Abstract
Purpose
This study evaluates the feasibility of delivering a virtual (online) falls prevention intervention for older adults with mild cognitive impairment (MCI).
Methods
Community-dwelling older adults with MCI (mean age = 76.2 years, 72% women) were randomized to either a Tai Ji Quan (n = 15) or stretching group (n = 15) and participated in 60-minute virtual exercise sessions, via Zoom, twice weekly for 24 weeks. The primary outcome was the incidence of falls. Secondary outcomes were the number of fallers and changes from baseline in the 4-Stage Balance Test, 30-second chair stands, and Timed Up and Go Test under both single- and dual-task conditions.
Results
The intervention was implemented with good fidelity, an overall attendance rate of 79%, and 13% attrition. Compared with stretching, Tai Ji Quan did not reduce falls (incidence rate ratio = 0.58; 95% confidence interval [CI], 0.32 to 1.03) or the number of fallers (relative risk ratio = 0.75; 95% CI, 0.46 to 1.22) at week 24. The Tai Ji Quan group, however, performed consistently better than the stretching group in balance (between-group difference in change from baseline, 0.68 points; 95% CI, 0.12 to 1.24), 30-second chair stands (1.87 stands; 95% CI, 1.15 to 2.58), and Timed Up and Go under single-task (−1.15 seconds; 95% CI, −1.85 to −0.44) and dual-task (−2.35; 95% CI, −3.06 to −1.64) conditions. No serious intervention-related adverse events were observed.
Conclusion
Findings from this study suggest the feasibility, with respect to intervention fidelity, compliance, and potential efficacy, of implementing an at-home, virtual, interactive Tai Ji Quan program, delivered in real-time, as a potential balance training and falls prevention intervention for older adults with MCI. The study provides preliminary data to inform future trials.
Keywords: cognitive function, dual-task, incidental falls, elderly, exercise, e-health
Introduction
Falls among community-dwelling older adults are a major public health problem.1,2 The magnitude of the problem, however, is greater among those who experience cognitive impairment, including Alzheimer’s disease and related dementias (ADRD) and mild cognitive impairment (MCI). Studies show that between 30% and 50% of community-dwelling older adults with cognitive impairment have reported falling,3–5 and they also have a higher likelihood of falling (2–5 times higher risk) compared to those who are cognitively unimpaired.5,6 In addition, this population experiences other high-risk factors related to falling, with poor outcomes for balance, gait, dual-task activities, and cognitive function.5,7–9
Research shows that exercise, especially balance-based training interventions, prevents falls in community-dwelling older adults.10–12 Evidence, however, is less conclusive for those who have cognitive impairment.13–15 There are currently few exercise interventions that are efficacious, easily accessible, and specifically tailored for this population.15 The much-needed effort to develop effective interventions is further hampered by the on-going global coronavirus disease (COVID-19) pandemic. This unprecedented public health crisis has left many older adults with cognitive impairment, who are at highest risk for severe illness from coronavirus infection,16 constrained at home with few resources and limited opportunities to continue physical activity in the community, thus increasing their risk for falls and worsening their physical performance.
Motivated by these public health challenges, we designed a study to explore the feasibility of an online (virtual) balance training exercise program targeting older adults with cognitive impairment. Specifically, on the basis of our prior work,17,18 we evaluated the feasibility of delivering a virtual dual-task Tai Ji Quan intervention and assessed the potential efficacy of the intervention for reducing falls and improving balance, mobility, and dual-task performances in community-dwelling older adults with MCI.
Methods
Study Design and Participants
The study involved a single-blinded, randomized, parallel-group feasibility trial. Individuals who qualified per the study eligibility criteria were randomized to either a Tai Ji Quan or stretching group and participated in virtual exercise classes for 24 weeks. The study protocol was approved by the Institutional Review Board of the Oregon Research Institute and conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from each participant. This feasibility study was performed with data analyzed between April 2020 and March 2021 as a supplement to a randomized controlled trial registered at ClinicalTrials.gov (NCT04070703).
The target population was community-dwelling older adults with MCI. To participate, individuals had to meet the following inclusion criteria: (a) be 65 years of age or older, (b) have had a complaint of memory loss (reported by the participant and corroborated by an informant), (c) recorded a score of ≤0.5 on the Clinical Dementia Rating (CDR) scale19 and ≥24 on the Mini Mental State Evaluation (MMSE),20 (d) not participated in a rigorous and structured physical activity or exercise program in the past 3 months, and (e) have medical clearance from a healthcare provider. Individuals who could not commit to the 24-week study period, were physically weak or unable to ambulate, or refused to accept group assignment were excluded.
Procedures
Participants were recruited primarily through promotions in local newspapers and through mass mailings. Additional recruitment methods included word of mouth, postings on social media, and existing research databases of individuals who had participated in prior research projects. Because the study took place during the COVID-19 pandemic, subject recruitment and outcome assessment activities were conducted primarily via phone communications and online via Zoom. Recruitment and enrollment activities were conducted in two phases described in detail below.
