Abstract
Aim
To investigate the effect of self‐administration of medication programme on medication adherence in cardiovascular inpatients and nurse's satisfaction.
Design
Randomized clinical trial with parallel‐group design guided by the CONSORT checklist.
Methods
In this study, sixty cardiovascular inpatients were selected through convenience sampling and then randomly assigned to control and intervention groups, in 2018, Iran.
The intervention group took responsibility for consuming their prescribed medication according to the self‐administration of medication programme and the control group took medications routinely. Medication adherence was measured one and two weeks after the discharge via telephonic follow‐up by Morisky Medication Adherence Scale MMAS‐8‐item and nurses' satisfaction by researcher‐made questioner.
Result
There was a higher medication adherence level in the intervention group rather than the usual care group at the follow‐up. Most nurses in the study environment were very satisfied.
Conclusion
The self‐administration of medication programme can effectively increase patients' medication adherence and nurses' satisfaction.
Keywords: adherence, cardiovascular diseases, medication, nurses' satisfaction, self‐administration
1. INTRODUCTION
Coronary heart disease mortality causes about one‐third of all deaths in people older than 35 years (Sanchis‐Gomar et al., 2016). According to 2013 death statistic information, about more than 2,200 American people die of cardiovascular disease (CVD) daily and approximately 155,000 of them were less than 65 years old (Mozaffarian et al., 2016). In Iran, CVD is the prime mover of death in all ages and both sexes (yavari.p, 1394). Patients with CVD are at risk of recurrence of illness that can lead to undergoing long‐term treatment (Mega et al., 2012). In patients with CVD, one of the most important treatments is medication therapy and medication adherence is a fundamental prerequisite for effective pharmacological therapy (Tajouri et al., 2014). Non‐adherence to medications has been documented to occur in >60% of cardiovascular patients (Baroletti & Dell'Orfano, 2010).
Medication adherence is outlined by the World Health Organization as “the degree to which the person's behaviour corresponds with the agreed recommendations from a health care provider,” (Jimmy & Jose, 2011). Results of many studies indicated many patients are non‐adherence to medications particularly for medications related to CVD (such as antihypertensive medication and statins) with a rate of less than 50% (Tajouri et al., 2014).
2. BACKGROUND
Non‐adherence to medication is a major public health problem that compromises the effectiveness of therapies and results in suboptimal clinical outcomes (Lam & Fresco, 2015; Tajouri et al., 2014). Adherence rates are higher in acute disease compared with chronic diseases. Unfortunately, the level of medication adherence in chronic diseases is remarkably low and its rate is greatly reduced after six months of treatment (Haynes et al., 2002; Jackevicius et al., 2002).
Medication training can help patients to improve their medication adherence (Yazdanpanah et al., 2019). Accordingly, the WHO to achieve adherence suggests self‐management programmes, which include educational, behavioural strategies or combination in the form of multidisciplinary care. The educational nursing intervention and self‐management behavioural strategies progress adherence to a treatment, arranged by putting absent that patients to specific themselves not as they were as people that rely upon health care (Ghasemi et al., 2018). However, as heroes in a position to correctly manage their disorder and to empower themselves with the aid of acquiring disease administration competencies (Schneider et al., 2011). Moreover, fitting the intervention to the patients’ needs is necessary (Barfarazi et al., 2018). This includes investigating patients’ preferences, simplifying dosing regimens and using adherence aids (Kalogianni, 2012). With this regard, self‐administration of medication (SAM) programme seems a suitable intervention for response to these important patients’ needs. The idea of patients self‐administering their medication in hospital is not new (Vanwesemael et al., 2020). SAM programme includes permitting patients to require their medicines in the hospital, beneath shifting levels of supervision from health professionals such as pharmacists, nurses and healthcare providers (Anderson et al., 2014). SAM programme allows patients to have more time to participate in their medication management programme (Wright et al., 2006). The focus of SAM is setting up a standardized approach for selecting the capability of patients to want their possess accurately and safely, increase the patient's facts and grasp of their medication and develop and hold up persistent autonomy and independence (Richardson et al., 2014). Self‐administration suits with the concept of team nursing and current thinking about patient‐centred care. Nurses have a major function in medication education where possible and as long as it is safe for patients in hospitals patients should be encouraged to self‐administer their medication (Latter et al., 2001), and implementing self‐management programme with self‐administration strategy approves this position to be developed (Richardson et al., 2014).
Nevertheless, few studies were assessed the nurse satisfaction with implementing the self‐administered medication programme. Accordingly, the results of a systematic review showed significantly higher levels of nurse satisfaction with implementing the SAM programme; however, there are still differences in the results of studies on the challenges of implementing such a programme by nurses and its effects on their work (Richardson et al., 2014).
At present, the usual routine of medication administration at hospitals in Iran is the prescribing of medications by physicians and nurses without any involvement of patients admitted to it. However, immediately after discharge, the responsibility for managing the use of medications is left to the patient or his family, while the patient has no readiness for this, either in knowledge or self‐efficacy. This process can be accompanied by confusion, anxiety, medication error and eventually medication non‐adherence. Despite the researches regarding the performance of the SAM programme abroad, according to our wide search, no study and operational programme were developed to use the SAM programme in the country. On the other hand, due to the influence of cultural factors, pharmaceutical knowledge, belief in the treatment team and environmental conditions in this regard, the results of other countries studies cannot be generalized. The idea of compliance is associated too closely with blame, from providers or patients, so to maintain optimal health in people with chronic diseases the concept of adherence is a better way of capturing the dynamic and complex changes required of many players over long periods (Sabaté, 2003). It ought to be that considers most studies carried out before this have investigated medication compliance, whereas the current study was conducted to assess the adherence of the medication regimen. Therefore, this study sought to investigate the effect of self‐administration of medication programme on medication adherence in cardiovascular inpatients and nurse's satisfaction with the implementation of this programme. The research question was “what is the effect of Self‐administration of Medication Programme on Cardiovascular Inpatients’ Medication Adherence and Nurses' satisfaction?”
