hematologic malignancies.[6] Vorinostat (suberoylanilide hydroxamic acid, SAHA) and romidepsin (depsipeptide) are approved for relapsed cutaneous T-cell lymphoma (CTCL) by the Food and Drug Administration (FDA).[7,8] Efficacy was also found in phase II trials of vorinostat in indolent non-Hodgkin’s lymphoma and diffuse large B cell lymphoma (DLBCL),[9–11] panobinostat in CTCL and Hodgkin’s lymphoma,[12,13] and mocetinostat (MGCD0103) in Hodgkin’s lymphoma, relapsed follicular lymphoma, and DLBCL.[14,15] However, the role of HDAC inhibitors in the treatment of solid tumors is less clear. There are no FDA approvals for single agent HDAC inhibitors, though phase II trials have shown activity of AN-9 (pivaloyloxymethyl butyrate) in metastatic non-small cell lung cancer (NSCLC)[16] and vorinostat in recurrent glioblastoma multiforme (GBM).[17]
AR-42 (previously licensed by Arno Therapeutics, now licensed by Recursion Pharma, REC-2282) is an orally bioavailable, small molecule pan-HDAC inhibitor containing hydroxamate-tethered phenylbutyrate, promoting histone H3 and H4 lysine acetylation, tubulin acetylation, inhibition of the PI3K/AKt pathway, cell-cycle arrest at G2, and apoptosis via a caspase-dependent mechanism.[18–22] In preclinical studies, AR-42 has activity in vitro in prostate cancer[22,23] and breast cancer[24] cell lines. AR-42 has activity both in vitro and in vivo in cell lines and animal models of CLL,[20] mantle cell lymphoma,[20] acute lymphoblastic leukemia/lymphoma,[20] multiple myeloma,[25] Burkitt lymphoma,[20] hepatocellular carcinoma,[26] urothelial carcinoma,[27,28] colon cancer,[29] embryonal carcinoma,[30] ovarian cancer,[31,32] pancreatic cancer,[33] vestibular schwannomas,[19] and meningiomas.[34] In fact, the activity of AR-42 was superior to that of vorinostat in Burkitt lymphoma mouse models.[20] Preclinical pharmacology studies in rodents showed that AR-42 penetrates the blood brain barrier, suggesting it may be effective in central nervous system (CNS) tumors.[19,35] A phase 1 trial of AR-42 in patients with multiple myeloma and T- and B-cell lymphomas found a maximum tolerated dose (MTD) of 40 mg three times weekly for three weeks of a 28-day cycle, with durable responses in a patient with multiple myeloma and a patient with mantle cell lymphoma, concluding that AR-42 is safe and that further investigation of combination regimens of AR-42 should be performed in lymphoma and multiple myeloma.[36]
In this phase 1 study in patients with primary CNS and advanced solid tumors, the primary objectives were to investigate the safety and tolerability of AR-42 given as a single agent by defining the MTD and describing dose-limiting toxicities (DLTs). The secondary objectives included description of preliminary clinical activity in patients with CNS and solid tumors, and determination of the pharmacokinetics (PK) of AR-42.
MATERIALS AND METHODS
Patients
This phase I trial (NCT01129193) was approved by The Ohio State University Cancer Institutional Review Board and written informed consent was obtained from all patients. The study was performed in accordance with the Declaration of Helsinki. Eligible patients included adults with histologically or cytologically confirmed advanced or recurrent solid tumors for which no standard therapy was available, or who declined available standard treatment. Effort was made to enroll patients with tumor types for which there was preclinical data supporting the use of AR-42. Up to three prior cytotoxic chemotherapy treatments in the metastatic setting and prior hormonal, biologic or targeted therapy were allowed. Patients were required to have adequate renal (creatinine ≤ 1.5 × upper limit of normal (ULN) or creatinine clearance ≥ 50 mL/min), hepatic (total bilirubin < 1.5 mg/dL, AST/ALT ≤ 2.5 × ULN or ≤ 5 × ULN with liver metastasis), and bone marrow function (absolute neutrophil count ≥1500/μL and platelets ≥ 100,000/μL). Patients were excluded if they had a prolonged QTc >450 ms in males and >470 ms in females, or symptomatic CNS metastases. Asymptomatic, treated brain metastases were allowed.
Study Design
This was a phase I, open-label, single-center, first-in-human, dose-escalation study of single-agent oral AR-42, which followed a 3+3 cohort design and included an expansion cohort at the MTD. In the dose escalation phase, the starting dose was 30 mg/day, one dose level below the MTD of 40 mg/day found in a previous phase I trial of this agent in patients with hematologic malignancies.[36] During stage A of the dose escalation, the dose for successive cohorts was increased by 100% until the first grade 2 drug-related (definite, probable, or possible) toxicity was observed in one patient, which initiated stage B. In stage B, three more patients were enrolled at the last dose level of stage A, then subsequent dose increases were by 33%, rounded to the nearest 10 mg. Intra-patient dose escalation was not allowed. The MTD was planned to be the highest dose at which no more than 1 of 6 patients experienced a DLT. Once the MTD was determined, up to an additional 10 patients could be enrolled at the MTD dose level to investigate the activity of AR-42.
AR-42 was obtained from Arno Therapeutics (Parsippany, NJ). The drug was administered orally on an empty stomach three times weekly, every other day, for three consecutive weeks of a 28-day cycle. Premedication included at least one antiemetic. Upfront prophylactic growth factors were not allowed, but could be used for neutropenic fever. Concurrent radiation was only allowed for palliation of pain from bone metastasis, and the irradiated area could not be used for response assessment. Treatment was continued until disease progression, unacceptable toxicity, or patient withdrawal from study.
Safety and Tolerability
In addition to close monitoring of physical exam, vital signs, performance status, and labs, electrocardiograms (EKGs) were performed frequently to monitor the QTc. Specifically, twelve-lead EKGs were obtained in triplicate pre-dose and 2, 4, 8, and 24 hours post-dose on cycle 1 days 1 and 19. EKGs were also collected prior to AR-42 administration on cycle 1 days 5 and 8, cycle 2 day 1, day 1 of every other subsequent cycle (i.e. C4D1, C6D1, etc.), and at the end of the study. Toxicities were graded based on the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) v4.0. A DLT was defined as any grade 3–4 non-hematologic adverse event during cycle 1, excluding clinically insignificant lab abnormalities that resolved within 24 hours, nausea/vomiting that resolved to grade 2 or less within 24 hours, or liver function test abnormalities that resolved to less than grade 1 within 7 days. Hematologic DLTs included grade 4 neutropenia for >7 days, febrile neutropenia, grade 3 neutropenia with infection, grade 3 thrombocytopenia, or grade 2 thrombocytopenia with clinically meaningful bleeding that occurred during cycle 1. Dose delays and dose reductions due to drug-related toxicities were performed per study protocol (Supplemental Table 1). Dose delays longer than 2 weeks for toxicity, or more than 4 weeks for any reason, resulted in removal from the study. Safety was evaluated in all patients who received at least one dose of AR-42. All patients were followed after the end of active study participation for toxicity evaluation for at least 30 days, or longer until resolution of treatment related adverse events.
Response Evaluation
Disease assessment was performed by computed tomography (CT) or magnetic resonance imaging (MRI) at baseline, and after every two cycles, approximately every 6–8 weeks. Response, progression, and stable disease were defined by the NCI Response Evaluation Criteria in Solid Tumors (RECIST) guidelines, v1.1.[37] Patients were evaluable for response if they had measurable disease at baseline and completed at least one cycle of treatment prior to repeat imaging, or had objective disease progression prior to the end of cycle 1. Patients were contacted monthly after the end of study participation to assess survival.
Statistical Methods
Patient characteristics, type and frequency of adverse events, as well as dose and toxicity characteristics were summarized through descriptive statistics. The proportion of patients with stable disease by dose level was summarized, and includes the exact 95% confidence interval for the overall proportion. For evaluable participants, progression free survival (PFS) was defined as the time from enrollment to the date of progression or to the date last known to have stable disease. Patients who began other treatments prior to disease progression were censored on the date of initiation of alternative therapy. The method of Kaplan and Meier summarized PFS time, with confidence intervals calculated based on the log-log transformation. The median PFS of the subsets of patients with CNS and non-CNS tumors were calculated post hoc. All reported p-values and confidence intervals were two-sided, and reported at the nominal level; all analyses were performed using Stata 15.0.
Pharmacokinetics
Plasma pharmacokinetic (PK) samples were collected to investigate AR-42 PK following the first dose (Day 1) and last dose (Day 19) of cycle 1. Plasma sampling time points included pre-dose and post-dose at 0.25, 0.5, 1, 1.5, 2, 4, 8, 10, 24 hours on cycle 1 days 1 and 19. An additional 48-hour sample was obtained post-dose on cycle 1, day 1. Plasma concentrations of AR-42 were measured using a validated LC-MS/MS method as previously described.[38,36]
Non-compartmental analysis (NCA) of plasma AR-42 concentration-time data was completed in WinNonlin (v.6.3, Pharsight, St. Louis, MO) to estimate PK parameters using trapezoidal linear interpolation with extravascular dosing. Uniform weighting and the BestFit method were used for terminal phase regression. Estimation of the elimination rate constant (λz) was estimated using regression of the last three or four measurable time points when an adjusted R2 value >0.85 could be obtained. Area under the curve from zero to 24 hours (AUC0–24h), terminal Half-life (t1/2), terminal volume of distribution (Vz/F), systemic plasma clearance (CL/F) and area under the curve from zero to infinity (AUC0–∞) were estimated and summarized using geometric mean and geometric standard deviation unless otherwise noted. To evaluate for association of cycle 1 pharmacokinetic parameters and incidence of grade 3 or 4 toxicities during cycle 1 or 2, the Mann Whitney U test was used to compare the Cmax, AUC0–24h, and CL/F between patients that experienced a grade 3 or 4 toxicity and patients that did not have a grade 3 or 4 toxicity.
