Abstract
Mile Square Health Center (MSHC), a network of Federally Qualified Health Centers (FQHCs) run by the University of Illinois Hospital (UIH) in Chicago, established Drive-Thru and Walk-Up COVID-19 testing sites. The primary aim of the UIH/MSHC testing project was to increase testing capacity in the most affected, racial/ethnic minority communities. More than 7,500 tests were performed over a six-month period. Half of those who were tested were Black and Latinx residents. The majority of those tested at the Walk-Up sites were Black, while “Other” race group tended to get tested in Drive Thru testing sites. Latinx residents had the highest positivity rate, followed by Other race group. Younger age groups were more likely to have higher positivity rates. Overall, UH/MSHC testing results reflected the overall Chicago COVID-19 testing results. Our findings substantiate the need to advocate for equitable resource allocation to counter the disproportionate burden of COVID-19 infection among minority communities. FQHCs were shown to be an effective approach to reduce structural barriers to COVID-19 testing and subsequently reduce disparities. Going forward, FQHCs can be key to ensuring COVID-19 vaccine outreach and dissemination.
Keywords: Federally Qualified Health Centers, COVID-19, Testing, Health Equity
1. Introduction
Since the beginning of the COVID-19 pandemic, testing has been one of the most important tools to mitigate infection transmission.1 As of August 15, 2020, the United States (US) had the most COVID-19 cases in the world, with more than 5 million confirmed cases and 160,000 deaths.2, 3 In Illinois, there were over 166,000 confirmed cases and 7,367 deaths4 by mid-August. Particularly, Chicago was one of the first metropolitan cities to have reported COVID-19 and continues to have a high rate of confirmed cases and deaths in Illinois, representing over 45% of Illinois cases and deaths.4
Reliable testing and rapid turnaround for results are critical to quickly identify and isolate infected individuals, effectively interrupting potential transmission.1 Although testing has become a hotly contested issue in the political arena and the general public, public health consensus is that adequate testing capacity is crucial to curb the pandemic.1, 5 Despite issues in the early days of the pandemic, daily testing numbers have increased dramatically.3 Currently in Illinois over 3 million tests are performed daily, averaging 2.9 million tests per day since early August.4
As the country prepares for reopening, there is an increased need for sufficient access to testing. In particular, access to testing in minority communities has been shown to be less than optimal.6, 7 As a result, strategies to address racial/ethnic disparities in COVID-19 require including expanding testing in minority communities, which are most affected by the pandemic.
1.1. COVID-19 Testing and Racial/Ethnic minorities
Within the United States, there has been no federal level testing standardization available, which has made it difficult for local governments to establish effective testing protocols.6 In countries such as South Korea and Taiwan, efficient and organized testing programs using networks of drive-through testing facilities combined with contact tracing efforts have shown to be remarkably effective in containing COVID-19 transmission.8 For example, in mid-March, 2020, South Korea had a testing rate of 5,200 per million individuals, while the testing rate in the U.S. was at 74 per million individuals.8 Such effective early testing response made swift case identification, isolation, and contact tracing possible, resulting in successful national level mitigation, while the testing shortages in the US had led to an explosion of cases.9
Additionally, the distribution of testing kits and testing sites are managed by state and local agencies, which could contribute to suboptimal allocations of resources and testing sites.1 While the availability of COVID-19 testing has continued to improve, testing sites are still relatively inaccessible for minority communities in many parts of the US cities.7, 10 It has been well documented that the COVID-19 infection and death rates are higher for racial/ethnic minority communities.11 Reports showed that 70% of the first 100 people who died due to COVID-19 in Chicago were African American.12
Currently, over 3 million tests are performed daily in Illinois4 but detailed demographic data on those who took the test and those who tested positive at the individual level are unavailable. Aggregate data available from the Chicago Department of Public Health (CDPH) show that racial/ethnic distributions of COVID-19 infection and deaths in Chicago have changed over time. During the early pandemic period, African Americans represented over 50% of COVID-19 cases, followed by Whites and Latinx. However, the trend began to shift; Latinx cases exceeded White cases by mid-April and continued to increase.13 Now, Latinx account for 48% and African Americans account for 30% of Chicago’s confirmed cases. And yet, residents living in poorer or immigrant communities are less likely to be tested, in part due to the lack of testing sites within their communities.11
Furthermore, the risk of COVID-19 related deaths is significantly higher for minority groups.13 While there is no evidence showing that certain race/ethnicity groups have a greater biological mortality risk of COVID-19, existing structural inequality increases these communities’ vulnerabilities to COVID-19.14 A higher prevalence of underlying medical conditions, including obesity, hypertension, and heart disease,10 among minorities with economic disadvantage exacerbates the risk of resulting in poor COVID-19 outcomes.15
1.2. Factors for Exposure to COVID-19
Social distancing orders, such as maintaining six feet distance and avoiding crowded places, have shown to be an effective public health mitigation policy.16 In Illinois, shelter in place executive orders were issued on March 20th, which effectively brought the infection down. The number of weekly new cases has steadily decreased since the first week of May from over 17,000 new cases per week to just over 4,000 cases per week by the third week of June.13
And yet, not everyone can benefit from these public health interventions. Individuals living in crowded housing may have difficulty safely staying at home or social distancing with family members who may have exposed to COVID-19.17 Indeed, Latinx and Black households are more likely to live in crowded housing conditions compared to Whites.18
In addition, “essential workers” are required to continue working during the pandemic. Although the Centers for Disease Control and Prevention (CDC) released guidelines for essential work settings in April, the CDC recommendations19 were not mandated by the federal government. Essential work includes primarily low-wage service jobs with the majority of essential workers being racial/ethnic minorities.20 This contributes to increased exposure to COVID-19 among these communities.
