Abstract
Coronavirus disease 2019 (COVID-19), an emergent disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has rapidly spread throughout the globe since its discovery in December 2019. Although first appreciated to cause pneumonia, numerous organ systems are now known to be involved. The objective of this article is to review the broad spectrum of cutaneous manifestations reported in association with SARS-CoV-2 infection. The most commonly reported cutaneous manifestations associated with COVID-19 infection include pernio (chilblain)-like acral lesions, morbilliform (exanthematous) rash, urticaria, vesicular (varicella-like) eruptions, and vaso-occlusive lesions (livedo racemosa, retiform purpura). It is important to consider SARS-CoV-2 infection in the differential diagnosis of a patient presenting with these lesions in the appropriate clinical context, as cutaneous manifestations may be present in otherwise asymptomatic individuals, or present before developing other symptoms of infection. With increased access to diagnostic testing, we are beginning to understand the utility and limitations of currently available assays.
Keywords: COVID-19, SARS-CoV-2, Dermatology, Morphology
Key points
-
•
Numerous skin manifestations associated with COVID-19 have been reported. Dermatologists should be aware of these cutaneous manifestations, which may help with diagnosis, management, and prognosis.
-
•
The most commonly reported cutaneous manifestations associated with COVID-19 infection include pernio (chilblain)-like acral lesions, morbilliform (exanthematous) rash, urticaria, vesicular (varicella-like) eruptions, and vaso-occlusive lesions (livedo racemosa, retiform purpura).
-
•
It is important to consider COVID-19 on the differential diagnosis for these disease entities in the proper clinical context, as dermatologic findings of COVID-19 can be a presenting sign in an otherwise minimally or asymptomatic individual.
Introduction
In December 2019, unexplained pneumonia cases were reported in Wuhan, China. The new pathogen, named SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), was isolated from samples of the respiratory tract of infected patients, and the resulting disease was called COVID-19 (coronavirus disease 2019). The virus traveled rapidly throughout the globe and was characterized as a pandemic by the World Health Organization on March 11, 2020.
It was soon recognized that COVID-19 patients were experiencing myriad clinical manifestations involving multiple organ systems (including the central nervous, gastrointestinal, and cardiovascular systems), as well as viral illness-induced coagulopathy.1, 2, 3, 4 Initial case series rarely documented skin changes, possibly due to the lack of dermatologists caring for patients with COVID-19 infection as well as the inability to perform complete skin examinations in critically ill patients. Dermatologists also experienced significant challenges collecting samples and taking clinical images while maintaining strict infection prevention techniques, particularly with a widespread limited supply of personal protective equipment.5 In an early cohort study of 1099 patients with laboratory-confirmed COVID-19, only 2 patients were noted to have “skin rash.”6
Shortly thereafter, small cohorts of patients were being reported to have cutaneous findings possibly associated with COVID-19 infection.7 , 8 The reported findings ranged from those more commonly seen in viral infections, such as morbilliform eruptions and urticaria, to more unique, such as pernio and varicelliform eruptions. A large case series describing patterns of skin manifestations among 375 patients highlighted 5 predominant morphologic patterns: maculopapular, urticarial, pernio-like, vesicular, and livedoid.9 This series also provided for the first time, a temporal relationship between cutaneous lesions, systemic symptoms, as well as severity of disease. As COVID-19 testing was initially only available to those with severe disease, the true incidence of cutaneous manifestations with COVID-19 infection is not yet known. The pandemic has encouraged broad collaboration among physicians and scientists around the world,10 facilitated by multiple registries, which are helping us increase our understanding of dermatologic manifestations in patients with COVID-19.11 , 12
Virology/Immunology
SARS-CoV-2 is a single-stranded RNA virus composed of 16 nonstructural proteins, each of which plays a specific role in replication.13 SARS-CoV-2 binds to angiotensin-converting enzyme 2 (ACE2) receptors, which is known to be found in the lungs (surfactant producing alveolar type 2 cells) as well as the cardiovascular, gastrointestinal, pulmonary, and renal systems.14 Expression of ACE2 in the skin is highest in keratinocytes, followed by sweat glands. The widespread expression of ACE2 in the skin is just one of the potential reasons for cutaneous manifestations seen with COVID-19 infection.15 , 16
Pernio (chilblain)-Like Acral Lesions
Since the outbreak of SARS-CoV-2, reports of pernio-like acral lesions have rapidly accumulated. Pernio (chilblains) is an idiopathic cold-sensitive inflammatory disorder that manifests as pink to violaceous macules, papules, plaques, or nodules at sites of cold exposure, commonly on the fingers or toes.17 Chilblains may be idiopathic or may be associated with autoimmune conditions (ie, chilblains lupus), hematologic malignancies, genetic mutations, and less commonly infections, such as Epstein-Barr virus (EBV).18 When EBV-associated, cold agglutinins are thought to play a role in pathogenesis.18 Skin findings may be accompanied by pruritus, pain, burning, and sometimes blistering or ulceration. When making a diagnosis of chilblains, it is important to rule out Parvovirus B19 infection, which can present with acral purpuric lesions.
The first report of pernio-like lesions thought to be associated with COVID-19 was of an Italian adolescent (with family members suspected of having COVID-19 infection) who developed purpuric lesions on the feet before developing systemic symptoms such as fever and myalgias.19 Reports of young adults with skin lesions on hands and feet identical to chilblains began appearing, seemingly later in the course of their infection.9 Analysis of Google Trends data, which illustrates popularity of search trends over a period in a particular location, demonstrated that there were sharp increases in search terms including chilblains, fingers, and toes in early 2020.20 , 21 As this phenomenon became better known and circulated on social media, it was colloquialized as “COVID-toes,” although the precise relationship with SARS-CoV-2 continues to be elucidated. The association was first suspected for multiple reasons: there was a spike in cases during the pandemic, at an atypical time of year for symptoms to occur (spring), in temperate areas, and in patients typically at low risk (ie, no known comorbid conditions associated with chilblains such as autoimmunity,22 connective tissue disease such as lupus erythematosus, Raynaud phenomenon/syndrome, or a history of chilblains).
Before the pandemic, pernio was uncommon; one case series reported an average of 9 to 10 diagnoses per year across an entire tertiary academic center.18 Since the onset of the pandemic, studies from around the world have reported numerous individuals with pernio-like lesions thought to be associated with COVID-19 infection. In a French retrospective study on skin manifestations during the early COVID-19 outbreak, pernio-like lesions were noted in 38.3% (106 of 277) of dermatologic outpatients.23 More recently, an international registry of COVID-19 dermatologic manifestations has recorded 619 cases of pernio in patients with suspected or confirmed COVID-19 infection.24 Patients with pernio-like lesions are noted to present with pruritus and pain of their toes (less often fingers or heels), which progresses to pink-red papules or plaques and then to violaceous purpuric lesions.25 Rarely, pernio-like lesions have been reported in other acral sites, such as on the ear.26 In addition to pernio-like lesions, variations in morphologies have been reported, including erythema multiforme (EM)-like (round, maculopapular, or targetoid lesions), punctiform purpuric lesions, diffuse vascular erythema, and edema of the dorsum/sole of foot or palms.27 Patients with COVID-19 who develop pernio have relatively mild courses; with 2% to 16% of patients with pernio-like lesions being hospitalized.9 , 28, 29, 30, 31, 32 This can be compared to other dermatologic manifestations associated with more severe disease such as retiform purpura, where 100% of patients were hospitalized, with 82% of patients developing acute respiratory distress syndrome.28 Pernio-like acral lesions should be recognized as distinct from acroischemic lesions. The two terms were initially used synonymously, but acroischemic lesions are now known to represent a separate manifestation seen among critically ill patients with hypercoagulopathy and/or disseminated intravascular coagulation.8
Histopathology of pernio-like lesions is similar to that of idiopathic or systemic disease-associated chilblains. Pathology frequently contains vascular changes, dermal edema, and a superficial and deep perivascular lymphocytic infiltrate. In select reports, immunohistochemistry has confirmed vasculitis of dermal vessels, deposition of immunoglobulins or complement on dermal vessels, and platelet aggregation.22 , 31 When histologic findings of pernio-like lesions in multiple reports were reviewed, it appears that these lesions are primarily inflammatory, nonischemic, and not reflective of systemic coagulopathy, unlike retiform purpura or acral ischemia.28 Furthermore, the microthrombi seen in a small subset of patients with chilblains are likely secondary to the inflammation and clinically correlate with a bullous or necrotic phenotype.33
In a study of dermoscopy features of COVID-19–related chilblains in children and adolescents, dermoscopic findings were found to correlate with clinical and histopathologic findings of COVID-19–related chilblains. For example, the background color noted on dermoscopy is an indicator of vascular macules, hemosiderin, and inflammatory cells in the dermis; gray areas may be indicative of an ischemic phenomenon, and globules likely representing damaged vessels with extravasated red cells. The specificity of these findings, however, is unclear as there is no dermoscopic study of primary chilblains or chilblains secondary to other causes.34 , 35
Overall, pernio-like lesions are typically seen in patients with relatively mild COVID-19 disease courses and resolve within 2 to 8 weeks (median 12 days in laboratory-confirmed cases).32 , 36 , 37 However, persistent and recurrent lesions have been reported. Recent data illustrate a subset of patients with “long COVID” in the skin who had dermatologic signs of COVID-19 that persisted longer than 60 days, including 7 of 103 cases of pernio.37 Recurrent pernio-like lesions in the absence of reinfection have also been noted, with patients who complained of pernio in the fall experiencing an absence of symptoms in the summer, despite surges of COVID-19 infections in the warmer months.24 Of note, pernio lesions in type I interferonopathies are also known to flare with cold exposure.38
