Abstract
Obstructive sleep apnea (OSA) in children is leading to several consequences as reported in adults. A continuous positive airway pressure (CPAP) machine is one of the effective treatments in pediatric OSA. However, the CPAP adherence rate is approximately 50%. This study aimed to evaluate if any interventions that improve CPAP adherence in pediatric patients with OSA using a systematic review. We included intervention studies on CPAP adherence in pediatric patients with OSA regardless of machine types. Five databases were used for article searching. Search terms included OSA, adherence, compliance, and CPAP. The outcomes of this study were adherence rate and usage hours/minutes. The outcomes were compared between the intervention and comparator groups with descriptive statistics. There were 2931 articles from 5-database searching. There were 41 articles related with children. There were 7 articles conducted with any intervention on CPAP compliance. Of those, 4 studies included in the analysis. There were 3 significant differences between both groups in 2 studies. Those with caregiver support had significantly longer CPAP use/night by 86.60 minutes (95% CI 10.90, 162.30) and percentage of CPAP usage more than 4 hours/night by 18.10% (95% CI 3.87, 32.33) than those without caregiver support. Those who received BPAP therapy had higher chance of good PAP adherence than those who received CPAP by 18.17 times (95% CI 5.19, 63.70). Caregiver support and BPAP therapy significantly improved CPAP adherence in children with OSA. Further studies are required to add additional comparisons and also other interventions.
Keywords: APAP, BPAP, CPAP, caregivers, compliance
Introduction
Obstructive sleep apnea (OSA) is a disease with collapse of upper airway repeatedly resulting in intermittent hypoxemia during sleep.1 A diagnosis of OSA in children can be made by polysomnography with an apnea-hypopnea index of 2 times/hour.2 In adults, OSA is reported to be associated with several cardiovascular diseases.3 Similarly, OSA in children is associated with several conditions including attention deficit and hyperactivity disorders, poor attention, lower IQ, failure to thrive, hypertension, left ventricular hypertrophy, and poor quality of life.4 Children with OSA had significantly lower IQ than control group (85.8 vs 101.1: P .002).5
A continuous positive airway pressure (CPAP) machine is one of the effective treatments in pediatric OSA.2 A previous study found that adolescent patients with OSA and being adherent to CPAP had significantly improved school performance and quality of life than those without CPAP (P .012 and .034).6 Even though CPAP is effective in 90% of patients, it has a compliance of approximately 50%. In adults, meta-analysis studies showed that an additional intervention such as educational, behavioral, or telemonitoring intervention was shown to improve CPAP adherence by 0.54 to 0.70 hours/night.7,8 However, there is limited data on an effect of additional interventions to improve CPAP adherence in pediatric patients with OSA. This study aimed to evaluate if any interventions that improve CPAP adherence in pediatric patients with OSA using a systematic review.
Methods
This study was a systematic review to evaluate if any interventions on PAP therapy in pediatric patients with OSA were associated with good CPAP adherence. We included intervention studies on CPAP adherence in pediatric patients with OSA. The studies were either observational or randomized controlled trial studies with 2 groups: intervention and comparator group. We excluded studies with any of the following: non-English, conference paper, study protocol, case report, case series, commentary, or non CPAP treatment.
