Abstract
An expert committee was formed to reach consensus on the use of tilt table testing (TTT) in the diagnosis of disorders that may cause transient loss of consciousness (TLOC) and to outline when other provocative cardiovascular autonomic tests are needed. While TTT adds to history taking, it cannot be a substitute for it. An abnormal TTT result is most meaningful if the provoked event is recognised by patients or eyewitnesses as similar to spontaneous events. The minimum requirements to perform TTT are a tilt table, a continuous beat-to-beat blood pressure monitor, at least one ECG lead, protocols for the indications stated below and trained staff. This basic equipment lends itself to the performance of (1) additional provocation tests, such as the active standing test, carotid sinus massage and autonomic function tests; (2) additional measurements, such as video, EEG, transcranial Doppler, NIRS, end-tidal CO2 or neuro-endocrine tests; and (3) tailor-made provocation procedures in those with a specific and consistent trigger of TLOC. TTT and other provocative cardiovascular autonomic tests are indicated if the initial evaluation does not yield a definite or highly likely diagnosis, but raises a suspicion of (1) reflex syncope, (2) the three forms of orthostatic hypotension (OH), i.e. initial, classic and delayed OH, as well as delayed orthostatic blood pressure recovery, (3) postural orthostatic tachycardia syndrome or (4) psychogenic pseudosyncope. A therapeutic indication for TTT is to teach patients with reflex syncope and OH to recognise hypotensive symptoms and to perform physical counter manoeuvres.
Keywords: Transient loss of consciousness, Syncope, Tilt table testing, Vasovagal, Reflex syncope, Orthostatic hypotension, Psychogenic pseudosyncope
Introduction
Tilt table testing (TTT), while initially developed to study physiological compensatory responses to orthostatic stress, proved useful as a diagnostic test for vasovagal syncope (VVS) in 1986 [1]. TTT is now widely used in clinical practice with a variety of protocols, variants and extensions. On 6 July 2018, the European Federation of Autonomic Societies (EFAS) organised a round table discussion to obtain consensus on the use of TTT in the diagnosis of disorders that may cause transient loss of consciousness (TLOC) and to outline when other provocative cardiovascular autonomic tests are needed. The 2018 guidelines of the European Society of Cardiology [2] and the 2011 EFAS/American Autonomic Society (AAS) Consensus paper [3] were used as starting points. Definitions of various conditions and tests are used as presented in these sources, where necessary preference was given to the more recent ESC guidelines. Two authors (RDT and JGvD) searched PubMed for additional articles from 2014, with the keywords ‘tilt table’ AND ‘syncope’ OR ‘orthostatic intolerance’ (449 hits). We also cite occasional earlier articles and reviews, when these are relevant. The resulting consensus statement was reviewed by all participants, discussed at a second session on 30 June 2019, a third session on 27 January 2020, and sent for endorsement to the autonomic nervous system (ANS) panel of the European Academy of Neurology (EAN). This consensus statement reflects the opinion of experts in the field, but is not a formal evidence-based clinical guideline.
Indications
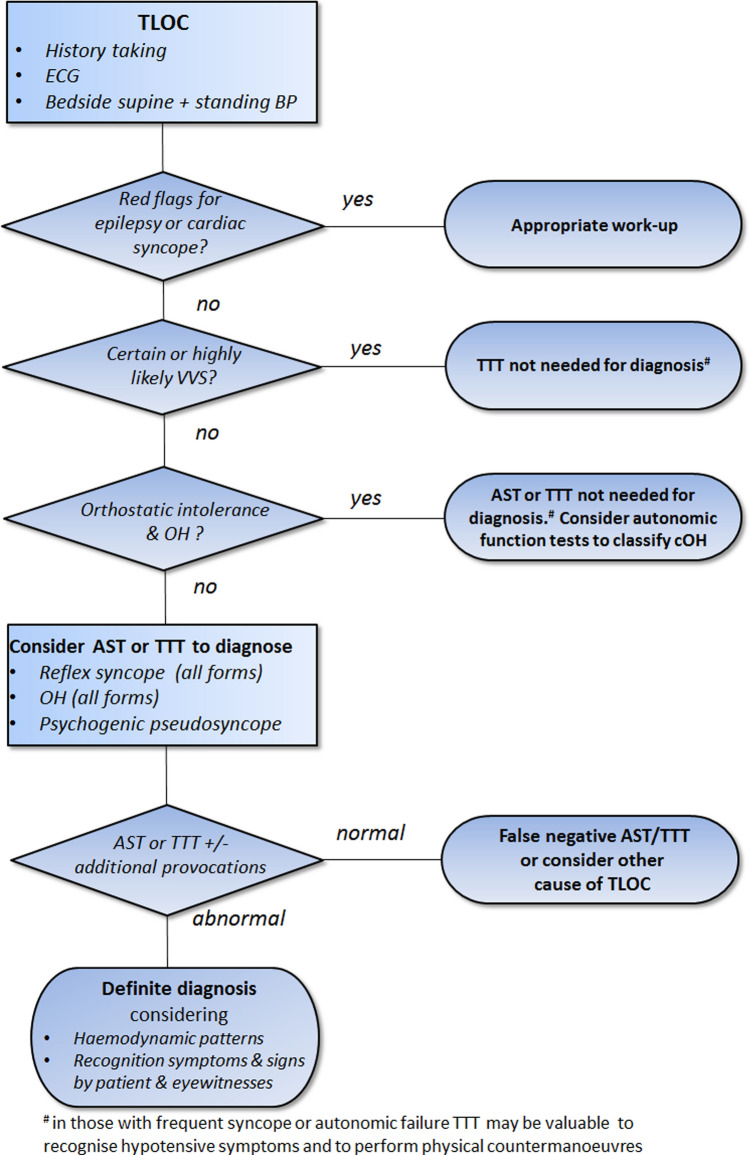
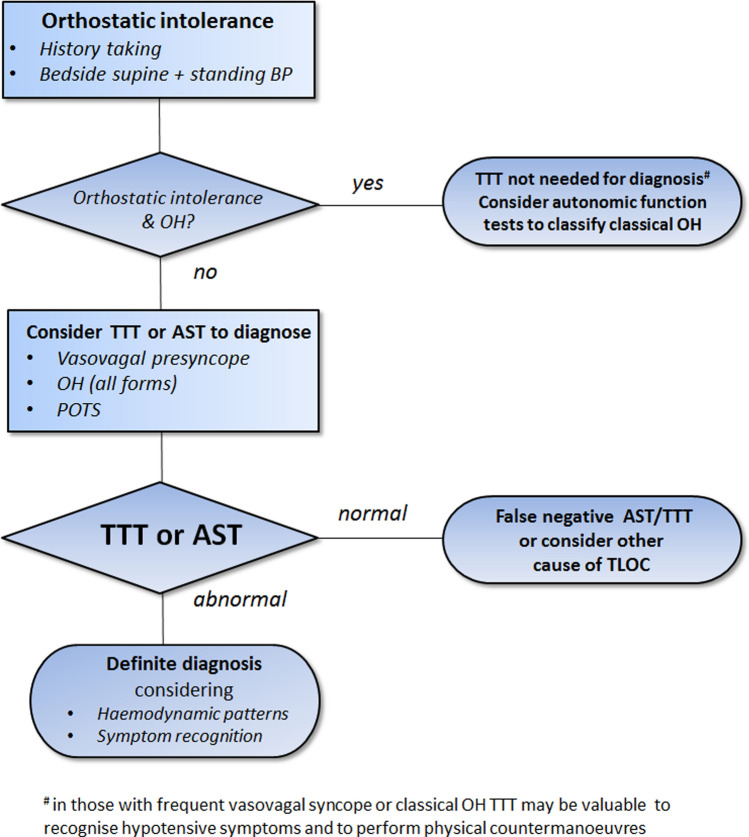
TTT and other provocative cardiovascular autonomic tests primarily aim to obtain a pathophysiological correlate for orthostatic intolerance and TLOC. The fundamental tool for the differential diagnosis is history taking of patients and eyewitnesses [2, 4]. TTT may provide an important addition to history taking if the initial evaluation does not yield a definite or highly likely diagnosis. TTT should neither be used as a substitute for history taking nor isolated from history taking. Figure 1 shows a pragmatic approach, beginning with the initial evaluation of TLOC including history taking, ECG and bedside orthostatic blood pressure measurements. Figure 2 provides a flow chart for the work-up of patients with orthostatic intolerance.
Fig. 1.
Flow chart of the diagnostic work-up following the initial evaluation of transient loss of consciousness (TLOC), i.e. history taking, ECG and bedside supine and standing blood pressure measurements. AST active standing test with continuous blood pressure measurements, BP blood pressure, cOH classic orthostatic hypotension, CSM carotid sinus massage, TLOC transient loss of consciousness, TTT tilt table testing, VVS vasovagal syncope
Fig. 2.