There are increasing number of reports suggesting a direct association between pernio-like lesions and SARS-CoV-2. Positive anti–SARS-CoV-2 immunostaining and viral spike protein have been demonstrated in lesional skin biopsy specimens (endothelial cells and eccrine glands) in adult and pediatric patients with pernio-like lesions.39, 40, 41 However, owing to lack of specificity, some authors have suggested that these findings be interpreted with caution.42, 43, 44
The pathogenesis of pernio-like lesions is not well understood but is thought to be predominantly an inflammatory process similar to idiopathic and autoimmune-related chilblains. The striking similarity of pernio-like lesions to those observed in type 1 interferonopathies (ie, Aicardi-Goutieres syndrome and STING-associated vasculopathy) has raised the suspicion of the important role of interferon (IFN) despite the absence of other manifestations of interferonopathies in patients with COVID-19 infection.45, 46, 47 One group demonstrated induction of the type I IFN pathway in lesional sections of COVID-19–associated chilblain-like lesions.48 Type I interferon is known to have an important role in the pathogenesis of lupus erythematosus.49 , 50 Furthermore, interferons are also thought to induce microangiopathic changes contributing to the development of chilblains lupus.46 , 47
As mounting evidence suggests a direct association with SARS-CoV-2, pernio-like lesions are currently believed to represent a postviral or late-onset finding after COVID-19 infection, especially in those who can mount a robust IFN response. In a report by Freeman and colleagues, 80 of 318 cases developed pernio-like lesions after the onset of other symptoms of COVID-19 infection; a similar finding has been noted in at least one other study.9 , 32 Conversely, pernio-like lesions have also been reported to occur concurrently with RT-PCR test positivity.32 , 51 Negative nasopharyngeal reverse-transcription polymerase chain reaction (RT-PCR) or anti–SARS-CoV-2 serologies in many patients52, 53, 54, 55, 56, 57, 58 created uncertainty early in the pandemic regarding the precise relationship.39 , 54 , 57, 58, 59 Indeed, some patients who were RT-PCR negative after developing pernio, were later found to have positive COVID-19 antibodies (immunoglobulin M, G, or A).24 , 26 , 32 , 60 , 61
- What was initially surprising, however, was that serologic testing for IgM or IgG antibodies was often negative. There is increased understanding of this mechanism:
-
I.Early in the pandemic, interpretation of RT-PCR/antibody results in patients with skin rash and probable COVID-19 was difficult due to lack of understanding of timing and antibody kinetics. Much of the available antibody data were drawn from patients with more severe illness as widespread testing was not available. Many patients with pernio-like lesions were undergoing serologic evaluation for SARS-CoV-2 antibodies early in the disease course. In one study, patients had antibody testing between 3 and 30 days after pernio developed, with most evaluated less than 15 days after pernio onset.57 It is now appreciated that delayed antibody development after infection with SARS-CoV-2 is common.62 In one early report, positive antibodies were detected a median of 30 days from disease onset, beyond the typical 14- to 21-day testing window.63
-
II.Population level antibody testing from the past year has revealed that there is a relationship between disease severity and the level of SARS-CoV-2 antibodies. In one particular hospital, for both IgG and IgA isotypes, patients with moderate/severe infection had significantly higher antibody titers within the first 1.5 months after diagnosis compared to those with milder disease.64 As previously discussed, it is now well-established that those with COVID-19 who develop chilblains have relatively mild clinical courses and may not mount a marked antibody response, similar to others with minimal symptoms of infection.60 Despite a more muted antibody response, data suggest that patients with milder SARS-CoV-2 infection are able to elicit in vitro neutralizing antibodies (preventing the virus from entering epithelial cells).65 Negative RT-PCR on nasopharyngeal swabs is supportive of the notion that pernio-like lesions are a late symptom of COVID-19.28
-
III.Most serologic testing for SARS-CoV-2 currently is against SARS-CoV-2 IgM and IgG. It is appreciated that the host immune response to SARS-CoV-2 infection includes synthesis of several types of virus-specific antibodies including IgM, IgG, and IgA.66 , 67 There are also reports that some patients with pernio-like lesions have positive serology for anti–SARS-CoV-2 IgA.55 , 60 The authors postulated that children with mild or asymptomatic infection may develop an IgA humoral response, rather than IgG. Secretory IgA plays a vital role in host protection of mucosal surfaces by preventing entry and subsequent infection by respiratory viruses including influenza; elevated levels are also associated with improved influenza vaccine efficacy.68 With SARS-CoV-2, a pathogen that first interacts with the immune system at mucosal surfaces/lungs due to person-to-person respiratory transmission, a robust IgA response appears before IgG. IgA serum levels reach their peak earlier than IgG (10–14 days) suggesting that both IgA and IgG are part of the initial humoral immune response. Given that currently widely used commercial antibody tests do not look for IgA, a “negative antibody test” may not truly reflect the absence of prior infection and/or antibody production.
-
IV.The kinetics of early interferon production may determine overall COVID-19 disease severity and antibody production. Interferons are early antiviral response proteins that interfere with intracellular viral replication, recruit other cells for antiviral response, and cause “flu-like symptoms” such as fever and muscle pain. It is thought that robust production of interferon-I is associated with early viral control, suppressed antibody response, and mild COVID-19 infection. This may be an additional explanation for why some patients fail serologic detection.69 Conversely, patients with severe COVID-19 have notably depressed/absent interferon responses or interferon deficiency that can lead to severe, life-threatening COVID-19 infection.70, 71, 72, 73 Several authors hypothesize that chilblains, specifically, could be the cutaneous expression of a strong type I interferon response.74, 75, 76, 77 This could therefore explain the absence of antibodies in patients with chilblains.
-
I.
There is a correlation between the severity of COVID and the timing of appearance of COVID-antigen–specific CD4 T-cells in circulation. Patients with the early expansion of antigen-specific CD4 T-cells (2 days after symptom onset) seem to have mild COVID and those who have a late response (CD4 appearance >20 days after symptoms) have severe disease, suggesting that an early CD4 T-cell response is important in fighting SARS-CoV-2 infection.78 Sekine and colleagues have demonstrated T-cell immunity to SARS-CoV-2 in those with mild COVID-19 infection who were also subsequently seronegative.79
Morbilliform Eruptions
Morbilliform (maculopapular) eruptions frequently arise as a result of viral infections or adverse drug reactions, and are the most commonly reported cutaneous manifestation of COVID-19 with a prevalence as high as 47%.7 , 9 , 23 , 28 , 80 Predominantly involving the trunk, the rash has been noted either at disease onset, or more frequently, after hospital discharge, with a reported median duration of 7 days.7 , 37 , 81 Morbilliform eruptions are associated with intermediate severity of disease.82 It is difficult to definitively associate morbilliform eruptions with SARS-CoV-2 infection as many reported patients may have received concomitant drug therapy for their infection. Although medications given as a part of COVID-19 treatment (ie, ribavarin, IVIG, and antiretroviral drugs) may cause morbilliform eruptions, this manifestation has been noted in patients with no new medications.83 , 84 Taking a detailed history is critical, and it is important to consider COVID-19 testing in patients when the eruption is not better explained by medications or other infections.
Urticarial Eruptions
Urticaria (hives) is a common feature among COVID-19 patients who experienced rashes. Acute urticaria, defined as a self-limited lesion lasting less than 6 weeks, has been reported as a presenting sign of COVID-19 infection, although it can also occur later in the disease course.7 , 9 , 23 , 28 , 45 COVID-associated urticaria has also been reported to present with fever as an early prodromal sign in otherwise asymptomatic individuals.85, 86, 87 Acute urticaria can be triggered by infections, medications, insect bites/stings, and type I immune reactions. It has been hypothesized that viral IgM/IgG can cross-react with mast cell IgE and cause mast cell degranulation, which could explain urticaria in the setting of COVID-19 infection.88 It is important to note that urticaria is also a possible side-effect for numerous medications used to treat COVID-19.84 COVID-19–associated urticarial eruptions are reported to last a median of 4 days with a maximum duration of 28 days.37 Although the specificity of urticaria to COVID-19 infection is low, in patients with new onset urticaria developing during the pandemic, one should consider evaluation for COVID-19 infection with RT-PCR and serologic studies.
Vesicular Eruptions
Vesicles are fluid-filled collections in the epidermis less than ½ cm in diameter. Vesicles can be caused by a variety of viral infections including varicella-zoster, herpes simplex, echovirus, and coxsackievirus infections.89 Most patients with COVID-19 presenting with varicella-like exanthem also have general respiratory and general symptoms of COVID-19 infection. One Italian study including 22 patients reported vesicular, varicelliform lesions, which developed on average 3 days after onset of COVID-19 symptoms.90 Although more often being reported as developing early after onset of systemic signs of COVID-19 infection (up to 79.2%),91 15% of patients in one study developed this rash before other symptoms.9 The papulovesicular exanthems noted in association with COVID-19 infection differ from true varicella infection with their truncal involvement, scattered distribution, and minimal pruritus.90 Vesicular lesions are thought to be associated with moderate severity of COVID-19.9 , 91 In the appropriate clinical context, COVID-19 testing (in addition to HSV/VZV PCR) should be performed in a patient presenting with varicelliform cutaneous eruption.
