Highlights
-
•
This study provides the prevalence estimates of physical activity, sedentary behavior, and sleep duration (isolation and combination) in a nationally representative sample (n = 114,072) of Chinese children and adolescents of grades 4–12.
-
•
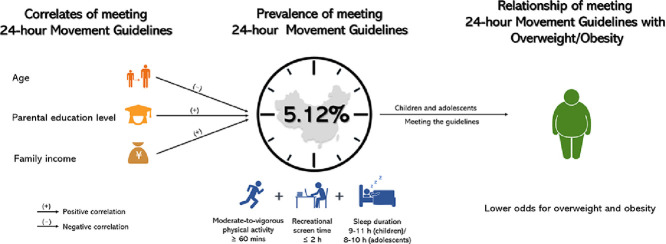
Only about 5% of Chinese children and adolescents show the most ideal combination of 24-h movement behaviors.
-
•
Chinese children and adolescents with younger ages, higher parental education levels, and higher family incomes exhibit favorable 24-h movement behaviors.
-
•
Chinese children and adolescents with the most ideal 24-h movement behaviors have lower risks of overweight and obesity, especially in children of grades 4–6 and girls of grades 7–9.
Keywords: Body weight, China Youth Study, Moderate-to-vigorous physical activity, School-aged children, Screen time, Sleep duration
Abstract
Background
Meeting 24-h movement guidelines by children and adolescents has been associated with improved indicators of health, although it has been under-studied in China. Hence, this study aimed to investigate the prevalence of meeting the 24-h movement guidelines, its correlates, and its relationships with body mass index in children and adolescents in China.
Methods
Cross-sectional data from the 2017 Youth Study in China of 114,072 children and adolescents (mean age = 13.75 years, 49.18% boys) were used. Meeting 24-h movement guidelines (≥60 min of daily moderate-to-vigorous physical activity, ≤2 h of daily leisure screen time, 9–11 h and 8–10 h nightly sleep duration for 6–13-year-olds and 14–17-year-olds, respectively) and height and weight of all participants were assessed. The prevalence of meeting the 24-h movement guidelines and World Health Organization weight status categories were determined. Generalized linear models were used to determine the correlates of meeting the 24-h movement guidelines and the relationships of meeting the 24-h movement guidelines with overweight (OW) and obesity (OB).
Results
Only 5.12% of Chinese children and adolescents met the 24-h movement guidelines, and 22.44% were classified as OW/OB. Older children and adolescents were less likely to meet the 24-h movement guidelines. Parental education level and family income were positively related to meeting the 24-h movement guidelines. Children and adolescents meeting the 24-h movement guidelines showed lower odds ratios for OW/OB. Compared with participants meeting the 24-h movement guidelines, boys in 4th–6th grades met none of the recommendations (OR = 1.22, 95%CI: 1.06–1.40), met the screen time recommendation only (OR = 1.13, 95%CI: 1.01–1.28), met the nightly sleep duration recommendation only (OR = 1.14, 95%CI: 1.03–1.28), and had significantly higher odds ratios for OW/OB. Similar trends were observed for girls in 4th–6th grades: meeting none of the guidelines (OR = 1.35, 95%CI: 1.14–1.59), meeting sleep duration guidelines only (OR = 1.23, 95%CI: 1.08–1.39), and meeting moderate-to-vigorous physical activity + nightly sleep duration guidelines (OR = 1.24, 95%CI: 1.01–1.54). For girls in 7th–9th grades, the following trend was observed: meeting none of the guidelines (OR = 1.30, 95%CI: 1.01–1.67).
Conclusion
Very few Chinese children and adolescents met the 24-h movement guidelines. Age (negatively correlated), parental education level, and family income (both positively correlated) were correlates of meeting the 24-h movement guidelines. Children and adolescents meeting the 24-h movement guidelines were more likely to have lower risks for OW/OB, especially in the youngest age group (Grades 4–6); and girls in the middle age group (Grades 7–9) were also more likely to have lower risks for OW/OB. Further research studies should explore additional correlates and determinants for meeting the 24-h movement guidelines. Also, future studies should use longitudinal or interventional designs to determine the relationships between meeting the 24-h movement guidelines and OW/OB and other health indicators, while taking sex and age differences into account.
Graphic Abstract
1. Background
Child and adolescent overweight (OW) and obesity (OB) have been a growing global health problem.1 Despite increasing concern and awareness, the prevalence of OW/OB in children and adolescents remains high.2 The Global Burden of Disease 2015 Obesity Collaborators found that 107.7 million children around the world were obese.3 In China, specifically, data from 2010 show that 8.1% of children aged 7–18 years were obese.4 From 1991 to 2011, the prevalence of Chinese children aged 6–18 years who were OW doubled.5 One study using nationally representative samples showed that the prevalence of OW/OB among Chinese school-aged children was approximately 30%.6 This public health concern has garnered the attention of Chinese policymakers.7
Studies have shown that sufficient moderate-to-vigorous physical activity (MVPA),8 limited screen time (ST),9 and appropriate sleep duration (SLP),10 collectively referred to as movement behaviors, are important and modifiable determinants of OW/OB in young people. For example, studies from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE)11 found that more MVPA, less ST, and adequate SLP were associated with reduced OB.12, 13, 14 Other studies have provided similar findings.15, 16, 17 One study found that the international prevalence of sufficient MVPA among youth was 44.1%.12 Based on a questionnaire survey, the prevalence of Chinese children and adolescents meeting MVPA guidelines was 34.1%.18 Adherence to ST guidelines among youth is also low, with only 8.1%19 of Canadian youth and 23.1% of UK youth meeting the recommendation.20 In Hong Kong, China, 38.6% of adolescents achieved the recommended SLP duration,21 which is similar to results from surveys in the USA12 and the mainland of China.12 Collectively, there is compelling evidence of poor adherence to individual movement-behavior guidelines.