Furthermore, for the Latinx community, in particular, immigration status is another major factor in choosing to get tested. Undocumented immigrants may avoid seeking care or testing for fear of deportation.10 Even documented immigrants may also refuse to seek care, even with apparent symptoms, because of concerns around the public charge rule affecting their citizenship application.21 Federally Qualified Health Centers (FQHCs) provide primary care services to underserved populations, without requiring immigration status.10 However, even with FQHCs, immigration status affects how people access and utilize COVID-19 testing and necessary healthcare.22
The aim of this study is to describe how a university-based FQHC system addressed disparities in testing in Chicago that contributed to reducing racial/ethnic inequality in access to COVID-19 testing. In this paper, we discuss how outpatient testing facilities throughout the University of Illinois Hospital (UIH) and its associated FQHC, Mile Square Health Center (MSHC) which is UIH supported, contributed to a substantial increase in COVID-19 testing in the most affected Chicago Community Areas (CCAs). We further consider the significant role of FQHCs in providing primary care including testing and vaccination to underserved populations, which has become clear during the COVID-19 pandemic.
2. Methods
The MSHC has provided quality health care services to underserved residents of the Chicagoland area for over 50 years.23 MSHC is made up of 14 practice sites, including six community clinics and seven school-based clinics in Chicagoland, and a community clinic in Rockford. Since the beginning of the pandemic, MSHC has implemented COVID-19 guidelines from the CDC and the Chicago Department of Public Health (CDPH) to test, treat and prevent transmission of COVID-19. Since March 28th, the City of Chicago reported a daily number of confirmed COVID-19 cases and deaths in the city.24 Very quickly, the MSHC team recognized that the high-risk community areas on the West and South sides of Chicago, which are predominantly minority and economically disadvantaged neighborhoods, were disproportionately affected by COVID infection.25 Such racial disparities in the confirmed COVID-19 cases, as well as deaths, have been observed nationally.26 Locally, COVID-19 has disproportionately affected highly segregated minority community areas on the West and South Side of Chicago.27 In response to address disparities in COVID-19 infection and deaths, MSHC prioritized its effort in the city’s “high risk” communities, where nearly all MSHC clinics are located.
One of the MSHC COVID-19 response efforts was establishing testing capacity in these most affected community areas. UIH and MSHC began to set up an outpatient testing response, inclusive of Drive Through as well as Walk-Up testing capability in March of 2020, being one of the first COVID-19 testing locations in Chicago. The primary aim of MSHC testing sites was to establish testing capacity in the most affected, predominantly African American and Latinx communities in the city. The UIH/MSHC testing sites were available to anyone wanting to get tested regardless of insurance status or ability to pay.
The MSHC testing sites have collaborated with other FQHCs to coordinate the City’s testing access efforts. Equally importantly, the UIH/MSHC multidisciplinary team, including UIH physicians, emergency medicine, ambulatory care, primary care, and public health individuals, helped establish COVID-19 testing sites throughout the city. UIH/MSHC’s rapid response to COVID-19 received funding supports from multiple sources, including Coronavirus Aid, Relief, and Economic Security (CARES) ACT.
