Abstract
Background
Oral 5‐aminosalicylic acid (5‐ASA) preparations were intended to avoid the adverse effects of sulfasalazine (SASP) while maintaining its therapeutic benefits. It was previously found that 5‐ASA drugs in doses of at least 2 g/day were more effective than placebo but no more effective than SASP for inducing remission in ulcerative colitis (UC). This review is an update of a previously published Cochrane Review.
Objectives
To assess the efficacy, dose‐responsiveness and safety of oral 5‐ASA compared to placebo, SASP, or 5‐ASA comparators (i.e. other formulations of 5‐ASA) for induction of remission in active UC. A secondary objective was to compare the efficacy and safety of once‐daily dosing of oral 5‐ASA versus conventional dosing regimens (two or three times daily).
Search methods
We searched MEDLINE, Embase and the Cochrane Library on 11 June 2019. We also searched references, conference proceedings and study registers to identify additional studies.
Selection criteria
We considered randomized controlled trials (RCTs) including adults (aged 18 years or more) with active UC for inclusion. We included studies that compared oral 5‐ASA therapy with placebo, SASP, or other 5‐ASA formulations. We also included studies that compared once‐daily to conventional dosing as well as dose‐ranging studies.
Data collection and analysis
Outcomes include failure to induce global/clinical remission, global/clinical improvement, endoscopic remission, endoscopic improvement, adherence, adverse events (AEs), serious adverse events (SAEs), withdrawals due to AEs, and withdrawals or exclusions after entry. We analyzed five comparisons: 5‐ASA versus placebo, 5‐ASA versus sulfasalazine, once‐daily dosing versus conventional dosing, 5‐ASA (e.g. MMX mesalamine, Ipocol, Balsalazide, Pentasa, Olsalazine and 5‐ASA micropellets) versus comparator 5‐ASA (e.g. Asacol, Claversal, Salofalk), and 5‐ASA dose‐ranging. We calculated the risk ratio (RR) and 95% confidence interval (95% CI) for each outcome. We analyzed data on an intention‐to‐treat basis, and used GRADE to assess the overall certainty of the evidence.
Main results
We include 54 studies (9612 participants). We rated most studies at low risk of bias.
Seventy‐one per cent (1107/1550) of 5‐ASA participants failed to enter clinical remission compared to 83% (695/837) of placebo participants (RR 0.86, 95% CI 0.82 to 0.89; 2387 participants, 11 studies; high‐certainty evidence). We also observed a dose‐response trend for 5‐ASA. There was no difference in clinical remission rates between 5‐ASA and SASP. Fifty‐four per cent (150/279) of 5‐ASA participants failed to enter remission compared to 58% (144/247) of SASP participants (RR 0.90, 95% CI 0.77 to 1.04; 526 participants, 8 studies; moderate‐certainty evidence).
There was no difference in remission rates between once‐daily dosing and conventional dosing. Sixty per cent (533/881) of once‐daily participants failed to enter clinical remission compared to 61% (538/880) of conventionally‐dosed participants (RR 0.99, 95% CI 0.93 to 1.06; 1761 participants, 5 studies; high‐certainty evidence). Eight per cent (15/179) of participants dosed once daily failed to adhere to their medication regimen compared to 6% (11/179) of conventionally‐dosed participants (RR 1.36, 95% CI 0.64 to 2.86; 358 participants, 2 studies; low‐certainty evidence).
There does not appear to be any difference in efficacy among the various 5‐ASA formulations. Fifty per cent (507/1022) of participants in the 5‐ASA group failed to enter remission compared to 52% (491/946) of participants in the 5‐ASA comparator group (RR 0.94, 95% CI 0.86 to 1.02; 1968 participants, 11 studies; moderate‐certainty evidence).
There was no evidence of a difference in the incidence of adverse events and serious adverse events between 5‐ASA and placebo, once‐daily and conventionally‐dosed 5‐ASA, and 5‐ASA and comparator 5‐ASA formulation studies. Common adverse events included flatulence, abdominal pain, nausea, diarrhea, headache and worsening UC. SASP was not as well tolerated as 5‐ASA. Twenty‐nine per cent (118/411) of SASP participants experienced an AE compared to 15% (72/498) of 5‐ASA participants (RR 0.48, 95% CI 0.36 to 0.63; 909 participants, 12 studies; moderate‐certainty evidence).
Authors' conclusions
There is high‐certainty evidence that 5‐ASA is superior to placebo, and moderate‐certainty evidence that 5‐ASA is not more effective than SASP. Considering relative costs, a clinical advantage to using oral 5‐ASA in place of SASP appears unlikely. High‐certainty evidence suggests 5‐ASA dosed once daily appears to be as efficacious as conventionally‐dosed 5‐ASA. There may be little or no difference in efficacy or safety among the various 5‐ASA formulations.
Plain language summary
Oral 5‐aminosalicylic acid for the treatment of active ulcerative colitis
What is ulcerative colitis?
Ulcerative colitis (UC) is a condition that causes inflammation of your large intestine (colon). Some of the symptoms associated with UC include diarrhea, abdominal pain, rectal pain, rectal bleeding, weight loss, fatigue and fever.
What is 5‐aminosalicylic acid (5‐ASA)?
Sulfasalazine (SASP) has been used for treating UC for decades. SASP is made up of 5‐aminosalicylic acid (5‐ASA) linked to a sulfur molecule. Up to a third of people treated with SASP have reported side effects, which are thought to be related to the sulfur part of the molecule. Common side effects associated with SASP include nausea, indigestion, headache, vomiting and abdominal pain. 5‐ASA drugs were developed to avoid the side effects associated with SASP. 5‐ASA is commonly taken by mouth.
What did the researchers investigate?
The researchers examined whether oral 5‐ASA helps to cause remission in people with UC. The researchers investigated whether oral 5‐ASA was better than placebo (a fake medication) or a different 5‐ASA formulation.
Key results
This review includes 54 randomized trials with a total of 9612 people taking part. The review includes studies published up to June 2019. Oral 5‐ASA was found to be more effective than placebo (fake drug). Although oral 5‐ASA drugs are effective for treating active UC, they are no more effective than SASP therapy. People taking 5‐ASA are less likely to experience side effects than those taking SASP. Side effects associated with 5‐ASA are generally mild in nature, and common side effects include digestive tract symptoms (e.g. flatulence, abdominal pain, nausea, and diarrhea), headache and worsening UC. 5‐ASA compounds are more expensive than SASP, so SASP may be the preferred option where cost is an important factor. 5‐ASA given once daily appears to be as effective as 5‐ASA given in the usual way (two or three times daily). There do not appear to be any differences in effectiveness or safety among the various 5‐ASA formulations.
Conclusions
High‐certainty evidence suggests that 5‐ASA is superior to placebo and that 5‐ASA once‐daily dose has the same effectiveness and safety as the conventional 5‐ASA dose. Moderate‐certainty evidence also suggests that 5‐ASA is not superior to SASP. Sticking to the medication does not appear to improve with once‐daily dosing compared to conventional dosing. Lastly, there may be little or no difference in effectiveness or safety among the various 5‐ASA formulations.
Summary of findings
Summary of findings 1. Oral 5‐ASA versus placebo for induction of remission in ulcerative colitis.
| Oral 5‐ASA versus placebo for induction of remission in ulcerative colitis | ||||||
| Patient or population: People with active mild‐to‐moderate ulcerative colitis Settings: Outpatient Intervention: Oral 5‐ASA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Oral 5‐ASA | |||||
|
Failure to induce complete global or clinical remission Follow‐up: 6 ‐ 12 weeks |
830 per 1000a | 714 per 1000 (681 to 739) | RR 0.86 (0.82 to 0.89) | 2387 (11 studies) | ⊕⊕⊕⊕ HIGH | Global or clinical remission was defined as a score of 0 points for stool frequency and rectal bleeding |
|
Failure to induce global or clinical improvement Follow‐up: 6 ‐ 12 weeks |
651 per 1000a | 443 per 1000 (397 to 488) | RR 0.68 (0.61 to 0.75) | 2256 (14 studies) | ⊕⊕⊕⊝ MODERATEb | Clinical improvement was defined as a decrease of 3 points from baseline in the overall modified UC‐DAI score |
|
Failure to induce endoscopic remission Follow‐up: 6 ‐ 14 weeks |
639 per 1000 |
492 per 1000 (428 to 569) |
RR 0.77 (0.67 to 0.89) |
1154 (4 studies) |
⊕⊕⊕⊝ MODERATEc | Endoscopic improvement was defined as endoscopy/sigmoidoscopy score of ≤ 1 |
| Failure to adhere to medication regimen | This outcome is not reported | Not reported | ||||
|
Adverse events Follow‐up: 6 ‐ 12 weeks |
486 per 1000a | 462 per 1000 (413 to 520) | RR 0.95 (0.85 to 1.07) | 1218 (8 studies) | ⊕⊕⊕⊕ HIGH | Adverse events included headache, nausea, abdominal pain or cramps, nasopharyngitis or symptoms of upper respiratory infection, rash. anorexia or loss of appetite, flatulence or gas, gastrointestinal disorders and fever |
|
Serious adverse events Follow‐up: 6 ‐ 12 weeks |
21 per 1,000a |
11 per 1000 (4 to 33) |
RR 0.53 (0.18 to 1.56) |
746 (4 studies) |
⊕⊕⊝⊝ LOWd | Serious adverse events included aggravation of UC, malaise, abdominal abscess, pancreatitis and an inguinal hernia |
|
Withdrawal due to adverse events Follow‐up: 6 ‐ 12 weeks |
88 per 1000a | 63 per 1000 (47 to 85) | RR 0.72 (0.54 to 0.97) | 2372 (13 studies) | ⊕⊕⊕⊝ MODERATEe | Common adverse events leading to withdrawal were not reported |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio UC: ulcerative colitis; UC‐DAI: ulcerative colitis ‐ disease activity index | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aControl group risk estimates come from control arm of meta‐analysis, based on included trials. bDowngraded one level due to heterogeneity I2 = 47%. cDowngrade one level due to heterogeneity I2 = 42%. dDowngraded two levels due to very sparse data (13 events). eDowngraded one level due to sparse data (164 events).