Based on convincing evidence of the combined health benefits of meeting MVPA, ST, and SLP recommendations,22 the Canadian 24-Hour Movement Guidelines propose specific integrated recommendations for MVPA, ST, and SLP in children and adolescents,23 and these recommendations have been applied as the research paradigm.24 Time-use epidemiology provides a solid theoretical foundation for integrative health-behavior research.25 The theoretical foundation highlights the importance of combining MVPA, ST, and SLP because these 3 time-use compositions cover the 24-h period, and a balance among them is required for optimal health.26 Within the time-use framework, prevalence, correlates/determinants, and health outcomes are 3 essential components.25 Many researchers have applied the Canadian 24-Hour Movement Guidelines to conduct time-use epidemiological research among young people.27, 28, 29, 30, 31
To capture the prevalence of meeting the 24-h movement guidelines, 2 kinds of measures (i.e., accelerometers and self-reported questionnaires) have been used. Using accelerometers (ActiGraph GT3X+; ActiGraph LLC, Penscola, FL, USA) in free-living conditions, 1 international study reported that about 7% of children aged 9–11 years had sufficient MVPA, limited ST, and adequate SLP concurrently.12 A recent study of Chinese adolescents (Hong Kong, China) using activPAL (Glasgow, Scotland) accelerometers indicated that only 1% of adolescents met the 24-h movement guidelines.21 Investigations using self-reported questionnaires have also shown low levels of meeting guidelines for healthy 24-h movement behaviors. Two studies indicated that the prevalence of meeting the 24-h movement guidelines in Canadian children and adolescents ranged from 2.6%19 (using the Health Behavior School-aged Children Questionnaire) to 17.5%28 (using the Canadian Health Measures Survey). Lee et al.29 reported that only 3% of South Korean adolescents met the 24-h movement guidelines. This large variation in the prevalence of meeting the guidelines may be due to the use of different measures. Despite the higher accuracy of accelerometers in estimating 24-h movement behaviors, self-reported measures are an ideal measurement method for large-scale monitoring and surveillance owing to their lower testing burden and costs. To our knowledge, however, little is known about the prevalence of meeting the 24-h movement guidelines among young people in China.32
With regard to the correlates of meeting the 24-h movement guidelines, a limited number of studies have been conducted.30,31 Two studies suggested that parental support, residence, and outdoor time were the key correlates.30,31 However, such evidence pertaining to Asia is not available and is insufficient for fully understanding the pattern of movement behaviors in Chinese children and adolescents.32 Further studies are required in this field, especially studies that seek to identify sociodemographic correlates.20
Recent evidence has demonstrated that different combinations of MVPA, ST, and SLP (e.g., MVPA + ST, MVPA + SLP, or all of them) rather than 1 single behavior can lower the risks of OW/OB in children and adolescents.12,21,27,28 For example, Carson et al.27 found that the greater number of guidelines that children and adolescents meet, the lower the odds of their having a high body mass index (BMI) z-score, after controlling for age, sex, and level of parents’ education. Similar findings were also reported by Roman-Viñas et al.12 (who adjusted for sex, age, household education, and diet) and Laurson et al.33,34 (who adjusted for age, grade, and ethnicity). In sum, these studies, which all used objective measures to determine the BMI of participants, consistently showed that having sufficient MVPA, limited ST, and adequate SLP may be effective in preventing OW/OB. However, a study in Asia (Hong Kong, China) generated mixed results and showed that the combination of MVPA, ST, and SLP may not be associated with lower odds of OW/OB (adjusted for sex, age, and clustering school effects).21 These inconsistent findings point to the need for more evidence to clarify the relationships between movement behaviors and OW/OB, especially in Asia. The Behavioral Epidemiology Framework suggests that an essential element in determining whether behaviors should be targeted for intervention is determining the associations between the behaviors and health outcomes.35 However, the relationships reported in previous research have not been investigated in Chinese children and adolescents.32 Thus, studying the relationships as they pertain to Chinese children and adolescents can provide public health insights for OW/OB prevention in China.
Using the time-use epidemiology framework25 as a foundation, and to fill the gaps in the previous literature, the aims of this study were (1) to establish for the first time the prevalence of a national sample of Chinese children and adolescents meeting the 24-h movement guidelines (in insolation or in combination); (2) to determine, in relation to Chinese children and adolescents, the correlates of meeting the 24-h movement guidelines; and (3) to examine the relationships between meeting the 24-h movement guidelines and OW/OB in Chinese children and adolescents.
2. Methods
2.1. Study design and participants
This study used a sample from a nationwide survey drawn from the 2017 Physical Activity and Fitness in China—The Youth Study (PAFCTYS).36 The overall study design for PAFCTYS can be found elsewhere.37 In brief, PAFCTYS is a nationally representative surveillance survey that assessed the physical fitness and health level of children and adolescents in China, with administrative support of the Ministry of Education. Using a multistage sampling design, a balanced representation of geography, economic development, and rural-urban diversity was achieved. Public schools in 31 administrative regions in the mainland of China were recruited. The sampling procedure involved sampling administrative cities and districts, towns, and local community districts that represented a mix of rural and urban areas. The smallest sampling units were primary schools (Grades 4–6), junior middle schools (Grades 7–9), and junior high schools (Grades 10–12). The student sampling took place in classes selected randomly from each grade in the selected schools. The Ministry of Education selected 4 regions in each province or administrative region, of which 1 urban and 1 rural area in each region were identified. In each area (urban or rural), 4 schools (2 primary, 1 junior middle, and 1 junior high schools) were selected. At the school level, 2 classes from each grade in the primary schools, and 1 class from each grade in the junior middle and junior high schools were randomly selected. Using the above procedure, a sex-balanced sample size of more than 30 students for each grade in the primary schools was achieved, and a sample size of more than 60 students was achieved for the junior middle and junior high schools.
Grades 1–3 were not included in this study because of the students’ limited cognitive ability to take part in the study survey. In total, 131,992 targeted students were recruited into the 2017 PAFCTYS. A total of 131,859 students (response rate = 99.90%) completed the questionnaire survey and physical assessments. They were recruited from 490 primary schools, 251 junior middle schools, and 245 junior high schools, from a total of 31 provinces, 4 direct-controlled municipalities, and 6 regions.
The study protocol was approved by the Institutional Review Board of Shanghai University of Sport in 2017, and permission to conduct the study was obtained from the teachers and principals at the participating schools. All the children and adolescents participating in the study and their parents or guardians were informed that participation was voluntary. Verbal informed consent was obtained from all parents or guardians, and positive assent was obtained verbally from all the children before data collection. Data were collected and analyzed anonymously.
2.2. Procedures
All selected students were informed about the research project prior to participation. A research assistant registered each verbal consent/assent, which was put into a subject file with a numeric identification code and subsequently entered into a computer database accessed exclusively by authorized project staff. Data collection took place at school between October and December of 2017. This period was selected so that physical fitness and health examinations could be conducted with administrative support from the Ministry of Education in China. Participants received detailed directions on how to answer the survey. Following a standardized survey-administration protocol,37 trained research assistants conducted a survey of physical activity and assessment of body weight and height during regular school time. Students first had body weight and height assessments. Then they independently completed the survey questionnaire either online (68%) or on a paper version (32%) in a classroom setting.
2.3. Measures
2.3.1. Demographics and socioeconomic status
Demographic information about the children and adolescents was collected via a student self-reported questionnaire, including gender (boy or girl), grade (4, 5, … 12), ethnicity (Han or others), and residence location (urban or rural).
Socioeconomic status (SES) information, including parental educational level (both parents: less than college or university, college or university or higher; in our study, the former was defined as low education level, while the latter was defined as high education level) and family income per person annually (Chinese currency (RMB): <9000, 9000–30,000, 30,001–100,000, >100,000), was collected via a parent-reported questionnaire based on the method developed by Cirino et al.38 (reliability coefficient = 0.78, validity coefficient = 0.30).
2.3.2. Movement behaviors
PA was measured by the reliable and valid item derived from the Health Behavior in School-aged Children survey questionnaire (reliability coefficient = 0.82).39 The following item was used: How many days did you engage in MVPA at least 60 min on weekdays over the past week? (0 = none, 1 = 1 day, 2 = 2 days, 3 = 3 days, 4 = 4 days, 5 = 5 days, 6 = 6 days, and 7 = 7 days). So that students would have a better understanding of MVPA, it was explained as “any kind of physical activity increasing your heart rate and breathing frequencies during a period (including physical education, physical exercising, sports training, and various regular daily activities, such as brisk walking, hiking, and excursion)”. According to the Canadian 24-Hour Movement Guidelines,23 meeting the MVPA guideline requires that participants report 7 days with a minimum of 60 min of MVPA daily.