On March 27, the first testing site was launched in the parking lot of the MSHC Main clinic, located on Chicago’s West Side and vicinity of UIH. Over the first three days of opening the MSHC Main testing site, we implemented the Plan-Do-Study-Act (PDSA) model to guide our efforts to quickly plan and implement, evaluate work done, and modify real-time. Following the PDSA model, rapid modifications were made to the original strategies based on the initial experiences of implementing the testing launch. Two drive-thru sites, in the Near West side and South West side, opened by April 2020. In addition, six walk-up testing sites were incorporated to mitigate limitations for testing due to transportation access. After the launch of a testing site on the west side, MSHC collaborated with community stakeholders on the south side, where another COVID-19 infection has been clustered. MSHC engaged local politicians and small businesses in South Shore, which had one of the highest COVID-19 death rates. Utilizing the PDSA approach, MSHC subsequently launched another testing site for the Near West side and the southwest side, with predominantly Latinx communities.
3. Results
Between March 24 and August 31, 2020, a total of 7,523 tests were performed at the UIH/MSHC testing sites, including 5,289 tests at the Drive-Thru sites and 2,234 tests at the MSHC Walk-Up sites (Table 1). Figure 1 shows the UIH/MSHC testing sites throughout the city of Chicago. Walk-Up sites showed a slightly higher positive rate, an overall 19.3% of tests being COVID positive, compared with an 18.1% positive rate for the Drive-Thru site. There was large variability in the positivity rates among Walk-Up testing sites, however. Cicero site which is located in predominantly Hispanic communities had the highest positivity rate, followed by the Urgent Care site located by the UI hospital campus. The Englewood site located in predominantly Black communities on the south side of the city had a 15.5% positivity rate.
Table 1.
The number of tests performed and % positive by testing site
| Testing site | Number of tests | % positive |
|---|---|---|
| Drive Thru | 5,289 | 18.1 |
| Walk Up | 2,234 | 19.3 |
| Back of the Yards | 17 | 11.8 |
| Cicero | 49 | 26.5 |
| Englewood | 84 | 15.5 |
| Main | 100 | 7.0 |
| South Shore | 1,046 | 17.8 |
| Urgent Care | 938 | 22.4 |
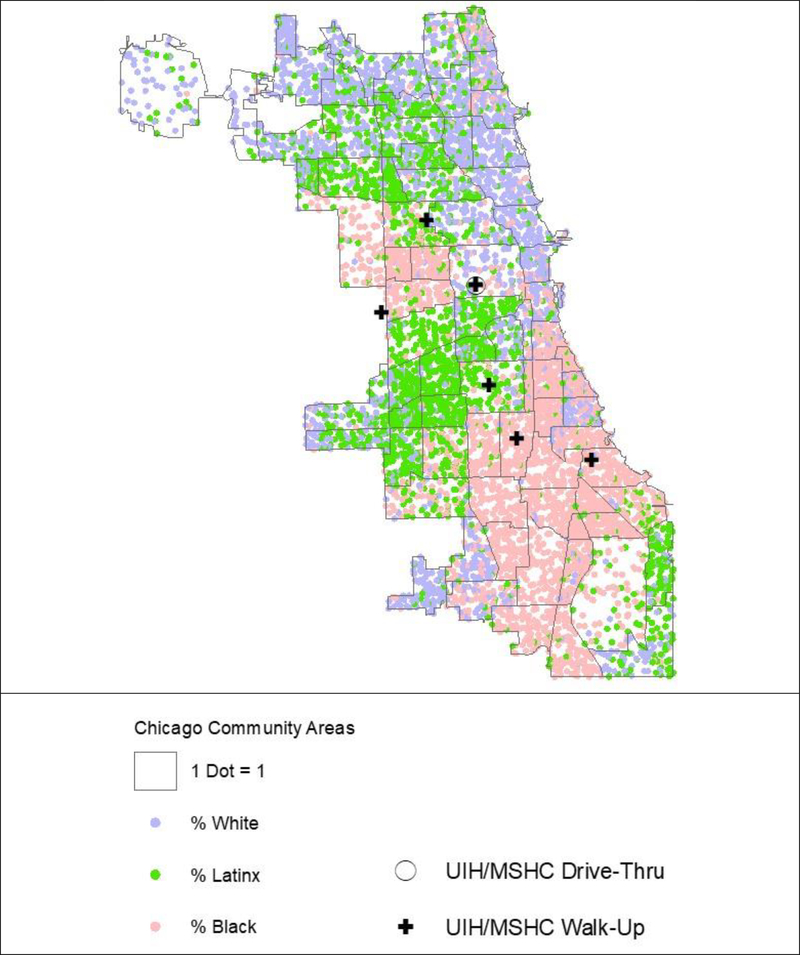
Figure 1.
