Abstract
Background and aims
To propose an integrative model for post-COVID symptoms by considering the absence/presence of previous symptomatology.
Methods
We searched different databases for original articles and reviews on post-COVID symptoms.
Results
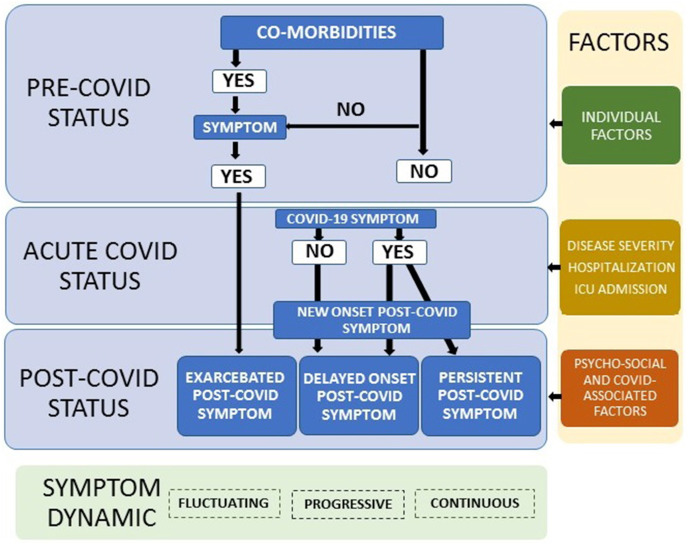
The first consideration is to define which symptoms are of “new-onset” (symptoms never experienced by a patient before COVID-19 and experienced the first time after) and which symptoms are “exacerbated” (symptoms experienced by a patient prior to COVID-19 but aggravated later) after infection. The second consideration includes defining “persistent” (symptoms experienced at the acute phase and continuing after without remission period) and “delayed-onset” (symptoms not experienced at the acute phase of the infection but appearing after a “latency period”). This model integrates predisposing individual factors, biological factors associated to the severity of disease, hospitalization/treatment factors, and outbreak surrounding factors which may promote post-COVID.
Conclusion
Since current literature on post-COVID is heterogeneous, this integrative model could help to a better characterization of long-COVID.
Keywords: COVID-19, Long COVID, Persistent, Symptoms, Classification, Definition
The presence of sequelae after coronavirus disease 2019 (COVID-19) has provoked a unexpected second pandemic, the “long-haulers” i.e., individuals suffering from post-COVID symptoms (long-COVID) [1]. The term long-COVID is probably the first medical disease term firstly promoted by the patients themselves [2]. In fact, the term long-COVID is now recognized by the World Health Organization (WHO) as a worldwide health care problem and an “emergency-use” ICD code has been assigned (U09.9 Post-COVID) [3]. Long-COVID is a term generally used for describing individuals who had recovered from COVID-19, but they continue exhibiting associated-symptoms after the acute phase, once the infection has been theoretically ceased [4]. No consensus in post-COVID terminology exists [5]. Some authors have discussed the topic if these symptoms should be associated or not with a positive diagnosis [6,7] and also potential timeframes [8,9] for considering the term “post-acute” or “long-COVID”. Nevertheless, a discussion about the different scenarios in relation to the development of post-COVID symptoms is scarce.
It seems that 80% of COVID-19 survivors could exhibit post-COVID symptoms after surpassing the acute phase of the infection [10]. A recent meta-analysis, published as a preprint, has reported that fatigue, headache, and attention disorders are the top three post-COVID symptoms [11]. However, the heterogeneity in the presentation of these symptoms supports the priority of better phenotyping and defining post-COVID [12].
Therefore, this paper aims to propose an integrative model by considering different classifications, based on the absence or presence of previous symptomatology and the presence or absence of a remission/delayed period.