Summary of findings 2. Oral 5‐ASA versus SASP for induction of remission in ulcerative colitis.
| Oral 5‐ASA versus SASP for induction of remission in ulcerative colitis | ||||||
| Patient or population: People with active mild‐to‐moderate ulcerative colitis Settings: Outpatient Intervention: Oral 5‐ASA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| SASP | Oral 5‐ASA | |||||
|
Failure to induce global or clinical remission Follow‐up: 4 ‐ 8 weeks |
583 per 1000a | 525 per 1000 (449 to 606) | RR 0.90 (0.77 to 1.04) | 526 (8 studies) | ⊕⊕⊕⊝ MODERATEb | Global or clinical remission was defined as the return to stool frequency (2 ‐ 3 stools or fewer a day) without the presence of blood |
|
Failure to induce global or clinical improvement Follow‐up: 4 ‐ 8 weeks |
467 per 1000a | 411 per 1000 (355 to 472) | RR 0.88 (0.76 to 1.01) | 1053 (14 studies) | ⊕⊕⊕⊕ HIGH | Clinical improvement was defined as reduction in their clinical activity index |
| Failure to induce endoscopic remission | See comment | 2 studies reported this outcome but meta‐analysis not performed as they used different measurement indices. Neither study showed significant differences in complete endoscopic remission between 5‐ASA and SASP | ||||
| Failure to adhere to medication regimen | See comment | Outcome not reported | ||||
|
Adverse events Follow‐up: 4 ‐ 8 weeks |
287 per 1000a | 138 per 1000 (103 to 181) | RR 0.48 (0.36 to 0.63) | 909 (12 studies) | ⊕⊕⊕⊝ MODERATEc | Adverse events included nausea, headache, dyspepsia, vomiting, abdominal pain and rash |
|
Serious adverse events Follow‐up: 4 ‐ 8 weeks |
38 per 1000 |
51 per 1000 (11 to 246) |
RR 1.36 (0.28 to 6.52) |
107 (2 studies) |
⊕⊕⊝⊝ LOWd | Serious adverse events included erythematous rash, venous thrombosis, carcinoma, acute pancreatitis, rheumatoid arthritis and erythema nodosum |
|
Withdrawal due to adverse events Follow‐up: 4 ‐ 8 weeks |
129 per 1000a | 52 per 1000 (31 to 88) | RR 0.40 (0.24 to 0.68) | 640 (10 studies) | ⊕⊕⊕⊝ MODERATEe | Common adverse events leading to withdrawal included nausea, headaches and rashes |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aControl group risk estimates come from control arm of meta‐analysis, based on included trials. bDowngraded one level due to sparse data (294 events). cDowngraded one level due to sparse data (190 events). dDowngraded two levels due to very sparse data (5 events). eDowngraded one level due to sparse data (54 events).
Summary of findings 3. Once daily dosing versus conventional dosing for induction of remission in ulcerative colitis.
| Once‐daily dosing versus conventional dosing for induction of remission in ulcerative colitis | ||||||
| Patient or population: People with active mild‐to‐moderate ulcerative colitis Settings: Outpatient Intervention: Once‐daily dosing | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventional dosing | Once daily dosing | |||||
|
Failure to induce global or clinical remission Follow‐up: 8 weeks |
611 per 1000a | 605 per 1000 (569 to 648) | RR 0.99 (0.93 to 1.06) | 1761 (5 studies) | ⊕⊕⊕⊕ HIGH | Global or clinical remission was defined as UC‐DAI score of ≤ 1 |
|
Failure to induce global or clinical improvement Follow‐up: 8 weeks |
367 per 1000a | 272 per 1000 (180 to 404) | RR 0.74 (0.49 to 1.10) | 564 (3 studies) | ⊕⊕⊕⊝ MODERATEb | Clinical improvement was defined as decrease of ≤ 3 points from baseline in the total modified UC‐DAI score |
| Failure to induce endoscopic remission | 892 per 1000a | 910 per 1000 (180 to 404) | RR 1.02 (0.98 to 1.07) | 817 (1 study) | ⊕⊕⊕⊕ HIGH | Endoscopic remission was defined as Mayo Clinic Endoscopic Subscale subscore of 0 |
|
Failure to adhere to medication regimen Follow‐up: 8 weeks |
61 per 1000a | 84 per 1000 (39 to 176) | RR 1.36 (0.64 to 2.86) | 358 (2 studies) | ⊕⊕⊝⊝ LOWc | Adherence to medication regimen was defined as compliance with taking medications |
|
Adverse events Follow‐up: 8 weeks |
318 per 1000a | 324 per 1000 (283 to 375) | RR 1.02 (0.89 to 1.18) | 1586 (4 studies) | ⊕⊕⊕⊝ MODERATEd | Adverse events included flatulence, abdominal pain, nausea, diarrhea, nasopharyngitis, dyspepsia, headache and worsening of ulcerative colitis |
|
Serious adverse events Follow‐up: 8 weeks |
18 per 1000a |
24 per 1000 (12 to 47) |
RR 1.34 (0.68 to 2.66) |
1586 (4 studies) |
⊕⊕⊝⊝ LOWe | Serious adverse events included pancreatitis, hepatitis, polyuria, chromaturia, upper respiratory tract infection and measles |
|
Withdrawal due to adverse events Follow‐up: 8 weeks |
33 per 1000a | 29 per 1000 (18 to 49) | RR 0.89 (0.54 to 1.49) | 1757 (5 studies) | ⊕⊕⊝⊝ LOWf | Common adverse events leading to withdrawal were not reported |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: risk ratio; UC: ulcerative colitis; UC‐DAI: ulcerative colitis ‐ disease activity index | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aControl group risk estimates come from control arm of meta‐analysis, based on included trials. bDowngraded one level due to sparse data (153 events). cDowngraded two levels due to very sparse data (26 events). dDowngraded one level due to sparse data (271 events). eDowngraded two levels due to very sparse data (33 events). fDowngraded two levels due to very sparse data (9 events).
Summary of findings 4. Oral 5‐ASA versus comparator 5‐ASA for induction of remission in ulcerative colitis.
| Oral 5‐ASA versus comparator 5‐ASA for induction of remission in ulcerative colitis | ||||||
| Patient or population: People with active mild‐to‐moderate ulcerative colitis Settings: Outpatient Intervention: Oral 5‐ASA (MMX mesalamine, Ipocol, Balsalazide, Pentasa, Olsalazine and 5‐ASA micropellets) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Comparator 5‐ASA | Oral 5‐ASA | |||||
|
Failure to induce global or clinical remission Follow‐up: 8 ‐ 12 weeks |
519 per 1000a | 488 per 1000 (446 to 529) | RR 0.94 (0.86 to 1.02) | 1968 (11 studies) |
⊕⊕⊕⊝ MODERATEb | Global or clinical remission was defined as CAI ≤ 4 for patient functional assessment ratings or normal bowel movements and absence of rectal bleeding |
|
Failure to induce global or clinical improvement Follow‐up: 8 ‐ 12 weeks |
346 per 1000a | 308 per 1000 (267 to 350) | RR 0.89 (0.77 to 1.01) | 1647 (8 studies) |
⊕⊕⊕⊝ MODERATEc | Clinical improvement was defined as improved CAI by ≤ 3 from baseline |
| Failure to induce endoscopic remission | See comment | Outcome not reported | ||||
| Failure to adhere to medication regimen | See comment | Outcome not reported | ||||
|
Adverse events Follow‐up: 8 ‐ 12 weeks |
457 per 1000a | 461 per 1000 (420 to 511) | RR 1.01 (0.92 to 1.12) | 1576 (9 studies) |
⊕⊕⊕⊝ MODERATEd | Adverse events included headache, abdominal pain, nausea, flatulence, diarrhea, nasopharyngitis, dyspepsia and vomiting |
|
Serious adverse events Follow‐up: 8 ‐ 12 weeks |
30 per 1,000a |
18 per 1000 (7 to 47) |
RR 0.59 (0.22 to 1.56) |
677 (4 studies) |
⊕⊕⊝⊝ LOWe | Serious adverse events included aggravation of UC and a colonic polyp |
|
Withdrawal due to adverse events Follow‐up: 8 ‐ 12 weeks |
39 per 1000a | 37 per 1000 (22 to 60) | RR 0.94 (0.57 to 1.54) | 1489 (9 studies) |
⊕⊕⊕⊝ MODERATEf | Common adverse events leading to withdrawal include abdominal pain, rashes and cephalea |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAI: clinical activity index; CI: Confidence interval; RR: risk ratio; UC: ulcerative colitis | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aControl group risk estimates come from control arm of meta‐analysis, based on included trials. bDowngraded one level due to high risk of bias in two studies in the pooled analysis (both due to lack of blinding). cDowngraded one level due to high risk of bias in one study in the pooled analysis (lack of blinding). d Downgraded one level due to high risk of bias in one study in the pooled analysis (lack of blinding). eDowngraded two levels due to very sparse data (12 events). fDowngraded one level due to sparse data (57 events).
Background
Description of the condition
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by the inflammation of the colon. The pathogenesis of UC is still unknown, but there are genetic and environmental factors that have been correlated with the increased risk. Common symptoms for UC include abdominal pain, diarrhea, rectal pain, rectal bleeding, weight loss, fatigue and fever (Conrad 2014; Feuerstein 2014). Approximately 6% to 47% of patients experience extra‐intestinal manifestations affecting the eyes, joints, liver and skin. Some of these extra‐intestinal manifestations include arthritis, uveitis, oral ulcers, and primary sclerosing cholangitis (Rothfuss 2006). UC is more common in the industrialized world, especially in North America and Western Europe. The overall worldwide incidence is 1.2 to 20.3 cases per 100,000 persons a year, with a prevalence of 7.6 to 245 cases per 100,000 a year (Danese 2011; Loftus 2004). In North America, the prevalence of UC ranges from 120 to 250 cases per 100,000 people and the incidence ranges from 8 to 20 cases per 100,000 people (Loftus 2004).
UC occurs equally in both men and women and the diagnosis of UC may occur at any age; the disease has two peaks in incidence, at 15 to 30 years and at 50 to 70 years (Ordás 2012; Ponder 2013).
Treatments for UC are based on the severity of the symptoms and may include biological therapies (Adalimumab, Infliximab, Vedolizumab, Golimumab, Ustekinumab), corticosteroids, azathioprine or 6‐mercaptopurine and 5‐aminosalicylates (5‐ASAs). For people with mild‐to‐moderate UC, 5‐ASAs and corticosteroids are the conventional treatment for induction of remission. This is followed by thiopurines, anti‐TNFs or adhesion molecule inhibitors for moderate‐to‐severe UC (Feuerstein 2014).
Description of the intervention
The successful management of UC was greatly facilitated after the introduction of sulfasalazine (SASP) by Svartz (Svartz 1942). SASP is composed of 5‐ASA linked to sulfapyridine by a diazo bond. This bond is readily cleaved by bacterial azoreductases in the colon (Peppercorn 1972), to yield the two components. Of these, 5‐ASA has been found to be the therapeutically active component, while sulfapyridine, which is primarily absorbed into systemic circulation, is assumed to function solely as a carrier molecule (Azad Khan 1977; Klotz 1980; Van Hees 1980).
How the intervention might work
Administration of unbound or uncoated 5‐ASA revealed that it was readily absorbed in the upper jejunum and was unable to reach the colon in therapeutic concentrations (Myers 1987; Nielsen 1983; Schroeder 1972). Ingested SASP largely resists such premature absorption and thus is able to serve as a delivery system that transports the 5‐ASA to the affected regions of the lower intestinal tract (Schroeder 1972). While corticosteroid therapy is more effective for the treatment of severe UC (Truelove 1955; Truelove 1959) the use of SASP in maintaining remission has been well established (Misiewitz 1965; Sutherland 2006a).
Despite its benefits, up to 30% of patients receiving SASP have reported adverse events (AEs) (Nielsen 1982). It was concluded that many were due to the sulfapyridine moiety, especially those effects found to be dose‐dependent (Das 1973; Myers 1987). This discovery spawned more than a decade of research aimed at finding alternative 5‐ASA delivery systems.