RESULTS
Patients
Seventeen patients were enrolled between June 2012 and November 2013. Baseline demographics are shown in Table 1. The most common disease was NF2-associated schwannoma and meningioma (n=5), followed by urothelial carcinoma (n=3), breast cancer (n=2), non-NF2-related meningioma (n=2), carcinoma of unknown primary (n=2), small cell lung cancer (n=1), Sertoli cell carcinoma (n=1), and uveal melanoma (n=1). Going forward, NF2-associated schwannoma and meningioma will be referred to as “NF2” and non-NF2-related meningioma will be referred to as “meningioma.” Together NF2 and meningioma will be considered “CNS tumors” and the remaining solid tumors will be considered “non-CNS tumors.” Clinically, the two carcinomas of unknown primary were suspected to be urothelial carcinoma and pancreaticobiliary in origin. Patients were heavily pretreated with a median of 2 (range 0–3) prior systemic therapies.
Table 1.
Patient demographics and characteristics at baseline
| Characteristic | N = 17 |
|---|---|
| Median age (range) – year | 49 (20–80) |
| Gender - no. (%) | |
| Male | 6 (35.3) |
| Female | 11 (64.7) |
| Race - no. (%) | |
| White non-Hispanic | 15 (88.2) |
| Other | 2 (11.8) |
| ECOG performance status - no. (%) | |
| 0 | 10 (58.8) |
| 1 | 7 (41.2) |
| Primary tumor - no. (%) | |
| Neurofibromatosis type 2 | 5 (29.4) |
| Urothelial carcinoma | 3 (17.6) |
| Carcinoma of unknown primarya | 2 (11.8) |
| Breast | 2 (11.8) |
| Meningioma | 2 (11.8) |
| Small cell lung cancer | 1 (5.9) |
| Sertoli cell carcinoma of testis | 1 (5.9) |
| Uveal melanoma | 1 (5.9) |
| Prior lines of systemic therapy - no. (%) | |
| 0 | 5 (29.4) |
| 1–2 | 5 (29.4) |
| 3 | 7 (41.2) |
One likely urothelial carcinoma, one likely pancreaticobiliary
As shown in Table 2, three patients (cohort 1A) were enrolled at the starting dose of 30 mg with no DLTs. The dose was increased to 60 mg (cohort 2A), where the second patient experienced grade 2 thrombocytopenia, so dose escalation phase B was initiated. Three more patients were enrolled at 60 mg (cohort 1B) with one patient having a DLT of grade 3 thrombocytopenia. Another three patients were initiated at 60 mg (cohort 1B), with a fourth patient enrolled to replace a patient who was non-compliant and not evaluable. There were no DLTs in this group. At the 60 mg dose, there were two patients that required a dose reduction and four that had a dose delay. The dose was then increased by 33% to 80 mg, at which two patients were enrolled (cohort 2B). The first patient withdrew after two doses and was replaced; the second patient experienced grade 3 thrombocytopenia and a grade 4 psychiatric disorder, which was considered a DLT. At this point, although two DLTs were not reached at the 80 mg dose, the decision was made to define the recommended phase II dose (RP2D) as 60 mg once daily, three times weekly, every other day, for three consecutive weeks of a 28-day cycle. The episode of psychosis was only “possibly” related to AR-42 and may have been due to concurrent medications or underlying psychiatric illness, however, given the severity of the grade 4 psychosis in the context of multiple patients with transient, mild episodes of confusion in this study and the phase I study of AR-42 in hematologic malignancies,[36] as well as the frequency of thrombocytopenia, it was felt to be unsafe to enroll further patients at the 80 mg dose. This decision was further supported by the MTD of only 40 mg in the phase I trial of AR-42 in hematologic malignancies.[39] The expansion cohort enrolled three patients at the RP2D, for a total of twelve patients at 60 mg.
Table 2.
Dose levels with number of patients, dose delays, dose reductions and dose limiting toxicities (DLTs)
| Dose level | AR-42 dose (mg) | No. of patients enrolled (N=17) | No. of dose delays | No. of dose reductions | No. of patients with a DLT | Description of DLT |
|---|---|---|---|---|---|---|
| 1A | 30 | 3 | 0 | 0 | 0 | --- |
| 2A | 60 | 2a | 0 | 0 | 0 | --- |
| 1B | 60 | 7b | 4 | 2 | 1 | Thrombocytopenia (grade 3) |
| 2B | 80 | 2c | 0 | 0 | 1 | Thrombocytopenia (grade 3)d Psychiatric disorder (grade 4)d |
| Expansion cohort | 60 | 3 | 0 | 0 | --- |
Grade 2 thrombocytopenia experienced by second patient, so advanced to stage B.
Includes 2 cohorts of 3 patients, plus one patient to replace a patient who was non-compliant and not evaluable.
First patient withdrew after 2 doses due to progression and was replaced. Second patient experienced a DLT.
Grade 3 thrombocytopenia and grade 4 psychiatric disorder at dose level 2B occurred in the same patient, counting as one DLT.
The median duration of treatment was 85 days (range 5–838), equivalent to 3.0 cycles (range 0.2–29.9). Most commonly, patients stopped the study drug due to progression of disease (n=12), followed by patient decision to discontinue treatment resulting in withdrawal from the study (n=3).
Safety and Tolerability
Seventeen patients were evaluable for toxicity. As shown in Table 3, the most common treatment-related adverse events (TRAEs) of any grade were thrombocytopenia (n=13), fatigue (n=11), nausea (n=10), anemia (n=10), elevated creatinine (n=8), leukopenia (n=8), lymphopenia (n=7), hypophosphatemia (n=7), neutropenia (n=7), and diarrhea (n=6). Grade 3 TRAEs included thrombocytopenia (n=5), lymphopenia (n=3), hypophosphatemia (n=3), nausea (n=2), anemia (n=2), anorexia (n=1), weight loss (n=1), hematuria (n=1), and venous thromboembolism (n=1). The only grade 4 TRAE was psychosis at the 80 mg dose. There were no treatment-related deaths. The only cardiac toxicity observed was one patient with a grade 1 QTc prolongation. All treatment-related adverse events are listed in Supplemental Table 2 and all overall adverse events are listed in Supplemental Table 3.
Table 3.
All grade 3–4 and most common grade 1–2 treatment-related adverse events
| Grade 1–2, n (%) | Grade 3–4, n (%) | All grades, n (%) | |
|---|---|---|---|
| Thrombocytopenia | 8 (47.1%) | 5 (29.4%) | 13 (76.5%) |
| Fatigue | 11 (64.7%) | --- | 11 (64.7%) |
| Nausea | 8 (47.1%) | 2 (11.8%) | 10 (58.8%) |
| Anemia | 8 (47.1%) | 2 (11.8%) | 10 (58.8%) |
| Elevated creatinine | 8 (47.1%) | --- | 8 (47.1%) |
| Leukopenia | 8 (47.1%) | --- | 8 (47.1%) |
| Lymphopenia | 4 (23.5%) | 3 (17.6%) | 7 (41.2%) |
| Hypophosphatemia | 4 (23.5%) | 3 (17.6%) | 7 (41.2%) |
| Neutropenia | 7 (41.2%) | --- | 7 (41.2%) |
| Diarrhea | 6 (35.3%) | --- | 6 (35.3%) |
| Anorexia | 4 (23.5%) | 1 (5.9%) | 5 (29.4%) |
| Hypoalbuminemia | 5 (29.4%) | --- | 5 (29.4%) |
| Vomiting | 4 (23.5%) | --- | 4 (23.5%) |
| Dizziness | 4 (23.5%) | --- | 4 (23.5%) |
| Myalgia | 4 (23.5%) | --- | 4 (23.5%) |
| Constipation | 4 (23.5%) | --- | 4 (23.5%) |
| Elevated alanine aminotransferase (ALT) | 4 (23.5%) | --- | 4 (23.5%) |
| Elevated alkaline phosphatase | 4 (23.5%) | --- | 4 (23.5%) |
| Weight loss | 2 (11.8%) | 1 (5.9%) | 3 (17.6%) |
| Elevated aspartate aminotransferase (AST) | 3 (17.6%) | --- | 3 (17.6%) |
| Impaired concentration | 3 (17.6%) | --- | 3 (17.6%) |
| Dry mouth | 3 (17.6%) | --- | 3 (17.6%) |
| Dysgeusia | 3 (17.6%) | --- | 3 (17.6%) |
| Headache | 3 (17.6%) | --- | 3 (17.6%) |
| Hyponatremia | 3 (17.6%) | --- | 3 (17.6%) |
| Cough | 2 (11.8%) | --- | 2 (11.8%) |
| Dehydration | 2 (11.8%) | --- | 2 (11.8%) |
| Limb edema | 2 (11.8%) | --- | 2 (11.8%) |
| Hypermagnesemia | 2 (11.8%) | --- | 2 (11.8%) |
| Hypernatremia | 2 (11.8%) | --- | 2 (11.8%) |
| Hypersomnia | 2 (11.8%) | --- | 2 (11.8%) |
| Elevated international normalized ratio (INR) | 2 (11.8%) | --- | 2 (11.8%) |
| Psychiatric disorder | --- | 1 (5.9%) | 1 (5.9%) |
| Thromboembolic event | --- | 1 (5.9%) | 1 (5.9%) |
| Hematuria | --- | 1 (5.9%) | 1 (5.9%) |
During cycle one, one patient (5.9%) developed a grade 4 toxicity, five patients (29.4%) developed at most a grade 3 toxicity, five patients (29.4%) developed at most a grade 2 toxicity, four patients (23.5%) developed at most a grade 1 toxicity, and the remaining two patients (11.8%) experienced no toxicities. In subsequent cycles, there were no patients with a grade 4 toxicity, two of the patients with grade 2 toxicity during cycle one developed a grade 3 toxicity, and three of the patients with grade 1 toxicity during cycle one developed a grade 2 toxicity. One patient, who remained on study for 69 days, never experienced any toxicity of any grade.