Two morphologies of COVID-associated vesicular eruption have been described: localized, monomorphic lesions typically involving the trunk or back, and a more diffuse polymorphic eruption notable for small papules, vesicles, and pustules of varying sizes.91 The distribution of lesions involving the trunk and back mimics Grover disease (transient acantholytic dermatosis), a benign condition seen in older Caucasian men with crusted papules and papulovesicles on the trunk and back. COVID-19–associated varicella-like exanthem can share some histologic similarity to Grover disease. In one report of 3 cases, a prominent nonballooning acantholysis with intraepidermal vesicle and eosinophilic dyskeratosis without nuclear atypia was noted, leading to the suggestion that this entity would be better termed “COVID-19–associated acantholytic rash.”92 Conversely, in other histologic reports of COVID-19–associated vesicular eruptions, histology was consistent with viral infection, with vacuolar degeneration of the basal layer with multinucleate, hyperchromatic keratinocytes and dyskeratotic cells.90 , 93
Erythema Multiforme-like Lesions
EM is an acute, typically self-limited hypersensitivity reaction involving the skin and mucous membranes presenting with concentric three-ring targetoid plaques on acral surfaces. It is clinically characterized as presenting with acute onset of concentric (targetoid) plaques. In adults, more than 90% of EM is thought to be triggered by infection, particularly the herpes simplex virus. EM-like eruptions of targetoid lesions with either truncal or acral predominance have been observed in association with SARS-CoV-2 infection in adults and children.9 , 94, 95, 96, 97 Children with COVID-19 who develop EM generally have mild respiratory/gastrointestinal symptoms or are otherwise asymptomatic.98 In one series, 2 of 4 children with suspected COVID-related EM underwent skin biopsies with positive immunohistochemistry staining of endothelium to SARS-CoV-2 spike protein.99 Another study reported 4 hospitalized women with COVID-19 infection who developed pink truncal papules evolving to targetoid lesions, which resolved in all 4 patients within 2 to 3 weeks.94 A 60-year-old woman with fixed urticarial eruption (nonevanescent) underwent skin biopsy, which was notable for slight vacuolar-type interface dermatitis with necrotic keratinocytes and no eosinophils, most consistent with an EM-like pattern, highlighting that not all EM-like lesions present as targets.100
Pityriasis Rosea-like Eruption
Pityriasis rosea (PR) is a common papulosquamous eruption presenting with ovoid patches and plaques with fine collarettes of scale. In classic cases, a solitary lesion (herald patch) precedes the development of a more diffuse eruption. Lesions are classically formed along skin fold lines on the trunk. PR-like eruptions have been noted to be occurring in greater frequency and in association with SARS-CoV-2 infection.101, 102, 103, 104, 105, 106, 107 An atypical digitate papulosquamous variant in an elderly patient with COVID-19 infection has also been reported.108 Although the exact cause of typical PR is unclear, viral etiologies, including human herpesvirus (HHV)-6 and 7 have been favored. Reactivation of HHV-6 and EBV has been demonstrated in one patient with COVID-19 infection and PR.109 A recent report demonstrated 2 patients with PR-like rash and urticaria-like rash with COVID-19 infection with SARS-CoV-2 spike protein present in the endothelium of dermal blood vessels of affected skin.110 It is unclear if the increased incidence of PR is due to direct viral infection of SARS-CoV-2, reactivation of HHV-6/7, or other factors. Testing for infection is recommended in a patient who presents with this characteristic eruption in the appropriate clinical context.
Pediatric COVID-19
Despite more than 3.85 million testing positive for COVID-19 since the onset of the pandemic, children have been relatively spared from severe COVID-19–related complications, with less frequent infection, less severe respiratory sequelae, and generally a milder course.111 , 112 This milder course is attributed to children having fewer predisposing factors for severe disease (ie, cardiovascular disease, diabetes mellitus), healthy vascular endothelium, strong antiviral innate immunity, and fewer ACE receptors in nasal and lung epithelium, making viral entry and infection more difficult.113
In children, cutaneous signs of COVID-19 may be the predominant or only clue of infection and, in fact, are not uncommon. Cutaneous lesions of COVID-19 occur in more than 8% of hospitalized children114 and are the 7th most common extrapulmonary manifestation.115 There are several case reports and case series of various cutaneous eruptions in COVID-positive children. Children with COVID-19 and skin manifestations carry an overall better prognosis than those without.116
Multisystem Inflammatory Syndrome in Children (MIS-C)
Since April 2020, there have been multiple reports worldwide of severe pediatric disease several weeks (median 25 days) after SARS-CoV-2 infection with fevers, multiorgan involvement, and characteristics of Kawasaki disease (KD).117, 118, 119 This syndrome has been called MIS-C and is thought to be a postviral consequence of COVID-19 infection. There is confirmed laboratory evidence of COVID-19 infection in 99% of cases, antibody testing is positive, and RT-PCR tends to be negative. The US Centers for Disease Control and Prevention (CDC) has developed a case definition of MIS-C (Table 1 ).120
Table 1.
Case definition for Multisystem Inflammatory Syndrome in Children (MIS-C) associated with COVID-19 infection120
| Criteria | Additional Information | |
|---|---|---|
| Age <21 y | ||
| Fever | Fever ≥38.0°C for ≥24 h, or report of subjective fever lasting ≥24 h | |
| Laboratory evidence of inflammation | Including, but not limited to, one or more of the following: an elevated CRP, ESR, fibrinogen, procalcitonin, D-dimer, ferritin, LDH, or IL-6, elevated neutrophils, reduced lymphocytes, and low albumin | |
| Multisystem (≥2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic, or neurologic) | Organ system | Examples of involvement130,131 |
| Gastrointestinal | Abdominal pain, diarrhea, nausea, vomiting, abnormal hepatobiliary markers | |
| Hematologic | Fever, myalgias, lymphadenopathy, fatigue, abnormal blood counts | |
| Neurologic | Headache, irritability, altered mental status, dizziness | |
| Dermatologic | Cutaneous eruption, conjunctivitis, edema, mucositis | |
| Respiratory | Dyspnea, upper respiratory infection-like signs, cough, wheezing, respiratory failure, pulmonary infiltrates | |
| Cardiovascular | Shock, chest pain, myocarditis, coronary artery dilatation/aneurysm, elevated cardiac enzyme markers | |
| Renal | Acute kidney injury | |
| No alternative plausible diagnoses; AND | ||
| Positive for current or recent SARS-CoV-2 infection by RT-PCR, serology, or antigen test; or exposure to a suspected or confirmed COVID-19 case within the 4 wk before the onset of symptoms. |
Abbreviations: CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; IL-6, interleukin 6; LDH, lactic acid dehydrogenase.
MIS-S shares some features of KD and toxic shock syndrome, including fever and skin, mucous membrane, and distal extremity changes. However, it is considered a distinct disease. In contrast to KD, MIS-C is being seen in older children and adolescents (median age 9 years) and non-Hispanic black and Hispanic children, whereas KD more commonly affects children younger than 5 years who are of East Asian descent. In addition, children with MIS-C experience more gastrointestinal symptoms and less than 50% meet formal criteria for KD.121 , 122
The pathogenesis of MIS-C is thought to be multifactorial, including the robust immune system of children, immune complex activation, and the superantigen activity of SARS-CoV-2 spike protein all leading to cytokine storm and systemic inflammation.123, 124, 125 MIS-C cases and deaths unfortunately continue to accumulate; although most children with this condition require intensive care, patients with MIS-C carry a good prognosis, with current mortality estimated at 2%.