There were several available positive airway pressure machine (PAP) that can be used to treat OSA patients including standard CPAP, automatic CPAP or APAP, Bi-Flex CPAP, or bi-level PAP or BPAP. The standard CPAP has a fixed-level of CPAP pressure, while the APAP has variable CPAP pressure depending on severity of OSA. The Bi-Flex CPAP is a specific technology of the Philips Respironics which lower pressure during late inspiration and expiration. The Bi-Flex technology may improve comfort or adherence.9 The BPAP, non-invasive ventilator, produces positive airway pressure during inspiration and expiration. This machine may be used to improve adherence of PAP machine.10
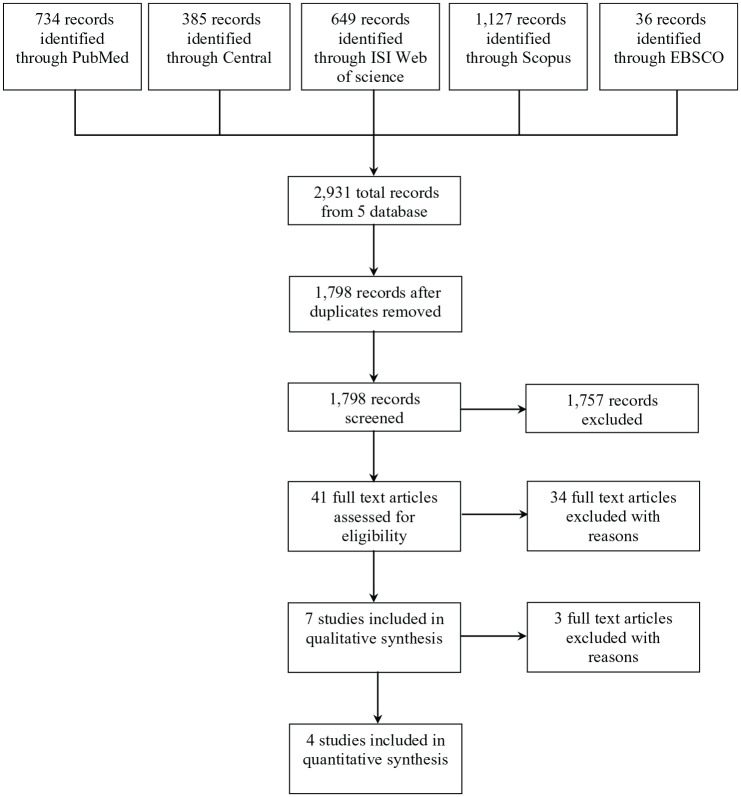
We searched 5 databases in this review: Pubmed, Central database, Scopus, CINAHL Plus, and Web of Science. Search terms included OSA, adherence, compliance, and CPAP. The full list of search terms are shown in an Appendix 1-5. The final search was performed on February 15, 2021. After duplication removal, initial screening was carried out for non-relevant articles. Only pediatric articles were eligible. Those articles without intervention were excluded. Of these, any articles met the study criteria were included in the final analysis. Data extraction and the full-text reviewed were performed by 2 independent authors (BS, KS). A prima flow chart of article searching and included studies was shown in Figure 1.
Figure 1.
Searching results on adherence or compliance of continuous positive airway pressure machine in patients with obstructive sleep apnea.
The outcomes of this study were adherence rate and usage hours/minutes. The definition of good adherence of CPAP in pediatric patients with OSA may be varied, while the usage data was average use of CPAP per night. The outcomes were compared between the intervention and comparator groups with descriptive statistics. For numerical variables, mean differences between both groups were calculated and reported with their 95% confidence interval (CI). Odds ratio with 95% CI was computed to compare differences of proportions between both groups for categorical variables. Heterogeneity was computed and reported as and I square (I2) when appropriate. A forest plot of each comparison was created.
Biases of eligible studies were evaluated across 6 domains (sequence generation, allocation concealment, blinding of participants/personnel and outcome assessors, incomplete outcome data, selective outcome reporting, and other potential sources of bias) for randomized controlled trial. Biases were categorized as low risk, high risk, or unclear according to the guidelines specified in the Cochrane Handbook for Systematic Reviews of Interventions.11 For observational studies, the Newcastle-Ottawa Scale adapted for cross-sectional studies was applied to evaluate study quality.12 The scale comprised of 3 categories: selection process, comparability, and outcome measurement with a score of 5, 2, and 3 points, respectively. The total score was 10 points and classified as very good (9-10 points), good (7-8 points), satisfactory (5-6 points), and unsatisfied (0-4 points). Biases or study quality were evaluated by 2 authors independently (BS, CN). Disagreements were reviewed and reported by a third reviewer (KS). All analyses were performed by Review Manager 5.4.
Ethical Approval and Informed Consent
Not required.
Results
There were 2931 articles from 5-database searching. Of those, there were 1798 articles after removal of duplicated articles. There were 41 articles related with children. Of those, 34 articles were excluded due to not intervention (16 articles), review/book (10 articles), case series (2 articles), poster presentation (2 articles), non-English (2 articles), and commentary (1 article). There were 7 articles conducted with any intervention on CPAP compliance. Of those, 3 articles were excluded due to no comparison group (2 articles) and study protocol (1 article). There 4 articles published from 2008 to 2020 and conducted in 4 countries: Mexico, USA, Australia, and Canada (Table 1).9,13-15 One study was a randomized controlled trial,9 while others were retrospective (2 articles) and cross-sectional study (1 article). Adherence data were objectively evaluated by download data from the PAP machine in all 4 articles with the longest follow up of 1 year.14 The comparator was CPAP machine, while the intervention groups were caregiver support, BPAP, APAP, or Bi-Flex CPAP.
