Abstract
Background.
The morbidity and mortality from alcohol-related liver disease (ALD) is increasing in the United States. However, little is known about gender differences in evaluation and listing for liver transplantation (LT) in patients with ALD.
Methods.
This is a retrospective review of adult patients with ALD evaluated for LT at a single transplant center from January 1, 2010, to March 1, 2017. Univariate, multivariate, and time-series analyses were performed.
Results.
Among the 949 patients with ALD evaluated, mean age was 53 years, 84% were Caucasian, and 33% were women. The median model for end-stage liver disease score was similar between the genders. Women were less likely to be listed for LT (10% versus 19%; P < 0.05). The proportion of women not listed due to active substance use was significantly higher versus men (42% versus 35%; P < 0.05), while the frequency of medical contraindications was comparable between the genders. During a median follow-up of 416 days (range: 0–2784), listed women with ALD were less likely to undergo transplantation (42% versus 47%; P < 0.05).
Conclusions.
Men with ALD were 95% more likely to be listed and 105% more likely to be transplanted compared to women with ALD. While men had more lifetime substance use and related consequences, women had more psychiatric comorbidities and were less likely to be listed due to active alcohol and opioid use. Early detection and effective treatment of psychiatric and substance use disorders in women with ALD may improve their transplant eligibility.
INTRODUCTION
Alcohol-related liver disease (ALD) is a spectrum of liver abnormalities caused by excessive and chronic alcohol use. Clinical manifestations range from asymptomatic hepatic steatosis to end-stage liver disease with complications of portal hypertension. Cirrhosis was the 12th leading cause of death in the United States in 2016, with about half of cirrhosis-related deaths due to ALD.1,2 Worldwide, approximately 2.3 billion people are current harmful users of alcohol, and the prevalence and mortality of ALD is increasing in the United States, particularly among younger adults.3,4 Consistent with these trends, the proportion of ALD patients being listed for LT has increased nationwide, from approximately 23% in 2006 to 27% in 2016.5-7
Among women in the United States, the prevalence of high-risk drinking increased nearly 60% over the past 10 years, while the prevalence of alcohol use disorder (AUD) has increased >80%.8,9 Although women generally consume less alcohol than men, they are at greater risk than men for developing ALD with lower levels of consumption and experience more rapid development of morbidity from ALD.10 The increased susceptibility of women to ALD may be due to several reasons, including a smaller volume of distribution, reduced gastric metabolism of alcohol, increased gut permeability, and a lower threshold of Kupffer cells to oxidative damage.11 Accordingly, the death rate for chronic liver disease and cirrhosis in the United States increased 18% for women aged 25–44 years and 31% for women aged 45–64 years between 2000 and 2015.12
While women represent only 30% of LT recipients, they are more likely to die on the waiting list than men.13 The exact reasons for this are unknown, but may in part be explained by lower laboratory model for end-stage liver disease (MELD) scores from lower serum creatinine levels when correcting for glomerular filtration rate (GFR), and smaller body size and height that reduce their access to donor organs.5 It is also possible that women may have a reduced likelihood of seeking transplant or being listed for transplant after evaluation. Whether or not women with ALD have equivalent access to transplant compared with men with the same diagnosis is not known. To further explore these potential disparities, we conducted a retrospective review of the medical records to identify gender differences in the evaluation and listing of patients with ALD for LT.
METHODS
The University of Michigan Institutional Review Board approved the research protocol for this retrospective chart review. All adult LT candidates over 18 years of age evaluated at the University of Michigan from January 1, 2010, to March 1, 2017, were included. Pediatric, living donor (24), repeat evaluations (321), and patients with missing data (6) were excluded. All patients were evaluated by a multidisciplinary team of hepatologists, surgeons, and social workers.
Data were abstracted from electronic medical records. Abstracted demographic features included patient age, gender, race, etiology of liver disease, MELD score at the time of evaluation, insurance, employment, and marital status. History of tobacco, alcohol, and illicit substance use; history of substance-related health or legal consequences; psychiatric comorbidities; and prior substance use related treatments were collected. Our process for toxicology assessment changed 4 years ago with the addition of a transplant psychiatrist. While we previously relied primarily on history and physical examination, we have more frequently employed serum and urinary alcohol biomarkers (urine ethyl glucuronide, urine ethyl sulfate, and serum phosphatidylethanol) for screening along with specialty referral to transplant psychiatry and psychology for ongoing assessment and management. At our center, ALD is diagnosed based on clinical assessment linking advanced liver disease to current/prior history of heavy alcohol use (with or without other comorbid liver disease) and exclusion of other causes of liver injury via laboratory and radiological evaluation. Toxicology screening at the initial evaluation and other prelisting test results were collected and analyzed.