In Phase 1, a research assistant made telephone contact with those who responded to the study promotion. This initial contact confirmed eligibility criteria regarding age, memory status, levels of habitual physical activity, and time availability. An independent interview was also conducted with an informant, who provided information regarding the respondent’s cognitive status based in part on a CDR assessment.19 In Phase 2, respondents were further evaluated, via a Zoom session, on additional eligibility criteria, including administration of the CDR and MMSE. Those who qualified then underwent a virtual baseline assessment conducted by a trained assessor. Those who met all inclusion criteria, were clear about research procedures, provided informed consent, and completed baseline assessment were then randomized.
Randomization and Masking
Eligible individuals were randomly assigned in a 1:1 ratio, via a computer-generated randomization sequence, to receive one of the two interventions, with a block size of 4 or 6 to prevent anticipation of assignment to a specific study group. Allocation concealment was ensured since the randomization was performed by a research assistant who was not involved in the assessment or intervention. Study participants were not blinded to the intervention group allocation. However, outcome assessors were masked to group allocation throughout the study period.
Intervention Protocol Set-Up
Participants in both interventions (described in detail below) received two 1-hour online exercise sessions per week, delivered on Mondays and Wednesdays or Tuesdays and Thursdays. Exercise instructors trained by the first author taught all sessions. The intervention lasted 24 weeks, with a total of 48 exercise sessions planned for each group. The study set an a priori goal of 75% or greater for class attendance rate (≥36 sessions of the total) and a 15% attrition rate over the entire intervention period. An orientation on the use of Zoom was provided to each participant at baseline.
The two interventions were delivered online via Zoom, with a class size for each intervention set between 4 and 8 participants in order to optimize viewability in Zoom’s Gallery View. We also constrained the instructor’s teaching movements to a square (marked on the floor) not exceeding 4 feet by 4 feet in order to provide (a) onscreen viewability, (b) instructional clarity, and (c) effective home space utilization and movement safety. On the participant end, we set an optimum physical distance of 8–10 feet for personal computer users and 6–8 feet for iPad or smart phone users for better viewability. On each class day, participants were given a secured Zoom link via an e-mail to allow them access to the scheduled online exercise session.
Intervention
Tai Ji Quan
Participants received an augmented dual-task Tai Ji Quan training program based on Tai Ji Quan: Moving for Better Balance,21 an evidence-based balance training falls prevention program for community-dwelling older adults.17,22,23 The protocol involved 10–15 minutes of preparatory exercises, 45–50 minutes of core training (learning, practicing) in the movements contained in an 8-form routine (“Move a Ball,” “Part Wild Horse’s Mane,” “Repulse Monkey,” “Brush Knees,” “Fair Lady Works the Shuttle,” “Grasp Peacock’s Tail,” “Waving Hands like Cloud,” and “Single Whip”), and 1–2 minutes of closing exercises. Training focused on practicing symmetrical and coordinated forms/movements that emphasized movement and breathing synchronization, trunk rotation, bilateral weight shifts, controlled displacement of the body’s center of mass over the varying sizes of the base of support, dynamic eyes-head movements, and multidirectional (anterior-posterior and medial-lateral) stepping. Additional training features involved form-based rotational ankle sway and self-induced reactive postural recovery exercises.17
Within a dual-task framework, the progressive core training involved concurrent, interactive cognitive-physical exercises aimed at challenging multiple cognitive domains (memory, executive function, spatial orientation, and processing speed). Drill features incorporated recalling forms/movements (based on either verbal or visual instructions); linking a form number (eg, Form 2) with the corresponding name (eg, Part Wild House’s Mane) or vice versa; practicing forms with verbalization of movement, word spelling, and narrow base of support (eg, feet together, semi-tandem stance); performing complex tasks involving obstacle negotiation and navigation (eg, doing forms around a chair, forms performed in different directions); engaging in forms switching, order reversing and retrieval; and performing “Do what I say” or “Do what I do” interference effect exercises. As part of the protocol, we also incorporated an additional set of training elements, including (a) 5–6 mini-therapeutic movements,21 (b) seated form practice, and (c) sit-to-stand and stand-to-sit form exercises.
Stretching
Participants in this group received stretching exercises, with the majority of activities performed in a seated position.17 Each exercise session began with a set of warm-up exercises, such as arm, neck, and leg circles; trunk rotation; and light walking. The core part of the training session consisted of a variety of combined seated and standing static (active) stretches involving the upper body (neck, arms, back, shoulders, and the chest) and lower extremities (quadriceps, hamstrings, calves, and hips), along with slow and gentle trunk rotations. Each session ended with abdominal breathing exercises that emphasized inhaling and exhaling to maximum capacity as well as progressive relaxation of major muscle groups.
Measurements
Primary Outcome
The primary outcome was the incidence of falls, ascertained via monthly phone calls, over the 24-week period. Participants were asked to record any fall on a falls calendar and to report any fall event (defined as “when you land on the floor or the ground, or fall and hit objects like stairs or pieces of furniture, by accident”) including any injurious falls.17 Data on falls were collected starting from the date of the first intervention class and continuing until 24 weeks later (ie, the end of the intervention period) or until a participant withdrew or was lost to follow-up.