3. THE STUDY
3.1. Design
This study was a randomized clinical trial with a parallel‐group design, including two arms (intervention and control) guided by the CONSORT checklist (Figure 1). Consolidated Standards of Reporting Trials (CONSORT) checklist was applied as the reporting guideline for this study (Appendix S1, CONSORT checklist).
FIGURE 1.
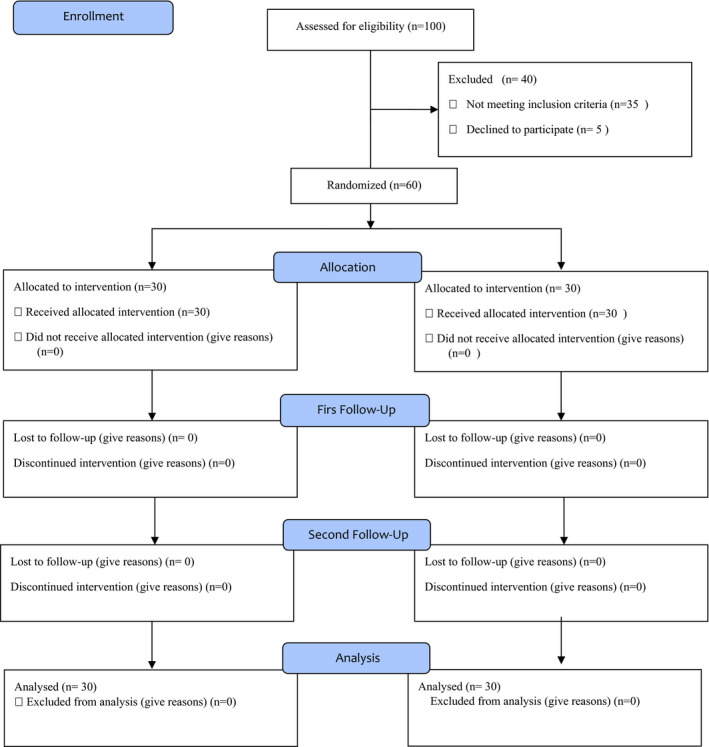
The CONSORT checklist of study
3.2. Methods
This study was conducted to compare the effect of self‐administration of medication programme on medication adherence. The primary outcome was the ratio of adherent patients to complete cardiac medication therapy at two weeks’ postdischarge and was measured one and two weeks after the discharge via telephonic follow‐up by Morisky Medication Adherence Scale. The secondary outcome was Nurses' satisfaction with SAM programme implementation that which was an assessment of nursing satisfaction with the implementation of SAM programme at the end of intervention.
3.3. Populations, inclusion, and exclusion criteria
This study was conducted with 60 patients hospitalized in the cardiovascular department of Emam Reza Educational, Research and Treatment Center in 2018. Participant was eligible for inclusion criteria that include having complete consciousness, diagnosis of cardiovascular disease, age under 60 and over 18, having at least a primary education, and no cognitive or psychological disorders based on medical records, do not have hearing and visual impairments, using the cell phones, and if exacerbation of disease and a patient's need for critical care, diagnosis of patient inability to manage medication use based on checklist at each step, early discharge, and short‐term memory loss were excluded. Also, about 20 staff nurses with at least seven years of experience were asked to help and complete the Nurses’ satisfaction scale to facilitate the SAM programme.
3.4. Instruments of measurement
Our research tools were Morisky Medication Adherence Scale MMAS‐8‐item (©MMAS‐8) and Nurses’ satisfaction scale.
MMAS‐8‐item is a well‐validated self‐reporting questionnaire with good predictive validity to assess medication‐taking behaviour and adherence (Berlowitz et al., 2017; Morisky et al., 2008). Previously the reliability and validity of the Persian version of the MMAS were assessed in a sample of Iranian hypertensive patients and was reported acceptable reliability and validity. Therefore, this scale to identify the level of medication adherence among Persian‐speaking patients with chronic conditions can be used as a standard and reliable tool in future studies. Internal consistency was acceptable with an overall Cronbach's α coefficient of .697 and test‐retest reliability showed good reproducibility (r = .940) (Moharamzad et al., 2015). Despite this to determine the reliability in our population, the test‐retest method with a 3 days interval was used on 20 persons. A correlation coefficient of .79 was confirmed the reliability of the scale. Data for Medication adherence level based on MMAS eight‐item assuming in three levels consist of high adherence (score of 8), medium adherence (score of 6 to <8) and low adherence (scores of <6).
Nurses’ satisfaction scale with the SAM programme was a researcher‐made scale and prepared by one of the authors based on the previous literature and through reusing texts and new references about the satisfaction index with the SAM programme and under the supervision of the research team. This questionnaire consisted of seven questions that determined nurses’ satisfaction with the impact of the SAM programme. This scale includes seven items and a 4‐point Likert‐type scale, as follows: 1 strongly disagree, 2 disagree, 3 agree and 4 strongly agree. The lowest and highest scores obtainable from the form were 7 and 28, respectively. The higher the score, means the higher the nurses’ satisfaction rate for SAM programme implementation in their ward. The content validity index method was performed to determine the validity, and then after considering the essential modifications and suggestions, the final version of the instrument was confirmed by the coefficient of .96. To determine the reliability, the test–retest method with a 2–3 days interval was used on 10 persons. A correlation coefficient of .89 was confirmed the reliability of the scale.
3.5. Sample size and randomization
The sample size was calculated based on a pilot study. A pilot study on 20 patients was done. So considering 95% confidence coefficient and 80% power, with the comparison formula of the two means in communities (10 in each group). Therefore, 22 patients ought to be examined in each group but to be sure, 30 patients in each group were enrolled in the study and all of them finished the study. All eligible patients in the cardiology ward that enrolled between 22 May 2018–22 August 2018 by nurse staff consisted of the study population and after obtaining informed consent patients were selected through convenience sampling and by the time block randomization method randomly allocated to control and intervention groups by nurse staff and researcher. The participants were randomly divided into intervention and control groups according to the sequences generated by SPSS software. In this way, the software generated a random sequence of letters A and B. This sequence was written on small cards and kept in a sealed envelope. At the beginning of each week, the envelope door was opened and based on the code on the cards, it was determined that the intervention should be performed or controlled during that week. In this way, all eligible inpatients in that week were assigned to the control or intervention group. In addition, the use of this method prevented the dissemination of information between patients who may be in the ward at the same time.
