Abstract
Objectives:
To determine the total number of privileged and full-time equivalent (FTE) intensivists in acute care hospitals with intensivists nationally and compare the characteristics of hospitals with and without intensivists.
Design:
Retrospective analysis of the American Hospital Association (AHA) Annual Survey Database (FY 2015).
Setting:
2814 acute care hospitals with intensive care unit (ICU) beds.
Patients:
None.
Interventions:
None.
Measurements and Main Results:
Of the 2,814 acute care hospitals studied, 1,469 (52%) had intensivists and 1,345 (48%) had no intensivists. There were 28,808 privileged and 19,996 FTE intensivists in the 1,469 hospitals with intensivists. In these hospitals, the median (25th, 75th percentile) numbers of privileged and FTE intensivists were 11 (5, 24) and 7 (2, 17), respectively. Compared to hospitals without intensivists, hospitals with privileged intensivists are primarily located in metropolitan areas (91% vs 50%, p<0.001) and at the aggregate level have nearly thrice the number of hospital beds [403,522 (75%) vs. 137,146 (25%)], 3.6 times the number of ICU beds [(74,222 (78%) vs. 20,615 (22%)] and almost twice as many ICUs [(3,383 (65%) vs 1,846 (35%)]. At the hospital level, hospitals with privileged intensivists had significantly more hospital beds (median, 213 vs 68; p<0.0001), ICU beds (median, 32 vs 8; p<0.0001), a higher ratio of ICU to hospital beds (15.6% vs 12.6%; p<0.0001) and a higher number of ICUs per hospital (2 vs 1, p<0.0001) than hospitals without intensivists.
Conclusions:
Analyzing the intensivist section of the AHA Annual Survey database is a novel approach to estimating the number of privileged and FTE intensivists in acute care hospitals with ICU beds in the US. This methodology opens the door to an enhanced understanding of the current supply and distribution of intensivists as well as future research into the intensivist workforce.
Keywords: critical care, intensive care, beds, intensivists, privileged, hospitals
Intensive care unit (ICU) care in the United States (US) is both common and expensive (1). The demand for intensive care is projected to increase due to an aging population with increasing comorbidities, and advances in complex healthcare therapeutics (2;3). Against this backdrop, there are multiple perspectives regarding the optimal utilization and number of ICU beds, the impact of hospital attributes and critical care medicine (CCM) delivery and organizational models on patient outcomes and variability in ICU use, and the benefits and adequacy of intensivist staffing (4–16). However, these discussions are occurring in an intensivist data vacuum because there are no recent studies addressing the number of intensivists in US hospitals.
Several methods can be employed to estimate the national supply of intensivists. One approach uses CCM certified physicians as surrogates for intensivists. Thus, in 2016, the American Board of Medical Specialties (ABMS) identified 14804 adult and 1090 pediatric CCM board certified physicians (17). A second utilizes data from the American Medical Association (AMA) Physician Master File as a stand-in for intensivists. In 2013, the AMA had 10897 physicians self-designated as adult and 2002 as pediatric intensivists (18). A third and markedly different approach relies upon “virtual” intensivist estimates generated by workforce projection studies. The oft-cited Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) study published in 2000 estimated a total of 12,000 full-time equivalent (FTE) intensivists for base year 1997 and projected a supply of approximately 13,500 FTE adult intensivists for 2015 (19). COMPACCS relied upon nationally representative surveys of intensivists and ICU directors identified from the 1996 AMA Physician Master File and the 1996 SMG Hospital Market database, respectively. Despite its arcane methodology (20), the COMPACCS study became the primary basis for the perception of an intensivist shortfall (21). The Health Resources and Services Administration (HRSA) 2006 and 2016 CCM workforce reports also used data from the AMA Physician Master File to establish their base years and projections (22;23). The HRSA data is far lower than the other estimates. The 2006 report estimated 1900 FTE intensivists for base year 2000 and projected a supply of 2770 for 2020 (22). The 2016 report estimated 3570 FTE intensivists for base year 2013 and projected a supply of 5620 for 2025 (23). None of these proxy or projection estimates of intensivist staffing actually determined the number of intensivists practicing CCM within acute care hospitals.
The American Hospital Association (AHA) voluntary survey annually gathers data nationally on ICU beds and privileged and FTE intensivists. The main objectives of our study were to determine from the 2015 AHA dataset the total number of privileged and FTE intensivists in acute care hospitals with intensivists and compare the characteristics of hospitals delivering critical care services with and without intensivists.
METHODS
Data source
The AHA Annual Survey Database for Fiscal Year (FY) 2015 was our sole data source (24). This dataset is derived from the annual surveys (Supplemental 1, AHA Survey, Supplemental Digital Content 1) sent to all AHA registered US hospitals and voluntarily completed. Survey data from respondent hospitals is merged into one master dataset each year.
AHA Hospital classifications
The AHA classifies registered hospitals into six categories (i.e. total, total nonfederal short term and other special, total community, nongovernment not-for-profit community, investor owned for-profit community, and state and local government community). Similar to our prior CCM analyses (1;25;26), we selected the “total community” cohort as the group most typical of acute care hospitals with CCM services. This category includes all nonfederal, short-term and other special hospitals (e.g., obstetrics and gynecology, eye, ear nose and throat; orthopedic, rehabilitation and childrens) as well as university and academic hospitals. Excluded from the total community category are federal, adult and children psychiatric and chronic disease, long-term, alcohol and other chemical dependency, and prison hospitals and college infirmaries.
The AHA categorizes hospitals by three Core Based Statistical Areas (CBSA) locations: Metropolitan (an urbanized area with a population of at least 50,000); Micropolitan (an area with a population of at least 10,000 but fewer than 50,000), and Rural (27).
