Abstract
The present study explored whether distress reduction in response to strong negative emotions, a putative transdiagnostic mechanism of action, is facilitated by mindfulness strategies. Seven patients (mean age = 31.14 years, SD = 12.28, range 19–48 years, 43% female, 86% Caucasian) with heterogeneous anxiety disorders (i.e., panic disorder with or without agoraphobia, social anxiety, generalized anxiety) were assigned a randomized order of weeklong blocks utilizing either mindfulness- or avoidance-based strategies while ascending a 6-week emotion exposure hierarchy. Participants completed three exposures per block and provided distress and avoidance use ratings following each exposure. Anxiety severity, distress aversion, and distraction/suppression tendencies were also assessed at baseline and the conclusion of each block. Visual, descriptive, and effect size results showing exposures utilizing mindfulness were associated with higher overall distress levels, compared with those utilizing avoidance. Within blocks, the majority of participants exhibited declining distress levels when employing mindfulness strategies, as opposed to more static distress levels in the avoidance condition. Systematic changes in anxiety severity, distress aversion, and distraction/suppression were not observed. These results suggest mindfulness strategies may be effective in facilitating emotion exposure; however, a minimum dosage may be necessary to overcome initial distress elevation. Potential transdiagnostic change mechanisms and clinical implications are discussed.
Keywords: transdiagnostic, mindfulness, exposure, treatment mechanisms, single-case experimental design
ANXIETY, DEPRESSIVE, AND RELATED emotional disorders (e.g., obsessive–compulsive disorders [OCDs], posttraumatic stress disorder, eating disorders) are prevalent, costly, and debilitating to daily functioning and quality of life (Barlow, 2002). Disorders within these diagnostic classes are highly comorbid, with lifetime comorbidity estimates as great as 81% (Brown, Campbell, Lehman, Grisham, & Mancill, 2001). An emerging literature indicates that this high rate of co-occurrence may be the result of a shared propensity toward the experience and intolerance of negative emotions (i.e., neuroticism), suggesting these conditions are phenotypically diverse expressions of a common syndrome (Brown, Chorpita, & Barlow, 1998). This neurotic vulnerability has been implicated in the development and maintenance of these “emotional disorders,” often leading to strong aversive reactions to negative emotional experience (Barlow, 2000; Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014). As a result, individuals with these disorders may attempt to reduce or avoid negative emotions by engaging in strategies that might initially succeed but often backfire (Mogg, Bradley, Miles, & Dixon, 2004), paradoxically exacerbating distress, symptoms, and neurotic temperament (Fledderus, Bohlmeijer, & Pieterse, 2010; Venta, Sharp, & Hart, 2012).
These commonalities suggest emotional disorders may be effectively treated via a transdiagnostic approach targeting shared maintenance factors. Recent years have seen a proliferation in treatments designed to address mental illness across diagnostic categories (e.g., Barlow, Ellard, et al., 2011a; Barlow, Farchione, et al., 2011b; Fairburn, Cooper, & Shafran, 2003); however, little research has explored the mechanisms by which these transdiagnostic interventions operate. Treatment mechanism research is essential for establishing the utility of transdiagnostic protocols, strengthening psycho-pathological theory, and advancing future research and therapies. Though various treatments have shown effective outcomes across disorders, transdiagnostic interventions grounded in a core rationale for disorder maintenance provide an ideal framework for mechanistic research.
The unified protocol for transdiagnostic treatment of emotional disorders (UP; Barlow, Ellard, et al., 2011a; Barlow, Farchione, et al., 2011b) is one such intervention built upon core transdiagnostic theory to address emotional disorders. Specifically, the UP purportedly targets underlying neuroticism by facilitating extinction of distress in response to strong emotions, leading to reduced emotional avoidance and, consequently, disorder symptoms. Across various skills modules, patients are taught to cultivate emotional acceptance in an effort to reduce reliance on maladaptive avoidant coping; less avoidant coping, in turn, leads to fewer instances of avoided emotions rebounding with increased frequency and intensity. Preliminary evidence has supported the UP’s targeted approach across emotional disorders for reducing both symptoms and neuroticism itself (Carl, Gallagher, Sauer-Zavala, Bentley, & Barlow, 2014; Farchione et al., 2012).
The UP’s putative mechanism of action, extinction of distress during strong emotional experience, has not yet been systematically tested. The UP consists of five core skills modules: (a) emotion awareness training, (b) cognitive appraisal and reappraisal, (c) emotion avoidance and emotion-driven behaviors, (d) awareness and tolerance of physical sensations, and (e) interoceptive and situation-based emotion exposures (see Payne, Ellard, Farchione, Fairholme, & Barlow, 2014, for details). However, two of these modules may be particularly relevant for targeting this putative mechanism in practice. First, mindfulness (emotion awareness) training may encourage patients to nonjudgmentally accept present-moment experiences through experiential exercises. Mindful awareness of distressing thoughts, emotions, or sensations in the absence of dire consequences hypothetically teaches individuals that emotions are not harmful, reducing reliance on avoidant coping strategies that ultimately worsen distress (Craske & Barlow, 2007). Mindfulness skills have demonstrated negative associations with neuroticism (Baer, Smith, & Allen, 2004; Giluk, 2009), and recent work by Boswell, Anderson, and Barlow (2014) found that increases in mindfulness temporally preceded decreases in anxious and depressive symptoms during UP treatment. Research further suggests that increased emotional acceptance mediates the relationship between mindfulness practice and the tendency to experience negative emotions (van den Hurk et al., 2011).
The final core module, emotion exposure, may also be particularly effective in extinguishing distress from emotional experience. Based on conditioning principles, exposure therapy encourages patients to repeatedly confront emotion-provoking situations with the goal of reducing distress associated with these experiences. Exposure procedures have been linked to symptom improvement across a range of anxiety disorders (Barlow, Allen, & Basden, 2007; Lindsay, Crino, & Andrews, 1997) and are based on a number of established learning theories. For example, emotional processing theory (Foa & Kozak, 1986) proposes that activating negative emotional responses via feared stimuli (i.e., fear activation) allows the distressed individual to habituate to the feared stimuli. Additionally, belief (or expectancy) disconfirmation theory (Salkovskis, Clark, Hackmann, Wells, & Gelder, 1999) holds that the greatest benefits of exposure are garnered when patients actively seek to disconfirm catastrophic beliefs and counter safety behaviors that may reinforce these beliefs. Accumulating evidence has shown greater improvements in anxiety symptoms and avoidance tendencies when exposure procedures maximize belief disconfirmation, as opposed to utilizing emotional processing alone (Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014; Salkovskis, Hackmann, Wells, Gelder, & Clark, 2007).
