Abstract
Tooth loss can have not just a physical handicap but also a psychological bearing on an individual.Avulsion or complete displacement of the tooth from the socket can result due to various factors ranging from road traffic accidents to domestic abuse. Replantation of such avulsed teeth has been a topic of debate owing to the duration of extra oral time, storage medium and long term success. In this case report we discuss the successful replantation of an avulsed permanent tooth with an increased extra oral dry time using Injectable form of Platelet rich fibrin (i- PRF).
Keywords: Biomaterials, platelet-rich fibrin, reimplantation, tooth avulsion, tooth loss
INTRODUCTION
Avulsion is the complete displacement of the tooth from the socket.[1] It is a severe form of injury that can occur as a result of sports-related injuries, domestic violence, falls, and road traffic accidents. Maxillary central incisors are the most commonly affected teeth with a slight male predilection.[2] Tooth avulsion results in the significant damage to the periodontal structures as well as the pulpal tissue. Several factors conglomerate toward the outcome of reimplantation such as patient's general health, the maturity of the root, the time the tooth is out of its socket, and storage medium.[3,4] The presence of viable periodontal ligament (PDL) cells on a hydrated tooth surface plays a significant role in the success of reimplantation cases. Furthermore, it is possible for new cementum formation to occur after the initial inflammation subsides.[5] For the above-mentioned reasons, reimplantation of an avulsed tooth with minimum extraoral time is advocated as the most appropriate treatment.
However, it might not always be possible for reimplantation to be done, within the speculated time frame, owing to determinants such as, patient ignorance and delay in seeking treatment. In such instances, especially when the avulsed tooth has long extraoral time without the use of a storage medium, the success rate dwindles.
Platelet-rich fibrin (PRF) is a second-generation platelet concentrate that is prepared from the patient's own blood without the use of anticoagulants and a single-step centrifugation process. It is classified as L-PRF or PRF based on leukocyte content; standard PRF, and advanced PRF depending on the centrifugation process and membrane or injectable form depending on the centrifugation process and consistency of the final product. PRF has the ability to enhance the tissue regeneration, accelerate wound-healing, and induce stem cell differentiation through its growth factors.[6] Further, it shows significantly longer release periods of platelet-derived growth factor (PDGF), epidermal growth factor, and insulin-like growth factor-1 compared to the earlier generation-platelet concentrates. Due to these properties, PRF has been extensively used in periodontal regeneration. This case report, to our knowledge is the first of its kind, in using I-PRF (injectable) in reimplantation of a maxillary central incisor with delayed periods of dry extraoral time.
CASE REPORT
A 21-year-oldfemale patient reported to Asan Memorial Dental College and Hospital, seeking treatment for her missing 11 [Figure 1]. She gave a history of trauma due to fall from a motorcycle, 4 days ago. On further probing, she revealed that she had kept the avulsed central incisor wrapped in a paper in her purse that she had left at home. The patient was conscious and cooperative, systemically healthy and did not exhibit any soft-tissue injury. The socket of 11 was examined and found to be devoid of any inflammation or infection. An orthopantamogram (OPG) and IOPA of the region showed no signs of alveolar fracture or pathology [Figure 2]. The patient was prescribed antibiotics – Amoxycillin 500 mg thrice a day (TID)for 5 days and metronidazole 400 mg twice a day (BID)for 5 days and instructed to place the tooth in milk solution and report the next day. A written consent was obtained from the patient following explanation of the intended procedure. The avulsed tooth was closely examined for intactness and presence of any foreign matter. Subsequently, it was cleansed using saline and betadine solution. Using a sterile curette, the PDL and calculus were removed. The socket was thoroughly rinsed with saline and 0.2% chlorhexidine gluconate, following which, i-PRF prepared from 5 ml of patient's own blood, centrifuged at 700 rpm for 3 min was directly injected into the socket. The avulsed tooth was re-implanted immediately and held in place for 5 min [Figure 3]. Flexible splint [Figure 4] was placed along with an acrylic stent [Figure 5] to avoid any occlusal interference during the healing phase. Postoperative instructions were given, and the patient was advised to rinse twice daily with 0.2% chlorhexidine gluconate and analgesic Ibuprofen 200 mg TID was prescribed for 3 days. Follow-up was done after a week during which time the acrylic stent was removed. Root canal treatment was completed during the same visit. Regular review at weekly intervals was done for a month. The splint was removed in the 4th week, and the tooth was tested for the signs of mobility and pain [Figure 6]. Frequent recall visits were scheduled every 3 months up to 1 year during which radiographs were taken, and the tooth was tested for the signs of mobility and any soft-tissue changes [Figures 7 and 8]. Adjacent tooth 21 showed periapical radiolucency when IOPA was taken for the avulsed tooth 11. The patient was informed that RCT had to be done, but since it was asymptomatic, she denied treatment and only wanted an esthetic filling for the fractured 21. Composite filling was given in 21, and the patient will be continued to be monitored for any signs of root resorption, infection, or ankylosis in 11 and any symptoms in relation to 21.