The primary outcomes were listing for LT, transplantation or removal from the waitlist. Secondary outcomes included reasons for not listing for transplant and reasons for not receiving a LT while on the waiting list.
Continuous variables were expressed as mean ± SD and categorical variables were expressed as percentages. The baseline characteristics at the time of LT evaluation were compared using independent sample t test for continuous variables and χ2 tests for categorical data. We used multi-variable logistic regression analysis to assess the candidate factors associated with listing status and transplant outcome. These models were adjusted for covariates with statistical significance (P < 0.05) on univariate analysis. These included gender, presence of hepatitis C virus (HCV) or hepatocellular carcinoma (HCC) diagnosis, employment status, substance use history, prior substance-related consequences, and psychiatry comorbidity. Time series analysis was performed for the proportion of patients with ALD evaluated for liver transplant over time. We used SPSS 25.0 (IBM Co., Armonk, NY) for all the analyses.
RESULTS
Among the 2694 adult LT candidates evaluated for LT between January 1st, 2010 and March 1st, 2017, a total of 949 patients had a diagnosis of ALD (Figure 1). The mean age of the ALD candidates was 53 ± 8 years, 84% were Caucasian, and 33% were women. The proportion of LT candidates with ALD significantly increased over time (P = 0.02; Figure 2). The median age, MELD score, % Medicaid, education level, and marital status were similar between men and women (Table 1). Concomitant hepatitis C infection and HCC were significantly more common in men versus women (21% versus 15% and 5% versus 2%; P < 0.05, respectively). Women were more likely to be unemployed (77% versus 65%; P < 0.05), report a history of psychiatric comorbidities (44% versus 27%; P < 0.05), and be prescribed psychiatric pharmacotherapy at evaluation (24% versus 14%; P < 0.05). In contrast, men were significantly more likely to report a history of lifetime tobacco (64% versus 56%; P < 0.05), marijuana (36% versus 21%; P < 0.05), or other substance use (16% versus 10%; P < 0.05) as well as substance-related health or legal consequences compared to women (25% versus 15%; P < 0.05). Of those patients who completed toxicology testing, positive results were similar between men and women.
FIGURE 1.
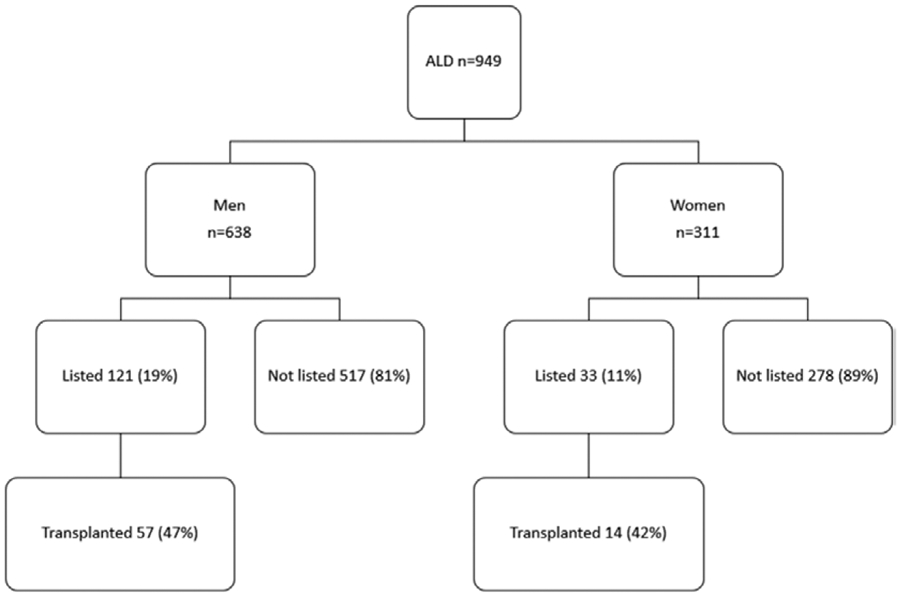
Study cohort. Flow diagram of all patients with alcoholic liver disease evaluated during study period (2010–2017). ALD, alcohol-related liver disease.