Flow chart of the diagnostic work-up of orthostatic intolerance, i.e. history taking and supine and standing blood pressure measurements. AST active standing test with continuous blood pressure measurements, classic OH classical orthostatic hypotension, POTS postural orthostatic tachycardia syndrome, TTT tilt table testing
To obtain a pathophysiological correlate for orthostatic intolerance and TLOC
The primary aim of TTT is to provoke an event with complaint recognition and to demonstrate the pathophysiological correlate [2, 5]. These aspects are both crucial: recognition may concern subjective sensations reported by patients as well as visible aspects, such as changes in facial colour or movements, recognised by eyewitnesses as similar to spontaneous ones. Together with demonstration of pathophysiological measurements, a clinical-pathophysiological correlate is obtained, thereby proving the cause of TLOC. For most indications, TTT relies on prolonged orthostatic stress in the near-vertical position (‘head-up tilt’). TTT is not useful for all TLOC forms, as epileptic seizures and cardiac syncope are not commonly provoked by the upright posture. In contrast, TTT is useful for diagnosing syncope forms with an orthostatic component, i.e. reflex syncope and syncope due to orthostatic hypotension. TTT is also useful to provoke psychogenic TLOC, i.e. short-lasting apparent unconsciousness due to conversion. TTT can provide a definite diagnosis of psychogenic TLOC by excluding epilepsy or syncope. In the elderly it may be difficult to distinguish between falls with and without loss of consciousness. Hence, TTT may be used to investigate unexplained falls in the elderly, as these may be due to syncope [6, 7].
The role of TTT in diagnosing vasovagal syncope (VVS) has been debated [8–11]. The yield of a certain or highly likely diagnosis with history taking following an initial evaluation by hospital physicians and long-term follow-up as a reference may amount to 60%, with an accuracy of about 90% [12]. The diagnostic yield can increase to as much as 85% with additional history taking by an expert in syncope [13]. In view of these findings, TTT is not needed in the majority of cases presenting with syncope. Another concern is the specificity of TTT. Syncope during TTT reflects a tendency towards hypotension due to low preload in the upright position, rather than a specific diagnosis [14]. TTT modulates the occurrence not only of orthostatic VVS, but also of other forms of syncope such as cardiac syncope [14]. TTT should therefore only be performed after a careful and detailed medical history and examination. The results of the test should be interpreted in the context of that history and examination. Estimates of sensitivity (overall 59%; 95% CI 53–64%; range 21–72%) and specificity (overall 91%; 95% CI 87–93%) of TTT in diagnosing VVS differ [15]. Important factors contributing to the variability relate to the specific test protocol (e.g. the use of pharmacological provocation, tilt angle, duration of TTT, etc.), interpretation of the results, meaning whether complaint recognition or pathophysiological measurements are used as the standard to judge abnormality, and the lack of an agreed reference standard other than long-term follow-up [2, 5, 15, 16]. The most marked contrasts are seen between 'passive' TTT, i.e. upright tilt without pharmacological provocation [sensitivity 37%; (95% CI 29–46%); specificity 99% (95% CI 97–99%)], and ‘active’ protocols [e.g. nitroglycerin provocation sensitivity 66% (95% CI 60–72%); specificity 89% (95% CI 84–92%) [15]. As TTT relies predominantly on the orthostatic, literally meaning ‘upright’, position, TTT indications comprise the conditions bundled under ‘orthostatic intolerance’ [2, 5, 16]. Orthostatic intolerance includes all three forms of OH (i.e. initial, classic and delayed OH), delayed orthostatic BP recovery, orthostatic VVS and postural orthostatic tachycardia syndrome (POTS). Although some forms of reflex syncope, e.g. emotional VVS and cough syncope, primarily rely on other triggers, subjects with these forms are often also susceptible to orthostatic VVS [17, 18]. TTT may therefore still help to provoke syncope in these cases. In other cases, specific additional provocations may be needed to provoke TLOC.
The role of TTT and other provocative cardiovascular autonomic tests is similar for the three forms of orthostatic hypotension (OH), i.e. initial, classic and delayed, in that a definite diagnosis can be made when complaint recognition coincides with the type of BP decrease that is specific for each form (Table 1). The three forms may, however, require specific test protocols: (1) initial OH is commonly not provoked by passive tilt, but requires an active standing test with continuous BP measurements [19, 20]; (2) classic OH is most commonly screened at bedside with intermittent BP measurements, but can also be assessed with TTT or an active standing test [21]; delayed OH may require prolongation of the test protocol to allow a blood pressure decrease to occur [21–23]. Note that classic OH and presumably delayed OH often fluctuate in severity, so the absence of complaints and a blood pressure decrease during the test do not exclude OH (Table 2) [2, 21]. Conversely, the finding of classic OH does not automatically provide an explanation for orthostatic intolerance or TLOC, as it is a common finding affecting up to one in five community-dwelling elderly [2, 24]. When there is such a discrepancy between measurement results and complaints, the question of whether the measured OH represents a clinically relevant finding critically depends on the clinical presentation. When doubt remains, home measurements during complaints may settle the issue.
Table 1.
| TTT/AST indication | Fall in SBP upon standing | Fall in DBP upon standing | Increase in HR upon standing | Timing |
|---|---|---|---|---|
| Initial OH | > 40 mmHg | > 20 mmHg | Not specified | Transient BP fall within 15 s upon standing |
| Classic OHa,b | ≥ 20 mmHgf | ≥ 10 mmHg | Not specifiedc | Sustained BP fall within 3 min standing |
| Delayed OHa | ≥ 20 mmHg | ≥ 10 mmHg | Not specified | Sustained BP fall > 3 min standing |
| POTSd | SBP fall not meeting OH criteria | DBP fall not meeting OH criteria | > 30 bpme or > 120 bpm | Sustained HR increase within 10 min standing |
| Vasovagal presyncope | No formal criteriag | No formal criteriag | No formal criteriag | No formal criteriag |
| Delayed orthostatic BP recovery | Inability of SBP to recover to supine values within 30 s of standing. Standing SBP should be ≥ 20 mmHg lower than supine values but not meet criteria of classic or initial OH | Not meeting initial OH/classic OH criteria | Not specified | BP fall within 30 s upon standing |
AST active standing test, classic OH classical orthostatic hypotension, DBP diastolic blood pressure, delayed OH delayed orthostatic hypotension, HR heart rate, initial OH initial orthostatic hypotension, POTS postural orthostatic tachycardia syndrome, SBP systolic blood pressure, TTT tilt table test
aBP fall should be sustained to avoid confusion with transient BP falls seen in initial OH or VVS
bPlease note that the ESC guidelines [2] added an additional (optional) criterion of SBP < 90 mmHg, as these values are strongly associated with the occurrence of symptoms. An abnormal orthostatic fall in DBP without an abnormal fall in SBP is rare among patients with syncope and orthostatic intolerance [86]
cA ΔHR/ΔSBP ratio < 0.5 bpm/mmHg argues for neurogenic OH [27]
dPOTS is a clinical diagnosis and requires symptoms of orthostatic intolerance and the documentation of an exaggerated postural tachycardia using TTT or an active standing test
eFor individuals aged 12–19 years, the required increment is > 40 bpm
fFor patients with supine hypertension, a reduction in SBP ≥ 30 mmHg is required, as the magnitude of the orthostatic BP fall is dependent on the baseline BP
gNo formal criteria to differentiate between vasovagal (pre)syncope and other causes of presyncope. The haemodynamic patterns associated with vasovagal (pre)syncope are heterogeneous [30] and may or may not be accompanied by HR slowing. Various criteria have been proposed to differentiate between subtypes
Table 2.
Association of orthostatic intolerance and orthostatic hypotension [2]
Reproduced with permission from the 2018 ESC Guidelines for the diagnosis and management of syncope
| History of syncope and orthostatic complaints | |||
|---|---|---|---|
| Highly suggestive of OH (pre)syncope present during standing, absent while lying, and less severe or absent while sitting; a predilection for the morning; sitting or lying down must help; complaints may get worse after exercise, after meals or in high temperatures; no signs of ‘autonomic activation’ (sweating, nausea, etc.) | Possibly due to OH not all of the features highly suggestive of OH are present | ||
| Supine and standing BP measurement | Symptomatic abnormal BP fall | Syncope is due to OH | Syncope is likely due to OH |
| Asymptomatic abnormal BP fall | Syncope is likely due to OH | Syncope may be due to OH | |
| No abnormal BP drop | Unproven | Unproven | |
BP blood pressure, OH orthostatic hypotension
A diagnosis of psychogenic TLOC preferably requires documentation of an event, for which video or video-EEG recordings provide the most convincing evidence. History taking often raises a strong suspicion of psychogenic TLOC, but may not always be reliable enough to rule out other causes of TLOC [25]. The use of video-EEG is particularly important to exclude epilepsy when the clinical event is accompanied by positive motor phenomena [25]. Note that a normal EEG during a provoked event excludes syncope with certainty, but need not exclude all possible forms of epilepsy. It does, however, exclude those forms of epilepsy that present with TLOC, i.e. tonic, clonic and tonic–clonic seizures [26]. A diagnosis of psychogenic TLOC can also be established on clinical grounds if a clinician witnesses the event and observes features favouring psychogenic TLOC (e.g. eye closure, resisted eye-opening, partial responsiveness during the event, etc.) [25].
To classify classic OH
TTT and other autonomic tests (active standing test, Valsalva manoeuvre and deep breathing) may help to distinguish between neurogenic and non-neurogenic causes for classic OH and to identify sympathetic or parasympathetic dysfunction in those with neurogenic OH [2, 21, 27, 28]. A blunted heart rate increase during classic OH makes a neurogenic cause more likely. A ΔHR/ΔSBP ratio < 0.5 bpm/mmHg argues for neurogenic OH (sensitivity 91%; specificity 88% AUC = 0.96) [27]. It should be noted, however, that cardiac disorders (e.g., pacemaker, arrhythmias, etc.) or certain drugs may preclude heart rate augmentation; thus an ECG, cardiac history and a medication review should be part of the evaluation of classic OH [21]. Specialised autonomic function tests including responses to deep breathing and Valsalva manoeuvre may also help to diagnose neurogenic OH as well as to identify sympathetic or parasympathetic dysfunction in those with neurogenic OH [2, 21, 28–31]. The absence of a blood pressure overshoot and the absence of a heart rate increase during the Valsalva manoeuvre is pathognomonic for neurogenic classic OH. There is also consensus that a blunted or abolished heart rate variation during deep breathing is suggestive of neurogenic classic OH. Interpretation of these findings requires age-adjusted, normative values [31].