In the UP, exposure procedures emphasize facing and tolerating strong emotions, rather than the situations that elicit them; type and content of exposures are of secondary importance as long as sufficient emotional intensity is reached. Thus, UP exposure procedures may draw from a wide array of emotion-eliciting stimuli: in vivo exposures that focus on situations that lead to strong emotions (e.g., taking public transportation, being assertive), interoceptive exposures that induce physical sensations associated with distress (e.g., shortness of breath, dizziness; Barlow, 2002; Boswell et al., 2013), and imaginal exposures that are used for situations that cannot be readily or ethically simulated (e.g., getting fired, harming another person; Koerner & Fracalanza, 2012).
In a recent review, Craske and colleagues (2014) enumerated several factors that appear to enhance exposure efficacy: identifying and eliminating safety behaviors, focusing on fear-inducing stimuli, labeling emotions during exposure, and varying the intensity and duration of exposures. Conversely, exposures lacking these elements may be hindered in their effectiveness. The present-focused attention and nonjudgmental awareness inherent in mindfulness may then be ideal prerequisites for maximizing each of these effective exposure factors. Previous research has suggested that mindfulness-based strategies reduce experiential avoidance (Roemer et al., 2009) and produce improved clinical outcomes in anxiety and depressive disorders (Boswell et al., 2014; Wahl, Huelle, Zurowski, & Kordon, 2013). Mindfulness strategies may facilitate fully experiencing emotions during exposure, thereby accelerating distress reduction and sustaining beneficial outcomes across disorders maintained by neuroticism and avoidance. Reminiscent of previous work utilizing interoceptive exposure for feared physical sensations (Craske & Barlow, 2007), emotion exposures utilizing mindfulness encourage attention and nonjudgmental acceptance toward negative emotions (rather than cognitive restructuring or experiential habituation), allowing individuals to learn that distressing emotions are harmless and can be tolerated without dire consequence (Baer, 2003).
Confirming such a putative mechanism of action is a crucial step in further advancing and disseminating transdiagnostic treatment for emotional disorders. Single-case experimental design is a research methodology well suited to the exploration of mechanisms. Alternating treatment designs (ATDs; Barlow & Hayes, 1979) are a form of single-case design structured such that two interventions are administered to each participant in an alternating fashion, allowing for comparison of these strategies on outcomes within the individual. This strategy controls for threats to internal validity, since any change witnessed between conditions must be due to the condition variable and not extraneous factors such as history, maturation, or regression to the mean (Barlow, Nock, & Hersen, 2009). Visual analysis allows the researcher to identify preliminary evidence for condition differences through consistent nonoverlap, trend, and covariation in phase data (Kratochwill et al., 2010). Recent years have also seen a proliferation of quantitative methods to evaluate single-case design types (see Smith, 2012, for a review), and in conjunction with visual inspection, these techniques offer a wide range of supplemental tools for quantifying and communicating observed effects.
The present study utilized an exposure-based ATD to test whether mindfulness strategies were superior to emotional avoidance strategies in facilitating the putative mechanism of action in the UP: extinction of distress during negative emotional experience. Because emotional avoidance mirrors behaviors often employed by emotional disordered individuals to manage negative emotions, support for the UP’s proposed mechanism depends upon both lack of evidence for distress reduction using avoidance strategies, as much as evidence supporting use of mindfulness strategies. Our first goal was to determine whether individuals with a range of anxiety disorders could effectively be trained to utilize mindfulness strategies while engaging in emotion exposures. We hypothesized that mindfulness strategies would lead to reduced use of avoidance strategies during negative emotional experience. Our second goal was to determine if phases utilizing “mindful exposure” lead to reduced subjective distress, anxiety severity, and experiential avoidance, as compared with “avoidance exposure” phases. We hypothesized that individuals would report decreases in all three variables following mindful (rather than avoidance) exposure. Last, we aimed to explore patterns of change across both exposure strategies in order to uncover potential factors influencing strategy use and function during the treatment process. As we are not aware of previous research examining these strategies in this context, we withheld any a priori hypotheses.
Method
PARTICIPANTS
Participants were recruited from a pool of individuals seeking treatment at the Center for Anxiety and Related Disorders (CARD) at Boston University (BU). The study was fully approved by the BU Institutional Review Board. Inclusion criteria included a principal diagnosis of social anxiety disorder (SOC), panic disorder with or without agoraphobia (PD/A), generalized anxiety disorder (GAD), or OCD, based on a clinician-administered assessment using the Anxiety Disorders Interview Schedule for DSM-IV-Lifetime Version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994; see description below). Participants were also required to be 18 years of age or older, fluent in English, provide informed consent, and possess the ability to complete all study sessions and assessments. Individuals with comorbid diagnoses, including all anxiety disorders and depression, were accepted, and individuals currently on psychotropic medications were included if agreeing to a stable dosage throughout the study.
Exclusion criteria prioritized participant safety and well-being, and included clinical conditions warranting immediate or alternative treatment. Specifically, exclusion criteria included Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV; American Psychiatric Association, 1994) diagnoses for bipolar disorder, schizophrenia, schizoaffective disorder, or organic mental disorder, as well as current suicidal risk and current or recent history of substance abuse or dependence within the past 3 months. Furthermore, individuals electing to continue ongoing psychotherapy during the study period were excluded.
A total of seven individuals consented to procedures and were randomized to a predetermined order of alternating mindfulness and avoidance conditions, balanced across a 6-week study period. Participants consisted of four males and three females, with a mean age of 31.14 years (SD = 12.28, range 19–48 years). The study sample was primarily Caucasian (86%, n = 6), with one participant identifying as Asian (14%, n = 1). Principal diagnoses for each participant are shown in Figure 1. Of the seven participants initially enrolled, five completed study procedures. Two participants were deemed unable to complete study procedures (described below) and ultimately withdrawn and provided with follow-up treatment through CARD.
FIGURE 1.
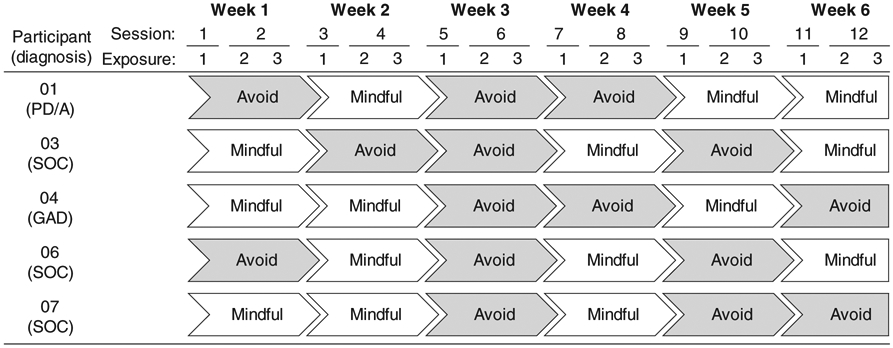
Strategy randomization by participant. Weeks represent single blocks. PD/A = panic disorder with or without agoraphobia; SOC = social anxiety disorder; GAD = generalized anxiety disorder.