Secondary Measures
These included measures of (a) number of fallers, derived from the falls calendars and monthly phone calls by research staff, (b) 4-Stage Balance Test,24 (c) 30-second chair stands,25 and (d) Timed Up and Go26 Test performed under both single- and dual-task conditions. Measures in (b) through (d), described below, were collected at baseline and 6-month follow-up via Zoom.
The 4-Stage Balance Test asks the participant to perform, for 10 seconds each, four progressively more challenging standing positions involving (a) parallel stance, (b) semi-tandem stance, (c) tandem (heel-toe) stance, and (d) one-legged stance. For scoring purposes, a score of 1 (success) was recorded for each testing position if the participant was able to complete the task for 10 seconds; 0 (failure) if the participant could not complete the task for 10 seconds. Scores (range: 0–4) were summed across the four testing conditions, with high values indicating better balance. The 30-second chair stands test was administered using a standard chair with the total number of chair stands recorded within 30 seconds. The Timed Up and Go Test (under the single-task condition) measured the time (in seconds) it took for a participant to complete an 20-foot walk that involved (a) standing up from a chair, (b) walking (10 feet forward) at normal pace to a line on the floor, (c) turning, (d) walking back (10 feet) to the chair, and (e) sitting down. The test protocol was repeated under a dual-task condition where the participant was asked to walk while performing an arithmetic task (ie, starting at the number 81 and sequentially subtracting 5 from the resulting number). No instructions were provided for prioritization of one of the tasks (walking or cognitive task) during the dual-task trial. Lower scores on both single- and dual-task conditions indicated better performance.
Other Measures
At enrollment, participants completed a self-survey that collected their demographic, health status, medical and chronic conditions, and fall-related information. Other information included self-reported weight, height, and blood pressure.
Assessment Procedures
One day prior to baseline assessment, an e-mail was sent to each participant with a link connecting the participant to a secured Zoom session. On the day of the assessment, both the participant and study assessor signed on to the Zoom session, which began with a general orientation by the assessor about the assessment activities to be performed and detailed instructions on performance using screen sharing on Zoom. Participants were also asked to locate an armless chair to be used during the assessment and then perform the 4-Stage Balance Test, 30-second chair stands, and Timed Up and Go Test. The protocol was kept consistent between the two assessment points (baseline and follow-up).
Intervention-Related Process Assessment
We evaluated intervention fidelity by assessing the extent to which instructors successfully implemented the following prespecified program protocol components:23 (a) 60-minute session delivered twice weekly over a 24-week period, (b) instructor’s adherence to the teaching protocols specified in an instructional teaching plan, and (c) class participation rate of 75% or better. Information on intervention class attendance was collected at each online session by a research assistant. Adverse events were also monitored throughout the intervention period. A serious adverse event was defined as any undesirable experience associated with the prescribed exercise intervention programs. These included death, falls that resulted in an injury, hospitalization, or important medical events such as a heart attack that required treatment in an emergency room. The cause of each event, either intervention-related or non-intervention-related, was documented.
Statistical Analysis
Baseline characteristics of the study population and study outcome measures were summarized by intervention group using descriptive statistics, such as means, standard deviations (SDs), and percentages. To assess between-group equivalence at baseline, demographic descriptors were compared across groups by using analysis of variance for continuous variables and the χ2 (or Fisher’s Exact Test) for categorical variables. The descriptive information on number of falls, person-months of follow-up, and fallers was tabulated across the intervention groups.
Because all secondary outcomes were assessed via Zoom, we also performed a 16-week test-retest on the 4-Stage Balance Test, 30-second chair stands, and the Timed Up and Go Test under the single-task condition. In addition, we conducted preliminary validity analyses of baseline scores that examined (a) the correlation between Zoom-ascertained physical performance measures and in-person assessment of Short Physical Performance Battery (SPPB)27 and Functional Reach28 in a subsample of 18 participants for whom we had the data available based on both assessment approaches and (b) the association between the Zoom-ascertained Timed Up and Go scores and fall status (ie, a faller) on the whole sample.
Due to the exploratory nature of the study, power calculations were not conducted a priori. In our primary analysis of the falls count outcome, we used negative binomial regression to estimate absolute differences in the incidence rate ratio (IRR) with its corresponding 95% confidence interval (CI) comparing the Tai Ji Quan intervention with the stretching exercise intervention. The number of fallers in the two intervention groups was compared by examining the relative risk ratio (RR) of fallers, using modified Poisson regression models for binary outcomes. Faller status was compared using 0 falls versus 1+ falls. Using an intention-to-treat protocol, we analyzed the secondary (continuous) outcomes with estimates and their 95% CIs generated from the linear mixed-effects models. Incomplete data resulting from premature intervention dropouts (n = 2) were handled through the last observation carried forward method. All primary and secondary outcome analyses were conducted with and without adjustment for prespecified baseline covariates (including age, sex, health status, number of chronic disease conditions, and medications). Two-sided P values of <0.05 were considered statistically significant. Analyses were conducted using SPSS version 23 (IBM Corp).