3.6. Blinding
Due to the nature of the intervention, it was not possible to blind either the participants or the researcher to the study group assignment. Because the usual method of medication administration was performed by the nurse, the patient in the intervention group noticed a change in the method of medication administration, so it was not possible to hide the intervention from the research units. In the case of the person prescribing the medication, it was not possible to conceal the intervention because he/she noticed a change in method, and the researcher was supervised the proper implementation of the intervention. Therefore, the study is considered without blinding.
3.7. Intervention
In this study, the self‐administration of medication (SAM) programme was performed with the participation of staff nurses and patients under the supervision of the researcher. The educational intervention programme was designed and implemented based on a self‐administrated medicine guideline and principles. The intervention group took responsibility for consuming their prescribed medication according to the protocol of self‐administration of medication in three steps. According to the guideline, implementing the programme may not be appropriate for all patients, and first must ensure that the patient can be involved in the process. Each patient should be assessed for their ability to self‐administer their prescribed medicines by a staff nurse. Therefore, in the current study before implementing the programme patients' ability to administer their medicines and also the degree of education and management which they will need were assessed using the self‐administration assessment form. Then, the programme was implemented for cardiovascular patients in three stages as follows:
3.7.1. First stage
During the first 24 hr of hospitalization, the medications were administered by the staff nurse that is a member of the medication management team in this study and under the supervision of the researcher. Then, patients were taught verbally and face to face about medication information such as their name, dose, purpose, frequency, dosing time and side effects around twenty minutes. Based on the guideline, any supporting education should also be provided where appropriate and consideration should be given to providing patients with a medication reminder card. Therefore, standard brochures and pamphlets related to each medication and a checklist of reminder cards were provided to these patients for more information and to improve their medication adherence.
3.7.2. Second stage
In the second 24 hr, patients were responsible for taking their oral medications with the direct coordination of the staff nurse. At this stage, prescribed medications of patients for one day were placed in a special medication box that could be locked and the key was given to the nurses. The boxes, which were designed based on the research team's idea, included three partitions so that morning, noon and night medications could be separated to make it easier for patients to identify when to take the medication. According to the instructions given in the first step, patients requested their medications by calling the nurse with an alarm ring, so that they could take their medications after opening the box and under the coordinated supervision of the nurse. Important information such as medication name, dosage and time of use was necessarily attached to each medication by a Persian label (Figure 2).
FIGURE 2.
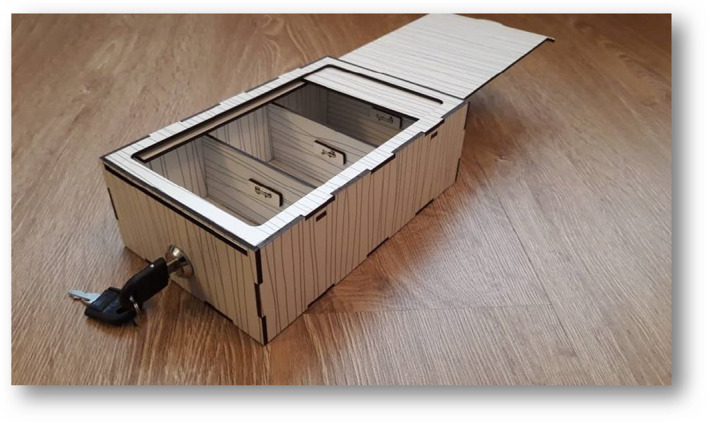
Medication box for intervention group
3.7.3. Third stage
At this stage, the patient's oral medications were placed in the box for the next two days so that they could take full responsibility for their medication use under the indirect nurse's supervision and continue the programme for days. The nurse was coordinated for indirect control by pill count. This process continued until discharge time from the hospital (4–6 days).
Additional considerations for implementing the intervention programme (SAM):
Confirmation of the qualification to pass each stage was subject to the approval of the nurse based on the checklists prepared for each stage.
At each stage, the patient was given a checklist of prescription medication to complete after taking the medication. This checklist was prepared to confirm that the patient and the nurse were taking the correct medication at the right time and to prevent forgetfulness of the medication or re‐use due to doubts about the medication and was seen and signed by the nurse at each shift. The nurse was coordinated for indirect control of the pill count. This counting took place at specific times and before the end of the shift (6:30 a.m., 12:30 p.m. and 6:30 p.m.).
If the patient delays obtaining permission to take the medications for one hour, it is considered as the first sign of unpreparedness while taking the medication and if it is repeated in the next meal, it was returned to the first stage. Use the medication again by the nurse. This was repeated up to 2 times, and if the patient was unable to take the medication on his or her own, he or she was excluded. In both cases, if the above was delayed, the patient was given the medication according to the routine.
It is to be noticed that any changes in the medication prescription made by the treating physician were notified to the patient by the nurse, and changes were made to the medication inside the box.
The intervention was performed by dividing the research units into two groups by the time block method. Therefore, one of the two methods was performed every week according to the sequences generated by SPSS software, which was coordinated with all nurses, as well as the head nurse and the doctor at the beginning of the week. So there was no interference.
3.8. Control
The medications were administrated to the patients by the nurse according to the usual method (at the appointed time, the nurse was present at the patient's bedside, giving the patient medication to use), and the patients received routine face‐to‐face training about their medications during the hospitalization and used the pharmaceutical pamphlets as more information.
3.9. Statistical analysis
Data analysis using the computer program Statistical Packages for Social Sciences (SPSS) version21 with considering the significance level α = .05 was done. Patients’ demographic and clinical characteristics were compared between the groups by using independent samples t tests for continuous variables or chi‐square tests for categorical variables. Also, the Mann–Whitney U test and Wilcoxon test were used for medication adherence scores between the groups and intergroup comparison.