Table 1.
Characteristics of Pediatric Studies with Obstructive Sleep Apnea (OSA) with Any Intervention on Adherence of a Continuous Positive Airway Pressure Machine (CPAP).
| Study | Country | Study design | Inclusion | Definition of adherence | Source | Duration of evaluation | Follow up | Devices |
|---|---|---|---|---|---|---|---|---|
| Castorena-Maldonado et al13 | Mexico | Cross-sectional | Children with OSA | 1. Numbers of days/hours of CPAP use 2. Time that interface is on |
Download data | Weekly | Preoperative 7-71 days | APAP, CPAP |
| Machaalani et al14 | Australia | Retrospective | Age 0-18 years with CPAP or BPAP | 70% of nights with ≥4 hours/night | Download data | 4 weeks | 1 year | BPAP, CPAP |
| Marcus et al9 | USA | RCT | Age 2-16 years with OSA, naïve to PAP | Usage in minutes | Download data | 3 months | 3 months | Bi-Flex CPAP, CPAP |
| Parmar et al15 | Canada | Retrospective | Age 10-18 years with OSA | 1. Average use (minutes/night) 2. % use >4 hours/night |
Download data | 30 nights | 3 months | APAP, CPAP, BPAP |
Abbreviations: APAP: automatic CPAP; BPAP: bi-level positive airway pressure machine.
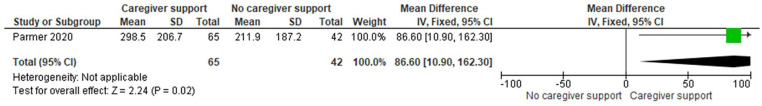
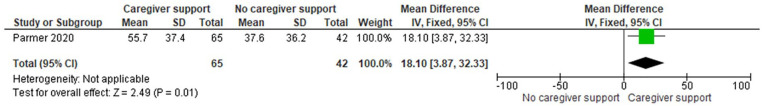
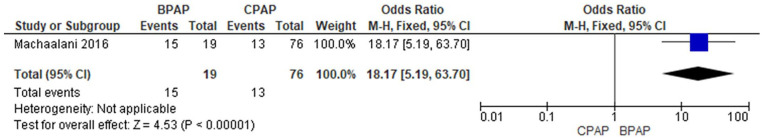
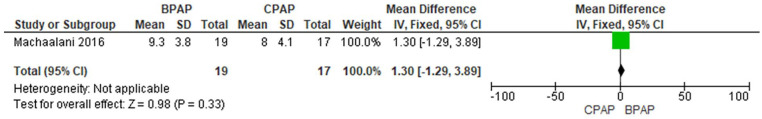
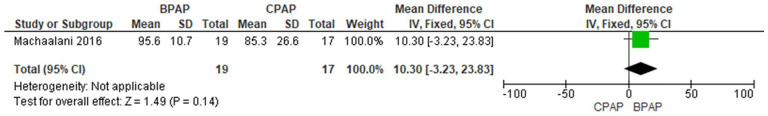
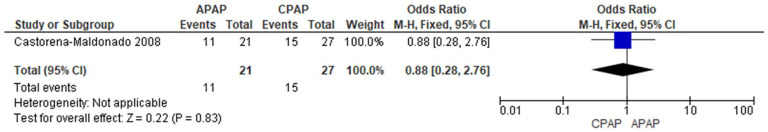
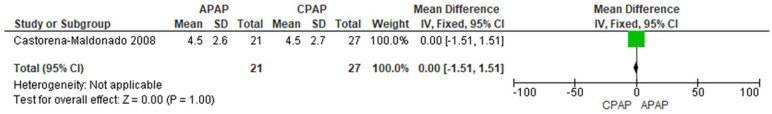
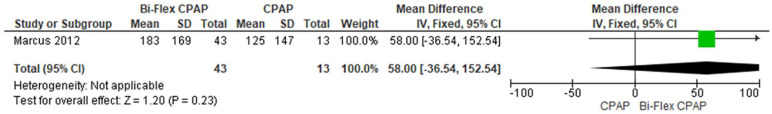
There were 247 pediatric patients enrolled in these 4 articles: 148 patients in the intervention group and 99 patients in the comparator group (Table 2). Regarding outcomes between the intervention and comparator groups (Table 2 and Figures 2–9), 3 studies reported on average PAP used/night and adherence rate.13-15 Among the outcomes, there were 3 significant differences between both groups in 2 studies as shown in Figures 2 to 4.14,15 Those with caregiver support had significantly longer CPAP use/night by 86.60 minutes (95% CI 10.90, 162.30) and percentage of CPAP usage more than 4 hours/night by 18.10% (95% CI 3.87, 32.33) than those without caregiver support (Figures 2 and 3). Those who received BPAP therapy had higher chance of good PAP adherence than those who received CPAP by 18.17 times (95% CI 5.19, 63.70) as shown in Figure 4. For study quality of those observational studies, 2 studies were good studies and 1 study was satisfactory (Table 3). There were 2 questionable biases and low risk for biases in 4 items including blinding of participants/personnel/outcome assessment, incomplete outcome data, selective reporting, and others (Figure 10).