MEASURES
Clinician Ratings
Intake diagnoses were assessed with the ADIS-IV-L (DiNardo et al., 1994) prior to enrollment. This semistructured, diagnostic clinical interview focuses on DSM-IV diagnoses of anxiety disorders and their accompanying mood states, somatoform disorders, and substance and alcohol use. Principal and additional diagnoses receive a clinical severity rating (CSR) on a scale from 0 (no symptoms) to 8 (extremely severe symptoms), with a rating of 4 or higher (definitely disturbing/disabling) meeting DSM-IV diagnostic criteria. This measure has demonstrated acceptable to excellent interrater reliability for the anxiety and mood disorders (Brown, DiNardo, Lehman, & Campbell, 2001).
Change Measures
The Subjective Units of Distress Scale (SUDS; Wolpe, 1969) is an intersession rating scale designed to measure subjective distress severity during and across exposure sessions. Participants rate subjective feelings of distress on a 0- to 10-point scale. In the present study, averages of participants’ SUDS ratings were recorded for each exposure.
The Multidimensional Experiential Avoidance Questionnaire (MEAQ; Gámez, Chmielewski, Kotov, Ruggero, & Watson, 2011) is a 62-item scale designed to assess the tendency to avoid negative internal experience (thoughts, emotions, physical sensations). The degree to which participants agree with each item is rated on a 6-point Likert-type scale, with higher scores indicating greater avoidance. In the present study, only the 13-item Distress Aversion (DA) subscale and 7-item Distraction/Suppression (D/S) subscale were collected. The measure and these subscales have exhibited good internal consistency and a high degree of convergent and discriminant validity (Gámez et al., 2011). Although change sensitivity has yet to be extensively validated, Gámez and colleagues have noted the potential for subscale responsiveness to targeted treatment approaches.
The Overall Anxiety Severity and Impairment Scale (OASIS; Norman, Hami-Cissell, Means-Christensen, & Stein, 2006) is a brief five-item questionnaire that was developed as a continuous measure of anxiety-related symptom severity and impairment that may be used across anxiety disorders, with multiple anxiety disorders, and with subthreshold anxiety symptoms. This measure has good internal consistency, excellent test-retest reliability, and convergent and discriminant validity (Norman et al., 2011). Previous research has shown the OASIS possesses good sensitivity to temporal changes in anxiety severity and impairment during treatment administration (Boswell et al., 2014; Joesch et al., 2013).
Adherence Check
The Responses to Emotions Questionnaire (REQ; Campbell-Sills, Barlow, Brown, & Hofmann, 2006) is an eight-item scale assessing the degree to which individuals use different emotion regulation strategies during emotion-eliciting tasks. The measure contains four items relevant to avoiding or changing emotional experience (e.g., “I tried to hold back or suppress my emotional reactions”) and four items relating to awareness and acceptance of emotional experience (e.g., “I recognized what I was feeling during the exercises but didn’t try to change what I was feeling”). Participants rate their degree of strategy use from 0 (not at all) to 10 (all the time). In the present study, three of the four mindfulness (awareness/acceptance) items were reverse scored and combined with all four avoidance items to create a mean composite “avoidance use” score. This composite score served as a manipulation check for adherence to condition instructions. The content of one mindfulness item (“I didn’t mind feeling uncomfortable during the exercises”) was judged to be conceptually similar to distress level, an outcome variable of interest, and therefore excluded from our mean composite score.
PROCEDURE
Participants were asked to complete 12 one-hour exposure sessions over 6 weeks. Each week (or block), participants were instructed to utilize either mindfulness- or avoidance-based strategies while engaging in emotion exposures. Participants were assigned a randomized order of mindfulness and avoidance exposure blocks prior to the first session, balanced such that three mindfulness blocks and three avoidance blocks occurred over the course of the study, with no more than two consecutive blocks of the same condition. Block exposures took place over two sessions, with one exposure occurring in the first session and two exposures occurring in the second session (see Figure 1). Participants were told the study aimed to test two different strategies of coping more effectively with emotions in order to ascertain the most effective strategy for them. Both strategies were presented as credible methods of managing distressing emotions, and participants were explicitly informed that the study contained elements of treatment but was not equivalent to formal therapy (i.e., the UP).
Within mindfulness-based blocks, participants were instructed to experience their emotions during exposure (including thoughts, physical feelings, and urges to act) without engaging in efforts to escape or avoid their experience; examples of how patients might attend to their internal experience were provided (e.g., “Bring an attitude of openness to observing the thoughts that are in your mind,” “Notice your thoughts without having to react to them,” “Observe the sensations in your body with curiosity and interest”). In contrast, avoidance-based blocks asked participants to reduce any emotions experienced during exposure by pushing them out of awareness. Participants were encouraged to keep emotion levels as low as possible and were provided with strategies to assist them in this goal (e.g., “If you notice distressing thoughts, focus your attention on something else,” “Try to hold back or suppress any emotions you may be having,” “Try to focus your attention away from any physical sensations that you notice”).
Clinicians for the study were three licensed doctoral-level psychologists. The study’s initial session was allotted extra time for clinicians to assist participants in constructing a fear and avoidance hierarchy (fully described in the UP therapist guide; Barlow, Farchione, et al., 2011b). Participants were asked to rank these situations by severity of emotional distress. At the start of each successive block, participants ascended their fear hierarchy, and clinicians aided in designing idiographic exposures to be used throughout each block. For homework between blocks, participants were asked to continue utilizing the strategy employed in the most recent session. Clinicians were instructed to encourage each strategy’s use during respective blocks and avoid reinforcing comments in response to participants’ preference or experience. Study staff also met weekly to discuss participant progress and monitor clinician adherence.
Participants completed baseline OASIS and MEAQ measures at the start of the first session; these same measures were subsequently administered at the conclusion of each block (i.e., after each block’s second session). Following each exposure, individuals were asked to rate their average SUDS level during the exposure. Participants also completed the REQ immediately after exposures and at the start of each new block, serving as a manipulation check for cognitive strategy use both in-session and during homework periods. An odd number of homework periods resulted in one fewer REQ rating for the final block.
PROCEDURAL CHANGES
Initially, imaginal exposures were administered exclusively while ascending the participant’s fear hierarchy, and clinician and participant collaborated in constructing personalized scripts to be read aloud during exposures. While imagining these scenarios, participants were asked to employ the appropriate block strategy when experiencing distress. A minimum average SUDS rating of 5 was required during the first block exposure in order to ensure an adequate level of baseline distress.