FIGURE 2.
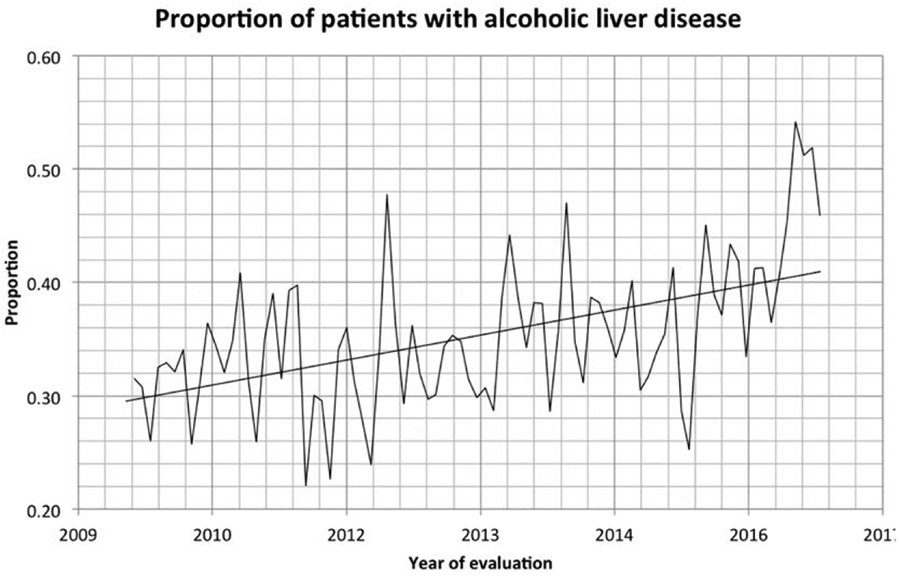
Proportion of patients with alcoholic liver disease evaluated for liver transplant over time (P = 0.02).
Table 1.
Characteristics of adult patients with ALD evaluated for liver transplant
| Evaluations (n = 949) | Men (n = 638) | Women (n = 311) | P |
|---|---|---|---|
| Age, y | 54 ± 9 | 52 ± 9 | 0.75 |
| White | 551 (86%) | 255 (82%) | 0.07 |
| with HCC | 35 (5%) | 7 (2%) | 0.02a |
| with HCV infection | 137 (21%) | 47 (15%) | 0.02a |
| MELD | 16 ± 8 | 16 ± 8 | 0.14 |
| Medicaid | 164 (26%) | 96 (31%) | 0.09 |
| College or higher | 215 (34%) | 97 (31%) | 0.56 |
| Unemployed | 415 (65%) | 240 (77%) | 0.001a |
| Married | 354 (56%) | 164 (53%) | 0.42 |
| Has children | 451 (71%) | 232 (75%) | 0.21 |
| Lifetime alcohol use | 616 (97%) | 301 (97%) | 0.85 |
| Lifetime tobacco use | 406 (64%) | 175 (56%) | 0.03a |
| Lifetime Marijuana use | 231 (36%) | 70 (21%) | <0.005a |
| Lifetime opiate use | 111 (17%) | 53 (17%) | 0.89 |
| Lifetime substance use | 103 (16%) | 30 (10%) | 0.007a |
| Health/legal consequences | 162 (25%) | 48 (15%) | 0.001a |
| History of substance use treatment | 186 (29%) | 89 (29%) | 0.86 |
| Psychiatry comorbidities | 169 (27%) | 138 (44%) | <0.005a |
| Prior psychiatric pharmacotherapy | 91 (14%) | 74 (24%) | <0.005a |
| SIPAT score+ | 4.36 ± 12.69 | 5.86 ± 15.07 | 0.11 |
| Toxicology completed | 513 (80%) | 244 (78%) | 0.48 |
| Substance use treatment | 237 (37%) | 140 (45%) | 0.02a |
| Substance use pharmacotherapy | 7 (1%) | 1 (0.3%) | 0.22 |
P < 0.05.
ALD, alcohol-related liver disease; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; MELD, model for end stage liver disease, SIPAT, Stanford Integrated Psychosocial Assessment for Transplantation; +obtained in 50 women and 79 men.