Table 2.
Details and Outcomes of Pediatric Studies with Obstructive Sleep Apnea (OSA) with Any Intervention on Adherence of a Continuous Positive Airway Pressure Machine (CPAP).
| Studies | Intervention | Comparator | N | Intervention outcome | Comparator outcome |
|---|---|---|---|---|---|
| Castorena-Maldonado et al13 | APAP (n = 21) | CPAP (n = 27) | 48 | Hours of use/night 4.5 (2.6) % >4 hours/night 11 (52%)* |
Hours of use/night 4.5 (2.7) % >4 hours/night 15 (56%)* |
| Machaalani et al14 | BPAP (n = 19) | CPAP (n = 17) | 36 | % adherence 15 (80%)*
Hours of use 9.3 (3.8) % day used 95.6 (10.7) % >4 hours/night 86.8 (22.7) |
% adherence 13 (76%)*
Hours of use 8.0 (4.1) % day used 85.3 (26.6) % >4 hours/night 72.4 (35.3) |
| Marcus et al9 | Bi-Flex CPAP (n = 43) |
CPAP (n = 13) | 56 | Minutes of used/night 183 (169) | Minutes of used/night 125 (147) |
| Parmar et al15 | Caregiver support (n = 65) |
No caregiver support (n = 42) | 107 | Minutes of used/night 298.5 (206.7) % use >4 hours/night 55.7 (37.4) |
Minutes of used/night 211.9 (187.2) % use >4 hours/night 37.6 (36.2) |
Indicated proportion.
Abbreviations: APAP: automatic CPAP; BPAP: bi-level positive airway pressure machine.
Figure 2.
Usage of continuous positive airway pressure machine (minutes) in pediatric patients with obstructive sleep apnea compared between those received caregiver support and those did not receive caregiver support.
Figure 3.
Percentage of usage of continuous positive airway pressure machine more than 4 hours/night in pediatric patients with obstructive sleep apnea compared between those received caregiver support and those did not receive caregiver support.
Figure 4.
Proportions of adherence in positive airway pressure machine (PAP) in pediatric patients with obstructive sleep apnea compared between those received bi-level positive airway pressure machine (BPAP) and those received continuous PAP (CPAP).
Figure 5.
Hour usage of positive airway pressure machine (PAP) in pediatric patients with obstructive sleep apnea compared between those received bi-level positive airway pressure machine (BPAP) and those received continuous PAP (CPAP).
Figure 6.
Percentage of day usage of positive airway pressure machine (PAP) in pediatric patients with obstructive sleep apnea compared between those received bi-level positive airway pressure machine (BPAP) and those received continuous PAP (CPAP).
Figure 7.
Proportions of adherence in continuous positive airway pressure machine (CPAP) in pediatric patients with obstructive sleep apnea compared between those received automatic CPAP (APAP) and those received CPAP.
Figure 8.
Hour usage of continuous positive airway pressure machine (CPAP) in pediatric patients with obstructive sleep apnea compared between those received automatic CPAP (APAP) and those received CPAP.
Figure 9.
Minutes usage of continuous positive airway pressure machine (CPAP) in pediatric patients with obstructive sleep apnea compared between those received Bi-Flex CPAP and those received CPAP.