Treatment
TTT is not completely restricted to diagnosis. Patients may exhibit a decrease in syncope frequency after TTT, which may be due to patients having learned to recognise early signs of syncope, allowing them to take measures to prevent it [32]. TTT may easily be expanded with a biofeedback session to teach the ‘counter manoeuvres’ [33, 34]. This session can be performed when subjects are still symptomatic after syncope, thus allowing strong feedback regarding the effectiveness of these interventions. The session is also extremely important for patients’ education, as patients can see their own blood pressure fluctuate and discover which manoeuvres decrease (e.g., squat-to-stand) and which manoeuvres increase (e.g., leg crossing) their blood pressure. Applying these measures using biofeedback reduces the recurrence risk in patients with reflex syncope by 39% compared to conventional treatment only, i.e. explanation and life-style advice [33]. Patients with definite VVS and no need for additional testing could be referred to an animated video on physical counter manoeuvres [35]. TTT also allows the study of the temporal relation between onset of asystole and TLOC in those with asystolic VVS and helps to guide pacemaker recommendations. In one-third of cases of tilt-induced asystolic reflex syncope, asystole occurred too late to have been the primary cause of TLOC, thus making pacemaker implantation likely ineffective [36].
Recommendations
TTT should be considered
-
To increase the probability of a diagnosis of reflex syncope
This holds for those in whom the initial evaluation, including history taking, ECG, and supine and standing blood pressure measurements raised a suspicion but not a definite or highly likely (probability 80–100%) diagnosis, or in those in whom confirmation of a diagnosis is required for other purposes, such as convincing patients, parents or medicolegal requirements.
-
To assess classic OH and delayed OH
The recommended screening test for classic OH is a bedside active standing test with conventional intermittent BP measurements. TTT or an active standing test with continuous BP measurements should be considered if the bedside test does not show classic OH while the symptoms suggest classic OH (Table 2) [2]. TTT is particularly useful in detecting delayed OH, i.e. those with a sustained blood pressure fall of the magnitude of classic OH, but occurring later than 3 min upon standing [3, 22]. TTT may also be used to diagnose classic OH in subjects for whom active standing is difficult or unlikely to succeed, such as frail elderly and patients with significant motor impairments.
-
To support a clinical diagnosis of POTS [3, 37]
Documentation of an exaggerated postural tachycardia using TTT or an active standing test may support a clinical diagnosis of POTS.
To differentiate between syncope with myoclonus (‘convulsive’ syncope) and tonic–clonic seizures [38].
-
To discriminate between neurogenic and non-neurogenic classic OH
A blunted heart rate increase during classic OH makes a neurogenic cause more likely. A ΔHR/ΔSBP ratio < 0.5 bpm/mmHg argues for neurogenic OH [27].
To differentiate between vasovagal syncope and psychogenic TLOC [39, 40].
-
To study the timing between asystole and the onset of TLOC
Asystole in VVS may occur too late to have been the prime cause of TLOC, making pacemaker implantation likely ineffective [36].
To teach patients with reflex syncope and orthostatic hypotension to recognise hypotensive symptoms and how to perform physical counter manoeuvres [33, 34].
Counter manoeuvres are effective measures to counteract impending reflex syncope or syncope due to orthostatic hypotension. Applying these measures using biofeedback reduces recurrence risk in patients with reflex syncope by 39% compared to conventional treatment (i.e. explanation and lifestyle advice) [33].
TTT should not be used
-
To evaluate the treatment of reflex syncope
TTT should not be used for the routine clinical evaluation of treatment efficacy, although it might have a role in the evaluation of treatment approaches for reflex syncope in the research context [2, 11].
-
To exclude cardiac syncope
Syncope during TTT suggests the presence of hypotensive susceptibility. This tendency is common and modulates the occurrence not only of orthostatic VVS, but also of other forms of syncope such as cardiac syncope [14].
-
To exclude VVS
The sensitivity of TTT, especially TTT without pharmacological provocation, is too low to exclude VVS [14, 15].
To diagnose initial OH
Documentation of initial OH requires an active standing test with a beat-to-beat blood pressure monitor (see paragraph 5.2) [19, 20, 41].
Indications for additional provocations and measurements
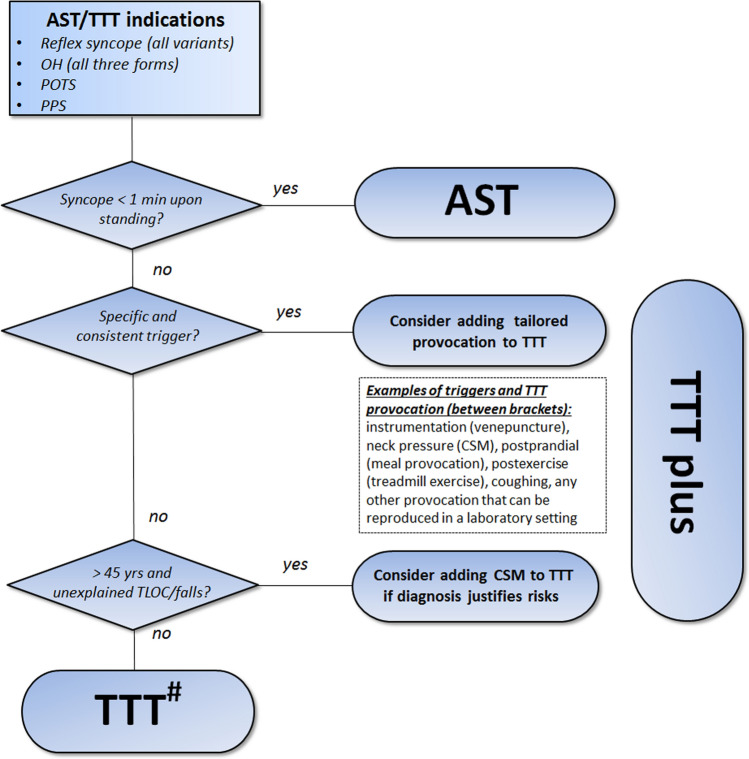
The committee recommends that additional provocations and measurements are tailored to the patient's needs. Figure 3 provides guidance as to when these auxiliary measures could be considered. Recommendations for TTT protocols and supplementary measurements are summarised in Table 3 and detailed in the following section.
Fig. 3.
Choice of type of tilt table testing (TTT) protocol. #Pharmacological provocation with sublingual trinitroglycerin (TNG) may be considered to increase the sensitivity for VVS but should be avoided in those for whom delayed OH is suspected. AST active standing test with continuous blood pressure measurements, CSM carotid sinus massage, OH orthostatic hypotension, POTS postural orthostatic tachycardia syndrome, PPS psychogenic pseudosyncope, TTT tilt table testing
Table 3.
TTT protocols and supplementary measurements for each TTT indication
| TTT indication | Duration of tilta | Pharmacological provocation | Additional measurements |
|---|---|---|---|
|
Orthostatic intoleranceb - Classic OH - POTS - Delayed OH - Vasovagal presyncope |
At least 10 min - 3 min - 10 min - Up to 40 min - Up to 45 min |
Not recommended |
Optional Video, EEG, Respiratory, TCD, Catecholamines |
|
Transient loss of consciousness - Reflex syncope - PPS |
Up to 45 minc | Optional |
Optional Video, EEG, Respiratory, NIRS, TCD |
Classic OH classical orthostatic hypotension, delayed OH delayed orthostatic hypotension, LBNP lower body negative pressure, NIRS near-infrared spectroscopy, POTS postural orthostatic tachycardia syndrome, PPS psychogenic pseudosyncope, TCD transcranial Doppler
aTTT should be terminated earlier in the event a clinical endpoint (i.e. (pre)syncope) is reached
bPlease note that an active standing test may also be used to establish a diagnosis in patients with orthostatic intolerance (see ‘Indications’ in the main manuscript)
cIn the case of pharmacological provocation (TNG), TTT may be shortened to 40 min (20 min before and 20 min after TNG administration)
Equipment
Basic equipment
Beat-to-beat blood pressure monitor
In the context of syncope, blood pressure (BP) can change substantially in a few seconds, so it must be measured with an appropriate temporal resolution. Conventional intermittent BP measurements allow one measurement per minute at best and are therefore unsuitable for syncope assessment. Classic OH and delayed OH are, however, accompanied by sustained decrease in BP lasting minutes, and hence can be detected with conventional intermittent BP measurements [19, 21, 42]. Delayed OH, however, often occurs after 10 min of passive standing [22]. TTT is therefore more appropriate for identifying delayed OH. In frail elderly and those with major motor impairments, TTT may also be preferred over active standing to prevent falling. Several commercial devices are available for non-invasive beat-to-beat measurements of blood pressure and heart rate using finger photoplethysmography and the volume clamp method [43]. Additional software yields estimates of other circulatory parameters including stroke volume, cardiac output and total peripheral resistance; these may be used to quantify the relative contributions of vasodilation and cardioinhibition [44], but this is not required for routine clinical testing.
ECG
At least one ECG channel is required to detect bradycardia or asystole and to identify its underlying mechanism (e.g. intermittent AV block) [45, 46].