ST was also measured using reliable and valid items derived from the Health Behavior in School-aged Children.39 The following items were used: (1) How many hours did you spend watching TV or movies in your leisure time on weekdays and weekend days over the past week, respectively? (reliability coefficients: 0.74 and 0.72, respectively); (2) How many hours did you spend playing video games in your leisure time on weekdays and weekend days over the past week, respectively? (reliability coefficients: 0.54 and 0.69, respectively); and (3) How many hours did you spend in activities using electronic screen-based devices in leisure time on weekdays and weekend days over the past week, respectively? (reliability coefficients: 0.33 and 0.50, respectively); The responses to these questions could be: none, about 0.5 h, 1 h, 2 h, or 3 h or more. According to the Canadian 24-Hour Movement Guidelines,23 meeting the ST guideline requires daily ST ≤ 2 h per day.
SLP was measured by 1 item from the China Health and Nutrition Survey, which has accepted validation (reliability coefficient = 0.83).40 The item asked participants to report their usual nightly sleep duration (in hours) on a normal day. According to the Canadian 24-Hour Movement Guidelines,23 9–11 h are recommended for 6–13-year-olds and 8–10 h are recommended for 14–17-year-olds. Participants who reported the recommended nightly sleep duration were regarded as meeting the SLP guidelines. Based on the above definitions, the combined prevalence(s) were defined as meeting two or all three of the guidelines (e.g., the prevalence of meeting the MVPA, ST, and SLP guidelines).
2.3.3. Weight status
Weight status was determined by BMI, calculated as the participants’ weight–height ratio. These measurements were conducted by well-trained research staff who followed a standardized protocol.37 Weight was measured to the nearest 0.1 kg with a balance-beam scale while the participants were wearing lightweight clothing. Height was measured to the nearest 0.1 cm with a portable stadiometer while the participants were barefoot. Both measures were assessed using a portable instrument (GMCS-IV; Jianmin, Beijing, China). BMI values were calculated (BMI = Weight (kg)/Height (cm)2; kg/m2). According to sex- and age-specific cut-offs for OW and OB established by the World Health Organization,41 participants were dichotomized into non-OW/OB or OW/OB.
2.4. Statistical analysis
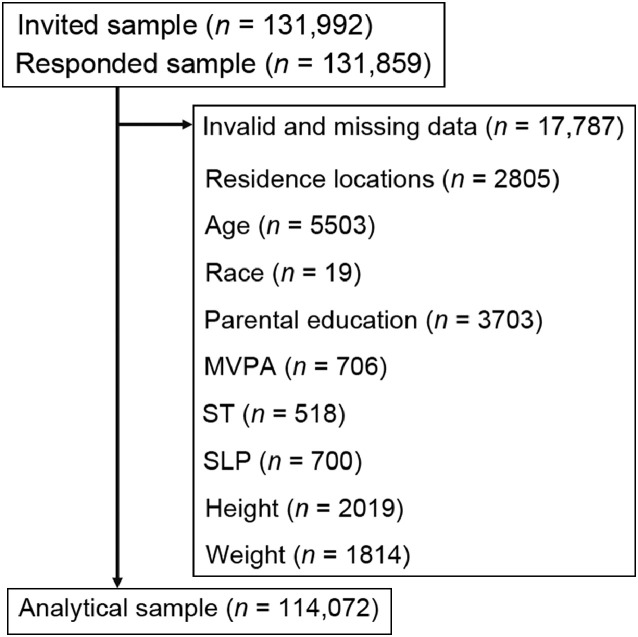
After cleaning invalid and abnormal values of all independent and dependent variables (Fig. 1), the final analytical sample size was 114,072. Descriptive analyses were performed to report the characteristics of the sample, the prevalence of meeting the recommendations (in isolation or in combination), and the prevalence of non-OW/OB and OW/OB. To produce nationally representative results, prevalence estimates (reported as percentages with 95% confidence interval (95%CI)) of the 2017 PAFCTYS sample were weighted according to the Chinese school-aged population of children in the current school education system (i.e., primary, junior middle, and junior high schools). Because of the non-normal distribution of age and BMI in our sample, Mann-Whitney tests were performed to examine sex differences by age and BMI. Generalized linear models were used to examine the associations between the prevalence of meeting the recommendations (in isolation or in combination) and weight status. Models set the study sites as fixed effects and the school as random effects. There was a sex × age group interaction between the prevalence of meeting the various combinations of the 24-h movement guidelines and weight status. Thus, the models were presented by total samples, and then by sex and age group. The level of statistical significance was set at p < 0.05. Cohen d was calculated as a measure of effect size. All statistical analyses were executed using SPSS (Version 24.0; IBM Corp., Corp. Armonk, NY, USA).
Fig. 1.
The procedure used for cleaning invalid and missing data in this study. MVPA = moderate-to-vigorous physical activity; SLP = sleep duration; ST = sedentary time.
3. Results
The descriptive characteristics of the samples in this study are shown in Table 1. The percentages for boys and girls were 49.18% and 50.82%, respectively. The mean age of the participants was 13.75 ± 2.61 years old (weighted: 13.16, 95%CI: 13.14–13.17), with statistical difference between sex groups (p < 0.001). The mean BMI was 19.93 ± 3.65 and was significantly different between sexes (p < 0.001, Cohen d = 0.06). The proportions of the sample across the 3 age groups were 34.83% (4th–6th graders; weighted: 42.85%, 95%CI: 42.55%–43.16%); 33.21% (7th–9th graders; weighted: 37.28%, 95%CI: 36.98%–37.57%); and 31.96% (10th–12th graders; weighted: 19.87%, 95%CI: 19.67%–20.07%), respectively. Most participants identified as Han ethnicity (86.37%; weighted: 86.19%, 95%CI: 85.98%–86.39%). There were no sex differences in age or ethnicity groups (both p > 0.05, both Cohen d = 0.01). The participants living in urban areas accounted for about 60% (weighted: 61.87%, 95%CI: 61.58%–62.16%) of the sample, and there was a sex difference in residence locations (p < 0.001, Cohen d = 0.02). The majority of participants’ parents had low education levels (81.38%, weighted: 80.92%, 95%CI: 80.68%–81.16%; no sex difference, p = 0.927, Cohen d = 0.01). More than 57% of families (weighted: 57.80%, 95%CI: 57.50%–58.09%) had 2 or more children (p for sex difference < 0.001, Cohen d = 0.18). Only about 7% (weighted = 7.27%, 95%CI: 7.12%–7.43%) of families had an income > 100,000 RMB per person (p for sex difference < 0.001, Cohen d = 0.06). More than 22% (weighted: 23.79%, 95%CI: 23.53%–24.05%) of participants were classified as OW/OB (p for sex difference < 0.001, Cohen d = 0.27).
Table 1.
