Abstract
COVID-19 is a unique disaster, which has placed extreme stress on Healthcare Workers (HCWs) and the systems in which they work. Eradicating the pandemic requires sustainment of the healthcare workforce through actions that mitigate stress, promote resilience, and enhance performance. A major barrier is the lack of organizational practices and procedures designed to sustain HCWs during prolonged crisis events, such as COVID-19. Adapting existing best practices from other high-risk occupations allows for a more rapid, efficient response to optimize workforce well-being and preserve healthcare organizational functioning. This paper discusses current and emerging literature on the unique impacts of COVID-19 on HCWs and provides actionable, evidence-informed recommendations for individuals, teams, and leaders to enhance sustainment of HCWs that is critical to the preservation of national and global health security.
Keywords: COVID-19, healthcare worker, intervention, mental health, resilience
Learning Objectives
Summarize the unique aspects of the COVID-19 pandemic and the extreme stresses it has placed on healthcare workers (HCWs).
Discuss the importance of sustaining HCWs through the pandemic by actions to reduce stress, promote resilience, and enhance performance.
Identify existing best practices from other high-risk occupations to optimize HCWs’ well-being and preserve the functioning of healthcare organizations.
Human-generated and natural disaster events are increasing in frequency and severity,1,2 causing extreme disruption, injury, suffering, and death. Pandemics, such as COVID-19, have origins in nature but are propagated by human systems and behavior. They result in adverse mental health effects that are similar to many other disaster events, but also unique responses including altered risk perception, stigma and blaming, fear of resource shortages, and prolonged uncertainty that broadly impact a society.3 Adverse psychological and behavioral effects begin early during a disaster and can last for months or years,4–6 resulting in chronic occupational dysfunction7 for those involved in disaster response and recovery. In addition to the myriad stressors affecting all of society, Healthcare Workers (HCWs) have experienced unique occupational challenges related to the pandemic. COVID-19 has had a broad impact on a wide range of healthcare personnel and managing the pandemic requires a “whole of healthcare” approach. For these reasons, it is important to think of HCWs as inclusive of those delivering care as well as logistics, cleaning, food services, maintenance, administrative staff, and other personnel supporting the operations of health systems.
Sustainment of HCWs is critical to ensure public health and safety during surges of infection, illness, and death, a need that will continue well after the epidemiological curves begin to flatten. Identifying HCWs at risk for a range of adverse mental health outcomes, including the unique aspects of risk brought by COVID-19, allows for more efficient and targeted occupational interventions. Throughout COVID-19 and other disasters, the most effective way to optimize functioning is with interventions that enhance the five “essential elements”, including: sense of safety, calming, social connectedness, self- and community-efficacy, and hope in the future.8 Literature on previous disasters offers a partial roadmap for integration of these “essential elements” to mitigate risk and enhance sustainment in HCWs. However, the scope, magnitude, and duration of this event necessitate that we borrow best practices from other high-risk professions that work with limited resources for prolonged periods of time under extremes of stress. Instituting interventions to enhance sustainment, which targets those at highest risk, is critical to optimize sustainment of function and enhance the trajectory of recovery for HCWs.
UNIQUE ASPECTS OF COVID-19
COVID-19 differs from other disasters by the very nature of the threat, as well as its scope, magnitude, and duration. The unprecedented level of ongoing uncertainty has made it difficult to plan, challenging our ability to maintain a sense of hope in the future. Most HCWs are experienced in dealing with various medical aspects of natural and climate-related disasters, such as injuries from tornado debris, infections associated with floodwaters, and gunshot wounds. But, COVID-19 is different. HCWs are dealing with a novel virus that has been hard to predict, caused significant illness and sequelae for many, resulted in a relatively high mortality rate, and presented a significant risk of contagion to themselves and their families. Further, there is no cure, a limited understanding of treatment, and a vaccine that has just recently become available under emergency use authorization.
Though risk mitigation is essential during COVID-19, risk cannot be eliminated. When the threat is a highly contagious respiratory virus, there is nowhere safety can be guaranteed. HCWs and the rest of society may start to perceive loved ones, friends, and colleagues—those we traditionally turn to for comfort, connection, and companionship—as threats. These supportive resources may also be less accessible due to either required or voluntary physical distancing or quarantine after an exposure. Facing an ever-present, invisible threat, and exposed to the challenges to values and way of life that all are facing (see Fig. 1), HCWs have unique risks. This population has, and will continue to experience, significant stressors during the COVID-19 pandemic.9
FIGURE 1.