Tilt table
The tilt-down time should preferably be short for syncope, as longer times may lengthen circulatory arrest and thus the duration of cerebral hypoperfusion [47]. The optimal time is not known. The panel recommends the tilt-back period from 70° to horizontal should be less than 15 s. The subject should be protected against falling with safety straps, with at least one strap at the chest and one above the knee.
Equipment extensions
Video and EEG recordings
For reflex syncope, adding video to TTT has the advantage that key clinical events that usually last less than 20 s can be studied in detail after the fact. Adding EEG provides additional guidance in control over the tilt procedure in that slowing of the EEG should always result in tilting the patient back; in reverse, tilting back is not yet needed if the EEG is still normal. The EEG pattern consists of either slowing or a slow-flat-slow pattern; this provides information about the degree of cerebral perfusion [38, 48]. Adding video and EEG has limited clinical value in OH because TTT in OH forms rarely induces syncope, and if complaints occur, these usually concern presyncope only, not usually accompanied by EEG changes.
For psychogenic TLOC, video and EEG recordings during TTT are very important, as they enable a definite diagnosis of psychogenic TLOC [2, 39, 40] and recognition of mixed presentations of psychogenic pseudosyncope and VVS [40]. A complete clinical identification of the presence of TLOC requires assessment of loss of responsiveness, abnormal motor control, amnesia for the period of apparent unconsciousness and a short duration [2, 26]. Adding video allows these phenomena to be assessed with certainty. The addition of EEG helps to confirm the presence of normal brain activity during psychogenic TLOC and thereby to exclude TLOC due to syncope (slowing and/or flattening) or epilepsy (epileptiform abnormalities). Video without EEG does allow a highly probable diagnosis of psychogenic pseudosyncope, i.e. attacks with loss of muscle tone but without jerking movements, by proving that the recorded event fulfils the clinical criteria of TLOC in the absence of hypotension [25, 39, 40]. If TLOC is accompanied by stiffening or jerks, however, additional EEG recordings are recommended to discriminate between psychogenic non-epileptic seizures and epileptic seizures [25]. A diagnosis of psychogenic TLOC can also be established on clinical grounds if a clinician witness observed TLOC and documented examination findings typically found in psychogenic TLOC (e.g. eye closure, resisted eye-opening, partial responsiveness during the event, etc.) [25].
Adding video-EEG to TTT can be accomplished by using an EEG machine to record and store all signals, including the output from the beat-to-beat BP monitor. As this is easily accomplished in a neurological setting, the panel encourages adding video and EEG to most TTT procedures. The video should record facial expression to assess eye closure and skin colour and, preferably, the upper extremities to evaluate the presence of jerking movements.
Respiratory recordings
Respiration can be recorded using strain gauges around the thorax or abdomen, blood oxygen saturation and end-tidal CO2. Of these, CO2 recordings may offer the most insight. CO2 recordings are useful to detail the pathophysiological cascade, as hypocapnia may precede reflex syncope [49]. Adding CO2 recordings to TTT may also be of clinical interest, as it may help to identify POTS subtypes that are consequent upon postural hyperventilation [50] or episodes of hyperventilation in those who report dizziness without concomitant hypotension [51].
Blood sampling
Blood sampling of neuro-endocrine substances holds promise as a means to improve pathophysiological understanding [21, 52–54]. Measuring catecholamines before and after head-up tilt offers insights into baroreflex-mediated sympathetic activation, mostly to help distinguish between causes of neurogenic OH such as pure autonomic failure, Parkinson's disease and multiple system atrophy, and to classify POTS variants [21, 52–55]. Catecholamine assessments may also help to predict conversion from pure autonomic failure to multiple system atrophy [56]. The measurements require placement of an indwelling venous line and established protocols regarding the material (cooling, centrifugation and type of assay) and TTT, as the catheter implies a needle to obtain venous or arterial access and may thereby provoke VVS. To avoid this, a longer period of supine rest is recommended before tilt up. The panel recommends restricting the use of catecholamine assays to those with a diagnosis of neurogenic OH where the clinical work-up fails to discriminate between pre- and postganglionic causes.
Transcranial Doppler (TCD)
TCD monitoring during TTT aids in the assessment of alterations in cerebral blood flow velocity at a high temporal resolution. This is of interest for investigating the pathophysiology of syncope [57], but has so far been of no help in the differential diagnosis of orthostatic intolerance or TLOC. TCD monitoring has been advocated as an additional tool to help establish psychogenic pseudosyncope [58].
Near-infrared spectroscopy (NIRS)
Near-infrared spectroscopy of the brain reflects the relative amount of deoxygenated blood in the scalp and brain. At present, the technique shows promise. as it suggests that decreased brain perfusion may be identified prior to clinical manifestations [59, 60].
TTT protocols
Classic TTT
We first present classic TTT and then discuss all variants and extensions that can be performed using the same equipment. The choice of the TTT protocol will depend on the clinical presentation (Figs. 2, 3).
Indication reflex syncope
Several protocols for TTT have been reported with or without pharmacological challenges [15, 61]. The available evidence suggests that 30–60 min is optimal for the diagnosis of VVS [2, 5, 15]. The panel did not reach consensus as to whether TTT should be performed with or without pharmacological provocation. While the majority of the panel preferred to perform TTT for 45 min without pharmacological provocation, there is evidence that pharmacological provocation increases sensitivity, with a minimal effect on the number of false positive results [15, 62]. For pharmacological provocation, we advocate against the use of intravenous isoproterenol and instead recommend sublingual trinitroglycerin (TNG) (300–400 mcg): TNG does not require cannulation and is easier and quicker to administer, while sensitivity and specificity of TNG and isoproterenol are similar [15]. TNG is usually administered in a fixed dose (0.3 or 0.4 mg) rather than a dose based on body mass. It is not known at which mass side effects become a limiting factor, but the panel discourages the use TNG in those with a mass below 50 kg. Arguments favouring TNG provocation include the increased sensitivity for VVS [sensitivity 66% (95% CI 60–72%) vs passive TTT (37%; (95% CI 29–46%)] [15]. TNG may also impact specificity, albeit to a lesser extent. The lower specificity of the TNG protocols [89% (95% CI 84–92%) vs passive 99% (95% CI 97–99%)] requires a critical evaluation of whether the provoked event resembles the spontaneous one. Another drawback of TNG provocation is that it may provoke delayed OH. This is of particular concern in those with orthostatic (pre)syncope without specific clues for VVS or delayed OH (e.g. orthostatic (pre)syncope without autonomic activation in an elderly subject). Another factor to consider is the health care setting, as in some countries application of TNG for diagnostic purposes may be restricted or require a specific clinical environment.
Lower body negative pressure (LBNP) is an alternative non-pharmacological measure to provoke syncope during TTT. While LBNP has been studied extensively to assess haemodynamic responses to orthostatic stress, little is known of the validity of LBNP to detect VVS in patients with unexplained TLOC [63, 64]. This does not mean that LBNP cannot be useful in this context, but its clinical value has not yet been proven.
Supine rest phase of at least 5 min with reliable and constant BP and HR values as a baseline.
Head-up tilt angle between 60° and 80°, measured from the horizontal [15]. At 60°, 70° and 80°, the force component pulling blood towards nether parts of the body presents 0.87, 0.94 and 0.98 of that of the fully vertical position. The positive yield of TTT seems optimal at 70°, as the sensitivity is higher compared with TTT at 60° and 80° [15].
TTT without pharmacological provocation: head-up tilt for 45 min,
TTT with pharmacological provocation: start with 20 min head-up tilt, followed by administration of TNG in the tilted position and continuation for another 20 min,
TTT can be terminated when clinical events occur or, in case no symptoms are provoked, when the end of the recording period is reached. Which symptoms can serve as an endpoint will critically depend on the clinical context. Presyncope may be used as an endpoint in cases with a high pre-test likelihood of reflex syncope; patients may then be tilted back when recognised complaints are accompanied by hypotension. When the a priori probability is low, or when syncope with myoclonus needs to be distinguished from a convulsive seizure, syncope should be the endpoint. The decision to tilt back should be taken by someone with direct access to the patient and all recorded signals. The presence of asystole or EEG slowing, if recorded, is always a reason to tilt back immediately.
A key element of TTT is to ask patients for recognition of symptoms. Eyewitnesses may confirm whether the provoked event resembled the spontaneous episodes, which may help to reduce false positive results.
Indication OH
Pharmacological provocation should not be used for any form of OH. Initial OH is not a reason for a TTT, but requires an active standing test with continuous blood pressure measurements. TTT may be used for those with orthostatic intolerance (1) when the active standing test does not reveal classic OH, (2) when delayed OH is suspected at history taking or (3) when a complaint correlation is needed. The TTT duration may be tailored to individual needs. Syncope occurs rarely in classic or delayed OH during TTT and should not be the primary endpoint.
Supine rest phase of at least 5 min before head-up tilt, with reliable and constant BP and HR values as a baseline. Supine measurements can be used to assess neurogenic supine hypertension [65].
Head-up tilt angle between 60° and 80°, measured from the horizontal.
Head-up tilt of 3 min would suffice to establish a diagnosis of classic OH, but longer TTT may be needed to rule out other causes of OI (e.g. delayed OH, POTS). The diagnosis of delayed OH may require a head-up tilt of up to 45 min [22, 23]. Patients may be tilted back when a complaint correlation is obtained, when syncope occurs or when patients can no longer withstand the head-up position.