Participant 01 completed the study within this framework. However, Participant 02 reported difficulty imagining script content during initial exposures and was unable to achieve this minimum SUDS rating, resulting in early withdrawal and referral to individual therapy. Following this withdrawal, we elected to revise procedures in order to allow for multiple types of exposure within sessions. Although only imaginal exposure would be utilized initially, interoceptive and in vivo exposures could be incorporated as needed in the first block exposure to achieve sufficient fear activation. After these revisions, only one withdrawal occurred (Participant 05) because minimum SUDS were not achieved through imaginal plus interoceptive exposures, and adding in vivo exposures was infeasible due to specific contextual requirements.
These changes were deemed appropriate for several reasons. First, systematic between-subject changes in single-case research are often an important and necessary step in the context of discovering treatment mechanisms. Furthermore, these procedural changes did not affect this investigation’s focus on intrasubject variability. Finally, because the UP focuses on exposure to emotions rather than explicit content, exposure type should be inconsequential so long as a moderate level of distress is achieved. So although only Participants 03, 04, 06, and 07 completed the study with these updated procedures in place, all study completers (including Participant 01) experienced the required distress levels during emotion exposures. Thus, these changes still allowed for comparison of processes across participants, while simultaneously providing greater flexibility and improved engagement in both conditions.
DATA ANALYTIC APPROACH
Analysis for the present study was conducted in several phases using a combination of visual interpretation, descriptive statistics, and single-case effect size estimates. Visual interpretation was first utilized to evaluate level differences in REQ and SUDS by condition, as well as functional relationships among these variables over time. Condition means and degree of change were evaluated to confirm visual results and more closely examine condition effects for each participant. We followed these descriptives with effect size measures of condition difference for both REQ and SUDS (Hedges, Pustejovsky, & Shadish, 2012). This adapted Hedges’s g for single-case design contrasts condition means across multiple cases to provide a statistic comparable to Cohen’s d, adjusting for small sample bias. Finally, OASIS and MEAQ subscale scores were compared from baseline to the final block of each condition, with normative cutoff scores provided to determine if clinically significant reductions had occurred.
Results
STRATEGY ADHERENCE
Figure 2 provides visual displays of participants’ avoidance strategy use. Separate line graphs represent patterns of mean-level change for each condition, both in-session and during homework periods. Ideally, participants would provide higher scores during avoidance conditions, compared to low scores for mindfulness phases. Visual inspection suggested the majority did adhere to block instructions, particularly in session. Additionally, three participants (01, 03, and 06) showed greater separation between conditions as the study progressed, indicating continued improvement in strategy use. One participant (04) displayed little line separation, suggesting potential difficulties employing both strategies consistently. Finally, the graphs were also examined for congruency between in-session and homework adherence. Here, two participants (01 and 07) appeared to deviate on block instructions during homework periods, yet each deviated in a unique manner. Whereas 01 shifted to moderate avoidance use during mindfulness homework, 07 reverted to low avoidance use during the final avoidance homework.
FIGURE 2.
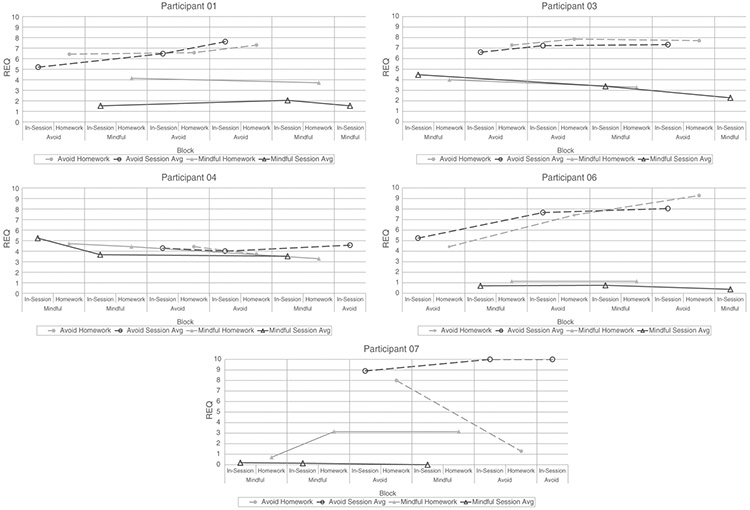
REQ (Responses to Emotions Questionnaire) by block. Higher scores indicate greater avoidance use.
Table 1 provides condition mean scores of avoidance use, as well as the difference between homework and in-session means for each condition. In line with visual analysis, the majority of participants demonstrated higher avoidance use in and out of session during avoidance conditions, as compared to mindfulness conditions. The only exception (04) used moderate amounts of avoidance across both conditions.
Table 1.
Avoidance Use (REQ) Between and During Blocks
| Participant | Strategy | Homework Mean |
Session Mean |
Difference Score |
|---|---|---|---|---|
| 01 (PD/A) | Avoid | 6.76 | 6.43 | 0.33 |
| Mindful | 3.93 | 1.70 | 2.23 | |
| 03 (SOC) | Avoid | 7.62 | 7.06 | 0.56 |
| Mindful | 3.64 | 3.38 | 0.26 | |
| 04 (GAD) | Avoid | 4.07 | 4.29 | −0.21 |
| Mindful | 4.14 | 4.14 | 0.00 | |
| 06 (SOC) | Avoid | 7.05 | 6.98 | 0.06 |
| Mindful | 1.14 | 0.62 | 0.52 | |
| 07 (SOC) | Avoid | 4.64 | 9.63 | −4.99 |
Note. Higher scores indicate more avoidance use. REQ = Responses to Emotions Questionnaire; PD/A = panic disorder with or without agoraphobia; SOC = social anxiety disorder; GAD = generalized anxiety disorder.
Table 1 also provides difference scores for homework and in-session means, revealing any discrepancies in adherence within versus outside of session. Greater difference scores in either direction indicate greater deviance between the two settings. Consistent with visual analyses, two participants (01 and 07) each showed notable discrepancies in and out of session. Last, a standardized mean difference effect size was calculated to determine if the observed differences between conditions in session avoidance use were statistically significant across all cases. Avoidance use was shown to be significantly higher in avoidance versus mindfulness blocks across the five participants, g = 2.1, s2 = .86, p < .05.