Descriptive characteristics of the study sample (mean ± SD or n (%)).
| Overall (n = 114,072) |
Boys (n = 56,103; 49.18%) |
Girls (n = 57,969; 50.82%) |
p | d | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted | Weighted | 95%CI | Unweighted | Weighted | 95%CI | Unweighted | Weighted | 95%CI | |||
| Age (year) | 13.75 ± 2.61 | 13.16 | 13.14–13.17 | 13.80 ± 2.61 | 13.20 | 13.18–13.22 | 13.70 ± 2.60 | 13.11 | 13.09–13.13 | <0.001 | 0.02 |
| BMI (kg/m2) | 19.93 ± 3.65 | 19.65 | 19.62–19.67 | 20.23 ± 3.89 | 19.95 | 19.92–19.98 | 19.65 ± 3.38 | 19.35 | 19.32–19.38 | <0.001 | 0.06 |
| Age groups | |||||||||||
| 4th–6th graders | 39,736 (34.83) | 42.85 | 42.55–43.16 | 19,556 (34.86) | 42.92 | 42.49–43.35 | 20,180 (34.81) | 42.79 | 42.36–43.21 | 0.237 | 0.01 |
| 7th–9th graders | 37,881 (33.21) | 37.28 | 36.98–37.57 | 18,509 (32.99) | 37.07 | 36.65–37.49 | 19,372 (33.42) | 37.48 | 37.07–37.89 | ||
| 10th–12th graders | 36,455 (31.96) | 19.87 | 19.67–20.07 | 18,038 (32.15) | 20.01 | 19.73–20.29 | 18,417 (31.77) | 19.74 | 19.46–20.01 | ||
| Ethnicity | |||||||||||
| Han | 98,523 (86.37) | 86.19 | 85.98–86.39 | 48,560 (86.56) | 86.36 | 86.06–86.65 | 49,963 (86.19) | 86.02 | 85.72–86.31 | 0.073 | 0.01 |
| Others | 15,549 (13.63) | 13.81 | 13.61–14.02 | 7543 (13.44) | 13.64 | 13.35–13.94 | 8006 (13.81) | 13.98 | 13.69–14.28 | ||
| Residence locations | |||||||||||
| Urban | 69,102 (60.58) | 61.87 | 61.58–62.16 | 34,307 (61.15) | 62.22 | 61.80–62.63 | 34,795 (60.02) | 61.53 | 61.12–61.94 | <0.001 | 0.02 |
| Rural | 44,970 (39.42) | 38.13 | 37.84–38.42 | 21,796 (38.85) | 37.78 | 37.37–38.20 | 23,174 (39.98) | 38.47 | 38.06–38.88 | ||
| Parental educationa | |||||||||||
| Low education level | 92,833 (81.38) | 80.92 | 80.68–81.16 | 45,651 (81.37) | 81.03 | 80.69–81.37 | 47,182 (81.39) | 80.82 | 80.48–81.15 | 0.927 | 0.01 |
| High education level | 21,239 (18.62) | 19.08 | 18.84–19.32 | 10,452 (18.63) | 18.97 | 18.63–19.31 | 10,787 (18.61) | 19.18 | 18.85–19.52 | ||
| Family composition | |||||||||||
| Single child | 48,763 (42.75) | 42.20 | 41.91–42.50 | 26,533 (47.29) | 46.42 | 45.99–46.85 | 22,230 (38.35) | 38.13 | 37.72–38.53 | <0.001 | 0.18 |
| Two or more children | 65,309 (57.25) | 57.80 | 57.50–58.09 | 29,570 (52.71) | 53.58 | 53.15–54.01 | 35,739 (61.65) | 61.87 | 61.47–62.28 | ||
| Family income/person (RMB/year) | |||||||||||
| <9000 | 36,733 (32.20) | 31.76 | 31.48–32.04 | 17,253 (30.75) | 30.49 | 30.10–30.88 | 19,480 (33.60) | 32.98 | 32.59–33.38 | <0.001 | 0.06 |
| 9001–30,000 | 41,048 (35.99) | 36.00 | 35.71–36.29 | 20,262 (36.12) | 36.06 | 35.65–36.47 | 20,786 (35.86) | 35.94 | 35.54–36.35 | ||
| 30,001–100,000 | 28,302 (24.81) | 24.97 | 24.72–25.24 | 14,494 (25.83) | 25.89 | 25.52–26.27 | 13,808 (23.82) | 24.09 | 23.73–24.45 | ||
| >100,000 | 7989 (7.00) | 7.27 | 7.12–7.43 | 4094 (7.30) | 7.56 | 7.34–7.80 | 3895 (6.72) | 6.99 | 6.78–7.21 | ||
| Weight status | |||||||||||
| Non-OW/OB | 88,471 (77.56) | 76.21 | 75.95–76.47 | 40,379 (71.97) | 70.28 | 69.88–70.67 | 48,092 (82.96) | 81.94 | 81.61–82.27 | <0.001 | 0.27 |
| OW/OB | 25,601 (22.44) | 23.79 | 23.53–24.05 | 15,724 (28.03) | 29.72 | 29.33–30.12 | 9877 (17.04) | 18.06 | 17.73–18.39 | ||
Notes: The weighted prevalence uses PAFCTYS sampling weights to be representative of the Chinese grade school population in 2017 (unweighted sample size = 114,072; weighted sample size = 102,739,979). d denotes effect size. a High education level was defined as both parents’ educational levels being equal to or higher than college and university.
Abbreviations: 95%CI = 95% confidence interval; BMI = body mass index; MVPA = moderate-to-vigorous physical activity; OB = obesity; OW = overweight; PAFCTYS = Physical Activity and Fitness in China—The Youth Study; SLP = sleep duration; ST = screen time.
Table 2 presents the prevalence of participants meeting various combinations of the 24-h movement guidelines. The percentage meeting the 24-h movement guidelines was 5.12% (weighted: 6.04%, 95%CI: 5.89%–6.19%) (no sex difference, Cohen d = 0.01). The prevalence of meeting the MVPA, ST, and SLP guidelines was 11.80% (weighted: 12.89%, 95%CI: 12.68%–13.10%), 65.26% (weighted: 64.75%, 95%CI: 64.46%–65.03%) and 44.40% (weighted: 50.74%, 95%CI: 50.44%–51.04%), respectively. More boys reported meeting the MVPA and SLP guidelines than did girls (p < 0.001, Cohen d = 0.09 and 0.06, respectively). The prevalence of meeting some combination of the 24-h movement guidelines (e.g., MVPA + ST, MVPA + SLP, and ST + SLP) varied greatly, from 7.10% (weighted: 8.35%, 95%CI: 8.18%–8.53%) to 28.49% (weighted: 32.71%, 95%CI: 32.42%–33.00%). Boys had significantly higher prevalence of the combination of the MVPA + ST guidelines and MVPA + SLP guidelines than did girls (p < 0.001, Cohen d = 0.03 and 0.05, respectively).
Table 2.
Prevalence of meeting different combinations of 24-h movement behavior guidelines by gender n (%).
| Meeting different recommendation(s) | Overall (n = 114,072) |
Boys (n = 56,106; 49.18%) |
Girls (n = 57,969; 50.82%) |
p | d | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted | Weighted | 95%CI | Unweighted | Weighted | 95%CI | Unweighted | Weighted | 95%CI | |||
| MVPA | 13,462 (11.80) | 12.89 | 12.68–13.10 | 7422 (13.23) | 14.26 | 13.96–14.57 | 6040 (10.42) | 11.56 | 11.29–11.84 | <0.001 | 0.09 |
| ST | 74,439 (65.26) | 64.75 | 64.46–65.03 | 35,117 (62.59) | 61.86 | 61.44–62.27 | 39,322 (67.83) | 67.54 | 67.14–67.93 | <0.001 | 0.11 |
| SLP | 50,649 (44.40) | 50.74 | 50.44–51.04 | 25,756 (45.91) | 52.10 | 51.67–52.52 | 24,893 (42.94) | 49.42 | 49.00–49.84 | <0.001 | 0.06 |
| MVPA+ST | 9627 (8.44) | 9.21 | 9.03–9.39 | 4972 (8.86) | 9.52 | 9.27–9.78 | 4655 (8.03) | 8.90 | 8.66–9.15 | <0.001 | 0.03 |
| MVPA+SLP | 8098 (7.10) | 8.35 | 8.18–8.53 | 4349 (7.75) | 9.04 | 8.79–9.30 | 3749 (6.47) | 7.68 | 7.45–7.92 | <0.001 | 0.05 |
| ST+SLP | 32,501 (28.49) | 32.71 | 32.42–33.00 | 15,649 (27.89) | 31.70 | 31.29–32.11 | 16,852 (29.07) | 33.68 | 33.27–34.09 | <0.001 | 0.03 |
| All | 5837 (5.12) | 6.04 | 5.89–6.19 | 2920 (5.20) | 6.08 | 5.87–6.30 | 2917 (5.03) | 5.99 | 5.78–6.20 | 0.188 | 0.01 |
Notes: The weighted prevalence use PAFCTYS sampling weights to be representative of the Chinese grade school population in 2017 (unweighted sample size = 114,072; weighted sample size = 102,739,979). d denotes effect size.