Although many studies have described cutaneous involvement with MIS-C, the type of rash, distribution, and clinical course needs to be studied further. Greater than 50% of cases of MIS-C are reported to have mucocutaneous changes. Reported mucocutaneous findings include morbilliform, scarlatiniform, urticarial, and reticulated patterns, as well as periorbital edema, malar rash, and reticulated exanthems similar to erythema infectiosum.126 In addition, distal extremity changes, oral mucous membrane changes, conjunctivitis, and purpura are reported.127 The molecular mechanisms underlying the relationship between COVID-19 and MIS-C are poorly understood. There are increasing numbers of adults being reported to have COVID-19–associated MIS-C, characterized by multiorgan dysfunction (particularly cardiac) in the absence of severe respiratory illness.128 , 129
Vascular Lesions
Petechiae and purpura
Petechiae and purpura (visible hemorrhage into the skin or mucous membranes) are among the less commonly described cutaneous manifestations of COVID-19 infection. The first COVID-19–associated cutaneous manifestation with purpuric features was reported by Joob and colleagues, who described a petechial rash misdiagnosed as dengue in a COVID-19 patient.132 Only 3% of patients in a French study of 277 patients had petechial skin lesions.23 Petechial eruptions can have many etiologies including platelet deficiency or dysfunction, disorders of coagulation, and loss of vascular wall integrity. This morphology is associated with certain viral infections including enterovirus, parvovirus B19, and dengue virus.133 COVID-19–associated petechial and purpuric lesions have been noted on acral surfaces, intertriginous regions, extremities, or diffusely.9 , 23 , 134, 135, 136 When secondary to vasculitis, lesions can progress to form blisters.137 Henoch-Schonlein Purpura and IgA vasculitis has been reported to be triggered by SARS-CoV-2 infection.138, 139, 140
Livedo reticularis-like lesions
Livedo reticularis (LR) is a transient finding that classically presents with a blue-purple reticulated vascular pattern. LR results from alterations in vascular flow, which results in accumulation of deoxygenated blood in the cutaneous venous plexis. LR has been observed in association with COVID-19 infection.141, 142, 143 Although cases of LR were grouped with more severe necrosis in a major early study,9 more recent reports estimate that this manifestation was present in 3.5% of patients.28
Fixed livedo racemosa, retiform purpura, and necrotic vascular lesions
Vaso-occlusive lesions (livedo racemosa, thrombotic retiform purpura, and acral ischemia) have been noted in elderly, critically ill patients with severe COVID-19 infection.9 , 28 , 144 These clinical entities exist at the opposite end of the disease severity spectrum compared to perniosis, which occurs in those with mild or asymptomatic disease. Patients with this clinical finding have been noted to have markedly elevated D-dimer levels and disseminated intravascular coagulation.8 , 144 Skin biopsy of a COVID patient with retiform purpuric patches showed multiple occlusive thrombi in most small vessels of the superficial and mid-dermis.145 Direct immunofluorescence in this patient was notable for IgM, C3 and C9 deposition within dermal vessel walls.145 In a subsequent study of a series of COVID patients with retiform purpura, terminal complements C5b-9 and other complement components were found in the microvasculature. This may be suggestive of systemic complement activation and pathophysiology similar to atypical hemolytic uremic syndrome or other microthrombotic syndromes.144 Pauci-inflammatory purpuric (most often on buttocks) pressure ulcers have also been noted in several critically ill COVID patients with limited mobility, incontinence, and malnutrition.146 Histopathology of these purpuric pressure ulcers were consistent with pressure necrosis (epidermal necrosis, eccrine gland necrosis); SARS-CoV-2 RNA in-situ hybridization of all 4 skin biopsies was negative. The reported patients did not have any laboratory evidence of coagulopathy such as disseminated intravascular coagulation.146 It is important to recognize that this clinical finding is distinct from the thrombotic vasculopathy noted by Magro and colleagues144
In a recent review of the literature, vaso-occlusive lesions were found to be the least commonly reported cutaneous manifestation with COVID-19 infection but may portend a worse prognosis with the highest mortality rate of all COVID-associated cutaneous manifestations (18.2%).82 , 147
Other reported cutaneous manifestations/associations
| Cutaneous Manifestation | Subtype, if Applicable | Morphology | Additional Clinical Findings |
|---|---|---|---|
| Alopecia | Androgenetic alopecia | Hair loss from the anterior hairline moving posteriorly or thinning at the vertex scalp | Associated with worse clinical outcomes in some studies148,149 |
| Telogen effluvium | Diffuse hair shedding 2–3 mo after a stressor150,151 | ||
| Gianotti-Crosti-like rash | Pruritic erythematous papules and vesicles on elbows, anterior thighs, and bilateral popliteal fossa coalescing into plaques.152 | Rash started 18 d after onset of symptoms, 13 d after +COVID test, and 3 d after resolution of all respiratory and systemic symptoms. | |
| SDRIFE-like | Erythematous rash on bilateral axillae and antecubital fossae, which subsequently extended to trunk and inner thighs153,154 | ||
| Grover-disease-like | Red papules and papulovesicles distributed on the trunk155 Note: some evidence suggests clinical overlap with vesicular, or “varicella-like” eruptions | ||
| Erythema elevatum diutinum-like | Firm symmetric smooth nodules on extensor surfaces, particularly joints156 | ||
| Reactive infectious mucocutaneous eruption (formerly known as Mycoplasma-induced rash and mucositis) | Shallow erosions of the vermilion lips, hard palate, periurethral glans penis.157 | Reported patient with +COVID PCR 1 wk before rash onset, and again positive at rash onset. Mycoplasma PCR negative, IgM negative, IgG positive (consistent with past exposure). | |
| Enanthems (eruptions of the mucous membranes) | 83% (5 patients) with petechial enanthem ± macular enanthem158 | Recorded from a group of 21 patients with COVID-19 and skin rash ranging from papulovesicular, purpuric periflexural, and erythema multiforme-like. | |
| Oral lesions | Aphthous-like, ulcerations, and macules, tongue depapillation, angular cheilitis, ulcers, blisters, white plaques, dark pigmentations.159 | Etiology postulated to be multifactorial. Hypotheses include direct action of SARS-CoV-2 on oral mucosal cells, coinfection, immunity impairment, or adverse drug reactions160 | |
| Acute genital ulcers (Lipschütz ulcers) | Necrotic ulcers with raised, sharply demarcated borders of the labia minora with no evidence of “kissing lesions.”161 | Single oral aphtha was also observed, with no cutaneous involvement | |
| Transient rash in newborns | Transient “rash” (morphology not described) in babies born to mothers with COVID-19.162 Mottling noted in a neonate with sepsis and +COVID-19.163 |
Abbreviation: SDRIFE, symmetric drug-related intertriginous and flexural exanthema.
Discussion
As the novel SARS-CoV-2 virus rapidly spread throughout the world, the scientific and medical community has worked with remarkable pace to understand its full clinical effects. Early in the pandemic, scarcity of diagnostic assays limited our ability to confirm infection in patients presenting with an array of cutaneous manifestations. Most young patients presenting with pernio-like lesions had mild clinical courses, which precluded them from having access to COVID-19 testing early in the pandemic when diagnostic resources were limited.
Viral infections are known to produce a variety of clinical findings due not only to their direct action on human cells but also to the host immune response and resulting inflammatory cascade. Further complicating the clinical picture, patients with COVID-19 infections were often treated with a multitude of medications, many of which can be associated with the reported cutaneous manifestations. Now with relative widespread availability of RT-PCR assays and serologic testing, we are beginning to understand the utility and limitations of testing (including timing in relation to a patient’s infection course and imperfect sensitivities and specificities of available tests).62 , 164 It is now understood that a negative swab or antibody test at one point in time does not necessarily rule out SARS-CoV-2 as a causative agent.164 Data derived from a UK COVID Symptoms Study app suggest that those with cutaneous rash are more likely to test positive for SARS-CoV-2 (odds ratio 1.67).165 Although less prevalent than fever, the authors also found rash to be more specific for COVID-19 infection, which lends support to the diagnostic value of cutaneous manifestations of SARS-CoV-2 infection.165
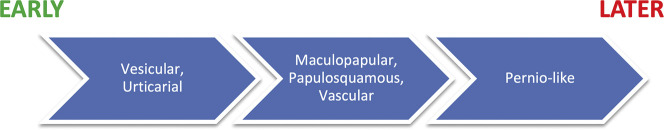
The most commonly reported cutaneous manifestations associated with COVID-19 infection include pernio-like, urticarial, morbilliform, and retiform purpura. As previously discussed, identifying cutaneous eruptions and their possible association with SARS-CoV-2 infection can allow for early identification of infection, sometimes even before onset of more classic symptoms such as respiratory distress.82 As seen in Fig. 1 , Jamshidi and colleagues in their systematic review found that vesicular and urticarial eruptions are seen early relative to other COVID-19 symptoms. Maculopapular, papulosquamous, vascular lesions tend to occur around the time that a patient is symptomatic. Pernio-like lesions occur later in the disease course.82 Certain cutaneous morphologies are noted to correlate to severity of illness and overall prognosis. According to a study by Galvan and colleagues, pernio-like, vesicular, urticarial, maculopapular, and livedoid/necrotic lesions were associated with progressively increasing disease severity.9 This has been corroborated by another study by Freeman and colleagues, which demonstrated cutaneous manifestations associated with a spectrum of severity, with pernio-like lesions noted in mild disease, vesicular/urticarial/macular erythema/morbilliform eruption in intermediate severity, and retiform purpura in critically ill patients.28 Similarly, pernio-like lesions and morbilliform eruptions are associated with the highest survival rates (98.7% and 98.2%, respectively), whereas vaso-occlusive lesions are associated with the lowest survival rate of 78.9%.147 It is important to consider SARS-CoV-2 infection in the differential diagnosis of a patient presenting with these lesions (ie, new onset pernio-like lesions, vesicular or morbilliform eruption) in the appropriate clinical context, as cutaneous manifestations may be present in otherwise asymptomatic individuals, or present before developing other symptoms of infection.
Fig. 1.
Timing of skin lesions relative to other COVID-19 symptoms.82
The coronavirus pandemic has been found to disproportionally affect people of color in both the United States and the United Kingdom, yet registry data on cutaneous manifestations in this population is lacking.28 A systematic review of literature describing cases of cutaneous manifestations associated with COVID-19 found a significant paucity of reports and photographs of manifestations in skin of color, and no published photos of cutaneous manifestations in Fitzpatrick type V or VI skin.166 A recent study suggests there are geographic differences in the morphology and prevalence of COVID-19–associated skin manifestations.147 More work must be done to better understand the true prevalence of skin findings in COVID-19 across all populations and ethnicities.
Summary
The clinical phenotype of COVID-19 includes a broad spectrum of cutaneous manifestations of varying degrees of severity and specificity. Although initially thought to be an infection with primarily internal/systemic manifestations, COVID-19 has taught us that dermatologists play an important role in the treatment of COVID-19 patients, as well as in the broad scientific collaboration to learn more about the pathophysiology of infection. Widespread availability of COVID-19 tests, as well as improved diagnostic assays, will further assist our understanding of how skin manifestations are related to this viral infection, and parse out potential confounding factors such as concurrent pharmacotherapy or lifestyle changes.