Location of MSHC testing sites and the racial/ethnic distribution by Chicago Community Areas
Figure 2 depicts the spatial distribution of the number of tests conducted and % positivity. Overall, the Drive-Thru and Walk-Up testing sites covered primarily the West and South sides of the city which are known racial/ethnic minority communities. The racial/ethnic distribution of Chicago is shown in Figure 1.
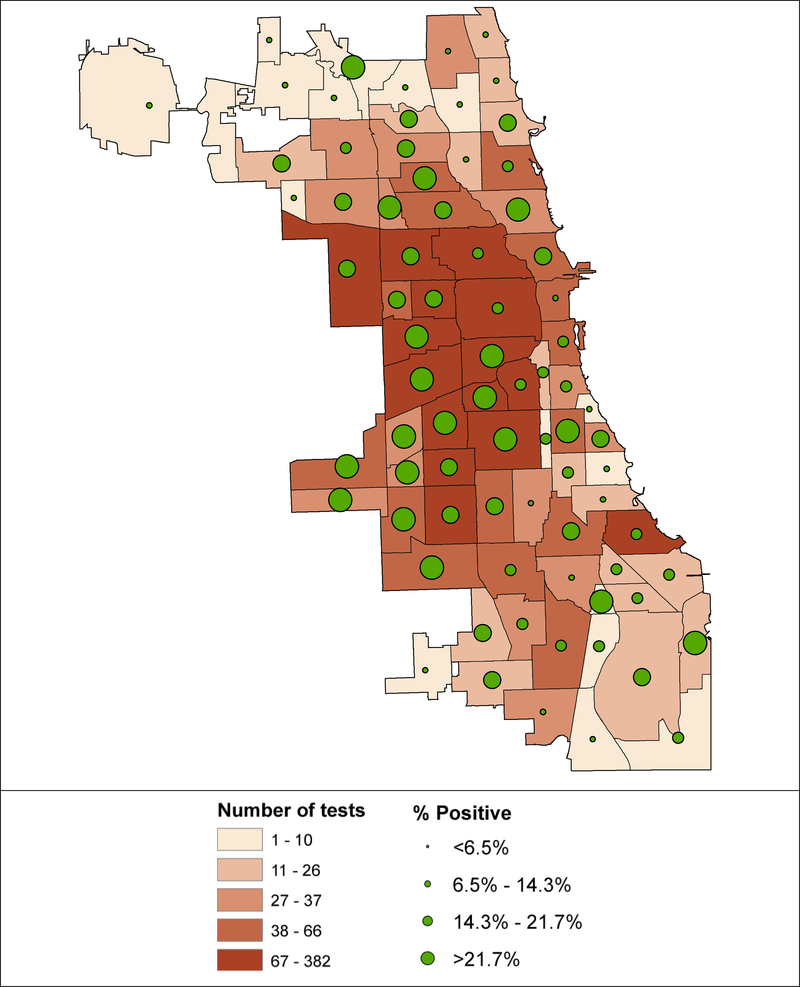
Figure 2.
Number of tests and % positivity by Chicago Community Areas
Table 2 summarizes test positive rates by race/ethnicity. Hispanics had the highest positivity rate, 33.5% for the Drive-Thru and 36.0% for the Walk-Up sites.
Table 2.
Number of tests and the test positive rate by race/ethnicity by testing site
| Drive-Thru | Walk-Up | Total | ||||
|---|---|---|---|---|---|---|
| Number of tests | % positive | Number of tests | % positive | Number of tests | % positive | |
| Black | 2,067 | 14.0 | 1,419 | 17.6 | 3,486 | 15.5 |
| Hispanic | 442 | 33.5 | 125 | 36.0 | 567 | 34.0 |
| Other | 1,582 | 24.4 | 394 | 20.3 | 1,980 | 23.5 |
| White | 998 | 8.9 | 208 | 12.0 | 1,206 | 9.5 |
| Unknown | 200 | 21.4 | 84 | 25.0 | 285 | 22.5 |
| Total | 5,289 | 18.1 | 2,234 | 18.8 | 7,524 | 18.3 |
Whites had the lowest positive rate, 8.9% for Drive-Thru and 9.5% for the Walk-Up sites. Interestingly, the “Other” race group including Asians, American Indians, and Pacific Islanders, showed 24% for both types of testing sites, which was higher than Black and White race groups. In addition, those who did not provide information about their race/ethnicity or missing also had a higher positivity rate than Black and White groups. Overall, the pattern of racial/ethnic differences does not appear to change significantly by type of testing site. However, the “Other” racial/ethnic group tended to get tested in Drive-Thru testing sites, while the majority of those tested at the Walk-Up sites were Black.