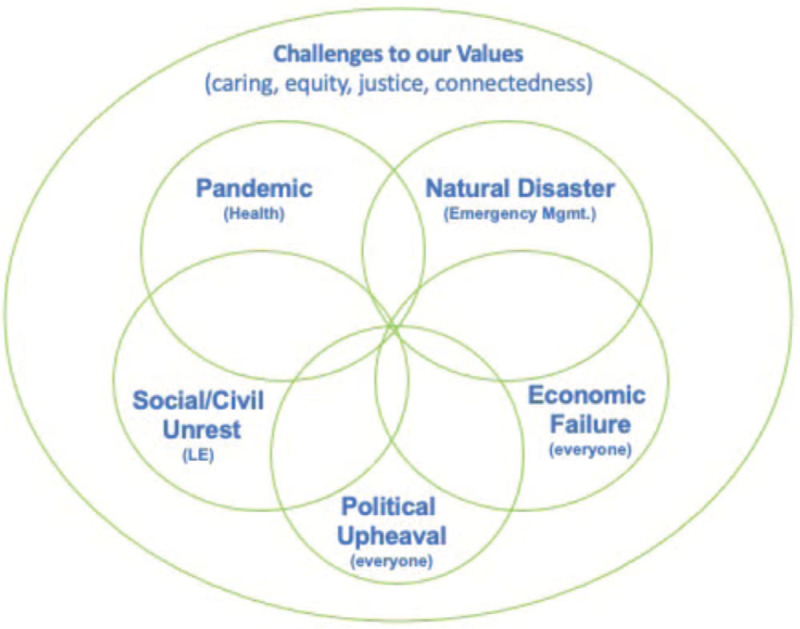
When disasters collide.
Most disasters have a clear beginning, response, and recovery phases. During “blue sky” periods between disaster events, the focus is typically on mitigation and preparedness efforts. Many hazards, such as climate-related and natural disasters, have a geographic distribution allowing for more effective preparedness and response planning. COVID-19 is a national and global disaster, unprecedented in scope and distribution, impacting virtually all aspects of society and the economy. It continues without a clear end in sight and organizations and communities are all involved in various aspects of responding, recovering, and mitigating for future waves of the pandemic while, in many cases, simultaneously planning for and responding to other disaster events, such as hurricanes, wildfires, and floods.10–12
During most disasters, society turns to reassuring helpers, such as HCWs. They provide visual and emotional reassurance that help is on the way, care and support are near, and things will eventually be “okay”. HCWs remove people from hazardous environments, provide assistance, facilitate healing, and return people to normal life. When those helpers fall ill during COVID-19, or become psychologically compromised, it challenges society's confidence in that support and recovery process and compounds the fear people experience. Many HCWs have encountered members of society who are resistant or hostile to the help and recommendations they are providing, pulling at the fault lines within communities and furthering stress among these personnel.13 Some HCWs have colleagues who question the significance of the pandemic and its impact on healthcare and society, as well as diminish the importance of protective measures needed to control the pandemic, further amplifying distress and divisions.
HCWs, as well as the organizations in which they work, are inextricably linked to the functioning of other parts of the health system, such as public health; other parts of community systems such as education, faith, and social services; government at all levels; and political structures and influences. These linkages create a profound interdependence, whereby the well-being of HCWs becomes critical to the sustainment of myriad systems throughout our society.
PSYCHOLOGICAL AND BEHAVIORAL RESPONSES TO DISASTERS
Historically, exposure to extremes of stress and trauma during pandemics and other disasters manifest predominantly as distress reactions and health risk behaviors with some people developing psychiatric disorders (Fig. 2). Distress reactions and risky health behaviors typically emerge early on, whereas psychiatric disorders take weeks, months, or longer to manifest.3,14,15
FIGURE 2.

Psychological and behavioral responses to pandemics and disasters.
Most people exposed to the pandemic, including those who have difficulties along the way, will ultimately find ways to manage. Some will even experience an increased perception of their ability to manage future stressors, often termed “posttraumatic growth.” However, COVID-19 has led to a sizable portion of the population experiencing distress reactions and engaging in risky health behaviors. It is likely that some will ultimately develop psychiatric disorders.9,16
THE MENTAL HEALTH EFFECTS OF COVID-19 ON HCWS
The psychological and behavioral effects of disasters, including pandemics, are far-reaching and long-lasting.3,6,17,18 Though research continues to emerge, there is evidence of profound mental health effects of COVID-19 on HCWs, at all levels of training and experience,19 which threatens our healthcare response and the ability to ultimately control the pandemic.20 Personnel are experiencing a range of responses, including distress, insomnia, acute stress, depression, and posttraumatic stress.21–23 While successive “waves” have come with improved access to protective equipment and enhanced knowledge in the treatment of COVID patients, other challenges have emerged. HCWs are tired and remain concerned about their safety and that of their families. HCWs are working in systems functioning under altered standards of care with rationing of scarce resources exacerbating moral distress.24,25 Bed capacity, access to critical respiratory equipment, and lack of adequate personnel staff remain commonplace, particularly in hotspot areas.
As with many disasters, early in the pandemic, instrumental (practical) concerns represented the most significant challenge for HCWs.26 Challenges with child-care and requirements to transition to virtual schooling severely disrupted family routines. Even for those whose job could be done remotely, their children had become their new officemates with interruptions and elevated emotions taxing families, particularly those with children who were younger or had additional special needs. In some families, spouses lost jobs, creating abrupt and profound economic hardship, a significant predictor of adverse outcomes following disasters.14 Simply paying the bills and feeding their family became an uncertainty, perhaps for the first time ever.