Table 3.
Study Quality Evaluation by the Newcastle-Ottawa Scale Adapted for Cross-Sectional Studies of the Included Studies of Pediatric Studies with Obstructive Sleep Apnea with Any Intervention on Adherence of a Continuous Positive Airway Pressure Machine.
Figure 10.
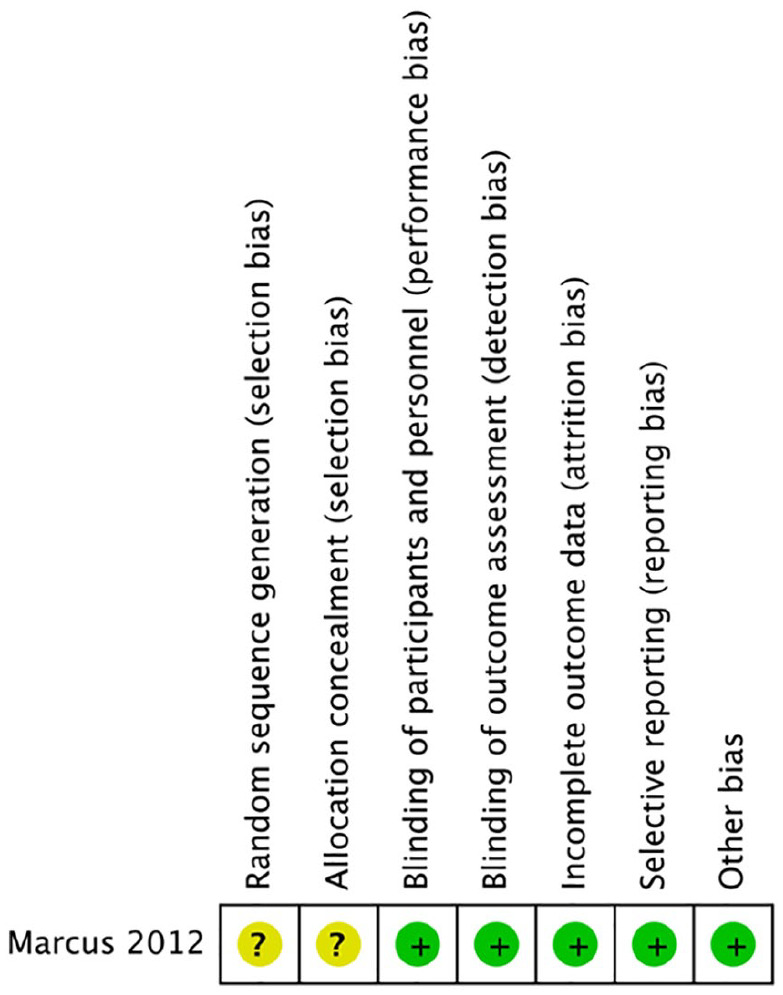
Biases of a randomized controlled trial of pediatric studies with obstructive sleep apnea with any intervention on adherence of a continuous positive airway pressure machine.
Discussion
This systematic review showed that caregiver support and BPAP significantly improved CPAP adherence in pediatric patients with OSA.
Adherence of medical devices or CPAP may be complex.16 There are several factors associated with medical devices such as perception, or experiences on the device.17 A qualitative study conducted in patients with chronic obstructive airway disease who required to be treated with non-invasive ventilation. Similarly to CPAP, discomfort may be associated with chances of non-adherence.18-20 Experiences of CPAP users with side effects were another factor of non-adherence.20,21 Note that these experiences were reported by adult patients with OSA. In children or adolescent patients with OSA, factors associated with non-adherence including sex, development status, and perception.22,23 Girls had higher rate of CPAP adherence than boys (56.5% vs 43.5%; P .01) and those with developmental delay had higher chance of CPAP adherence than those without developmental delay (odds ratio of 2.55; P .007). Additionally, perceptions or experiences with CPAP for non-adherence were some excuses such as does not use when away from home (47%), just want to forget about OSA (43.1%), not feeling well (42.0%), or forgets (39.2%).