Results
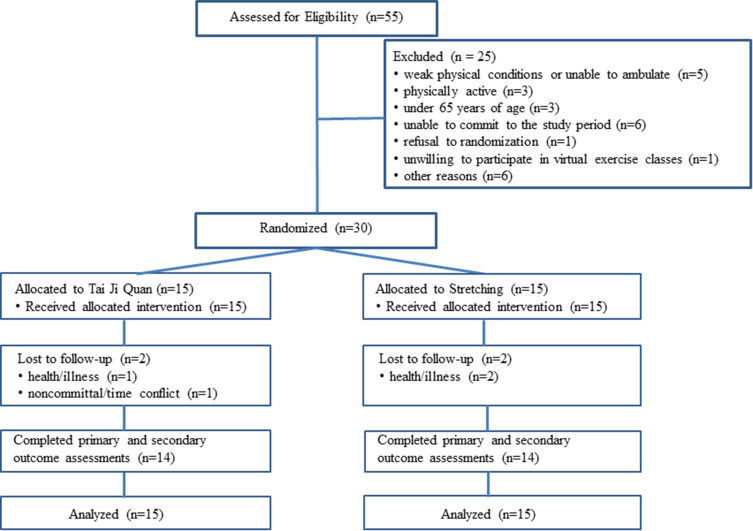
Of the 55 participants contacted and pre-screened for eligibility, 30 were qualified and randomized (15 to Tai Ji Quan and 15 to stretching) (Figure 1). There were no statistically significant differences in demographic variables between the two study groups at baseline (Table 1). Twenty-eight participants (93%) provided full follow-up data on primary and secondary study outcome measures at week 24.
Figure 1.
Flow of Participants through the Study.
Table 1.
Baseline Demographic and Clinical Characteristics of the Study Population
| Characteristic | Tai Ji Quan (n = 15) | Stretching Exercise (n = 15) |
|---|---|---|
| Age, mean (SD), y | 76.13 (6.2) | 76.20 (6.3) |
| Sex, No. (%) | ||
| Men | 6 (40.0) | 3 (20.0) |
| Women | 9 (60.0) | 12 (80.0) |
| Race, No. (%) | ||
| White | 14 (93.3) | 13 (86.7) |
| Others | 1 (6.7) | 2 (13.3) |
| Educational level, No. (%) | ||
| High school diploma or lower | 6 (40.0) | 7 (46.7) |
| College degree or higher | 9 (60.0) | 8 (53.3) |
| Self-reported health status, No. (%) | ||
| Poor or very poor | 4 (26.7) | 5 (33.3) |
| Good or fair | 9 (60.0) | 7 (46.7) |
| Very good or excellent | 2 (13.3) | 3 (20.0) |
| Resting blood pressure, mean (SD), mm Hg | ||
| Systolic | 135.87 (3.20) | 135.07 (3.38) |
| Diastolic | 81.00 (2.85) | 79.67 (2.16) |
| Self-reported falls in previous 6 months, No. (%) | ||
| 0 | 5 (33.3) | 6 (40.0) |
| 1 | 8 (53.3) | 7 (46.7) |
| 2 | 1 (6.7) | 2 (13.3) |
| ≥3 | 1 (6.7) | 0 (0) |
| Self-reported chronic conditions, No. (%) | ||
| 1 | 8 (53.3) | 7 (46.7) |
| 2 | 5 (33.3) | 6 (40.0) |
| ≥3 | 2 (13.4) | 2 (13.3) |
| Self-reported medication use, No. (%) | ||
| None | 2 (13.3) | 2 (13.3) |
| 1 | 6 (40.0) | 8 (53.3) |
| 2 | 3 (20.0) | 3 (20.0) |
| ≥3 | 4 (26.7) | 2 (13.4) |
| MMSE | 25.07 (0.80) | 25.27 (1.03) |
| GDS, mean (SD) | 4.67 (1.23) | 4.53 (0.74) |
Abbreviations: MMSE, Mini-Mental State Examination; GDS, Geriatric Depression Scale.
Participant Characteristics
The mean (SD, range) age of the study population was 76.2 years (6.2, 66–90 years), and 21 (72%) of the participants were women. A majority of the study participants (90%) were white. Nineteen participants (63%) reported having at least 1 fall in the 6 months before the intervention, 15 (50%) reported having 2 or more chronic conditions, and 12 (40%) were taking 2 or more medications. The average MMSE score for the study population was 25.18 (SD = 0.19).
Intervention Fidelity, Adherence, and Attrition
The intervention was successfully delivered via Zoom in participants’ homes. Of the total 30 participants, 22 (72%) used a personal computer and 8 (18%) used an iPad. Program fidelity was well maintained during implementation in that (a) all instructors successfully delivered the content of the 24-week program per the protocol and (b) a class participation rate of 75% or better was achieved (overall rate of 79%; 80% in the Tai Ji Quan group; 79% in the stretching exercise group). The mean (SD) number of completed sessions was 38 (8.5) (median, 39 sessions; range, 16–48 sessions) (38 sessions [9.3] in the Tai Ji Quan group and 37.8 sessions [7.8] in the stretching exercise group; P = 0.87). Four participants withdrew from the interventions (three of them due to health reasons and one was non-committal). The overall attrition rate was 13%. The median time to stop the intervention for these dropouts was 5.88 months (range: 5.25 to 6 months).