Clinics care points
-
•
Cutaneous manifestations of COVID-19 are generally benign and self-limited. These manifestations have prognostic significance depending on type of skin lesion. Pernio (chilblain)-like acral lesions are generally associated with mild disease; retiform purpura is typically seen in patients on the severe end of the disease severity spectrum.
-
•
Cutaneous manifestations may be present in otherwise asymptomatic individuals, or present before developing other symptoms of infection.
-
•
With increased access to diagnostic testing, we are beginning to understand the utility and limitations of currently available assays.
Acknowledgments
Disclosure
The authors have nothing to disclose.
References
- 1.Hajifathalian K., Mahadev S., Schwartz R.E., et al. SARS-COV-2 infection (coronavirus disease 2019) for the gastrointestinal consultant. World J Gastroenterol. 2020;26(14):1546–1553. doi: 10.3748/wjg.v26.i14.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helms J., Kremer S., Merdji H., et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020;382(23):2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bikdeli B., Madhavan M.V., Jimenez D., et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batlle D., Soler M.J., Sparks M.A., et al. Acute kidney injury in COVID-19: Emerging evidence of a distinct pathophysiology. J Am Soc Nephrol. 2020;31(7):1380–1383. doi: 10.1681/ASN.2020040419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez-Nieto D., Ortega-Quijano D., Segurado-Miravalles G., et al. Comment on: Cutaneous manifestations in COVID-19: a first perspective. Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol. 2020;34(6):e252–e254. doi: 10.1111/jdv.16470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan W., Ni Z., Hu Y., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y., Cao W., Xiao M., et al. Clinical and coagulation characteristics in 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020;41(4):302–307. doi: 10.3760/cma.j.issn.0253-2727.2020.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galván Casas C., Català A., Carretero Hernández G., et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson P.C., Yazdany J. The COVID-19 Global Rheumatology Alliance: collecting data in a pandemic. Nat Rev Rheumatol. 2020;16(6):293–294. doi: 10.1038/s41584-020-0418-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freeman E.E., McMahon D.E., Fitzgerald M.E., et al. The American Academy of Dermatology COVID-19 registry: Crowdsourcing dermatology in the age of COVID-19. J Am Acad Dermatol. 2020;83(2):509–510. doi: 10.1016/j.jaad.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freeman E.E., McMahon D.E., Hruza G.J., et al. International collaboration and rapid harmonization across dermatologic COVID-19 registries. J Am Acad Dermatol. 2020;83(3):e261–e266. doi: 10.1016/j.jaad.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Y., Liu Q., Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prompetchara E., Ketloy C., Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38(1):1–9. doi: 10.12932/AP-200220-0772. [DOI] [PubMed] [Google Scholar]
- 15.Li M.Y., Li L., Zhang Y., et al. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1) doi: 10.1186/s40249-020-00662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xue X., Mi Z., Wang Z., et al. High Expression of ACE2 on Keratinocytes Reveals Skin as a Potential Target for SARS-CoV-2. J Invest Dermatol. 2021;141(1):206–209.e1. doi: 10.1016/j.jid.2020.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hedrich C.M., Fiebig B., Hauck F.H., et al. Chilblain lupus erythematosus - A review of literature. Clin Rheumatol. 2008;27(8):949–954. doi: 10.1007/s10067-008-0942-9. [DOI] [PubMed] [Google Scholar]
- 18.Cappel J.A., Wetter D.A. Clinical characteristics, etiologic associations, laboratory findings, treatment, and proposal of diagnostic criteria of pernio (chilblains) in a series of 104 patients at Mayo Clinic, 2000 to 2011. Mayo Clin Proc. 2014;89(2):207–215. doi: 10.1016/j.mayocp.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Mazzotta F., Troccoli T. Acute Acro-ischemia in the Child at the time of COVID-19. Eur J Pediat Dermatol. 2020;30(2):71–74. [Google Scholar]
- 20.Kluger N., Scrivener J.N. The use of Google Trends for acral symptoms during COVID-19 outbreak in France. J Eur Acad Dermatol Venereol. 2020;34(8):e358–e360. doi: 10.1111/jdv.16572. [DOI] [PubMed] [Google Scholar]
- 21.Hughes M., Rogers S., Lepri G., et al. Further evidence that chilblains are a cutaneous manifestation of COVID-19 infection. Br J Dermatol. 2020;183(3):596–598. doi: 10.1111/bjd.19243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanitakis J., Lesort C., Danset M., et al. Chilblain-like acral lesions during the COVID-19 pandemic (“COVID toes”): Histologic, immunofluorescence, and immunohistochemical study of 17 cases. J Am Acad Dermatol. 2020;83(3):870–875. doi: 10.1016/j.jaad.2020.05.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Masson A., Bouaziz J.D., Sulimovic L., et al. Chilblains is a common cutaneous finding during the COVID-19 pandemic: A retrospective nationwide study from France. J Am Acad Dermatol. 2020;83(2):667–670. doi: 10.1016/j.jaad.2020.04.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freeman E.E., McMahon D.E., Lipoff J.B., et al. Cold and COVID: recurrent pernio during the COVID-19 pandemic. Br J Dermatol. 2021 doi: 10.1111/bjd.19894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hubiche T., Cardot-Leccia N., Le Duff F., et al. Clinical, Laboratory, and Interferon-Alpha Response Characteristics of Patients with Chilblain-like Lesions during the COVID-19 Pandemic. JAMA Dermatol. 2020 doi: 10.1001/jamadermatol.2020.4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Proietti I., Tolino E., Bernardini N., et al. Auricle perniosis as a manifestation of Covid-19 infection. Dermatol Ther. 2020;33(6) doi: 10.1111/dth.14089. [DOI] [PubMed] [Google Scholar]
- 27.Le Cleach L., Dousset L., Assier H., et al. Most chilblains observed during the COVID-19 outbreak occur in patients who are negative for COVID-19 on PCR and serology testing. Br J Dermatol. 2020 doi: 10.1111/bjd.19377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freeman E.E., McMahon D.E., Lipoff J.B., et al. The spectrum of COVID-19–associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):1118–1129. doi: 10.1016/j.jaad.2020.06.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez-Nieto D., Jimenez-Cauhe J., Suarez-Valle A., et al. Characterization of acute acral skin lesions in nonhospitalized patients: A case series of 132 patients during the COVID-19 outbreak. J Am Acad Dermatol. 2020;83(1):e61–e63. doi: 10.1016/j.jaad.2020.04.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andina D., Noguera-Morel L., Bascuas-Arribas M., et al. Chilblains in children in the setting of COVID-19 pandemic. Pediatr Dermatol. 2020;37(3):406–411. doi: 10.1111/pde.14215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kolivras A., Dehavay F., Delplace D., et al. Coronavirus (COVID-19) infection–induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 2020;6(6):489–492. doi: 10.1016/j.jdcr.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freeman E.E., McMahon D.E., Lipoff J.B., et al. Pernio-like skin lesions associated with COVID-19: A case series of 318 patients from 8 countries. J Am Acad Dermatol. 2020;83(2):486–492. doi: 10.1016/j.jaad.2020.05.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baeck M., Herman A., Peeters C., et al. Are chilblains a skin expression of COVID-19 microangiopathy? J Thromb Haemost. 2020;18(9):2414–2415. doi: 10.1111/jth.15008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Navarro L., Andina D., Noguera-Morel L., et al. Dermoscopy features of COVID-19-related chilblains in children and adolescents. J Eur Acad Dermatol Venereol. 2020;34(12):e762–e764. doi: 10.1111/jdv.16800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piccolo V., Bassi A., Argenziano G., et al. Dermoscopy of chilblain-like lesions during the COVID-19 outbreak: A multicenter study on 10 patients. J Am Acad Dermatol. 2020;83(6):1749–1751. doi: 10.1016/j.jaad.2020.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marzano A.V., Genovese G., Moltrasio C., et al. The clinical spectrum of COVID-19-associated cutaneous manifestations: an Italian multicentre study of 200 adult patients. J Am Acad Dermatol. 2021 doi: 10.1016/j.jaad.2021.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMahon D.E., Gallman A.E., Hruza G.J., et al. Long COVID in the skin: a registry analysis of COVID-19 dermatological duration. Lancet Infect Dis. 2021 doi: 10.1016/s1473-3099(20)30986-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orcesi S., La Piana R., Fazzi E. Aicardi-Goutires syndrome. Br Med Bull. 2009;89(1):183–201. doi: 10.1093/bmb/ldn049. [DOI] [PubMed] [Google Scholar]