The only dose delay or reduction during cycle 1 was for a patient on 60 mg, who experienced the DLT of grade 3 thrombocytopenia. In subsequent cycles, there were four patients at the 60 mg dose who required dose delays and one of these four patients required a dose reduction. The dose delays, regardless of attribution, were due to creatinine elevation, thrombocytopenia, upper respiratory infection, and a hospitalization for fatigue and urinary tract infection. The dose reduction for one patient during cycle 2 was due to fatigue, which was ultimately attributed to hypopituitarism from previous cranial irradiation for meningioma.
Response
Fifteen patients were evaluable for response. Two of the seventeen patients did not complete cycle 1, one due to non-compliance and one due to a DLT (grade 4 psychosis) without evidence of progression, and thus were not evaluable. The best overall response was stable disease, seen in 1 of 3 patients who received 30 mg and 7 of 11 patients who received 60 mg, resulting in 8 of 15 patients, or 53% (95% CI: 26.6–78.7) of patients experiencing stable disease. Among the patients with stable disease, three patients had a 5–18% decrease in the sum of the diameters of the target lesions from baseline. These patients had NF2, Sertoli cell carcinoma, and carcinoma of unknown primary, suspected to be urothelial carcinoma.
As shown in Figure 1, the median PFS time was 3.6 months (95% CI 1.2–9.1). In patients with non-CNS solid tumors (n=10), median PFS was 1.7 months (95% CI: 0.1 – 5.0). The two patients that were non-evaluable for response had CNS tumors, but among the remaining evaluable patients with NF2 or meningioma (n=5), median PFS was 9.1 months (95% CI: 1.9-not reached (NR)). All evaluable patients with NF2 or meningioma received 60 mg.
Figure 1.
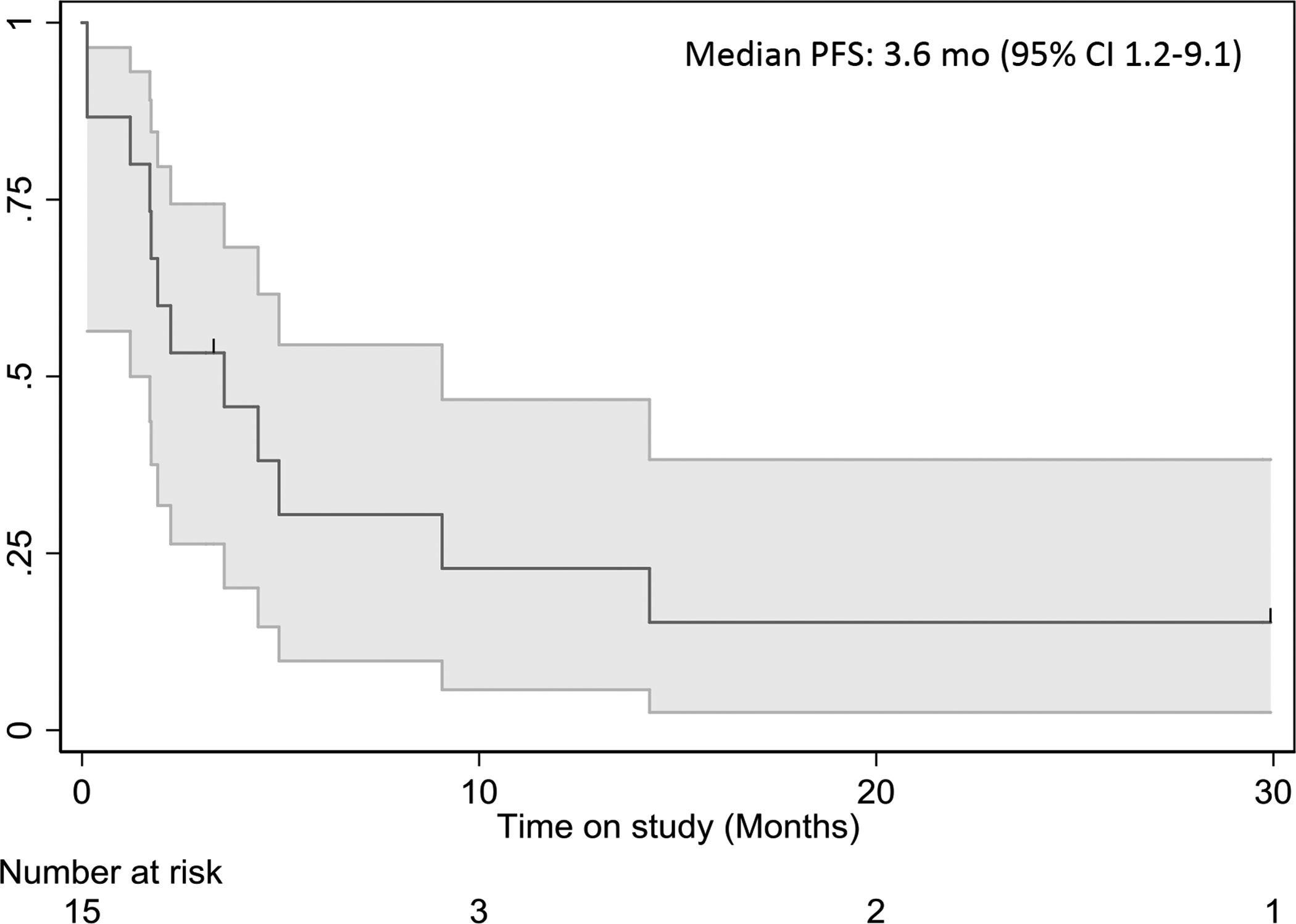
Median PFS of primary CNS and advanced solid tumors treated with AR-42.
Pharmacokinetics
Analysis was performed using data from 3, 12, and 2 patients at the 30 mg, 60 mg, 80 mg dose levels, respectively. Mean plasma concentration and time profiles of AR-42 in patients on day 1 and day 19 after an oral administration of AR-42 are shown in Figure 2. Individual plasma AR-42 peak plasma concentration (Cmax) and AUC0–24hr values ranged from 0.54 to 3.25 μM and 4.93 to 27.6 μM*Hr across the dose range, respectively. The elimination rate constant λz was not estimable on day 19 for two patients taking 60 mg daily. Elimination t1/2 ranged from approximately 8 to 13 hours. AR-42 did not accumulate in these patients when given 3 times weekly for three weeks of a four-week cycle. Cmax, AUC0–24 and AUC0–∞ remained consistent between Day 1 and Day 19 (Supplemental Table 4). AUC0–24 and AUC0–∞ were roughly 50% higher in the 80 mg dose group as compared to the 60 mg dose group, which suggests a potential loss of dose proportionality. However, only two patients were treated at the 80 mg dose level, and a conclusion cannot be drawn.
Figure 2.