Complaint recognition: see above. It is important to note that a mean standing BP < 75 mmHg had optimal sensitivity (97%) and specificity (98%) for detecting symptomatic OH in patients with Parkinson’s disease [66]. The symptom threshold may, however, vary between causes of OH. In a study of patients with diverse causes of OH, many patients were asymptomatic despite a substantial fall in SBP and low orthostatic blood pressure, suggesting that symptoms may not always be a reliable indicator of impaired cerebral perfusion or risk of syncope [67].
Indication psychogenic TLOC
For psychogenic TLOC, pharmacological provocation may be used as for reflex syncope, for two reasons: firstly, VVS occurs more often in psychogenic pseudosyncope than chance predicts [40] and the occurrence of psychogenic TLOC may depend on suggestion [68], which may be aided by a provocation procedure. The same protocol may be used for psychogenic TLOC as for reflex syncope, except for the endpoint.
Ensure a supine rest phase of at least 5 min before head-up tilt.
Head-up tilt angle between 60° and 80°, measured from the horizontal.
Head-up tilt for up to 40 min (pharmacological provocation) or 45 min (no pharmacological provocation).
Pharmacological provocation may be chosen and performed as for reflex syncope.
The test ends when the allotted time has passed or when psychogenic TLOC occurs. As blood pressure is not low and cerebral hypoperfusion is absent in psychogenic TLOC, tilting back may safely be postponed until all symptoms and signs are recognised.
Complaint recognition: see above.
Indication POTS
Documentation of an exaggerated postural tachycardia using TTT or an active standing test may support a clinical diagnosis of POTS. The panel recommends the use of TTT in those with complaints of both orthostatic intolerance and TLOC, as TTT has the advantage of provoking VVS as well. The diagnostic criteria of POTS require a head-up tilt period of 10 min. If other causes of orthostatic intolerance are considered (notably vasovagal presyncope or delayed OH), a longer head-up tilt is needed to establish a diagnosis. As the pathophysiological relation between orthostatic tachycardia and symptoms is as yet unclear, the panel stresses that orthostatic tachycardia without symptoms is a non-specific finding. Dehydration should be considered as an explanation. The test does not aim to provoke syncope, but if it occurs, it should be considered that the initial high heart rate upon standing may be a reflection of compensatory mechanisms and thus an expression of VVS. In such case it would be worthwhile repeating TTT to see whether POTS is a consistent finding.
Ensure a supine rest phase of at least 5 min before head-up tilt, with reliable and constant BP and HR values as a baseline.
Head-up tilt angle between 60° and 80°, measured from the horizontal.
Head-up tilt for 10 min.
The test ends when the allotted time has passed, when 10 min have passed or when syncope inadvertently occurs, in which case the rules for tilting back of reflex syncope apply.
Complaint recognition: see above.
TTT: possible extensions and variants
Active standing test with continuous blood pressure measurements
The active standing test can be used to provoke initial orthostatic hypotension (initial OH), classical OH (classic OH) or POTS, or to demonstrate delayed orthostatic BP recovery. It includes supine rest for at least 5 min followed by 3 min of standing. For a more detailed description of the active standing test, see the recent review by Finucane et al. [19]. A diagnosis of initial OH can be established if a transient BP drop (> 40 mmHg systolic blood pressure or > 20 mmHg diastolic blood pressure) occurs within 15 s of standing. [3] Delayed orthostatic BP recovery is defined as the inability of systolic BP to recover to supine baseline values within 30 s of standing; the orthostatic BP should be ≥ 20 mmHg lower than the supine baseline values, but should not meet the criteria of classic or initial OH [41]. In view of the short duration of the blood pressure decrease in initial OH, the active standing test requires a beat-to-beat blood pressure measurement device. The active standing test can also be used to detect classic OH, as the criteria only require a measurement period of 3 min after standing up. In contrast to initial OH, classic OH or delayed OH can be detected with conventional intermittent BP measurements [42].
Valsalva manoeuvre and deep breathing
Autonomic function tests may help to (1) identify autonomic failure as the underlying cause of classic OH (2) to characterize cardiovascular sympathetic and parasympathetic autonomic function and (3) quantify the severity of autonomic dysfunction [2, 28, 30, 31]. To ensure valid results, it is extremely important that the tests are performed by trained personnel and under controlled circumstances, meaning a quiet and temperature-controlled room; no meals for 3 h before the test, and no vasoactive substances (nicotine or caffeine-, theine-, or taurine-containing drinks) or medications on the day of examination. During the Valsalva manoeuvre, the patient is asked to conduct a maximally forced expiration for 15 s with an open glottis, i.e. with open nose and mouth, or into a closed loop system with a resistance of 40 mmHg. During the deep breathing test, the patient is asked to breathe deeply at six breaths per minute for 1 min.
Carotid sinus massage (CSM)
The diagnostic yield of the TTT can be enhanced by adding carotid sinus massage (CSM). CSM has been advocated in adults over 40 years of age with a history of unexplained reflex syncope or falls, and those in whom TLOC is triggered by head rotation or pressure on carotid sinus [2, 69]. The need for a definite diagnosis should always be weighed against the risk for complications (see “Safety”).
Venepuncture
Adding venepuncture provocation may increase diagnostic yield, especially in those with a history of syncope during instrumentation [17]. If intended for blood sampling during the test it is recommended to be performed at least 20 min before TTT, so as to avoid provocation.
Meal provocation
A meal provocation can be used to diagnose postprandial hypotension [70]. Postprandial hypotension can be detected with conventional intermittent BP measurements. The panel recognises that there is no consensus regarding the definition and the assessment of postprandial hypotension. Most authors define postprandial hypotension as a fall of ≥ 20 mmHg in systolic blood pressure or SBP drop from > 100 mmHg to SBP < 90 mmHg within 2 h after completion of the meal [70]. Various provocations have been used including orally administered glucose, a standard (normal) meal or a mixed liquid meal [70]. Consensus is also lacking regarding the frequency of measurements and the body position during the test (supine, sitting) [70]. The panel recognises the need for uniform definitions and protocols to foster our understanding of postprandial hypotension.
Tailored provocations
A personally tailored provocation may be carried out in those with a specific and consistent trigger of TLOC. Examples include standing still following exercise [71, 72], coughing [18] or bending forward [45]. It should, however, be noted that many specific triggers suggest situational reflex syncope with high confidence and usually do not require diagnostic confirmation. Tailored provocation should therefore be reserved for those with unusual triggers or specific triggers but conflicting ictal signs or symptoms. Some provocation may require precautions to avoid injuries, such as floor mats.
Counter-pressure manoeuvres
The beat-to-beat blood pressure monitor can be used to teach patients suffering from reflex syncope or orthostatic hypotension to recognise hypotensive symptoms and to perform physical counter manoeuvres [33, 34]. Various manoeuvres including leg crossing, handgrip or arm tensing can be taught while patients view the blood pressure response on the monitor [33, 34]. Such training sessions allow tailoring of the manoeuvres. For example, leg crossing may not be feasible for those with movement disorders, but handgrip, arm tensing or tensing of the buttocks may help to improve orthostatic tolerance. Ideally, these manoeuvres are taught when patients experience mild symptoms of OH without the risk of immediate syncope or falls, e.g. immediately following TTT or active standing test.
Patient information
The panel recognises that there is ample literature to support specific patient recommendations to prepare for TTT. It could be considered to instruct patients to refrain from easily preventable vasoactive substances (e.g. caffeinated beverages, tobacco smoking) as this may limit the ability of TTT to provoke symptoms. The recommendation regarding medication fully depends upon the clinical context: if symptoms are likely provoked by medication, the patient should continue the drug regimen. In other cases, it may be necessary to test the patients off medication, as certain drugs may confound the assessment of autonomic functions. In either case, reporting of the drug regimen is important to properly interpret TTT, as drug-induced orthostatic intolerance is a major cause of all three patterns of OH, particularly among the elderly [2, 24]. The panel recommends advising patients to empty the bladder prior to test to avoid sympathetic stress [73] and incontinence in case TTT provokes syncope. Another consideration is the timing of the tests, as TTT is more likely to provoke syncope in the morning hours [74].
Safety
TTT is safe, and major complications are very rare [2, 11, 75, 76]. Although we found no evidence that TTT is harmful, the low blood pressure during syncope might theoretically harm those with ischaemic disorders of the heart or brain, so risks and benefits should be weighed in such patients. There is an association between frequent syncope, defined as five or more syncopal spells during life, with more white matter lesions [77]. The panel felt that the advantages of a definite diagnosis, with possibly fewer future syncopal spells as a result, outweigh the theoretical risk of adding white matter lesions by one syncopal spell during TTT. TTT may provoke atrial fibrillation, but this is usually self-limiting [2]. Other side effects include headache or migraine following TNG challenge.
Complications following CSM are uncommon (< 0.5%) and predominantly involve transient neurological symptoms, while some cases with stroke have been reported [78–83]. One death after CSM resulting from massive brain infarction has, however, been reported [84]. The risks and benefits of CSM therefore have to be carefully weighed. According to the ESC guidelines, CSM should be undertaken with caution in patients with previous stroke, TIA or known carotid stenosis > 70% [2]. The American Heart Association (AHA) and the American College of Cardiology (ACC) guidelines discourage the use of CSM in patients with a carotid bruit, TIA, stroke or myocardial infarction in the preceding months, except if carotid Doppler excludes a significant stenosis [11]. The expert group noticed that the more stringent criteria by the AHA/ACC more closely resemble the selection criteria employed in the studies assessing complication risks (bruits: 3 out of 4 studies; myocardial infarction: 2 out of 4 studies). The expert group feels that the need for a definite diagnosis of carotid sinus hypersensitivity should always be weighed against the risk for complications. Ultrasound investigation of the carotid arteries may be carried out to screen for atherosclerosis. There is, however, no evidence that this approach prevents complications.