- 39.Colmenero I., Santonja C., Alonso-Riaño M., et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br J Dermatol. 2020;183(4):729–737. doi: 10.1111/bjd.19327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santonja C., Heras F., Núñez L., et al. COVID-19 chilblain-like lesion: immunohistochemical demonstration of SARS-CoV-2 spike protein in blood vessel endothelium and sweat gland epithelium in a polymerase chain reaction-negative patient. Br J Dermatol. 2020;183(4):778–780. doi: 10.1111/bjd.19338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gambichler T., Reuther J., Stücker M., et al. SARS-CoV-2 spike protein is present in both endothelial and eccrine cells of a chilblain-like skin lesion. J Eur Acad Dermatol Venereol. 2021;35(3):e187–e189. doi: 10.1111/jdv.16970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ko C.J., Harigopal M., Damsky W., et al. Perniosis during the COVID-19 pandemic: Negative anti-SARS-CoV-2 immunohistochemistry in six patients and comparison to perniosis before the emergence of SARS-CoV-2. J Cutan Pathol. 2020;47(11):997–1002. doi: 10.1111/cup.13830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baeck M., Hoton D., Marot L., et al. Chilblains and COVID-19: why SARS-CoV-2 endothelial infection is questioned. Br J Dermatol. 2020;183(6):1152–1153. doi: 10.1111/bjd.19489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brealey J.K., Miller S.E. SARS-CoV-2 has not been detected directly by electron microscopy in the endothelium of chilblain lesions. Br J Dermatol. 2021;184(1):186. doi: 10.1111/bjd.19572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bouaziz J.D., Duong T.A., Jachiet M., et al. Vascular skin symptoms in COVID-19: a French observational study. J Eur Acad Dermatol Venereol. 2020;34(9):e451–e452. doi: 10.1111/jdv.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rodero M.P., Crow Y.J. Type I interferonâ-mediated monogenic autoinflammation: The type i interferonopathies, a conceptual overview. J Exp Med. 2016;213(12):2527–2538. doi: 10.1084/jem.20161596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Papa R., Volpi S., Gattorno M. Monogenetic causes of chilblains, panniculitis and vasculopathy: The Type I interferonopathies. G Ital di Dermatologia e Venereol. 2020;155(5):590–598. doi: 10.23736/S0392-0488.20.06709-7. [DOI] [PubMed] [Google Scholar]
- 48.Aschoff R., Zimmermann N., Beissert S., et al. Type I Interferon Signature in Chilblain-Like Lesions Associated with the COVID-19 Pandemic. Dermatopathology. 2020;7(3):57–63. doi: 10.3390/dermatopathology7030010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saeed M. Lupus pathobiology based on genomics. Immunogenetics. 2017;69(1):1–12. doi: 10.1007/s00251-016-0961-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ivashkiv L.B., Donlin L.T. Regulation of type i interferon responses. Nat Rev Immunol. 2014;14(1):36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guarneri C., Venanzi Rullo E., Gallizzi R., et al. Diversity of clinical appearance of cutaneous manifestations in the course of COVID-19. J Eur Acad Dermatol Venereol. 2020;34(9):e449–e450. doi: 10.1111/jdv.16669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baeck M., Peeters C., Herman A. Chilblains and COVID-19: further evidence against a causal association. J Eur Acad Dermatol Venereol. 2021;35(1):e2–e3. doi: 10.1111/jdv.16901. [DOI] [PubMed] [Google Scholar]
- 53.Colonna C., Genovese G., Monzani N.A., et al. Outbreak of chilblain-like acral lesions in children in the metropolitan area of Milan, Italy, during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(3):965–969. doi: 10.1016/j.jaad.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Denina M., Pellegrino F., Morotti F., et al. All that glisters is not COVID: Low prevalence of seroconversion against SARS-CoV-2 in a pediatric cohort of patients with chilblain-like lesions. J Am Acad Dermatol. 2020;83(6):1751–1753. doi: 10.1016/j.jaad.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.El Hachem M., Diociaiuti A., Concato C., et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain-like lesions: lights and shadows on the relationship with COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(11) doi: 10.1111/jdv.16682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Garcia-Lara G., Linares-González L., Ródenas-Herranz T., et al. Chilblain-like lesions in pediatrics dermatological outpatients during the COVID-19 outbreak. Dermatol Ther. 2020;33(5) doi: 10.1111/dth.13516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Herman A., Peeters C., Verroken A., et al. Evaluation of Chilblains as a Manifestation of the COVID-19 Pandemic. JAMA Dermatol. 2020;156(9):998–1003. doi: 10.1001/jamadermatol.2020.2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stavert R., Meydani-Korb A., de Leon D., et al. Evaluation of SARS-CoV-2 antibodies in 24 patients presenting with chilblains-like lesions during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83(6):1753–1755. doi: 10.1016/j.jaad.2020.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roca-Ginés J., Torres-Navarro I., Sánchez-Arráez J., et al. Assessment of Acute Acral Lesions in a Case Series of Children and Adolescents during the COVID-19 Pandemic. JAMA Dermatol. 2020;156(9):992–997. doi: 10.1001/jamadermatol.2020.2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hubiche T., Le Duff F., Chiaverini C., et al. Negative SARS-CoV-2 PCR in patients with chilblain-like lesions. Lancet Infect Dis. 2020 doi: 10.1016/s1473-3099(20)30518-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Papa A., Salzano A.M., Di Dato M.T., et al. Images in Practice: Painful Cutaneous Vasculitis in a SARS-Cov-2 IgG-Positive Child. Pain Ther. 2020;9(2):805–807. doi: 10.1007/s40122-020-00174-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sethuraman N., Jeremiah S.S., Ryo A. Interpreting Diagnostic Tests for SARS-CoV-2. JAMA - J Am Med Assoc. 2020;323(22):2249–2251. doi: 10.1001/jama.2020.8259. [DOI] [PubMed] [Google Scholar]
- 63.Freeman E.E., McMahon D.E., Hruza G.J., et al. Timing of PCR and antibody testing in patients with COVID-19–associated dermatologic manifestations. J Am Acad Dermatol. 2021;84(2):505–507. doi: 10.1016/j.jaad.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ma H., Zeng W., He H., et al. Serum IgA, IgM, and IgG responses in COVID-19. Cell Mol Immunol. 2020;17(7):773–775. doi: 10.1038/s41423-020-0474-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Robbiani D.F., Gaebler C., Muecksch F., et al. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature. 2020;584(7821):437–442. doi: 10.1038/s41586-020-2456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Long Q.X., Liu B.Z., Deng H.J., et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med. 2020;26(6):845–848. doi: 10.1038/s41591-020-0897-1. [DOI] [PubMed] [Google Scholar]
- 67.Sterlin D., Mathian A., Miyara M., et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci Transl Med. 2021;(577):13. doi: 10.1126/scitranslmed.abd2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Abreu R.B., Clutter E.F., Attari S., et al. IgA Responses Following Recurrent Influenza Virus Vaccination. Front Immunol. 2020;11:902. doi: 10.3389/fimmu.2020.00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baeck M., Herman A. COVID toes: Where do we stand with the current evidence? Int J Infect Dis. 2021;102:53–55. doi: 10.1016/j.ijid.2020.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hadjadj J., Yatim N., Barnabei L., et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369(6504):718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Meffre E., Iwasaki A. Interferon deficiency can lead to severe COVID. Nature. 2020;587(7834):374–376. doi: 10.1038/d41586-020-03070-1. [DOI] [PubMed] [Google Scholar]
- 72.Magro C.M., Mulvey J.J., Laurence J., et al. The differing pathophysiologies that underlie COVID-19-associated perniosis and thrombotic retiform purpura: a case series. Br J Dermatol. 2021;184(1):141–150. doi: 10.1111/bjd.19415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park A., Iwasaki A. Type I and Type III Interferons – Induction, Signaling, Evasion, and Application to Combat COVID-19. Cell Host Microbe. 2020;27(6):870–878. doi: 10.1016/j.chom.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lipsker D. A chilblain epidemic during the COVID-19 pandemic. A sign of natural resistance to SARS-CoV-2? Med Hypotheses. 2020;144:109959. doi: 10.1016/j.mehy.2020.109959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Battesti G., El Khalifa J., Abdelhedi N., et al. New insights in COVID-19–associated chilblains: A comparative study with chilblain lupus erythematosus. J Am Acad Dermatol. 2020;83(4):1219–1222. doi: 10.1016/j.jaad.2020.06.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Damsky W., Peterson D., King B. When interferon tiptoes through COVID-19: Pernio-like lesions and their prognostic implications during SARS-CoV-2 infection. J Am Acad Dermatol. 2020;83(3):e269–e270. doi: 10.1016/j.jaad.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rodríguez-Villa Lario A., Vega-Díez D., González-Cañete M., et al. Histological findings in chilblain lupus-like COVID lesions: in search of an answer to understand their aetiology. J Eur Acad Dermatol Venereol. 2020;34(10):e572–e574. doi: 10.1111/jdv.16733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sette A., Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861–880. doi: 10.1016/j.cell.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sekine T., Perez-Potti A., Rivera-Ballesteros O., et al. Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19. Cell. 2020;183(1):158–168.e14. doi: 10.1016/j.cell.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Najarian D.J. Morbilliform exanthem associated with COVID-19. JAAD Case Rep. 2020;6(6):493–494. doi: 10.1016/j.jdcr.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rubio-Muniz C.A., Puerta-Peña M., Falkenhain-López D., et al. The broad spectrum of dermatological manifestations in COVID-19: clinical and histopathological features learned from a series of 34 cases. J Eur Acad Dermatol Venereol. 