The proportion of patients with ALD evaluated for LT increased overtime (P = 0.02) (Figure 2). Women with ALD were significantly less likely to be listed for LT (10% versus 19%; P < 0.05) and less likely to undergo LT (40% versus 44%; P < 0.05); this trend continued over time (Figure 3A and B). In women, the number of patients not listed due to active substance use was significantly higher than in men (42% versus 35%; P < 0.05), while the proportion not listed due to medical contraindication was comparable between the groups. During a median follow-up of 416 days (range 0–2784), listed women with ALD were less likely to undergo deceased organ donor transplant (42% versus 47%; P < 0.05) but the proportion removed from the waitlist and stated reasons for removal were similar in the 2 groups (Table 2).
FIGURE 3.
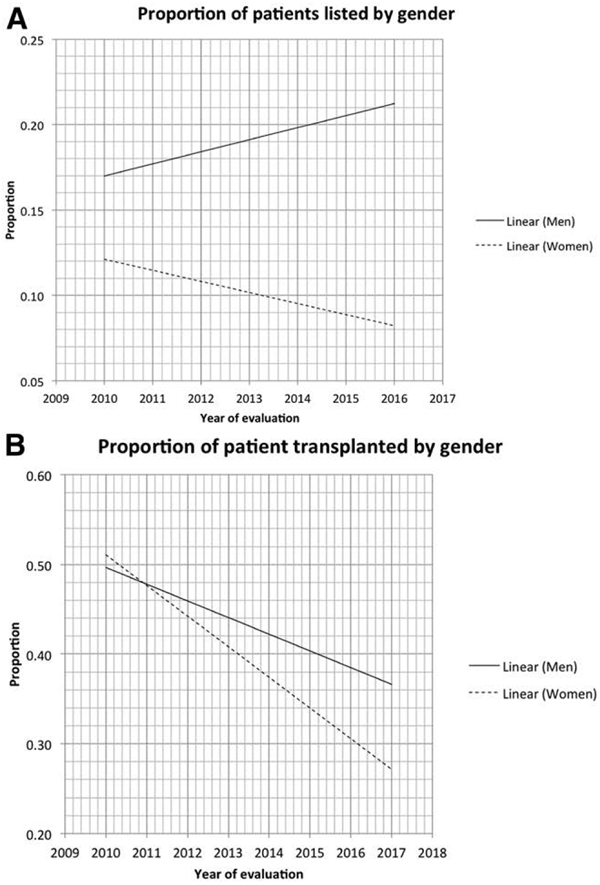
Proportion of patients with alcoholic liver disease listed for liver transplant (A) and transplanted (B) by gender.
Table 2.
Natural history of ALD patients evaluated for LT
| Evaluated (n = 949) | Male (n = 638) | Female (n = 311) | P |
|---|---|---|---|
| Listed | 121 (19%) | 33 (11%) | 0.009a |
| Evaluation to list, d | 128 ± 97 | 120 ± 86 | 0.63 |
| Not listed reason | |||
| Too well | 113 (18%) | 64 (21%) | 0.29 |
| Medical issues | 88 (14%) | 36 (12%) | 0.34 |
| Substance use | 221 (35%) | 129 (42%) | 0.04a |
| Others | 95 (15%) | 49 (16%) | 0.63 |
| Listed (n = 154) | Male (n=121) | Female (n=33) | P |
| Transplanted | 57 (47%) | 14 (42%) | 0.03a |
| Remain on list | 25 (21%) | 6 (18%) | 0.09 |
| Not transplanted reason Deceased | |||
| Deceased | 13 (11%) | 5 (15%) | 0.1 |
| Medical issues | 11 (9%) | 3 (9%) | 0.12 |
| Substance use | 10 (8%) | 3 (9%) | 0.1 |
| Others | 5 (4%) | 2 (6%) | 0.1 |
P < 0.05.
ALD, alcohol-related liver disease; LT, liver transplantation.
As noted in Table 3, a number of baseline clinical features in ALD candidates were associated with being listed for LT on univariate analysis. However, on multivariate analysis, only male gender, presence of HCC, prior history of substance use treatment, and the absence of prior substance use health consequences were predictive factors for being listed for LT. Similarly, a number of baseline clinical features were associated with an increased likelihood of receiving an LT. However, on multivariate analysis, only male gender and the presence of HCC remained as significant factors (Table 4).
Table 3.