Hospital and ICU beds
Bed totals are collected on all staffed (operational) beds within each hospital for acute care and long-term beds. Acute care beds include general medical and surgical adult, pediatrics, obstetrics, neonatal intermediate, six ICU bed types (Medical-Surgical, Cardiac, Other, Pediatric, Neonatal and Burn) and Other Special Care (observation, step-down, or progressive). Long-term beds include physical rehabilitation, alcohol / drug abuse or dependency, psychiatric, skilled nursing care, intermediate nursing, acute and other long term.
The AHA gathers data on the number of beds per each ICU type; however, the number of units housing these beds is not requested. For example, if a hospital states that it has either 5 or 20 Medical-Surgical ICU beds, the AHA classifies that hospital as offering “one” Medical-Surgical ICU service or unit (24).
Privileged and FTE physicians and intensivists
The AHA survey requests data on privileged and FTE physicians. Privileged is defined as those physicians on the medical staff with “privileges.” Physicians with courtesy, honorary or provisional privileges provide only non-clinical service, and trainees are excluded. FTE values are calculated as the total number of hours worked by physicians over the full 12-month reporting period divided by the normal number of hours worked by a full-time employee for that same period.
A privileged “intensivist” is defined by the AHA as a physician with “special training” to work with critically ill patients and generally provides Medical-Surgical, Cardiac, Other, Pediatric and Neonatal intensive care services (24). The survey initiates the query on privileged intensivists by asking hospitals to identify if intensivists provide care for their patients. If they do, hospitals are asked to provide the “total” number of privileged intensivists for the hospital and the number of FTE intensivists specifically assigned to the Medical-Surgical, Cardiac, Other, Pediatric and Neonatal ICUs. Hospitals also had the option to provide the FTE “total” for all their ICUs rather than FTEs by ICU type.
Inclusion and exclusion of hospitals and beds
In this study, we focused on the cohort of registered AHA total community hospitals that responded to the AHA 2015 survey and had at least 10 acute care beds and one ICU bed. Within the included hospitals, we focused on acute care beds and excluded long-term beds from analysis. We also compare key parameters (hospital size, Core Based Statistical Areas, regions, locations and hospital types) and perform a sensitivity analysis between respondent and non-respondent hospitals.
Internal data validation and decision rules
To detect potential issues common to survey data, we developed and conducted a series of internal data validations, decision rules, and sensitivity analyses (Supplemental 2, Table E1 Supplemental Digital Content 2) to address inconsistent reporting in three areas. The first focused upon the primary survey variable - “Do intensivists provide care for patients in your hospital?;” the second concerned the consistency in the reporting of privileged intensivists; and the third addressed FTE intensivist numbers. The decision rules on resolving privileged and FTE data inconsistencies are founded on our core assumptions that all FTE intensivists are privileged and the number of privileged intensivists must equal or exceed the number of FTE intensivists. Sensitivity analyses are presented in Table E2 (Supplemental 2, Table E2, Supplemental Digital Content 2).
Statistical Analysis
Characteristics related to hospital and ICU beds are summarized in aggregate as total N or at the hospital-level as N (%) or median (25th, 75th percentile). Comparisons between hospitals with and without intensivists were conducted with the Wilcoxon rank-sum test for continuous variables and the Fisher’s exact test for categorical variables. Additionally, the number of acute care hospital and ICU beds were assessed within and across three CBSA locations (metropolitan, micropolitan and rural). Comparisons between hospitals with and without privileged intensivists were further stratified by ICU types (Medical-Surgical, Cardiac, Other, Pediatric, Neonatal). With regards to ICU beds and FTE per unit type, we concentrated on data in Medical-Surgical, Cardiac, Other, Pediatric, and Neonatal ICUs.
Hospital, bed and unit data were analyzed for Burn ICUs and Other Special Care units separately as there is no FTE data available for these two bed categories. Additionally, Burn units are rare and Other Special Care units are not considered ICUs. Analyses were conducted in Stata 15 (StataCorp, College Station, Texas).
All statistical tests were two-sided, and p<0.05 was considered statistically significant. In accordance with our local Institutional Review Board (IRB) determination, this study did not require IRB oversight (April 28, 2017).
