Abstract
This study evaluated the feasibility and effectiveness of translating the evidence-based program, Fit & Strong!, into a Spanish program, ¡En Forma y Fuerte!. A single-group, quasi-experimental design (n = 34, mean age = 58.8 [8.1], 87.2% female, 87.2% reported speaking mostly Spanish) was used to assess implementation feasibility and the impact of ¡En Forma y Fuerte! on arthritis-related outcomes in Hispanics with arthritis. Significant improvements in lower-extremity strength, perceived physical function, and pain were observed from baseline to 8 weeks (p < .05); these improvements were maintained at 6 months. Significant improvements in aerobic endurance and stiffness were observed from baseline to 6 months (p < .05). No major program adaptations (other than language) were observed or reported. However, the instructors provided several suggestions for program improvements, including adjusting the literacy level and length of the program. Findings suggest ¡En Forma y Fuerte! is feasible and effective, potentially providing a much-needed program for older Hispanics with arthritis.
Keywords: physical activity, exercise, arthritis, aging, physical function
Primarily due to the aging of the U.S. population, the public health burden of arthritis is expected to increase substantially. The proportion of adults with arthritis is projected to increase to nearly 1 in 4 adults by 2030. While it is anticipated adults over the age of 65 will account for 50% of all arthritis diagnoses, nearly one-third of all cases will occur in adults aged 45–64 (Hootman & Helmick, 2006). The most common form of arthritis is osteoarthritis (OA), affecting nearly 27 million individuals (Lawrence et al., 2008). Arthritis is the leading cause of disability (Centers for Disease Control and Prevention [CDC], 2009; Hootman, Helmick, & Brady, 2012) and it is associated with high medical care utilization. Nearly 10% of all ambulatory care visits in 2010 were in persons with a primary or secondary diagnosis of arthritis or other rheumatic conditions, accounting for more than 100 million visits. Likewise, joint replacements accounted for 3.5% of all inpatient procedures (1.3 to 1.4 million procedures) during 2010 and 2011 (United States Bone and Joint Initiative, 2014). Medical costs associated with arthritis increased by 42 billion dollars between 1997 and 2003 (Yelin et al., 2007) and total national medical expenditures among U.S. adults with arthritis increased by 100 billion from 1997–2005 (Cisternas et al., 2009).
As the U.S. population ages, it will become more ethnically diverse. Hispanics are the fastest growing segment of the older adult population and will comprise nearly 20% of the older adult population by 2050 (Ortman, Velkoff, & Hogan, 2014). This growth in the Hispanic population may have a substantial impact on the public health burden associated with arthritis. Findings from one study suggest the prevalence of arthritis is higher in Hispanic older adults (44%) than non-Hispanic White (25%) older adults (Dunlop, Manheim, Song, & Chang, 2001), while other studies find Hispanics have a lower or similar age-adjusted prevalence of arthritis (Centers for Disease Control and Prevention [CDC], 2005, 2010, 2011, 2013). However, research consistently indicates Hispanics are more affected by their arthritis. Hispanics consistently report higher rates of arthritis-related activity limitations than non-Hispanic White individuals (Abraído-Lanza, White, Armbrister, & Link, 2006; Centers for Disease Control and Prevention [CDC], 2005, 2013; Dunlop et al., 2001; Hootman & Helmick, 2006; Song et al., 2007) and more severe pain (Centers for Disease Control and Prevention [CDC], 2005, 2011), suggesting the need for interventions to improve self-management of arthritis and arthritis-related symptoms in this population. Moreover, there is a growing recognition of the need for culturally-tailored health promotion and behavior change programs to reduce health disparities. Incorporating cultural components into health behavior change programs may enhance their appeal, appropriateness, and effectiveness (Barrera, Berkel, & Castro, 2017; Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1999).
Exercise is considered a cornerstone in the management of arthritis (Bennell, Dobson, & Hinman, 2014; Brosseau et al., 2015; Hochberg et al., 2012). Regular exercise is known to decrease pain, improve physical function, and may delay disability in people with arthritis (Ettinger & Afable, 1994; Ettinger et al., 1997; Hughes et al., 2006; G.A. Kelley, Kelley, Hootman, & Jones, 2011; Messier et al., 2000; Miller, Rejeski, Reboussin, Ten Have, & Ettinger, 2000; Penninx et al., 2001). Yet, Hispanics with arthritis may be less likely than non-Hispanic Whites to participate in regular physical activity (PA) (Fontaine, Heo, & Bathon, 2004; Shih, Hootman, Kruger, & Helmick, 2006), which may contribute to disparities in arthritis-related health outcomes.
Currently there are few evidence-based self-management or PA programs specifically for arthritis that have been adapted for use in the Hispanic population. This lack of programming may be a salient barrier to participation in PA and may contribute to the observed disparities in arthritis-related outcomes. To the best of our knowledge, the only evidence-based (EB) programs targeting arthritis that have been adapted for use in the Hispanic population are the Chronic Disease Self-Management Program (Lorig, Gonzalez, & Ritter, 1999; Lorig, Ritter, & González, 2003), the Arthritis Self-Management Program (Lorig et al., 1999; Lorig et al., 2003), and Walk with Ease (Camine con Gusto) by the Arthritis Foundation, suggesting the need to expand the number of evidence-based programming for the Hispanic population (Brady, Jernick, Hootman, & Sniezek, 2009).
Fit & Strong! is one of nine programs recommended by the Centers for Disease Control and Prevention for people with osteoarthritis (Brady et al., 2009). It has demonstrated significant benefits on PA, self-efficacy for exercise, pain, and joint stiffness as well as improved lower extremity strength and mobility among older non-Hispanic adults with OA (Hughes et al., 2004, 2006, 2010). Fit & Strong! has been widely disseminated. As of 2015, Fit & Strong! is operating in seven states within the U.S. and over 4,000 people have participated in the program. Based on the success of this program and the apparent need for programs for the Hispanic community, the purpose of this study was to translate Fit & Strong! (¡En Forma y Fuerte!) into a Spanish-language-based program and to evaluate the feasibility of implementing ¡En Forma y Fuerte! with Hispanics who have lower extremity osteoarthritis. The aim of this study was to examine the feasibility of implementing ¡En Forma y Fuerte! in Hispanics with arthritis. The assessment of feasibility included an evaluation of the effectiveness of ¡En Forma y Fuerte! on lower-extremity strength, aerobic endurance, and perceived physical function, pain, and stiffness in Hispanics with lower extremity arthritis; an assessment of implementation fidelity, participant and instructor satisfaction with the program, and program adaptations needed to enhance the program’s cultural relevancy.
Methods
Study Design
We used a single-group, pre-post quasi-experimental design to examine the effectiveness of the program on lower-extremity strength, aerobic endurance, perceived pain, physical function and stiffness, self-efficacy for arthritis management, and self-efficacy for exercise to assess the feasibility of implementing a Spanish version of Fit & Strong! All outcome measures were taken at baseline, 8 weeks (at the end of the program), and 4 months after completion of the program (6 months from baseline assessment). To assess feasibility components, attendance was tracked by the instructors. Fit & Strong! research staff randomly observed classes to assess program fidelity and participants completed satisfaction surveys at the end of the program. At the end of the 8-week program, focus groups were held with program participants to examine their experiences with the program, barriers and facilitators for program attendance, and areas where the program warranted improvement and cultural tailoring. Additionally, in-depth interviews were held with exercise instructors to examine their perceptions regarding ease of delivery of the program, participant satisfaction, strengths and weaknesses of the program, and suggested areas for improvement and/or cultural tailoring.