Abbreviations: 95%CI = 95% confidence interval; MVPA = moderate-to-vigorous physical activity; PAFCTYS = Physical Activity and Fitness in China—The Youth Study; SLP = sleep duration; ST = screen time.
The associations between demographics and the prevalence of meeting the 24-h movement guidelines are presented in Table 3. The odds ratios for meeting the 24-h movement guidelines among 4th–6th graders (odds ratio (OR) = 15.70, 95%CI: 13.89–17.74) and 7th–9th graders (OR = 4.10, 95%CI: 3.59–4.67) were significantly higher when compared to 10th–12th graders. Boys living in urban locations were more likely (OR = 1.11, 95%CI: 1.02–1.21) to meet the 24-h movement guidelines compared with either boys or girls living in rural locations. Participants whose parents had high education levels were 1.23 times more likely to meet the 24-h movement guidelines compared to participants whose parents had low education levels. These statistically significant trends were observed for both sexes (OR for boys = 1.25, 95%CI: 1.13–1.37; OR for girls = 1.23, 95%CI: 1.11–1.35). Participants in the higher family-income groups were more likely to meet the 24-h movement guidelines than participants in the lowest family-income group. A consistent gradient related to family income was observed among girls; however, only boys from families with the second highest (30,001–100,000) and the highest (> 100,000) family income categories were significantly more likely to meet the 24-h movement guidelines (OR for the second highest = 1.12, 95%CI: 1.00–1.25; OR for the highest = 1.46, 95%CI: 1.26–1.68). Ethnicity and family composition were not significantly correlated with the prevalence of meeting the 24-h movement guidelines.
Table 3.
The associations between meeting the 24-h movement guidelines and sociodemographic correlates.
| Overall |
Boys |
Girls |
||||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Age groups | ||||||
| 4th–6th graders | 15.70 | 13.89–17.74 | 11.31 | 9.71–13.17 | 24.21 | 19.69–29.77 |
| 7th–9th graders | 4.10 | 3.59–4.67 | 3.54 | 3.00–4.17 | 5.21 | 4.18–6.50 |
| 10th–12th graders | 1 | 1 | 1 | |||
| Ethnicity | ||||||
| Han | 1.08 | 1.00–1.18 | 1.09 | 0.97–1.23 | 1.08 | 0.96–1.21 |
| Others | 1 | 1 | 1 | |||
| Residence locations | ||||||
| Urban | 1.06 | 1.00–1.13 | 1.11 | 1.02–1.21 | 1.01 | 0.93–1.10 |
| Rural | 1 | 1 | 1 | |||
| Parental educationa | ||||||
| Low education level | 1 | 1 | 1 | |||
| High education level | 1.23 | 1.15–1.32 | 1.25 | 1.13–1.37 | 1.23 | 1.11–1.35 |
| Family composition | ||||||
| Single child | 1.06 | 1.00–1.12 | 1.04 | 0.96–1.13 | 1.07 | 0.99–1.16 |
| Two or more children | 1 | 1 | 1 | |||
| Family income/person (RMB/year) | ||||||
| <9000 | 1 | 1 | 1 | |||
| 9001–30,000 | 1.12 | 1.04–1.20 | 1.08 | 0.98–1.19 | 1.16 | 1.05–1.28 |
| 30,001–100,000 | 1.22 | 1.13–1.32 | 1.12 | 1.00–1.25 | 1.33 | 1.20–1.49 |
| >100,000 | 1.41 | 1.27–1.57 | 1.46 | 1.26–1.68 | 1.35 | 1.16–1.58 |
Note: Reference category (respectively): age group 10th–12th graders; minority; rural; low education; 2 or more children; and < 9000 family income (RMB per year). a High education level was defined as both parents' educational levels being equal to or higher than college and university. Abbreviations: 95%CI = 95% confidence interval; OR = odds ratio.
Table 4 shows the associations between meeting different 24-h movement guidelines with OW/OB among the participants. After controlling for all the covariates (e.g., sex, grade, and parental education level), meeting none or fewer of the guidelines showed higher ORs for OW/OB when compared with the group meeting the MVPA+ST+SLP guidelines. However, only meeting none (OR = 1.25, 95%CI: 1.16–1.34), ST (OR = 1.20, 95%CI: 1.12–1.28), SLP (OR = 1.15, 95%CI: 1.07–1.23), and MVPA+SLP (OR = 1.12, 95%CI: 1.01–1.25) guidelines exhibited higher statistically significant odds for OW/OB compared with those meeting the MVPA+ST+SLP guidelines (all p < 0.05).
Table 4.
ORs for overweight and obesity associated with meeting different 24-h movement guidelines.
| OR | 95%CI | |
|---|---|---|
| None | 1.25 | 1.16–1.34 |
| MVPA | 1.14 | 0.99–1.29 |
| ST | 1.20 | 1.12–1.28 |
| SLP | 1.15 | 1.07–1.23 |
| MVPA+ST | 1.02 | 0.92–1.13 |
| MVPA+SLP | 1.12 | 1.01–1.25 |
| ST+SLP | 1.04 | 0.97–1.11 |
| MVPA+ST+SLP | 1 |
Notes: All models were adjusted for sex, grade, parental education level, ethnicity, residence location, family composition, and family income. Reference group: MVPA+ST+SLP.
Abbreviations: 95%CI = 95% confidence interval; MVPA = moderate-to-vigorous physical activity; OR = odds ratio; SLP = sleep duration; ST = screen time.
The summarized results for the OR for OW/OB participants meeting the different 24-h movement guidelines by sex and grade levels are shown in Table 5. A general pattern emerged, with lower odds of OW/OB participants’ meeting more 24-h movement guidelines, though most were not significant. The relationships appeared to be stronger in younger children and girls than in adolescents and boys.
Table 5.