SUBJECTIVE DISTRESS
Figure 3 displays average SUDS for each participant during exposure sessions. Isolated data points represent individual exposures, whereas line graphs for both strategies connect block averages (comprising the three proximal within-block exposure ratings). These line graphs provide broad patterns of change in average SUDS across condition blocks. Visual inspection suggested that for most participants (01, 03, 06, and 07), SUDS averages in mindfulness blocks appeared to be systematically higher than avoidance blocks. However, some participants (01 and 07) showed only slight separation between lines, indicating differences may not be consistent across all cases. Additional inspection revealed varying participant trends of downward, static, or increasing exposure ratings within each block—findings that we explored further below.
FIGURE 3.
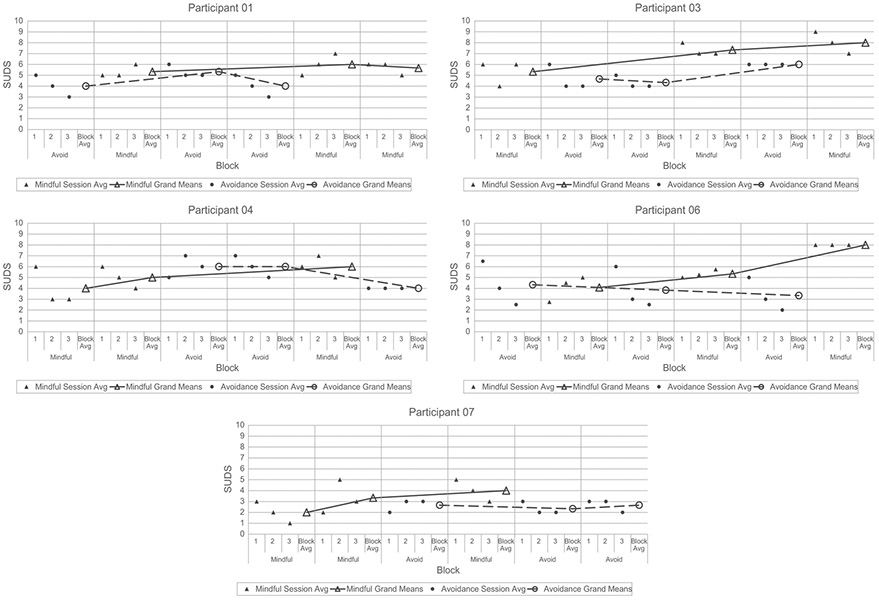
Average SUDS (Subjective Units of Distress Scale), both within- and across block. Higher scores indicate greater distress.
Table 2 provides strategy grand means for SUDS ratings over the course of the study, as well as mean changes in distress at the across- and within-block levels. These last two columns provide summary statistics to supplement the visual analyses of block lines and individual exposure points, respectively. Mean changes were calculated by averaging SUDS change from block to block (across blocks) or exposure to exposure (within blocks).
Table 2.
Mean Level and Change in Average Distress (SUDS)
| Participant | Strategy | Grand Mean |
Mean Change Across Blocks |
Mean Change Within Blocks |
|---|---|---|---|---|
| 01 (PD/A) | Avoid | 4.44 | 0.00 | −0.83 |
| Mindful | 5.67 | 0.17 | 0.33 | |
| 03 (SOC) | Avoid | 5.00 | 0.75 | −0.50 |
| Mindful | 6.89 | 1.33 | −0.50 | |
| 04 (GAD) | Avoid | 5.33 | −1.00 | −0.17 |
| Mindful | 5.00 | 1.00 | −1.00 | |
| 06 (SOC) | Avoid | 3.83 | −0.50 | −1.75 |
| Mindful | 5.81 | 1.96 | 0.50 | |
| 07 (SOC) | Avoid | 2.56 | −0.17 | −0.17 |
| Mindful | 3.11 | 1.00 | −0.50 |
Note. Bolded numbers indicate superior condition. SUDS = Subjective Units of Distress Scale; PD/A = panic disorder with or without agoraphobia; SOC = social anxiety disorder; GAD = generalized anxiety disorder.
Over the 6-week study, four participants (01, 03, 06, and 07) exhibited less distress, on average, during avoidance as compared to mindfulness conditions. Participant 04 was the single exception, exhibiting slightly less distress, on average, during mindfulness blocks. However, all participants experienced increases in mean distress levels from the first to third mindfulness block, compared with varied patterns across avoidance blocks. A standardized mean difference effect size was calculated to test the magnitude of strategy effect on overall distress across all five cases. Consistent with visual inspection and descriptives, overall distress levels were shown to be significantly higher in mindfulness versus avoidance strategies, g = .62, s2 = .05, p < .01.
When examining mean changes in distress at the exposure (within blocks) level, participants varied in superior strategy for distress reduction. Two participants (01 and 06) experienced distress reductions within avoidance blocks but increases within mindfulness blocks from first to third exposures. Conversely, two other participants (04 and 07) evidenced greater reductions within mindfulness blocks compared to avoidance blocks. Participant 03, however, displayed equivalent mean change patterns within both strategy blocks.
ANXIETY SEVERITY AND EXPERIENTIAL AVOIDANCE
Table 3 displays participants’ baseline and final block scores for each condition on the OASIS and separate MEAQ subscales. Clinical cutoff scores for each scale are also provided from existing normative data in order to evaluate clinically significant reductions from baseline.
Table 3.
Baseline and Final Block Scores for MEAQ Subscales and OASIS
| MEAQ DA |
MEAQ D/S |
OASIS |
|||||
|---|---|---|---|---|---|---|---|
| Cutoff ≥ 41 |
Cutoff ≥ 25 |
Cutoff ≥ 7 |
|||||
| Participant | Strategy | Baseline | Final Block | Baseline | Final Block | Baseline | Final Block |
| 01 (PD/A) | Avoid | 52 | 51 | 31 | 30 | 6 * | 9 |
| Mindful | 49 | 26 | 8 | ||||
| 03 (SOC) | Avoid | 60 | 52 | 31 | 36 | 13 | 8 |
| Mindful | 46 | 28 | 11 | ||||
| 04 (GAD) | Avoid | 43 | 27 * | 28 | 29 | 7 | 7 |
| Mindful | 30 * | 29 | 8 | ||||
| 06 (SOC) | Avoid | 55 | 42 | 30 | 29 | 8 | 5 * |
| Mindful | 48 | 35 | 10 | ||||
| 07 (SOC) | Avoid | 38 * | 30 * | 34 | 33 | 3 * | 3 * |
| Mindful | 31 * | 27 | 3 * | ||||
Note. MEAQ DA = Multidimensional Experiential Avoidance Questionnaire–Distress Aversion; MEAQ D/S = Multidimensional Experiential Avoidance Questionnaire–Distraction/Suppression; OASIS = Overall Anxiety Severity and Impairment Scale; Cutoff = threshold scores separating clinical from subclinical levels (Gámez et al., 2011; Norman et al., 2011); PD/A = panic disorder with or without agoraphobia; SOC = social anxiety disorder; GAD = generalized anxiety disorder.