Participants and Recruitment
Eligible participants were Hispanic individuals with a self-report of a diagnosis of arthritis in the lower extremity (lower back, hip, knee, ankle, or foot). Eligibility criteria included being at least 45 years of age, Hispanic or Latino ethnicity, a self-reported physician diagnosis of lower extremity OA, ability to speak and read in Spanish, no known contraindications to exercise as assessed by the Revised Physical Activity Readiness Questionnaire (R-PARQ) (Cardinal, Esters, & Cardinal, 1996) or physician approval to participate in the physical activity program, currently engaging in less than 150 min of PA per week, and no recent hip or knee replacement surgery (<1 year). Participants were excluded if they had rheumatoid arthritis, evidence of severe cognitive impairment as assessed by a modified version of the Short Portable Mental Status Questionnaire (SPMSQ; Gornemann, Zunzunegui, Martínez, & Onís, 1999; Pfeiffer, 1975), a steroid injection in the hip or knee within the past 3 months, any hip or knee surgery within the past 6 months, or a hip or knee replacement within the past year. The SPMSQ was modified and adapted to make it more culturally appropriate for the Hispanic population. Specifically, as suggested by Gornemann et al. (1999), the adaptations we made included removal of the questions regarding maiden name and the name of the previous president. Participants were also asked to name the days of the week in reverse order instead of counting down from 20 by 3s, as numeracy was perceived as challenging in this population; this is a validated modification (Gornemann et al., 1999).
Participants were recruited from two federally-qualified community health centers, one in Chicago, IL, and one in Phoenix, AZ, both of which served a predominantly Hispanic population. We also recruited from organizations serving Hispanic seniors in the areas surrounding the community health centers (e.g., churches, senior centers, senior apartments, etc.) via presentations, fliers, and manned information tables within the settings. In the Phoenix site, a promotora associated with the health clinic spoke to individuals awaiting appointments and provided them with information about the study. The two sites for delivering ¡En Forma y Fuerte! were chosen to enhance diversity of participants. The Hispanic population in Arizona is 91% Mexican or Mexican American, whereas Chicago has greater diversity with Hispanics of Mexican, Mexican-American, Cuban, Puerto-Rican and South American descent. The study was approved by the institutional review boards at the Arizona State University and the University of Illinois at Chicago. All participants provided informed consent prior to participation in the study. Participants could provide informed consent in either Spanish or English based on their language preference; bilingual researchers obtained informed consent.
Intervention
¡En Forma y Fuerte! was delivered in Spanish by bilingual, bicultural, qualified exercise instructors. To lead Fit & Strong!, exercise instructors are required to have an exercise instructor/specialist certification through a national organization such as the American College of Sports Medicine, American Council on Exercise, or Aerobics and Fitness Association of America, or to have an undergraduate degree in an exercise science related field. Additionally, the instructors completed an 8-hr Fit & Strong! training which provided didactical information and hands-on experience delivering Fit & Strong! To ensure consistency of program delivery, one instructor per site delivered the program for the duration of the 8-week intervention. All classes were delivered within the community health centers’ facilities.
Consistent with the original format of Fit & Strong! (Hughes et al., 2004, 2006, 2010), ¡En Forma y Fuerte! is an exercise and health education program designed to improve arthritis-related outcomes. The classes met three times per week for 90 min each for 8 weeks. Each class session consisted of 60 min of exercise and 30 min of health education. The exercise protocol included 10 min of warm-up and cool-down exercises, 20 min of low-intensity aerobic exercises, and 20 min of lower extremity strengthening exercises. The exercise program was progressive in nature and tailored to individual capabilities. The health education program focused on arthritis management and behavioral strategies to increase PA.
Translation Process
Fit & Strong! was translated from English to Spanish by a team of translators who were primarily Mexican-American. Two of the translators were certified translators; the other two were bilingual students. The Fit & Strong! manual was forward translated to Spanish and back translated to English. Discrepancies between the forward and back translation and concerns regarding the ideal Spanish wording were discussed and resolved among the team of translators (n = 4). After the forward and back translations were completed and the Spanish version of the manual was finalized, a fifth individual who was a certified translator and high school Spanish instructor reviewed the manuscript for errors and any mistakes were corrected. The exercise instructors also kept track of any mistakes or problems they identified in the manual when they delivered the program.
Measures
Physical Function
Lower extremity strength.
Participants were asked to perform five successive chair stands as fast as they could to assess lower extremity strength. Time in seconds to the nearest tenth was recorded using a standard stop watch. This tests correlates well with measures of knee flexor and extensor muscle strength (Csuka & McCarty, 1985).
Aerobic endurance.
Aerobic endurance was assessed using the 6-min walk (Guyatt et al., 1985). Participants were asked to cover as much distance as possible on a standard 50-m course. The distance, covered in feet to the nearest inch, was recorded using a rolling measuring tape. Participants could stop to rest if necessary and standardized motivational prompts were used (e.g., you have completed 1 min, you have 1 min left to go). Due to the small sample size, the distance walked was converted to meters/second for analyses. Individuals who could not finish the 6-min duration were included in the analyses. This test measures functional exercise capacity reliably (Guyatt et al., 1985; Pankoff, Overend, Lucy, & White, 2000a, 2000b).
All measures of physical function were administered by trained research staff at each site. Most of the research staff had an undergraduate degree in an exercise science, kinesiology, or health-related degree and previous experience assessing physical function outcomes. All research staff underwent a protocol-specific training to administer the tests of physical function. Staff were required to demonstrate proficiency and accuracy (compared to the trainer) prior to obtaining the data in the field. All efforts were made to have the same individual administer the pre- and posttest evaluations. The instructors of the program were not involved with any of the outcome assessments. The individuals conducting the assessments were bilingual.
Arthritis symptoms: perceived pain, stiffness, and physical function impairment.
A Spanish-language version of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to assess the impact of arthritis on pain, stiffness, and physical function (Bellamy, Buchanan, Goldsmith, Campbell, & Stitt, 1988). The pain subscale consists of five questions and participants ranked their pain from 0 (no pain) to 4 (extreme pain). The stiffness scale consists of two questions and participants were asked to rank the amount of stiffness they have from 0 (no stiffness) to 4 (extreme stiffness). The physical function scale consists of 17 questions and participants were asked to rank their level of difficulty in performing a task from 0 (no difficulty) to 4 (extreme difficulty). For each of the three subscales, the scores were summed; a higher score is indicative of poorer outcomes. In previous research, these three subscales had internal consistency values of 0.86, 0.71, and 0.96, respectively (Bellamy et al., 1988). In the present study, the internal consistency values for pain, stiffness, and mobility were 0.85, 0.83, and 0.86, respectively.
Self-Efficacy
Self-efficacy for exercise.
A Spanish-language version of the Lorig self-efficacy scale for exercise was used to assess exercise self-efficacy (González, Stewart, Ritter, & Lorig, 1995; Lorig et al., 1996). The scale consists of four questions regarding individual’s perceptions about their confidence in their ability to perform exercise on a regular basis. Participants were asked to rank their confidence from 1 (not at all confident) to 10 (totally confident). Scores were summed and ranged from 4–40. A high score indicates a high amount of confidence in their ability to perform various exercises regularly. In previous research, this survey had an internal consistency reliability of .83 and a test-retest reliability of .86 (Lorig et al., 1996). In the present study, this scale had an internal consistency of 0.86.
Self-efficacy for arthritis management.