Figure 1.

Preoperative photograph
Figure 2.
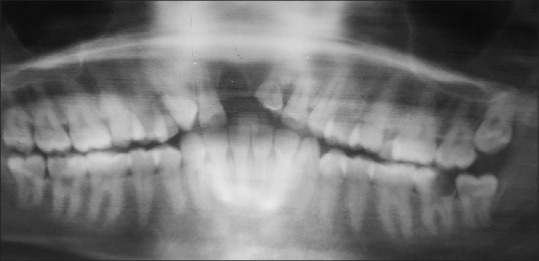
Pre op OPG
Figure 3.
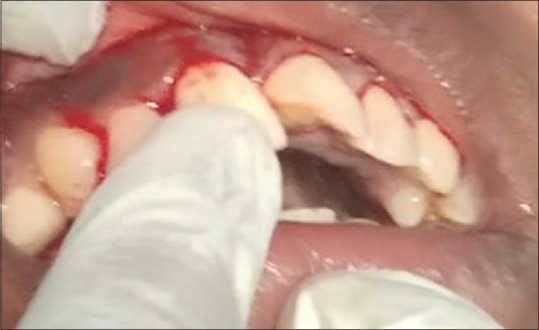
Re implantation of avulsed tooth
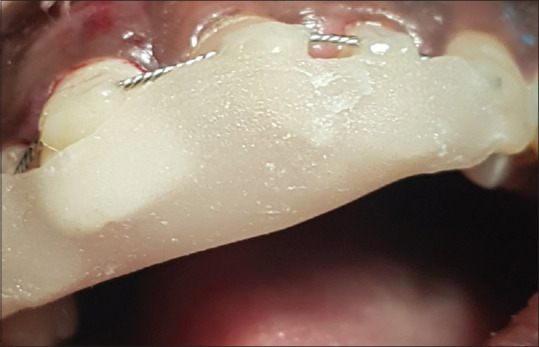
Figure 4.

Composite wire splinting
Figure 5.
Acrylic stent placed
Figure 6.

Four weeks post op photograph
Figure 7.
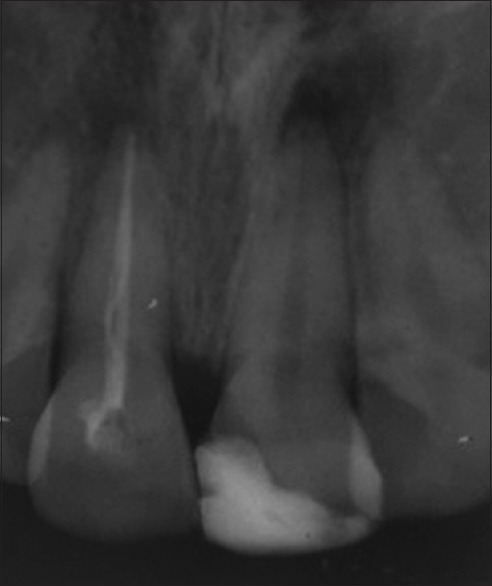
Post op IOPA 1 year
Figure 8.