RESULTS
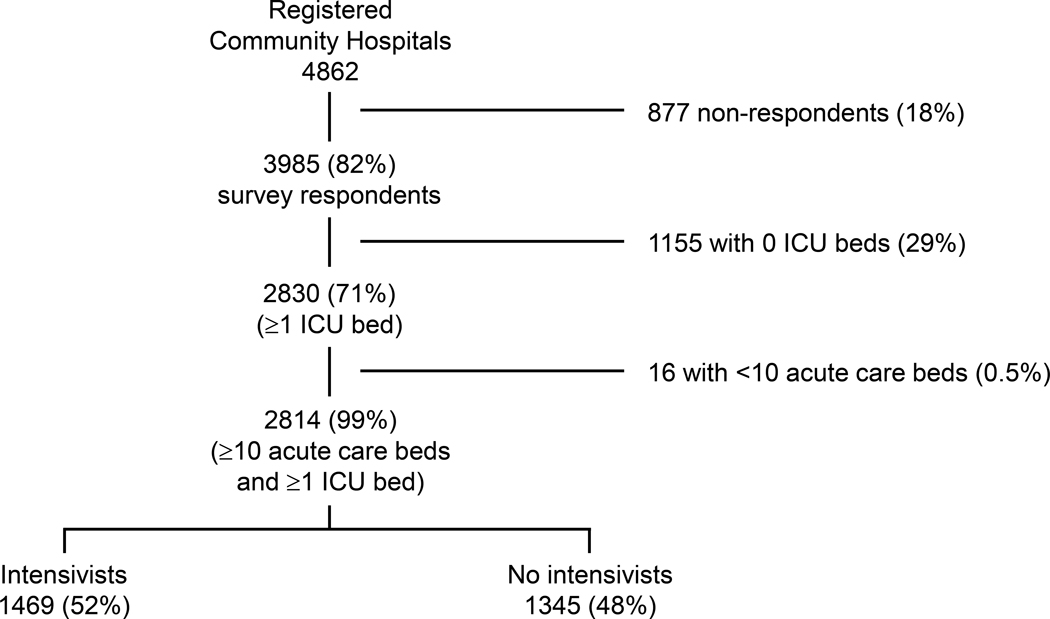
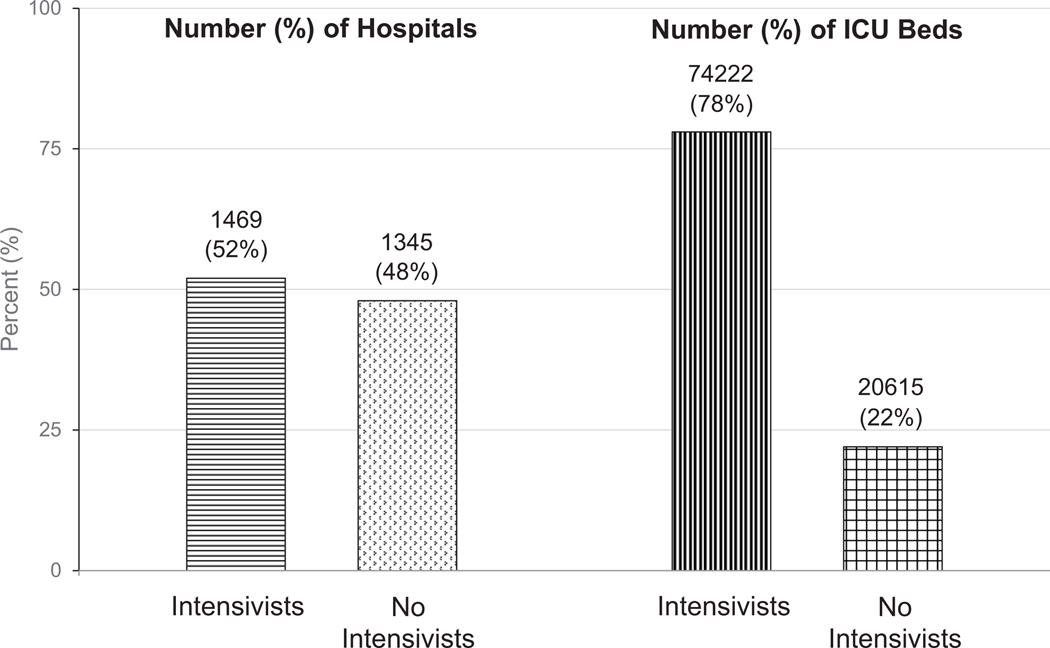
In FY 2015, there were 4862 AHA registered community hospitals; 3985 (82%) responded to the AHA survey (Figure 1) and 877 (18%) did not (Supplemental 3, Tables E3 and E4, Supplemental Digital Content 3). Of the respondents, 2814 (71%) had at least 10 acute care beds and at least 1 ICU bed and comprised the study hospitals. Of the 2814 hospitals, 1469 (52%) had 28,808 privileged intensivists while 1345 (48%) had none (Figure 2, left bars).
Figure 1.
There were a total of 4862 American Hospital Association (AHA) registered community hospitals located in the 50 states. 3985 (82%) responded to the AHA survey. Of these, 2814 (71%) met inclusion criteria (>10 hospital beds and > 1 ICU bed) and were divided fairly evenly with 1469 hospitals (52%) having privileged intensivists and 1345 (48%) without privileged intensivists.
Figure 2.
Approximately 52% of hospitals with ICU beds had privileged intensivists (left bars). However, 78% of ICU beds were in hospitals with privileged intensivists (right pars).
Hospitals and ICU beds by location
Of the 2814 study hospitals, 2008 (71%) are located in metropolitan areas, 525 (19%) in micropolitan and the remainder in rural (Table 1). The distribution of hospitals across the three locations is significantly different between hospitals with and without intensivists (p<0.0001) (Table 1): 1335 (91%) of hospitals with intensivists are located in metropolitan areas and 111 (7.6%) in micropolitan areas, compared to a broader distribution among hospitals without intensivists with 673 (50%) of hospitals located in metropolitan and 414 (31%) in micropolitan areas.
TABLE 1.