3.10. Certificate of ethics approval
According to the law and the rules of best practice concerning research involving human participants, we sought and obtained the approval of the School of Nursing & Midwifery, Mashhad University of Medical Sciences, research ethic committee (REC) and then Iran Registry of Clinical Trials (IRCT). The REC issued approval for the clinical research proposal entitled “The effect of self‐administration of medication programme on level of self‐efficacy and medication adherence of patients with ischemic heart disease admitted in cardiac unit” on 2018‐04‐10 under the reference numbers “IR.MUMS.REC.1396.381,” and then confirmed it by Iran Registry of Clinical Trials on 2018‐ under the reference numbers of (20171223038022N1).
4. RESULTS
Thirty patients in each group were enrolled in the study, and all of them finished the study.
4.1. Sociodemographic variables
In the current study, 60 patients were examined. Sociodemographic variables such as age, gender, occupational status and hospitalization history caused by cardiovascular diseases, housing, level of education and other chronic diseases. According to the results, 21 (70%) of intervention group cases were women, and 18 (60%) of control group cases were men. The mean ages of patients in the control and intervention groups were 44.4 ± 8.5 and 40.9 ± 8.6 years, respectively. There was no significant difference between the two groups in terms of age, occupational status and hospitalization history caused by cardiovascular diseases, housing, level of education and other chronic diseases. However, a significant difference was observed between the two groups regarding gender (Table 1).
TABLE 1.
Comparison of the demographic characteristics of patients in two groups
| Variables | Group | Results of the intergroup test | |
|---|---|---|---|
| Control (N = 30) | Intervention (N = 30) | ||
| Gender (number %) | |||
| Male | 18 (%60) | 9 (%30) | p = .02 a |
| Female | 12 (%40) | 21 (%70) | |
| Hospitalization history (number %) | |||
| Yes | 6 (%20) | 12 (%30) | p = .09 a |
| No | 24 (%80) | 18 (%60) | |
| Other chronic diseases (number %) | |||
| Yes | 15 (%50) | 9 (%30) | p = .11 a |
| No | 15 (%50) | 21 (%70) | |
| Occupational status (number %) | |||
| Self‐employed | 18 (%60) | 9 (%30) | p = .053 b |
| Housewife | 11 (%37) | 19 (%63.3) | |
| Employee | 1 (%3.3) | 2 (%6.6) | |
| Level of education (number %) | |||
| Primary studies | 9 (%30) | 13 (%43.3) | p = .6 b |
| Secondary studies | 18 (%60) | 14 (%46.7) | |
| University studies | 3 (%10) | 3 (%10) | |
|
Age (years) Mean ± Standard deviation |
44.4 ± 8.5 | 40.9 ± 8.6 | p = .08 c |
Chi‐square test.
The Fisher's exact test.
The Mann‐Whitney U test.
4.2. Medication adherence
According to the results of the Mann–Whitney U test, in the first week after discharge, there was a significant difference in two groups (p < .001) for the medication adherence mean score and in the second week after discharge phase also, there was a significant difference in the mean score of medication adherence between the groups (p < .001).
Wilcoxon test results showed there is a significant difference (p = .014) between the mean score of medication adherence at first and second weeks after discharge in the intervention group, but no significant difference (p = .317) showed in the control group simultaneously (Table 2).
TABLE 2.
Mean and standard deviation of medication adherence score (©MMAS‐8) a in intervention and control groups
| Medication adherence | Group | Results of the intergroup test | |
|---|---|---|---|
| Control (N = 30) | Intervention(N = 30) | ||
| One week after discharge | |||
| Mean ± SD | 6.1 ± 3.1 | 7.6 ± 0.5 | p < .001 b |
| CI = %95 | 4.99, 7.210 | 7.42, 7.78 | |
| Two week after discharge | |||
| Mean ± SD | 6.0 ± 0.9 | 7.8 ± 0.4 | p < .001 b |
| CI = %95 | 5.68, 6.32 | 7.66, 7.94 | |
| Difference between two week | |||
| Mean ± SD | −0.1 ± 0.5 | 0.2 ± 0.4 | p = .022 b |
| CI = %95 | −0.279, 0.079 | 0.057, 0.343 | |
| Intragroup comparison result | p = .317 c | p = .014 c | |
The MMAS (8‐item) content, name and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from Donald E. Morisky, ScD, ScM, MSPH, MMAR, LLC, 294 Lindura Ct., Las Vegas, NV 89138, USA; dmorisky@gmail.com.
Mann–Whitney U test.
Wilcoxon test.
In addition to the medication adherence score, their levels were also compared. In the first week after discharge, the majority of the intervention group including 18 (60%) patients had high adherence score compared with 3 patients (10%) in the control group. Regarding the frequency of the medication adherence level, the result of the exact chi‐square test illustrated that there is a significant statistical difference between the groups (p < .001).
In follow‐up step two weeks after discharge, the majority of the intervention group including 24 (80%) patients had high adherence score which was three patients (10%) in the control group, and the exact chi‐square test showed a significant statistical difference between the two groups for the frequency of medication adherence level (p < .001) (Table 3).
TABLE 3.
Frequency distribution of patients with heart disease studied according to medication adherence levels 1 and 2 weeks after discharge in two groups of intervention and control
| Range | Group | Results of the intergroup test | |||
|---|---|---|---|---|---|
| Control | Intervention | ||||
| Percentage | (N = 30) | Percentage | (N = 30) | ||
| Adherence 1 week after discharge | |||||
| Low | %30 | 9 | – | – | p < .001 a |
| Middle | %60 | 18 | %40 | 12 | |
| High | %10 | 3 | %60 | 18 | |
| Adherence 2 week after discharge | |||||
| Low | %30 | 9 | – | – | p < .001 a |
| Middle | %60 | 18 | %20 | 6 | |
| High | %10 | 3 | %80 | 24 | |
Exact chi‐square test.
4.3. Nurses' satisfaction
According to the results of the nurse's satisfaction questionnaire presented that overall 60% (12 persons) of the nurses in the study area were very satisfied with the self‐management plan of medication use and none of them were very unsatisfied (Table 4). More than half (60%) of nurses believed that such a programme would reduce their workload and only less than half (45%) of them reported the programme would increase the time that the nurse would execute medication orders.