Subclinical score.
Upon inspection, only Participant 04 exhibited a clinically meaningful reduction in distress aversion. Participants 03 and 07 also achieved notable reductions in distress aversion; however, 03 concluded the study at clinical levels, whereas 07 actually began the study at baseline subclinical levels. There were also no apparent distinctions in distress aversion changes between conditions. Furthermore, none of the participants showed systematic changes in distraction/suppression tendencies. On the OASIS, only 06 scored significantly lower on the final avoidance block, whereas 01 elevated from subclinical to clinical levels in both conditions.
Discussion
A strong foundation in transdiagnostic theory is essential in order to develop novel treatment research, enhance treatment strategies, and effectively target underlying vulnerabilities among disorders. The UP is an extension of this bottom-up approach, designed to treat common neurotic tendencies in emotionally disordered individuals by extinguishing distress associated with strong negative emotions. By isolating two core UP modules, our study aimed to test the potential for mindfulness-based strategies to facilitate this putative mechanism of action. We initially hypothesized that (a) mindfulness strategies would lead to less avoidance during negative emotional experience, and (b) mindful exposure would lead to less subjective distress and consequentially less anxiety severity and experiential avoidance, as compared to avoidance exposure. In line with our first hypothesis, analyses indicated that participants successfully used fewer avoidance strategies following mindfulness instruction. In fact, all participants either maintained or continued to reduce their avoidance use with each successive mindfulness block. Contrary to our second hypothesis, results demonstrated no apparent differences between strategies on anxiety severity and experiential avoidance. Furthermore, mean levels of subjective distress were found to be significantly greater across mindfulness blocks, as compared to avoidance blocks. However, several interesting observations emerged from changes in distress level both within strategy blocks and across the course of the study.
STRATEGY INSTRUCTION AND ADHERENCE
Results clearly indicated most participants differed between conditions in the expected directions for in-session avoidance use, despite minor deviations during homework. Only Participant 04 showed little deviation, suggesting potential difficulty in differentiating assigned strategies. However, 04’s generally low avoidance use suggests this participant may have been inclined toward mindfulness strategies. Noting caution in interpretation of 04’s data, we next investigated whether in-session versus homework avoidance use revealed patterns that might have contributed to our null findings elsewhere.
Participants 01 and 07 in particular showed lower adherence to block strategy during homework, compared to in-session exposures; specifically, Participant 01 deviated frequently during mindfulness strategy homework, whereas Participant 07 deviated for avoidance strategies, using virtually no avoidance strategies during the final avoidance homework. When considered in conjunction with subjective distress, Participant 01 had also previously been more successful at reducing distress when utilizing avoidance strategies. Conversely, Participant 07 experienced greater distress reduction during past mindful exposures. In both circumstances, participants may have either deliberately or automatically reverted to the more successful strategy. Furthermore, participant 07’s shift away from avoidance use after multiple mindfulness exposures may indicate a need for more thorough mindfulness instruction prior to exposures in order to significantly facilitate treatment change.
Unlike sessions within the UP and other protocols, study sessions did not develop mindfulness strategies prior to initiating exposures. Additionally, homework instructions encouraged continued strategy use but did not assess frequency or duration of use. Even for participants who showed better adherence, quality of strategy use may still have suffered. Extant research assessing mindfulness instruction has revealed that structured practice, rather than informal practice or frequency of practice, significantly reduces rumination and depressive symptoms within mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) protocols (Hawley et al., 2014). Alternatively, frequency of between-session practice in MBCT has also been connected with fewer anxiety and depression symptoms for individuals with bipolar disorder (Perich, Manicavasagar, Mitchell, & Ball, 2013). Future research may benefit from closer attention to instruction guidelines, including quantity and quality of work, to determine standards for facilitating change mechanisms across diagnoses.
CHANGES IN DISTRESS AND EXPERIENTIAL AVOIDANCE
Contrary to our second hypothesis, results revealed mindfulness exposures actually exceeded avoidance exposures in average subjective distress. These observations are consistent with previous research showing increases in mindful observation are related to anxiety elevation (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) and support the rival hypothesis that immediate attention to negative emotional stimuli could initially raise distress level. This is also in line with findings linking increased avoidance with reduced distress in some short-term contexts (Mogg et al., 2004).
Examination of changes in experiential avoidance and anxiety severity also revealed no consistent patterns. Several participants exhibited reductions in distress aversion, yet there were no apparent distinctions between strategies. Though Participant 04 alone experienced a drop from clinical to subclinical distress aversion levels, these findings remain difficult to interpret, given 04’s previously noted adherence checks. Across participants, distraction and suppression tendencies appeared particularly resistant to change. These results suggest the MEAQ subscales may capture more dispositional traits, and as such may be less sensitive to short-term changes, particularly amid shifting condition strategies. Similarly, the OASIS showed little consistent change, perhaps due to these same strategy disruptions. Still, these null findings may be understandable, given that this investigation was not a formal treatment and may have been hindered by limited duration, contraindicated avoidance strategies, or absent UP modules (e.g., psychoeducation, cognitive appraisal).
Despite higher distress levels overall, visual and descriptive statistics revealed a downward trend in distress within mindfulness blocks (i.e., between exposures) for participants 03, 04, and 07. Our data indicated that this mean rate of change matched the reduction in avoidance for Participant 03, suggesting mindfulness was just as effective at extinguishing distress as the avoidance strategies for this individual. Furthermore, mindful exposures actually demonstrated greater mean reductions for Participants 04 and 07, compared with more static, shallow changes when employing avoidance strategies.
Considering both across- and within-block results together, the majority of participants appeared to make greater strides in extinguishing distress through continuous use of mindfulness strategies, despite initially heightened distress levels. Conversely, avoidance use produced lower overall distress initially but was incapable of further eliminating distress over time, suggesting that focus away from distressing emotions may dampen optimal cognitive engagement, experiential habituation, and long-term extinction. These findings coincide with previous evidence suggesting nonjudgmental awareness is well suited to maximizing key factors for effective exposure (Boswell et al., 2014; Craske et al., 2014; Wahl et al., 2013). Further, declining distress using mindfulness (as opposed to static distress when avoiding) lends support to emerging theory that emotion awareness is a powerful tool for targeting underlying neuroticism. Thus, mindfulness-based strategies may enhance the UP’s putative mechanism of action, as well as those of other exposure-based treatments. However, more research is needed to determine if this process in turn leads to sustained improvements in symptom severity.