Asacol® (Proctor and Gamble) consists of a pellet of 5‐ASA destined for release in the terminal ileum or colon due to a coating known as Eudragit‐S, a resin that dissolves at a pH greater than 7 (Dew 1982). Claversal®/Mesasal® (Smith, Kline and French), Salofalk® (Axcan Pharma, Falk Foundation), and Rowasa® (Reid‐Rowell) are similar delayed‐release preparations of 5‐ASA pellets coated with Eudragit L, a resin that dissolves at a pH greater than 6 (the approximate pH of the ileum/colon) (Hardy 1987; Myers 1987). Pentasa® (Marion‐Merrell‐Dow) is a microsphere formulation that consists of 5‐ASA microgranules enclosed within a semi‐permeable membrane of ethylcellulose. It is designed for controlled release that begins in the duodenum and continues into the affected regions of the lower bowel (Rasmussen 1982). Olsalazine/Dipentum® (Pharmacia & Upjohn) consists of two 5‐ASA molecules linked by a diazo bond (Staerk Laursen 1990; Willoughby 1982). Other formulations, such as benzalazine, Balsalazide/Colazide® (Astra Zeneca), and Balsalazide disodium/Colazal® (Salix Pharmaceuticals) are composed of 5‐ASA molecules azo‐bonded to various benzoic acid derivatives (Chan 1983; Fleig 1988). Like SASP, these compounds are poorly absorbed in the upper digestive tract
but are readily metabolized by the intestinal flora in the lower bowel. MMX mesalamine (Lialdaa® or Mezavant®) uses MMX Multi Matrix System (MMX) technology to delay and extend delivery of active drug throughout the colon (Kamm 2007; Lichtenstein 2007). The newer 5‐ASA preparations were intended to avoid the adverse effects of SASP while maintaining its therapeutic benefits; however, they are more expensive and have also been shown to cause adverse effects in some people (Rao 1987). The efficacy and safety of 5‐ASA preparations have been evaluated in numerous clinical trials that have often lacked sufficient statistical power to arrive at definitive conclusions.
Many patients are non‐adherent to conventional multi‐dose treatment regimens (two or three times daily), which may result in reduced efficacy and can lead to an increased risk of relapse in patients with quiescent disease (Kane 2001; Kane 2003a), a poorer long‐term prognosis (Kane 2008; Kruis 2009) and increased healthcare costs (Beaulieu 2009; Kane 2008). Poor adherence may be particularly problematic in quiescent disease (Kane 2001; Kane 2003a), since patients lack continuing symptoms that incentivize them to take medication. Although multiple factors have been shown to influence medication adherence in people with UC, it is commonly believed that a high pill burden and multi‐dose regimens are major determinants (Ediger 2007; Kane 2008). Other factors affecting adherence in people with UC include disease extent and duration, medication costs, fear of side effects, individual psychosocial characteristics and the patient‐physician relationship (Kane 2008). Mesalamine formulations that involve once‐daily dosing may improve adherence and outcomes.
Previous systematic reviews (Feagan 2012; Sutherland 1993; Sutherland 1997; Sutherland 2006b) found that oral 5‐ASA, in doses of at least 2 g/day, was more effective than placebo, but no more effective than SASP for induction of remission in UC. We proceeded with this updated review in order to include more recent studies as well as to evaluate the efficacy, dose‐responsiveness (including dose‐ranging studies of various 5‐ASA formulations), and safety of oral 5‐ASA preparations compared to placebo or SASP. We also aimed to investigate any differences in efficacy and safety between various formulations of oral 5‐ASA.
Why it is important to do this review
We conducted this review to assess the evidence supporting the use of oral 5‐ASA for the treatment of UC. A secondary objective of this systematic review was to investigate the efficacy and safety of once‐daily dosing of mesalamine compared to conventional dosing for the treatment of active UC. This systematic review is an update of a previously‐published Cochrane Review (Feagan 2012; Sutherland 1993; Sutherland 1997; Sutherland 2006b; Wang 2016).
Objectives
To assess the efficacy, dose‐responsiveness, and safety of oral 5‐aminosalicylic acid (5‐ASA) compared to placebo, sulfasalazine (SASP), or 5‐ASA comparators (i.e. other formulations of 5‐ASA) for induction of remission in active UC. A secondary objective was to compare the efficacy and safety of once‐daily dosing of oral 5‐ASA with conventional dosing regimens (two or three times daily) .
Methods
Criteria for considering studies for this review
Types of studies
We considered prospective, randomized controlled clinical trials of parallel design for inclusion, with a minimum treatment duration of four weeks.
Types of participants
Adult participants (aged 18 years or more) with active mild‐to‐moderate UC as defined by Truelove 1955.
Types of interventions
Studies of oral 5‐ASA therapy for treatment of participants with active UC compared with placebo, SASP or other formulations of 5‐ASA. We also considered studies that compared once‐daily 5‐ASA treatment with conventional dosing of 5‐ASA (two or three times daily), and 5‐ASA dose‐ranging studies for inclusion.
Types of outcome measures
Outcome measures included endoscopic, global or clinical measures of improvement or complete remission, as defined by the authors of each study.
Primary outcomes
The primary outcome was the proportion of participants who failed to enter complete global or clinical remission, as defined by the authors of each study and expressed as a percentage of total participants randomized (intention‐to‐treat (ITT) analysis).
Secondary outcomes
Secondary outcomes included:
proportion of participants who failed to improve clinically;
proportion of participants who failed to enter endoscopic remission;
proportion of participants who failed to improve endoscopically;
proportion of participants who failed to adhere to their medication regimen;
proportion of participants who experienced at least one adverse event (AE);
proportion of participants who experienced at least one serious adverse event (SAE);
proportion of participants who withdrew due to AEs; and
proportion of participants excluded or withdrawn after entry.
Search methods for identification of studies
Electronic searches
We searched the following databases from inception to 11 June 2019:
The Cochrane IBD group Specialized Register;
MEDLINE (Ovid);
Embase (Ovid):
The Cochrane Library; and
Clinicaltrials.gov.
We applied no language or document type restrictions. The search strategies are listed in Appendix 1.
Searching other resources
We also searched review articles and conference proceedings to identify additional studies.
Data collection and analysis
Selection of studies
Two review authors (AM and TN) independently selected relevant studies for analysis on the basis of the inclusion criteria described above. When necessary, we contacted the original investigators to clarify points about trial methodology. Disagreement between review authors were discussed and agreement was reached by consensus.
Data extraction and management
Two review authors (AM and TN) independently extracted data using a standard data extraction form. We recorded results on an ITT basis, regardless of whether or not the original authors had done so. We settled any discrepancies between review authors by consensus. We extracted the following data:
Baseline characteristics of the participants (age, sex, disease severity, disease duration)
Intervention type (dose, mode of administration)
Control type (placebo, no control, other intervention)
Prespecified primary and secondary outcomes
Assessment of risk of bias in included studies
Two review authors (AM and TN) independently assessed the risks of bias in the included studies using the Cochrane 'Risk of bias' tool (Higgins 2011). Factors assessed included:
Random sequence generation;
Allocation concealment;
Blinding;
Incomplete outcome data;
Selective outcome reporting; and
Other potential sources of bias.
Based on these criteria, studies were judged to have a low, high or unclear risk of bias for each category. Disagreements resolved by consensus. We contacted study authors when insufficient information was provided to determine risks of bias.
Measures of treatment effect
For dichotomous outcomes, we calculated the risk ratio (RR) and corresponding 95% confidence interval (95% CI). We pooled the results for each comparison group to determine the RR and 95% CI for each outcome resulting from 5‐ASA therapy relative to either placebo, SASP or 5‐ASA comparator, and for once‐daily 5‐ASA therapy relative to conventional dosing. We used a fixed‐effect model. We pooled studies for analysis if participants, outcomes and interventions were similar (determined by consensus among review authors). We pooled studies comparing 5‐ASA formulations for analysis if they compared equimolar doses of oral 5‐ASA.
Unit of analysis issues
In trials consisting of multiple arms (i.e. different dose groups), we divided the placebo group across treatment groups. For trials with an odd number of participants, we divided the groups to ensure the group for the lower dose had the larger number of participants, to avoid overestimating the effects of the higher‐dose arm. For recurring events such as AEs and SAEs, we used the primary endpoint defined by the study. Lastly, we assessed the fixed intervals for follow‐up for outcomes that are measured at different time points.
Dealing with missing data
We analyzed missing dichotomous outcomes according to the ITT principle. Participants with missing data were assumed to be treatment failures. For continuous outcomes we used the number of participants who completed the trial and did not impute any missing variables.
Assessment of heterogeneity
We assessed the presence of heterogeneity among studies using the Chi2 test (with a P value of 0.10 regarded as statistically significant) and the I2 statistic (Higgins 2003). If we found statistically significant heterogeneity, we calculated the RR and 95% CI using a random‐effects model. We did not pool data for meta‐analysis if we identified a high degree of heterogeneity (e.g. I2 > 75%).
Assessment of reporting biases
We compared the outcomes listed in the protocol to the outcomes listed in the final study report. However, if we could not located the protocol we compared the outcomes listed in the Methods section to the outcomes in the Results section. If there were a sufficient number of studies included ( i.e. 10 or more ) in the pooled analyses, we planned to use a funnel plot to investigate a potential publication bias.
Data synthesis
We separated the trials into five comparison groups: 5‐ASA versus placebo; 5‐ASA versus sulfasalazine; once‐daily dosing versus conventional dosing; 5‐ASA versus comparator 5‐ASA; and 5‐ASA dose‐ranging. We pooled data from studies where the intervention, participant groups and outcomes were similar. The RR and 95% CI were pooled for dichotomous outcomes and the MD and corresponding 95% CI were pooled for continuous outcomes. We used the standardized mean difference (SMD) and a 95% CI when different scales were used to measure the same outcome (e.g. different quality‐of‐life instruments).
Subgroup analysis and investigation of heterogeneity
We subgrouped once‐daily versus conventional‐dosing studies by formulation. We subgrouped the tables for 5‐ASA‐controlled trials by common 5‐ASA comparators (e.g. Asacol, Claversal, Salofalk and Pentasa). We subgrouped the tables for dose‐ranging studies by 5‐ASA formulation. Trials were also subgrouped according to the specific 5‐ASA preparation for those outcomes for which there were two or more studies that used a similar drug.
Sensitivity analysis
We conducted sensitivity analyses as appropriate, to investigate heterogeneity. We also conducted sensitivity analyses excluding studies with a high risk of bias. We conducted all statistical analyses using Cochrane Review Manager 5 software.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach for rating the overall certainty of evidence for the primary outcomes and selected secondary outcomes of interest. Randomized trials start as high‐certainty evidence, but may be downgraded due to: (1) limitations in design and implementation (risk of bias), (2) indirectness of evidence, (3) inconsistency (unexplained heterogeneity), (4) imprecision (sparse data), and (5) reporting bias (publication bias). The overall certainty of evidence for each outcome is determined after considering each of these elements, and categorized as high certainty (i.e. further research is very unlikely to change our confidence in the estimate of effect); moderate certainty (i.e. further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate); low certainty (i.e. further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate); and very low certainty (i.e. we are very uncertain about the estimate) (Guyatt 2008; Schünemann 2019).