Even though there are several factors for CPAP non-adherence, caregiver support, and BPAP may increase CPAP use almost 1 hour. A previous report found that children with OSA do not use CPAP because no one helps them to use CPAP at night in 31.4%.23 Therefore, caregiver support may significantly improve CPAP adherence. Additionally, parents or caregivers may assist children to solve with some CPAP issues such as mask leakage.24 BPAP, non-invasive ventilation, is more comfort than CPAP resulting in better adherence.25 A previous study showed that BPAP had significantly used hours/night than CPAP (2.72 vs 1.49 hours, P < .001) in OSA patients with poor adherence to CPAP.10 The patients using BPAP reported that BPAP is more comfortable than CPAP by visual analog scale (P .02).
There are some limitations in this study. First, there are no definite criteria for adherence in children. Criteria used in the included studies may be varied. Second, the maximum duration of follow up period was 1 year. Third, interventions had only 1 included study resulting in unable to calculate as a meta-analysis. Finally, some interventions are not studied such as educational intervention.
Conclusion
Caregiver support and BPAP therapy significantly improved CPAP adherence in children with OSA. Further studies are required to add additional comparisons and also other interventions.
Appendix
Appendix 1.
Searching Strategy for PubMed (Retrieved on 15 February 2021).
| Search ID | Search terms |
|---|---|
| 1 | obstructive sleep apnea[MeSH Terms] |
| 2 | sleep apnea syndrome[MeSH Terms] |
| 3 | ((obstructive sleep apnea[Title/Abstract]) OR (sleep apnea syndrome[Title/Abstract])) OR (OSA[Title/Abstract]) |
| 4 | (#1 OR #2) OR #3 |
| 5 | “Patient Compliance”[Mesh] OR “Medication Adherence”[Mesh] OR “Treatment Adherence and Compliance”[Mesh] OR “Compliance”[Mesh] OR “Guideline Adherence”[Mesh] |
| 6 | (compliance[Title/Abstract]) OR (adherence[Title/Abstract]) |
| 7 | #5 OR #6 |
| 8 | Continuous Positive Airway Pressure[MeSH Terms] |
| 9 | CPAP[Title/Abstract] |
| 10 | #8 OR #9 |
| 11 | (((predict*[Title/Abstract]) OR (independent[Title/Abstract])) OR (factor*[Title/Abstract])) OR (variable*[Title/Abstract]) |
| 12 | (#4 AND #7) AND (#10 AND #11) |
Appendix 2.
Searching Strategy for Central (Retrieved on 15 February 2021).
| Search ID | Search terms |
|---|---|
| 1 | MeSH descriptor: [Sleep Apnea Syndromes] explode all trees |
| 2 | MeSH descriptor: [Sleep Apnea, Obstructive] explode all trees |
| 3 | (obstructive sleep apnea):ti,ab,kw OR (sleep apnea syndrome):ti,ab,kw OR (OSA):ti,ab,kw |
| 4 | (#1 OR #2) OR #3 |
| 5 | MeSH descriptor: [Patient Compliance] explode all trees |
| 6 | MeSH descriptor: [Treatment Adherence and Compliance] explode all trees |
| 7 | (compliance):ti,ab,kw OR (adherence):ti,ab,kw (Word variations have been searched) |
| 8 | #5 OR #6 OR #7 |
| 9 | MeSH descriptor: [Continuous Positive Airway Pressure] explode all trees |
| 10 | (CPAP):ti,ab,kw (Word variations have been searched) |
| 11 | #9 OR #10 |
| 12 | (((predict* OR independent) OR (factor* OR variable*))):ti,ab,kw (Word variations have been searched) |
| 13 | (#4 AND #8) AND (#11 AND #12) |
Appendix 3.
Searching Strategy for ISI Web of Science (Retrieved on 15 February 2021).
| Search ID | Search terms |
|---|---|
| 1 | TI=(obstructive sleep apnea) OR AB=(obstructive sleep apnea) |
| 2 | TI=(sleep apnea syndrome*) OR AB=(sleep apnea syndrome*) |
| 3 | TI=OSA OR AB=OSA |
| 4 | (#1 OR #2) OR #3 |
| 5 | TI=compliance OR AB=compliance |
| 6 | TI=adherence OR AB=adherence |
| 7 | #6 OR #5 |
| 8 | KP=compliance OR KP=adherence |
| 9 | TI=(Continuous Positive Airway Pressure) OR AB=(Continuous Positive Airway Pressure) |
| 10 | TI=CPAP OR AB=CPAP |
| 11 | KP=CPAP OR KP=(Continuous Positive Airway Pressure) |
| 12 | #8 OR #7 |
| 13 | #11 OR #10 OR #9 |
| 14 | TI=predict* OR AB=predict* |
| 15 | TI=independent OR AB=independent |
| 16 | TI=factor* OR AB=factor* |
| 17 | TI=variable* OR AB=variable* |
| 18 | #17 OR #16 OR #15 OR #14 |
| 19 | #18 AND #13 AND #12 AND #4 |
Appendix 4.