ORs for overweight and obesity associated with meeting different 24-h movement guidelines by sex and grade levels.
| Grades 4–6 |
Grades 7–9 |
Grades 10–12 |
||||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Boys | ||||||
| None | 1.22 | 1.06–1.40 | 1.10 | 0.91–1.33 | 1.19 | 0.80–1.75 |
| MVPA | 1.23 | 0.94–1.61 | 0.91 | 0.68–1.21 | 1.08 | 0.68–1.74 |
| ST | 1.13 | 1.01–1.28 | 1.06 | 0.88–1.28 | 1.21 | 0.82–1.78 |
| SLP | 1.14 | 1.03–1.28 | 0.96 | 0.79–1.16 | 1.10 | 0.72–1.67 |
| MVPA+ST | 0.97 | 0.78–1.21 | 0.87 | 0.68–1.10 | 1.06 | 0.70–1.62 |
| MVPA+SLP | 1.14 | 0.97–1.34 | 0.84 | 0.62–1.13 | 0.59 | 0.27–1.26 |
| ST+SLP | 1.06 | 0.96–1.17 | 0.96 | 0.79–1.16 | 0.98 | 0.65–1.47 |
| MVPA+ST+SLP | 1 | 1 | 1 | |||
| Girls | ||||||
| None | 1.35 | 1.14–1.59 | 1.30 | 1.01–1.67 | 2.36 | 0.95–5.85 |
| MVPA | 1.24 | 0.85–1.81 | 1.32 | 0.88–1.97 | 1.68 | 0.58–4.82 |
| ST | 1.13 | 0.98–1.30 | 1.16 | 0.90–1.48 | 2.33 | 0.94–5.75 |
| SLP | 1.23 | 1.08–1.39 | 1.17 | 0.90–1.52 | 2.14 | 0.84–5.45 |
| MVPA+ST | 1.02 | 0.80–1.31 | 1.00 | 0.73–1.37 | 2.04 | 0.80–5.20 |
| MVPA+SLP | 1.24 | 1.01–1.54 | 1.32 | 0.85–2.04 | 1.98 | 0.44–8.81 |
| ST+SLP | 1.01 | 0.90–1.13 | 1.14 | 0.88–1.47 | 1.78 | 0.71–4.49 |
| MVPA+ST+SLP | 1 | 1 | 1 | |||
Notes: All models were adjusted for parental education level, ethnicity, residence location, family composition, and family income. Reference group: MVPA+ST+SLP.
Abbreviations: 95%CI = 95% confidence interval; MVPA = moderate-to-vigorous physical activity; OR = odds ratio; SLP = sleep duration; ST = screen time.
4. Discussion
Using nationally representative data, this study aimed to investigate the prevalence among Chinese children and adolescents of meeting the 24-h movement guidelines, determine the sociodemographic correlates of the prevalence, and explore the relationships between meeting the integrated guidelines and OW/OB. We found that the prevalence of meeting the integrated guidelines was low, which was associated with age, parental education level, and family income. Meeting the 24-h movement guidelines was related to a lower OR of being OW/OB for boys in the 4th through 6th grades and girls in the 7th through 9th grades but not for the other age or sex groups (though a similar pattern was observed).
Gaining a thorough understanding of prevalence of meeting the 24-h movement guidelines is beneficial in promoting movement behavior in young people.32 The current study demonstrated that 5.12% (weighted: 6.04%) of Chinese children and adolescents met the 24-h movement guidelines. This is the first study to investigate the prevalence of meeting the 24-h movement guidelines in a nationally representative sample of Chinese children and adolescents. The prevalence found in this study is consistent with level of prevalence found among youth in the USA (5%).42 Although the level of prevalence of meeting the 24-h movement guidelines in our study was higher than that among children and adolescents in Hong Kong, China (1%),21 South Korea (3.2%);43 and Canada (<3%),19 it is lower than the prevalence found in other previously published studies using international12 and national samples.20,42 These variations may be attributed to differences in measurements. For example, some studies used accelerometers to estimate the prevalence,12,21,30 while others used self-reported questionnaires.19,29 Considering the cumulative health benefits of meeting the 24-h movement guidelines,12,22,27 our study can provide insightful information for developing programs that will improve movement behaviors in a young Chinese population.
The low prevalence in our study of meeting the 24-h movement guidelines was due mainly to the low prevalence in meeting the PA guidelines (which was lowest compared to meeting the ST and SLP guidelines by themselves). This finding is supported by studies conducted in Hong Kong, China,21 and internationally.12 The low prevalence of meeting the PA guidelines by Chinese children and adolescents is also consistent with previous national surveys.18,37 It is also important to recognize that the main driver of low prevalence in meeting the 24-h movement guidelines varies. For UK youth, the low prevalence of meeting the ST guidelines is a primary contributor.20 Thus, studying the time-use patterns and their distribution for children and adolescents12 and identifying the main driver of low prevalence is a necessity in movement-behavior and time-use research.25 Our study has identified a lower PA level as possibly being a main driver for the lower prevalence of meeting the 24-h movement guidelines and, thus, offers some practical implications for promoting movement behaviors among Chinese children and adolescents.
Understanding the correlates of meeting the 24-h movement guidelines is of vital importance for designing effective public health initiatives and targeting populations with health risks.25,32 Some recently published studies have examined the correlates of meeting the 24-h movement guidelines in children and adolescents.30,31 In our study, age, parental education level, and family income were key correlates of meeting the 24-h movement guidelines. Increasing age was negatively associated with the prevalence of meeting the guidelines. Compelling evidence has shown that there are age-related declines in MVPA,18,37 increases in ST,6,18 and lower SLP duration44,45 in children and adolescents. To secure improved education, the increased academic pressure that comes with increasing age often results in more time spent studying,46 which perhaps displaces PA opportunities and SLP. Furthermore, older Chinese children and adolescents typically have mobile smart devices, which increases the probability of sedentary screen-based behaviors.46 These 2 factors may have contributed to our findings that very few Chinese children and adolescents met the 24-h movement guidelines. Parental education level and family income can be considered strong indicators of SES and have been shown to be significantly correlated with children's and adolescents’ MVPA,47,48 ST,49,50 and SLP.44,51 The underlying mechanism may be that parents in higher SES categories have better awareness of their children's health behaviors and help them pursue healthy lifestyles. They may also be able to provide better financial support, which helps to facilitate healthful PA and sport opportunities. However, family SES is hard to modify. Therefore, reinforcing the importance of equitable access to interventions for children and adolescents from different SES levels is necessary.51 Although our study provides some preliminary evidence for understanding time use in a 24-h timeframe by Chinese children and adolescents, additional studies that explore the association between 24-h movement behaviors and multidimensional factors are encouraged.32
It has been suggested that it is inappropriate to examine the relationship between a single behavior (e.g., MVPA, ST, or SLP) and health.32 Therefore, if researchers use 24-h movement guidelines, they can better examine the relationship between integrated behaviors within a 24-h cycle and health outcomes, and the implications of their findings for promoting young people's health will be increased.23,24,32 The relationships between meeting the 24-h movement guidelines and OW and OB have been reported in previous studies.12,21,27,33,34 A systematic review by Saunders and colleagues22 indicated that the combination of sufficient MVPA, limited ST, and adequate SLP may result in lower odds of being OW/OB. Our study supports their findings, which are also supported by other empirical evidence.12,33,34 We found that MVPA may not be an effective predictor of OW and OB, which is inconsistent with other studies that suggest that MVPA is a strong predictor of these conditions.34 Possible reasons for this inconsistency may lie in the fact that different measures of PA were used. However, our finding that those not meeting the 24-h movement guidelines had the highest OR for OW/OB compared with those who met the guidelines is consistent with the findings of Roman-Viñas et al.12 and Laurson et al.33 Our finding reinforces the importance of combining MVPA, ST, and SLP in the prevention of OW/OB in Chinese children and adolescents rather than promoting a single behavior (MVPA, ST, or SLP) in isolation. Our study supports the time-use epidemiological framework,25 in which combinations of sufficient MVPA, limited ST, and appropriate SLP lead to improved health conditions in young people. Because our study design does not establish a true cause-and-effect relationship, future studies should address this research issue.