Clinical environment
It is strongly recommended that TTT is an integral part of a clinical facility for the diagnosis and management of syncope and related symptoms, with dedicated staff and access to appropriate diagnostics and therapies. A consensus statement of the European Heart Rhythm Association (EHRA) offers guidance on how to set up such a facility [85]. The panel endorses the ESC recommendations regarding TTT performance: the test should be conducted by a physician, technician or a nurse trained in syncope and resuscitation [2]. Clinical TTT should typically be conducted within a clinical environment with established procedures for life-threatening events [85].
Compliance with ethical standards
Conflict of interest
Dr. Thijs reports personal fees from Medtronic, Union Chimique Belge (UCB), GlaxoSmithKline (GSK), Theravance, Novartis and grants from Dutch National Epilepsy Fund, Christelijke Vereniging voor de Verpleging van Lijders aan Epilepsie, AC Thomson Foundation, Medtronic, The Netherlands Organisation for Health Research and Development (843002707), outside the submitted work. Dr Fanciulli reports royalties from Springer Nature Publishing Group and Thieme Verlag, speaker fees from the Austrian Autonomic Society, Austrian Neurology Society, Austrian Parkinson Society, Ordensklinikum Linz, International Parkinson Disease and Movement Disorders Society and Theravance Biopharma, research grants from the Stichting ParkinsonFond, MSA Coalition and the Österreichischer Austausch Dienst, outside the submitted work. Prof Sutton serves as consultant to Medtronic Inc., is a member of the Speakers Bureau of SJM Abbott Laboratories, and shareholder in Edwards Lifesciences and Boston Scientific Corp., outside of the submitted work. Prof Pavy-Le Traon reports a research grant from the French Ministry of Health outside the submitted work. Prof Jordan served as advisor for Novo-Nordisk, Bayer, received research support from Boston Scientific and Boehringer Ingelheim and is cofounder of Eternygen GmbH, outside the submitted work. Prof. Habek participated as clinical investigator, speaker and/or advisor for Biogen, Sanofi Genzyme, Merck, Bayer, Novartis, Pliva/Teva, Roche, Alvogen, Actelion, Alexion Pharmaceuticals, outside the submitted work. Prof Struhal reports consultancy for Boehringer, Eli Lilly, royalties from Manz-Rechtsverlag, Springer, Oxford University Press, speaker fees from Boehringer, Merz, Medconvent, Donau-Universität Krems, Austrian Society of Neurology, Manz-Rechtsverlag. Prof. Hilz received consulting honoraria from Alnylam and Sanofi-Genzyme, lecturing honoraria and travel support from Bayer HealthCare, Amicus, Sanofi-Genzyme, and research funding from Novartis Pharma and Bayer Health Care.
Footnotes
This article is co-published in the journals “Clinical Autonomic Research” and “Autonomic Neuroscience”. 10.1007/s10286-020-00738-6 and 10.1016/j.autneu.2021.102792. These articles are identical except for minor stylistic and spelling differences in keeping with each journal’s style.
References
- 1.Kenny RA, Ingram A, Bayliss J, Sutton R. Head-up tilt: a useful test for investigating unexplained syncope. Lancet (London, England) 1986;1:1352–1355. doi: 10.1016/s0140-6736(86)91665-x. [DOI] [PubMed] [Google Scholar]
- 2.Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martin A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A, van Dijk JG (2018) 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J [DOI] [PubMed]
- 3.Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz I, Schondorff R, Stewart JM, van Dijk JG. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21:69–72. doi: 10.1007/s10286-011-0119-5. [DOI] [PubMed] [Google Scholar]
- 4.Wieling W, van Dijk N, de Lange FJ, Olde Nordkamp LR, Thijs RD, van Dijk JG, Linzer M, Sutton R. History taking as a diagnostic test in patients with syncope: developing expertise in syncope. Eur Heart J. 2015;36:277–280. doi: 10.1093/eurheartj/ehu478. [DOI] [PubMed] [Google Scholar]
- 5.Saal DP, Thijs RD, van Dijk JG. Tilt table testing in neurology and clinical neurophysiology. Clin Neurophysiol. 2016;127:1022–1030. doi: 10.1016/j.clinph.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Heitterachi E, Lord SR, Meyerkort P, McCloskey I, Fitzpatrick R. Blood pressure changes on upright tilting predict falls in older people. Age Ageing. 2002;31:181–186. doi: 10.1093/ageing/31.3.181. [DOI] [PubMed] [Google Scholar]
- 7.Menant JC, Wong AK, Trollor JN, Close JC, Lord SR. Depressive symptoms and orthostatic hypotension are risk factors for unexplained falls in community-living older people. J Am Geriatr Soc. 2016;64:1073–1078. doi: 10.1111/jgs.14104. [DOI] [PubMed] [Google Scholar]
- 8.Sheldon R. Tilt testing for syncope: a reappraisal. Curr Opin Cardiol. 2005;20:38–41. [PubMed] [Google Scholar]
- 9.Kulkarni N, Mody P, Levine BD. Abolish the Tilt Table Test for the Workup of Syncope! Circulation. 2020;141:335–337. doi: 10.1161/CIRCULATIONAHA.119.043259. [DOI] [PubMed] [Google Scholar]
- 10.Sutton R, Fedorowski A, Benditt DG. Letter by Sutton et al regarding article, “Abolish the Tilt Table Test for the Workup of Syncope!”. Circulation. 2020;141:e944–e945. doi: 10.1161/CIRCULATIONAHA.120.046864. [DOI] [PubMed] [Google Scholar]
- 11.Shen WK, Sheldon RS, Benditt DG, Cohen MI, Forman DE, Goldberger ZD, Grubb BP, Hamdan MH, Krahn AD, Link MS, Olshansky B, Raj SR, Sandhu RK, Sorajja D, Sun BC, Yancy CW. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2017;14:e155–e217. doi: 10.1016/j.hrthm.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 12.van Dijk N, Boer KR, Colman N, Bakker A, Stam J, van Grieken JJ, Wilde AA, Linzer M, Reitsma JB, Wieling W. High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: the Fainting Assessment study. J Cardiovasc Electrophysiol. 2008;19:48–55. doi: 10.1111/j.1540-8167.2007.00984.x. [DOI] [PubMed] [Google Scholar]
- 13.Sutton R, van Dijk N, Wieling W. Clinical history in management of suspected syncope: a powerful diagnostic tool. Cardiol J. 2014;21:651–657. doi: 10.5603/CJ.2014.0097. [DOI] [PubMed] [Google Scholar]
- 14.Sutton R, Brignole M. Twenty-eight years of research permit reinterpretation of tilt-testing: hypotensive susceptibility rather than diagnosis. Eur Heart J. 2014;35:2211–2212. doi: 10.1093/eurheartj/ehu255. [DOI] [PubMed] [Google Scholar]
- 15.Forleo C, Guida P, Iacoviello M, Resta M, Monitillo F, Sorrentino S, Favale S. Head-up tilt testing for diagnosing vasovagal syncope: a meta-analysis. Int J Cardiol. 2013;168:27–35. doi: 10.1016/j.ijcard.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 16.Cheshire WP, Jr, Goldstein DS. Autonomic uprising: the tilt table test in autonomic medicine. Clin Auton Res. 2019;29:215–230. doi: 10.1007/s10286-019-00598-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Humm AM, Z'Graggen WJ. Venepuncture during head-up tilt testing in patients with suspected vasovagal syncope—implications for the test protocol. Eur J Neurol. 2015;22:389–394. doi: 10.1111/ene.12590. [DOI] [PubMed] [Google Scholar]
- 18.Mereu R, Taraborrelli P, Sau A, Di Toro A, Halim S, Hayat S, Bernardi L, Francis DP, Sutton R, Lim PB. Diagnostic role of head-up tilt test in patients with cough syncope. Europace. 2016;18:1273–1279. doi: 10.1093/europace/euv283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finucane C, van Wijnen VK, Fan CW, Soraghan C, Byrne L, Westerhof BE, Freeman R, Fedorowski A, Harms MPM, Wieling W, Kenny R. A practical guide to active stand testing and analysis using continuous beat-to-beat non-invasive blood pressure monitoring. Clin Auton Res. 2019;29:427–441. doi: 10.1007/s10286-019-00606-y. [DOI] [PubMed] [Google Scholar]
- 20.Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (London, England: 1979) 2007;112:157–165. doi: 10.1042/CS20060091. [DOI] [PubMed] [Google Scholar]
- 21.Gibbons CH, Schmidt P, Biaggioni I, Frazier-Mills C, Freeman R, Isaacson S, Karabin B, Kuritzky L, Lew M, Low P, Mehdirad A, Raj SR, Vernino S, Kaufmann H. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264:1567–1582. doi: 10.1007/s00415-016-8375-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006;67:28–32. doi: 10.1212/01.wnl.0000223828.28215.0b. [DOI] [PubMed] [Google Scholar]