Self-efficacy for arthritis management was assessed with a Spanish-language version of the Lorig Self-Efficacy for Arthritis Management Scale (González et al., 1995). Participants were asked to rank their confidence in their ability to manage their arthritis symptoms on a scale from 1 (very uncertain) to 10 (very certain). Scores were summed and could range from 8–80. A higher score indicates a high amount of certainty in one’s ability to manage their arthritis symptoms. In previous research, this survey had an internal consistency reliability of .94 (Lorig, Chastain, Ung, Shoor, & Holman, 1989). In the present study, this scale had an internal consistency of 0.91.
Feasibility Assessment
Implementation fidelity.
A structured checklist was used to assess fidelity of program implementation (see Supplemental Material [available online]). The checklist contained a list of the essential elements of the program such as key exercise components, expected interaction between the instructors and the participants, classroom environment, use of ¡En Forma y Fuerte! materials, etc. Trained Fit & Strong! research staff attended and observed one to two sessions of ¡En Forma y Fuerte! unannounced. Research staff used the structured fidelity checklist to note any adaptations, modifications, omissions, or deviations from the protocol. The observers also discussed any observed fidelity concerns with the instructors to understand the reasons and as training opportunities.
Attendance.
The instructor kept daily attendance logs for the participants during the 8-week program. The number of classes attended by each participant was summed to examine attendance.
Participant satisfaction.
Participants completed a 40-item survey regarding their satisfaction with ¡En Forma y Fuerte!. Participants were asked to evaluate their satisfaction with the quality of the environment in which the program was delivered, the exercise program, the exercise instructors, the ¡En Forma y Fuerte! manual, and the group discussions using a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree). Examples of questions include: the equipment was available and adequate (environment); the instructor clearly explained how to do the exercises (instructor); the exercises progressed at an appropriate pace for me (exercise); the manual was clearly written and understandable (manual); and the health topics discussed help me understand my arthritis (discussion groups). Participants were asked to rank whether or not components of the program were helpful for improving their health using a 1 (not helpful at all) to 5 (very helpful) Likert scale. Participants were also asked questions regarding their preferences for exercise program (e.g., Do they prefer exercising at in a group or alone? Do they prefer exercising at home or at an exercise facility?, etc). Finally, participants were asked to rank their overall reaction to the program components (i.e., the class, the instructor, and the manual) from poor to excellent.
Focus groups with participants.
Upon completion of the intervention, all participants were invited to attend a focus group regarding their experiences with ¡En Forma y Fuerte!. One focus group was held at each location after the last class of the program. A trained moderator who was not involved with the delivery of the program moderated the groups. The groups were held in Spanish and the moderator used an established moderator’s guide. Participants (n = 22) were asked a series of questions regarding their satisfaction with the program, perceived barriers to and benefits of participation, and suggestions for improvement of the program. The focus groups were audio-recorded and transcribed verbatim in Spanish. After the transcripts were verified, they were translated to English for analysis.
Interviews with instructors.
In-depth interviews with the exercise instructors were conducted by a study team member using a semi-structured interview guide. The instructors were asked a series of questions regarding their experiences with delivering the program, suggestions for improvement, barriers to program implementation, and perceived acceptability of the program by the participants. The interviews were audio-recorded and transcribed verbatim.
Data Analysis
Descriptive statistics were used to examine participant characteristics and satisfaction with the program. Data was examined for normality prior to any data analysis using the Klosgomorov-Smirnoff statistic, skewness, and kurtosis. To examine the effect of the intervention on outcome variables over time, a repeated measures ANOVA test was used. Sphericity was evaluated with Mauchly’s test of sphericity. If sphericity was violated, Green-house-Geisser values were used. All analyses were conducted in SPSS version 21 (IBM, Inc., Armonk, NY) and the significance level was set to p < .05. Outcomes data are presented only for individuals with complete data (n = 33) at all three time points. Participant satisfaction data were analyzed individually and separately; data shown represent pooled data across sites as the results were similar across sites.
A thematic analysis approach was used to assess the focus group and interview data. Two individuals independently coded the focus group and interview transcripts and inductively identified themes that emerged from the data. N-Vivo (Version 8) was used to facilitate data analysis.
Results
Participant Characteristics
Figure 1 provides an overview of participant flow through the study. In the Chicago site, 17 participants (77.2%) completed the intervention. In the Phoenix site, 20 individuals (95%) completed the intervention; however, 8-week data were only obtained from 16 participants due to scheduling conflicts and the December holiday season. Baseline characteristics of the study participants are presented in Table 1. Participants were mostly female (87.2%), had less than a high school level education (81.6%), and a yearly income less than $20,000 (86.1%). Most participants reported speaking only or mostly Spanish (87.2%). Diabetes (25.6%) and high blood pressure (35.9%) were the most frequently reported comorbidities.
Figure 1 —
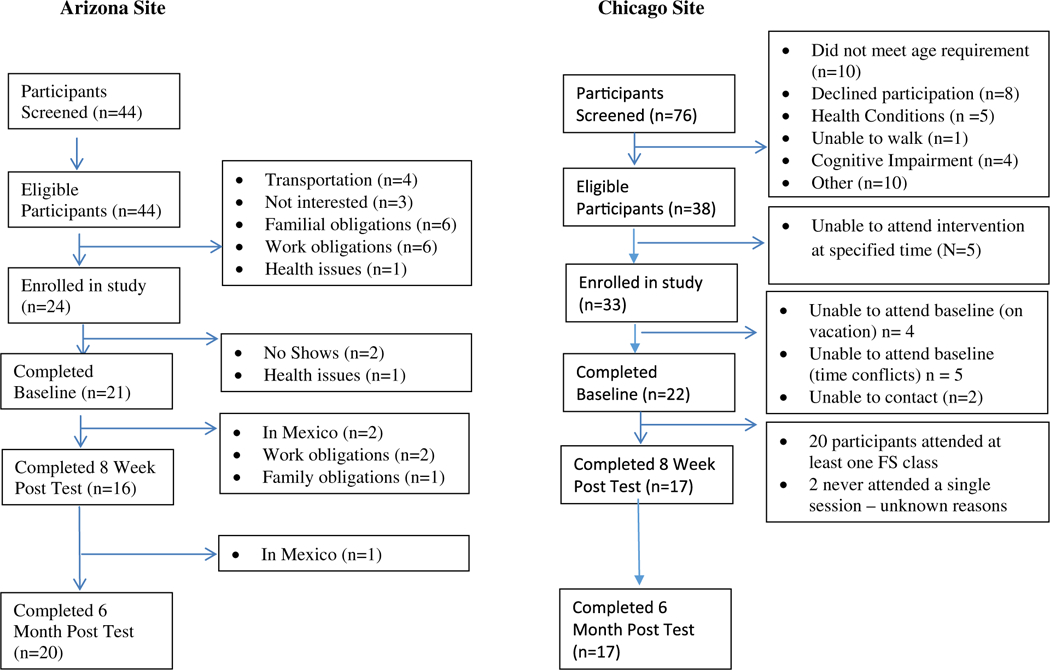
Consort diagram of participant flow.
Table 1.