Results
Description of studies
Results of the search
A literature search conducted on 11 June 2019 identified 3331 studies. We found 32 additional studies through searching of references. After duplicates were removed, 2300 reports remained for review of titles and abstracts. Two review authors (AM and TMN) independently reviewed the titles and abstracts of these studies and selected 115 reports of oral 5‐ASA for treatment of active UC for full‐text review (See Figure 1). We excluded 22 reports of 21 of these studies (see Characteristics of excluded studies), leaving 92 reports of 54 included studies (Andreoli 1987; Bresci 1990; Cai 2001; D'Haens 2006; D'Haens 2017; Ewe 1988; Farup 2001; Feagan 2013; Feurle 1989;Fleig 1988; Flourié 2013; Forbes 2005; Gibson 2006; Good 1992; Green 1998;Green 2002; Hanauer 1993; Hanauer 1996; Hanauer 2005; Hanauer 2007; Hetzel 1986; Hiwatashi 2011; Ito 2010; Jiang 2004; Kamm 2007; Kruis 1998; Kruis 2003; Kruis 2009; Levine 2002; Lichtenstein 2007; Maier 1985; Mansfield 2002; Marakhouski 2005; Miglioli 1990; Mihas 1988; Munakata 1995; Pontes 2014; Pruitt 2002; Qian 2004; Rachmilewitz 1989; Raedler 2004; Rao 1989; Rijk 1991; Riley 1988; Robinson 1994; Sandborn 2009; Sandborn 2012; Scherl 2009; Schroeder 1987; Sninsky 1991; Sutherland 1990; Tursi 2004; Willoughby 1988; Zinberg 1990) (See Characteristics of included studies). There was one ongoing study identified from clinicaltrials.gov (NCT02522767).
1.
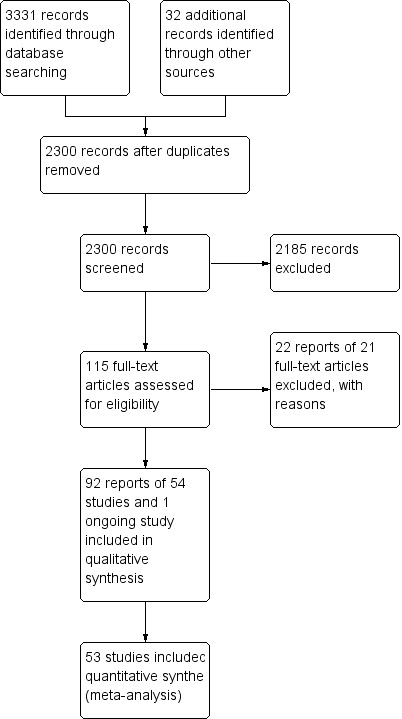
Study flow diagram.
Included studies
Of the 54 included studies, 16 were placebo‐controlled (Feagan 2013; Feurle 1989; Hanauer 1993; Hanauer 1996; Hetzel 1986; Ito 2010; Kamm 2007; Lichtenstein 2007; Pontes 2014; Robinson 1994; Sandborn 2012; Scherl 2009; Schroeder 1987; Sninsky 1991;Sutherland 1990; Zinberg 1990). Eighteen studies compared 5‐ASA to SASP (Andreoli 1987; Bresci 1990; Cai 2001; Ewe 1988; Fleig 1988; Good 1992; Green 2002; Jiang 2004; Maier 1985; Mansfield 2002; Mihas 1988; Munakata 1995; Qian 2004; Rachmilewitz 1989; Rao 1989; Rijk 1991;Riley 1988; Willoughby 1988). Five studies compared once‐daily dosing of mesalamine with conventional dosing (D'Haens 2017; Flourié 2013; Kamm 2007; Kruis 2009; Lichtenstein 2007). Twelve trials compared the efficacy and safety of various formulations of oral 5‐ASA (e.g. MMX mesalamine, Ipocol, Balsalazide, Pentasa, Olsalazine and 5‐ASA micropellets) to other formulations of oral 5‐ASA (e.g. Asacol, Claversal, Salofalk, Pentasa) (Farup 2001; Forbes 2005; Gibson 2006; Green 1998; Ito 2010; Kamm 2007; Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002; Raedler 2004; Tursi 2004). Eleven trials were dose‐ranging studies of oral 5‐ASA (D'Haens 2006; Hanauer 2007; Hanauer 2005; Hiwatashi 2011; Ito 2010; Kamm 2007; Kruis 2003; Miglioli 1990; Sandborn 2009; Schroeder 1987; Sninsky 1991).
Excluded studies
Twenty‐two reports of 21 of these studies were excluded (See Characteristics of excluded studies). Four studies were excluded because they were not classified as RCTs (Ahluwalia 1992; Irvine 2008; Kamm 2009; Pruitt 1991), seven studies were excluded because they did not have a control group (Behrens 2013; Dignass 2018; Paoluzi 2002; Rubin 2017; Vernia 2000; Ye 2018; Yoshimura 2018), two studies because they had an ineligible comparator group (Adrizzone 2006; Gross 2011), four studies because they did not include an oral 5‐ASA formulation (Levine 2017; Mahmood 2005; Safdi 1997; Vecchi 2001), two studies were not induction studies (Park 2018; Suzuki 2017), one study was a pediatric study (Turner 2017) and one study because the study drug included a combination of 5‐ASA and sodium hyaluronate (Fiorino 2019).
Risk of bias in included studies
We provide a summary of the 'Risk of bias' assessment in Figure 2. Most of the included studies were of high methodological quality. We rated five studies at high risk of bias due to incomplete outcome data and lack of blinding. Thirty‐two of 54 included studies did not describe the method used for randomization and we rated them as unclear for this domain. Twenty‐six studies did not describe methods used for allocation concealment and we rated them as unclear for this domain. The methods used for blinding were not described in five studies, and these studies were rated as unclear. We judged 20 studies to be at unclear risk for incomplete outcome data because reasons for withdrawal were either not described or were not attributed to intervention groups. We rated six studies as unclear for selective reporting.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
1. 5‐ASA versus placebo
Failure to induce complete global or clinical remission
Eleven studies (2387 participants) reported treatment outcomes as failure to induce complete global or clinical remission (Feagan 2013; Hanauer 1993; Hanauer 1996; Ito 2010; Kamm 2007; Lichtenstein 2007; Pontes 2014; Sandborn 2012; Schroeder 1987; Sninsky 1991; Scherl 2009). Seventy‐one per cent (1107/1550) of 5‐ASA participants failed to enter remission compared to 83% (695/837) of placebo participants (risk ratio (RR) 0.86, 95% confidence interval (CI) 0.82 to 0.89; I2 = 25%; high‐certainty evidence; Analysis 1.1) . There was a trend towards greater efficacy with higher doses of 5‐ASA for the 2 to 2.9 g/day (RR 0.88, 95% CI 0.82 to 0.94; I2 = 27%; 956 participants, 8 studies) and the > 3 g/day subgroups (RR 0.83, 95% CI 0.77 to 0.88; I2 = 25%; 1200 participants, 8 studies). The five trials that involved Asacol (Feagan 2013; Ito 2010; Kamm 2007; Schroeder 1987; Sninsky 1991) had a pooled RR of 0.84 (95% CI 0.79 to 0.90). Two trials using MMX mesalazine (Kamm 2007; Lichtenstein 2007) had a pooled RR of 0.81 (95% CI 0.73 to 0.89).
1.1. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 1: Failure to induce global/clinical remission
Failure to induce global or clinical improvement
Fourteen studies (Feagan 2013; Feurle 1989; Hanauer 1993; Hetzel 1986; Ito 2010; Kamm 2007; Lichtenstein 2007; Pontes 2014; Schroeder 1987; Robinson 1994; Sutherland 1990; Scherl 2009; Sninsky 1991; Zinberg 1990) (2256 participants) provided data on the failure to induce global or clinical improvement (including remission). Forty‐one per cent (605/1459) of 5‐ASA participants failed to improve clinically compared to 65% (519/797) of placebo participants (RR 0.68, 95% CI 0.61 to 0.75, I2 = 47%; moderate‐certainty evidence; Analysis 1.2).There was a trend towards greater efficacy with higher doses of 5‐ASA for all dosage subgroups: < 2 g/day (RR 0.79, 95% CI 0.64 to 0.97; I2 = 0%); 2 to 2.9 g/day (RR 0.77, 95% CI 0.67 to 0.88; I2 = 32%); > 3 g/day (RR 0.57, 95% CI 0.51 to 0.65; I2 = 5%). Five trials involving Asacol (Feagan 2013; Ito 2010; Kamm 2007; Schroeder 1987; Sninsky 1991) had a pooled RR of 0.68 (95% CI 0.58 to 0.80). Four studies involved Olsalazine (Feurle 1989; Hetzel 1986; Robinson 1994; Zinberg 1990), and resulted in a pooled RR of 0.80 (95% CI 0.65 to 0.97). Two trials using MMX mesalazine (Kamm 2007; Lichtenstein 2007) had a pooled RR of 0.64 (95% CI 0.55 to 0.75).
1.2. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 2: Failure to induce global/clinical improvement (including remission)
Failure to induce endoscopic remission
Four studies (Hanauer 1993; Hanauer 1996; Kamm 2007; Scherl 2009) (1154 participants) reported on failure to induce complete endoscopic remission. Fifty per cent (399/805) of 5‐ASA participants failed to enter endoscopic remission compared to 64% (223/349) of placebo participants (RR 0.77, 95% CI 0.67 to 0.89; I2 = 42%; moderate‐certainty evidence; Analysis 1.3). The doses of 3 g or more were shown to be more effective compared to the other doses (RR 0.70, 95% CI 0.56 to 0.87; I2 = 51%).
1.3. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 3: Failure to induce endoscopic remission
Failure to induce endoscopic improvement
Four studies (Hanauer 1996; Hetzel 1986; Robinson 1994; Zinberg 1990) (416 participants), all involving Olsalazine, reported failure to induce endoscopic remission or improvement. Forty‐four per cent (113/255) of 5‐ASA participants failed to improve endoscopically compared to 63% (102/161) of placebo participants (RR 0.71, 95% CI 0.59 to 0.86; I2 = 43%; low‐certainty evidence; Analysis 1.4).
1.4. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 4: Failure to induce endoscopic improvement (including remission)
Adverse events
Eight studies (1218 participants) reported the proportion of participants who experienced at least one AE (Feurle 1989; Feagan 2013; Hetzel 1986; Ito 2010; Lichtenstein 2007; Pontes 2014; Schroeder 1987; Scherl 2009). There was no difference in the incidence of AEs between 5‐ASA and placebo participants. Fifty‐two per cent (386/749) of 5‐ASA participants experienced at least one AE compared to 49% (228/469) of placebo participants (RR 0.95, 95% CI 0.85 to 1.07; I2 = 0%; high‐certainty evidence; Analysis 1.5). Three trials that involved Asacol (Feagan 2013; Ito 2010; Schroeder 1987) had a pooled RR of 1.03 (95% CI 0.87 to 1.21). Two studies that involved Olsalazine (Hetzel 1986; Feurle 1989) had a pooled RR of 1.09 (95% CI 0.55 to 2.15). Commonly‐reported AEs included: headache, nausea, abdominal pain or cramps, nasopharyngitis or symptoms of upper respiratory infection, rash. anorexia or loss of appetite, flatulence or gas, gastrointestinal disorders and fever. Diarrhea was reported in four studies involving Olsalazine (Feurle 1989; Hanauer 1996; Robinson 1994; Zinberg 1990) and one study of Pentasa (Hanauer 1993).