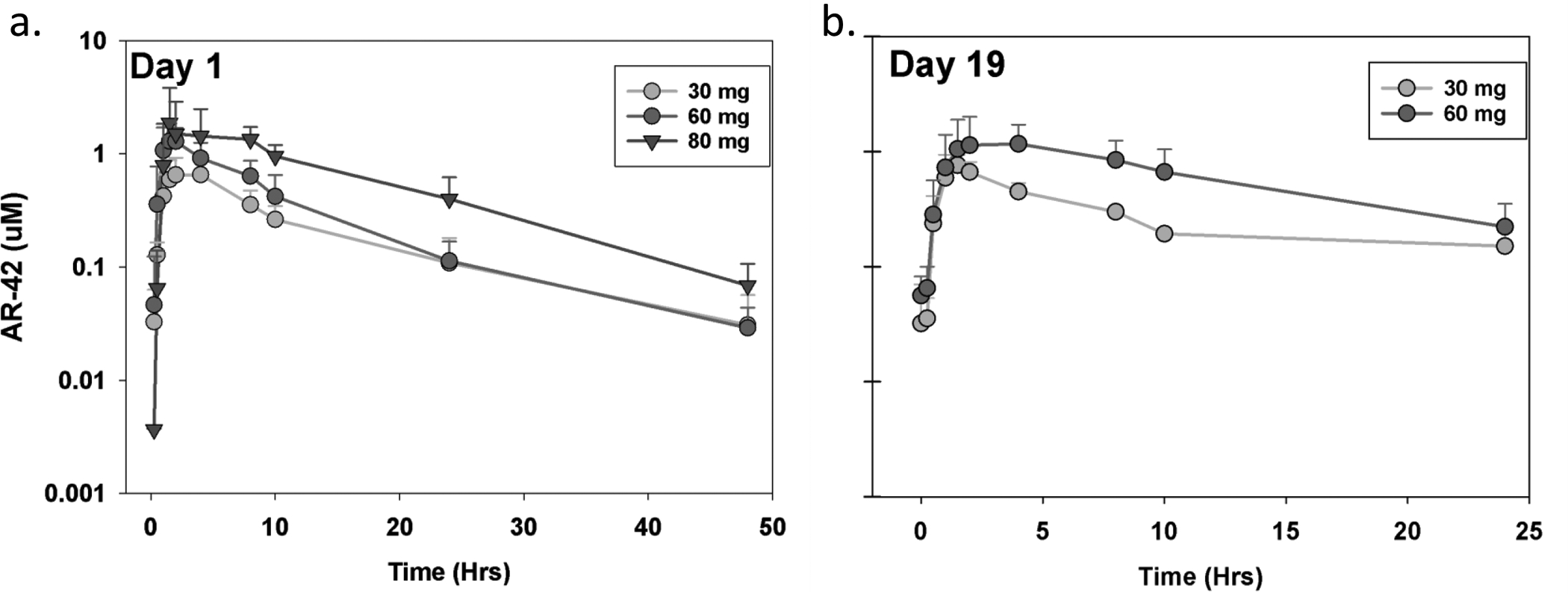
Pharmacokinetics by dose on a) Day 1 and b) Day 19.
During cycle 1 and 2, patients that experienced a grade 3 or 4 toxicity had significantly higher median Cmax (1.54 uM vs. 1.04 uM, p=0.0016) and median AUC (16.45 μM*hr vs 11.3 μM*hr, p=0.036), but not median CL/F (10.48 L/hr vs 15.8 L/hr, p=0.0745), compared to patients that did not experience a grade 3 or 4 toxicity. These data support an observable plasma exposure-toxicity relationship, which may be useful for management of grade 3–4 toxicities in future studies.
DISCUSSION
This phase 1 study demonstrates that AR-42 is safe and tolerable in patients with primary CNS and advanced solid tumors. The phase II recommended dose is 60 mg orally once daily, three times weekly, every other day, for three consecutive weeks of a 28-day cycle.
The most common toxicities were cytopenias, fatigue, and nausea. The toxicities seen with AR-42 are consistent with the reported side effect profile of other HDAC inhibitors. Previously reported side effects of AR-42 and other HDAC inhibitors include cytopenias, fatigue, nausea, vomiting, diarrhea, anorexia, weight loss, asthenia, dehydration, and non-specific GI symptoms.[17,9,10,40,41,36,42–44] The most common toxicity of any grade was thrombocytopenia, but there were no clinically significant bleeding events, and platelet count improved with dose hold and reduction, if necessary. Thrombocytopenia was also common in the phase I trial of AR-42 in hematologic malignancies (16 of 27 patients), but the degree was less severe here, with no grade 4 thrombocytopenia. Historically, there has been concern for cardiac toxicity with HDAC inhibitors, particularly QTc prolongation, non-specific ST and T wave changes, and arrhythmias.[45–47] In this study there was only one patient who experienced a grade 1 QTc prolongation at 30 mg and there were no other cardiac toxicities observed at any dose. This is consistent with the clinically insignificant QT prolongation seen in the phase I study of AR-42 in hematologic malignancies, where 8 of 27 patients had a grade 1 QTc prolongation, with a mean QTc change of 27.4 ms, which all spontaneously resolved without dose hold or adjustment.[36] Overall, AR-42 is safe and tolerable.
Although this was only a phase I study, not designed to evaluate efficacy, the anti-tumor activity of this small, heterogeneous cohort of patients is reported. The best response to AR-42 was stable disease in 53% (95% CI: 26.6–78.7) of patients. The overall cohort median PFS was 3.6 months (95% CI 1.2–9.1) with the wide confidence interval likely due to the inclusion of patients with NF2, which has a more indolent natural history than the non-CNS malignant solid tumors included in this study. In patients with non-CNS solid tumors, median PFS was 1.7 months (95% CI: 0.1 – 5.0). The seeming lack of activity of single-agent AR-42 seen here in advanced non-CNS solid tumors is consistent with phase II studies of other single agent HDAC inhibitors in solid tumors including romidepsin in metastatic castrate resistant prostate cancer,[42] GBM,[48] and colorectal cancer,[49] panobinostat in metastatic renal cell carcinoma,[43] and vorinostat in recurrent GBM,[17] ovarian carcinoma, primary peritoneal carcinoma,[50] head and neck cancer,[41] NSCLC, colorectal cancer, and metastatic breast cancer.[51,40] Overall, the lack of single-agent activity of AR-42 in non-CNS solid tumors is consistent with the limited activity of other single agent HDAC inhibitors in solid tumors, and does not warrant further investigation.
NF2 is a rare disease of multiple, slow-growing tumors for which the standard of care is surgery and radiation, with no effective systemic therapies.[52,53] In this study, the median PFS was 9.1 months (95% CI: 1.9-NR) in patients with NF2 or meningioma, with 1 of these 5 patients having longer than 27 months of follow up without progression. Based on preclinical studies, the mechanism of action of AR-42 in NF2 involves deacetylation and deactivation of AKT. The NF2 gene encodes the tumor suppressor protein merlin and loss of merlin in NF2 results in proliferation of Schwann and leptomeningeal cells, in part through activation of the PI3K/AKT pathway.[54] AR-42 dephosphorylates and deactivates AKT.[55] In preclinical studies in vitro, AR-42 decreased AKT phosphorylation and suppressed proliferation of schwannoma and meningioma cell lines by cell cycle arrest at G2 and apoptosis.[18] In vivo, AR-42 crossed the blood brain barrier in a mouse model and suppressed peripherally implanted xenograft and allograft schwannoma growth.[19] Based on the current preclinical and clinical data for AR-42 in NF2, and given the lack of effective systemic therapies for this disease, further investigation of the clinical activity of AR-42 in a larger cohort of patients with NF2 may be considered. For future clinical studies in NF2, in accordance with published suggested response criteria in NF2, use of volumetric radiographic measurements and validated hearing response assessments with word recognition scores should be considered.[53] Also, notably, one of the five patients with NF2 in this study eventually chose to discontinue treatment after many months on therapy due to persistent mild side effects, highlighting that it may be difficult for young patients to adhere to a long-term treatment with even low-grade, symptomatic toxicities. This population may benefit from the minimum effective dose, rather than the maximum tolerated dose.
Future studies should explore AR-42 in combination with other cancer-directed therapies for advanced solid tumors. There have been attempts to combine HDAC inhibitors with DNA damaging agents including platinum-based chemotherapy,[56] PARP inhibitors,[57] topoisomerase inhibitors,[58] and radiation,[59] as well as other cytotoxic chemotherapy agents,[60] proteasome inhibitors,[61] hormonal therapy,[62] tyrosine kinase inhibitors,[63] hypomethylating agents,[64] rituximab,[65] bevacizumab,[66] and immune checkpoint inhibitors.[67–69] The only FDA approved HDAC inhibitor in combination is panobinostat with bortezomib and dexamethasone for relapsed or refractory multiple myeloma.[70] Specifically AR-42 has shown preclinical activity when combined with decitabine for AML, doxorubicin for osteosarcoma, 5-FU for breast cancer, cisplatin for urothelial carcinoma, and pazopanib for melanoma cells resistant to trametinib plus dabrafenib.[71–75] A recent preclinical study also demonstrated potential for AR-42 to overcome anabolic resistance in cancer-associated cachexia.[76] AR-42 and other HDAC inhibitors downregulate thymidylate synthetase, so AR-42 may be able to overcome resistance to pemetrexed or 5-FU, and AR-42 has also been shown to modulate ERBB2 receptor phosphorylation.[77,74,78–80] Both of these effects may be exploited with combination therapies. A phase I study of AR-42 combined with decitabine in thirteen patients with acute myeloid leukemia (AML) demonstrated similar safety and toxicities to those reported here, though the biological endpoint of increased miR-29b expression was not reached, and AR-42 will not be explored further in AML.[39] Unfortunately, the only phase I study of AR-42 in combination for a solid tumor to date, which used AR-42 with pazopanib in sarcoma and kidney cancer, was terminated due to two DLTs at the first dose level (NCT02795819), highlighting the risk for higher toxicity with combination regimens.