- 23.Gibbons CH, Freeman R. Clinical implications of delayed orthostatic hypotension: a 10-year follow-up study. Neurology. 2015;85:1362–1367. doi: 10.1212/WNL.0000000000002030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saedon NI, Tan MP, Frith J (2018) The prevalence of orthostatic hypotension: a systematic review and meta-analysis. J Gerontol (Series A, Biological sciences and medical sciences) [DOI] [PMC free article] [PubMed]
- 25.LaFrance WC, Jr, Baker GA, Duncan R, Goldstein LH, Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia. 2013;54:2005–2018. doi: 10.1111/epi.12356. [DOI] [PubMed] [Google Scholar]
- 26.van Dijk JG, Thijs RD, Benditt DG, Wieling W. A guide to disorders causing transient loss of consciousness: focus on syncope. Nat Rev Neurol. 2009;5:438–448. doi: 10.1038/nrneurol.2009.99. [DOI] [PubMed] [Google Scholar]
- 27.Norcliffe-Kaufmann L, Kaufmann H, Palma JA, Shibao CA, Biaggioni I, Peltier AC, Singer W, Low PA, Goldstein DS, Gibbons CH, Freeman R, Robertson D. Orthostatic heart rate changes in patients with autonomic failure caused by neurodegenerative synucleinopathies. Ann Neurol. 2018;83:522–531. doi: 10.1002/ana.25170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hilz MJ, Dutsch M. Quantitative studies of autonomic function. Muscle Nerve. 2006;33:6–20. doi: 10.1002/mus.20365. [DOI] [PubMed] [Google Scholar]
- 29.Goldstein DS, Cheshire WP., Jr Beat-to-beat blood pressure and heart rate responses to the Valsalva maneuver. Clin Auton Res. 2017;27:361–367. doi: 10.1007/s10286-017-0474-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martin A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A, van Dijk JG (2018) Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J
- 31.Low PA. Testing the autonomic nervous system. Semin Neurol. 2003;23:407–422. doi: 10.1055/s-2004-817725. [DOI] [PubMed] [Google Scholar]
- 32.Sheldon RS, Sheldon AG, Serletis A, Connolly SJ, Morillo CA, Klingenheben T, Krahn AD, Koshman ML, Ritchie D. Worsening of symptoms before presentation with vasovagal syncope. J Cardiovasc Electrophysiol. 2007;18:954–959. doi: 10.1111/j.1540-8167.2007.00892.x. [DOI] [PubMed] [Google Scholar]
- 33.van Dijk N, Quartieri F, Blanc JJ, Garcia-Civera R, Brignole M, Moya A, Wieling W. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial) J Am Coll Cardiol. 2006;48:1652–1657. doi: 10.1016/j.jacc.2006.06.059. [DOI] [PubMed] [Google Scholar]
- 34.Wieling W, van Dijk N, Thijs RD, de Lange FJ, Krediet CT, Halliwill JR. Physical countermeasures to increase orthostatic tolerance. J Intern Med. 2015;277:69–82. doi: 10.1111/joim.12249. [DOI] [PubMed] [Google Scholar]
- 35.In:
- 36.Saal DP, Thijs RD, van Zwet EW, Bootsma M, Brignole M, Benditt DG, van Dijk JG. Temporal relationship of asystole to onset of transient loss of consciousness in tilt-induced reflex syncope. JACC Clin Electrophysiol. 2017;3:1592–1598. doi: 10.1016/j.jacep.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Sheldon RS, Grubb BP, 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12:e41–63. doi: 10.1016/j.hrthm.2015.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shmuely S, Bauer PR, van Zwet EW, van Dijk JG, Thijs RD. Differentiating motor phenomena in tilt-induced syncope and convulsive seizures. Neurology. 2018;90:e1339–e1346. doi: 10.1212/WNL.0000000000005301. [DOI] [PubMed] [Google Scholar]
- 39.Tannemaat MR, van Niekerk J, Reijntjes RH, Thijs RD, Sutton R, van Dijk JG. The semiology of tilt-induced psychogenic pseudosyncope. Neurology. 2013;81:752–758. doi: 10.1212/WNL.0b013e3182a1aa88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blad H, Lamberts RJ, van Dijk GJ, Thijs RD. Tilt-induced vasovagal syncope and psychogenic pseudosyncope: overlapping clinical entities. Neurology. 2015;85:2006–2010. doi: 10.1212/WNL.0000000000002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Wijnen VK, Finucane C, Harms MPM, Nolan H, Freeman RL, Westerhof BE, Kenny RA, Ter Maaten JC, Wieling W. Noninvasive beat-to-beat finger arterial pressure monitoring during orthostasis: a comprehensive review of normal and abnormal responses at different ages. J Intern Med. 2017;282:468–483. doi: 10.1111/joim.12636. [DOI] [PubMed] [Google Scholar]
- 42.Pavy-Le Traon A, Piedvache A, Perez-Lloret S, Calandra-Buonaura G, Cochen-De Cock V, Colosimo C, Cortelli P, Debs R, Duerr S, Fanciulli A, Foubert-Samier A, Gerdelat A, Gurevich T, Krismer F, Poewe W, Tison F, Tranchant C, Wenning G, Rascol O, Meissner WG. New insights into orthostatic hypotension in multiple system atrophy: a European multicentre cohort study. J Neurol Neurosurg Psychiatry. 2016;87:554–561. doi: 10.1136/jnnp-2014-309999. [DOI] [PubMed] [Google Scholar]
- 43.Imholz BP, Wieling W, van Montfrans GA, Wesseling KH. Fifteen years experience with finger arterial pressure monitoring: assessment of the technology. Cardiovasc Res. 1998;38:605–616. doi: 10.1016/s0008-6363(98)00067-4. [DOI] [PubMed] [Google Scholar]
- 44.van Dijk JG, Ghariq M, Kerkhof FI, Reijntjes R, van Houwelingen MJ, van Rossum IA, Saal DP, van Zwet EW, van Lieshout JJ, Thijs RD, Benditt DG. Novel methods for quantification of vasodepression and cardioinhibition during tilt-induced vasovagal syncope. Circ Res. 2020;127:e126–e138. doi: 10.1161/CIRCRESAHA.120.316662. [DOI] [PubMed] [Google Scholar]
- 45.Taal W, van der Dussen DH, van Erven L, van Dijk JG. Neurally-mediated complete heart block. Lancet Neurol. 2003;2:255–256. doi: 10.1016/s1474-4422(03)00355-7. [DOI] [PubMed] [Google Scholar]
- 46.Brignole M, Deharo JC, De Roy L, Menozzi C, Blommaert D, Dabiri L, Ruf J, Guieu R. Syncope due to idiopathic paroxysmal atrioventricular block: long-term follow-up of a distinct form of atrioventricular block. J Am Coll Cardiol. 2011;58:167–173. doi: 10.1016/j.jacc.2010.12.045. [DOI] [PubMed] [Google Scholar]
- 47.Zysko D, Fedorowski A, Nilsson D, Rudnicki J, Gajek J, Melander O, Sutton R. Tilt testing results are influenced by tilt protocol. Europace. 2016;18:1108–1112. doi: 10.1093/europace/euv262. [DOI] [PubMed] [Google Scholar]
- 48.van Dijk JG, Thijs RD, van Zwet E, Tannemaat MR, van Niekerk J, Benditt DG, Wieling W. The semiology of tilt-induced reflex syncope in relation to electroencephalographic changes. Brain. 2014;137:576–585. doi: 10.1093/brain/awt332. [DOI] [PubMed] [Google Scholar]
- 49.Norcliffe-Kaufmann LJ, Kaufmann H, Hainsworth R. Enhanced vascular responses to hypocapnia in neurally mediated syncope. Ann Neurol. 2008;63:288–294. doi: 10.1002/ana.21205. [DOI] [PubMed] [Google Scholar]
- 50.Stewart JM, Pianosi P, Shaban MA, Terilli C, Svistunova M, Visintainer P, Medow MS (2018) Postural hyperventilation as a cause of postural tachycardia syndrome: increased systemic vascular resistance and decreased cardiac output when upright in all postural tachycardia syndrome variants. J Am Heart Assoc 7 [DOI] [PMC free article] [PubMed]
- 51.Naschitz JE, Rosner I, Rozenbaum M, Gaitini L, Bistritzki I, Zuckerman E, Sabo E, Yeshurun D. The capnography head-up tilt test for evaluation of chronic fatigue syndrome. Semin Arthritis Rheum. 2000;30:79–86. doi: 10.1053/sarh.2000.9201. [DOI] [PubMed] [Google Scholar]
- 52.Goldstein DS, Cheshire WP. Roles of catechol neurochemistry in autonomic function testing. Clin Auton Res. 2018;28:273–288. doi: 10.1007/s10286-018-0528-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goldstein DS, Holmes C, Sharabi Y, Brentzel S, Eisenhofer G. Plasma levels of catechols and metanephrines in neurogenic orthostatic hypotension. Neurology. 2003;60:1327–1332. doi: 10.1212/01.wnl.0000058766.46428.f3. [DOI] [PubMed] [Google Scholar]