1.5. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 5: Adverse events
Serious adverse events
Four studies (546 participants) reported on the proportion of participants who experienced at least one SAE (Feagan 2013; Ito 2010; Lichtenstein 2007; Pontes 2014). Two per cent (7/466) of participants in the 5‐ASA group experienced an SAE compared to 2% (6/280) of placebo participants (RR 0.53, 95% CI 0.18 to 1.56,I2 = 0%; low‐certainty evidence; Analysis 1.6). SAEs reported include aggravation of UC, malaise, abdominal abscess, pancreatitis and an inguinal hernia.
1.6. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 6: Serious adverse events
Withdrawals due to adverse events
Thirteen studies (2372 participants) reported the proportion of participants withdrawn due to AEs (Feagan 2013; Feurle 1989; Hanauer 1993; Hanauer 1996; Hetzel 1986; Ito 2010; Kamm 2007; Lichtenstein 2007; Robinson 1994; Schroeder 1987; Scherl 2009; Sninsky 1991; Zinberg 1990). Withdrawals due to AEs were reported for 6% (91/1542) of 5‐ASA participants compared to 9% (73/830) of placebo participants (RR 0.72, 95% CI 0.54 to 0.97; I2 = 13%; moderate‐certainty evidence; Analysis 1.7). The pooled analysis of five Asacol trials (Feagan 2013; Ito 2010; Kamm 2007; Schroeder 1987; Sninsky 1991) showed a higher proportion of placebo participants (9.7%) were withdrawn due to AEs compared to Asacol participants (3.5%) (RR 0.50, 95% CI 0.30 to 0.84). However, when five Olsalazine studies (Feurle 1989; Hanauer 1996; Hetzel 1986; Robinson 1994; Zinberg 1990) were pooled a higher proportion of Olsalazine participants (8.8%) were withdrawn due to AEs compared to placebo (3.3%) (RR 2.58, 95% CI 1.16 to 5.70). When two MMX mesalamine studies were pooled (Kamm 2007; Lichtenstein 2007) a higher proportion of placebo participants (7.3%) were withdrawn due to AEs compared to MMX mesalamine (2.2%) (RR 0.31, 95% CI 0.14 to 0.72). An inspection of the forest plot showed the difference in withdrawals favoring 5‐ASA over placebo was driven by the large Feagan 2013 study, which reported that worsening of UC was the most common AE leading to withdrawal. Worsening of UC leading to withdrawal was reported for 10 of 12 withdrawals in the 5‐ASA group compared to all 30 withdrawals in the placebo group (Feagan 2013). A sensitivity analysis excluding Feagan 2013 showed no difference in withdrawals due to AEs between 5‐ASA and placebo. Withdrawals due to AEs occurred in 6% (79/1402) of 5‐ASA participants compared to 6% (43/689) of placebo participants (RR 0.88, 95% CI 0.62 to 1.24; I2 = 5%). The common AEs leading to withdrawal were not reported.
1.7. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 7: Withdrawals due to adverse events
Exclusions or withdrawals after study entry
Fifteen studies (2529 participants) reported the proportion of participants excluded or withdrawn after entry (Feagan 2013; Feurle 1989; Hanauer 1993; Hanauer 1996; Hetzel 1986; Ito 2010; Kamm 2007; Lichtenstein 2007; Pontes 2014; Scherl 2009; Schroeder 1987; Sutherland 1990; Robinson 1994; Sninsky 1991; Zinberg 1990). Twenty‐four per cent (388/1642) of 5‐ASA participants were withdrawn or excluded after entry compared to 37% (332/887) of placebo participants (R 0.61, 95% CI 0.51 to 0.72; I2 = 37%; See Analysis 1.8).
1.8. Analysis.

Comparison 1: 5‐ASA versus placebo, Outcome 8: Exclusions and withdrawals after study entry
2. 5‐ASA versus sulfasalazine
Failure to induce complete global or clinical remission
The failure to induce complete global or clinical remission was reported in eight studies (526 participants) (Andreoli 1987; Green 2002; Jiang 2004; Mansfield 2002; Maier 1985; Rachmilewitz 1989; Riley 1988; Riley 1988). Fifty‐four per cent (150/279) of 5‐ASA participants failed to enter remission compared to 58% (144/247) of SASP participants (RR 0.90, 95% CI 0.77 to 1.04; I2 = 0%; moderate‐certainty evidence; Analysis 2.1). Two studies involving Claversal (Andreoli 1987; Rachmilewitz 1989) had a pooled RR of 1.00 (95% CI 0.83 to 1.21). Two studies involving Balsalazide (Green 2002; Mansfield 2002) had a pooled RR of 0.93 (95% CI 0.57 to 1.51). Two studies involving Olsalazine (Jiang 2004; Rijk 1991) had a pooled 0.66 (95% CI 0.43 to 1.02).
2.1. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 1: Failure to induce global/clinical remission
Failure to induce global or clinical improvement
Fourteen studies (Bresci 1990; Cai 2001; Ewe 1988; Fleig 1988; Good 1992; Maier 1985; Mihas 1988; Munakata 1995; Jiang 2004; Rao 1989; Rachmilewitz 1989; Riley 1988; Qian 2004; Willoughby 1988) (1053 participants) reported failure to induce global or clinical improvement (including remission). Thirty‐seven per cent (227/608) of 5‐ASA participants failed to improve compared to 47% (208/445) of SASP participants (RR 0.88, 95% CI 0.76 to 1.01; I2 = 0%; high‐certainty evidence; Analysis 2.2). Six Olsalazine trials (Cai 2001; Ewe 1988; Jiang 2004; Qian 2004; Rao 1989; Willoughby 1988) had a pooled RR of 0.76 (95% CI 0.57 to 1.00).
2.2. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 2: Failure to induce global/clinical improvement (including remission)
Failure to induce endoscopic remission
Since only two studies (Jiang 2004; Rachmilewitz 1989) reported failure to induce complete endoscopic remission, we did not conduct a meta‐analysis for this outcome. We did not pool the studies, as they used different indices to measure endoscopic remission. Neither study showed significant differences in complete endoscopic remission between 5‐ASA and SASP.
Failure to induce endoscopic improvement
Six studies (Fleig 1988; Munakata 1995; Rao 1989; Rijk 1991; Riley 1988; Willoughby 1988) (362 participants) provided data on failure to induce endoscopic improvement (including remission). Forty‐one per cent (78/189) of 5‐ASA participants failed to improve endoscopically compared to 45% (78/173) of SASP participants: RR 0.82, 95% CI 0.65 to 1.02; I2 = 0%; moderate‐certainty evidence; Analysis 2.3). Three trials involving Olsalazine (Rao 1989; Rijk 1991; Willoughby 1988) had a pooled RR of 0.93 (95% CI 0.62 to 1.39).
2.3. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 3: Failure to induce endoscopic improvement (including remission)
Failure to adhere to medication regimen
No studies reported this outcome.
Adverse events
Twelve studies (909 participants) reported the proportion of participants who experienced at last one AE (Bresci 1990; Cai 2001; Ewe 1988; Fleig 1988; Green 2002; Mansfield 2002; Mihas 1988; Munakata 1995; Qian 2004; Rachmilewitz 1989; Rao 1989; Rijk 1991). It should be noted that, with two exceptions (Mihas 1988; Rao 1989), the inclusion criteria for entry included tolerance of SASP. Nevertheless, SASP participants were significantly more likely than 5‐ASA participants to experience an AE. Fourteen per cent (72/498) of 5‐ASA participants experienced at least one AE compared to 29% (118/411) of SASP participants (RR 0.48, 95% CI 0.36 to 0.63; I2 = 0%; moderate‐certainty evidence; Analysis 2.4). Five Olsalazine trials (Cai 2001; Ewe 1988; Rao 1989; Rijk 1991; Qian 2004) had a combined RR of 0.48 (95% CI 0.32 to 0.71), and two Balsalazide trials (Green 2002; Mansfield 2002) had a combined RR of 0.16 (95% CI 0.05 to 0.52).Commonly‐reported AEs included: nausea, headache, dyspepsia, vomiting, abdominal pain and rash. Diarrhea was reported in three studies involving Olsalazine (Ewe 1988; Jiang 2004; Willoughby 1988).
2.4. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 4: Adverse events
Serious adverse events
Two studies (107 participants) reported on the proportion of participants who experienced at least one SAE (Green 2002; Mansfield 2002). There was no difference between the 5‐ASA and SASP groups. Six per cent of participants (3/54) in the 5‐ASA group experienced an SAE compared to 4% (2/53) of SASP participants (RR 1.36, 95% CI 0.28 to 6.52; low‐certainty evidence; Analysis 2.5). SAEs reported include erythematous rash, venous thrombosis, carcinoma, acute pancreatitis, rheumatoid arthritis and erythema nodosum.
2.5. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 5: Serious adverse events
Withdrawals due to adverse events
Ten studies (640 participants) reported the proportion of participants withdrawn due to AEs (Ewe 1988; Fleig 1988; Green 2002; Mansfield 2002; Mihas 1988; Qian 2004; Rachmilewitz 1989; Rao 1989; Riley 1988; Willoughby 1988). SASP resulted in a higher proportion of participants withdrawn due to AEs.Thirteen per cent (39/303) of SASP participants were withdrawn due to AEs compared to 4% (15/337) of 5‐ASA participants (RR 0.40, 95% CI 0.24 to 0.68; I2 = 0%; moderate‐certainty evidence; Analysis 2.6). When four Olsalazine trials were combined (Ewe 1988; Rao 1989; Qian 2004; Willoughby 1988), the RR was 0.63 (95% CI 0.24 to 1.66). The pooling of two Balsalazide trials (Green 2002; Mansfield 2002) had a combined RR of 0.16 (95% CI 0.05 to 0.52).The common AEs leading to withdrawal include nausea, headaches and rashes.
2.6. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 6: Withdrawals due to adverse events
Exclusions or withdrawals after study entry
Ten studies (701 participants) reported the proportion of participants excluded or withdrawn after entry (Andreoli 1987; Fleig 1988; Green 2002; Mansfield 2002; Munakata 1995; Rachmilewitz 1989; Rao 1989; Rijk 1991; Riley 1988; Willoughby 1988).Twenty‐six per cent (86/337) of SASP participants were withdrawn or excluded after entry compared to 19% (70/364) of 5‐ASA participants (RR 0.76, 95% CI 0.58 to 0.99; I2 = 28%; Analysis 2.7).
2.7. Analysis.

Comparison 2: 5‐ASA versus sulfasalazine, Outcome 7: Exclusions and withdrawals after study entry
3. Once‐daily dosing versus conventional dosing
Failure to induce complete global or clinical remission
Five studies (1761 participants) reported treatment outcomes for failure to induce complete global or clinical remission (D'Haens 2017; Flourié 2013; Kamm 2007; Kruis 2009; Lichtenstein 2007). Sixty per cent (533/881) of conventionally‐dosed 5‐ASA participants failed to enter remission compared to 61% (538/880) of participants who were dosed once daily (RR 0.99, 95% CI 0.93 to 1.06; I2 = 0%; high‐certainty evidence; Analysis 3.1). None of the subgroup comparisons by formulation showed any differences in efficacy between once‐daily dosing and conventional dosing. However, only five formulations were evaluated in this pooled analysis.