Many healthcare providers—particularly at the beginning of the pandemic—chose to physically distance themselves from their loved ones to reduce risk. Some were stigmatized by friends and family, due to perceptions of risk associated with their professions. Fear and stigma are common during pandemics and exacerbate feelings of social isolation and worsened mental health outcomes for HCWs during COVID-19.13 Many hospital administrative staff were told to work remotely early on. While this helped safeguard physical health, not having the casual and candid conversations that naturally occur in an in-person workplace made it harder to determine if a colleague is having a difficult time psychologically. Even in the workplace, it is hard to “read” a teammate's face or body language when much of it is covered by protective equipment. Very fine cues to emotional state are based upon facial expression and are not visible when covered by protective equipment. This results in missed cues that can alert others when people are having difficulties. Because social connections are protective, especially in crisis events, the loss of these cues and connections can be particularly problematic by eliminating early warning opportunities and diminishing a sense of togetherness.
The inability to fully experience grief (“disenfranchised grief”) during COVID-19 remains a significant challenge for society, including HCWs, particularly during surge periods.27 While death is a reality in the medical field, most HCWs have an expectation about the frequency and volume of death to which they will be exposed. COVID-19 changed that for many, as patients came in extremely ill and rapidly deteriorated. Some workers were exposed to mass death and human remains, bringing risk for psychological identification. This occurs when an individual viewing remains thinks “that could be me” or “that could be my child”, which increases risk for adverse mental health outcomes.28 Visitation restrictions and other protocols often resulted in a single HCW being the only other person in the room with a patient as they took their last breath. Perhaps they were holding a phone or tablet as the patient's loved ones shared the experience virtually. Being present for patients in this way and supporting family who cannot be with them in expressions of grief during a patient's final moments is an extraordinary act of caring. At the same time, providing this intense level of support can exact a significant toll on HCWs.
Many HCWs are also extremely fatigued. Long hours, threats to safety for themselves and family, constant resource limitations, shifting policies, and procedures and, in some cases, leadership challenges, have served to physically and emotionally exhaust caregivers and other personnel. It is important to acknowledge that sustaining behavior change, such as mask-wearing, physical distancing, virtual school, and the myriad other life modifications that have been required during the pandemic, is very taxing to individuals, families, and communities. Leadership communication and media coverage that promotes the notion of sound and prosocial pandemic behaviors as oppressive and a hindrance to individual rights has served to foster resistance among community members, exacerbate spread of illness, and compound work and personal difficulties for HCWs.
UNDERSTANDING RISK IN HCWS DURING COVID-19
Stressors are like a toxin, such as lead or radon. Understanding risk requires knowledge of which personnel are exposed to stress, how much, when, the impact, and what factors buffered against potential adverse effects. All HCWs are at risk for adverse impacts given the convergence of these factors. No one is immune. It is important to be cautious about assuming a certain person or group is at higher risk (eg, “frontline” personnel) when those not on the frontline of disasters can experience unique risks associated with increased work demands, diminished meaning in the work they are doing, decreased esteem from those around them, and guilt for not being on the “frontlines.”
Resilience for any given individual is not static or innate but the byproduct of an evolving network of stressors and factors buffering against them. As highlighted in Table 1, risk and resilience are factors that manifest during all stages of disaster events and amplify or buffer against stress. Certain factors are present starting in the pre-disaster time period, some emerge as the result of disaster event characteristics, and others result from aspects of the recovery period.
TABLE 1.
Risk and Resilience in HCWs During COVID-19
| Definition | Risk Examples | Resilience Examples | |
| Pre-event period | Considerations related to status factors (health, occupational, psychosocial, educational, trauma history, etc), support systems | -Active and uncontrolled health problems, mental health, substance use-Requirement to access system of care to self/family healthcare-Limited/poor coping skills unresolved trauma-No/few social supports, isolation-Financial difficulties-Lack of training-Poor unit cohesion-Resistance to help-seeking | -Pre-event positive health status-Availability and use of appropriate health resources-Limited exposure to adverse environmental health factors-History of positive adaptation to stress or stress resistance-Hopeful outlook-Creative coping skills/strategies-Screening and identification of health risk status-Monitoring of changed risk factors-Identifying mission critical roles for those unable to serve as front line workers (eliminate stigma)-Adequate training and preparation (including psychosocial anticipatory guidance) |
| Event/impact period | Considerations of what occurs during the most active/acute phase of events, exposure, immediate/early reactions and nature of exposure, stressors, supports, occupational and home and community environments | -Requirement to use crisis (altered) standards of care-Inadequate PPE-Moral distress/injury-High exposure to infection and other health risks-Exposure to death, dying, and human remains (increased risk for “psychological identification”)-Required work outside specialty training-Weakened/destroyed community fabric-Punitive or unsupportive work environment-Toxic leadership-Lack of empathy-Poor communication regarding policies and procedures-Death of loved ones or close contacts; bereavement | -Short duration, minimal disruption to work/personal life-Community fabric intact-Adequate PPE-Exposure risks and sacrifices shared equitably-Clear communication about evolving infection control and personnel safety policies & procedures-Supportive & accessible leaders-Help-seeking org culture-Appropriate and flexible expectation-Regular monitoring of health and BH status through multiple means-Early identification and intervention with health and BH issues-Close monitoring of health status of workers recovered from COVID-19-Provide range of supports, interventions, and referral options-Monitor impact of organizational status and change on wellbeing of all personnel |
| Recovery period | Considerations of the nature of longer-term impacts/experiences, status and changes in work environment, psychosocial status, family/community status | -Illness stigma from neighbors/family/friends-Disjointed community response further prolonging response efforts and uncertainty-Isolation from social support systems-Inability to grieve (“disenfranchised grief”)-Job loss (self or significant other)-Extended virtual/home school requirements-Lack of access to child-care-Fatigue; inability to reset or recover-Diminished health-Vaccination concerns and barriers | -Strong, intact, expanded social support in the workplace and in personal life following the crisis-Provide range of supports and interventions-Provide options and opportunities for personnel interactions-Promote family friendly personnel policies and strategies-Adapt to changing patterns of needs, demands-Work culture continues to encourage interventions and support-Rest and reset options provided and encouraged-Health issues addressed-Leadership remains engaged and communicating regularly with personnel |
ASSESSING RISK IN HCWS… WHO? WHAT? WHEN?