Multivariate logistic regression of factors associated with being listed for liver transplant (n = 949)
| Variable | Odds ratio* | 95% CI, low value | 95% CI, high value | P |
|---|---|---|---|---|
| Male | 1.95 | 1.25 | 3.02 | 0.001a |
| HCV diagnosis | 1.19 | 0.73 | 1.97 | 0.48 |
| HCC diagnosis | 4.04 | 2.07 | 7.86 | <0.005a |
| Unemployment status | 1.18 | 0.81 | 1.71 | 0.38 |
| Psychiatric comorbidities | 0.71 | 0.47 | 1.09 | 0.12 |
| History of substance use treatment | 2.43 | 1.58 | 3.73 | <0.005a |
| Prior substance use–related health/legal consequences | 0.524 | 0.31 | 0.87 | 0.014a |
| Substance use treatment recommended at evaluation | 1.45 | 0.98 | 2.13 | 0.06 |
P < 0.05.
Adjusted for gender, presence of HCV or HCC diagnosis, employment status, substance use history, prior consequences, and psychiatry comorbidity. CI, confidence interval; HCC, hepatocellular carcinoma; HCV, hepatitis C virus.
Table 4.
Multivariate logistic regression of factors associated with being transplanted (n = 71)
| Variable | Odd ratio* | 95% CI, low value | 95% CI, high value | P |
|---|---|---|---|---|
| Male | 2.05 | 1.01 | 3.87 | 0.028a |
| HCV diagnosis | 1.63 | 0.66 | 3.99 | 0.28 |
| HCC diagnosis | 2.79 | 0.97 | 8.08 | 0.05 |
| Unemployment status | 1.15 | 0.67 | 1.94 | 0.58 |
| Psychiatric comorbidities | 1.29 | 0.59 | 2.82 | 0.52 |
| Prior substance use treatment | 1.29 | 0.61 | 2.72 | 0.51 |
| Prior substance use-related health/legal consequences | 1.56 | 0.62 | 3.96 | 0.34 |
| Substance use treatment recommended at evaluation | 0.62 | 0.31 | 1.25 | 0.18 |
P < 0.05.
Adjusted for gender, presence of HCV or HCC diagnosis, employment status, substance use history, prior consequences, and psychiatry comorbidity. CI, confidence interval; HCC, hepatocellular carcinoma; HCV, hepatitis C virus.
The clinical characteristics of ALD patients listed for LT by gender are provided in Table S1 (SDC, http://links.lww.com/TP/B762). The median MELD score at evaluation was higher in women (19 ± 10 versus 18 ± 6; P = 0.002). There was no difference in the proportion of patients with concomitant hepatitis C infection or HCC. Women with concomitant HCC and higher education were more commonly listed for LT (Table S2, SDC, http://links.lww.com/TP/B762).
DISCUSSION
ALD is a leading cause of cirrhosis worldwide and now accounts for nearly half of cirrhosis-associated deaths in the United States.1 Our study examined patients with ALD evaluated for LT at a single center over a 7-year period. Men with ALD were 95% more likely to be listed and 105% more likely to be transplanted compared to women with ALD. These findings are consistent with prior research that has demonstrated a lower rate of listing for transplant in women with cirrhosis, as well as an increased likelihood of removal from the waitlist. Cullaro et al recently found an additional 692 women were removed from the waitlist between 2007 and 2014 than would have been expected had they been men. The disparity persisted despite adjustment for other factors known to be associated with sickness and transplant rates, and despite similar survival after delisting.14 The higher rate of delisting and increased mortality on the waiting list observed in women may in part be due to the lower frequency of HCV and HCC, the lower lab MELD scores when accounting for GFR from gender differences in serum creatinine as well as the smaller stature of women LT candidates that reduce their access to donor organs.14 However, clinical characteristics and natural history of patients evaluated for liver transplant remained unchanged when patients with HCC were removed from our cohort, and women with ALD remained less likely to undergo deceased organ donor transplant (Tables S3 and S4, SDC, http://links.lww.com/TP/B762).