TABLE 4.
Frequency distribution of nurses' opinions about the implementation of self‐administration of medication programme in terms of satisfaction
| Nurse satisfaction | Number (N) | Percentage |
|---|---|---|
| Low satisfaction | – | – |
| Middle satisfaction | 8 | 40 |
| High satisfaction | 12 | 60 |
| Total | 20 | 100 |
5. DISCUSSION
The effect of self‐administration of medication programme on medication adherence among cardiovascular inpatients following discharge was the aim of this research. The results come about basically appeared a more noteworthy level of adherence among patients who gotten self‐administration of medication programme following discharge. Therefore with the implementation of the SAM programme, medication adherence increases in cardiovascular inpatients. Medication adherence follow‐up one week after discharge shows 60% of the patient had high medication adherence score while, the usual method that nurse was in charge of the administration of medication, only) 10.0%( had high medication adherence score. Also, in the medication follow‐up two weeks after discharge, medication adherence was increased in the intervention group (2.6%), while this was reduced (1.6%) in the control group compared to the first week. The trend of these changes may cause more differences in the long‐term.
Poor medication adherence due to its predominance and affiliation with unfavourable outcomes is a basic issue for patients, medical attendants, healthcare systems and society (Cutrona et al., 2012; Ho et al., 2008), and seriously control may avoid cardiovascular disease events in high‐risk patients and decrease healthcare costs (Bress et al., 2017). Besides, based on the results of a recent systematic review, five barriers related to medication adherence consist of patient factors, medication factors, physician factors, system‐based factors and other factors that were recognized (Lamarche et al., 2018). Somehow the finding of many researches revealed that medication adherence can be affected by these barriers. One might argue that this suggests the influence of these factors dependents on condition or setting. In this regard, one study stated that factors such as gender, race, age, education level and income were affected medication adherence. Nonetheless, researchers were stated that medication belief may be a more strength predictor of medication adherence than other mentioned factors. In this regard, one study investigated the effect of educational programmes using the health belief model on medication adherence of older people with hypertension. The results showed medication adherence by changing the beliefs of older people was improved (Yazdanpanah et al., 2019). Moreover, the results of another study showed implementing an inpatient SAM programme successfully recognized barriers to medication adherence that else may not have been identified and addressed that something tended to earlier to a patient's release the hospital (Tran et al., 2011).
Also, the results of one study indicate that individualized medication education has positive effects on patient quality of life and medication adherence (Serap Korkmaz et al., 2016). These findings are consistent with our study. Because in our study after determining the medication's educational needs of patients, the specific information was given to patients individually in both written and verbal form and it was presented with clear statements and comprehensively and also followed up by nurses. Therefore, it can lead to improve their medication adherence. Perhaps it can be stated that similarity in the educational intervention programmes, research procedure, and adherence measurement can be the reasons behind the consistency of the mentioned studies and current study.
Many researchers also were suggested that the application of these programmes may be improving medication adherence; thus, based on the results of these studies implementing a medication educational programme such as SAM may better manage this barrier and improving medication adherence. For example, Lam Study showed that the SAM programme could increase the competence and adherence of elder patients (10.8%) to manage their medication use and also, the non‐adherence with the medication regimen decreased by (12.3%) (Lam et al., 2011). Findings of the one study showed a significant relationship between attitude and medication adherence (Saleem et al., 2012), and the finding of another research indicated that patients had a positive attitude towards SAM and (83.9%) of them were presented their interest to self‐administer their medication (Vanwesemael et al., 2018). Moreover, increase self‐efficacy in medication use is directly related to medication adherence (Wu et al., 2011)., In this case, the result of the study by Haji Ali Beigloo et al. (2019) for performing the SAM among CVD hospitalized patients was shown to increase about (41%) of self‐efficacy of appropriate medication use at the time of discharge.
Also, Morisky et al. (2008) revealed that important concepts such as knowledge, patient satisfaction, coping skills, stress level, and medication complexity are associated with medication adherence. Accordingly, another study revealed that the SAM programme in qualified patients with CVD can improve medication knowledge and patient satisfaction (Haji Ali Beigloo et al., 2019). In the current study, implementing the medication education with SAM programme indirectly may lead to increase knowledge and satisfaction of patients. Therefore, this reason perhaps was to improve coping skills and was lead to increased medication adherence among these patients.
Accordingly, a recent study by Kaday et al. (2020), was showed the SAM programme significantly improved knowledge of and adherence in patients with chronic diseases (Kaday & Ratanajamit, 2020). Therefore, such a programme can increase patients knowledge of medication, and this awareness may be effective in increasing patients medication adherence because this increase in awareness of the benefits of regular use of medication and the side effects of quitting them can encourage patients to use their medications regularly (Haji Ali Beigloo et al., 2019; Kaday & Ratanajamit, 2020).
In another point of view, in our study, the SAM programme significantly increased patient adherence compared with the control group at the first follow‐up visit. This might be related to the knowledge received after SAM intervention, especially that regarding information labelled on the medication packages, medication indication and side effects and although patients in both groups were received medication information, patients in the study group should use the information more effectively as they were more familiar with the symbols/images than those in the control group. Therefore, knowledge about medication side effects that temporarily occurred and ceased over continuing use would enhance medication adherence, while patients’ lack of awareness of medication indication and side effects in the control group potentially affect the adherence and clinical consequences. Similar results were reported from other studies (Haji Ali Beigloo et al., 2019; Richardson et al., 2014).
Meanwhile, the results of the present study showed a good agreement with the previous studies in a variety of medical conditions and it seems that the use of the MMAS‐8 and the educational intervention based on the SAM is the possible reasons behind this consistency. However, in another study, there was no statistically significant difference between groups on medication adherence as a result of the implementation of the SAM programme (Jensen, 2003). Increased patient compliance by the SAM programme was confirmed by an RCT, although a qualitative systematic review revealed diverse results among included trials. It should be noted that in many studies conducted to investigate the effect of self‐administration of medication programme, medication “compliance” has been evaluated but in this study, the concept of “adherence” has been evaluated and this may be the reason for the difference in results. However, results on adherence might be compromised in the validity as most of the studies used pill count conducted by staff, very few used more reliable methods, such as urine tests or disguised observation. The present study also used a pill count method, as no sensitive or specific methods were available in the study hospital but using a valid and recognized tool for measuring the medication adherence (©MMAS‐8) and would be strange for this study. Medication adherence was retained at the second follow‐up visit in both groups. The effects of SAM on adherence were expected to sustain over time.