Summary of hospitals, and hospital and ICU beds by Core Based Statistical Areas (CBSA)*
| Variables | Hospitals Combined (N=2814) |
Hospitals With Intensivists (N=1469; 52%) |
Hospitals Without Intensivists (N=1345; 48%) |
P |
|---|---|---|---|---|
| Number of Hospitals by location | ||||
| Metropolitan | 2008 (71%) | 1335 (91%) | 673 (50%) | <0.0001 |
| Micropolitan | 525 (19%) | 111 (7.6%) | 414 (31%) | |
| Rural | 281 (10%) | 23 (1.6%) | 258 (19%) | |
| Aggregate across all hospitals | ||||
| Number of Hospital beds by location | ||||
| Metropolitan | 487,193 (90%) | 389,095 (96%) | 98,098 (72%) | |
| Micropolitan | 42,392 (8%) | 13031 (3%) | 29,361 (21%) | |
| Rural | 11,083 (2%) | 1,396 (1%) | 9,687 (7%) | |
| Number of ICU beds by location | ||||
| Metropolitan | 87,986 (93%) | 72,128 (97%) | 15,858 (77%) | |
| Micropolitan | 5,418 (6%) | 1,833 (2%) | 3,585 (17%) | |
| Rural | 1,433 (1%) | 261 (1%) | 1,172 (6%) | |
| Hospital-level, median (IQR)a | ||||
| Number of Hospital beds by location | <0.0001 | |||
| Metropolitan | 194 (105, 315) | 230 (143, 373) | 115 (55, 213) | <0.0001 |
| Micropolitan | 66 (40, 101) | 99 (58, 152) | 59 (34, 94) | <0.0001 |
| Rural | 26 (25, 47) | 28 (26, 84) | 26 (25, 46) | 0.058 |
| Number of ICU beds by location | <0.0001 | |||
| Metropolitan | 28 (12, 58) | 36 (18, 71) | 14 (7, 32) | <0.0001 |
| Micropolitan | 8 (5, 12) | 12 (7, 19) | 7 (4, 10) | <0.0001 |
| Rural | 4 (3, 6) | 6 (4, 11) | 4 (3, 6) | 0.002 |
Abbreviations: ICU, Intensive Care Unit.
Core based statistical areas (CBSA): Metropolitan: urbanized area with a population of at least 50,000. Micropolitan: urbanized area with a population of 10,000–50,000; Rural: geographies not defined by metropolitan or micropolitan.
Hospital-level refers to summary where hospital is the unit of analysis; IQR refers to 25th and 75th percentile.
In aggregate, 540668 (90%) of all hospital beds and 87986 (93%) of all ICU beds are located in metropolitan areas, and the remainder in micropolitan and rural areas (Table 1). Across the two hospital groups, 72218 (97%) of ICU beds with intensivists are located in metropolitan areas, whereas 15858 (77%) of ICU beds without intensivists are located in metropolitan areas. Within hospitals located in metropolitan regions, the number of hospital (median, 230 vs 115; p<0.001) and ICU (median, 36 vs 14; p<0.001) beds per hospital were significantly higher among hospitals with intensivists than without. These patterns were similarly observed in the micropolitan locations.
Hospitals and ICU beds nationally
In aggregate, the 2814 study hospitals had a total of 540,668 hospital beds, of which 94,837 are ICU beds with a median ICU to hospital bed ratio of 14.3%. Hospitals with intensivists had 2.9 times the number of hospital beds (403,522 vs. 137,146), 3.6 times the number of ICU beds (74,222 vs. 20,615), and 1.8 times the number of units (3383 vs. 1846) when compared to hospitals without intensivists (Table 2). In aggregate, 78% of the total ICU beds are in hospitals with privileged intensivists (Figure 2, right bars).
TABLE 2:
Summary of hospital beds, ICU beds and units between hospitals with and without privileged intensivists
| Variables | Hospitals Combined (N=2814) |
Hospitals With Intensivists (N=1469; 52%) |
Hospitals Without Intensivists (N=1345; 48%) |
P |
|---|---|---|---|---|
| Aggregate across all hospitals | ||||
| Number of Hospital beds | 540,668 | 403,522 | 137,146 | |
| Number of ICU beds | 94,837 | 74,222 (18.4%) | 20,615 (15%) | |
| Number of ICU units b | 5229 | 3383 | 1846 | |
| Number of ICU beds by unit-type b | ||||
| Medical-Surgical | 46,490 | 33,421 (45%) | 13,069 (63%) | |
| Cardiac | 14,731 | 11,885 (16%) | 2,846 (14%) | |
| Other | 6,588 | 5,323(7%) | 1,265 (6%) | |
| Pediatrics | 4,698 | 4,265 (6%) | 433 (2%) | |
| Neonatal | 22,330 | 19,328 (26%) | 3,002 (15%) | |
| Hospital-level, median (IQR)a | ||||
| Number Hospital beds | 133 (58, 258) | 213 (128, 358) | 68 (33, 133) | <0.0001 |
| Number of ICU beds | 16 (7, 42) | 32 (16, 67) | 8 (4, 16) | <0.0001 |
| ICU beds/Hospital beds ratio | 14.3% (10.5, 19.2) | 15.6% (11.4, 20.7) | 12.6% (9.8, 16.7) | <0.0001 |
| Number of ICU beds by unit-type | ||||
| Medical-Surgical | 12 (6, 23) | 18 (12, 30) | 8 (4, 12) | <0.0001 |
| Cardiac | 12 (8, 20) | 12 (9, 22) | 8 (5, 12) | <0.0001 |
| Other | 12 (8, 22) | 14 (10, 23) | 8 (5, 16) | <0.0001 |
| Pediatric | 10 (6, 19) | 10 (6, 19) | 8 (6, 12) | 0.1 |
| Neonatal | 18 (10, 32) | 20 (10, 36) | 12 (6, 20) | <0.0001 |
| Number of ICU units b | 1.0 (1.0, 2.0) | 2.0 (1.0, 3.0) | 1.0 (1.0, 2.0) | <0.0001 |
| Number of ICU units b | ||||
| 1 | 1468 (52%) | 480 (33%) | 988 (73%) | <0.0001 |
| 2 | 669 (24%) | 430 (29%) | 239 (18%) | |
| 3 | 380 (14%) | 286 (19%) | 94 (7.0%) | |
| 4 | 202 (7.2%) | 180 (12%) | 22 (1.6%) | |
| 5 | 95 (3.4%) | 93 (6.3%) | 2 (0.1%) |
Abbreviations: ICU, Intensive Care Unit,
Hospital-level refers to summary where hospital is the unit of analysis; IQR refers to 25th and 75th percentile.
Units refers to the number of hospitals reporting >1 beds per specific ICU type. Each hospital can have a maximum of 5 types of ICUs.