1. New-onset or exacerbated post-COVID symptoms?
The first consideration is based on the previous presence/experience of a symptom. Therefore, the first step is to identify if a particular post-COVID symptom experienced by a COVID-19 survivor is new. We define “new-onset post-COVID” as a new symptom never experienced by a patient before COVID-19 but appearing after the acute infection. For instance, a patient who has never experienced fatigue (or dyspnoea) before suffering COVID-19 who starts with these symptoms after surpassing the infection. By definition, a new-onset post-COVID symptom appears in subjects without previous comorbidities or with comorbidities not sharing common symptoms with COVID-19 such as diabetes or hypertension. As example, it has been found that almost half of % COVID-19 patients experiencing post-COVID headache did not exhibit previous history of headache before the infection [13]. New-onset post-COVID could also appear in individuals with pre-existing comorbidities. In such a scenario, a patient with pre-existing history of migraine before infection could experience anosmia after COVID-19 (symptom not related to the previous migraine). We define “exacerbated post-COVID” as a symptom experienced by a patient before COVID-19 which is aggravated after the infection. For instance, an individual with migraine before COVID-19 who experience a worsening of migraine symptoms after the infection [14]. An exacerbated post-COVID symptom can only appear in individuals with previous experience of a particular symptom, e.g., previous medical comorbidity sharing common symptoms with COVID-19.
Overall, post-COVID symptoms are mainly attributed to biological consequences, such as persistent viral replication or long-lasting pro-inflammatory response (cytokine storm) associated with SARS-CoV-2 infection. These biological responses may influence the immune system affecting multiple organ systems and promoting the development of post-COVID symptoms [15]. Additionally, those surrounding factors associated to COVID-19 outbreak (e.g., social alarm, familiar situation, lockdown, unemployment, fear) could also promote psychological disorders (such as anxiety, depression or posttraumatic stress) and enhance post-COVID symptomatology.
2. Persistent or delayed-onset post-COVID symptoms?
The second consideration is the moment when the symptom appears in relation to the acute phase of infection. We define “persistent post-COVID” as a symptom experienced by a patient at the acute phase of the infection (e.g., headache, myalgia) which does not disappear at any time after (post-COVID). It would be a patient experiencing headache as symptom during the acute COVID-19 phase and that persists after COVID-19 without interruption, e.g., fulfilling pattern of new-daily persistent headache. We define “delayed-onset post-COVID” as a symptom not experienced by a patient at the acute COVID-19 phase but appearing after a latency period (post-COVID). For instance, a patient who has not experienced e.g., headache as a symptom at the acute phase of infection but it appears several days or weeks after resolution of the infection, e.g., fulfilling pattern of migraine-like headache.
Increasing evidence supports that COVID-19 onset symptoms may influence the development of post-COVID symptomatology. For example, the presence of multiple symptoms such as cough, shortness of breath, headache, diarrhea, and hoarseness of voice at COVID-19 onset has been associated with a higher risk of long-COVID symptoms in non-hospitalized patients [16]. Our research group observed that the presence of myalgia at the acute phase of infection was associated with a higher prevalence of musculoskeletal long-term post-COVID pain in hospitalized survivors [17]. Current results suggest that early monitoring of onset/acute symptoms of SARS-CoV-2 infection could help identify people at a higher risk of developing future post-COVID symptoms.
3. Proposed integrative model for post-COVID symptoms
Based on these considerations, we would like to propose a model for post-COVID symptoms (Fig. 1 ). This integrative model could be applied to the plethora of symptoms that can exhibit long-haulers, e.g., fatigue, dyspnoea, abdominal pain, concentration loss, headaches or musculoskeletal pain. An important factor to consider in the proposed model is the relapsing/remitting nature of post-COVID symptomatology, since long-haulers can exhibit wide fluctuations in their symptoms [18]. Therefore, the proposed integrative model should be considered as a dynamic process. Further, this model also integrate individual factors (age, gender, genetics, medical comorbidities), biological factors associated to the severity of COVID-19 (immune responses, inflammatory biomarkers), hospitalisation and treatment factors (days at hospital, Intensive Care Unit admission or not, prolonged bedding, adverse events derived from treatment, ventilator related barotrauma) and social or contextual factors surrounding COVID-19 outbreak (isolation, psychological distress, modulation of information by social media, lockdown, catastrophizing thoughts, etc.).
Fig. 1.
Proposed Integrative Model for Post-COVID Symptoms. The model determines three steps: pre-COVID status; acute-COVID status and post-COVID status. It also integrates the presence of individual factors, biological COVID-associated factors, hospitalization factors and COVID-19 outbreak surrounding factors.