Finally, patient selection for genetic or molecular markers may identify a subset of patients most likely to respond to AR-42 and other HDAC inhibitors. Unfortunately, despite encouraging preclinical studies, in a phase II study that enrolled patients with urothelial carcinoma with mutations or deletions in CREB binding protein (CREBBP) and/or E1A binding protein p300 (EP300), mocetinostat failed to show efficacy.[81] However, for example, mutations in BRCA1-associated protein (BAP1), which predispose to mesotheliomas, uveal melanomas, cutaneous melanoma, and renal cell carcinoma, dysregulate HDAC proteins and sensitize cells to HDAC inhibitors.[82–84] Targeting solid tumors with BAP1 mutations may reveal a subset of patients that respond to AR-42.
In summary, AR-42 is safe and tolerable in primary CNS and advanced solid tumors. A larger study is needed to evaluate efficacy in NF2. Consideration may be given to studies of AR-42 in combination with other agents for solid tumors and in subsets of patients with sensitizing mutations.
Supplementary Material
Funding:
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Numbers U01CA076576 and R01CA201382. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Craig C. Hofmeister has received research grants from Takeda and Oncolytics Biotech; research and personal grants from Janssen, BMS, Sanofi, Nektar, Karyopharm, Imbrium and Oncopeptides, all outside the submitted work.
This study was performed under the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of the Ohio State University (Protocol 2010C0006, approval date 3/24/2010).
Amir Mortazavi is on the advisory board for Seattle Genetics and Pfizer and is on the scientific advisory board for Debiopharm Group. His institution (not him) has received research funding from Acerta Pharma, Genentech, Roche, Merck, Novartis, Seattle Genetics, Astellas Pharma, Mirati Therapeutics, and Bristol-Myers Squibb.
Footnotes
Conflicts of interest:
Christopher C. Coss, Sophia G. Liva, and Mitch A. Phelps are listed as inventors on a provisional patent for AR-42 for cancer-related cachexia (U.S. Patent Application No. 62/898,992).
The other authors declare no potential conflict of interest.
The Ohio State University (OSU) holds the patent on the investigational drug AR-42 (US 10/597,022). The Technology Commercialization Office has licensed AR-42 (now called REC-2282) to Recursion Pharmaceuticals using the institution’s standard terms, conditions and approval process, in which no author participated. To assure absence of institutional conflict of interest in assessment of response and attribution of toxicity, both were reviewed by the Cancer Therapy Evaluation Program (CTEP) of the National Cancer Institute (NCI) prior to reporting results. Safety issues related to dose increases and attribution of response were monitored by the Ohio State University Data Safety Monitoring Committee and the OSU Cancer Center Institutional Review Board (IRB).
Availability of data and materialx: The authors confirm that the data supporting the findings of this study are available within the article and/or supplementary materials. Further data are available on request from the corresponding author, Amir Mortazavi. The data are not publicly available to prevent compromise of the privacy of the research participants.
D. Bradley Welling is a consultant for CereXis who is a subsidiary of Recursion Pharamceuticals.
REFERENCES
- 1.Choudhary C, Kumar C, Gnad F, Nielsen ML, Rehman M, Walther TC, Olsen JV, Mann M (2009) Lysine acetylation targets protein complexes and co-regulates major cellular functions. Science 325 (5942):834–840. doi: 10.1126/science.1175371 [DOI] [PubMed] [Google Scholar]
- 2.Seto E, Yoshida M (2014) Erasers of histone acetylation: the histone deacetylase enzymes. Cold Spring Harb Perspect Biol 6 (4):a018713. doi: 10.1101/cshperspect.a018713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y, Seto E (2016) HDACs and HDAC Inhibitors in Cancer Development and Therapy. Cold Spring Harb Perspect Med 6 (10). doi: 10.1101/cshperspect.a026831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dawson MA, Kouzarides T (2012) Cancer epigenetics: from mechanism to therapy. Cell 150 (1):12–27. doi: 10.1016/j.cell.2012.06.013 [DOI] [PubMed] [Google Scholar]
- 5.Glozak MA, Seto E (2007) Histone deacetylases and cancer. Oncogene 26 (37):5420–5432. doi: 10.1038/sj.onc.1210610 [DOI] [PubMed] [Google Scholar]
- 6.Federico M, Bagella L (2011) Histone deacetylase inhibitors in the treatment of hematological malignancies and solid tumors. J Biomed Biotechnol 2011:475641. doi: 10.1155/2011/475641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olsen EA, Kim YH, Kuzel TM, Pacheco TR, Foss FM, Parker S, Frankel SR, Chen C, Ricker JL, Arduino JM, Duvic M (2007) Phase IIb multicenter trial of vorinostat in patients with persistent, progressive, or treatment refractory cutaneous T-cell lymphoma. J Clin Oncol 25 (21):3109–3115. doi: 10.1200/JCO.2006.10.2434 [DOI] [PubMed] [Google Scholar]
- 8.Piekarz RL, Frye R, Turner M, Wright JJ, Allen SL, Kirschbaum MH, Zain J, Prince HM, Leonard JP, Geskin LJ, Reeder C, Joske D, Figg WD, Gardner ER, Steinberg SM, Jaffe ES, Stetler-Stevenson M, Lade S, Fojo AT, Bates SE (2009) Phase II multi-institutional trial of the histone deacetylase inhibitor romidepsin as monotherapy for patients with cutaneous T-cell lymphoma. J Clin Oncol 27 (32):5410–5417. doi: 10.1200/JCO.2008.21.6150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crump M, Coiffier B, Jacobsen ED, Sun L, Ricker JL, Xie H, Frankel SR, Randolph SS, Cheson BD (2008) Phase II trial of oral vorinostat (suberoylanilide hydroxamic acid) in relapsed diffuse large-B-cell lymphoma. Ann Oncol 19 (5):964–969. doi: 10.1093/annonc/mdn031 [DOI] [PubMed] [Google Scholar]
- 10.Kirschbaum M, Frankel P, Popplewell L, Zain J, Delioukina M, Pullarkat V, Matsuoka D, Pulone B, Rotter AJ, Espinoza-Delgado I, Nademanee A, Forman SJ, Gandara D, Newman E (2011) Phase II study of vorinostat for treatment of relapsed or refractory indolent non-Hodgkin’s lymphoma and mantle cell lymphoma. J Clin Oncol 29 (9):1198–1203. doi: 10.1200/JCO.2010.32.1398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogura M, Ando K, Suzuki T, Ishizawa K, Oh SY, Itoh K, Yamamoto K, Au WY, Tien HF, Matsuno Y, Terauchi T, Yamamoto K, Mori M, Tanaka Y, Shimamoto T, Tobinai K, Kim WS (2014) A multicentre phase II study of vorinostat in patients with relapsed or refractory indolent B-cell non-Hodgkin lymphoma and mantle cell lymphoma. Br J Haematol 165 (6):768–776. doi: 10.1111/bjh.12819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duvic M, Dummer R, Becker JC, Poulalhon N, Ortiz Romero P, Grazia Bernengo M, Lebbe C, Assaf C, Squier M, Williams D, Marshood M, Tai F, Prince HM (2013) Panobinostat activity in both bexarotene-exposed and -naive patients with refractory cutaneous T-cell lymphoma: results of a phase II trial. Eur J Cancer 49 (2):386–394. doi: 10.1016/j.ejca.2012.08.017 [DOI] [PubMed] [Google Scholar]
- 13.Younes A, Sureda A, Ben-Yehuda D, Zinzani PL, Ong TC, Prince HM, Harrison SJ, Kirschbaum M, Johnston P, Gallagher J, Le Corre C, Shen A, Engert A (2012) Panobinostat in patients with relapsed/refractory Hodgkin’s lymphoma after autologous stem-cell transplantation: results of a phase II study. J Clin Oncol 30 (18):2197–2203. doi: 10.1200/JCO.2011.38.1350 [DOI] [PubMed] [Google Scholar]
- 14.Crump M, Andreadis C, Assouline S, Rizzieri D, Wedgwood A, McLaughlin P, Laille E, Li Z, Martell RE, Younes A (2008) Treatment of relapsed or refractory non-hodgin lymphoma with the oral istoype-selective histone deacetylase inhibitor MGCD0103: interim results from a phase II study. Proc Am Soc Clin Oncol [Google Scholar]
- 15.Bociek RG, Kuruvilla J, Pro B, Wedgwood A, Li Z, Drouin M, Patterson T, Ward R, Martell RE, Younes A (2008) Isotype-selective histone deacetylase (HDAC) inhibitor MGCD0103 demonstrates clinical activity and safety in patients with relapsed/refractory classical Hodgkin Lymphoma (HL). Journal of Clinical Oncology [Google Scholar]