Based on the distribution of hospital beds per hospital, the number of hospital beds was significantly higher among hospitals with intensivists compared to those without (median, 213 vs. 68; p<0.0001) (Table 2). Similarly, the number of ICU beds per hospital was significantly higher among hospitals with intensivists compared to those without (median, 32 vs. 8; p<0.0001). The ICU to hospital beds ratio was significantly higher among hospitals with intensivists compared to those without (median, 15.6% vs. 12.6%; p<0.0001) as was the number of ICU units (median, 2 vs. 1; p<0.0001).
Within each ICU type, the greatest percentages of ICU beds were in the Medical-Surgical and Neonatal ICUs (Table 2). The median number of ICU beds per unit type was significantly greater in hospitals with intensivists in all unit types except for Pediatric ICUs (Table 2). Among hospitals with intensivists, 33% of hospitals had 1 ICU and 67% have two or more ICUs, whereas 73% of hospitals without intensivists had 1 ICU and only 27% had 2 or more ICUs (p<0.0001) (Table 2). A greater percentage of hospitals with intensivists had 4 or 5 ICU types than those without intensivists (18% vs 2%).
Intensivist-related characteristics at hospital level
In the hospitals with intensivists, there were 28,808 privileged intensivists and 19,996 FTE intensivists. Per hospital, the median (25th, 75th percentile) number of privileged intensivists was 11 (5, 24), while the median number of FTEs was 7 (2, 17).
Beds and staff in units with FTEs reported
Overall, 1235 hospitals (84% of hospitals with intensivists) provided ICU by ICU FTE data totaling 18568 FTEs (Table 3). Within hospitals with privileged intensivists, over 80% of adult Medical-Surgical ICUs report at least 1 FTE per unit, whereas Cardiac and Other ICUs report at least 1 FTE per unit in 33% and 36%, respectively (Table 3). In non-adult ICUs, Pediatric ICUs and Neonatal ICUs reported at least 1 FTE per unit in 83% and 68% respectively. The median number of beds per adult unit was 19 in the Medical-Surgical ICUs and 16 in Cardiac and Other ICUs. In non-adult ICUs, the median number of beds was 19 in Pediatric and 22 in Neonatal ICUs. The median FTEs for Medical-Surgical ICUs was 5, Cardiac and Other ICUs had 4; and Pediatric and Neonatal ICUs had 6.
TABLE 3.
Characteristics among hospitals with privileged intensivists and FTEs by ICU unit-types
| ICU unit-type | Data |
|---|---|
| Medical surgical ICUs | |
| Number of medical-surgical ICUs in hospitals with privileged intensivists | 1381 |
| Number of ICUs reporting at least 1 FTE per unit | 1115 (81%) |
| Number of beds* | 28202 |
| Number of beds per unit** | 19 (12, 32) |
| Number of FTEs | 10415 |
| Number of FTEs per unit** | 5 (3, 11) |
| Cardiac ICUs | |
| Total cardiac ICUs in hospitals with privileged intensivists | 700 |
| ICUs reporting at least 1 FTE per unit | 231 (33%) |
| Number of beds* | 4595 |
| Number of beds per unit** | 16 (10, 24) |
| Number of FTEs | 1659 |
| Number of FTEs per unit** | 4 (2, 9) |
| Other ICUs | |
| Total other ICUs in hospitals with privileged intensivists | 278 |
| ICUs reporting at least 1 FTE per unit | 99 (36%) |
| Number of beds* | 2004 |
| Number of beds per unit** | 16 (10, 25) |
| Number of FTEs | 729 |
| Number of FTEs per unit** | 4 (2, 8) |
| Pediatric ICUs | |
| Total pediatric ICUs in hospitals with privileged intensivists | 297 |
| ICUs reporting at least 1 FTE per unit | 246 (83%) |
| Number of beds* | 3816 |
| Number of beds per unit** | 12 (8, 20) |
| Number of FTEs | 1826 |
| Number of FTEs per unit** | 6 (4, 10) |
| Neonatal ICUs | |
| Total neonatal ICUs in hospitals with privileged intensivists | 727 |
| ICUs reporting at least 1 FTE per unit | 493 (68%) |
| Number of beds* | 13990 |
| Number of beds per unit** | 22 (12, 39) |
| Number of FTEs | 3957 |
| Number of FTEs per unit** | 6 (3, 10) |
Abbreviations: FTE, Full time equivalent; ICU, Intensive Care Unit.
Beds in units with FTEs;
Median (25th, 75th pct). The FTE data in this table represents the 1,235 hospitals (84% of the 1,469 hospital respondents with intensivists) that provided ICU by ICU FTE data and totals 18,586 FTEs (Adult FTE – 12,803 and Pediatrics/Neonatal – 5,783).
Burn and Other Special Care
Burn and Other Special Care unit and bed data are presented in (Supplemental 4, Table E5, Supplemental Digital Content 4). The majority of Burn and Other Special Care units and beds were in hospitals with intensivists. Additionally, the median number of other special care beds is significantly higher in hospitals with intensivists.
DISCUSSION
Using nationally representative intensivist workforce data derived from the AHA survey, we found that for FY 2015, there were 28,808 privileged intensivists generating 19,996 FTEs in the 1469 acute care hospitals with intensivists. These intensivist workforce estimates are unique because they are the first to rely upon a national hospital dataset versus estimates from CCM board certification and self-designation totals and workforce projection studies (17–20, 22). Within the construct of the AHA dataset, we perceive that the number of privileged intensivists reflects the totality of intensivists “available” and interested in CCM practice. In contrast, FTE data refers primarily to the time that intensivists are effectively assigned to ICU service.