Searching Strategy for Scopus (Retrieved on 15 February 2021).
| (((TITLE-ABS-KEY (obstructive AND sleep AND apnea) OR TITLE-ABS-KEY (sleep AND apnea AND syndrome*) OR TITLE-ABS-KEY (osa))) AND ((TITLE-ABS-KEY (compliance) OR TITLE-ABS-KEY (adherence)))) AND (((TITLE-ABS-KEY (continuous AND positive AND airway AND pressure) OR TITLE-ABS-KEY (cpap))) AND ((TITLE-ABS-KEY (predict*) OR TITLE-ABS-KEY (independent) OR TITLE-ABS-KEY (factor*) OR TITLE-ABS-KEY (variable*)))) |
Appendix 5.
Searching Strategy for EBSCO (Retrieved on 15 February 2021).
| Search ID | Search terms |
|---|---|
| S1 | TI (obstructive sleep apnea or osa) OR AB (obstructive sleep apnea or osa) |
| S2 | TI sleep apnea syndrome* OR AB sleep apnea syndrome* |
| S3 | S1 OR S2 |
| S4 | TI compliance OR AB compliance |
| S5 | TI adherence OR AB adherence |
| S6 | (TI adherence OR AB adherence) AND (S4 OR S5) |
| S7 | TI (continuous positive airway pressure or cpap) OR AB (continuous positive airway pressure or cpap) |
| S8 | TI predict* OR AB predict* |
| S9 | TI independent OR AB independent |
| S10 | TI factor* OR AB factor* |
| S11 | TI variable* OR AB variable* |
| S12 | (TI variable* OR AB variable*) OR (S8 OR S9 OR S10 OR S11) |
| S13 | ((TI variable* OR AB variable*) AND (S8 OR S9 OR S10 OR S11)) AND (S3 AND S6 AND S7 AND S12) |
Footnotes
Author Contributions: BS conceived of the study, conducted the initial reviews, analyzed data, and composed the draft of the article. CN performed the article searches. CN and KS assisted with the reviews of the articles and their analyses and helped prepared the final version of the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kittisak Sawanyawisuth  https://orcid.org/0000-0003-3570-8474
https://orcid.org/0000-0003-3570-8474
References
- 1. Kaditis AG, Alonso Alvarez ML, Boudewyns A, et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47:69-94. doi: 10.1183/13993003.00385-2015 [DOI] [PubMed] [Google Scholar]
- 2. Al-Shamrani A, Alharbi AS. Diagnosis and management of childhood sleep-disordered breathing. Clinical approach. Saudi Med J. 2020;41:916-929. doi: 10.15537/smj.2020.9.25262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315-2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blechner M, Williamson AA. Consequences of obstructive sleep apnea in children. Curr Probl Pediatr Adolesc Health Care. 2016;46:19-26. doi: 10.1016/j.cppeds.2015.10.007 [DOI] [PubMed] [Google Scholar]
- 5. Halbower AC, Degaonkar M, Barker PB, et al. Childhood obstructive sleep apnea associates with neuropsychological deficits and neuronal brain injury. PLoS Med. 2006;3:e301. doi: 10.1371/journal.pmed.0030301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beebe DW, Byars KC. Adolescents with obstructive sleep apnea adhere poorly to positive airway pressure (PAP), but PAP users show improved attention and school performance. PLoS One. 2011;6:e16924. doi: 10.1371/journal.pone.0016924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aardoom JJ, Loheide-Niesmann L, Ossebaard HC, Riper H. Effectiveness of eHealth interventions in improving treatment adherence for adults with obstructive sleep apnea: meta-analytic review. J Med Internet Res. 2020;22:e16972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Askland K, Wright L, Wozniak DR, Emmanuel T, Caston J, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2020;4:CD007736. doi: 10.1002/14651858.cd007736.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marcus CL, Beck SE, Traylor J, et al. Randomized, double-blind clinical trial of two different modes of positive airway pressure therapy on adherence and efficacy in children. J Clin Sleep Med. 2012;8:37-42. doi: 10.5664/jcsm.1656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gulati A, Oscroft N, Chadwick R, Ali M, Smith I. The impact of changing people with sleep apnea using CPAP less than 4 h per night to a Bi-level device. Respir Med. 2015;109:778-783. doi: 10.1016/j.rmed.2015.01.020 [DOI] [PubMed] [Google Scholar]