It is critical to ensure accountability and responsibility, especially in high stress and high demand situations that sometimes evolve into environments where traditional lines become blurred or changed. Occupational functioning is the responsibility of individuals, team members, and leaders. During a public health emergency, it may make sense to apply the military public mental health approach within the framework of Combat and Operational Stress. Figure 3 depicts the four phases of the stress continuum, including “Ready”, “Reacting”, “Injured”, and “Ill”.29,30
FIGURE 3.
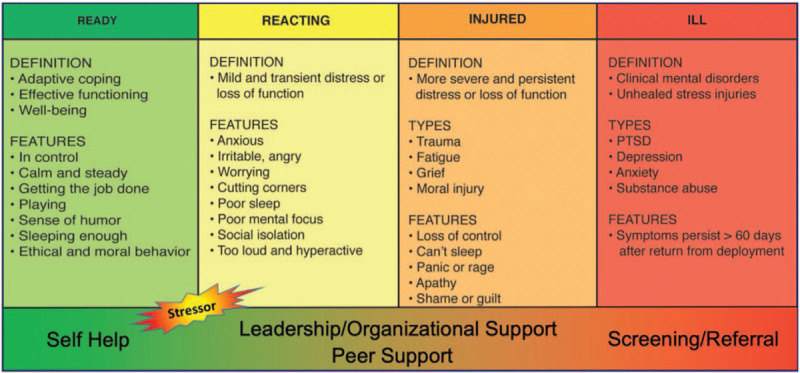
Combat and operational stress continuum.
This model recognizes several mental health factors critical to organizational sustainment during a crisis event:
-
(1)
Much of what HCWs experience occurs along a continuum of expectable responses and does not always need to be medicalized.
-
(2)
HCWs and the communities in which they live and work heavily influence well-being and will serve as the primary means of support and sustainment.
-
(3)
Focus should be less on diagnosing and treating illness in HCWs, and more on identifying reactions, determining where along the continuum they are, and implementing interventions to move individuals and teams back toward a state of wellness, while strengthening the ability to adapt to the crisis.
Assessment is an ongoing process carried out by individuals (ie, self-assessment, etc), peers (ie, buddy system, team huddles, etc), supervisors (ie; walkarounds, surveys, After Action Reviews, etc). As a result, having regular contact with personnel is important to alert supervisors and leaders when changes occur. It is these changes that warrant further assessment as they may signal developing problems. Because the vast majority of HCWs will not seek formal healthcare interventions for stress and trauma exposure, coworkers can also play a significant role in identifying and supporting peer HCWs that are experiencing negative mental health effects associated with the pandemic.
Measuring stress and resilience can be done using formal and informal processes. In addition to clinical measures of mental health symptoms, leaders can assess human performance factors (eg, team cohesion, presenteeism, sick leave use, recovery time) to better understand risk levels in their staff31 that have quantifiable impacts on human performance that are often readily addressed through actionable interventions. Also, consider self-report, informal observation, and performance quality problems (quality, volume, etc). Leaders and supervisors know their staff best. If someone who is usually chipper and upbeat is now withdrawn and withdrawn, this might be an initial indicator that further assessment and support are warranted.
Questions to ask might include:
-
(1)
Are any changes being observed in demeanor or absenteeism?
-
(2)
Are certain personnel receiving lower patient satisfaction scores?
-
(3)
Which personnel are repeating tasks or having conflict that is out of the ordinary?
A critical component of both measuring and intervening in risk is providing avenues. The use of post-shift huddles, establishing peer buddies, informal walkarounds, and other strategies can aid in “taking the temperature” of a group or organization. These strategies complement the use of organizational surveys and often lead to greater engagement by personnel.