3.1. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 1: Failure to induce global/clinical remission
Failure to induce global or clinical improvement
Three studies (564 participants) reported treatment outcomes for failure to induce global or clinical improvement including remission (Flourié 2013; Kamm 2007; Lichtenstein 2007). Thirty‐seven per cent (104/283) of conventionally‐dosed 5‐ASA participants failed to improve clinically compared to 28% (79/281) of participants who were dosed once daily (RR 0.74, 95% CI 0.49 to 1.10; I2 = 59%; moderate‐certainty evidence; Analysis 3.2). A visual inspection of the forest plot indicated that Flourié 2013 was the likely source of the heterogeneity. When we performed a sensitivity analysis excluding this study at high risk of bias the I2 value dropped to 0%. Forty‐six per cent (82/179) of conventionally‐dosed 5‐ASA participants failed to improve clinically compared to 40% (71/179) of participants who were dosed once daily (RR 0.87, 95% CI 0.68 to 1.10; I2 = 0%; Analysis 3.3).
3.2. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 2: Failure to induce global/clinical improvement (including remission)
3.3. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 3: Failure to induce global/clinical improvement (sensitivity analysis)
Failure to induce endoscopic remission
One study (D'Haens 2017) (817 participants) reported on the failure to induce endoscopic remission. Eighty‐nine per cent (364/408) of conventionally‐dosed participants failed to induce endoscopic remission compared to 91% (373/409) of once‐daily participants (RR 1.02, 95% CI 0.98 to 1.07; high‐certainty evidence; Analysis 3.4).
3.4. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 4: Failure to induce endoscopic remission
Failure to induce endoscopic improvement
One study (D'Haens 2017) (817 participants) reported on the failure to induce endoscopic response. Fifty‐two percent (212/408) of conventionally‐dosed participants failed to induce endoscopic response compared to 55% (224/409) of participants in the once‐daily group (RR 1.05, 95% CI 0 0.93 to 1.20) (Analysis 3.5).
3.5. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 5: Failure to induce endoscopic improvement (including remission)
Failure to adhere to medication regimen
Two studies (358 participants) provided dichotomous data for failure to adhere to the medication regimen at study endpoint (Kamm 2007; Lichtenstein 2007). Eight per cent (15/179) of once‐daily dosed participants compared to 6% (11/179) of conventionally‐dosed participants failed to adhere to the medication regimen (RR 1.36, 95% CI 0.64 to 2.86; I2 = 34%; low‐certainty evidence; Analysis 3.6). Only one study (Flourié 2013) reported on a continuous outcome for compliance with medication (MD −4.00, 95% CI −17.38 to 9.38; Analysis 3.7).
3.6. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 6: Failure to adhere to medication regimen
3.7. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 7: Compliance
Adverse events
Four studies (1586 participants) reported the proportion of participants who experienced at least one AE (D'Haens 2017; Flourié 2013; Kruis 2009; Lichtenstein 2007). Thirty‐three per cent (259/796) of participants who were dosed once daily experienced at least one AE compared to 32% (251/790) of conventionally‐dosed participants (RR 1.02, 95% CI 0.89 to 1.18; I2 = 37%; moderate‐certainty evidence; Analysis 3.8). Common AEs included flatulence, abdominal pain, nausea, diarrhea, nasopharyngitis, dyspepsia, headache and worsening of UC.
3.8. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 8: Adverse events
Serious adverse events
Four studies (1586 participants) reported on the proportion of participants who experienced at least one SAE (D'Haens 2017; Flourié 2013; Kruis 2009; Lichtenstein 2007).Two per cent (19/796) of participants in the once‐daily group experienced an SAE compared to 2% (14/790) of participants in the conventional‐dosing group (RR 1.34, 95% CI 0.68 to 2.66; low‐certainty evidence; Analysis 3.9). SAEs reported include pancreatitis, hepatitis, polyuria, chromaturia, upper respiratory tract infection and measles.
3.9. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 9: Serious adverse events
Withdrawals due to adverse events
Five studies (1757 participants) reported the proportion of participants withdrawn due to AEs (D'Haens 2017; Flourié 2013; Kamm 2007; Kruis 2009; Lichtenstein 2007).There was no difference in the proportion of participants withdrawn due to AEs between once‐daily and conventionally‐dosed participants. Three per cent (29/876) of conventionally‐dosed participants were withdrawn due to AEs compared to 3% (26/881) of participants dosed once daily (RR 0.89, 95% CI 0.54 to 1.49; I2 = 0%; low‐certainty evidence; Analysis 3.10). The common AEs leading to withdrawal were not reported.
3.10. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 10: Withdrawals due to adverse events
Withdrawals or exclusions after study entry
Four studies (944 participants) reported on the proportion of participants excluded or withdrawn after entry (Flourié 2013; Kamm 2007; Kruis 2009; Lichtenstein 2007). There was no difference in the proportion of participants excluded or withdrawn after entry between once‐daily and conventionally‐dosed participants. Fourteen per cent (67/472) of participants dosed once daily were excluded or withdrawn after entry compared to 14% (66/472) of conventionally‐dosed participants (RR 1.02, 95% CI 0.74 to 1.39; I2 = 0%; Analysis 3.11).
3.11. Analysis.

Comparison 3: Once daily dosing versus conventional dosing, Outcome 11: Exclusions and withdrawals after study entry
4. 5‐ASA versus comparator 5‐ASA
Failure to induce complete global or clinical remission
Eleven studies (1968 participants) reported treatment outcomes for failure to induce complete global or clinical remission (Farup 2001; Forbes 2005; Gibson 2006; Ito 2010; Kamm 2007; Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002; Raedler 2004; Tursi 2004). 5‐ASA formulations included MMX mesalamine, Ipocol, Balsalazide, Pentasa, Olsalazine and 5‐ASA micropellets. Comparator 5‐ASA formulations included Asacol, Claversal, Salofalk, and Pentasa.
We did not include Green 1998 in the pooled analysis because it enrolled participants with moderate‐to‐severe disease, whereas the other studies in the pooled analysis enrolled participants with mild to moderately‐active UC. Green 1998 also allowed the use of rectal steroid foam to relieve active symptoms, which was not allowed in the other 5‐ASA controlled studies. Fifty per cent (507/1022) of participants in the 5‐ASA group failed to enter remission compared to 52% (491/946) of participants in the 5‐ASA comparator group (RR 0.94, 95% CI 0.86 to 1.02; I2 = 0%; moderate‐certainty evidence; Analysis 4.1). However, a sensitivity analysis excluding the two studies at high risk of bias (Farup 2001; Tursi 2004) produced similar results (1681 participants, 9 studies). Forty‐eight per cent (405/842) of participants in the 5‐ASA group failed to enter remission compared to 50% (424/839) of participants in the 5‐ASA comparator group (RR 0.95, 95% CI 0.87 to 1.04; I2 = 0%). Green 1998 compared Balsalazide 6.75 g/day (n = 50) to Asacol 2.4 g/day (n = 49). At eight weeks 22% of participants in the Balsalazide group failed to enter remission compared to 45% of participants in the Asacol group (RR 0.49; 95% CI 0.27 to 0.90).
4.1. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 1: Failure to induce global/clinical remission
Failure to induce global or clinical improvement
Eight studies (1647 participants) reported treatment outcomes for failure to induce global or clinical improvement including remission (Farup 2001; Gibson 2006; Ito 2010; Kamm 2007; Kruis 1998; Levine 2002; Marakhouski 2005; Raedler 2004). Thirty per cent (260/862) of participants in the 5‐ASA group failed to improve clinically compared to 35% (272/785) of participants in the 5‐ASA comparator group (RR 0.89, 95% CI 0.77 to 1.01; I2 = 0%; moderate‐certainty evidence; Analysis 4.3). The various formulations of 5‐ASA included Balsalazide, Pentasa, Olsalazine, MMX mesalazine, and 5‐ASA micropellets; the comparator formulations of 5‐ASA included Asacol, Claversal, Salofalk and Pentasa. However, a sensitivity analysis excluding the study at high risk of bias (Farup 2001) produced similar results (1420 participants, 7 studies). Thirty‐two per cent (226/712) of participants in the 5‐ASA group failed to improve clinically compared to 35% (247/708) of participants in the 5‐ASA comparator group (RR 0.91, 95% CI 0.79 to 1.05; I2 = 0%; Analysis 4.4).
4.3. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 3: Failure to induce global/clinical improvement (including remission)
4.4. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 4: Failure to induce global/clinical improvement (sensitivity analysis)
Failure to induce endoscopic remission
No studies reported this outcome.
Failure to induce endoscopic improvement
No studies reported this outcome.
Failure to adhere to medication regimen
No studies reported this outcome.
Adverse events
Nine studies (1576 participants) reported the proportion of participants who experienced at least one AE (Forbes 2005; Gibson 2006; Ito 2010; Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002; Raedler 2004; Tursi 2004). The pooled risk ratio showed no difference in the incidence of AEs between various formulations of 5‐ASA (including Balsalazide, Pentasa, Olsalazine, Ipocol and 5‐ASA micropellets) and comparator formulations of 5‐ASA (including Asacol, Claversal and Salofalk). Forty‐six per cent (365/792) of participants in the 5‐ASA group experienced at least one AE compared to 46% (358/784) of participants in the 5‐ASA comparator group (RR 1.01, 95% CI 0.92 to 1.12; I2 = 10%; moderate‐certainty evidence; Analysis 4.5). Common AEs included headache, abdominal pain, nausea, flatulence, diarrhea, nasopharyngitis, dyspepsia, vomiting and the worsening of UC.
4.5. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 5: Adverse events
Serious adverse events
Four studies (677 participants) reported on the proportion of participants who experienced at least one SAE (Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002). Two per cent (6/343) of participants experienced an SAE in the 5‐ASA group compared to 3% (10/334) of participants in the comparator 5‐ASA group. There was no difference between the 5‐ASA versus comparator 5‐ASA group (RR 0.59, 95% CI 0.22 to 1.56; low‐certainty evidence; Analysis 4.6). SAEs reported include aggravation of UC and a colonic polyp.
4.6. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 6: Serious adverse events
Withdrawals due to adverse events
Nine studies (1489 participants) reported the proportion of participants withdrawn due to AEs (Forbes 2005; Ito 2010; Kamm 2007; Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002; Raedler 2004; Tursi 2004). The pooled risk ratio showed no difference in withdrawals due to AEs between various formulations of 5‐ASA (including Balsalazide, Pentasa, Olsalazine, MMX mesalazine; Ipocol and 5‐ASA micropellets) and comparator formulations of 5‐ASA (including Asacol, Claversal and Salofalk). Four per cent (28/749) of participants in the 5‐ASA group were withdrawn due to AEs compared to 4% (29/740) of participants in the 5‐ASA comparator group (RR 0.94, 95% CI 0.57 to 1.54; I2 = 15%; moderate‐certainty evidence; Analysis 4.7). The common AEs leading to withdrawal include abdominal pain, rashes and cephalea.