1 year post op photograph
DISCUSSION
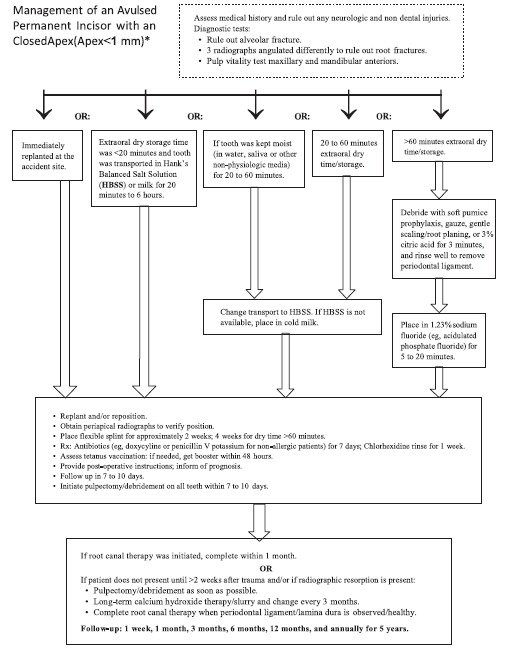
Most cases of avulsion occur as a result of trauma and commonly in the younger age groups. Lack of proper information and knowledge can result in improper storage of the avulsed tooth and delay in seeking professional treatment. The success and long-term prognosis of an avulsed tooth depends on the time lapse between avulsion and replantation. A decision tree has been proposed by McIntyre et al. for replantation of an avulsed permanent tooth to achieve the best possible outcome depending on the duration and storage form, i.e., dry or wet and the stage of root completion [Table 1].[7] The protocol for replantation described by the International Association of Dental Traumatology states that for a tooth that has been dry for more than 60 min, endodontic treatment can be done either extraorally or intraorally within 7–10 days. Since in this case, the root apex was completely closed, re-vascularization is unlikely and so the treatment was aimed at preventing or eliminating bacterial toxins from the root canal space by endodontic therapy.[8]
Table 1.
Decision Tree for delayed replantation of avulsed permanent tooth
 |
The long-term survival of a replanted tooth depends on the inflammatory and osseous root resorption that occurs as sequelae to delayed replantation cases. To slow down this process of osseous replacement or ankyloses from occurring, it is advocated to completely remove the remaining PDL that might act as a nidus of infection. Several treatment modalities to delay this outcome have been tried with finite success such as soaking the tooth in fluoride or tetracycline or doxycycline; use of Emdogain® to coat the entire root surface and usage of intracanal medicaments such as Ledermix.
The viability of PDL exposed to the extraoral environment, decreases rapidly after 18 min, making it necessary to reduce this time for successful replantation to occur.[9] However, so far no attempts have been made, to regenerate the degenerated PDL. In this case, PRF was used in the injectable form instead of the regular membrane form since it occupies less space and possesses better properties than the latter. Centrifuging blood at lower speeds causes the separation of platelets and significantly increases the number of leukocytes, platelets and growth factors compared to the conventional protocol. Injectable form of PRF also possesses the increased concentration of growth factors such as vascular endothelial growth factor and transforming growth factor (TGF-β1) required for angiogenesis and neovascularization as well as B- and T-lymphocytes, monocytes, and stem cells.[10] PRF stimulates cell proliferation in a specific manner.[11] It induces cell proliferation of osteoblasts, PDL cells, and growth factors, suppressing oral epithelial cell growth. It also contains and releases growth factors, such as PDGF, TGF-β that have a strong effect on the proliferation of gingival fibroblasts and osteoblasts.