Once an operationally effective strategy to identify factors that might increase risk is developed, it is critical to have a strategy that addresses who contacts individuals, provides supports, develops, or links to helpful support interventions. Such strategies will necessarily reveal contributory factors that should be the focus of mitigation efforts. As with other elements discussed in this paper, identifying and promoting mitigation strategies is a responsibility of all parts of the organization.
INTERVENTIONS TO ENHANCE SUSTAINMENT IN HCWS
The ability to sustain performance and maintain well-being during disaster events is facilitated by enhancing a sense of safety, calming, self- and team-efficacy, social connection, and hope or optimism.8 These five “essential elements”, mentioned earlier, form the foundation of Psychological First Aid, an evidence-based, resilience-focused framework. Early efforts have been made to adapt these elements to address the unique aspects of the protracted COVID-19 global pandemic.32 Online training33 and actionable education fact sheets34 are readily available as rapid resources, along with larger repositories of educational material,35 to support organizational sustainment during COVID-19.
Consistent with the “Stress Continuum”, featured in Figure 3, efforts to enhance sustainment require actions by HCWs, team members, supervisors, and leaders. Though healthcare systems are equipped to provide basic support to HCWs during normal operations, they often lack policies, processes, and procedures to sustain personnel during a prolonged crisis. Research has revealed critical organizational behaviors that are associated with optimal mental health and performance outcomes for HCWs during infectious disease outbreaks36 and leveraging these within healthcare systems is important for sustainment during COVID-19. Leadership actions and communication play a vital role in the overall well-being of organizations and communities after crisis events.37,38 Understanding what to say and do allows leaders and supervisors to more effectively support and influence their personnel during COVID-19. Because available time and energy are insufficient to create new systems, it is ideal to borrow lessons learned and best practices from high-risk occupations that have experience sustaining operations through extended periods of heightened stress. Below is an overview of individual, organizational, and leadership practices that can sustain performance and functioning for HCWs during COVID-19 and other protracted crisis events by enhancing the “essential elements of PFA. When available, actionable resources have been provided to support implementation of these practices.
Individual Interventions
Self-Care. Sleep, nutrition, hydration, and exercise enhance the ability to make decisions and improve immune functioning.39–41
Social Connections. Feeling connected to others is protective during and following crisis events.42 Using existing social connections and reaching out to others can improve well-being and functioning.
Traditional and Social Media use. Limit exposure to disaster-related and other negative media, which worsens outcomes during disaster events.43
Self-Monitoring. Taking our own “pulse” through self-checks and getting feedback from those around us can alert us to the need for additional self-care and support.
Self-Advocacy. Speaking up when things are wrong reminds us that our voice matters.
Organizations Practices
Practical Supports. Food, parking, lodging, and child-care are essential to allow HCWs to focus on work duties and reduce absenteeism and presenteeism.
Family Safety. Procedures to reduce infection risk allow HCWs to feel comfortable coming to work and reduce stress for them and their family members.
Training. Timely, thorough, realistic, and updated training that prepares HCWs for anticipated exposures optimizes safe task performance and reduces stress of uncertainty.36
Equipment. Providing adequate supplies of effective equipment to protect HCWs for which they are adequately trained to use enhances perceived safety and reduces risk to HCWs and patients.36
Camaraderie. Efforts to enhance connections among personnel (colleagues, managers, others), both in-person and remotely, helps individuals and teams feel connected to the mission and work they are doing.36
Communication. Timely, regular, updated, truthful messages that articulate what is known, what is not known, and create realistic times for sharing additional information will enhance trust in organizations and leaders, improve compliance with recommendations, and optimize functioning.36,44
Education. Ensuring HCWs understand normal psychological and behavioral responses to adverse exposures, providing them with resources to facilitate rapid recovery, and giving them information about when and where to get help when needed improves self- and team -efficacy and overall functioning.36
Growth Mindset. Team learning and growing together improves functioning, collaboration, and performance.45,46 Team huddles (post-shift or post-event) as well as After Action Reviews allow opportunities to learn together, check-in on team members, and correct distortions of thought that can lead to self-blame and moral injury. These non-attributional events convey that team members are valued and foster a sense of learning and cohesion.
Buddy Systems. Collaborative selection of a peer “buddy” serves as formal, rather than ad hoc, peer support.47 This is particularly useful in occupations where personnel have difficulty asking for help and serves to enhance safety, self-/team-efficacy, and social connection.48
Reintegration. Challenges returning to routine work and family after intense and prolonged operations can be more stressful than the actual occupational activities.49,50 Anticipating and planning for the challenges, educating and supporting personnel will improve the transition and optimize organizational functioning.
Leadership Behaviors
Modeling Self-Care. Leaders who model crisis behaviors give permission to their personnel to do the same.51 This can be challenging, particularly in professions that have an ethos of caring for others, often at their own expense. Taking steps to demonstrate desired behavior to subordinates, encouraging supervisors at all levels to do the same, and instituting processes and procedures that facilitate self-care actions strengthen a workforce.52
Effective Communication. Knowing and practicing effective strategies for communication before, during, and following a crisis reduces the frequency and dissemination of rumors, enhances trust and collaboration with personnel, and enhances compliance of personnel with recommended occupational and other health behaviors.53,54
Grief Leadership. Grief is the most universal experience for society during COVID-19,55,56 and other disasters.57 Grief over the loss of routines, certainty in the future, jobs, health, and loved ones. Leading an organization during crisis58 involves communicating effectively while anticipating and acknowledging grief, honoring losses through community-conceived activities59 (ie, ritual events like memorials, and symbolic acts), helping the work community make meaning of the event, and then helping personnel to look hopefully to the future.