- 16.Reid T, Valone F, Lipera W, Irwin D, Paroly W, Natale R, Sreedharan S, Keer H, Lum B, Scappaticci F, Bhatnagar A (2004) Phase II trial of the histone deacetylase inhibitor pivaloyloxymethyl butyrate (Pivanex, AN-9) in advanced non-small cell lung cancer. Lung Cancer 45 (3):381–386. doi: 10.1016/j.lungcan.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 17.Galanis E, Jaeckle KA, Maurer MJ, Reid JM, Ames MM, Hardwick JS, Reilly JF, Loboda A, Nebozhyn M, Fantin VR, Richon VM, Scheithauer B, Giannini C, Flynn PJ, Moore DF Jr., Zwiebel J, Buckner JC (2009) Phase II trial of vorinostat in recurrent glioblastoma multiforme: a north central cancer treatment group study. J Clin Oncol 27 (12):2052–2058. doi: 10.1200/JCO.2008.19.0694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bush ML, Oblinger J, Brendel V, Santarelli G, Huang J, Akhmametyeva EM, Burns SS, Wheeler J, Davis J, Yates CW, Chaudhury AR, Kulp S, Chen CS, Chang LS, Welling DB, Jacob A (2011) AR42, a novel histone deacetylase inhibitor, as a potential therapy for vestibular schwannomas and meningiomas. Neuro Oncol 13 (9):983–999. doi: 10.1093/neuonc/nor072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacob A, Oblinger J, Bush ML, Brendel V, Santarelli G, Chaudhury AR, Kulp S, La Perle KM, Chen CS, Chang LS, Welling DB (2012) Preclinical validation of AR42, a novel histone deacetylase inhibitor, as treatment for vestibular schwannomas. Laryngoscope 122 (1):174–189. doi: 10.1002/lary.22392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lucas DM, Alinari L, West DA, Davis ME, Edwards RB, Johnson AJ, Blum KA, Hofmeister CC, Freitas MA, Parthun MR, Wang D, Lehman A, Zhang X, Jarjoura D, Kulp SK, Croce CM, Grever MR, Chen CS, Baiocchi RA, Byrd JC (2010) The novel deacetylase inhibitor AR-42 demonstrates pre-clinical activity in B-cell malignancies in vitro and in vivo. PLoS One 5 (6):e10941. doi: 10.1371/journal.pone.0010941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang S, Suvannasankha A, Crean CD, White VL, Chen CS, Farag SS (2011) The novel histone deacetylase inhibitor, AR-42, inhibits gp130/Stat3 pathway and induces apoptosis and cell cycle arrest in multiple myeloma cells. Int J Cancer 129 (1):204–213. doi: 10.1002/ijc.25660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu Q, Wang DS, Chen CS, Hu YD, Chen CS (2005) Structure-based optimization of phenylbutyrate-derived histone deacetylase inhibitors. J Med Chem 48 (17):5530–5535. doi: 10.1021/jm0503749 [DOI] [PubMed] [Google Scholar]
- 23.Lu Q, Yang YT, Chen CS, Davis M, Byrd JC, Etherton MR, Umar A, Chen CS (2004) Zn2+-chelating motif-tethered short-chain fatty acids as a novel class of histone deacetylase inhibitors. J Med Chem 47 (2):467–474. doi: 10.1021/jm0303655 [DOI] [PubMed] [Google Scholar]
- 24.Chao MW, Chu PC, Chuang HC, Shen FH, Chou CC, Hsu EC, Himmel LE, Huang HL, Tu HJ, Kulp SK, Teng CM, Chen CS (2016) Non-epigenetic function of HDAC8 in regulating breast cancer stem cells by maintaining Notch1 protein stability. Oncotarget 7 (2):1796–1807. doi: 10.18632/oncotarget.6427 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Canella A, Cordero Nieves H, Sborov DW, Cascione L, Radomska HS, Smith E, Stiff A, Consiglio J, Caserta E, Rizzotto L, Zanesi N, Stefano V, Kaur B, Mo X, Byrd JC, Efebera YA, Hofmeister CC, Pichiorri F (2015) HDAC inhibitor AR-42 decreases CD44 expression and sensitizes myeloma cells to lenalidomide. Oncotarget 6 (31):31134–31150. doi: 10.18632/oncotarget.5290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu YS, Kashida Y, Kulp SK, Wang YC, Wang D, Hung JH, Tang M, Lin ZZ, Chen TJ, Cheng AL, Chen CS (2007) Efficacy of a novel histone deacetylase inhibitor in murine models of hepatocellular carcinoma. Hepatology 46 (4):1119–1130. doi: 10.1002/hep.21804 [DOI] [PubMed] [Google Scholar]
- 27.Mortazavi A, Hoot D, Carlton P, Wang S, DeGroff V, Lu Q, Kulp S, Chen C, Clinton SK Inhibition of cell growth and induction of apoptosis in bladder cancer cell lines by a novel histone deacetylase inhibitor derived from phenylbutyrate. In: AACR, 2005. vol Supplement S. p 422 [Google Scholar]
- 28.Mortazavi A, Bhave SL, Haghighat P, Rengel RC, Phillips GS, Yu J, Sargeant AM, Kulp SK, Chen CS,Clinton SK Antitumor effects of OSU-HDAC42, a histone deacetylase inhibitor, in bladder cancer. In: Genitourinary Cancers Symptosium, 2009. [Google Scholar]
- 29.Xu W, Xu B, Yao Y, Yu X, Shen J (2015) The novel HDAC inhibitor AR-42-induced anti-colon cancer cell activity is associated with ceramide production. Biochem Biophys Res Commun 463 (4):545–550. doi: 10.1016/j.bbrc.2015.05.078 [DOI] [PubMed] [Google Scholar]
- 30.Bhinder AS, Varma V, Abbaoui B, Thomas-Ahner JM, Kulp SK, Chen C, Clinton SK, Mortazavi A (2011) Antitumor effects of AR-42, a novel histone deacetylase inhibitor, in embryonal carcinoma. Journal of Clinical Oncology 29 (7_suppl):232–232. doi: 10.1200/jco.2011.29.7_suppl.232 [DOI] [Google Scholar]
- 31.Yang YT, Balch C, Kulp SK, Mand MR, Nephew KP, Chen CS (2009) A rationally designed histone deacetylase inhibitor with distinct antitumor activity against ovarian cancer. Neoplasia 11 (6):552–563, 553 p following 563. doi: 10.1593/neo.09204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mand M, Edwards C, Tumati V, Kulp SK, Chen C-S, Nephew KP, Balch C (2006) A novel histone deacetylase inhibitor with potent antiproliferative activity in ovarian cancer cells. Cancer Research 66 (8 Supplement):1183–1183 [Google Scholar]
- 33.Chen YJ, Wang WH, Wu WY, Hsu CC, Wei LR, Wang SF, Hsu YW, Liaw CC, Tsai WC (2017) Novel histone deacetylase inhibitor AR-42 exhibits antitumor activity in pancreatic cancer cells by affecting multiple biochemical pathways. PLoS One 12 (8):e0183368. doi: 10.1371/journal.pone.0183368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burns SS, Akhmametyeva EM, Oblinger JL, Bush ML, Huang J, Senner V, Chen CS, Jacob A, Welling DB, Chang LS (2013) Histone deacetylase inhibitor AR-42 differentially affects cell-cycle transit in meningeal and meningioma cells, potently inhibiting NF2-deficient meningioma growth. Cancer Res 73 (2):792–803. doi: 10.1158/0008-5472.CAN-12-1888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng H, Xie Z, Jones WP, Wei XT, Liu Z, Wang D, Kulp SK, Wang J, Coss CC, Chen CS, Marcucci G, Garzon R, Covey JM, Phelps MA, Chan KK (2016) Preclinical Pharmacokinetics Study of R- and S-Enantiomers of the Histone Deacetylase Inhibitor, AR-42 (NSC 731438), in Rodents. The AAPS journal 18 (3):737–745. doi: 10.1208/s12248-016-9876-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sborov DW, Canella A, Hade EM, Mo X, Khountham S, Wang J, Ni W, Poi M, Coss C, Liu Z, Phelps MA, Mortazavi A, Andritsos L, Baiocchi RA, Christian BA, Benson DM, Flynn J, Porcu P, Byrd JC, Pichiorri F, Hofmeister CC (2017) A phase 1 trial of the HDAC inhibitor AR-42 in patients with multiple myeloma and T- and B-cell lymphomas. Leuk Lymphoma 58 (10):2310–2318. doi: 10.1080/10428194.2017.1298751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45 (2):228–247. doi: 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 38.Cheng H, Liu Z, Kulp SK, Chen C-S, Covey JM, Chan KK (2006) Preclinical pharmacokinetic studies with s-HDAC-42 (NSC 736012), an inhibitor of histone deacetylase, by LC-MS/MS. Proc Amer Assoc Cancer Res 47 [Google Scholar]
- 39.Liva SG, Coss CC, Wang J, Blum W, Klisovic R, Bhatnagar B, Walsh K, Geyer S, Zhao Q, Garzon R, Marcucci G, Phelps MA, Walker AR (2020) Phase I study of AR-42 and decitabine in acute myeloid leukemia. Leukemia & Lymphoma:1–9. doi: 10.1080/10428194.2020.1719095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vansteenkiste J, Van Cutsem E, Dumez H, Chen C, Ricker JL, Randolph SS, Schoffski P (2008) Early phase II trial of oral vorinostat in relapsed or refractory breast, colorectal, or non-small cell lung cancer. Invest New Drugs 26 (5):483–488. doi: 10.1007/s10637-008-9131-6 [DOI] [PubMed] [Google Scholar]