Concerning the test positivity rate by age group (Table 3), those who were 20 years and younger had the highest % positive tests (28.7%) for the Drive-Thru site, while the 30–49 age group had the highest % positivity (23.0%) for Walk-Up sites. Interestingly, the test positivity rate gradually decreased with age. The decreasing trend of positivity rate by age was consistent with the overall Chicago trend which showed higher positivity rates for younger age groups.28
Table 3.
The test positive rate by age group by testing site
| Drive-Thru | Walk-Up | Total | ||||
|---|---|---|---|---|---|---|
| Number of tests | % positive | Number of tests | % positive | Number of tests | % positive | |
| <20 | 94 | 28.7 | 207 | 21.3 | 301 | 23.6 |
| 20–29 | 1054 | 25.1 | 494 | 21.1 | 1548 | 23.8 |
| 30–49 | 1997 | 18.1 | 868 | 23.0 | 2865 | 19.6 |
| 50–64 | 1466 | 16.0 | 512 | 17.0 | 1978 | 16.2 |
| >65 | 678 | 10.0 | 127 | 7.9 | 805 | 9.7 |
| Total | 5289 | 18.1 | 2208 | 20.2 | 7497 | 18.7 |
Table 4 compares the overall Chicago testing results by age and race/ethnicity and UIH testing sites. Overall, UIH testing sites showed higher positivity rates for all three age groups compared to the city average. In particular, the positivity rate for those who were 29 and younger was nearly double for the UIH test participants compared with the rate for the city overall. In terms of the test positivity rate by race/ethnicity, UIH test results showed a slightly lower % positivity for Black test participants (16%) than the city average (17%), while the positivity rate for Hispanics (34%) for UIH testing sites was higher than the rate for the city average (32%). A significantly higher positivity rate for the “Other” race group was shown in the UIH test sites (24%) compared with the city average (13%).
Table 4.
Comparison of the number of tests and the test positive rate between Chicago and UIH testing sites
| Chicago** | UIH | |||
|---|---|---|---|---|
| N of tested | % Positive | N of tested | % Positive | |
| Total | 531,131 | 13.2 | 7,497 | 18.7 |
| Age | ||||
| <29 | 164,385 | 12.0 | 1,849 | 23.8 |
| 30–49 | 181,773 | 13.7 | 2,865 | 19.6 |
| >50 | 184,973 | 13.8 | 2,783 | 14.3 |
| Race/Ethnicity | ||||
| Black | 94,970 | 16.9 | 3,486 | 15.5 |
| Hispanic | 88,754 | 31.6 | 567 | 34.0 |
| Other* | 32,299 | 13.4 | 1,980 | 23.5 |
| White | 99,755 | 9.8 | 1,206 | 9.5 |
| Unknown | 216,362 | 5.8 | 285 | 22.5 |
Includes Asian and Other
Chicago data retrieved from Chicago Data Portal. Chicago tests and cases from March 24-August 31, 2020 were included.
COVID-19 Daily Rolling Average Chicago Case Rates by Age: https://data.cityofchicago.org/Health-Human-Services/COVID-19-Daily-Rolling-Average-Chicago-Case-Rates-/f2e5-djzs; COVID-19 Daily Rolling Average Chicago Case Rates by Race/Ethnicity: https://data.cityofchicago.org/Health-Human-Services/COVID-19-Daily-Rolling-Average-Chicago-Case-Rates-/nfdw-3y3r.