CONCLUSION
The global disaster of COVID-19 brings considerable risk to our society with unique challenges for HCWs and the organizations and systems in which they work. The sustainment of the healthcare workforce is vital to an effective response and the ability to ultimately bring the pandemic to an end. Assessing and mitigating risk during COVID-19 through interventions that enhance the “essential elements” are ideal. It is important that interventions involve actions for individuals (and their families), organizations, and leaders to ensure an effective “whole of healthcare” approach. Health systems will benefit from borrowing and adapting existing practices from other high-risk occupations developed to improve functioning and optimize sustainment during prolonged crisis events.
Acknowledgments
The authors wish to thank and acknowledge Abeer Iqbal, Center for the Study of Traumatic Stress, Department of Psychiatry, Uniformed Services University of the Health Sciences for her assistance in the preparation of this manuscript.
Footnotes
No external funding used in preparation of this article.
Morganstein and Flynn have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
The views expressed are those of the authors and do not necessarily reflect the views of the Department of Defense, the Uniformed Services University, the Department of Health and Human Services or the United States Public Health Service.
Clinical significance: Healthcare workers’ (HCWs) occupational stress has increased during COVID-19. Identifying and addressing stress requires efforts by individuals, teams, and leaders. Interventions to sustain HCWs during prolonged crisis are not part of standard operations. Borrowing existing practices from high-risk occupations allows for timely, adaptable, evidence-informed interventions. Specific recommendations are provided.
REFERENCES
- 1. EM-DAT [database online]. Brussels, Belgium: Centre for Research on the Epidemiology of Disasters. [Google Scholar]
- 2. Quick Look: 277 Active Shooter Incidents in the United States From 2000 to 2018 [FBI website]. Available at: https://www.fbi.gov/about/partnerships/office-of-partner-engagement/active-shooter-incidents-graphics. Accessed January 7, 2021. [Google Scholar]
- 3.Morganstein JC, Fullerton CS, Ursano RJ, Donato D, Holloway HC. Raphael B, Fullerton CS, Weisaeth L, Ursano RJ. Pandemics: health care emergencies. Textbook of Disaster Psychiatry. Cambridge: Cambridge University Press; 2017. 270–284. [Google Scholar]
- 4.National Academies of Sciences, Engineering, and Medicine. Long-Term Health Monitoring of Populations Following a Nuclear or Radiological Incident in the United States: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2019. [PubMed] [Google Scholar]
- 5.Hansel TC, Osofsky JD, Osofsky HJ, Friedrich P. The effect of long-term relocation on child and adolescent survivors of Hurricane Katrina. J Trauma Stress 2013; 26:613–620. [DOI] [PubMed] [Google Scholar]
- 6.van der Velden PG, Wong A, Boshuizen HC, Grievink L. Persistent mental health disturbances during the 10 years after a disaster: four-wave longitudinal comparative study. Psychiatry Clin Neurosci 2013; 67:110–118. [DOI] [PubMed] [Google Scholar]
- 7.Nagamine M, Giltay EJ, Shigemura J, et al. Assessment of factors associated with long-term posttraumatic stress symptoms among 56 388 first responders after the 2011 Great East Japan Earthquake. JAMA Netw Open 2020; 3:e2018339–e12018339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hobfoll SE, Watson P, Bell CC, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry 2007; 70:283–315. discussion 316-269. [DOI] [PubMed] [Google Scholar]
- 9.Zhang H, Shi Y, Jing P, Zhan P, Fang Y, Wang F. Posttraumatic stress disorder symptoms in healthcare workers after the peak of the COVID-19 outbreak: a survey of a large tertiary care hospital in Wuhan. Psychiatry Res 2020; 294:113541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. In photos: wildfires burning in the West [CNN web site]; October 28, 2020. Available at: https://www.cnn.com/2020/08/14/us/gallery/western-wildfires-2020/index.html. Accessed January 7, 2021. [Google Scholar]
- 11. Masters J. A look back at the horrific 2020 Atlantic hurricane season [Yale Climate Connections web site]; December 1, 2020. Available at: https://yaleclimateconnections.org/2020/12/a-look-back-at-the-horrific-2020-atlantic-hurricane-center/. Accessed January 7, 2021. [Google Scholar]
- 12. Hollingsworth J. More than 100 dead as Vietnam reels from ‘worst floods in decades’ [CNN web site]. October 21, 2020. Available at: https://www.cnn.com/2020/10/21/asia/vietnam-floods-weather-intl-hnk/index.html. Accessed January 7, 2021. [Google Scholar]
- 13.Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability 2020; 12:3834. [Google Scholar]
- 14.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature. Psychiatry 2002; 65:207–239. [DOI] [PubMed] [Google Scholar]