Regarding nurse satisfaction, in the current study as stated before 60% of the nurses in the study area were very satisfied with the implementation of a self‐management plan of medication use, and (60%) of nurses believed that such a programme would reduce their workload and also only less than half of the nurses about 45% believed the programme may increase the time that the nurse would execute medication orders. Similar results were indicated from other studies. In this regard, the finding of the study by Desborough (2009) showed that (91%) of 46 nurses would favour using the SAM programme, and about (52%) of them had been blissful to use this programme to grant PRN medication. but regarding the controlled medication their opinion was different. Most nurses were presented that time spent on administering medicines (87%) and discharge times (59%) was decreased. Also according to Grantham et al. (2006) study that nurses (N = 14) were surveyed at 1‐, 3‐ and 5‐month intervals (response rates of 62%, 62% and 57%, respectively). They reported being satisfied with the self‐medication process, and satisfaction did not change over time (Grantham et al., 2006). At three‐month post‐SAM scheme implementation, the 57% of staff believed that the SAM scheme increased their workload and time spent on education activities, but the decreased time spent on procedures related to patient discharge (Grantham et al., 2006). These suggestions are consistent with the current study. Besides, a study by Kaday et al. (2020), among inpatients with chronic diseases, indicated implementing the SAM programme significantly increased knowledge and adherence to prescribed medications and reduced hospital readmission. Moreover, researchers revealed that implementing such a programme reduces nurses' workload and saves more time for them. Also, medication errors regarding administration errors were infrequent but significantly higher in the control group.
It should be noted that pharmacists also participated in the study to implement of SAM programme (Kaday & Ratanajamit, 2020). However, due to the lack of pharmacists in the clinical areas of the study site in Iran, more workload may be imposed on nurses. Therefore, it seems that the implementation of such a programme requires the full cooperation of those in charge of treatment and care, including the physician in charge of the patient, pharmacist, nurses and other healthcare providers. Overall, the results obtained from the present study showing an increase in the level of nurse satisfaction and consistent with the findings of the mentioned research.
According to the results of the statistical tests, the two groups considered were homogeneous concerning background and interruptive variables. Besides, their impact on dependent variables was not noteworthy based on the comes about of three‐way ANOVA. Be that as it may, they were diverse in terms of executing the self‐administration medicine utilization programme. In this manner, the observed difference in medication adherence between the two groups can be attributed to the intervention impact. Besides, this programme was once looking to make people adhere to their medication and so inclined to the risks threatening their health status and assist them to identify the deterioration of their illness and improving medication adherence.
Thus, the research hypothesis on medication adherence was accepted by executing a self‐administration of medication use programme in the hospital. The results obtained from four days of implementing SAM programme initiation can be generalized, and qualified patients with the necessary abilities can execute the protocol.
6. LIMITATION
The brief follow‐up, single‐centre setting and impossibility to blind patients due to the nature of the interventions limit the generalizability of the study findings. Hence, further research inquiries that incorporate more participants from different centres with a longer follow‐up term are required to affirm the display comes about.
7. CONCLUSION
In conclusion, implementing an intervention programme as self‐administration of medication was associated with high adherence to cardiac medications and more nurse satisfaction. Since poor adherence is not only an issue relating to cardiac medication therapy, it is proposed that this programme can be connected to optimize medication adherence for a more extensive range of chronic diseases. Also, most nurses in the study environment were very satisfied with the implementation of the programme and more than half of nurses believed that such a programme would reduce their workload, and regarding the time only less than half reported the programme may increase the time that the nurse would execute medication orders. This programme (SAM) in cardiovascular patients could help to analyse the individual patient factor and behavioural strategies that might become barriers to medication adherence and to apply nursing interventions that promote better patient medication adherence and nurse satisfaction.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS CONTRIBUTIONS
Study design: RH, SRM, SM; data collection and analysis: RH, SRM and manuscript preparation: RH, SRM, SM, DEM. Professor Donald E. Morisky is the developer/owner of the copyrighted MMAS intellectual property and receives a license fee for the use of the MMAS diagnostic adherence scale. He was not involved in any data analysis in this study. All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE [https://www.icmje.org/recommendations/]): substantial contributions to conception and design, acquisition of data or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content.
RESEARCH REPORTING CHECKLIST
Guidelines for reporting parallel‐group randomized trials, Appendix S1.
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
This article is extracted from a thesis of MSc student in Medical ‐Surgery nursing with the ethical code of IR.MUMS.REC.1396.381 and registration code of IRCT20171223038022N1 at the Clinical Practice Database under the financial aegis of Research Deputy of Mashhad University of Medical Sciences, Mashhad, Iran. The authors would like to express their gratitude to all managers, authors and dear patients who were involved in this study. Also, we would like to acknowledge from Professor Donald E. Morisky for permission the use of the scale of the Morisky Medication Adherence Scale MMAS‐8‐item (©MMAS‐8), The MMAS (8‐item) content, name and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from Donald E. Morisky, ScD, ScM, MSPH, MMAR, LLC, 294 Lindura Ct., Las Vegas, NV 89138, USA; dmorisky@gmail.com.
Hajialibeigloo R, Mazlum SR, Mohajer S, Morisky DE. Effect of self‐administration of medication programme on cardiovascular inpatients' medication adherence and nurses' satisfaction: A randomized clinical trial. Nurs Open. 2021;8:1947–1957. 10.1002/nop2.870
Prospective Clinical Trial Registration code: IRCT20171223038022N1.
Ethical Approval Code: IR.MUMS.REC.1396.381.