Data Ascertainment, Test-Retest Reliability, and Validity
All study participants successfully completed their online assessment at baseline with no major issues encountered (eg, Internet connection, movement space, or safety concerns). Similarly, 28 participants completed their outcome assessment at 6 months. Due to health reasons, two participants who dropped out of the study were unable to complete their end point assessment. Blinding was 100% maintained during baseline and follow-up assessment. For the online assessment ascertained via Zoom, we had a 3-month test-retest coefficient of 0.85 for 4-Stage Balance Test, 0.84 for repeated chair stands, and 0.89 for the Timed Up and Go Test under the single-task condition.
With respect to validity, the Zoom-ascertained measures were moderately correlated with the in-person assessment of SPPB and Functional Reach. Specifically, for SPPB, r = −0.69 for Timed Up and Go, r = −0.81 for 30-second chair stands, and r = 0.75 for 4-Stage Balance Test. For Functional Reach, r = −0.71 for Timed Up and Go, r = -0.79 for 30-second chair stands, and r = 0.66 for 4-Stage Balance Test. We also found that, controlling for age, sex, health, number of chronic disease conditions, and medications, participants who scored high on the Zoom-ascertained Timed Up and Go measure were associated with greater risk of being a faller relative to those who scored low on the measure (odds ratio = 6.67, p < 0.05).
Adverse Events
No intervention-related major adverse events were observed among the study participants. Two participants underwent surgery for a medical condition; one participant was admitted into hospital with pneumonia for two nights; all three participants subsequently returned to the classes and successfully completed their assigned intervention.
Primary Outcome
At 6 months, 41 falls were recorded among 21 of the 30 participants (72%) (15 falls in the Tai Ji Quan group and 26 falls in the stretching exercise group). The Tai Ji Quan group had 89.25 person-months of follow-up whereas the stretching group had 89.75 person-months of follow-up, with an incidence rate of 17 falls per 100 person-months in Tai Ji Quan and 29 falls per 100 person-months in stretching (mean difference = −0.12, 95% CI, −0.25 to 0.01, P = 0.07). Table 2 shows falls-related information ascertained from the two study groups.
Table 2.
Incidence of Falls and Number of Fallers During the 24-Week Intervention by Intervention Group
| Falls | Tai Ji Quan (n = 15) | Stretching Exercise (n = 15) | P-value |
|---|---|---|---|
| Total falls, No. (mean, SD) | 15 (1.00, ±1.0) | 26 (1.73, ±1.10) | 0.07a |
| No. of falls, No. (%) | |||
| 1 | 4 (26.7) | 2 (13.3) | |
| 2 | 8 (26.7) | 12 (40.0) | |
| 3 | 3 (6.7) | 12 (26.7) | 0.28b |
| No. of injurious falls (%)d | 2 (13) | 3 (20) | 0.57c |
| Person-months of follow-up, mean | 89.25 | 89.75 | |
| Incidence rate (person-months) | 0.17 | 0.29 | 0.07 |
| Faller, No. (%) | 9 (60) | 12 (80) | 0.43c |
Notes: aBased on the difference in means. bBased on Pearson Chi-square test. cBased on Fisher’s Exact Test. dDefined as those that resulted in sprains, strains, contusions, or abrasions.
Binomial regression of unadjusted analyses showed no statistical difference in the incidence rate between Tai Ji Quan and stretching (IRR, 0.58; 95% CI, 0.32 to 1.03). The estimates of the intervention effects between the two groups showed no change after adjusting for the prespecified covariates (IRR, 0.67; 95% CI, 0.35 to 1.29).
Secondary Outcomes
At 6 months, there were fewer fallers in the Tai Ji Quan group than in the stretching group (9 versus 12, respectively). However, there was no statistical difference in the number of fallers between the two intervention groups (RR = 0.75; 95% CI, 0.46 to 1.22). Participants in the Tai Ji Quan intervention performed significantly better than those in the stretching intervention on tests of physical and dual-task performances: 4-Stage Balance Test (mean difference, 0.68, P = 0.02), 30-second chair stands (mean difference, 1.87, P < 0.001), Timed Up and Go Test under single-task condition (mean difference, −1.15, P = 0.002), Timed Up and Go Test under dual-task condition (mean difference, −2.35, P < 0.001). Results on these performanced-based measures are summarized in Table 3.
Table 3.