Three hypotheses may explain the greater number of privileged than FTE intensivists. First, intensivist privileging is 1:1 per intensivist possibly in more than one hospital at a time; whereas FTE coding is more exact and may be <1 within each ICU as applicable. Second, in large teaching hospitals, there are commonly a high number of ‘privileged’ intensivists because of the presence of hybrid clinician-intensivists (i.e. anesthesiologist-intensivist, surgeon-intensivist, or pulmonary-intensivist) who spend time both on ICU and non-ICU services. Third, in small community hospitals, the hospitals may privilege intensivists but report lower FTE values because salary support is not assigned.
The total numbers of privileged or FTE intensivists in the AHA database are higher than those recorded in other national physician inventories [ABMS CCM board certification totals (15894), Association of American Medical Colleges (10,159) and AMA Physician Master file (12899)] (17;28;29). The Society of Critical Care Medicine reports 10,360 US intensivists online (30). We attribute the disparities in intensivist totals between the AHA and other datasets to differences in intensivist definitions and counting methods. For example, since the 2010 survey (31), the AHA has defined a privileged intensivist as a physician with special training in critical care; the other datasets require current or past CCM board certification. Thus the AHA hospitals may privilege and include physicians as intensivists that were, but are no longer, or were never, CCM certified, as well as pulmonologists and hospitalists (with special training in CCM) caring for critically ill patients (32). Additionally, the AHA may include neurology-certified intensivists not currently included in the ABMS datasets.
The AHA FTE intensivist estimates were more aligned with the workforce projections of COMPACCS (19) than the unrealistically low base year and projections from the HRSA Health Workforce reports (22;23). Focusing on the 2016 HRSA report, we cannot explain the HRSA’s gross undercounting of FTE intensivists. Furthermore, this report suggested a “surplus” of 1480 intensivists in 2025. It is worth noting that the 2016 HRSA report does not provide their data sources or define the type of intensivists included (22;23). We have since determined that the HRSA data is sourced from a mix of primary, secondary or self-designation AMA Physician Master File codes and that the 2016 report focused primarily on internal medicine CCM certified intensivists (Personal Communication Oct. 7, 2018, Tim Dall, Executive Director, Life Sciences Consulting, Washington, D.C.). Unless the HRSA CCM reports are redressed, the US Congress may erroneously sense that intensivist manpower is going to be over-staffed and decrease federal support for CCM fellowship training positions.
Intensivist staffing models commonly utilize “intensivist-to-patient” ratios to suggest the optimal and maximal number of patients that can be safely and efficiently cared for by an intensivist (33;34). Herein, we offer a different perspective and present FTE intensivists at the ICU, rather than patient, level. For example, we show that Medical-Surgical ICUs and Cardiac units have a median of 5 and 4 FTEs, respectively. Although our FTE data per ICU does not account for FTE movement between one ICU and another, as well as administrative time, variability in ICU management, staffing and care models, this data may assist ICU leaders seeking to benchmark intensivist FTEs or justify intensivist per unit targets (35).
Another instructive finding is the percentage of units in hospitals that report intensivist FTE assignments. For example, 81% of Medical Surgical ICUs have FTEs assigned; whereas only 33% of Cardiac ICUs have FTEs assigned. A recent study showed that only 25% of Cardiac ICUs have dedicated cardiac intensivists (36). With improved outcomes recently reported in Cardiac ICUs with cardiac intensivists, there may be a rising demand for training in this subspecialty (37). We cannot comment on the low FTE values observed in “Other” ICUs, because the AHA survey does not provide specific ICU types of “other” ICUs.
Our analysis of intensivists, hospitals and ICU beds allows us to present two competing data-driven relationships on the deployment of the intensivist workforce. At the hospital level, approximately half (48%) of the acute care hospitals with ICU beds have no intensivists; however, over three quarters (78%) of all ICU beds are located in hospitals with intensivists. These findings suggest differing inferences. The hospital data alludes to a major intensivist shortfall, while the ICU bed data indicates fairly adequate intensivist staffing. However, beyond highlighting these two approaches, it is beyond our scope to actually resolve the long standing and challenging question of the adequacy of the intensivist workforce (4;9;10;15;16). That determination would require a large scale study of ICU bed numbers, allocation and utilization, ICU staffing inclusive of CCM Advance Practice Providers or non-CCM physicians (i.e. hospitalists), ICU management and care models with related patient outcomes, and approaches that rely upon regionalization and telemedicine.
As this is the first study to address the intensivist sections of the AHA survey in detail, we itemize limitations related to survey design, approaches to survey completion and hospital response. First, the AHA intensivist definition does not require CCM board certification or subspecialty CCM designation; thus, comparisons with other large physician-centric inventories are inexact. Second, the survey utilizes a non-specific “Other” ICU category instead of listing subspecialty ICUs (i.e. neuroscience or surgical); the Other category precludes the availability of subspecialty ICU bed and FTE intensivist data (38). Third, hospitals are given the choice in the survey’s FTE section to provide either FTE data by ICU type or FTE totals. This variability led to a small difference in FTE totals (Table 3). Fourth, the survey does not request the number of ICUs corresponding to beds; thus, the number of ICUs must be estimated. Lastly, despite the high survey response rate of 82%, intensivist data is still missing from the 18% (877) non-respondent AHA registered hospitals. As a result, the numbers of privileged and FTE intensivists may be underestimated, and the proportion of hospitals with and without any intensivists may differ slightly from our presented values. Our comparison and sensitivity analyses of respondent and non-respondent hospitals shows that the latter were primarily small, non-teaching hospitals less likely to have intensivists than the respondents (Supplemental 3, Tables E3 and E4, Supplemental Digital Content 3).