Baseline Participant Characteristics for the Sample and by Site (n = 39)
| Characteristic | Total |
Phoenix |
Chicago |
|---|---|---|---|
| N (%) or Mean [SD] | N (%) or Mean [SD] | N (%) or Mean [SD] | |
| Sex | |||
| Female | 34 (87.18) | 19 (90.48) | 15 (83.33) |
| Male | 5 (12.82) | 2 (9.52) | 3 (16.67) |
| Age | 58.8 [8.1] | 59.5 [7.9] | 60.4 [8.8] |
| Education level | |||
| Never attended/only kindergarten | 4 (10.53) | 4 (19.05) | 0 |
| Grade 1–8 | 21 (55.26) | 12 (57.14) | 9 (52.94) |
| Some high school (grades 9–11) | 6 (15.79) | 3 (14.29) | 3 (17.65) |
| High school graduate or GED | 2 (5.26) | 0 | 2 (11.76) |
| Some college | 3 (7.89) | 2 (9.52) | 1 (5.88) |
| College graduate | 2 (5.26) | 0 | 2 (11.76) |
| Income | |||
| <$9,999 | 20 (55.66) | 9 (47.37) | 11 (64.71) |
| $10,000–19,999 | 11 (30.55) | 6 (31.58) | 5 (29.41) |
| $20,000–24,999 | 3 (8.33) | 3 (15.79) | 0 |
| $25,000–34,999 | 1 (2.78) | 0 | 1 (5.88) |
| Refused | 1 (2.78) | 1 (5.26) | 0 |
| Body mass index (kg/m2) | 31.9 (7.30) | 31.6 (4.69) | 32.2 (9.69) |
| Chronic conditions (%yes) | |||
| High blood pressure | 14 (35.9) | 5 (23.81) | 9 (50.0) |
| Heart disease | 2 (5.13) | 0 | 2 (11.11) |
| Diabetes | 10 (25.64) | 7 (33.33) | 3 (16.67) |
| Cancer | 2 (5.13) | 1 (4.76) | 1 (5.56) |
| Lung disease | 3 (7.69) | 1 (4.76) | 2 (11.11) |
| Kidney disease | 4 (10.26) | 2 (9.52) | 2 (11.11) |
| Liver disease | 5 (12.82) | 1 (4.76) | 4 (22.22) |
| Stomach disease | 9 (23.68) | 4 (19.05) | 5 (29.41) |
| Blood disease | 1 (2.56) | 0 | 1 (5.56) |
| Stroke or neurological problems | 3 (7.69) | 1 (4.76) | 2 (11.11) |
| Thyroid disease | 6 (15.38) | 6 (28.57) | 0 |
| Acculturation measure (% Spanish only or mostly Spanish) | |||
| Language spoken | 34 (87.18) | 19 (90.48) | 15 (83.33) |
| Language of TV and music | 24 (61.54) | 15 (74.43) | 9 (50.0) |
| Language of books, magazines, and newspapers | 32 (82.05) | 20 (95.24) | 12 (66.67) |
Intervention Outcomes
Intervention outcomes are presented in Table 2. There was a significant effect of time on all intervention outcomes. Specifically, there was a curvilinear and linear effect of time on lower extremity strength as assessed by the chair stands, perceived physical function, pain, arthritis self-efficacy, and self-efficacy for exercise. For each of these outcomes, participants improved significantly from baseline to 8 weeks (p < .05) and maintained these improvements from 8 weeks to 6 months (p < .05). The mean difference in the number of seconds to complete the repeated chair stands from baseline to 8 weeks was 6.95 (95% CI: 3.63–10.27) and the mean difference from baseline to 6 months was 6.35 (95% CI: 3.21–9.46), suggesting the participants were significantly faster at the chair stands after the intervention, a marker of lower extremity strength. The average decrease in perceived physical function score from baseline to 8 weeks and baseline to 6 months was 10.89 (95% CI: 5.92–15.87) and 12.71 (95% CI: 7.80–17.62), respectively, suggesting an improvement in physical function. The average decrease in pain scores from baseline to 8 weeks and baseline to 6 months was 2.79 (95% CI: 1.37–4.20) and 3.2 (95% CI: 1.70–4.87), respectively. The average increase in exercise self-efficacy from baseline to 8 weeks and from baseline to 6 months was 6.23 (95% CI: 2.06–10.40) and 5.68 (95% CI: 1.74–9.61), respectively. There was a linear effect of time on walk speed and stiffness (p < .05); significant improvements were observed from baseline to 6 months only. The mean improvement in walk speed from baseline to 6 months was 0.18 m/s (95% CI: 0.05–0.31). Similarly, the mean improvement in distance walked (meters) from baseline to 6 months was 65.90 (95% CI: 7.28– 124.52). Scores on the WOMAC stiffness scale improved, on average, 1.31 (95% CI: 0.52–2.11) points from baseline to 6 months.
Table 2.
Intervention Results From Repeated Measures Analysis of Variance
| Measure | Time 1 (Baseline) | Time 2 (8 Weeks) | Time 3 (6 Months) | (F Value) | (p Value) |
|---|---|---|---|---|---|
| Chair stand (seconds) | 18.96a | 12.01b | 12.62b | 16.92 | <.001 |
| WOMAC pain | 8.89a | 6.11b | 5.61b | 11.47 | <.001 |
| WOMAC stiffness | 4.12a | 3.34ab | 2.81b | 6.00 | .004 |
| WOMAC function | 31.64a | 20.75b | 18.93b | 18.04 | <.001 |
| Walk speed (m/s) | 0.84a | 0.92a | 1.02b | 4.48 | .016 |
| Exercise self-efficacy | 25.97a | 32.19b | 31.65b | 6.85 | .002 |
| Arthritis management self-efficacy | 36.97a | 66.26b | 63.42b | 45.76 | <.001 |
Note. A different superscript indicates a significant difference in pairwise comparisons. WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Feasibility Evaluation Outcomes
Participant attendance.
In Phoenix, the average number of classes participants attended was 14.9 (range = 4–24) whereas in Chicago the average number of classes attended was 16.6 (range = 5–23). In Chicago, 57.9% of participants attended at least 75% of the classes, while in Arizona, 66.7% of participants attended at least 75% of the classes. The main reasons for participant nonattendance included lack of transportation, acute and chronic illness, traveling out of town, and the holidays. Many participants (N = 5) in the Phoenix location traveled to and from Mexico to visit family members, causing them to miss class. The intervention also spanned the major fall holidays, ending just prior to Christmas (December 20th), causing some individuals to miss classes.
Program adaptations.
Based on observations of ¡En Forma y Fuerte! by Fit & Strong! research staff, the program was delivered with fidelity at both sites; no major cultural adaptations were observed. Minor and acceptable modifications to the exercise program were observed in the Phoenix location and these were primarily driven by space restrictions and weather conditions. To accommodate a small space, the instructor used line dancing for the aerobic exercise component and added outdoor walking once the weather was cool enough to do so.
Participant satisfaction survey results.
Results from the satisfaction survey indicated the participants viewed ¡En Forma y Fuerte! favorably. Overall, participants rated ¡En Forma y Fuerte! (89.3%), the instructor (89.3%), and the manual (67.9%) as excellent, and perceived the ¡En Forma y Fuerte! classes as worth their time (96.4%). The program was perceived as helpful for improving the participants’ health. More than 90% of participants (range 89.7–96.9%) perceived the individual exercise components (stretching, aerobic exercises, and strength training), the manual, and the group discussions as helpful or very helpful for their health. Illustrative comments regarding the quality of ¡En Forma y Fuerte! included, “Can you please continue the program? It is excellent. It helps us in many ways. Personally, it helped me a lot.” and “I liked it. I hope it continues. It’s the best thing I have done. I am very happy.”
Overall, the participants perceived the program environment, including the time it was offered (90.6%) and the equipment provided (93.8%), as acceptable. The main weakness identified by the participants was the adequacy of the space in which the program was offered; 18.3% of participants, primarily from the Phoenix location, did not think there was enough space to accommodate the exercise program. Illustrative quotes included, “Everything was good except for the small space” and “A little more space would have been nicer.”