In conclusion, this paper proposes an integrative model for defining post-COVID by considering the previous presence of a particular symptom and/or the moment when the symptom appears in relation to the infection, to better characterized its phenotype.
Declaration of competing interest
No conflict of interest is declared by the authors.
References
- 1.Marshall M. The lasting misery of coronavirus long-haulers. Nature. 2020;585:339–341. doi: 10.1038/d41586-020-02598-6. [DOI] [PubMed] [Google Scholar]
- 2.Callard F., Perego E. How and why patients made Long Covid. Soc Sci Med. 2021;268:113426. doi: 10.1016/j.socscimed.2020.113426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Emergency use ICD codes for COVID-19 disease outbreak. Available at: https://www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak.
- 4.Nabavi N. Long COVID: how to define it and how to manage it. BMJ. 2020;370:m3489. doi: 10.1136/bmj.m3489. [DOI] [PubMed] [Google Scholar]
- 5.Baig A.M. Chronic COVID syndrome: need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol. 2020 doi: 10.1002/jmv.26624. Oct 23. [DOI] [PubMed] [Google Scholar]
- 6.Raveendran A.V. Long COVID-19: challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab Syndr. 2020;15:145–146. doi: 10.1016/j.dsx.2020.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raveendran A.V., Jayadevanc R., Sashidharand S. Long COVID: an overview. Diabetes Metab Syndr. 2021 doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernández-de-las-Peñas C., Palacios-Ceña D., Gómez-Mayordomo V., Cuadrado M.L., Florencio L.L. Defining post-COVID symptoms (Post-acute COVID, long COVID, persistent Post-COVID): an integrative classification. Int J Environ Res Publ Health. 2021;18:2621. doi: 10.3390/ijerph18052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Datta S.D., Talwar A., Lee J.T. A Proposed framework and timeline of the spectrum of disease due to SARS-CoV-2 infection: illness beyond acute infection and public health implications. JAMA. 2020;324:2251–2252. doi: 10.1001/jama.2020.22717. [DOI] [PubMed] [Google Scholar]
- 10.Nalbandian A., Sehgal K., Gupta A., Madhavan M.V., McGroder C., Stevens J.S., et al. Post-acute COVID-19 syndrome. Nat Med. 2021 doi: 10.1038/s41591-021-01283-z. Mar 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P.A., Cuapio A., et al. More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis. medRxiv. 2021 doi: 10.1038/s41598-021-95565-8. Jan 1;2021.01.27.21250617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carson G. Long Covid Forum Group. Research priorities for Long COVID: refined through an international multi-stakeholder forum. BMC Med. 2021;19:84. doi: 10.1186/s12916-021-01947-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caronna E., Ballvé A., Llauradó A., et al. Headache: a striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia. 2020;40:1410–1421. doi: 10.1177/0333102420965157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uygun Ö., Ertaş M., Ekizoğlu E., Bolay H., Özge A., Kocasoy Orhan E., Çağatay A.A., Baykan B. Headache characteristics in COVID-19 pandemic-a survey study. J Headache Pain. 2020;21:12. doi: 10.1186/s10194-020-01188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afrin L.B., Weinstock L.B., Molderings G.J. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int J Infect Dis. 2020;100:327–332. doi: 10.1016/j.ijid.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang Y., Pinto M.D., Borelli J.L., Mehrabadi M.A., Abrihim H., Dutt N., et al. COVID symptoms, symptom clusters, and predictors for becoming a long-hauler: looking for clarity in the haze of the pandemic. medRxiv. 2021 doi: 10.1177/10547738221125632. Mar 5:2021.03.03.21252086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fernández-de-las-Peñas C., Rodríguez-Jiménez J., Fuensalida-Novo S., Palacios-Ceña M., Gómez-Mayordomo V., Florencio L.L., et al. Myalgia as a symptom at hospital admission by Sars-Cov-2 infection is associated to persistent musculoskeletal pain as long-term post-covid sequelae: a case-control study. Pain. 2021 Apr 8 doi: 10.1097/j.pain.0000000000002306. (in press) [DOI] [PubMed] [Google Scholar]
- 18.Long Mahase E. COVID could be four different syndromes, review suggests. BMJ. 2020;371:m3981. doi: 10.1136/bmj.m3981. [DOI] [PubMed] [Google Scholar]