Funding information
Under the financial aegis of Research Deputy of Mashhad University of Medical Sciences, Mashhad, Iran
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon request. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Anderson, J. , Manias, E. , Kusljic, S. , & Finch, S. (2014). Testing the validity, reliability and utility of the Self‐Administration of Medication (SAM) tool in patients undergoing rehabilitation. Research in Social & Administrative Pharmacy, 10(1), 204–216. 10.1016/j.sapharm.2013.04.013 [DOI] [PubMed] [Google Scholar]
- Barfarazi, H. , Pourghaznein, T. , Mohajer, S. , Mazlom, S. R. , & Asgharinekah, S. M. (2018). Evaluating the effect of painting therapy on happiness in the elderly. Evidence Based Care, 8(3), 17–26. [Google Scholar]
- Baroletti, S. , & Dell'Orfano, H. (2010). Medication adherence in cardiovascular disease. Circulation, 121(12), 1455–1458. 10.1161/circulationaha.109.904003 [DOI] [PubMed] [Google Scholar]
- Berlowitz, D. R. , Foy, C. G. , Kazis, L. E. , Bolin, L. P. , Conroy, M. B. , Fitzpatrick, P. , Gure, T. R. , Kimmel, P. L. , Kirchner, K. , Morisky, D. E. , Newman, J. , Olney, C. , Oparil, S. , Pajewski, N. M. , Powell, J. , Ramsey, T. , Simmons, D. L. , Snyder, J. , Supiano, M. A. , … Whittle, J. (2017). Effect of intensive blood‐pressure treatment on patient‐reported outcomes. New England Journal of Medicine, 377(8), 733–744. 10.1056/NEJMoa1611179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bress, A. P. , Bellows, B. K. , King, J. B. , Hess, R. , Beddhu, S. , Zhang, Z. , Berlowitz, D. R. , Conroy, M. B. , Fine, L. , Oparil, S. , Morisky, D. E. , Kazis, L. E. , Ruiz‐Negrón, N. , Powell, J. , Tamariz, L. , Whittle, J. , Wright, J. T. , Supiano, M. A. , Cheung, A. K. , … Moran, A. E. (2017). Cost‐effectiveness of intensive versus standard blood‐pressure control. New England Journal of Medicine, 377(8), 745–755. 10.1056/NEJMsa1616035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona, S. L. , Choudhry, N. K. , Fischer, M. A. , Servi, A. D. , Stedman, M. , Liberman, J. N. , Brennan, T. A. , & Shrank, W. H. (2012). Targeting cardiovascular medication adherence interventions. Journal of the American Pharmacists Association, 52(3), 381–397. 10.1331/JAPhA.2012.10211 [DOI] [PubMed] [Google Scholar]
- Desborough, J. A. C. , Saadvandi, R. , Sockett, R. , & Thomson, R. (2009). The impact of self‐administration of medicines on patients and nursing staff. International Journal of Pharmacy Practice B, 49. [Google Scholar]
- Ghasemi, A. , Karimi Moonaghi, H. , Mohajer, S. , Mazlom, S. R. , & Shoeibi, N. J. (2018). Effect of self‐management educational program on vision‐related quality of life among elderly with visual impairment. Evidence Based Care, 8(1), 35–44. [Google Scholar]
- Grantham, G. , McMillan, V. , Dunn, S. V. , Gassner, L. A. , & Woodcock, P. (2006). Patient self‐medication‐A change in hospital practice. Journal of Clinical Nursing, 15(8), 962–970. 10.1111/j.1365-2702.2006.01398.x [DOI] [PubMed] [Google Scholar]
- Haji Ali Beigloo, R. , Mohajer, S. , Eshraghi, A. , & Mazlom, S. R. (2019). Self‐administered medications in cardiovascular ward: A study on patients' self‐efficacy, knowledge and satisfaction. Evidence Based Care, 9(1), 16–25. [Google Scholar]
- Haynes, R. B. , McDonald, H. P. , & Garg, A. X. (2002). Helping patients follow prescribed treatment: Clinical applications. Journal of the American Medical Association, 288(22), 2880–2883. 10.1001/jama.288.22.2880 [DOI] [PubMed] [Google Scholar]
- Ho, P. M. , Magid, D. J. , Shetterly, S. M. , Olson, K. L. , Maddox, T. M. , Peterson, P. N. , Masoudi, F. A. , & Rumsfeld, J. S. (2008). Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. American Heart Journal, 155(4), 772–779. 10.1016/j.ahj.2007.12.011 [DOI] [PubMed] [Google Scholar]
- Jackevicius, C. A. , Mamdani, M. , & Tu, J. V. (2002). Adherence with statin therapy in elderly patients with and without acute coronary syndromes. Journal of the American Medical Association, 288(4), 462–467. 10.1001/jama.288.4.462 [DOI] [PubMed] [Google Scholar]
- Jensen, L. (2003). Self‐administered cardiac medication program evaluation. Canadian Journal of Cardiovascular Nursing, 13(2), 35–44. [PubMed] [Google Scholar]
- Jimmy, B. , & Jose, J. (2011). Patient medication adherence: Measures in daily practice. Oman Medical Journal, 26(3), 155–159. 10.5001/omj.2011.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaday, R. , & Ratanajamit, C. (2020). Inpatient self‐administered medication under the supervision of a multidisciplinary team: A randomized, controlled, blinded parallel trial. Pharmacy Practice, 18(2), 1766. 10.18549/PharmPract.2020.2.1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalogianni, A. (2012). Can nursing interventions increase adherence medication regimen? Health Science Journal, 6(1), 1. [Google Scholar]
- Lam, P. , Elliott, R. A. , & George, J. (2011). Impact of a self‐administration of medications programme on elderly inpatients' competence to manage medications: A pilot study. Journal of Clinical Pharmacy and Therapeutics, 36(1), 80–86. 10.1111/j.1365-2710.2009.01157.x [DOI] [PubMed] [Google Scholar]