Participants strongly agreed that the instructors were enthusiastic (90%), able to modify the exercises as needed for participants of varying levels (86.2%), and provided clear instructions (92.9%). Participants strongly agreed the exercise was fun (83.3%) and progressed at an appropriate pace (69%). However, 30% of participants indicated the exercises were too hard given their arthritis. Participants described their experience with the exercise program as, “The program offered everything. It was very complete.” and “The exercise routines were very good. They were wonderful. I liked them.” Participants were satisfied with the ¡En Forma y Fuerte! manual. All participants (100%) agreed it was clearly written and the exercise descriptions were clear; however, several participants recommended we include more pictures in the manual to make it more appealing. Finally, participants agreed or strongly agreed that the group discussions were helpful. Specifically, participants reported that the group discussions helped them to better understand their arthritis (100%), the importance of exercise for managing arthritis (100%), and motivated them to stay in ¡En Forma y Fuerte! (100%). Nearly all participants (90%) indicated they used what they learned in ¡En Forma y Fuerte! outside of class.
The majority of participants in ¡En Forma y Fuerte! indicated that they preferred to participate in facility (95.8%) and group-based (93%) exercise programs. Participants were mixed in their opinion of the length of ¡En Forma y Fuerte!. Fifty-six percent of participants thought the program should be longer while 44% indicated they would not change the length of the program. Of those who thought the program should last for a longer period of time, 62% thought the program should be ongoing and 24% thought it should be a 20-week program.
Participant focus group results.
Participants in the focus groups provided a positive evaluation of ¡En Forma y Fuerte!. Participants in both locations described obtaining numerous benefits from participating in the program. Participants stated that their program participation improved their arthritis. More specifically, they described having reduced pain, improved mobility, decreased stiffness, more energy/vigor, “feeling better,” and reduced medication use. Illustrative quotes are as follows:
“I couldn’t tie my shoes before; someone else would have to because I could not bend over. I felt like I was drowning. Now I can tie my own shoes easily, I can untie them, anything, and I can do it very well.”
“And well it helped me plenty with my back. I have improved in many ways. Before coming here I would take pill after pill for the pain that were only ‘calmantes.’ And, now I haven’t been taking them anymore. And, well thank you to the program.”
“It helped me because my hip hurt a lot. And they had told me that they couldn’t do anything for me. And now with exercising, I can now go up the stairs. I carry my wood. I carry my machines and I no longer have the pain. Thanks to the exercises and thank you to all of you and your entire team.”
“I feel very good because I was one of those people that everything hurt … my name was Dolor (pain). And since I came here, I feel very good. I am active at five in the morning”
Participants in both locations indicated overall enjoyment of ¡En Forma y Fuerte! Participants were satisfied with the health education manual and expressed they learned a lot from the program. For example, one participant stated, “… the book explains things very well. Everything is a matter of putting it to practice. And a rule that we should follow is that if someone doesn’t feel like exercising, we need to follow the ‘one-minute rule’ and from there we need to continue and continue.” Similarly, another said, “It’s a book that informs you about everything. There is information from “A” to “Z”. And I recommend that you don’t store it away for it to grow dust. Let’s keep reading it and everyday learn something new and … make it a routine.”
The participants provided limited feedback on program adaptations that would make the health education program more culturally appropriate. Suggestions included adding more pictures, including more culturally appropriate pictures, to the health education manual, and allowing them to take the book home to read it before coming to class. Participants did not perceive they had sufficient time to read the materials during the health education program. For example: “But I think we all needed a little more time to analyze it and for us to ask questions if we didn’t understand something.”
Similarly, the exercise component of ¡En Forma y Fuerte! was well received by the participants. They described the program as “ … Complete because all of the exercises were varied” and “motivating”, and generally liked the exercises they were asked to do, including the strengthening exercises. For example, one participant said, “I liked the dancing. I really liked the dancing. I like the walking too. And even though we sometimes thought it was hard and that we couldn’t lift the weights, we made it to the end, the ten pounds.” Another stated, “Everything was great combined, everything. The dancing, the dancing got me excited.”
The participants’ main critiques of the exercise program were related to insufficient space to exercise in the Phoenix location and program length. Many participants in both sites thought the program needed to be longer. In Phoenix, participants expressed a desire for the classes to be 2 hr in length and for the program to last for 12 weeks or to be ongoing. In Chicago, participants echoed the need for the program to be longer than 8 weeks. Embedded in the need for the program to last for a longer period of time was the need for programs addressing arthritis in the Hispanic community and a desire for group-based exercise programming in the Hispanic community.
The main barriers to participation in the program were competing responsibilities, sickness, and transportation. Several participants in the Phoenix site were working full- or part-time and their work schedule sometimes prevented them from attending the program. Others had children or family members for whom they provided care, which prevented them from coming to the program. Finally, in Phoenix, some expressed difficulties with transportation to and from the program. One person indicated they had to buy a bus pass in order to continue their participation. The main facilitator for program participation was the program itself. Participants enjoyed attending the program, found it motivating, and liked the group format. Embedded in this was the notion that participants felt better, were in less pain, and could do more things in their daily lives. These improvements kept them motivated to come to the program. In Phoenix, several participants indicated their family members were instrumental in providing support and motivation to attend the program. Participants described receiving encouragement to attend the program from their husbands, children, and even their doctors. In the Phoenix location only, the promotora was viewed as a motivating factor. Participants indicated the promotora made them feel “like family.” In both sites, the encouragement the instructors provided was viewed as a motivation to attend the program. Several also suggested that involving healthcare providers in encouraging participants to attend the program would be a good way to get Latinos to go to ¡En Forma y Fuerte!
Instructor interview results.
The instructors viewed ¡En Forma y Fuerte! favorably. Instructors from both sites indicated participants in the program improved their arthritis-related symptoms over the course of the program and perceived that participants were satisfied with the program. The instructors both perceived the exercise program was well sequenced and appropriate for the needs of Latino individuals with arthritis. Instructors at both sites indicated they added dance to the aerobic exercise routine to make it more acceptable and motivating for the participants. They also incorporated Latino music to make it more fun and acceptable. The instructors did not alter the strength training component of the program, however, instructors at both sites indicated some difficulties with implementing the strength training aspect of the program. In Phoenix, the instructor stated it took several weeks before the participants were comfortable with the use of the ankle weights because it was new to them. The instructor stated she had to spend a lot of one-on-one instruction time with the participants and she was only able to do this because a promotora was there to help. Specifically, the instructor stated, “It was also very helpful that she (the promotora) was with me in the classroom because I could not … it was a little chaotic or disorganized because there was a lot of people that needed help to put the weights on. So the days she was absent we had to extend the length of the class because I spent too much time working one-on-one with them.” She also recommended the possibility of adding a few classes at the beginning of the program to allow the participants to become familiar with using the weights and work on form and posture, especially if the participants are new to this type of exercise. The instructor in Chicago experienced some resistance from the participants when it came to increasing the weights in the ankle cuff as there was a fear of pain. She was able to work through it though by modifying her approach. In Chicago, the instructor also incorporated “partner work” for the more difficult exercises.
Both instructors positively evaluated the manual, however, there were some concerns and suggestions for improvement. Both instructors expressed concerns regarding the literacy level of the recipients and it was specifically recommended we reduce the reading level of the health education manual and add more pictures (which we have done). Related to this issue, the instructor in the Phoenix location perceived the participants needed more time during the health education program to digest the materials and complete worksheets during some lessons. She specifically stated, “They (the lessons) were too long for these participants, for their level of understanding. It was too much information to be covered in a half hour.” She recommended extending the program to 12 weeks and decreasing the content presented in each section. Having a promotora or second individual present was viewed as a necessity to help the participants fill out and comprehend the materials. She also mentioned another challenge with the instructor manual was adequately addressing the different dialects of the Spanish language. She recommended we incorporate into our training an understanding of the different use of language within the Spanish population and strategies for handling this when it arises.