4.7. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 7: Withdrawals due to adverse events
Withdrawals or exclusions following study entry
Ten studies (1574 participants) reported the proportion of participants excluded or withdrawn after entry (Forbes 2005; Gibson 2006; Ito 2010; Kamm 2007; Kruis 1998; Levine 2002; Marakhouski 2005; Pruitt 2002; Raedler 2004; Tursi 2004). The pooled risk ratio showed no difference in exclusions or withdrawals after entry between various formulations of 5‐ASA (including Balsalazide, Pentasa, Olsalazine, MMX mesalazine, Ipocol and 5‐ASA micropellets) and comparator formulations of 5‐ASA (including Asacol, Claversal and Salofalk). Eighteen per cent (144/792) of participants in the 5‐ASA group were excluded or withdrawn after entry compared to 18% (143/782) of participants in the 5‐ASA comparator group (RR 0.99, 95% CI 0.80 to 1.22; I2 = 0%; Analysis 4.8).
4.8. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 8: Exclusions and withdrawals after study entry
5. High‐dose versus low‐dose 5‐ASA
Failure to induce complete global or clinical remission
Several randomized trials have looked at dose‐ranging for various formulations of 5‐ASA (e.g. Asacol, Salofalk, Pentasa, MMX mesalamine). Two studies examined the efficacy of various doses of Salofalk or Pentasa for induction of global or clinical remission in participants with mild or moderately‐active UC (Hiwatashi 2011; Kruis 2003). Kruis 2003 found no difference in efficacy between Salofalk 4.5 g/day compared to 3 g/day (RR 1.35, 95% CI 0.96 to 1.89; 213 participants; Analysis 5.1) or 1.5 g/day (RR 0.91, 95% CI 0.69 to 1.22; 212 participants; Analysis 5.1). In Kruis 2003 34% (36/107) of participants in the 3 g/day group failed to enter remission compared to 50% (51/103) of participants in the 1.5 g/day group (RR 0.68, 95% CI 0.49 to 0.95). Hiwatashi 2011 examined the efficacy of Pentasa 4 g/day compared to 2.25 g/day in participants with moderately‐active UC and found 78% (47/60) in the 4 g group compared to 86% (54/63) in the 2.25 g group failed to achieve global or clinical remission (RR 0.91, 95% CI 0.77 to 1.08; Analysis 5.1). Ito 2010 compared Asacol 3.6 g/day with Asacol 2.4 g/day. Fifty‐five per cent (36/65) of participants in the 3.6 g/day Asacol group failed to enter remission compared to 70% (46/66) of participants in the 2.4 g/day dose group (RR 0.79, 95% CI 0.61 to 1.04).
5.1. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 1: Failure to Induce Global/Clinical Remission
D'Haens 2006 and Kamm 2007 investigated the efficacy of MMX mesalamine 2.4 g/day dosed once daily versus 4.8 g/day dosed once daily for induction of remission in active UC. Sixty‐one per cent (59/96) of participants in the 4.8 g/day group failed to enter remission compared to 60% (59/98) of participants in the 2.4 g/day group (RR 1.03, 95% CI 0.82 to 1.29, I2 = 0%).
Failure to induce global or clinical improvement
Six studies examined the efficacy of various doses of Asacol for global or clinical improvement including remission in participants with mild or moderately‐active UC (Hanauer 2005; Hanauer 2007; Miglioli 1990; Sandborn 2009; Schroeder 1987; Sninsky 1991). In Schroeder 1987 26% (10/38) in the 4.8 g/day group compared to 73% (8/11) in the 1.6 g/day group failed to induce clinical remission or improvement (RR 0.36, 95% CI 0.19 to 0.69; Analysis 5.2). Miglioli 1990 found 29% (7/24) of the 3.6 g/day dosing group compared to 48% (12/25) of the 1.2 g/day dosing group failed to induce clinical remission or improvement (RR 0.61, 95% CI 0.29 to 1.28; Analysis 5.2). A pooled analysis of two studies (Miglioli 1990; Sninsky 1991) found that 55% (42/77) of the 2.4 g/day group compared to 59% (46/78) of the 1.6 or 1.2 g/day group failed to induce clinical remission or improvement (RR 0.92, 95% CI 0.70 to 1.21; I2 = 0%; 155 participants; Analysis 5.2). A pooled analysis of two studies (Miglioli 1990; Ito 2010) found 35% (31/89) of the 3.6 g/day group failed to induce clinical remission or improvement compared with 51% (46/90) of participants in the 2.4 g/day group (RR 0.68, 95% CI 0.48 to 0.97; I2 = 0%; 179 participants; Analysis 5.2).
5.2. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 2: Failure to Induce Global/Clinical Remission or Improvement
A pooled analysis of the ASCEND studies (I, II and III; 1459 participants) found no difference in clinical improvement between Asacol 4.8 g/day and 2.4 g/day. Thirty‐seven per cent (266/727) of participants in the 4.8 g/day group failed to improve clinically compared to 41% (302/732) of participants in the 2.4 g/day group (RR 0.89, 95% CI 0.78 to 1.01; I2 = 0%; Analysis 5.2). Subgroup analyses indicated that participants with moderate disease may benefit from the higher dose of 4.8 g/day (Hanauer 2005; Hanauer 2007), particularly among participants previously treated with corticosteroids, oral 5‐ASA, rectal therapies or multiple UC medications (Hanauer 2005; Hanauer 2007; Sandborn 2009).
Kamm 2007 provided data for the failure to induce global/clinical remission or improvement. Thirty‐five per cent (30/85) of participants in the 4.8 g/day group failed to improve clinically compared to 39% (33/84) of participants in the 2.4 g/day group (RR 0.90, 95% CI 0.61 to 1.33; Analysis 5.2). Hiwatashi 2011 examined the efficacy of Pentasa 4 g/day compared to 2.25 g/day in participants with moderately‐active UC. Twenty‐five per cent (15/60) of participants in the 4 g/day group failed to improve clinically compared to 57% (36/63) of participants in the 2.25 g/day group (RR 0.44, 95% CI 0.27 to 0.71; Analysis 5.2).
Failure to induce endoscopic remission
No studies reported this outcome.
Failure to induce endoscopic improvement
No studies reported this outcome.
Failure to adhere to medication regimen
No studies reported this outcome
Adverse events
Three dose‐ranging studies (807 participants) reported the proportion of participants who experienced at least one AE (Hiwatashi 2011; Kruis 2003; Schroeder 1987). No differences in AE rates were found across any of the dosing subgroups: Asacol 4.8 g versus 1.6 g/day (RR 0.76, 95% CI 0.48 to 1.21; 49 participants); Salofalk 4.5 g versus 3 g/day (RR 0.96, 95% CI 0.78 to 1.20; 213 participants); Salofalk 4.5 g versus 1.5 g/day (RR 0.96, 95% CI 0.77 to 1.19; 209 participants); Salofalk 3 g versus 1.5 g/day (RR 1.04, 95% CI 0.84 to 1.29; 213 participants); Pentasa 4 g versus 2.25 g/day (RR 0.93, 95% CI 0.78 to 1.11; 123 participants). The most common AE reported in D'Haens 2006 was headache. Other less frequent AEs included diarrhea, nausea and abdominal pain. AEs for Kamm 2007, which included two different dose groups for once‐daily MMX mesalamine (2.4 g/day and 4.8 g/day), an Asacol reference arm and a placebo group, are reported above (Analysis 5.3.
5.3. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 3: Development of any adverse event
Serious adverse events
Two studies (336 participants) reported on the proportion of participants who experienced at least one SAE (Hiwatashi 2011; Kruis 2003). No differences in SAE rates were found across any of the dosing subgroups: Salofalk 4.5 g versus 3 g/day (RR 0.50, 95% CI 0.05 to 5.48; 213 participants); Pentasa 4 g versus 2.25 g/day (RR 5.25, 95% CI 0.26 to 107.07; 123 participants; Analysis 5.4). SAEs include aggravation of nasopharyngitis and UC aggravation.
5.4. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 4: Serious adverse events
Withdrawal due to adverse events
Five dose‐ranging studies (1178 participants) reported the proportion of participants who were withdrawn due to AEs (Hanauer 2005; Hiwatashi 2011; Kruis 2003; Schroeder 1987; Sninsky 1991). No differences in rates of withdrawal due to AEs were found in any of the dosing subgroups: Asacol 4.8 g/day versus 2.4 g/day (RR 0.93, 95% CI 0.24 to 3.63; 268 participants); Asacol 4.8 g/day versus 1.6 g/day (RR 0.29, 95% CI 0.02 to 4.26; 49 participants); Asacol 2.4 g/day versus 1.6 g/day (RR 5.00, 95% 0.25 to 101.73; 106 participants); Salofalk 4.5 g/day versus 3 g/day (RR 1.30, 95% CI 0.50 to 3.36; 213 participants); Salofalk 4.5 g/day versus 1.5 g/day (RR 0.80, 95% 0.34 to 1.84; 209 participants); Salofalk 3 g/day versus 1.5 g/day (RR 0.61, 95% CI 0.25 to 1.52; 210 participants); and Pentasa 4 g/day versus 2.25 g/day (RR 0.21, 95% CI 0.01 to 4.28; 123 participants; Analysis 5.5). The common AEs leading to withdrawal included UC aggravation, dizziness and headaches.
5.5. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 5: Withdrawal from study due to adverse event
Withdrawal or exclusions following study entry
Six dose‐ranging studies (1442 participants) reported the proportion of participants who were excluded or withdrawn after entry (Hanauer 2005; Hiwatashi 2011; Kruis 2003; Miglioli 1990; Schroeder 1987; Sninsky 1991). We found a difference between Salofalk 3 g/day and 1.5 g/day (RR 0.61, 95% CI 0.38 to 0.99; 210 participants) and between Salofalk 4.5 g/day and 1.5 g/day (RR 0.62, 95% CI 0.38 to 0.99; 209 participants). However, no other differences were found in rates of exclusions or withdrawals after entry in other dosing subgroups: Asacol 4.8 g/day versus 2.4 g/day (RR 0.68, 95% CI 0.40 to 1.16; 386 participants); Asacol 4.8 g/day versus 1.6 g/day (RR 0.19, 95% CI 0.04 to 1.01; 49 participants); Asacol 3.6 g/day versus 2.4 g/day (RR 0.50, 95% CI 0.10 to 2.48; 48 participants); Asacol 3.6 g/day versus 1.2 g/day (RR 0.42, 95% CI 0.09 to 1.95; 49 participants); Asacol 2.4 g/day versus 1.6 or 1.2 g/day (RR 1.07, 95% CI 0.60 to 1.92; 155 participants); Salofalk 4.5 g/day versus 3 g/day (RR 1.01, 95% CI 0.59 to 1.74; 213 participants); and Pentasa 4 g/day versus 2.25 g/day (RR 0.53, 95% CI 0.24 to 1.14; 123 participants; Analysis 5.6).
5.6. Analysis.

Comparison 5: 5‐ASA dose ranging, Outcome 6: Exclusions and withdrawals after entry
Discussion
Summary of main results
This systematic review largely confirms the results of previous meta‐analyses (Feagan 2012; Sutherland 1993; Sutherland 1997; Sutherland 2006b; Wang 2016), but differs from the previous work in a variety of ways. This update identified one new included study (D'Haens 2017) and one ongoing study (NCT02522767), and therefore now includes 54 studies with 9612 participants. D'Haens 2017 is a dosing study and assessed 3.2 g of oral mesalazine administered as two 1600 mg tablets taken once daily or four 400 mg tablets taken twice daily. NCT02522767 is an ongoing study assessing 4 g extended‐release granules of mesalamine and placebo. We have also added serious adverse events (SAEs) as a new secondary outcome in this version of this review.