Secondary Outcomes of Balance, Chair Stands, and Walking Performances (Under Single- and Dual-Task Conditions) at Baseline and 6 Months and Group Differences in Change
| Outcome | Tai Ji Quan (n = 15) | Stretching Exercise (n = 15) | Between-Group Difference in Mean Changes from Baseline (95% CI) |
|---|---|---|---|
| 4-Stage Balance Test, mean (SD), points | |||
| Baseline | 2.39 (0.49) | 2.47 (0.52) | |
| 6 months | 3.13 (0.52) | 2.53 (0.52) | 0.68 (0.12 to 1.24) |
| 30-second chair stands, mean (SD), No. of stands | |||
| Baseline | 11.00 (1.00) | 11.40 (1.12) | |
| 6 months | 13.07 (0.80) | 11.60 (1.06) | 1.87 (1.15 to 2.58) |
| Timed Up and Go Test (under single-task condition), mean (SD), seconds | |||
| Baseline | 13.38 (0.55) | 13.41 (0.73) | |
| 6 months | 11.86 (0.56) | 13.04 (0.89) | −1.15 (−1.85 to −0.44) |
| Timed Up and Go Test (under dual-task condition), mean (SD), seconds | |||
| Baseline | 16.05 (0.80) | 16.29 (0.98) | |
| 6 months | 14.33 (1.11) | 16.92 (1.21) | −2.35 (−3.06 to −1.64) |
Discussion
In this feasibility study, we showed that a dual-task Tai Ji Quan balance-training intervention designed for community-dwelling older adults with MCI was successfully implemented using a virtual format. While the intervention had no statistically significant impact on fall-related outcomes (incidence of falls and number of fallers) compared with the low-impact stretching control exercise, participants in the Tai Ji Quan training group were shown to have improved balance, mobility, and dual-task performances.
For the first time, we demonstrated that a Tai Ji Quan-based falls prevention intervention was deliverable to community-dwelling older adults with MCI via Zoom technology. We also showed that the 24-week intervention had good program fidelity, acceptable compliance among participants, and an overall low attrition rate. We received no major complaints while conducting our virtual classes, and there were no major intervention-related adverse events reported throughout the feasibility trial. In addition, we showed the feasibility of ascertaining physical and dual-task outcome data virtually, with good test-retest reliability and evidence for preliminary validity. These observations, along with the promising preliminary findings on falls and other performance outcomes, indicate the potential for delivering a virtual exercise program as either a home-based falls prevention strategy or an exercise intervention that can be used in response to a public health crisis, such as the ongoing COVID-19 pandemic, where the implementation of shelter-in-place and social distancing policies has imposed unintended personal life hurdles and major social constraints on older adults, including those with ADRD and MCI.29,30
Contrary to previous findings,17 the twice weekly, 24-week intervention resulted in no reduction in the incidence of falls among Tai Ji Quan participants compared to the stretching control participants. This result may be attributed to the fact that, as a feasibility trial, the study had a limited sample size and, consequently, was statistically underpowered to detect a clinical difference between the two study conditions. In addition, the current study did not specifically target older adults at high risk of falling, a population that likely would have had greater potential to benefit from our intervention. Nevertheless, our findings showed a promising trend in lowering the number falls and number of fallers among Tai Ji Quan participants relative to stretching participants. The data we collected are sufficient to provide a scientific premise for further refinement of the intervention and to power future falls prevention trials targeting older adults with cognitive impairment at high risk of falling.
Our study produced evidence that a dual-task Tai Ji Quan intervention, relative to a stretching control, significantly improved the physical and dual-task performances in older adults with MCI. These findings are largely consistent with our prior work17,18 and with the work of others who have focused on other types of exercise intervention programs targeting older adults with cognitive impairment.31–33 The findings, however, contrast with a previous Tai Ji Quan intervention study that ran for a similar length of time (6 months) but showed no significant impact on the Timed Up and Go Test.34
Although there has been an increasing number of falls prevention trials targeting community-dwelling older adults with cognitive impairment,13 ours is the first that focuses on evaluating a dual-task intervention specifically targeted at older adults with MCI, a precursor to ADRD. We base our conceptual framework on the increasing evidence suggesting that dual-task exercises can have a positive impact on balance, postural control, and physical performance and, consequently, reduce the likelihood of falling.35–37 By design, our training method involves physical Tai Ji Quan training augmented with a task-specific, cognitively stimulating component that is not made explicit in conventional Tai Ji Quan practice.38 Thus, our program offers a novel approach to ameliorating the risk of falls among older adults with MCI, with implications for reducing the fall risk associated with ADRD.
Practical Implications
Although wider implementation of virtual delivery of falls prevention interventions is promising with respect to intervention feasibility, some potential challenges need to be carefully considered. From a teaching perspective, instructors need to be trained to adapt their in-person class teaching experience to a virtual environment because computer hardware and software skills and the ability to appropriately modify spaces, audio capacity, and class sizes are necessary for successful delivery of virtual classes. From the viewpoint of participants, older adults with minimal computer or smart phone experience may feel uncomfortable accessing this new exercise platform, which requires completing various logistical tasks, ranging from tracking the online (Zoom) class link, signing on to a session, and positioning their device(s) for better viewing of the instructor (or vice versa) to controlling audio, video, and recording for high-quality instruction delivery and better learning and practice experiences. Additional implementation challenges include working around issues such as hearing difficulties (especially for those who use a hearing aid), mirroring vs non-mirroring classes during teaching, and muting and unmuting classes for clear communication and effective engagement during teaching.
As a result, to improve teaching quality, enhance participant learning experience, and maximize class motivation and retention, it is recommended that an instructional protocol be established before wider implementation. This should include (a) initial instructor training, (b) an orientation session for participants to familiarize them with the virtual environment, (c) pilot testing of teaching protocols, and (d) session recordings to encourage after-class practice. Future implementation evaluation should also consider (a) program need (demand) assessment for better reach into populations in need of falls prevention interventions, (b) intervention fidelity evaluation, (c) participants’ preferences regarding in-person versus virtual classes and perceptions of practical barriers to attending virtual exercise classes, and (d) engaging care providers as part of the intervention.