2020;34(10):e574–e576. doi: 10.1111/jdv.16734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jamshidi P., Hajikhani B., Mirsaeidi M., et al. Skin Manifestations in COVID-19 Patients: Are They Indicators for Disease Severity? A Systematic Review. Front Med. 2021;8:634208. doi: 10.3389/fmed.2021.634208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reymundo A., Fernáldez-Bernáldez A., Reolid A., et al. Clinical and histological characterization of late appearance maculopapular eruptions in association with the coronavirus disease 2019. A case series of seven patients. J Eur Acad Dermatol Venereol. 2020;34(12):e755–e757. doi: 10.1111/jdv.16707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Türsen Ü., Türsen B., Lotti T. Cutaneous sıde-effects of the potential COVID-19 drugs. Dermatol Ther. 2020;33(4) doi: 10.1111/dth.13476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hassan K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID-19) infection. BMJ Case Rep. 2020;13(7) doi: 10.1136/bcr-2020-236981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.van Damme C., Berlingin E., Saussez S., et al. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(7):e300–e301. doi: 10.1111/jdv.16523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Quintana-Castanedo L., Feito-Rodríguez M., Valero-López I., et al. Urticarial exanthem as early diagnostic clue for COVID-19 infection. JAAD Case Rep. 2020;6(6):498–499. doi: 10.1016/j.jdcr.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Imbalzano E., Casciaro M., Quartuccio S., et al. Association between urticaria and virus infections: A systematic review. Allergy Asthma Proc. 2016;37(1):18–22. doi: 10.2500/aap.2016.37.3915. [DOI] [PubMed] [Google Scholar]
- 89.Drago F., Ciccarese G., Gasparini G., et al. Contemporary infectious exanthems: An update. Future Microbiol. 2017;12(2):171–193. doi: 10.2217/fmb-2016-0147. [DOI] [PubMed] [Google Scholar]
- 90.Marzano A.V., Genovese G., Fabbrocini G., et al. Varicella-like exanthem as a specific COVID-19–associated skin manifestation: Multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83(1):280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fernandez-Nieto D., Ortega-Quijano D., Jimenez-Cauhe J., et al. Clinical and histological characterization of vesicular COVID-19 rashes: a prospective study in a tertiary care hospital. Clin Exp Dermatol. 2020;45(7):872–875. doi: 10.1111/ced.14277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mahé A., Birckel E., Merklen C., et al. Histology of skin lesions establishes that the vesicular rash associated with COVID-19 is not ‘varicella-like. J Eur Acad Dermatol Venereol. 2020;34(10):e559–e561. doi: 10.1111/jdv.16706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Trellu L.T., Kaya G., Alberto C., et al. Clinicopathologic Aspects of a Papulovesicular Eruption in a Patient with COVID-19. JAMA Dermatol. 2020;156(8):922–924. doi: 10.1001/jamadermatol.2020.1966. [DOI] [PubMed] [Google Scholar]
- 94.Jimenez-Cauhe J., Ortega-Quijano D., Carretero-Barrio I., et al. Erythema multiforme-like eruption in patients with COVID-19 infection: clinical and histological findings. Clin Exp Dermatol. 2020;45(7):892–895. doi: 10.1111/ced.14281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gargiulo L., Pavia G., Facheris P., et al. A fatal case of COVID-19 infection presenting with an erythema multiforme-like eruption and fever. Dermatol Ther. 2020;33(4) doi: 10.1111/dth.13779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bapst T., Romano F., Romano F., et al. Special dermatological presentation of paediatric multisystem inflammatory syndrome related to COVID-19: Erythema multiforme. BMJ Case Rep. 2020;13(6):e236986. doi: 10.1136/bcr-2020-236986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Janah H., Zinebi A., Elbenaye J. Atypical erythema multiforme palmar plaques lesions due to Sars-Cov-2. J Eur Acad Dermatol Venereol. 2020;34(8):e373–e375. doi: 10.1111/jdv.16623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.De Giorgi V., Recalcati S., Jia Z., et al. Cutaneous manifestations related to coronavirus disease 2019 (COVID-19): A prospective study from China and Italy. J Am Acad Dermatol. 2020;83(2):674–675. doi: 10.1016/j.jaad.2020.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Torrelo A., Andina D., Santonja C., et al. Erythema multiforme-like lesions in children and COVID-19. Pediatr Dermatol. 2020;37(3):442–446. doi: 10.1111/pde.14246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rodríguez-Jiménez P., Chicharro P., De Argila D., et al. Urticaria-like lesions in COVID-19 patients are not really urticaria – a case with clinicopathological correlation. J Eur Acad Dermatol Venereol. 2020;34(9):e459–e460. doi: 10.1111/jdv.16618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kutlu Ö., Metin A. Relative changes in the pattern of diseases presenting in dermatology outpatient clinic in the era of the COVID-19 pandemic. Dermatol Ther. 2020;33(6) doi: 10.1111/dth.14096. [DOI] [PubMed] [Google Scholar]
- 102.Merhy R., Sarkis A., Stephan F. Pityriasis rosea as a leading manifestation of COVID-19 infection. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.17052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ehsani A.H., Nasimi M., Bigdelo Z. Pityriasis rosea as a cutaneous manifestation of COVID-19 infection. J Eur Acad Dermatol Venereol. 2020;34(9):e436–e437. doi: 10.1111/jdv.16579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dursun R., Temiz S.A. The clinics of HHV-6 infection in COVID-19 pandemic: Pityriasis rosea and Kawasaki disease. Dermatol Ther. 2020;33(4) doi: 10.1111/dth.13730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Veraldi S., Spigariolo C.B. Pityriasis rosea and COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.26679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Veraldi S., Romagnuolo M., Benzecry V. Pityriasis rosea-like eruption revealing COVID-19. Australas J Dermatol. 2020 doi: 10.1111/ajd.13504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Martín Enguix D., Salazar Nievas M. del C., Martín Romero D.T. Pityriasis rosea Gibert type rash in an asymptomatic patient that tested positive for COVID-19. Med Clínica (English Ed. 2020;155(6):273. doi: 10.1016/j.medcle.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sanchez A., Sohier P., Benghanem S., et al. Digitate Papulosquamous Eruption Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020;156(7):819–820. doi: 10.1001/jamadermatol.2020.1704. [DOI] [PubMed] [Google Scholar]
- 109.Drago F., Ciccarese G., Rebora A., et al. Human herpesvirus-6, -7, and Epstein-Barr virus reactivation in pityriasis rosea during COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.26549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Welsh E., Cardenas-de la Garza J.A., Cuellar-Barboza A., et al. SARS-CoV-2 Spike Protein Positivity in Pityriasis Rosea-like and Urticaria-like Rashes of COVID-19. Br J Dermatol. 2021 doi: 10.1111/bjd.19833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Children and COVID-19: State-Level Data Report. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ Available at: Accessed May 13, 2021.
- 112.Assaker R., Colas A.E., Julien-Marsollier F., et al. Presenting symptoms of COVID-19 in children: a meta-analysis of published studies. Br J Anaesth. 2020;125(3):e330–e332. doi: 10.1016/j.bja.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zimmermann P., Curtis N. Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-320338. [DOI] [PubMed] [Google Scholar]
- 114.Kilani M.M., Odeh M.M., Shalabi M., et al. Clinical and laboratory characteristics of SARS-CoV2-infected paediatric patients in Jordan: serial RT-PCR testing until discharge. Paediatr Int Child Health. 2021;41(1):83–92. doi: 10.1080/20469047.2020.1804733. [DOI] [PubMed] [Google Scholar]
- 115.Pousa P.A., Mendonça T.S.C., Oliveira E.A., et al. Extrapulmonary manifestations of COVID-19 in children: a comprehensive review and pathophysiological considerations. J Pediatr (Rio J. 2021;97(2):116–139. doi: 10.1016/j.jped.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rekhtman S., Tannenbaum R., Strunk A., et al. Mucocutaneous disease and related clinical characteristics in hospitalized children and adolescents with COVID-19 and multisystem inflammatory syndrome in children. J Am Acad Dermatol. 2021;84(2):408–414. doi: 10.1016/j.jaad.2020.10.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Galeotti C., Bayry J. Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol. 2020;16(8):413–414. doi: 10.1038/s41584-020-0448-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Verdoni L., Mazza A., Gervasoni A., et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395:1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Feldstein L.R., Tenforde M.W., Friedman K.G., et al. Characteristics and Outcomes of US Children and Adolescents with Multisystem Inflammatory Syndrome in Children (MIS-C) Compared with Severe Acute COVID-19. JAMA - J Am Med Assoc. 2021;325(11):1074–1087. doi: 10.1001/jama.2021.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Information for Healthcare Providers about Multisystem Inflammatory Syndrome in Children (MIS-C) | CDC. https://www.cdc.gov/mis-c/hcp/ Available at: Accessed May 13, 2021.
- 121.Multisystem Inflammatory Syndrome in Children (MIS-C) | CDC. https://www.cdc.gov/mis-c/ Available at: Accessed May 13, 2021.