4. Discussion
The MSHC testing sites were able to test more than 7,500 residents, the majority of whom were racial/ethnic minorities living in highly disadvantaged communities in Chicago over a six-month period at the height of the pandemic. Testing has been a key measure to control the spread of COVID-19 since the beginning of the pandemic,1 while multiple barriers to the equitable distribution of and access to testing contribute to racial/ethnic disparities in COVID-19 outcomes.26 The city of Chicago made concerted efforts to address the disproportionate burden of COVID-19 among minority communities.29, 30 And yet, there have been difficulties in implementing mitigation measures and testing for the pandemic, in part, due to existing inequality in pubic health infrastructure.31 The MSHC strategies to increase testing capacity in predominantly minority communities are innovative in that in addition to usual drive-thru testing facilities, we set up walk-up sites to remove barriers for those who do not have private vehicles. The walk-up sites were based in our FQHCs in highly segregated racial/ethnic minority communities. As a result, 63.5% of those tested at the walk-up sites were Black, compared with 43.9% of individuals tested by the city. Black residents who had shown the highest death rates for COVID-19. Predominantly Black communities located on the West and South sides of Chicago have long been suffering poor access to care and, consequently, poor health outcomes.14 This finding indicates that targeting most vulnerable communities utilizing exiting primary care clinics, such as FQHCs, is an effective way to expand nessasary testing capacity.
Perhaps opening up testing sites in disadvantaged communities in and of itself may not be enough to increase testing participation, given the high level of medical mistrust in minority communities. Racial/ethnic minorities have a long history of being subjected to bias and discrimination in healthcare.32 Medical mistrust among minorities due to historical medical abuse has affected how people engage and utilize healthcare, which contributed to poor health outcomes among racial/ethnic minority communities.33 MSHC has long been an important source of community-based primary care for the city’s underserved areas. MSHC’s COVID-19 testing sites were established strategically in predominantly minority communities in order to tackle structural barriers to equitable access to testing. The MSHC team considered medical mistrust, immigration status, and perceived risk in testing. And based on the existing relationship, MSHC was able to contribute to overcoming barriers to COVID-19 testing in most affected communities in Chicago.
We found that the positivity rate was significantly higher for Black and Hispanic communities. This finding was consistent with the national-level findings.34 However, the level of positivity was substantially higher in Chicago. Furthermore, the positivity rate among Blacks from our walk-up and drive-thru sites was 15.5%, which was lower than the Chicago average (16.9%). One of the reasons might be that our testing sites were able to reach more people including lower-risk individuals in Black communities, rather than focusing on high-risk individuals. However, the positivity rate for Hispanic communities was higher for our testing sites (34.0%) compared with the city average (31.6%). Additionally, the “Other” race group showed a relatively high positivity rate, 23.5%, which was, in fact, higher than the rate for Blacks. Despite the high risk of COVID-19 infection, the “Other” group was not well examined, in part due to the way scholars and government administrators classify race/ethnicity. At the point of this study, we were not able to parse out who were included in this category. Often studies compared three major race/ethnic groups, Black, Hispanic, and White; but this finding suggests that the race/ethnicity category needs to be further refined.
Our finding showed that the positivity rate for those 29 years of age and younger from our testing sites (23.8%) was nearly twice as high as the positivity rate for the city average (12.0%). This finding may reflect that many minority workers are exposed to the virus because they are disproportionately more likely to be low-wage frontline workers.35 While these frontline workers were touted as “essential”, the reality is that they are continued to be paid low-wage while risking their health and well-being due to the unsafe work environment, and the public-facing work type would not allow for work at home arrangements.
5. Conclusion
FQHCs have been an important component of the U.S. health systems designed to address structural health inequities, and this is particularly true of COVID-19 testing due to the health centers’ ability to reach populations at higher risk for COVID-19. During the first weeks of the pandemic, there were few COVID-19 testing sites and many communities with a high burden of COVID-19 also experienced limited access to testing. Our testing project based on the MSHC network highlighted the crucial role of FQHCs in providing care for underserved communities.36 MSHC comprehensive response to COVID-19 contributed to filling service gaps amid the pandemic. Our results support the current literature that demonstrates the disproportionate effects of COVID-19 in Black and Latinx communities and indicates the key role of FQHCs in reducing inequality in COVID-19 testing. FQHCs across the US, including MSHC, help improve the lives of community members through cost-effective preventive care on a sliding scale. Regardless of the patient’s ability to pay for the care, MSHC provides primary care services for more than 40,000 disenfranchised Chicagoans every year. The types of care administered at the MSHC clinics range from immunization, health education, and screenings, such as COVID-19 testing.