THEORETICAL AND CLINICAL IMPLICATIONS
The differences in distress patterns within and across blocks were not anticipated, nor was the lack of clinical reductions in anxiety severity and avoidance tendencies. Alternation between the study conditions may explain these mixed results. Mindful exposures across only one or two blocks may have been insufficient for participants to fully grasp and consolidate nonjudgmental awareness strategies, suggesting these strategies may be effective only when a minimum duration or “dosage” is achieved. This could explain why participants returned to higher distress levels when beginning new mindfulness blocks, despite previous reductions.
Related research by Baer, Carmody, and Hunsinger (2012) found that mindfulness gains preceded stress benefits by several weeks in an MBSR course for individuals with chronic pain, and these same mindfulness increases were not apparent until at least 2 weeks into treatment. Additionally, Boswell et al. (2014) applied dynamic modeling techniques to mindfulness capacity and symptom time series, noting that increases in mindfulness capacity reliably predicted decreases in depressive and anxious symptoms over subsequent periods. Furthermore, introduction of mindfulness strategies demonstrated the biggest impact on the mindfulness time series, compared to introduction of other UP skills. Corresponding neurophysiological evidence has also noted that emotional processing appears to fundamentally change as a result of mindfulness practice, shifting from prefrontal cortical regulation (similar to cognitive reappraisal) to preconscious limbic regulation (Chiesa, Serretti, & Jakobsen, 2013). In essence, novice users may experience more emotional reactivity and attempt to control these experiences, whereas experienced users appear to react less from the outset, gaining emotional stability with less conscious effort. Taken together, these findings suggest that effective utilization of mindfulness-based strategies may require a processing period of days to weeks, with a similar degree of lag for distress, reactivity, and symptom improvements.
Further trials are needed to investigate such postulations—however, the implications of distinct short- and long-term effects of mindfulness skills during exposure are intriguing. Utilizing mindfulness strategies at first may heighten distress, as seen in our present study. However, these strategies may extinguish distress through continued practice by reducing urges to avoid or alter negative emotions. Thus, the UP may provide improvement via emotion acceptance and exposure that compound to treat distress and disorder symptoms long term.
LIMITATIONS
Some limitations should be noted in the present study. First, procedures relied, in part, on imaginal exposure scripts, and avoidance strategies may have unintentionally led to avoidance of not just emotional content but situational content during these exposures as well. Future research should explore this interaction between exposure strategy and type. Additionally, our adherence measure was not previously validated; however, despite the challenge of assessing state mindfulness, a growing number of state mindfulness scales may prove useful in future work. Finally, this study did not include exposure without strategy instructions, and future research could incorporate such a condition to better determine divergence between cognitive strategies.
Conclusion
Despite these limitations, we believe the present study provides important contributions toward understanding functional relationships between mindfulness and emotion exposure, as well as transdiagnostic treatment of emotional disorders and neuroticism. Future research should continue to explore instruction and dosage effects that may optimize mindfulness strategies. If a minimum dose of mindfulness practice does indeed facilitate beneficial exposure outcomes above and beyond avoidance strategies, future research should explore tailored mindfulness instruction against standard exposure practices to improve upon existing treatments.
Acknowledgments
This research was supported by a National Institute of Mental Health (NIMH) grant awarded to Dr. David H. Barlow (R01MH090053–S1) as part of the National Institutes of Health (NIH) Science of Behavior Change Initiative. The content reported here is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the NIH.
Footnotes
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Contributor Information
C. Alex Brake, University of Kentucky.
Shannon Sauer-Zavala, Center for Anxiety and Related Disorders, Boston University.
James F. Boswell, University at Albany
Matthew W. Gallagher, University of Houston
Todd J. Farchione, Center for Anxiety and Related Disorders, Boston University
David H. Barlow, Center for Anxiety and Related Disorders, Boston University
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Baer RA (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. 10.1093/clipsy/bpg015 [DOI] [Google Scholar]
- Baer RA, Carmody J, & Hunsinger M (2012). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 68(7), 755–765. 10.1002/jclp.21865 [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, & Allen KB (2004). Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment, 11(3), 191–206. 10.1177/1073191104268029 [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- Barlow DH (2000). Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist, 55(11), 1247–1263. [DOI] [PubMed] [Google Scholar]
- Barlow DH (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Barlow DH, Allen LB, & Basden SL (2007). Psychological treatments for panic disorders, phobias, and generalized anxiety disorder. In Nathan PE & Gorman JM (Eds.), A guide to treatments that work (3rd ed., pp. 351–394). New York, NY: Oxford University Press. [Google Scholar]
- Barlow DH, Ellard KK, Fairholme CP, Farchione TJ, Boisseau CL, Allen LB, & Ehrenreich-May J (2011a). Unified protocol for transdiagnostic treatment of emotional disorders: Client workbook. New York, NY: Oxford University Press. [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, & Ehrenreich-May J (2011b). Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Barlow DH, & Hayes SC (1979). Alternating treatments design: One strategy for comparing the effects of two treatments in a single subject. Journal of Applied Behavior Analysis, 12(2), 199–210. 10.1901/jaba.1979.12-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Nock MK, & Hersen M (2009). Single case experimental designs: Strategies for studying behavior change (3rd ed.). Boston, MA: Allyn & Bacon. [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2(3), 344–365. 10.1177/2167702613505532 [DOI] [Google Scholar]
- Boswell JF, Anderson LM, & Barlow DH (2014). An idiographic analysis of change processes in the unified transdiagnostic treatment of depression. Journal of Consulting and Clinical Psychology, 82(6), 1060–1071. 10.1037/a0037403 [DOI] [PubMed] [Google Scholar]