Navarro et al., in their study, concluded that PRF provided increased cell viability in relation to the different dry extra alveolar times analyzed. Autologous PRF presented effectiveness in maintaining and recovering PDL cells from extracted teeth and kept dry for up to 2 h. This concept was used clinically in our patient with the aim of regenerating the PDL.[12]
In a study conducted by Tsai et al., it was established that a combination of PDL stem cells along with PRF, regenerated PDL such as tissues and reduced the occurrence of ankyloses and inflammation in replanted tooth with 2 h of dry storage time, compared to PRF alone.[13] In our case, since the extraoral dry time was very long, the degenerated PDL cells would not serve the purpose, and hence, PRF was used alone with the aim of regenerating the lost periodontium. To the best of my knowledge, no reports have shown the use of injectable form of PRF in the treatment of an avulsed permanent tooth which has an extended extra oral dry period with a successful outcome.
CONCLUSION
Although delayed replantation is not considered as an “ideal” conventional treatment option, the advent of superior biomaterials that can promote physiological events of regeneration has increased the survival rates of such a treatment modality. Delayed replantation has several advantages such as reduced chairside time and nonsurgical manipulation and most importantly the privilege of retaining the patient's natural tooth, making it a good treatment option. However, the long-term prognosis of delayed replantation using PRF needs to be established through further studies in this direction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Andreasen JO, Andreasen FM. Classification, etiology and epidemiology. In: Andreasen JO, editor. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 3rd ed. St. Louis: Mosby; 1994. pp. 151–79. [Google Scholar]
- 2.Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: A review of the literature. Aust Dent J. 2000;45:2–9. doi: 10.1111/j.1834-7819.2000.tb00234.x. [DOI] [PubMed] [Google Scholar]
- 3.Ram D, Cohenca N. Therapeutic protocols for avulsed permanent teeth: Review and clinical update. Pediatr Dent. 2004;26:251–5. [PubMed] [Google Scholar]
- 4.Savas S, Kucukyilmaz E, Akcay M, Koseoglu S. Delayed Replantation of Avulsed Teeth: Two Case Reports. Case Reports in Dentistry Vol. 2015 doi: 10.1155/2015/197202. Article ID 197202, 5s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goswami M, Chaitra T, Chaudhary S, Manuja N, Sinha A. Strategies for periodontal ligament cell viability: An overview. J Conserv Dent. 2011;14:215–20. doi: 10.4103/0972-0707.85789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chandran P, Sivadas A. Platelet rich-fibrin: Its role in periodontal regeneration. Saudi J Dent Res. 2014;5:117–22. [Google Scholar]
- 7.McIntyre JD, Lee JY, Trope M, Vann WF., Jr Permanent tooth replantation following avulsion: using a decision tree to achieve the best outcome. Pediatr Dent. 2009;31(2):137–144. [PubMed] [Google Scholar]
- 8.McIntyre JD, Lee JY, Trope M, Vann WF., Jr Permanent tooth replantation following avulsion: Using a decision tree to achieve the best outcome. Pediatr Dent. 2009;31:137–44. [PubMed] [Google Scholar]
- 9.Marouane O, Turki A, Oualha L, Douki N. Tooth replantation: An update. Med Buccale Chir Buccale. 2017;23:103–10. [Google Scholar]
- 10.Arora R, Shukla S. Injectable-platelet-rich fibrin-smart blood with stem cells for the treatment of alopecia: A report of three patients. Int J Trichology. 2019;11:128–31. doi: 10.4103/ijt.ijt_73_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deshpande NM, Shah D, Wadekar S. Maintenance of cell viability in extraoral conditions for a case of intentional replantation to retrieve a separated endodontic instrument. J Conserv Dent. 2019;22:207–12. doi: 10.4103/JCD.JCD_461_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navarro LB, Barchiki F, Navarro Junior W, Carneiro E, da Silva Neto UX, Westphalen VPD. Assessment of platelet-rich fibrin in the maintenance and recovery of cell viability of the periodontal ligament. Sci Rep. 2019;9:19476. doi: 10.1038/s41598-019-55930-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsai CH, Shen SY, Zhao JH, Chang YC. Platelet-rich fibrin modulates cell proliferation of human periodontally related cells in vitro. J Dent Sci. 2009;4:130–5. [Google Scholar]