- Lam, W. Y. , & Fresco, P. (2015). Medication adherence measures: An overview. BioMed Research International, 2015, 217047. 10.1155/2015/217047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche, L. , Tejpal, A. , & Mangin, D. (2018). Self‐efficacy for medication management: A systematic review of instruments. Patient Preference and Adherence, 12, 1279–1287. 10.2147/PPA.S165749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latter, S. , Rycroft‐Malone, J. , Yerrell, P. , & Shaw, D. (2001). Nurses’ educational preparation for a medication education role: Findings from a national survey. Nurse Education Today, 21(2), 143–154. 10.1054/nedt.2000.0528 [DOI] [PubMed] [Google Scholar]
- Mega, J. L. , Braunwald, E. , Wiviott, S. D. , Bassand, J. P. , Bhatt, D. L. , Bode, C. , Burton, P. , Cohen, M. , Cook‐Bruns, N. , Fox, K. A. A. , Goto, S. , Murphy, S. A. , Plotnikov, A. N. , Schneider, D. , Sun, X. , Verheugt, F. W. A. , & Gibson, C. M. (2012). Rivaroxaban in patients with a recent acute coronary syndrome. New England Journal of Medicine, 366(1), 9–19. 10.1056/NEJMoa1112277 [DOI] [PubMed] [Google Scholar]
- Moharamzad, Y. , Saadat, H. , Nakhjavan Shahraki, B. , Rai, A. , Saadat, Z. , Aerab‐Sheibani, H. , Naghizadeh, M. M. , & Morisky, D. E. (2015). Validation of the Persian version of the 8‐item Morisky medication adherence scale (MMAS‐8) in Iranian hypertensive patients. Global Journal of Health Science, 7(4), 173–183. 10.5539/gjhs.v7n4p173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morisky, D. E. , Ang, A. , Krousel‐Wood, M. , & Ward, H. J. (2008). Predictive validity of a medication adherence measure in an outpatient setting. The Journal of Clinical Hypertension, 10(5), 348–354. 10.1111/j.1751-7176.2008.07572.x [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Mozaffarian, D. , Benjamin, E. J. , Go, A. S. , Arnett, D. K. , Blaha, M. J. , Cushman, M. , Das, S. R. , de Ferranti, S. , Després, J.‐P. , Fullerton, H. J. , Howard, V. J. , Huffman, M. D. , Isasi, C. R. , Jiménez, M. C. , Judd, S. E. , Kissela, B. M. , Lichtman, J. H. , Lisabeth, L. D. , Liu, S. , … Turner, M. B. (2016). Executive summary: Heart disease and stroke statistics–2016 update: A report from the American heart association. Circulation, 133(4), 447–454. 10.1161/cir.0000000000000366 [DOI] [PubMed] [Google Scholar]
- Richardson, S. J. , Brooks, H. L. , Bramley, G. , & Coleman, J. J. (2014). Evaluating the effectiveness of self‐administration of medication (SAM) schemes in the hospital setting: A systematic review of the literature. PLoS One, 9(12), e113912. 10.1371/journal.pone.0113912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabaté, E. (2003). Adherence to long‐term therapies: Evidence for action. World Health Organization. [PubMed] [Google Scholar]
- Saleem, F. , Hassali, M. , Shafie, A. , & Atif, M. (2012). Drug attitude and adherence: A qualitative insight of patients with hypertension. Journal of Young Pharmacists, 4(2), 101–107. 10.4103/0975-1483.96624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchis‐Gomar, F. , Perez‐Quilis, C. , Leischik, R. , & Lucia, A. (2016). Epidemiology of coronary heart disease and acute coronary syndrome. Annals of Translational Medicine, 4(13), 256. 10.21037/atm.2016.06.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, S. M. , Hess, K. , & Gosselin, T. (2011). Interventions to promote adherence with oral agents. Seminars in Oncology Nursing, 27(2), 133–141. 10.1016/j.soncn.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serap Korkmaz, R. , Sevinc Tastan, R. , & Salih Pay, M. (2016). The effect of individualized drug education on medication adherence among patients using biologic drugs. International Journal of Caring Sciences, 9(3), 965. [Google Scholar]
- Tajouri, T. H. , Driver, S. L. , & Holmes, D. R., Jr . (2014). ‘Take as directed’ [mdash] strategies to improve adherence to cardiac medication. Nature Reviews Cardiology, 11(5), 304–307. 10.1038/nrcardio.2013.208 [DOI] [PubMed] [Google Scholar]
- Tran, T. , Elliott, R. A. , Taylor, S. E. , & Woodward, M. C. (2011). A self‐administration of medications program to identify and address potential barriers to adherence in elderly patients. Annals of Pharmacotherapy, 45(2), 201–206. 10.1345/aph.1P473 [DOI] [PubMed] [Google Scholar]
- Vanwesemael, T. , Boussery, K. , & Dilles, T. J. (2020). Self‐Administration of medication in hospital: A literature review. Nursing Science Quarterly, 33(3), 249–257. [DOI] [PubMed] [Google Scholar]
- Vanwesemael, T. , Boussery, K. , van den Bemt, P. , & Dilles, T. (2018). The willingness and attitude of patients towards self‐administration of medication in hospital. Therapeutic Advances in Drug Safety, 9(6), 309–321. 10.1177/2042098618764536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, J. , Emerson, A. , Stephens, M. , & Lennan, E. (2006). Hospital inpatient self‐administration of medicine programmes: A critical literature review. Pharmacy World & Science, 28(3), 140–151. 10.1007/s11096-006-9014-x [DOI] [PubMed] [Google Scholar]
- Wu, S. F. V. , Kao, M. J. , Wu, M. P. , Tsai, M. W. , & Chang, W. W. (2011). Effects of an osteoarthritis self‐management programme. Journal of Advanced Nursing, 67(7), 1491–1501. 10.1111/j.1365-2648.2010.05603.x [DOI] [PubMed] [Google Scholar]
- yavari.p (1394). Epidemiology of common diseases Iran. Gap. [Google Scholar]
- Yazdanpanah, Y. , Saleh Moghadam, A. R. , Mazlom, S. R. , Haji Ali Beigloo, R. , & Mohajer, S. (2019). Effect of an educational program based on health belief model on medication adherence in elderly patients with hypertension. Evidence Based Care, 9(1), 52–62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request. The data are not publicly available due to privacy or ethical restrictions.