- 41.Blumenschein GR Jr., Kies MS, Papadimitrakopoulou VA, Lu C, Kumar AJ, Ricker JL, Chiao JH, Chen C, Frankel SR (2008) Phase II trial of the histone deacetylase inhibitor vorinostat (Zolinza, suberoylanilide hydroxamic acid, SAHA) in patients with recurrent and/or metastatic head and neck cancer. Invest New Drugs 26 (1):81–87. doi: 10.1007/s10637-007-9075-2 [DOI] [PubMed] [Google Scholar]
- 42.Molife LR, Attard G, Fong PC, Karavasilis V, Reid AH, Patterson S, Riggs CE Jr, Higano C, Stadler WM, McCulloch W, Dearnaley D, Parker C, de Bono JS (2010) Phase II, two-stage, single-arm trial of the histone deacetylase inhibitor (HDACi) romidepsin in metastatic castration-resistant prostate cancer (CRPC). Ann Oncol 21 (1):109–113. doi: 10.1093/annonc/mdp270 [DOI] [PubMed] [Google Scholar]
- 43.Hainsworth JD, Infante JR, Spigel DR, Arrowsmith ER, Boccia RV, Burris HA (2011) A phase II trial of panobinostat, a histone deacetylase inhibitor, in the treatment of patients with refractory metastatic renal cell carcinoma. Cancer Invest 29 (7):451–455. doi: 10.3109/07357907.2011.590568 [DOI] [PubMed] [Google Scholar]
- 44.Steele NL, Plumb JA, Vidal L, Tjornelund J, Knoblauch P, Rasmussen A, Ooi CE, Buhl-Jensen P, Brown R, Evans TR, DeBono JS (2008) A phase 1 pharmacokinetic and pharmacodynamic study of the histone deacetylase inhibitor belinostat in patients with advanced solid tumors. Clin Cancer Res 14 (3):804–810. doi: 10.1158/1078-0432.CCR-07-1786 [DOI] [PubMed] [Google Scholar]
- 45.Shah MH, Binkley P, Chan K, Xiao J, Arbogast D, Collamore M, Farra Y, Young D, Grever M (2006) Cardiotoxicity of histone deacetylase inhibitor depsipeptide in patients with metastatic neuroendocrine tumors. Clin Cancer Res 12 (13):3997–4003. doi: 10.1158/1078-0432.CCR-05-2689 [DOI] [PubMed] [Google Scholar]
- 46.Sandor V, Bakke S, Robey RW, Kang MH, Blagosklonny MV, Bender J, Brooks R, Piekarz RL, Tucker E, Figg WD, Chan KK, Goldspiel B, Fojo AT, Balcerzak SP, Bates SE (2002) Phase I trial of the histone deacetylase inhibitor, depsipeptide (FR901228, NSC 630176), in patients with refractory neoplasms. Clin Cancer Res 8 (3):718–728 [PubMed] [Google Scholar]
- 47.Porta-Sanchez A, Gilbert C, Spears D, Amir E, Chan J, Nanthakumar K, Thavendiranathan P (2017) Incidence, Diagnosis, and Management of QT Prolongation Induced by Cancer Therapies: A Systematic Review. J Am Heart Assoc 6 (12). doi: 10.1161/JAHA.117.007724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iwamoto FM, Lamborn KR, Kuhn JG, Wen PY, Yung WK, Gilbert MR, Chang SM, Lieberman FS, Prados MD, Fine HA (2011) A phase I/II trial of the histone deacetylase inhibitor romidepsin for adults with recurrent malignant glioma: North American Brain Tumor Consortium Study 03-03. Neuro Oncol 13 (5):509–516. doi: 10.1093/neuonc/nor017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Whitehead RP, Rankin C, Hoff PM, Gold PJ, Billingsley KG, Chapman RA, Wong L, Ward JH, Abbruzzese JL, Blanke CD (2009) Phase II trial of romidepsin (NSC-630176) in previously treated colorectal cancer patients with advanced disease: a Southwest Oncology Group study (S0336). Invest New Drugs 27 (5):469–475. doi: 10.1007/s10637-008-9190-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Modesitt SC, Sill M, Hoffman JS, Bender DP, Gynecologic Oncology G (2008) A phase II study of vorinostat in the treatment of persistent or recurrent epithelial ovarian or primary peritoneal carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 109 (2):182–186. doi: 10.1016/j.ygyno.2008.01.009 [DOI] [PubMed] [Google Scholar]
- 51.Luu TH, Morgan RJ, Leong L, Lim D, McNamara M, Portnow J, Frankel P, Smith DD, Doroshow JH, Wong C, Aparicio A, Gandara DR, Somlo G (2008) A phase II trial of vorinostat (suberoylanilide hydroxamic acid) in metastatic breast cancer: a California Cancer Consortium study. Clin Cancer Res 14 (21):7138–7142. doi: 10.1158/1078-0432.CCR-08-0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goutagny S, Raymond E, Esposito-Farese M, Trunet S, Mawrin C, Bernardeschi D, Larroque B, Sterkers O, Giovannini M, Kalamarides M (2015) Phase II study of mTORC1 inhibition by everolimus in neurofibromatosis type 2 patients with growing vestibular schwannomas. J Neurooncol 122 (2):313–320. doi: 10.1007/s11060-014-1710-0 [DOI] [PubMed] [Google Scholar]
- 53.Plotkin SR, Halpin C, Blakeley JO, Slattery WH 3rd, Welling DB, Chang SM, Loeffler JS, Harris GJ, Sorensen AG, McKenna MJ, Barker 2nd (2009) Suggested response criteria for phase II antitumor drug studies for neurofibromatosis type 2 related vestibular schwannoma. Journal of neuro-oncology 93 (1):61–77. doi: 10.1007/s11060-009-9867-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Asthagiri AR, Parry DM, Butman JA, Kim HJ, Tsilou ET, Zhuang Z, Lonser RR (2009) Neurofibromatosis type 2. Lancet 373 (9679):1974–1986. doi: 10.1016/S0140-6736(09)60259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen CS, Weng SC, Tseng PH, Lin HP, Chen CS (2005) Histone acetylation-independent effect of histone deacetylase inhibitors on Akt through the reshuffling of protein phosphatase 1 complexes. J Biol Chem 280 (46):38879–38887. doi: 10.1074/jbc.M505733200 [DOI] [PubMed] [Google Scholar]
- 56.Ramalingam SS, Maitland ML, Frankel P, Argiris AE, Koczywas M, Gitlitz B, Thomas S, Espinoza-Delgado I, Vokes EE, Gandara DR, Belani CP (2010) Carboplatin and Paclitaxel in combination with either vorinostat or placebo for first-line therapy of advanced non-small-cell lung cancer. J Clin Oncol 28 (1):56–62. doi: 10.1200/JCO.2009.24.9094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Min A, Im SA, Kim DK, Song SH, Kim HJ, Lee KH, Kim TY, Han SW, Oh DY, Kim TY, O’Connor MJ, Bang YJ (2015) Histone deacetylase inhibitor, suberoylanilide hydroxamic acid (SAHA), enhances anti-tumor effects of the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib in triple-negative breast cancer cells. Breast Cancer Res 17:33. doi: 10.1186/s13058-015-0534-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Garcia-Manero G, Tambaro FP, Bekele NB, Yang H, Ravandi F, Jabbour E, Borthakur G, Kadia TM, Konopleva MY, Faderl S, Cortes JE, Brandt M, Hu Y, McCue D, Newsome WM, Pierce SR, de Lima M, Kantarjian HM (2012) Phase II trial of vorinostat with idarubicin and cytarabine for patients with newly diagnosed acute myelogenous leukemia or myelodysplastic syndrome. J Clin Oncol 30 (18):2204–2210. doi: 10.1200/JCO.2011.38.3265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Groselj B, Ruan JL, Scott H, Gorrill J, Nicholson J, Kelly J, Anbalagan S, Thompson J, Stratford MRL, Jevons SJ, Hammond EM, Scudamore CL, Kerr M, Kiltie AE (2018) Radiosensitization In Vivo by Histone Deacetylase Inhibition with No Increase in Early Normal Tissue Radiation Toxicity. Mol Cancer Ther 17 (2):381–392. doi: 10.1158/1535-7163.MCT-17-0011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reid T, Weeks A, Vakil M, Cosgriff T, Harper T, Valone F, Magnuson D, Bhatnagar A (2004) Dose escalation study of pivanex (a histone deacetylase inhibitor) in combination with docetaxel for advanced non-small cell lung cancer. Journal of Clinical Oncology 22 (14_suppl):7279–7279. doi: 10.1200/jco.2004.22.90140.7279 [DOI] [Google Scholar]
- 61.Friday BB, Anderson SK, Buckner J, Yu C, Giannini C, Geoffroy F, Schwerkoske J, Mazurczak M, Gross H, Pajon E, Jaeckle K, Galanis E (2012) Phase II trial of vorinostat in combination with bortezomib in recurrent glioblastoma: a north central cancer treatment group study. Neuro Oncol 14 (2):215–221. doi: 10.1093/neuonc/nor198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Munster PN, Thurn KT, Thomas S, Raha P, Lacevic M, Miller A, Melisko M, Ismail-Khan R, Rugo H, Moasser M, Minton SE (2011) A phase II study of the histone deacetylase inhibitor vorinostat combined with tamoxifen for the treatment of patients with hormone therapy-resistant breast cancer. Br J Cancer 104 (12):1828–1835. doi: 10.1038/bjc.2011.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nakagawa T, Takeuchi S, Yamada T, Ebi H, Sano T, Nanjo S, Ishikawa D, Sato M, Hasegawa Y, Sekido Y, Yano S (2013) EGFR-TKI resistance due to BIM polymorphism can be circumvented in combination with HDAC inhibition. Cancer Res 73 (8):2428–2434. doi: 10.1158/0008-5472.CAN-12-3479 [DOI] [PubMed] [Google Scholar]