Limitations
Given the preliminary nature of our study, several limitations should be noted. First, falls data were ascertained monthly via self-reports, a method that is known to be subject to recall bias. Second, even though we did not encounter any individuals who lacked access to the Internet or to a viewing device, it is likely that in the future there may be a small proportion of older adults who may not have access to these resources and therefore would not be able to participate in technology-driven virtual exercise interventions. Third, we did not consider enrolling older adults at high risk of falling (ie, persons with multiple falls or impaired gait or balance). To increase the clinical relevance of the program, future trials should target persons at high risk of falling per current clinical guidelines.39,40 Fourth, our study was conducted at a time when outdoor activities were highly restricted due to the COVID-19 pandemic. Although it is clear from existing data that older adults fall in indoor and home settings,41 with the proportion increasing among persons aged 75+ years of age,42 it is likely that home-stay restrictions limited participants’ habitual or leisure outdoor activities, which consequently decreased their exposure to community (hazardous) environments where the risk of falls can be heightened. Thus, the findings in this study may underestimate the potential impact of this intervention on falls prevention. Lastly, as a feasibility study, our study was not powered on the primary outcome of falls. Nevertheless, our results provide useful information that will enable us to power a future large-scale trial.
Conclusions
The results of our study indicate the feasibility and potential benefits of a specially tailored dual-task Tai Ji Quan falls prevention intervention, delivered online via Zoom, for community-dwelling older adults with MCI. A fully powered randomized controlled trial with a clinical population of older adults with cognitive impairment should be undertaken to determine whether the program would result in a reduction in falls and amelioration of the risk of falls, thus informing clinical practice.
Data Sharing Statement
The de-identified data that support the findings of this study may be made available from the corresponding author (FL), upon reasonable request. Restrictions may apply to preserve participant confidentiality.
Author Contributions
All authors contributed to the conception and design, analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The study reported in this manuscript was supported by the National Institute on Aging (3R01AG059546-02S1). The opinions expressed are those of the authors and do not necessarily represent the official views of the National Institute on Aging. The authors of this paper reported no other conflicts of interest.
References
- 1.World Health Organization. WHO global report on falls prevention in older age. Available from: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf. Accessed April10, 2021.
- 2.Centers for Disease Control and Prevention. Older adults falls. Available from: https://www.cdc.gov/homeandrecreationalsafety/falls/index.html. Accessed April13, 2021.
- 3.Ansai JH, de Andrade LP, Masse FA, et al. Risk factors for falls in older adults with mild cognitive impairment and mild Alzheimer Disease. J Geriatr Phys Ther. 2019;42(3):E116–E121. doi: 10.1519/JPT.0000000000000135 [DOI] [PubMed] [Google Scholar]
- 4.Gllali G, Launay CP, Blumen HM, et al. Falls, cognitive impairment, and gait performance: results from the GOOD Initiative. J Am Med Dir Assoc. 2017;18(4):335–340. doi: 10.1016/j.jamda.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li F, Harmer P. Prevalence of falls, physical performance, and dual-task cost while walking in older adults at high risk of falling with and without cognitive impairment. Clin Interv Aging. 2020;15:945–952. doi: 10.2147/CIA.S254764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604 [DOI] [PubMed] [Google Scholar]
- 7.Montero-Odasso M, Speechley M. Falls in cognitively impaired older adults: implications for risk assessment and prevention. J Am Geriatr Soc. 2018;66(2):367–375. doi: 10.1111/jgs.15219 [DOI] [PubMed] [Google Scholar]
- 8.Bahureksa L, Najafi B, Saleh A, et al. The impact of mild cognitive impairment on gait and balance: a systematic review and meta-analysis of studies using instrumented assessment. Gerontol. 2017;63:67–83. doi: 10.1159/000445831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kearney FC, Harwood RH, Gladman JRF, Lincoln N, Masud T. The relationship between executive function and falls and gait abnormalities in older adults: a systematic review. Dement Geriatr Cogn Disord. 2013;36:20–35. doi: 10.1159/000350031 [DOI] [PubMed] [Google Scholar]
- 10.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9(9):CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tricco AC, Thomas SM, Veroniki AA, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. 2017;318(17):1687–1699. doi: 10.1001/jama.2017.15006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51:1750–1758. doi: 10.1136/bjsports-2016-096547 [DOI] [PubMed] [Google Scholar]
- 13.Peek K, Bryant J, Carey M, et al. Reducing falls among people living with dementia: a systematic review. Dementia. 2020;19(5):1621–1640. doi: 10.1177/1471301218803201 [DOI] [PubMed] [Google Scholar]
- 14.Burton E, Cavalheri V, Adams R, et al. Effectiveness of exercise programs to reduce falls in older people with dementia living in the community: a systematic review and meta-analysis. Clin Interv Aging. 2015;10:421–434. doi: 10.2147/CIA.S71691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li F, Harmer P, Eckstrom E, et al. Efficacy of exercise-based interventions in preventing falls among community-dwelling older persons with cognitive impairment: is there enough evidence? An updated systematic review and meta-analysis. Age Ageing. In Press 2021 (doi: 10.1093/ageing/afab110) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) – older Adults. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html. Accessed April13, 2021.