- 11. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. doi: 10.1002/14651858.ed000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sisay M, Mengistu G, Edessa D. Epidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studies. BMC Pharmacol Toxicol. 2018;19:56. doi: 10.1186/s40360-018-0248-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Castorena-Maldonado A, Torre-Bouscoulet L, Meza-Vargas S, Vázquez-García JC, López-Escárcega E, Pérez-Padilla R. Preoperative continuous positive airway pressure compliance in children with obstructive sleep apnea syndrome: assessed by a simplified approach. Int J Pediatr Otorhinolaryngol. 2008;72:1795-1800. doi: 10.1016/j.ijporl.2008.08.016 [DOI] [PubMed] [Google Scholar]
- 14. Machaalani R, Evans CA, Waters KA. Objective adherence to positive airway pressure therapy in an Australian paediatric cohort. Sleep Breath. 2016;20:1327-1336. doi: 10.1007/s11325-016-1400-6 [DOI] [PubMed] [Google Scholar]
- 15. Parmar A, Messiha S, Baker A, Zweerink A, Toulany A, Narang I. Caregiver support and positive airway pressure therapy adherence among adolescents with obstructive sleep apnea. Paediatr Child Health. 2020;25:491-497. doi: 10.1093/pch/pxz107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aalaei S, Rezaeitalab F, Tabesh H, et al. Factors Affecting patients’ adherence to continuous positive airway pressure therapy for obstructive sleep apnea disorder: a multi-method approach. Iran J Med Sci. 2020;45:170-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Beckert L, Wiseman R, Pitama S, Landers A. What can we learn from patients to improve their non-invasive ventilation experience? ‘It was unpleasant; if I was offered it again, I would do what I was told’. BMJ Support Palliat Care. 2020;10:e7. doi: 10.1136/bmjspcare-2016-001151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. El-Solh AA, Ayyar L, Akinnusi M, Relia S, Akinnusi O. Positive airway pressure adherence in veterans with posttraumatic stress disorder. Sleep. 2010;33:1495-1500. doi: 10.1093/sleep/33.11.1495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sawunyavisuth B. What are predictors for a continuous positive airway pressure machine purchasing in obstructive sleep apnea patients? Asia Pac J Sci Technol. 2018;23:APST-23-03-10. [Google Scholar]
- 20. van den Broek N, Broer L, Vandenbussche N, Tan I, Overeem S, Pillen S. Obstructive sleep apnea in people with intellectual disabilities: adherence to and effect of CPAP. Sleep Breath. Published online October 21, 2020. doi: 10.1007/s11325-020-02221-y [DOI] [PubMed] [Google Scholar]
- 21. Dinh-Thi-Dieu H, Vo-Thi-Kim A, Tran-Van H, Duong-Quy S. Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study. Multidiscip Respir Med. 2020;15:468. doi: 10.4081/mrm.2020.468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hawkins SMM, Jensen EL, Simon SL, Friedman NR. Correlates of Pediatric CPAP Adherence. J Clin Sleep Med. 2016;12:879-884. doi: 10.5664/jcsm.5892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Simon SL, Duncan CL, Janicke DM, Wagner MH. Barriers to treatment of paediatric obstructive sleep apnoea: Development of the adherence barriers to continuous positive airway pressure (CPAP) questionnaire. Sleep Med. 2012;13:172-177. doi: 10.1016/j.sleep.2011.10.026 [DOI] [PubMed] [Google Scholar]
- 24. Saconi B, Yang H, Watach AJ, Sawyer AM. Coping Processes, self-efficacy, and CPAP use in adults with obstructive sleep apnea. Behav Sleep Med. 2020;18:68-80. doi: 10.1080/15402002.2018.1545651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736-747. doi: 10.1016/s0140-6736(13)60734-5 [DOI] [PMC free article] [PubMed] [Google Scholar]