Rates of positive toxicology for all substances and history of substance use–related treatment were equal between men and women in our cohort. This contrasts with the known overall lower incidence of substance use in women, as well as the lower rate of substance use-related health and legal consequences.15 Despite this, significantly more women were not listed for LT due to active substance use (42% versus 35%). Several factors may contribute to the differential listing for LT of women and men. Women with ALD may not seek or complete treatment for substance use, their cases may be subject to bias, and available substance use treatment may be less effective for women with ALD due to a higher incidence of psychiatric comorbidity. Furthermore, existing screening protocols in other settings may under-identify women with substance use problems, an issue that has been noted in the substance abuse literature.16-18
Nearly all studies that measure lifetime abstinence from alcohol find it is much more common among women than among men, which makes the finding of higher rates of active substance use as reasons for not listing counterintuitive.19 Interestingly, we found a trend toward increased listing for transplant among women who completed substance use treatment on recommendation from our committee. Further investigation into the effect of substance use treatment on successful listing for LT is needed.
The prevalence of psychiatric comorbidities and history of psychiatric pharmacotherapy were also more prevalent in women (44% versus 27% and 24% versus 14%; P < 0.05), which is consistent with known higher rates of depression, anxiety, and psychiatric treatment in women.20 This may indicate that while women are likely to obtain general mental health treatment, identifying and treating a substance use in women may be more difficult. Psychosocial risk is an important determinant of both psychosocial and medical outcomes after transplant. Although there are several standardized assessment tools available, their use and predictive ability is variable and they are meant as additional tools for clinical judgment, not as replacements for it.21 Schneekloth et al assessed the relationship between the Psychosocial Assessment of Candidates for Transplantation scale and posttransplant outcomes at a single center over 12 years and found that women with ALD and low Psychosocial Assessment of Candidates for Transplantation scores, a marker of higher psychosocial risk, had a 2-fold hazard of death after transplant. This association did not hold for men. Among LT recipients, having a life partner was found to be marginally protective for men but not for women.22 Other validated scales such as the Stanford Integrated Psychosocial Assessment for Transplant, the Transplant Evaluation Rating Scale, and the High Risk for Alcohol Relapse score have been found to have some predictive value in determining candidacy for transplant.21,23,24
Women in our cohort were also more likely to be unemployed, which may indicate a lack of social support or financial resources that disproportionately affect women’s likelihood of being listed. Medicaid insurance rates for LT candidates rose in our population over the study period, and the burden of ALD in the Medicaid population is high, given that AUD and other mental health disorders disproportionately affect patients of lower socioeconomic status.25 Prior research has shown low SES patients have less ability to demonstrate social support adequate for listing for LT. Ladin et al recently surveyed 604 members of the American Society of Transplant Surgeons and Society for Transplant Social Workers from 202 transplant centers. Respondents reported that as many as 20% of candidates evaluated for LT were excluded due to lack of social support. Despite acknowledgment of the importance of social support as predicting success after LT, two-thirds of respondents believed that this burden disproportionately impacted patients of lower socioeconomic status and 25% believed it to be unfair.26 This concept is reinforced by our center’s data, where women with college education or higher were significantly more likely to be listed for LT.
Limitations of our study include the retrospective nature of our study design. The determination of ALD as the primary cause of liver disease was determined by review of medical and social work notes and not established using DSM-5 criteria for AUD. In addition, we unfortunately did not have a standardized metric to assess subject nutritional and frailty status at LT evaluation. Prior studies have suggested that among LT candidates, women may be frailer or have a lower functional reserve than men. In support of this, women who are delisted frequently enter the waiting list with a lower Karnofsky score and higher MELD score.14 In addition, we did not determine what proportion of listed LT candidates with ALD had received an exception score or how many women had livers turned down for them based on size, although both factors have been shown to contribute to lower rates of LT in women.5
In conclusion, our findings show that among LT candidates with ALD, women are less likely to be listed and, once listed, were less likely to be transplanted. Psychosocial factors, including ongoing substance use with higher rates of substance use treatment and more comorbid psychiatric illness, appear to play a role. Future studies are needed to investigate the more nuanced psychosocial and potential medical reasons women are not listed for LT. Once identified, potential solutions may include earlier AUD detection, prompt specialty referral, targeted interventions to strengthen support in patients with AUD, and effective treatment of women with comorbid psychiatric and addictive disorders. Transplant centers may also consider targeted outreach to women regarding LT in an effort to address this critical disparity.
Supplementary Material
Acknowledgments
R.J.F. has received grant support from Abbvie, BMS, and Gilead. He also does consulting for Alnylam pharmaceuticals. J.L.M. has received grant support from an NIAAA K23 Career Development Award (AA 026333-01).
Footnotes
The other authors declare no conflicts of interest.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantjournal.com).