Finally, both instructors perceived the group format as particularly motivating and relevant to the Latino population. The instructor in Phoenix suggested we develop strategies to enhance interactions among the participants. She perceived they enjoyed sharing their personal experiences with one another and stated, “that is just the way they learn.” She suggested adding “some more cooperative learning strategies” and “partner work” during the program to enhance collaboration and learning.
Discussion
Increasing the availability of evidence-based physical activity programs for people with arthritis has been identified as a priority for managing arthritis (Brady et al., 2009; Arthritis Action Plan). Fit & Strong! is one of the nine evidence-based programs by the Centers for Disease Control and Prevention for individuals with arthritis due to its effectiveness on arthritis-related outcomes including physical function, pain, and stiffness (Brady et al., 2009; Hughes et al., 2004, 2006, 2010). Translating and adapting the program for use in the Hispanic population is warranted for enhancing its reach and had not been previously evaluated. Findings from the present study suggest it is feasible and effective to deliver a Spanish version of Fit & Strong, ¡En Forma y Fuerte!, in Hispanics with arthritis, potentially providing a much-needed evidence-based physical activity and health education program for members of the Hispanic with arthritis.
In the present study, ¡En Forma y Fuerte! resulted in significant improvements in objective and perceived physical function, pain, stiffness, and self-efficacy for arthritis management and exercise. Findings from this study were similar to findings from previous clinical trials of Fit & Strong! (Hughes et al., 2010, 2006, 2004). The only subtle differences between the present study and our previous research were that in the present study we saw an improvement in pain at 8 weeks, immediately postintervention, and no improvement in stiffness until 6 months. Our previous research (Hughes et al., 2006, 2004) found the opposite improvements in stiffness at 8 weeks and no improvement in stiffness until 6 months. We also did not see an improvement in walking speed until 6 months and this may be due to the smaller sample size in the present study. The improvement we observed in walking speed has been shown to reduce mortality risk in elderly Spanish individuals with high blood pressure (Gutiérrez-Misis et al., 2015). Similarly, Perera, Mody, Woodman, and Studenski (2006) suggested an improvement of 19–22 m on the 6-min walk test results in small meaningful change and an improvement of 47– 49 m on the 6-min walk tests is association with substantially meaningful change in older adults with and without mobility limitations (Perera et al., 2006). In the present study, the average improvement in distance walked was 65 m, suggesting ¡En Forma y Fuerte! may be associated with substantial improvements in physical function.
Both self-efficacy for exercise and self-efficacy for arthritis management increased significantly from baseline to 8 weeks and these improvements were maintained at 6 months. Self-efficacy is one of the most consistent predictors of exercise participation and adherence in people with arthritis (Wilcox, Der Ananian, Sharpe, Robbins, & Brady, 2005). Maintenance of exercise is critically important for people with arthritis and improving self-efficacy for exercise may facilitate exercise adherence. The theoretical framework of Fit & Strong! focuses on improving self-efficacy for exercise (Hughes et al., 2006, 2004). In a previous clinical trial of Fit & Strong! (Hughes et al., 2006), improvements in self-efficacy and physical activity were maintained out to 12 months in the treatment group while both physical activity and self-efficacy declined over time in the control group, suggesting the importance of improving self-efficacy for maintaining physical activity. Collectively, our findings suggest ¡En Forma y Fuerte! can be effectively implemented in the Hispanic population and may be an effective way to reduce the disparities in arthritis-related outcomes including pain and impaired function (Abraído-Lanza et al., 2006; Centers for Disease Control and Prevention [CDC], 2005, 2011; Dunlop et al., 2001; Song et al., 2007).
Our feasibility assessment of the program suggested that it was feasible to implement ¡En Forma y Fuerte! in the Hispanic population; however, it also revealed some important lessons. Overall, the participants were highly satisfied with the program and reported gaining numerous benefits from participating in the program. They did not want the program to end, with 62% expressing a desire for the program to be offered on an ongoing basis. The instructors did not have to make any major adaptations to ¡En Forma y Fuerte! to successfully implement the program within the Hispanic population. Other than translating and delivering the program in Spanish, no major adaptations were made to the overall program. The instructors emphasized dance during the aerobic component of ¡En Forma y Fuerte!, an acceptable and common adaptation. For the aerobic component of Fit & Strong! instructors are encouraged to include dance, low-impact aerobics, aerobic walking, or a combination of these activities. The subtle distinction between the Hispanic version and the traditional Fit & Strong! may lay in the amount of time devoted to dancing and the fact that the participants preferred this mode of exercise. The instructors also incorporated Hispanic music into the program. Again, this was a minor adaptation as instructors are free to choose the type of music played and often allow the participants to make the music selections. The exercise instructors used in this study were highly experienced and passionate about the health of Hispanics, which may have contributed to our findings. The biggest challenge the instructors experienced was the lack of familiarity with the use of ankle cuffs and engaging in strength training. Possible solutions to this problem include lengthening the class time to 2 hr, adding an additional staff person to assist the lead instructor, or adding an additional week at the beginning of the program during which the participants would become familiarized with the equipment and proper strength training technique and form.
Another challenge encountered was the literacy level of the participants. The majority of the participants in the present trial had less than a high school level education and a significant proportion had less than an eighth grade level education. Literacy and numeracy levels were low for a large portion of the participants. The original version of the Fit & Strong! program was written at an eighth grade reading level. After conducting this trial we learned we needed to lower the literacy level of the program to fourth to sixth grade. Adjusting the format to 12 weeks and reducing the amount of information covered during each section may also be warranted. Related to this, adding more pictures to the manual and/ or adding other formats for disseminating the health information such as a podcast or DVD may be useful. Adding other collaborative learning strategies to enhance discussion among the participants may also be warranted. Finally, having extra staff to help lead the discussion and complete workbook components may be helpful.
Anecdotally, as the research team was planning and hiring staff for the implementation of the program, we discovered a few additional challenges that need to be taken into consideration. First, finding a bilingual, certified exercise instructor was quite challenging in the Phoenix location. This is despite the lead investigator residing at a large, metropolitan university with a well-established program in exercise science and health promotion. This is an important consideration and it may be necessary to test the effectiveness of the program when delivered by community health workers or promotoras. Alternatively, communities may have to establish partnerships with organizations that employ bilingual exercise instructors. In Chicago, this was not an issue because the site employed a certified exercise instructor. Similarly, in the Phoenix location, the use of a promotora was integral to program success. Attempts to recruit participants on site using a university student were unsuccessful; the participants did not know the student and did not want to speak with her. Once the promotora was hired, some of the participants who previously refused to speak with the university employee eagerly signed up for the program. The participants told research staff the promotora attending the sessions and assisting with the study helped create a “family-like” environment. The community health center in which the program was delivered uses a promotora model for the majority of their health programs, so the promotora was a known and trusted individual. Organizations that use a promotora model may need to consider how they can integrate the promotora into the program and the effectiveness of the program when delivered by a promotora warrants investigation.