- Boswell JF, Farchione TJ, Sauer-Zavala S, Murray HW, Fortune MR, & Barlow DH (2013). Anxiety sensitivity and interoceptive exposure: A transdiagnostic construct and change strategy. Behavior Therapy, 44(3), 417–431. 10.1016/j.beth.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, & Mancill RB (2001). Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology, 110(4), 585–599. 10.1037/0021-843X.110.4.585 [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, & Barlow DH (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107(2), 179–192. 10.1037/0021-843X.107.2.179 [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, & Campbell LA (2001). Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110(1), 49–58. 10.1037/0021-843X.110.1.49 [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, & Hofmann SG (2006). Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion, 6(4), 587–595. 10.1037/1528-3542.6.4.587 [DOI] [PubMed] [Google Scholar]
- Carl JR, Gallagher MW, Sauer-Zavala SE, Bentley KH, & Barlow DH (2014). A preliminary investigation of the effects of the Unified Protocol on temperament. Comprehensive Psychiatry, 55(6), 1426–1434. 10.1016/j.comppsych.2014.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A, Serretti A, & Jakobsen JC (2013). Mindfulness: Top-down or bottom-up emotion regulation strategy? Clinical Psychology Review, 33(1), 82–96. 10.1016/j.cpr.2012.10.006 [DOI] [PubMed] [Google Scholar]
- Craske MG, & Barlow DH (2007). Mastery of your anxiety and panic (MAP-4): Therapist guide for anxiety, panic, and agoraphobia (4th ed.). New York, NY: Oxford University Press. [Google Scholar]
- Craske MG, Treanor M, Conway CC, Zbozinek T, & Vervliet B (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. 10.1016/j.brat.2014.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, & Barlow DH (1994). Anxiety disorders interview schedule for DSM-IV: Lifetime version (ADIS-IV-L). New York, NY: Oxford University Press. [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. [DOI] [PubMed] [Google Scholar]
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, … Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43(3), 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fledderus M, Bohlmeijer ET, & Pieterse ME (2010). Does experiential avoidance mediate the effects of maladaptive coping styles on psychopathology and mental health? Behavior Modification, 34(6), 503–519. 10.1177/0145445510378379 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Gámez W, Chmielewski M, Kotov R, Ruggero C, & Watson D (2011). Development of a measure of experiential avoidance: The Multidimensional Experiential Avoidance Questionnaire. Psychological Assessment, 23(3), 692–713. 10.1037/a0023242 [DOI] [PubMed] [Google Scholar]
- Giluk TL (2009). Mindfulness, Big Five personality, and affect: A meta-analysis. Personality and Individual Differences, 47(8), 805–811. 10.1016/j.paid.2009.06.026 [DOI] [Google Scholar]
- Hawley LL, Schwartz D, Bieling PJ, Irving J, Corcoran K, Farb NS, … Segal ZV (2014). Mindfulness practice, rumination and clinical outcome in mindfulness-based treatment. Cognitive Therapy and Research, 38(1), 1–9. 10.1007/s10608-013-9586-4 [DOI] [Google Scholar]
- Hedges LV, Pustejovsky JE, & Shadish WR (2012). A standardized mean difference effect size for single case designs. Research Synthesis Methods, 3(3), 224–239. 10.1002/jrsm.1052 [DOI] [PubMed] [Google Scholar]
- Joesch JM, Golinelli D, Sherbourne CD, Sullivan G, Stein MB, Craske MG, & Roy-Byrne PP (2013). Trajectories of change in anxiety severity and impairment during and after treatment with evidence-based treatment for multiple anxiety disorders in primary care. Depression and Anxiety, 30(11), 1099–1106. 10.1002/da.22149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koerner N, & Fracalanza K (2012). The role of anxiety control strategies in imaginal exposure. In Neudeck P & Wittchen H (Eds.), Exposure therapy: Rethinking the model—refining the method (pp. 197–216). New York, NY: Springer Science + Business Media. [Google Scholar]
- Kratochwill TR, Hitchcock J, Horner RH, Levin JR, Odom SL, Rindskopf DM, & Shadish WR (2010). Single-case designs technical documentation. Retrieved from What Works Clearinghouse; website: http://ies.ed.gov/ncee/wwc/pdf/wwc_scd.pdf. [Google Scholar]
- Lindsay M, Crino R, & Andrews G (1997). Controlled trial of exposure and response prevention in obsessive–compulsive disorder. British Journal of Psychiatry, 171, 135–139. 10.1192/bjp.171.2.135 [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP, Miles F, & Dixon R (2004). Time course of attentional bias for threat scenes: Testing the vigilance-avoidance hypothesis. Cognition and Emotion, 18(5), 689–700. 10.1080/02699930341000158 [DOI] [Google Scholar]
- Norman SB, Campbell-Sills L, Hitchcock CA, Sullivan S, Rochlin A, Wilkins KC, & Stein MB (2011). Psychometrics of a brief measure of anxiety to detect severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS). Journal of Psychiatric Research, 45(2), 262–268. 10.1016/j.jpsychires.2010.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman SB, Hami-Cissell S, Means-Christensen AJ, & Stein MB (2006). Development and validation of an Overall Anxiety Severity and Impairment Scale (OASIS). Depression and Anxiety, 23(4), 245–249. 10.1002/da.20182 [DOI] [PubMed] [Google Scholar]
- Payne LA, Ellard KK, Farchione TJ, Fairholme CP, & Barlow DH (2014). Emotional disorders: A unified transdiagnostic protocol. In Barlow DH (Ed.), Clinical handbook of psychological disorders: A step-by-step treatment manual (5th ed.). New York, NY: Guilford Press. [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, & Ball JR (2013). The association between meditation practice and treatment outcome in mindfulness-based cognitive therapy for bipolar disorder. Behaviour Research and Therapy, 51(7), 338–343. 10.1016/j.brat.2013.03.006 [DOI] [PubMed] [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, & Mennin DS (2009). Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy, 40(2), 142–154. 10.1016/j.beth.2008.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis PM, Clark DM, Hackmann A, Wells A, & Gelder MG (1999). An experimental investigation of the role of safety-seeking behaviours in the maintenance of panic disorder with agoraphobia. Behaviour Research and Therapy, 37(6), 559–574. 10.1016/S0005-7967(98)00153-3 [DOI] [PubMed] [Google Scholar]
- Salkovskis PM, Hackmann A, Wells A, Gelder MG, & Clark DM (2007). Belief disconfirmation versus habituation approaches to situational exposure in panic disorder with agoraphobia: A pilot study. Behaviour Research and Therapy, 45(5), 877–885. 10.1016/j.brat.2006.02.008 [DOI] [PubMed] [Google Scholar]
- Smith JD (2012). Single-case experimental designs: A systematic review of published research and current standards. Psychological Methods, 17(4), 510–550. 10.1037/a0029312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Hurk PM, Wingens T, Giommi F, Barendregt HP, Speckens AM, & van Schie HT (2011). On the relationship between the practice of mindfulness meditation and personality—an exploratory analysis of the mediating role of mindfulness skills. Mindfulness, 2(3), 194–200. 10.1007/s12671-011-0060-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venta A, Sharp C, & Hart J (2012). The relation between anxiety disorder and experiential avoidance in inpatient adolescents. Psychological Assessment, 24(1), 240–248. 10.1037/a0025362 [DOI] [PubMed] [Google Scholar]
- Wahl K, Huelle JO, Zurowski B, & Kordon A (2013). Managing obsessive thoughts during brief exposure: An experimental study comparing mindfulness-based strategies and distraction in obsessive-compulsive disorder. Cognitive Therapy and Research, 37(4), 752–761. 10.1007/s10608-012-9503-2 [DOI] [Google Scholar]
- Wolpe J (1969). The practice of behavior therapy. New York: Pergamon. [Google Scholar]