- 122.Yasuhara J., Watanabe K., Takagi H., et al. COVID-19 and multisystem inflammatory syndrome in children: A systematic review and meta-analysis. Pediatr Pulmonol. 2021;56(5):837–848. doi: 10.1002/ppul.25245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yonker L.M., Neilan A.M., Bartsch Y., et al. Pediatric Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Clinical Presentation, Infectivity, and Immune Responses. J Pediatr. 2020;227:45–52.e5. doi: 10.1016/j.jpeds.2020.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Roe K. A viral infection explanation for Kawasaki disease in general and for COVID-19 virus-related Kawasaki disease symptoms. Inflammopharmacology. 2020;28(5):1219–1222. doi: 10.1007/s10787-020-00739-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Multisystem Inflammatory Syndrome in Children in the United States. N Engl J Med. 2020;383(18):1793–1796. doi: 10.1056/NEJMc2026136. [DOI] [PubMed] [Google Scholar]
- 126.Young T.K., Shaw K.S., Shah J.K., et al. Mucocutaneous Manifestations of Multisystem Inflammatory Syndrome in Children during the COVID-19 Pandemic. JAMA Dermatol. 2020 doi: 10.1001/jamadermatol.2020.4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Whittaker E., Bamford A., Kenny J., et al. Clinical Characteristics of 58 Children with a Pediatric Inflammatory Multisystem Syndrome Temporally Associated with SARS-CoV-2. J Am Med Assoc. 2020;324(3):259–269. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Shaigany S., Gnirke M., Guttmann A., et al. An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19. Lancet. 2020;396(10246):e8–e10. doi: 10.1016/S0140-6736(20)31526-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Morris S.B., Schwartz N.G., Patel P., et al. Morbidity and Mortality Weekly Report Case Series of Multisystem Inflammatory Syndrome in Adults Associated with SARS-CoV-2 Infection-United Kingdom and United States. 2020. https://www.cdc.gov/mis-c/pdfs/hcp/mis-c-form-fillable.pdf Available at: Accessed May 13, 2021. [DOI] [PMC free article] [PubMed]
- 130.Feldstein L.R., Rose E.B., Horwitz S.M., et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020;383(4):334–346. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ahmed M., Advani S., Moreira A., et al. Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine. 2020;26 doi: 10.1016/j.eclinm.2020.100527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.McGrath A., Barrett M.J. StatPearls Publishing; Treasure Island (FL): 2021. Petechiae. In: StatPearls [Internet] [Google Scholar]
- 134.Askin O., Altunkalem R.N., Altinisik D.D., et al. Cutaneous manifestations in hospitalized patients diagnosed as COVID-19. Dermatol Ther. 2020;33(6) doi: 10.1111/dth.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Karaca Z., Yayli S., Çalışkan O. A unilateral purpuric rash in a patient with COVID-19 infection. Dermatol Ther. 2020;33(4) doi: 10.1111/dth.13798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Silva D.H.M., Oppenheimer A.R., Cunha T do A.C. Purpuric rash on the legs of a patient with coronavirus disease. Rev Soc Bras Med Trop. 2020;53:e20200464. doi: 10.1590/0037-8682-0464-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Negrini S., Guadagno A., Greco M., et al. An unusual case of bullous haemorrhagic vasculitis in a COVID-19 patient. J Eur Acad Dermatol Venereol. 2020;34(11):e675–e676. doi: 10.1111/jdv.16760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Suso A.S., Mon C., Oñate Alonso I., et al. IgA Vasculitis With Nephritis (Henoch−Schönlein Purpura) in a COVID-19 Patient. Kidney Int Rep. 2020;5(11):2074–2078. doi: 10.1016/j.ekir.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.AlGhoozi D.A., AlKhayyat H.M. A child with Henoch-Schonlein purpura secondary to a COVID-19 infection. BMJ Case Rep. 2021;14(1) doi: 10.1136/bcr-2020-239910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jacobi M., Lancrei H.M., Brosh-Nissimov T., et al. Purpurona: A Novel Report of COVID-19-Related Henoch-Schonlein Purpura in a Child. Pediatr Infect Dis J. 2021;40(2):e93–e94. doi: 10.1097/INF.0000000000003001. [DOI] [PubMed] [Google Scholar]
- 141.García-Gil M.F., Monte Serrano J., Lapeña-Casado A., et al. Livedo reticularis and acrocyanosis as late manifestations of COVID-19 in two cases with familial aggregation. Potential pathogenic role of complement (C4c) Int J Dermatol. 2020;59(12):1549–1551. doi: 10.1111/ijd.15233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Khalil S., Hinds B.R., Manalo I.F., et al. Livedo reticularis as a presenting sign of severe acute respiratory syndrome coronavirus 2 infection. JAAD Case Rep. 2020;6(9):871–874. doi: 10.1016/j.jdcr.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Manalo I.F., Smith M.K., Cheeley J., et al. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J Am Acad Dermatol. 2020;83(2):700. doi: 10.1016/j.jaad.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Magro C., Mulvey J.J., Berlin D., et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bosch-Amate X., Giavedoni P., Podlipnik S., et al. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID-19) coagulopathy. J Eur Acad Dermatol Venereol. 2020;34(10):e548–e549. doi: 10.1111/jdv.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chand S., Rrapi R., Lo J.A., et al. Purpuric ulcers associated with COVID-19: A case series. JAAD Case Rep. 2021;11:13–19. doi: 10.1016/j.jdcr.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Tan S.W., Tam Y.C., Oh C.C. Skin manifestations of COVID-19: A worldwide review. JAAD Int. 2021;2:119–133. doi: 10.1016/j.jdin.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wambier C.G., Vaño-Galván S., McCoy J., et al. Androgenetic alopecia in COVID-19: Compared to age-matched epidemiologic studies and hospital outcomes with or without the Gabrin sign. J Am Acad Dermatol. 2020;83(6):e453–e454. doi: 10.1016/j.jaad.2020.07.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wambier C.G., McCoy J., Goren A. Male balding as a major risk factor for severe COVID-19: A possible role for targeting androgens and transmembrane protease serine 2 to protect vulnerable individuals. J Am Acad Dermatol. 2020;83(6):e401–e402. doi: 10.1016/j.jaad.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Olds H., Liu J., Luk K., et al. Telogen effluvium associated with <scp>COVID</scp> -19 infection. Dermatol Ther. 2021:e14761. doi: 10.1111/dth.14761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Domínguez-Santás M., Haya-Martínez L., Fernández-Nieto D., et al. Acute telogen effluvium associated with SARS-CoV-2 infection. Aust J Gen Pract. 2020;49 doi: 10.31128/ajgp-covid-32. [DOI] [PubMed] [Google Scholar]
- 152.Brin C., Sohier P., L’honneur A.S., et al. An isolated peculiar gianotti-crosti rash in the course of a covid-19 episode. Acta Derm Venereol. 2020;100(16):1–2. doi: 10.2340/00015555-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chicharro P., Rodríguez-Jiménez P., Muñoz-Aceituno E., et al. SDRIFE-like rash associated with COVID-19, clinicopathological correlation. Australas J Dermatol. 2020 doi: 10.1111/ajd.13444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mahé A., Birckel E., Krieger S., et al. A distinctive skin rash associated with coronavirus disease 2019? J Eur Acad Dermatol Venereol. 2020;34(6):e246–e247. doi: 10.1111/jdv.16471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Boix-Vilanova J., Gracia-Darder I., Saus C., et al. Grover-like skin eruption: another cutaneous manifestation in a COVID-19 patient. Int J Dermatol. 2020;59(10):1290–1292. doi: 10.1111/ijd.15104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Català A., Galván-Casas C., Carretero-Hernández G., et al. Maculopapular eruptions associated to COVID-19: A subanalysis of the COVID-Piel study. Dermatol Ther. 2020;33(6) doi: 10.1111/dth.14170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Holcomb Z.E., Hussain S., Huang J.T., et al. Reactive Infectious Mucocutaneous Eruption Associated With SARS-CoV-2 Infection. JAMA Dermatol. 2021;157(5) doi: 10.1001/jamadermatol.2021.0385. [DOI] [PubMed] [Google Scholar]
- 158.Jimenez-Cauhe J., Ortega-Quijano D., De Perosanz-Lobo D., et al. Enanthem in Patients with COVID-19 and Skin Rash. JAMA Dermatol. 2020;156(10):1134–1136. doi: 10.1001/jamadermatol.2020.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Brandini D.A., Takamiya A.S., Thakkar P., et al. Covid-19 and oral diseases: Crosstalk, synergy or association? Rev Med Virol Published Online. 2021 doi: 10.1002/rmv.2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.La Rosa G.R.M., Libra M., De Pasquale R., et al. Association of Viral Infections With Oral Cavity Lesions: Role of SARS-CoV-2 Infection. Front Med. 2021;7 doi: 10.3389/fmed.2020.571214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Falkenhain-López D., Agud-Dios M., Ortiz-Romero P.L., et al. COVID-19-related acute genital ulcers. J Eur Acad Dermatol Venereol. 2020;34(11):e655–e656. doi: 10.1111/jdv.16740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zimmermann P., Curtis N. COVID-19 in Children, Pregnancy and Neonates: A Review of Epidemiologic and Clinical Features. Pediatr Infect Dis J. 2020;39(6):469–477. doi: 10.1097/INF.0000000000002700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kamali Aghdam M., Jafari N., Eftekhari K. Novel coronavirus in a 15-day-old neonate with clinical signs of sepsis, a case report. Infect Dis (Auckl) 2020;52(6):427–429. doi: 10.1080/23744235.2020.1747634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Freeman E.E., McMahon D.E., Fox L.P. Emerging Evidence of the Direct Association Between COVID-19 and Chilblains. JAMA Dermatol. 2020 doi: 10.1001/jamadermatol.2020.4937. [DOI] [PubMed] [Google Scholar]
- 165.Visconti A., Bataille V., Rossi N., et al. Diagnostic value of cutaneous manifestation of SARS-CoV-2 infection. Br J Dermatol. 2021;(5):184. doi: 10.1111/bjd.19807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lester J.C., Jia J.L., Zhang L., et al. Absence of images of skin of colour in publications of COVID-19 skin manifestations. Br J Dermatol. 2020;183(3):593–595. doi: 10.1111/bjd.19258. [DOI] [PMC free article] [PubMed] [Google Scholar]