Study Limitations
This study evaluated the feasibility and effects of a Spanish version of the evidence-based program, Fit & Strong!, using a single-group, pre-post design. While having only one group is a major limitation of this study, the main goals of this study were to test the feasibility of implementing the program in Spanish and to evaluate the effectiveness of the program within this population. Given that the program has proven effectiveness (Hughes et al., 2010, 2006, 2004) and the lack of PA programs specifically designed for arthritis available to the Hispanic population, the research team did not perceive a randomized controlled trial was warranted at the present time. It is highly unlikely that sedentary individuals with arthritis would change their PA in the absence of an intervention as individuals with arthritis are fairly inactive (Dunlop et al., 2011; Shih et al., 2006).
Another limitation was with the generalizability of the study. The majority of the participants in the intervention were Mexican or Mexican American and the findings may not translate to other Hispanic individuals. Many of the cultural adaptations examined and identified in the present study were surface-level adaptations. Bilingual instructors facilitated the program in Spanish and culturally-appropriate adaptations were made to the music and exercise selections. A further examination of the deeper, cultural adaptations that enhance the cultural relevancy of the program may be warranted. Barrera et al. (2017) have highlighted the need to clearly identify the cultural elements that need to be added to evidence-based health promotion programs to improve their effectiveness. While we did attempt to identify these deeper adaptations through focus groups, the participants provided limited feedback regarding necessary cultural adaptions. The Hispanic population is diverse. The present study included primarily Mexican and Mexican-American individuals and the cultural implications and necessary adaptations may vary with other Hispanic individuals or in other settings. Fit & Strong! has been successfully implemented in a variety of community settings including senior centers, park and recreation facilities, and senior housing, to name a few. ¡En Forma y Fuerte! should be able to be disseminated in similar settings but further study of the barriers and facilitators to implementation of this program is warranted.
Finally, attendance at the program may have influenced the observed results. While we evaluated attendance rates at the program, we did not have the power to assess whether attendance influenced the results. Roughly 60% of the participants in the present study attended at least 75% of the classes offered and this may have reduced the effectiveness of the intervention on observed outcomes. The present feasibility trial was more of a “real-world” study with an underserved population. Identifying strategies to improve program attendance is warranted.
Conclusions
As an initial study evaluating the effectiveness of translating and delivering Fit & Strong! in Spanish to Hispanics, the results are positive and consistent with our previous trials evaluating the efficacy and effectiveness of Fit & Strong! (Hughes et al., 2010, 2006, 2004). Participants in the study showed significant improvements in lower extremity strength and perceived pain, stiffness, and physical function from baseline to 8 weeks and maintained these improvements at the 6-month time point. Walking speed improved from baseline to 6 months. The main suggestions for enhancing the cultural relevancy of the program included reducing the literacy level of the program to a fourth grade level, including dance and Spanish music, and using a promotora in the delivery of the program to enhance trust and relationship among the participants and the community center in which the program will be delivered. These findings coupled with the high participant satisfaction rates with ¡En Forma y Fuerte! suggests ¡En Forma y Fuerte! may be a viable PA program for use in the Hispanic population, although more research is warranted.
Supplementary Material
Acknowledgments
This study was funded by the Midwest Roybal Center for Health Promotion & Translation (P30 AG022849) and Retirement Research Foundation10.13039/100001311- Grant # 2011–238. The project described was supported by Grant Number P30AG022849 from the National Institute on Aging10.13039/100000049. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. We’d like to thank the individuals who participated in this research study. Without their assistance and participation, this research would not have been possible. We’d like to thank Andrew Miller and Jenny Quezada for their assistance with data collection. We’d also like to thank Vanessa Santiago and Veronica Segovia for their assistance with leading the program.
Contributor Information
Cheryl Der Ananian, School of Nutrition and Health Promotion, Arizona State University, Phoenix, AZ.
Renae Smith-Ray, Center for Research on Health and Aging, University of Illinois at Chicago, Chicago, IL.
Brad Meacham, School of Nutrition and Health Promotion, Arizona State University, Phoenix, AZ.
Amy Shah, American Academy of Pediatrics, Elk Grove Village, IL.
Susan Hughes, Center for Research on Health and Aging, University of Illinois at Chicago, Chicago, IL.
References
- Abraído-Lanza AF, White K, Armbrister AN, & Link BG (2006). Health status, activity limitations, and disability in work and house-work among Latinos and non-Latinos with arthritis: an analysis of national data. Arthritis and Rheumatism, 55(3), 442–450. 10.1002/art.21981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera M, Berkel C, & Castro FG (2017). Directions for the advancement of culturally adapted preventive interventions: local adaptations, engagement, and sustainability. Prevention Science. 18(6), 640–648 10.1007/s11121-016-0705-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, & Stitt LW (1988). Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. The Journal of Rheumatology, 15(12), 1833–1840. [PubMed] [Google Scholar]
- Bennell KL, Dobson F, & Hinman RS (2014). Exercise in osteoarthritis: moving from prescription to adherence. Best Practice and Research Clinical Rheumatology, 28(1), 93–117. 10.1016/j.berh.2014.01.009 [DOI] [PubMed] [Google Scholar]
- Brady TJ, Jernick SL, Hootman JM, & Sniezek JE (2009). Public health interventions for arthritis: expanding the toolbox of evidence-based interventions. Journal of Women’s Health (Larchmt), 18(12), 1905–1917. 10.1089/jwh.2009.1571 [DOI] [PubMed] [Google Scholar]
- Brosseau L, Wells GA, Pugh AG, Smith CA, Rahman P, Àlvarez Gallardo IC, … Longchamp G (2015). Ottawa panel evidence-based clinical practice guidelines for therapeutic exercise in the management of hip osteoarthritis. Clinical Rehabilitation, 30(10), 935–946. 10.1177/0269215515606198 [DOI] [PubMed] [Google Scholar]
- Cardinal BJ, Esters J, & Cardinal MK (1996). Evaluation of the revised physical activity readiness questionnaire in older adults. Medicine and Science in Sports and Exercise, 28(4), 468–472. 10.1097/00005768-199604000-00011 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2005). Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis–United States, 2002. MMWR. Morbidity and Mortality Weekly Report, 54(5), 119–123. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2009). Prevalence and most common causes of disability among adults–United States, 2005. MMWR. Morbidity and Mortality Weekly Report, 58(16), 421–426. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2010). Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2007–2009. MMWR. Morbidity and Mortality Weekly Report, 59(39), 1261–1265. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2011). Prevalence of doctor-diagnosed arthritis and arthritis-attributable effects among Hispanic adults, by Hispanic subgroup–United States, 2002, 2003, 2006, and 2009. MMWR. Morbidity and Mortality Weekly Report, 60(6), 167–171. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2013). Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation–United States, 2010–2012. MMWR. Morbidity and Mortality Weekly Report, 62(44), 869–873. [PMC free article] [PubMed] [Google Scholar]
- Cisternas MG, Murphy LB, Yelin EH, Foreman AJ, Pasta DJ, & Helmick CG (2009). Trends in medical care expenditures of US adults with arthritis and other rheumatic conditions 1997 to 2005. The Journal of Rheumatology, 36(11), 2531–2538. 10.3899/jrheum.081068 [DOI] [PubMed] [Google Scholar]