- 15.Ursano RJ, Fullerton CS, Weisaeth L, Raphael B. Raphael B, Fullerton CS, Weisaeth L, Ursano RJ. Individual and community responses to disasters. Textbook of Disaster Psychiatry. Cambridge: Cambridge University Press; 2017. 1–26. [Google Scholar]
- 16.Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goenjian AK, Steinberg AM, Walling D, Bishop S, Karayan I, Pynoos R. 25-year follow-up of treated and not-treated adolescents after the Spitak earthquake: course and predictors of PTSD and depression. Psychol Med 2020. 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clouston SAP, Guralnik JM, Kotov R, Bromet EJ, Luft BJ. Functional limitations among responders to the world trade center attacks 14 years after the disaster: implications of chronic posttraumatic stress disorder. J Traumatic Stress 2017; 30:443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med 2020; 21:1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Academies of Sciences, Engineering, and Medicine. Rapid expert consultation on understanding causes of health care worker deaths due to the COVID-19 pandemic (December 10, 2020). Washington, DC: The National Academies Press; 2020. [Google Scholar]
- 21.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open 2020; 3:e203976–e1203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag 2020; 28:1686–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu S, Li Z, Li Z, et al. The mental state and risk factors of Chinese medical staff and medical students in early stages of the COVID-19 epidemic. Compr Psychiatry 2020; 102:152202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020; 382:2049–2055. [DOI] [PubMed] [Google Scholar]
- 25. Berg S. 4 ways COVID-19 is causing moral distress among physicians [AMA web site]; June 18, 2020. Available at: https://www.ama-assn.org/practice-management/physician-health/4-ways-covid-19-causing-moral-distress-among-physicians. Accessed January 7, 2021. [Google Scholar]
- 26. Smith K. Caring for our caregivers during COVID-19 [AMA web site]; June 17, 2020. Available at: https://www.ama-assn.org/delivering-care/public-health/caring-our-caregivers-during-covid-19. Accessed January 7, 2021. [Google Scholar]
- 27.Cozza SJ, Fisher JE, Hefner KR, et al. Human remains identification, grief, and posttraumatic stress in bereaved family members 14 years after the September 11, 2011, Terrorist Attacks. J Trauma Stress 2020; 33:1137–1143. [DOI] [PubMed] [Google Scholar]
- 28.Herberman Mash HB, Ursano RJ, Benevides KN, Fullerton CS. Identification with terrorist victims of the Washington, DC sniper attacks: posttraumatic stress and depression. J Trauma Stress 2016; 29:41–48. [DOI] [PubMed] [Google Scholar]
- 29. Combat and Operational Stress Control (COSC) [Psychological Health Center of Excellence web site]. Available at: https://www.pdhealth.mil/readiness-early-intervention/combat-and-operational-stress-control. Accessed January 7, 2021. [Google Scholar]
- 30. The Stress Continuum [America's Navy web site]. Available at: https://www.med.navy.mil/sites/nmcphc/Documents/LGuide/op_stress.aspx#:∼:text=The%20Stress%20Continuum%20Model%20(SCM,the%20Red%20%22Ill%22%20Zone. Accessed January 7, 2021. [Google Scholar]
- 31. Assessment Instruments for First Responders and Public Health Emergency Workers [Center for the Study of Traumatic Stress web site]; 2017. Available at https://www.cstsonline.org/assets/media/documents/CSTS_FS_Assess_Inst_1st_Responders_PH_Emergency_Workers.pdf. Accessed January 7, 2021. [Google Scholar]
- 32.Sulaiman AH, Ahmad Sabki Z, Jaafa MJ, et al. Development of a remote psychological first aid protocol for healthcare workers following the COVID-19 pandemic in a University Teaching Hospital, Malaysia. Healthcare 2020; 8:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Baker J, Bradley JC, Fricchione GL, Isom J, Ryan K. Psychological First Aid: Healthy Recovery Now and in the Aftermath of the COVID-19 Public Health Crisis [Massachusetts Medical Society web site]. Available at: http://www.massmed.org/Continuing-Education-and-Events/Online-CME/Courses/Psychological-First-Aid/Psychological-First-Aid--Healthy-Recovery-Now-and-in-the-Aftermath-of-the-COVID-19-Public-Health-Crisis/. Accessed January 7, 2021. [Google Scholar]
- 34. COVID-19 Pandemic Response Resources [Center for the Study of Traumatic Stress web site]. Available at: https://www.cstsonline.org/resources/resource-master-list/coronavirus-and-emerging-infectious-disease-outbreaks-response. Accessed January 7, 2021. [Google Scholar]
- 35. Topic Collection: COVID-19 Behavioral Health Resources [U.S. Department of Health & Human Services web site]. Available at: https://asprtracie.hhs.gov/technical-resources/115/covid-19-behavioral-health-resources/99. Accessed January 7, 2021. [Google Scholar]
- 36.Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Med 2018; 60:248–257. [DOI] [PubMed] [Google Scholar]
- 37.Birkeland MS, Nielsen MB, Knardahl S, Heir T. Time-lagged relationships between leadership behaviors and psychological distress after a workplace terrorist attack. Int Arch Occup Environ Health 2016; 89:689–697. [DOI] [PubMed] [Google Scholar]