- 17.Li F, Harmer P, Eckstrom E, et al. Effectiveness of a therapeutic Tai Ji Quan intervention vs multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Intern Med. 2018;178(10):1301–1310. doi: 10.1001/jamainternmed.2018.3915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li F, Harmer P, Liu Y, Chou LS, Tai J. Quan and global cognitive function in older adults with cognitive impermanent: a pilot study. Arch Gerontol Geriatr. 2014;58(3):434–439. doi: 10.1016/j.archger.2013.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes C, Berg L, Danziger W, Coben L, Martin R. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566 [DOI] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 21.Li F. Transforming traditional tai ji quan techniques into integrative movement therapy—Tai Ji Quan: moving for better balance. J Sport Health Sci. 2014;3(1):9–15. doi: 10.1016/j.jshs.2013.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li F, Harmer P, Stock R, et al. Implementing an evidence-based fall prevention program in an outpatient clinical setting. J Am Geriatr Soc. 2013;61(12):2142–2149. doi: 10.1111/jgs.12509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li F, Harmer P, Fitzgerald K. Implementing an evidence-based fall prevention intervention in community senior centers. Am J Public Health. 2016;106(11):2026–2031. doi: 10.2105/AJPH.2016.303386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rossiter-Fornoff J, Walf S, Wolfson L. A cross-sectional validation study of the FICSIT common data base static balance measures. J Gerontol a Biol Sci Med Sci. 1995;50A(6):M291–M297. doi: 10.1093/gerona/50A.6.M291 [DOI] [PubMed] [Google Scholar]
- 25.Jones C, Rekli R, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113. doi: 10.1080/02701367.1999.10608028 [DOI] [PubMed] [Google Scholar]
- 26.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 27.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 28.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–M197. doi: 10.1093/geronj/45.6.M192 [DOI] [PubMed] [Google Scholar]
- 29.United Nation. Policy brief: the impact of COVID-19 on older persons. Available from: https://unsdg.un.org/sites/default/files/2020-05/Policy-Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf. Accessed April13, 2021.
- 30.Krendl AC, Perry BL. The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. J Gerontol Psychol Sci. 2021;72(2):e53–e58. doi: 10.1093/geronb/gbaa110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lamb SE, Sheehan B, Atherton N, et al. Dementia and physical activity (DAPA) trial of moderate to high intensity exercise training for people with dementia: randomised controlled trial. BMJ. 2018;361:k1675. doi: 10.1136/bmj.k1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldberg SE, van der Wardt V, Brand A, et al. Promoting activity, independence and stability in early dementia (PrAISED): a multisite, randomised, feasibility trial. BMC Geriatr. 2019;19:353. doi: 10.1186/s12877-019-1379-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lipardo DS, Tsang W. Effects of combined physical and cognitive training on fall prevention and risk reduction in older persons with mild cognitive impairment: a randomized controlled study. Clin Rehab. 2020;34(6):773–782. doi: 10.1177/0269215520918352 [DOI] [PubMed] [Google Scholar]
- 34.Nyman SR, Ingram W, Sanders J, et al. Randomised controlled trial of the effect of Tai Chi on postural balance of people with dementia. Clin Interv Aging. 2019;14:2017–2029. doi: 10.2147/CIA.S228931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Varela-Vásquez LA, Minobes-Molina E, Jerez-Roig J. Dual-task exercises in older adults: a structured review of current literature. J Frailty Sarcopenia Falls. 2020;5(2):31–37. doi: 10.22540/JFSF-05-031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghai S, Ghai I, Effenberg AO. Effects of dual tasks and dual-task training on postural stability: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:557–577. doi: 10.2147/CIA.S125201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li F, Harmer P, Chou LS. Dual-task walking capacity mediates Tai Ji Quan impact on physical and cognitive function. Med Sci Sports Exerc. 2019;51(11):2318–2324. doi: 10.1249/MSS.0000000000002051 [DOI] [PubMed] [Google Scholar]
- 38.Li F. The public health benefits of Tai Ji Quan – addressing the unmet needs of aging populations in the 21st century. J Sport Health Sci. 2016;5(3):304–307. doi: 10.1016/j.jshs.2016.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x [DOI] [PubMed] [Google Scholar]
- 40.U.S. Centers for Disease Control and Prevention. STEADI: older adults fall prevention. Available from: https://www.cdc.gov/steadi/materials.html. Accessed February10, 2021.
- 41.Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30-S4:3–7. doi: 10.1093/ageing/30.suppl_4.3 [DOI] [PubMed] [Google Scholar]
- 42.Pynoos J, Steinman BA, Nguyen A. Environmental assessment and modification as fall-prevention strategies for older adults. Clin Geriatr Med. 2010;26(4):633–644. doi: 10.1016/j.cger.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]