- Csuka M, & McCarty DJ (1985). Simple method for measurement of lower extremity muscle strength. The American Journal of Medicine, 78(1), 77–81. 10.1016/0002-9343(85)90465-6 [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Manheim LM, Song J, & Chang RW (2001). Arthritis prevalence and activity limitations in older adults. Arthritis and Rheumatism, 44(1), 212–221. [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, … Hootman JM (2011). Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? Arthritis and Rheumatism, 63(11), 3372–3382. 10.1002/art.30562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettinger WH, & Afable RF (1994). Physical disability from knee osteoarthritis: the role of exercise as an intervention. Medicine and Science in Sports and Exercise, 26(12), 1436–1440. 10.1249/00005768-199412000-00004 [DOI] [PubMed] [Google Scholar]
- Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, … Craven T (1997). A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). Journal of the American Medical Association, 277(1), 25–31. 10.1001/jama.1997.03540250033028 [DOI] [PubMed] [Google Scholar]
- Fontaine KR, Heo M, & Bathon J (2004). Are US adults with arthritis meeting public health recommendations for physical activity? Arthritis and Rheumatism, 50(2), 624–628. 10.1002/art.20057 [DOI] [PubMed] [Google Scholar]
- González VM, Stewart A, Ritter PL, & Lorig K (1995). Translation and validation of arthritis outcome measures into Spanish. Arthritis and Rheumatism, 38(10), 1429–1446. 10.1002/art.1780381010 [DOI] [PubMed] [Google Scholar]
- Gornemann I, Zunzunegui MV, Martínez C, & Onís MD (1999). Screening for impaired cognitive function among the elderly in Spain: reducing the number of items in the short portable mental status questionnaire. Psychiatry Research, 89(2), 133–145. 10.1016/S0165-1781(99)00089-X [DOI] [PubMed] [Google Scholar]
- Gutiérrez-Misis A, Sánchez-Santos MT, Banegas JR, Castell MV, González-Montalvo JI, & Otero A (2015). Walking speed and high blood pressure mortality risk in a Spanish elderly population. Journal of Human Hypertension, 29(9), 566–572. 10.1038/jhh.2015.32 [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, & Berman LB (1985). The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Canadian Medical Association Journal, 132(8), 919–923. [PMC free article] [PubMed] [Google Scholar]
- Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, … American College of Rheumatology. (2012). American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care and Research (Hoboken), 64(4), 465–474. 10.1002/acr.21596 [DOI] [PubMed] [Google Scholar]
- Hootman JM, & Helmick CG (2006). Projections of US prevalence of arthritis and associated activity limitations. Arthritis and Rheumatism, 54(1), 226–229. 10.1002/art.21562 [DOI] [PubMed] [Google Scholar]
- Hootman JM, Helmick CG, & Brady TJ (2012). A public health approach to addressing arthritis in older adults: the most common cause of disability. American Journal of Public Health, 102(3), 426–433. 10.2105/AJPH.2011.300423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell R, Desai P, Huber G, & Chang HJ, (2010). Fit and Strong!: bolstering maintenance of physical activity among older adults with lower-extremity osteoarthritis. American Journal of Health Behavior, 34(6), 750–763. 10.5993/AJHB.34.6.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell R, Huber G, Pollak N, Sharma L, & Desai P (2006). Long-term impact of fit and strong! on older adults with osteoarthritis. Gerontologist, 46(6), 801–814. 10.1093/geront/46.6.801 [DOI] [PubMed] [Google Scholar]
- Hughes SL, Seymour RB, Campbell R, Pollak N, Huber G, & Sharma L (2004). Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist, 44(2), 217–228. 10.1093/geront/44.2.217 [DOI] [PubMed] [Google Scholar]
- Kelley GA, Kelley KS, Hootman JM, & Jones DL (2011). Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res (Hoboken), 63(1), 79–93. 10.1002/acr.20347 [DOI] [PubMed] [Google Scholar]
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, … National Arthritis Data Workgroup. (2008). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis and Rheumatism, 58(1), 26–35. 10.1002/art.23176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Chastain RL, Ung E, Shoor S, & Holman HR (1989). Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis & Rheumatism, 32(1), 37–44. 10.1002/anr.1780320107 [DOI] [PubMed] [Google Scholar]
- Lorig K, Gonzalez VM, & Ritter P (1999). Community-based Spanish language arthritis education program: a randomized trial. Medical Care, 37(9), 957–963. 10.1097/00005650-199909000-00011 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, & Gonzalez VM (2003). Hispanic chronic disease self-management: a randomized community-based outcome trial. Nursing Research, 52(6), 361–369. 10.1097/00006199-200311000-00003 [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, & Lynch J (1996). Outcome measures for health education and other health care interventions. Thousand Oaks, CA: SAGE Publications. [Google Scholar]
- Messier SP, Royer TD, Craven TE, O’Toole ML, Burns R, & Ettinger WH (2000). Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST). Journal of the American Geriatrics Society, 48(2), 131–138. 10.1111/j.1532-5415.2000.tb03903.x [DOI] [PubMed] [Google Scholar]
- Miller ME, Rejeski WJ, Reboussin BA, Ten Have TR, & Ettinger WH (2000). Physical activity, functional limitations, and disability in older adults. Journal of the American Geriatrics Society, 48(10), 1264–1272. 10.1111/j.1532-5415.2000.tb02600.x [DOI] [PubMed] [Google Scholar]
- Ortman JM, Velkoff JA, & Hogan H (2014). An aging nation: the older population in the United States, current population reports (Report No. P25 – 1140). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Pankoff B, Overend T, Lucy D, & White K (2000a). Validity and responsiveness of the 6 minute walk test for people with fibromyalgia. The Journal of Rheumatology, 27(11), 2666–2670. [PubMed] [Google Scholar]
- Pankoff BA, Overend TJ, Lucy SD, & White KP (2000b). Reliability of the six-minute walk test in people with fibromyalgia. Arthritis Care and Research, 13(5), 291–295. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Messier SP, Rejeski WJ, Williamson JD, DiBari M, Cavazzini C, … Pahor M (2001). Physical exercise and the prevention of disability in activities of daily living in older persons with osteoarthritis. Archives of Internal Medicine, 161(19), 2309–2316. 10.1001/archinte.161.19.2309 [DOI] [PubMed] [Google Scholar]
- Perera S, Mody SH, Woodman RC, & Studenski SA (2006). Meaningful change and responiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society, 54(5), 743–749. 10.1111/j.1532-5415.2006.00701.x [DOI] [PubMed] [Google Scholar]
- Pfeiffer E (1975). A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society, 23(10), 433–441. 10.1111/j.1532-5415.1975.tb00927.x [DOI] [PubMed] [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, & Braithwaite RL (1999). Cultural sensitivity in public health: defined and demystified. Ethnicity and Disease, 9(1), 10–21. [PubMed] [Google Scholar]
- Shih M, Hootman JM, Kruger J, & Helmick CG (2006). Physical activity in men and women with arthritis national health interview survey, 2002. American Journal of Preventive Medicine, 30(5), 385–393. 10.1016/j.amepre.2005.12.005 [DOI] [PubMed] [Google Scholar]
- Song J, Chang HJ, Tirodkar M, Chang RW, Manheim LM, & Dunlop DD (2007). Racial/ethnic differences in activities of daily living disability in older adults with arthritis: a longitudinal study. Arthritis and Rheumatism, 57(6), 1058–1066. 10.1002/art.22906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Bone and Joint Initiative. (2014). United States bone and joint initiative: the burden of musculoskeletal diseases in the United States (BMUS). Third edition. Retrieved from http://www.boneandjointburden.org
- Wilcox S, Der Ananian C, Sharpe P, Robbins J, & Brady T (2005). Correlates of physical activity in persons with arthritis: review and recommendations. Journal of Physical Activity and Health, 2(2), 230–252. 10.1123/jpah.2.2.230 [DOI] [Google Scholar]
- Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, & Helmick CG (2007). Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis and Rheumatism, 56(5), 1397–1407. 10.1002/art.22565 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