- 38.Veronese G, Pepe A, Massaiu I, De Mol A-S, Robbins I. Posttraumatic growth is related to subjective well-being of aid workers exposed to cumulative trauma in Palestine. Transcult Psychiatry 2017; 54:332–356. [DOI] [PubMed] [Google Scholar]
- 39.Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry 2017; 78:882–888. [DOI] [PubMed] [Google Scholar]
- 40.Bergan T, Thomas D, Schwartz E, McKibben J, Rusiecki J. Sleep deprivation and adverse health effects in United States Coast Guard responders to Hurricanes Katrina and Rita. Sleep Health 2015; 1:268–274. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization, United Nations High Commissioner for Refugees UNCsF, World Food Programme. Food and Nutrition Needs in Emergencies. Geneva: World Health Organization; 2004. [Google Scholar]
- 42.Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. Social and occupational factors associated with psychological wellbeing among occupational groups affected by disaster: a systematic review. J Ment Health 2017; 26:373–384. [DOI] [PubMed] [Google Scholar]
- 43.Bendau A, Petzold MB, Pyrkosch L, et al. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur Arch Psychiatry Clin Neurosci 2020. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reynolds BS, Seeger M. Crisis and Emergency Risk Communication. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 45.Tannenbaum SI, Cerasoli CP. Do team and individual debriefs enhance performance? A meta-analysis. Hum Factors 2013; 55:231–245. [DOI] [PubMed] [Google Scholar]
- 46.Stoto MA, Nelson C, Piltch-Loeb R, Mayigane LN, Copper F, Chungong S. Getting the most from after action reviews to improve global health security. Globalization and Health 2019; 15:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Albott CS, Wozniak JR, McGlinch BP, Wall MH, Gold BS, Vinogradov S. Battle buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth Analg 2020; 131:43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramsberger PF, Legree P, Mills L. Evaluation of the Buddy Team Assignment Program. Alexandria, VA: United States Army Research Institute for the Behavioral and Social Sciences; 2002. [Google Scholar]
- 49. Loop P, Nicola P. Returning to the workplace after COVID-19: what boards should be thinking about [PricewaterhouseCoopers web site]. Available at: https://www.pwc.com/us/en/services/governance-insights-center/library/covid-19-returning-workplace-boards.html. Accessed January 10, 2021. [Google Scholar]
- 50.Creech SK, Hadley W, Borsari B. The impact of military deployment and reintegration on children and parenting: a systematic review. Prof Psychol Res Pr 2014; 45:452–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Leadership Stress Management [Center for the Study of Traumatic Stress web site]. Available at: https://www.cstsonline.org/assets/media/documents/CSTS_FS_Leadership_Stress_Management.pdf. Accessed January 10, 2021. [Google Scholar]
- 52.Wood MD, Walker T, Adler AB, Crouch CL. Post-traumatic growth leadership: mitigating stress in a high-risk occupation. Occup Health Sci 2020; 4:103–122. [Google Scholar]
- 53.Hsu Y-C, Chen Y-L, Wei H-N, Yang Y-W, Chen Y-H. Risk and outbreak communication: lessons from Taiwan's experiences in the post-SARS era. Health Secur 2017; 15:165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Leadership Communication: Anticipating and Responding to Stressful Events [Center for the Study of Traumatic Stress web site]. Available at: https://www.cstsonline.org/assets/media/documents/CSTS_FS_Leadership_Communication_Anticipating_Responding_to_Stressful_Events.pdf. Accessed January 10, 2021. [Google Scholar]
- 55. Glicksman E. How to Lead When an Employee Dies. [The Society for Human Resource Management web site]. Available at: https://www.shrm.org/resourcesandtools/hr-topics/employee-relations/pages/how-to-lead-when-an-employee-dies.aspx. Accessed January 10, 2021. [Google Scholar]
- 56. Chang E. When the world's in crisis, we need ‘grief leaders.’ Here's how to be one [The Washington Post web site]; September 17, 2020. Available at: https://www.washingtonpost.com/lifestyle/wellness/covid-grief-leadership/2020/09/16/51210be4-f444-11ea-bc45-e5d48ab44b9f_story.html. Accessed January 10, 2021. [Google Scholar]
- 57.Bartone P. Grief leadership: leader influences on resilience and recovery following community disaster. Cadet Diary 20: Psychology of Warrior Ethos and Cadet Leadership Development 2019; New Delhi: Rawat Publications, 179–191. [Google Scholar]
- 58. Grief Leadership During COVID-19 [Center for the Study of Traumatic Stress web site]. Available at: https://www.cstsonline.org/assets/media/documents/CSTS_FS_Grief_Leadership_During_COVID19.pdf. Accessed January 10, 2021. [Google Scholar]
- 59.Eyre A. In remembrance: post-disaster rituals and symbols. Austr J Emerg Manage 1999; 14:23–29. [Google Scholar]