In our study, the relationship between meeting the 24-h movement guidelines and OW/OB varied by age and sex. This finding is in line with previous research.52 Sex and age differences in biological growth are responsible for different trajectories of weight status among young people.1 In our study, we found that among children and adolescents in Grades 7–12, there generally was no significant relationship between meeting the 24-h movement guidelines and OW/OB, irrespective of sex, a finding that is not supported by previous studies. Some potential explanations for this inconsistency are useful. First, measurement errors caused by the use of self-reported questionnaires may result in inaccurate measures of movement behaviors, which may skew the link between movement behaviors and OW/OB. Second, evidence has been presented that questions the independent link between ST and SLP and OW/OB in a young population.53,54 This implies that ST and SLP may not be determinants of OW/OB. Yet another explanation may be diet. It has been found that childhood and adolescent OW/OB is related to nutrition and diet, especially in developing countries (e.g., China).55 Diet can cause excessive energy intake, thus contributing to OW/OB. Therefore, it is possible that despite meeting the 24-h movement guidelines, children and adolescents who have unhealthful diets can be at increased risk for OW/OB. These findings may be useful in informing sex- and age-tailored weight interventions.
The strengths of our study include the following. First, we used a large survey sample, which could lead to a wider generalization of the findings for China. Second, our study was the first to examine the association between movement behaviors and weight status in Chinese children and adolescents and, thus, can inform the design of effective interventions, prevention strategies, and policies. Third, we included additional sociodemographic factors related to meeting the 24-h movement guidelines, which could help researchers to better understand the patterns of movement behaviors. Some limitations, however, should also be mentioned. First, the cross-sectional design of this study precludes conclusions regarding causality between behaviors and weight status. Second, a self-reported questionnaire was used to collect data; therefore, measurement errors could have occurred. Third, our study considered only a few confounders influencing children's and adolescents’ weight status; some other significant cofounders (e.g., diet and nutrition)12 were not included.
5. Conclusion and clinical implications
The prevalence of meeting the 24-h movement guidelines among Chinese children and adolescents was relatively low. Unhealthful lifestyles were associated with increasing age, lower parental education level, and lower family income. Meeting the 24-h movement guidelines was related to lower ORs for OW/OB. This relationship was obvious among boys in Grades 4–6 and among girls in Grades 7–9. Future studies should use improved study designs (e.g., longitudinal designs) to determine the correlates/determinants of meeting the 24-h movement guidelines among Chinese children and adolescents. To better understand the relationship between meeting the 24-h movement guidelines and OW/OB, interventional studies should control for more confounders (e.g., diet and nutrition) while considering sex and age differences.
From a clinical perspective, our study suggests that promoting positive 24-h movement behaviors is needed urgently among Chinese children and adolescents because positive behaviors may, in turn, improve their future health outcomes. Older children and adolescents, especially those with lower parental education levels and lower family incomes, should be targeted as a priority. To address the health issue of OW/OB among children and adolescents, increasing MVPA, limiting screen time and improving sleep duration concurrently may be an effective approach, with sex- and age-specific strategies being encouraged.
Acknowledgments
Acknowledgments
We thank the students, parents, and staff for participating in the data collection and data entry. The study design and data collection were supported by the Key Project of the National Social Science Foundation of China (No. 16ZDA227). The first and corresponding authors (STC and YL) are supported by grants from the National Social Science Foundation of China (No. 19BTY077), the Philosophy and Social Science Foundation of Shanghai (No. A1904), and the Shanghai Key Laboratory of Human Performance (Shanghai University of Sport, No. 11DZ2261100).
Authors’ contributions
STC, YL, JTH, YT, and PC conceptualized, designed this study, analyzed the data, interpreted the data, and drafted the manuscript; MST provided intellectual guidance in improving the manuscript; ZBC, JZ, ZZ, XW, LW, and YC assisted in revising the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jshs.2020.07.002.
Appendix. Supplementary materials
References
- 1.Lobstein T, Jackson-Leach R, Moodie ML. Child and adolescent obesity: part of a bigger picture. The Lancet. 2015;385:2510–2520. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The GBD 2015 Obesity Collaborators Health effects of overweight and obesity in 195 countries over 25 years. New Engl J Med. 2017;377:13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun H, Ma Y, Han D, Pan CW, Xu Y. Prevalence and trends in obesity among China's children and adolescents, 1985–2010. PloS One. 2014;9 doi: 10.1371/journal.pone.0105469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon Larsen P, Wang H, Popkin BM. Overweight dynamics in Chinese children and adults. Obes Rev. 2014;15(Suppl. 1):S37–S48. doi: 10.1111/obr.12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai Y, Zhu X, Wu X. Overweight, obesity, and screen-time viewing among Chinese school-aged children: National prevalence estimates from the 2016 Physical Activity and Fitness in China—The Youth Study. J Sport Health Sci. 2017;6:404–409. doi: 10.1016/j.jshs.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li F, Chen P. Addressing the public health concerns of physical inactivity, low levels of fitness, and unhealthy weight among Chinese school-aged children. J Sport Health Sci. 2017;6:379–380. doi: 10.1016/j.jshs.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poitras VJ, Gray CE, Borghese MM. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S197–S239. doi: 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- 9.van Ekris E, Altenburg TM, Singh AS, Proper KI, Heymans MW, Chinapaw MJM. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: A systematic review and meta-analysis. Obes Rev. 2016;17:833–849. doi: 10.1111/obr.12426. [DOI] [PubMed] [Google Scholar]
- 10.Chaput JP, Gray CE, Poitras VJ. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S266–S282. doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- 11.Katzmarzyk PT, Barreira TV, Broyles ST. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): Design and methods. BMC Pub Health. 2013;13:900. doi: 10.1186/1471-2458-13-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roman-Viñas B, Chaput JP, Katzmarzyk PT. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. doi: 10.1186/s12966-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katzmarzyk PT, Barreira TV, Broyles ST. Relationship between lifestyle behaviors and obesity in children ages 9–11: Results from a 12-country study. Obesity. 2015;23:1696–1702. doi: 10.1002/oby.21152. [DOI] [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Barreira TV, Broyles ST. Physical activity, sedentary time, and obesity in an international sample of children. Med Sci Sports Exerc. 2015;47:2062–2069. doi: 10.1249/MSS.0000000000000649. [DOI] [PubMed] [Google Scholar]
- 15.Ekelund U, Luan J, Sherar LB. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307:704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques A, Minderico C, Martins S, Palmeira A, Ekelund U, Sardinha LB. Cross-sectional and prospective associations between moderate to vigorous physical activity and sedentary time with adiposity in children. Int J Obesity (Lond) 2015;40:28–33. doi: 10.1038/ijo.2015.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarzfischer P, Weber M, Gruszfeld D. BMI and recommended levels of physical activity in school children. BMC Pub Health. 2017;17:595. doi: 10.1186/s12889-017-4492-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu Z, Tang Y, Zhuang J. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: An update from the 2017 Physical Activity and Fitness in China—The Youth Study. BMC Pub Health. 2019;19:197. doi: 10.1186/s12889-019-6515-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janssen I, Roberts KC, Thompson W. Adherence to the 24-hour movement guidelines among 10- to 17-year-old Canadians. Health Promot Chronic Dis Can. 2017;37:369–375. doi: 10.24095/hpcdp.37.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pearson N, Sherar LB, Hamer M. Prevalence and correlates of meeting sleep, screen-time, and physical activity guidelines among adolescents in the United Kingdom. JAMA Pediatr. 2019;173:1–2. doi: 10.1001/jamapediatrics.2019.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi Y, Huang WY, Sit CH, Wong SH. Compliance with 24-hour movement guidelines in adolescents (Hong Kong, China): Associations with weight status. J Phys Act Health. 2020;17:287–292. doi: 10.1123/jpah.2019-0230. [DOI] [PubMed] [Google Scholar]