- 54.Benditt DG, Detloff BL, Adkisson WO, Lu F, Sakaguchi S, Schussler S, Austin E, Chen LY. Age-dependence of relative change in circulating epinephrine and norepinephrine concentrations during tilt-induced vasovagal syncope. Heart Rhythm. 2012;9:1847–1852. doi: 10.1016/j.hrthm.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 55.Raj SR. Postural tachycardia syndrome (POTS) Circulation. 2013;127:2336–2342. doi: 10.1161/CIRCULATIONAHA.112.144501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Singer W, Berini SE, Sandroni P, Fealey RD, Coon EA, Suarez MD, Benarroch EE, Low PA. Pure autonomic failure: predictors of conversion to clinical CNS involvement. Neurology. 2017;88:1129–1136. doi: 10.1212/WNL.0000000000003737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Norcliffe-Kaufmann L, Galindo-Mendez B, Garcia-Guarniz AL, Villarreal-Vitorica E, Novak V. Transcranial Doppler in autonomic testing: standards and clinical applications. Clin Auton Res. 2018;28:187–202. doi: 10.1007/s10286-017-0454-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Raj V, Rowe AA, Fleisch SB, Paranjape SY, Arain AM, Nicolson SE. Psychogenic pseudosyncope: diagnosis and management. Auton Neurosci. 2014;184:66–72. doi: 10.1016/j.autneu.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 59.Bachus E, Holm H, Hamrefors V, Melander O, Sutton R, Magnusson M, Fedorowski A. Monitoring of cerebral oximetry during head-up tilt test in adults with history of syncope and orthostatic intolerance. Europace. 2018;20:1535–1542. doi: 10.1093/europace/eux298. [DOI] [PubMed] [Google Scholar]
- 60.Kharraziha I, Holm H, Bachus E, Ricci F, Sutton R, Fedorowski A, Hamrefors V. Cerebral oximetry in syncope and syndromes of orthostatic intolerance. Front Cardiovascular Med. 2019;6:171. doi: 10.3389/fcvm.2019.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sutton R. The value of tilt testing and autonomic nervous system assessment. Cardiol Clin. 2015;33:357–360. doi: 10.1016/j.ccl.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 62.Bartoletti A, Gaggioli G, Menozzi C, Bottoni N, Del Rosso A, Mureddu R, Musso G, Foglia-Manzillo G, Bonfigli B, Brignole M. Head-up tilt testing potentiated with oral nitroglycerin: a randomized trial of the contribution of a drug-free phase and a nitroglycerin phase in the diagnosis of neurally mediated syncope. Europace. 1999;1:183–186. doi: 10.1053/eupc.1999.0036. [DOI] [PubMed] [Google Scholar]
- 63.El-Bedawi KM, Hainsworth R. Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res. 1994;4:41–47. doi: 10.1007/BF01828837. [DOI] [PubMed] [Google Scholar]
- 64.Goswami N, Blaber AP, Hinghofer-Szalkay H, Convertino VA. Lower body negative pressure: physiological effects, applications, and implementation. Physiol Rev. 2019;99:807–851. doi: 10.1152/physrev.00006.2018. [DOI] [PubMed] [Google Scholar]
- 65.Fanciulli A, Jordan J, Biaggioni I, Calandra-Buonaura G, Cheshire WP, Cortelli P, Eschlboeck S, Grassi G, Hilz MJ, Kaufmann H, Lahrmann H, Mancia G, Mayer G, Norcliffe-Kaufmann L, Pavy-Le Traon A, Raj SR, Robertson D, Rocha I, Struhal W, Thijs R, Tsioufis KP, van Dijk JG, Wenning GK. Consensus statement on the definition of neurogenic supine hypertension in cardiovascular autonomic failure by the American Autonomic Society (AAS) and the European Federation of Autonomic Societies (EFAS): Endorsed by the European Academy of Neurology (EAN) and the European Society of Hypertension (ESH) Clin Auton Res. 2018;28:355–362. doi: 10.1007/s10286-018-0529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Palma JA, Gomez-Esteban JC, Norcliffe-Kaufmann L, Martinez J, Tijero B, Berganzo K, Kaufmann H. Orthostatic hypotension in Parkinson disease: how much you fall or how low you go? Movement Disord. 2015;30:639–645. doi: 10.1002/mds.26079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Freeman R IB, Lapusca R, Campagnolo M, Abuzinadah AR, Bonyhay I, Sinn DI, Miglis M, White J, Gibbons CH (2020) Symptom recognition is impaired in patients with orthostatic hypotension. Hypertension (Dallas, Tex.: 1979):in press [DOI] [PubMed]
- 68.Whitehead K, Kane N, Wardrope A, Kandler R, Reuber M. Proposal for best practice in the use of video-EEG when psychogenic non-epileptic seizures are a possible diagnosis. Clin Neurophysiol Pract. 2017;2:130–139. doi: 10.1016/j.cnp.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pasquier M, Clair M, Pruvot E, Hugli O, Carron PN. Carotid sinus massage. New Engl J Med. 2017;377:e21. doi: 10.1056/NEJMvcm1313338. [DOI] [PubMed] [Google Scholar]
- 70.Pavelic A, Krbot Skoric M, Crnosija L, Habek M. Postprandial hypotension in neurological disorders: systematic review and meta-analysis. Clin Auton Res. 2017;27:263–271. doi: 10.1007/s10286-017-0440-8. [DOI] [PubMed] [Google Scholar]
- 71.Thijs RD, Reijntjes RH, van Dijk JG. Water drinking as a potential treatment for idiopathic exercise-related syncope: a case report. Clin Auton Res. 2003;13:103–105. doi: 10.1007/s10286-003-0083-9. [DOI] [PubMed] [Google Scholar]
- 72.Kim TH, Jang HJ, Kim S, Cho SY, Song KS, Pickett C, Schmitt HJ, Lee J. A new test for diagnosing vasovagal syncope: Standing after treadmill test with sublingual nitrate administration. PLoS ONE. 2017;12:e0179631. doi: 10.1371/journal.pone.0179631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fagius J, Karhuvaara S. Sympathetic activity and blood pressure increases with bladder distension in humans. Hypertension (Dallas, Tex.: 1979) 1989;14:511–517. doi: 10.1161/01.hyp.14.5.511. [DOI] [PubMed] [Google Scholar]
- 74.Hu K, Scheer FA, Laker M, Smales C, Shea SA. Endogenous circadian rhythm in vasovagal response to head-up tilt. Circulation. 2011;123:961–970. doi: 10.1161/CIRCULATIONAHA.110.943019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baron-Esquivias G, Pedrote A, Cayuela A, Valle JI, Fernandez JM, Arana E, Fernandez M, Morales F, Burgos J, Martinez-Rubio A. Long-term outcome of patients with asystole induced by head-up tilt test. Eur Heart J. 2002;23:483–489. doi: 10.1053/euhj.2001.2900. [DOI] [PubMed] [Google Scholar]
- 76.Gieroba ZJ, Newton JL, Parry SW, Norton M, Lawson J, Kenny RA. Unprovoked and glyceryl trinitrate-provoked head-up tilt table test is safe in older people: a review of 10 years’ experience. J Am Geriatr Soc. 2004;52:1913–1915. doi: 10.1111/j.1532-5415.2004.52518.x. [DOI] [PubMed] [Google Scholar]
- 77.Kruit MC, Thijs RD, Ferrari MD, Launer LJ, van Buchem MA, van Dijk JG. Syncope and orthostatic intolerance increase risk of brain lesions in migraineurs and controls. Neurology. 2013;80:1958–1965. doi: 10.1212/WNL.0b013e318293e1c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bastulli JA, Orlowski JP. Stroke as a complication of carotid sinus massage. Crit Care Med. 1985;13:869. doi: 10.1097/00003246-198510000-00022. [DOI] [PubMed] [Google Scholar]
- 79.Munro NC, McIntosh S, Lawson J, Morley CA, Sutton R, Kenny RA. Incidence of complications after carotid sinus massage in older patients with syncope. J Am Geriatr Soc. 1994;42:1248–1251. doi: 10.1111/j.1532-5415.1994.tb06505.x. [DOI] [PubMed] [Google Scholar]
- 80.Richardson DA, Bexton R, Shaw FE, Steen N, Bond J, Kenny RA. Complications of carotid sinus massage–a prospective series of older patients. Age Ageing. 2000;29:413–417. doi: 10.1093/ageing/29.5.413. [DOI] [PubMed] [Google Scholar]
- 81.Puggioni E, Guiducci V, Brignole M, Menozzi C, Oddone D, Donateo P, Croci F, Solano A, Lolli G, Tomasi C, Bottoni N. Results and complications of the carotid sinus massage performed according to the “method of symptoms”. Am J Cardiol. 2002;89:599–601. doi: 10.1016/s0002-9149(01)02303-7. [DOI] [PubMed] [Google Scholar]
- 82.Curro Dossi R, Roscia G, Turri E, Dall'ora E, Sansone S, Stockner I, Wiedermann CJ. Acute ischemic stroke complicating carotid sinus massage in the absence of carotid artery disease and failure of thrombolytic therapy. Minerva Med. 2010;101:193. [PubMed] [Google Scholar]
- 83.Ungar A, Rivasi G, Rafanelli M, Toffanello G, Mussi C, Ceccofiglio A, McDonagh R, Drumm B, Marchionni N, Alboni P, Kenny RA. Safety and tolerability of Tilt Testing and Carotid Sinus Massage in the octogenarians. Age Ageing. 2016;45:242–248. doi: 10.1093/ageing/afw004. [DOI] [PubMed] [Google Scholar]
- 84.van Munster CE, van Ballegoij WJ, Schroeder-Tanka JM, van den Berg-Vos RM. A severe stroke following carotid sinus massage. Ned Tijdschr Geneeskd. 2017;161:D826. [PubMed] [Google Scholar]
- 85.Kenny RA, Brignole M, Dan GA, Deharo JC, van Dijk JG, Doherty C, Hamdan M, Moya A, Parry SW, Sutton R, Ungar A, Wieling W. Syncope Unit: rationale and requirement–the European Heart Rhythm Association position statement endorsed by the Heart Rhythm Society. Europace. 2015;17:1325–1340. doi: 10.1093/europace/euv115. [DOI] [PubMed] [Google Scholar]
- 86.Fedorowski A, Hamrefors V, Sutton R, van Dijk JG, Freeman R, Lenders JW, Wieling W. Do we need to evaluate diastolic blood pressure in patients with suspected orthostatic hypotension? Clin Auton Res. 2017;27:167–173. doi: 10.1007/s10286-017-0409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]