CONCLUSIONS
Analyzing the intensivist section of the AHA Annual Survey database is a novel approach to estimating the number of privileged and FTE intensivists in acute care hospitals with ICU beds in the US. This methodology opens the door to an enhanced understanding of the current supply and distribution of intensivists as well as future research into the intensivist workforce. Additionally, this data may serve as a comparison to prior workforce estimates obtained from the specialty boards, the AMA Master Physician Master File and workforce projection studies.
Supplementary Material
Acknowledgments:
The authors acknowledge Elaine Ciccaroni, for preparation of the Figures and Tables, Peter D. Kralovec, Executive Director, Health Care Data Center, American Hospital Association (AHA), Chicago, IL for his guidance in analyzing the AHA master dataset and Tim Dall, Executive Director, Life Sciences Consulting, Washington, D.C. for his guidance in analyzing the HRSA reports.
Financial Support: Supported, in part, by the Core Grant (P30 CA008748) and the Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center, New York, NY
Copyright form disclosure: Dr. Halpern received funding from Instrumentation Lab, Inc., Cardiopulmonary Corp, and Pronia Medical (stock options). Dr. Tan received support for article research from the National Institutes of Health. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Conflicts: No financial or other potential conflicts of interest exist for all listed authors.
References
- (1).Halpern NA, Goldman DA, Tan KS, Pastores SM. Trends in Critical Care Beds and Use Among Population Groups and Medicare and Medicaid Beneficiaries in the United States: 2000–2010. Crit Care Med 2016. May 2;44(8):1490–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Our patients, Ourselves: Health Care for an Aging Population. A Report of the Dartmouth Atlas Project. 2016. The Dartmouth Institute for Health Policy & Clinical Practice. Available at: http://www.dartmouthatlas.org/downloads/reports/Our_Parents_Ourselves_021716.pdf. Accessed May 15, 2018 [PubMed] [Google Scholar]
- (3).Godel P, Shimabukuro-Vornhagen A, von Bergwelt-Baildon M. Understanding cytokine release syndrome. Intensive Care Med 2018. March;44(3):371–3. [DOI] [PubMed] [Google Scholar]
- (4).Gooch RA, Kahn JM. ICU Bed Supply, Utilization, and Health Care Spending: An Example of Demand Elasticity. JAMA 2014. January 9;311(6):567–8. [DOI] [PubMed] [Google Scholar]
- (5).Nguyen YL, Wunsch H, Angus DC. Critical care: the impact of organization and management on outcomes. Curr Opin Crit Care 2010. October;16(5):487–92. [DOI] [PubMed] [Google Scholar]
- (6).Weled BJ, Adzhigirey LA, Hodgman TM, Brilli RJ, Spevetz A, Kline AM, Montgomery VL, Puri N, Tisherman SA, Vespa PM, Pronovost PJ, Rainey TG, Patterson AJ, Wheeler DS. Critical Care Delivery: The Importance of Process of Care and ICU Structure to Improved Outcomes: An Update From the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med 2015. July;43(7):1520–5. [DOI] [PubMed] [Google Scholar]
- (7).Costa DK, Kahn JM. Organizing Critical Care for the 21st Century. JAMA 2016. February 23;315(8):751–2. [DOI] [PubMed] [Google Scholar]
- (8).Leung S, Gregg SR, Coopersmith CM, Layon AJ, Oropello J, Brown DR, Pastores SM, Kvetan V. Critical Care Organizations: Business of Critical Care and Value/Performance Building. Crit Care Med 2018. January;46(1):1–11. [DOI] [PubMed] [Google Scholar]
- (9).Halpern NA, Pastores SM, Oropello JM, Kvetan V. Critical care medicine in the United States: addressing the intensivist shortage and image of the specialty. Crit Care Med 2013. December;41(12):2754–61. [DOI] [PubMed] [Google Scholar]
- (10).Kahn JM, Rubenfeld GD. The Myth of the Workforce Crisis: Why the United States Does Not Need More Intensivist Physicians. Am J Respir Crit Care Med 2015;191(2):128–34. [DOI] [PubMed] [Google Scholar]
- (11).Admon AJ, Wunsch H, Iwashyna TJ, Cooke CR. Hospital Contributions to Variability in the Use of ICUs Among Elderly Medicare Recipients. Crit Care Med 2017. January;45(1):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Wallace DJ, Seymour CW, Kahn JM. Hospital-Level Changes in Adult ICU Bed Supply in the United States. Crit Care Med 2017. January;45(1):e67–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Seymour CW, Iwashyna TJ, Ehlenbach WJ, Wunsch H, Cooke CR. Hospital-level variation in the use of intensive care. Health Serv Res 2012. October;47(5):2060–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Chang DW, Shapiro MF. Association Between Intensive Care Unit Utilization During Hospitalization and Costs, Use of Invasive Procedures, and Mortality. JAMA Intern Med 2016. October 1;176(10):1492–9. [DOI] [PubMed] [Google Scholar]
- (15).Davidson BL. POINT: Does the United States Need More Intensivist Physicians? Yes. Chest 2016. March;149(3):621–5. [DOI] [PubMed] [Google Scholar]
- (16).Rubenfeld GD. COUNTERPOINT: Does the United States Need More Intensivist Physicians? No. Chest 2016. March;149(3):625–8. [DOI] [PubMed] [Google Scholar]
- (17).American Board of Medical Specialties. ABMS Board Certification Report 2015–2016. 2017. Chicago, IL. Available at: http://www.abms.org/media/131568/2015-16-abmscertreport.pdf. Accessed May 15, 2018 [Google Scholar]