- 22.Saunders TJ, Gray CE, Poitras VJ. Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S283–S293. doi: 10.1139/apnm-2015-0626. [DOI] [PubMed] [Google Scholar]
- 23.Tremblay MS, Carson V, Chaput JP. Canadian 24-Hour Movement Guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S311–S327. doi: 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- 24.Willumsen J, Bull F. Development of WHO guidelines on physical activity, sedentary behavior, and sleep for children less than 5 years of age. J Phys Act Health. 2020;17:96–100. doi: 10.1123/jpah.2019-0457. [DOI] [PubMed] [Google Scholar]
- 25.Pedisic Z, Dumuid D, Olds T. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology. 2017;49:252–269. [Google Scholar]
- 26.Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24-hour period for overall health. Int J Environ Res Pub Health. 2014;11:12575–12581. doi: 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carson V, Chaput JP, Janssen I, Tremblay MS. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev Med. 2017;95:7–13. doi: 10.1016/j.ypmed.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Roberts KC, Yao X, Carson V, Chaput JP, Janssen I, Tremblay MS. Meeting the Canadian 24-Hour Movement Guidelines for children and youth. Health Rep. 2017;28:3–7. [PubMed] [Google Scholar]
- 29.Lee EY, Carson V, Jeon JY, Spence JC, Tremblay MS. Levels and correlates of 24-hour movement behaviors among South Koreans: Results from the Korea National Health and Nutrition Examination Surveys, 2014 and 2015. J Sport Health Sci. 2019;8:376–385. doi: 10.1016/j.jshs.2018.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manyanga T, Barnes JD, Chaput JP, Katzmarzyk PT, Prista A, Tremblay MS. Prevalence and correlates of adherence to movement guidelines among urban and rural children in Mozambique: A cross-sectional study. Int J Behav Nutr Phys Act. 2019;16:94. doi: 10.1186/s12966-019-0861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rhodes RE, Spence JC, Berry T. Parental support of the Canadian 24-hour movement guidelines for children and youth: Prevalence and correlates. BMC Pub Health. 2019;19:1385. doi: 10.1186/s12889-019-7744-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rollo S, Antsygina O, Tremblay M. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9:493–510. doi: 10.1016/j.jshs.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laurson KR, Lee JA, Eisenmann JC. The cumulative impact of physical activity, sleep duration, and television time on adolescent obesity: 2011 Youth Risk Behavior Survey. J Phys Act Health. 2015;12:355–360. doi: 10.1123/jpah.2013-0402. [DOI] [PubMed] [Google Scholar]
- 34.Laurson KR, Lee JA, Gentile DA, Walsh DA, Eisenmann JC. Concurrent associations between physical activity, screen time, and sleep duration with childhood obesity. ISRN Obes. 2014;2014 doi: 10.1155/2014/204540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sallis JF, Owen N, Fotheringham MJ. Behavioral epidemiology: A systematic framework to classify phases of research on health promotion and disease prevention. Ann Behav Med. 2000;22:294–298. doi: 10.1007/BF02895665. [DOI] [PubMed] [Google Scholar]
- 36.Chen P. Physical activity, physical fitness, and body mass index in the Chinese child and adolescent populations: An update from the 2016 Physical Activity and Fitness in China–The Youth Study. J Sport Health Sci. 2017;6:381–383. doi: 10.1016/j.jshs.2017.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fan X, Cao ZB. Physical activity among Chinese school-aged children: National prevalence estimates from the 2016 Physical Activity and Fitness in China–The Youth Study. J Sport Health Sci. 2017;6:388–394. doi: 10.1016/j.jshs.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cirino PT, Chin CE, Sevcik RA, Wolf M, Lovett M, Morris RD. Measuring socioeconomic status: Reliability and preliminary validity for different approaches. Assessment. 2002;9:145–155. doi: 10.1177/10791102009002005. [DOI] [PubMed] [Google Scholar]
- 39.Liu Y, Wang M, Tynjälä J. Test–retest reliability of selected items of Health Behaviour in School-aged Children (HBSC) survey questionnaire in Beijing, China. BMC Med Res Methodol. 2010;10:73. doi: 10.1186/1471-2288-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 41.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knell G, Durand CP, Kohl HW, 3rd, Wu IHC, Gabriel KP. Prevalence and likelihood of meeting sleep, physical activity, and screen-time guidelines among US youth. JAMA Pediatr. 2019;173:387–389. doi: 10.1001/jamapediatrics.2018.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee EY, Spence JC, Tremblay MS, Carson V. Meeting 24-hour movement guidelines for children and youth and associations with psychological well-being among South Korean adolescents. Ment Health Phys Act. 2018;14:66–73. [Google Scholar]
- 44.Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Med Rev. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 45.Belmon LS, van Stralen MM, Busch V, Harmsen IA, Chinapaw MJM. What are the determinants of children's sleep behavior? A systematic review of longitudinal studies. Sleep Med Rev. 2019;43:60–70. doi: 10.1016/j.smrv.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 46.Chen ST, Liu Y, Hong JT. Co-existence of physical activity and sedentary behavior among children and adolescents in Shanghai, China: Do gender and age matter. BMC Pub Health. 2018;18:1287. doi: 10.1186/s12889-018-6167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu C, Stolk RP, Sauer PJJ. Factors of physical activity among Chinese children and adolescents: A systematic review. Int J Behav Nutr Phys Act. 2017;14:36. doi: 10.1186/s12966-017-0486-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yao CA, Rhodes RE. Parental correlates in child and adolescent physical activity: A meta-analysis. Int J Behav Nutr Phys Act. 2015;12:10. doi: 10.1186/s12966-015-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stierlin AS, De Lepeleere S, Cardon G. A systematic review of determinants of sedentary behaviour in youth: A DEDIPAC-study. Int J Behav Nutr Phys Act. 2015;12:133. doi: 10.1186/s12966-015-0291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mielke GI, Brown WJ, Nunes BP, Silva ICM, Hallal PC. Socioeconomic correlates of sedentary behavior in adolescents: Systematic review and meta-analysis. Sports Med. 2017;47:61–75. doi: 10.1007/s40279-016-0555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elgar FJ, Pförtner TK, Moor I, De Clercq B, Stevens GW, Currie C. Socioeconomic inequalities in adolescent health 2002–2010: A time-series analysis of 34 countries participating in the Health Behaviour in School-aged Children study. The Lancet. 2015;385:2088–2095. doi: 10.1016/S0140-6736(14)61460-4. [DOI] [PubMed] [Google Scholar]
- 52.Gao Z. Growth trajectories of young children's objectively determined physical activity, sedentary behavior, and body mass index. Child Obes. 2018;14:259–264. doi: 10.1089/chi.2018.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Biddle SJH, Bengoechea EG, Wiesner G. Sedentary behaviour and adiposity in youth: A systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act. 2017;14:43. doi: 10.1186/s12966-017-0497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chaput JP, Dutil C. Lack of sleep as a contributor to obesity in adolescents: Impacts on eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:103. doi: 10.1186/s12966-016-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dong F, Howard AG, Herring AH. Parent-child associations for changes in diet, screen time, and physical activity across two decades in modernizing China: China Health and Nutrition Survey 1991–2009. Int J Behav Nutr Phys Act. 2016;13:118. doi: 10.1186/s12966-016-0445-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.