Our findings substantiate the need to advocate for equitable resource allocation to counter the disproportionate burden of COVID-19 infection among minority communities. Accessible COVID-19 testing sites through FQHCs were shown to be an effective approach to reduce structural barriers to testing and subsequently reduce disparities. Going forward, community health centers and FQHCs have in eliminating racial inequities related to COVID 19 is on increasing access, awareness, and uptake of the COVID 19 vaccines. The ability of the MSHC team to utilize evidence-based indicators of need was essential for the successful response to testing needs, contributing to curbing the spread of disease. In the similar way that FQHCs have played an integral role in ensuring access to testing in some of the most under-served racial/ethnic minority communities, FQHCs can be key to COVID-19 vaccine outreach, messaging, and dissemination.
Acknowledgments
Drs. Kim and Watson are supported, in part, by the National Institutes on Minority Health and Health Disparities (U54MD012523).
Footnotes
CONFLICTS OF INTEREST AND SOURCE OF FUNDING:
The authors declare that there is no conflict of interest.
Contributor Information
Sage J. Kim, University of Illinois at Chicago, School of Public Health, Division of Health Policy & Administration.
Karriem Watson, Associate Executive Director, Mile Square Health Center, Research Assistant Professor, University of Illinois at Chicago, School of Public Health, Division of Community Health Science.
Nidhi Khare, University of Illinois at Chicago, School of Public Health.
Shreyas Shastri, University of Illinois at Chicago, School of Public Health.
Carla L. Da Goia Pinto, University of Illinois Cancer Center.
Noreen T. Nazir, University of Illinois at Chicago, College of Medicine.
References
- 1.Njuguna H, Wallace M, Simonson S, et al. Serial Laboratory Testing for SARS-CoV-2 Infection Among Incarcerated and Detained Persons in a Correctional and Detention Facility — Louisiana, April—May 2020. Morbidity and Mortality Weekly Report (MMWR). 2020;69(26):836–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The COVID Tracking Project. COVID Data Tracker. The Covid Tracking Project. https://covidtracking.com/ [Google Scholar]
- 3.Johns Hopkins Univeristy & Medicine Coronavirus Resource Center. DAILY STATE-BY-STATE TESTING TRENDS. Johns Hopkins. https://coronavirus.jhu.edu/testing/individual-states/illinois [Google Scholar]
- 4.Illinois Department of Public Health (IDPH). COVID-19 Statistics. Illinois Department of Public Health. 2020. https://www.dph.illinois.gov/covid19/covid19-statistics [Google Scholar]
- 5.Io Medicine, Council NR. Reducing the Odds: Preventing Perinatal Transmission of HIV in the United States. The National Academies Press; 1999:416. [PubMed] [Google Scholar]
- 6.Angulo FJ, Finelli L, Swerdlow DL. Reopening Society and the Need for Real-Time Assessment of COVID-19 at the Community Level. JAMA. 2020;323(22):2247–2248. 10.1001/jama.2020.7872 [DOI] [PubMed] [Google Scholar]
- 7.Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology. 2020/07/01/ 2020;47:37–44. 10.1016/j.annepidem.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen J, Kupferschmidt K. Countries test tactics in ‘war’ against COVID-19. Science. 2020;367(6484):1287–1288. 10.1126/science.367.6484.1287 [DOI] [PubMed] [Google Scholar]
- 9.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Affairs. 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 10.Solis J, Franco-Paredes C, Henao-Martínez AF, Krsak M, Zimmer SM. Structural Vulnerability in the United States Revealed in Three Waves of Novel Coronavirus Disease (COVID-19). The American Journal of Tropical Medicine and Hygiene. 2020; 10.4269/ajtmh.20-0391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borjas GJ. Demographic Determinants of Testing Incidence and COVID-19 Infections in New York City Neighborhoods. 2020. [Google Scholar]
- 12.Duaa Eldeib AG, Akilah Johnson, Waldman Annie, Martin Nina, Buford Talia and Briscoe Tony. The First 100. COVID-19 Took Black Lives First. It Didnť Have To.: ProPublica Illinois; 2020.