- 64.Kirschbaum M, Gojo I, Goldberg SL, Bredeson C, Kujawski LA, Yang A, Marks P, Frankel P, Sun X, Tosolini A, Eid JE, Lubiniecki GM, Issa JP (2014) A phase 1 clinical trial of vorinostat in combination with decitabine in patients with acute myeloid leukaemia or myelodysplastic syndrome. Br J Haematol 167 (2):185–193. doi: 10.1111/bjh.13016 [DOI] [PubMed] [Google Scholar]
- 65.Chen R, Frankel P, Popplewell L, Siddiqi T, Ruel N, Rotter A, Thomas SH, Mott M, Nathwani N, Htut M, Nademanee A, Forman SJ, Kirschbaum M (2015) A phase II study of vorinostat and rituximab for treatment of newly diagnosed and relapsed/refractory indolent non-Hodgkin lymphoma. Haematologica 100 (3):357–362. doi: 10.3324/haematol.2014.117473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee EQ, Reardon DA, Schiff D, Drappatz J, Muzikansky A, Grimm SA, Norden AD, Nayak L, Beroukhim R, Rinne ML, Chi AS, Batchelor TT, Hempfling K, McCluskey C, Smith KH, Gaffey SC, Wrigley B, Ligon KL, Raizer JJ, Wen PY (2015) Phase II study of panobinostat in combination with bevacizumab for recurrent glioblastoma and anaplastic glioma. Neuro Oncol 17 (6):862–867. doi: 10.1093/neuonc/nou350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Suraweera A, O’Byrne KJ, Richard DJ (2018) Combination Therapy With Histone Deacetylase Inhibitors (HDACi) for the Treatment of Cancer: Achieving the Full Therapeutic Potential of HDACi. Front Oncol 8:92. doi: 10.3389/fonc.2018.00092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Qiu T, Zhou L, Zhu W, Wang T, Wang J, Shu Y, Liu P (2013) Effects of treatment with histone deacetylase inhibitors in solid tumors: a review based on 30 clinical trials. Future Oncol 9 (2):255–269. doi: 10.2217/fon.12.173 [DOI] [PubMed] [Google Scholar]
- 69.Jespersen H, Olofsson Bagge R, Ullenhag G, Carneiro A, Helgadottir H, Ljuslinder I, Levin M, All-Eriksson C, Andersson B, Stierner U, Nilsson LM, Nilsson JA, Ny L (2019) Concomitant use of pembrolizumab and entinostat in adult patients with metastatic uveal melanoma (PEMDAC study): protocol for a multicenter phase II open label study. BMC Cancer 19 (1):415. doi: 10.1186/s12885-019-5623-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, Jedrzejczak WW, Gunther A, Nakorn TN, Siritanaratkul N, Corradini P, Chuncharunee S, Lee JJ, Schlossman RL, Shelekhova T, Yong K, Tan D, Numbenjapon T, Cavenagh JD, Hou J, LeBlanc R, Nahi H, Qiu L, Salwender H, Pulini S, Moreau P, Warzocha K, White D, Blade J, Chen W, de la Rubia J, Gimsing P, Lonial S, Kaufman JL, Ocio EM, Veskovski L, Sohn SK, Wang MC, Lee JH, Einsele H, Sopala M, Corrado C, Bengoudifa BR, Binlich F, Richardson PG (2014) Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol 15 (11):1195–1206. doi: 10.1016/S1470-2045(14)70440-1 [DOI] [PubMed] [Google Scholar]
- 71.Booth L, Roberts JL, Sander C, Lee J, Kirkwood JM, Poklepovic A, Dent P (2017) The HDAC inhibitor AR42 interacts with pazopanib to kill trametinib/dabrafenib-resistant melanoma cells in vitro and in vivo. Oncotarget 8 (10):16367–16386. doi: 10.18632/oncotarget.14829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mims A, Walker AR, Huang X, Sun J, Wang H, Santhanam R, Dorrance AM, Walker C, Hoellerbauer P, Tarighat SS, Chan KK, Klisovic RB, Perrotti D, Caligiuri MA, Byrd JC, Chen CS, James Lee L, Jacob S, Mrozek K, Bloomfield CD, Blum W, Garzon R, Schwind S, Marcucci G (2013) Increased anti-leukemic activity of decitabine via AR-42-induced upregulation of miR-29b: a novel epigenetic-targeting approach in acute myeloid leukemia. Leukemia 27 (4):871–878. doi: 10.1038/leu.2012.342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murahari S, Jalkanen AL, Kulp SK, Chen CS, Modiano JF, London CA, Kisseberth WC (2017) Sensitivity of osteosarcoma cells to HDAC inhibitor AR-42 mediated apoptosis. BMC Cancer 17 (1):67. doi: 10.1186/s12885-017-3046-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou R, Wu J, Tang X, Wei X, Ju C, Zhang F, Sun J, Shuai D, Zhang Z, Liu Q, Lv XB (2018) Histone deacetylase inhibitor AR-42 inhibits breast cancer cell growth and demonstrates a synergistic effect in combination with 5-FU. Oncol Lett 16 (2):1967–1974. doi: 10.3892/ol.2018.8854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li DR, Zhang H, Peek E, Wang S, Du L, Li G, Chin AI (2015) Synergy of Histone-Deacetylase Inhibitor AR-42 with Cisplatin in Bladder Cancer. J Urol 194 (2):547–555. doi: 10.1016/j.juro.2015.02.2918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liva SG, Tseng YC, Dauki AM, Sovic MG, Vu T, Henderson SE, Kuo YC, Benedict JA, Zhang X, Remaily BC, Kulp SK, Campbell M, Bekaii-Saab T, Phelps MA, Chen CS, Coss CC (2020) Overcoming resistance to anabolic SARM therapy in experimental cancer cachexia with an HDAC inhibitor. EMBO molecular medicine 12 (2):e9910. doi: 10.15252/emmm.201809910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Di Gennaro E, Bruzzese F, Pepe S, Leone A, Delrio P, Subbarayan PR, Avallone A, Budillon A (2009) Modulation of thymidilate synthase and p53 expression by HDAC inhibitor vorinostat resulted in synergistic antitumor effect in combination with 5FU or raltitrexed. Cancer Biol Ther 8 (9):782–791. doi: 10.4161/cbt.8.9.8118 [DOI] [PubMed] [Google Scholar]
- 78.Mortazavi A, Hoot D, Carlton P, Chen C, Clinton SK Modulation of ErbB family receptors by a novel histone deacetylase inhibitor, HDAC-42, in bladder cancer cell lines. In: Proc Amer Assoc Cancer Res, April 2006 2006. Cellular and Molecular Biology 68: Histone Modifications and Inhibitors. [Google Scholar]
- 79.Lee JH, Park JH, Jung Y, Kim JH, Jong HS, Kim TY, Bang YJ (2006) Histone deacetylase inhibitor enhances 5-fluorouracil cytotoxicity by down-regulating thymidylate synthase in human cancer cells. Mol Cancer Ther 5 (12):3085–3095. doi: 10.1158/1535-7163.MCT-06-0419 [DOI] [PubMed] [Google Scholar]
- 80.Del Bufalo D, Desideri M, De Luca T, Di Martile M, Gabellini C, Monica V, Busso S, Eramo A, De Maria R, Milella M, Trisciuoglio D (2014) Histone deacetylase inhibition synergistically enhances pemetrexed cytotoxicity through induction of apoptosis and autophagy in non-small cell lung cancer. Mol Cancer 13:230. doi: 10.1186/1476-4598-13-230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Grivas P, Mortazavi A, Picus J, Hahn NM, Milowsky MI, Hart LL, Alva A, Bellmunt J, Pal SK, Bambury RM, O’Donnell PH, Gupta S, Guancial EA, Sonpavde GP, Faltaos D, Potvin D, Christensen JG, Chao RC, Rosenberg JE (2019) Mocetinostat for patients with previously treated, locally advanced/metastatic urothelial carcinoma and inactivating alterations of acetyltransferase genes. Cancer 125 (4):533–540. doi: 10.1002/cncr.31817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cheung M, Testa JR (2017) BAP1, a tumor suppressor gene driving malignant mesothelioma. Transl Lung Cancer Res 6 (3):270–278. doi: 10.21037/tlcr.2017.05.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sacco JJ, Kenyani J, Butt Z, Carter R, Chew HY, Cheeseman LP, Darling S, Denny M, Urbe S, Clague MJ, Coulson JM (2015) Loss of the deubiquitylase BAP1 alters class I histone deacetylase expression and sensitivity of mesothelioma cells to HDAC inhibitors. Oncotarget 6 (15):13757–13771. doi: 10.18632/oncotarget.3765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Landreville S, Agapova OA, Matatall KA, Kneass ZT, Onken MD, Lee RS, Bowcock AM, Harbour JW (2012) Histone deacetylase inhibitors induce growth arrest and differentiation in uveal melanoma. Clin Cancer Res 18 (2):408–416. doi: 10.1158/1078-0432.CCR-11-0946 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