REFERENCES
- 1.Singal AK, Bataller R, Ahn J, et al. ACG clinical guideline: alcoholic liver disease. Am J Gastroenterol. 2018;113:175–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Status Report on Alcohol and Health. 2018. Geneva, Switzerland. Available at https://www.who.int/substance_abuse/publications/global_alcohol_report/gsr_2018/en. Accessed 2019. [Google Scholar]
- 3.Mellinger JL, Shedden K, Winder GS, et al. The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology. 2018;68:872–882. [DOI] [PubMed] [Google Scholar]
- 4.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ. 2018;362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nephew LD, Goldberg DS, Lewis JD, et al. Exception points and body size contribute to gender disparity in liver transplantation. Clin Gastroenterol Hepatol. 2017;15:1286–1293.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant. 2018;18(Suppl 1):172–253. [DOI] [PubMed] [Google Scholar]
- 7.Guirguis J, Chhatwal J, Dasarathy J, et al. Clinical impact of alcohol-related cirrhosis in the next decade: estimates based on current epidemiological trends in the United States. Alcohol Clin Exp Res. 2015;39:2085–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the united states: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64:830–842. [DOI] [PubMed] [Google Scholar]
- 9.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the united states, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74:911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frezza M, di Padova C, Pozzato G, et al. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322:95–99. [DOI] [PubMed] [Google Scholar]
- 11.Allen AM, Hay JE. Review article: the management of cirrhosis in women. Aliment Pharmacol Ther 2014;40:1146–1154. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Death Rates for Chronic Liver Disease and Cirrhosis, by Sex and Age Group. Morbidity and Mortality Weekly Report (MMWR). Available at https://www.cdc.gov/mmwr/volumes/66/wr/pdfs/mm6638.pdf. Accessed March 1, 2019. [Google Scholar]
- 13.Moylan CA, Brady CW, Johnson JL, et al. Disparities in liver transplantation before and after introduction of the MELD score. Jama. 2008;300:2371–2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cullaro G, Sarkar M, Lai JC. Sex-based disparities in delisting for being “too sick” for liver transplantation. Am J Transplant. 2018;18:1214–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71:573–581. [DOI] [PubMed] [Google Scholar]
- 16.Saitz R The best evidence for alcohol screening and brief intervention in primary care supports efficacy, at best, not effectiveness: you say tomāto, I say tomato? That’s not all it’s about. Addict Sci Clin Pract. 2014;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaner E, Bland M, Cassidy P et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ. 2013;346:e8501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green CA. Gender and use of substance abuse treatment services. Alcohol Res Health. 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- 19.Agabio R, Campesi I, Pisanu C, et al. Sex differences in substance use disorders: focus on side effects. Addict Biol. 2016;21:1030–1042. [DOI] [PubMed] [Google Scholar]
- 20.Seedat S, Scott KM, Angermeyer MC, et al. Cross-national associations between gender and mental disorders in the world health organization world mental health surveys. Arch Gen Psychiatry. 2009;66:785–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maldonado JR, Dubois HC, David EE, et al. The stanford integrated psychosocial assessment for transplantation (SIPAT): a new tool for the psychosocial evaluation of pre-transplant candidates. Psychosomatics. 2012;53:123–132. [DOI] [PubMed] [Google Scholar]
- 22.Schneekloth TD, Hitschfeld MJ, Petterson TM, et al. Psychosocial risk impacts mortality in women after liver transplantation. Psychosomatics. 2019;60:56–65. [DOI] [PubMed] [Google Scholar]
- 23.DiMartini A, Magill J, Fitzgerald MG, et al. Use of a high-risk alcohol relapse scale in evaluating liver transplant candidates. Alcohol Clin Exp Res. 2000;24:1198–1201. [PubMed] [Google Scholar]
- 24.Twillman RK, Manetto C, Wellisch DK, et al. The transplant evaluation rating scale. A revision of the psychosocial levels system for evaluating organ transplant candidates. Psychosomatics. 1993;34:144–153. [PubMed] [Google Scholar]
- 25.Rowan K, McAlpine DD, Blewett LA. Access and cost barriers to mental health care, by insurance status, 1999-2010. Health Aff (Millwood). 2013;32:1723–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ladin K, Emerson J, Berry K, et al. Excluding patients from transplant due to social support: results from a national survey of transplant providers. Am J Transplant. 2019;19:193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