- 13.Chicago Department of Public Health. Latest Data. Chicago Department of Public Health (CDPH). https://www.chicago.gov/city/en/sites/covid-19/home/latest-data.html [Google Scholar]
- 14.Kim S, Bostwick W. Social Vulnerability and Racial Inequality in COVID-19 Deaths in Chicago. Health Education & Behavior. 2020;47(4):509–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Center for Immunization and Respiratory Diseases (NCIRD) Division of Viral Diseases. Racial & Ethnic Minority Groups. Centers for Disease Control and Prevention. Accessed 6/20/20, 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
- 16.World Health Organization (WHO). Coronavirus disease (COVID-19) advice for the public. WHO. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Google Scholar]
- 17.Blake KS, Kellerson RL, Simic A. Measuring Overcrowding in Housing. U.S. Department of Housing and Urban Development. 2020. https://www.census.gov/content/dam/Census/programs-surveys/ahs/publications/Measuring_Overcrowding_in_Hsg.pdf
- 18.Raifman MA, Raifman JR. Disparities in the Population at Risk of Severe Illness From COVID-19 by Race/Ethnicity and Income. Am J Prev Med. April 27 2020; 10.1016/j.amepre.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019 (COVID-19), May 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html [Google Scholar]
- 20.Gould E, Wilson V. Black workers face two of the most lethal preexisting conditions for coronavirus—racism and economic inequality. 2020. June 1, 2020. https://www.epi.org/publication/black-workers-covid/
- 21.Rosenbaum S. The New “Public Charge” Rule Affecting Immigrants Has Major Implications for Medicaid and Entire Communities. The Commonwealth Fund. October 10, 2020. htps://www.commonwealthfund.org/blog/2019/new-public-charge-rule-affecting-immigrants-has-major-implications-medicaid-and-entire
- 22.Page KR, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. Immigrants and Covid-19. New England Journal of Medicine. 2020;382(21):e62. 10.1056/NEJMp2005953 [DOI] [PubMed] [Google Scholar]
- 23.Mile Square Health Center (MSHC). Mile Square Health Center (MSHC). University of Illinois Health System. https://hospital.uillinois.edu/patients-and-visitors/mile-square-federally-qualified-health-center [Google Scholar]
- 24.City of Chicago. Latest Data: Report Date March 28, 2020. City of Chicago. November 17,2020. https://www.chicago.gov/city/en/sites/covid-19/home/latest-data/2020-03-28.html [Google Scholar]
- 25.City of Chicago. Latest Data: Report Date April 5, 2020. City of Chicago. Accessed October 16, 2020, https://www.chicago.gov/content/dam/city/sites/covid/reports/2020-04-05/COVID-19_Confirmed%20case%20rate%20by%20zipcode%20April%205.pdf [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). COVID-19 Hospitalization and Death by Race/Ethnicity. Centers for Disease Control and Prevention. Accessed October 17, 2020, https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html [Google Scholar]
- 27.Chicago Tribune. Chicago’s coronavirus disparity: Black Chicagoans are dying at nearly six times the rate of white residents, data show. Chicago Tribune. Accessed October 12, 2020, https://www.chicagotribune.com/coronavirus/ct-coronavirus-chicago-coronavirus-deaths-demographics-lightfoot-20200406-77nlylhiavgjzb2wa4ckivh7mu-story.html [Google Scholar]
- 28.Chicago Department of Public Health. COVID Dashboard. Chicago Department of Public Health. https://www.chicago.gov/city/en/sites/covid-19/home/covid-dashboard.html [Google Scholar]
- 29.Rentsch C, Kidwai-Khan F, Tate J, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLOS Medicine. 2020;17(9): 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahajan U, Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. Journal of Public Health. 2020;42(3):445–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention (CDC). February 12, 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html#fn9 [Google Scholar]
- 32.Collins K, Tenney K, Hughes D. Collins KS, Tenney K, Hughes DL. Quality of health care for African Americans: Findings from the Commonwealth Fund 2001 Health Care Quality Survey. 2002. 2001 Health Care Quality Survey. https://www.commonwealthfund.org/publications/surveys/2002/mar/2001-health-care-quality-survey
- 33.Jaiswal J, Halkitis P. Towards a More Inclusive and Dynamic Understanding of Medical Mistrust Informed by Science. Behav Med. 2019;45(2):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaufman H, Niles J, Nash D. Disparities in SARS-CoV-2 Positivity Rates: Associations with Race and Ethnicity. Population Health Management. 2021;24(1):20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abel J, Deitz R. Some Workers Have Been Hit Much Harder than Others by the Pandemic. Federal Reserve Bank of New York. https://libertystreeteconomics.newyorkfed.org/2021/02/some-workers-have-been-hit-much-harder-than-others-by-the-pandemic.html [Google Scholar]
- 36.Heintzman J, O–Malley J, Marino M, et al. SARS-CoV-2 Testing and Changes in Primary Care Services in a Multistate Network of Community Health Centers During the COVID-19 Pandemic. JAMA. 2020;324(14):1459–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]