- (18).Physician Characteristics and Distribution in the US. Smart DR, editor. 2015 edition. 2015. Division of Survey and Data Resources. American Medical Association. Chicago, IL [Google Scholar]
- (19).Angus DC, Kelly MA, Schmitz RJ, White A, Popovich J. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease. JAMA 284[21], 2762–2770. [DOI] [PubMed] [Google Scholar]
- (20).Cooper RA. The COMPACCS Study: questions left unanswered. The Committee on Manpower for Pulmonary and Critical Care Societies. Am J Respir Crit Care Med 2001. January;163(1):10–1. [DOI] [PubMed] [Google Scholar]
- (21).Kelley MA, Angus D, Chalfin DB, Crandall ED, Ingbar D, Johanson W, Medina J, Sessler CN, Vender JS. The critical care crisis in the United States: a report from the profession. Chest 2004. April;125(4):1514–7. [DOI] [PubMed] [Google Scholar]
- (22).HRSA. The Critical Care Workforce: A Study of the Supply and Demand for Critical Care Physicians. Requested by: Senate Report 108–81. Rockville, MD: US Department of Health and Human Services; Health Resources and Services Administration. Report to Congress.; 2006. Available at: https://www.mc.vanderbilt.edu/documents/CAPNAH/files/criticalcare.pdf. Accessed September 7, 2018 [Google Scholar]
- (23).National Center for Health Workforce Analysis. Health Workforce Projections: Critical Care Physicians and Nurse Practitioners. 2016. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/critical-care-fact-sheet.pdf. Accessed September 7, 2018
- (24).Health Forum LLC. AHA Hospital Statistics 2017 Edition. 2017. Health Forum, LLC, an affiliate of the American Hospital Association. Chicago, IL. [Google Scholar]
- (25).Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use, and costs. Crit Care Med 2004. June;32(6):1254–9. [DOI] [PubMed] [Google Scholar]
- (26).Halpern NA, Pastores SM. Critical care medicine in the United States 2000–2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med 2010;38(1):65–71. [DOI] [PubMed] [Google Scholar]
- (27).Metropolitan and Micropolitan Areas. United States Census Bureau; Available from: https://www.census.gov/programs-surveys/metro-micro.html. Accessed May 15, 2018 [Google Scholar]
- (28).American Board of Internal Medicine. 2017. Philadelphia, PA. Available at: http://www.abim.org/~/media/ABIM%20Public/Files/pdf/statistics-data/candidates-certified-all-candidates.pdf. Accessed May 15, 2018 [Google Scholar]
- (29).Association of American Medical Colleges. 2016 Physician Specialty Data Report (Table 1.1 Number of Active Physicians in the Largest Specialties by Major Professional Activity, 2015). Available from: https://www.aamc.org/data/workforce/reports/458480/1-1-chart.html. Accessed May 15, 2018
- (30).Society of Critical Care Medicine. Critical Care Statistics. Society of Critical Care Medicine. 2015. Mount Prospect, IL. Available from:http://www.sccm.org/Communications/Critical-Care-Statistics. Accessed May 15, 2018 [Google Scholar]
- (31).Health Forum LLC. AHA Hospital Statistics 2012 Edition. Health Forum, an American Hospital Association Company. Chicago, IL, [Google Scholar]
- (32).Sweigart JR, Aymond D, Burger A, Kelly A, Marzano N, Mcllraith T, Morris P, Williams MV, Siegal EM. Characterizing Hospitalist Practice and Perceptions of Critical Care Delivery. J Hospital Med 13[1], 6–12. 2018. [DOI] [PubMed] [Google Scholar]
- (33).Ward NS, Afessa B, Kleinpell R, Tisherman S, Ries M, Howell M, Halpern N, Kahn J. Intensivist/patient ratios in closed ICUs: a statement from the Society of Critical Care Medicine Taskforce on ICU Staffing. Crit Care Med 2013. February;41(2):638–45. [DOI] [PubMed] [Google Scholar]
- (34).Gershengorn HB, Harrison DA, Garland A, Wilcox ME, Rowan KM, Wunsch H. Association of Intensive Care Unit Patient-to-Intensivist Ratios With Hospital Mortality. JAMA Intern Med 2017. March 1;177(3):388–96. [DOI] [PubMed] [Google Scholar]
- (35).Pastores SM, Halpern NA, Oropello JM, Kostelecky N, Kvetan V. Critical Care Organizations in Academic Medical Centers in North America: A Descriptive Report. Crit Care Med 2015. August 7;43(10):2239–44. [DOI] [PubMed] [Google Scholar]
- (36).van Diepen S, Fordyce CB, Wegermann ZK, Granger CB, Stebbins A, Morrow DA, Solomon MA, Soble J, Henry TD, Gilchrist IC, Katz JN, Cohen MG, Newby LK. Organizational Structure, Staffing, Resources, and Educational Initiatives in Cardiac Intensive Care Units in the United States: An American Heart Association Acute Cardiac Care Committee and American College of Cardiology Critical Care Cardiology Working Group Cross-Sectional Survey. Circ Cardiovasc Qual Outcomes 2017. August;10(8):e003864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Na SJ, Chung CR, Jeon K, Park CM, Suh GY, Ahn JH, Carriere KC, Song YB, Choi JO, Hahn JY, Choi JH, Choi SH, On YK, Gwon HC, Jeon ES, Kim DK, Yang JH. Association Between Presence of a Cardiac Intensivist and Mortality in an Adult Cardiac Care Unit. J Am Coll Cardiol 2016. December 20;68(24):2637–48. [DOI] [PubMed] [Google Scholar]
- (38).Halpern NA, Pastores SM. Critical Care Medicine Beds, Use, Occupancy, and Costs in the United States: A Methodological Review. Crit Care Med 2015. August 25;43(11):2452–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.