The effectiveness of oral 5‐ASA preparations for the treatment of mild‐to‐moderate active UC was confirmed. Oral 5‐ASA is superior to placebo for induction of remission and clinical improvement in participants with active mild‐to‐moderate UC. The number needed to treat for an additional beneficial outcome from treatment is nine patients.
As we found in our previous meta‐analysis, there was a trend in favor of a slight benefit for the newer 5‐ASA preparations over SASP for the induction of global/clinical and endoscopic improvement (including remission). There are several points to be considered. It is possible that larger sample populations would confirm this finding, but the clinical relevance of such a difference would be debatable. Another possible explanation for the difference may be related to our use of the ITT principle, which should benefit medications with lower dropout rates, in this case 5‐ASA.
The assumption that SASP serves only as a pro‐drug to deliver 5‐ASA to its site of action has been questioned in light of the observation that increasing doses of 5‐ASA, within the dose‐response range of SASP, fail to enhance its efficacy beyond that of the standard 2 to 4 g therapeutic doses of SASP (Hayllar 1991). In active disease, a variety of 5‐ASA to SASP mass ratios were studied; doses of 5‐ASA corresponding to up to 10 g of SASP were commonly prescribed while just 2 to 4 g/day of SASP were used as controls. Despite this discrepancy, we could not confirm a significant superiority of 5‐ASA. Furthermore, when trial arms were subdivided according to their 5‐ASA/SASP mass ratios, r (r < 1/2, 1/1 > r ≥ 1/2, r ≥ 1/1), no general dose trends could be detected (data not shown). It has been suggested that if an increase in the colonic concentration of 5‐ASA within the range of SASP dose‐dependence does not parallel an enhanced efficacy, then 5‐ASA is unlikely to be the only mediator of therapeutic activity (Hayllar 1991). Elucidation of the mechanisms of action of 5‐ASA, sulfapyridine, and SASP (reviewed by Greenfield 1993), corroborated by their individual clinical effects, may explain this curious finding, as well as facilitate the determination of the currently unknown etiology of UC.
It was apparent that the newer 5‐ASA preparations were not entirely free of causing adverse effects in a number of participants. However, the incidence of AEs, SAEs and withdrawals due to the 5‐ASA formulations did not significantly differ from that associated with placebo. Furthermore, there were significantly more withdrawals due to AEs with SASP than with 5‐ASA.
Olsalazine caused a significantly higher proportion of withdrawals due to AEs relative to placebo, but lower than the proportion caused by SASP. The most common AE attributed to Olsalazine was diarrhea, an effect previously observed in approximately 10% of participants receiving the drug (Ireland 1987). It should be noted that there may have been a bias in favor of SASP, since many of the studies involved participants who were known to have tolerated SASP in the past. It has been suggested that protocol alterations may reduce the withdrawal rates in future trials, since encouraging participants to take Olsalazine with meals appears to reduce the incidence of diarrhea to approximately 3% of participants (Jarnerot 1996); of the included Olsalazine trials, only two reported that participants were instructed to take their medication with meals (Hetzel 1986; Zinberg 1990). Mesalamine‐induced interstitial nephritis is a serious but rare AE (Elseviers 2004). Although there have been case reports of interstitial nephritis in people with IBD treated with 5‐ASA (Arend 2004; Frandsen 2002; Maeda 2001), there were no reports of interstitial nephritis in the studies included in this systematic review.
This meta‐analysis indicates that oral 5‐ASA administered once daily is as effective as conventional dosing (twice or three times daily) for induction therapy in mild to moderately‐active UC. High‐certainty evidence suggests no difference between once‐daily and conventional dosing for induction of remission, and moderate‐certainty evidence suggests no differences in clinical improvement. Furthermore, subgroup analyses by drug formulation (MMX mesalazine, Salofalk, Asacol and Pentasa) showed no differences in efficacy between once‐daily and conventional dosing for induction of remission. However, the latter results should be interpreted cautiously since only five formulations were evaluated in this analysis.
We found no differences between once‐daily and conventionally‐dosed oral 5‐ASA for safety outcomes, including the overall incidence of AEs, SAEs, withdrawal from treatment due to an AE or exclusions or withdrawals after entry. In keeping with the well‐established safety profile of oral 5‐ASA, most of the AEs reported in the studies were mild‐to‐moderate in intensity. Common AEs were gastrointestinal symptoms (e.g. flatulence, abdominal pain, nausea, and diarrhea), headache and worsening UC.
Important patient preference and adherence differences may exist between dosing regimens. In the study that measured participant preference, most preferred once‐daily dosing to conventional dosing (Kruis 2009). Although it is generally believed that administration of fewer tablets and less frequent dosing improves both efficacy and adherence, we could not demonstrate the superiority of once‐daily dosing for either of these outcomes. This result suggests that patient adherence may not be enhanced by once‐daily dosing in the clinical trial setting. Several possible explanations exist for these observations, but the most plausible one concerns the unique aspects of the clinical trial environment. It is noteworthy that adherence was remarkably high in the studies that measured this outcome (Kamm 2007; Lichtenstein 2007). The pooled adherence rate was 92% in the once‐daily dosing group compared to 94% in the conventional‐dosing group. These rates likely reflect the highly supervised environment in which the studies were conducted. Adherence to medication in clinical trials is generally greater than in clinical practice, since participants are highly selected volunteers who are more likely, in general, to adhere to drug regimens (Andrade 1995; Kane 2001; Kane 2006; Kane 2008). In addition, adherence is continuously reinforced during the clinical trial process. Thus, it may be difficult to detect differences in adherence between once‐daily and multiple‐dose regimens in this setting. Accordingly, there is a need to compare dosing regimens in large‐scale community‐based studies.Reported adherence rates in community‐based studies range from 40% to 60% and are especially poor among people in remission (Kane 2001; Kane 2003a; Levy 1999; Shale 2003). However, whether once‐daily dosing regimens improve adherence in the community remains unknown.
Experience from other indications suggests that factors other than the dosing regimen are important for long‐term compliance (Brixner 2007; Kane 2008). Long‐term observations in people with UC as well as in other indications indicate that patients' and physicians' behaviors play a dominant role in adherence (Beaulieu 2009; Magowan 2006). The patient‐physician relationship should reinforce adherence through education, open communication and mutual agreement about the value of treatment (Kane 2008).
Moderate‐certainty evidence suggests that there may be little or no difference in efficacy or safety between the various formulations of oral 5‐ASA. To further support the conclusion that there is no difference in efficacy between 5‐ASA formulations, it should be noted that only one induction study reported a difference in efficacy between two different formulations of 5‐ASA (Green 1998). Green 1998 reported that Balsalazide 6.75 g/day was superior to Asacol 2.4 g/day for induction of complete remission (none or mild symptoms and sigmoidoscopy score of 0 or 1 at 12 weeks). However, two similar trials did not support these findings (Levine 2002; Pruitt 2002).
Pharmacokinetic studies suggest that systemic exposure to 5‐ASA is similar for all oral 5‐ASA formulations and 5‐ASA pro‐drugs (Sandborn 2002a; Sandborn 2002b; Sandborn 2002c; Sandborn 2003). With the exception of Olsalazine‐related diarrhea (Feurle 1989; Hanauer 1996; Robinson 1994; Zinberg 1990), there does not appear to be any difference in safety between the various formulations of oral 5‐ASA. The overall pooled risk ratios showed no differences in the incidence of AEs, SAEs, withdrawal due to AEs or exclusions or withdrawals after entry. Thus, all of the 5‐ASA formulations can be considered safe and effective for the treatment of active UC, and from a practical standpoint they can be considered therapeutically equivalent at equimolar doses (Sandborn 2002a). Treatment with sulfasalazine and Olsalazine may not be preferable due to the high frequency of AEs. When selecting among the remaining 5‐ASA formulations, physicians and patients should consider dose‐response data for 5‐ASA doses up to 4 to 4.8 g/day of 5‐ASA, adherence issues related to dose forms (size of dose form and total number of tablets or capsules per day), and price, when deciding which formulations to use (Sandborn 2002a).
The ASCEND I, ASCEND II and ASCEND III studies compared Asacol 4.8 g/day to Asacol 2.4 g/day in people with mild to moderately‐active UC (Hanauer 2005; Hanauer 2007), or in people with moderately‐active disease (Sandborn 2009). A pooled analysis of the three studies (1459 participants) showed no difference between the dose groups in failure to induce clinical improvement. However, subgroup analyses indicated that participants with moderate disease may benefit from the higher dose of 4.8 g/day (Hanauer 2005; Hanauer 2007), particularly among participants previously treated with corticosteroids, oral 5‐ASA, rectal therapies or multiple UC medications (Hanauer 2005; Hanauer 2007; Sandborn 2009). Both doses appear to have similar efficacy in participants with mild disease, which suggests that a dose of 2.4 g/day may be preferred for people with mildly‐active disease. Hiwatashi 2011 compared Pentasa 4 g/day to Pentasa 2.25 g/day in people with moderate disease and found a difference in favor of the higher‐dose group for clinical improvement which appears to confirm the results of the ASCEND studies. Hiwatashi 2011 concluded that people with severe symptoms such as relapse‐remitting and moderately‐active disease should be treated initially with 4 g/day.
A pooled analysis of two studies (194 participants) comparing MMX mesalazine 4.8 g to 2.4 g day did not show a difference between the dose groups in failure to induce clinical remission or improvement, suggesting that both dosage groups are efficacious in people with mild to moderately‐active UC (D'Haens 2006; Kamm 2007). A subgroup analysis by severity did not show any advantage for the higher dose (4.8 g/day) in participants with moderate disease (Kamm 2007). However, further research may be necessary to identify those who will benefit from varying doses of MMX mesalamine (Kamm 2007). Kruis 2003 evaluated the efficacy of three doses of Salofalk mesalamine pellets (1.5, 3.0, and 4.5 g/day) in people with active UC, and found no difference in remission rates between 4.5 g/day and 3 g/day, and a difference in remission rates between 3 g and 1.5 g/day. Kruis 2003 concluded that there was no dose response between the three dose groups and recommended the lowest effective dose (1.5 g/day) for treatment of people with mild‐to‐moderate UC. People failing at this dose might benefit from an increase to 3 g/day, but doses higher than this amount do not appear to provide any additional benefit (Kruis 2003).
Overall completeness and applicability of evidence
We believe the evidence from this review is applicable to most people with mild‐to‐moderate ulcerative colitis. The evidence assesses 5‐ASA compared with placebo, sulfasalazine and comparator 5‐ASA. The studies also assess 5‐ASA dose‐ranging studies and once‐daily dosing studies compared to conventional‐dosing studies. All the safety and efficacy outcomes which we aimed to report on were included in the studies, but there were a couple of outcomes that were rarely reported, including failure to adhere to the medication regimen and endoscopic remission. The review found mainly moderate‐to‐high‐certainty evidence for the oral 5‐ASA versus placebo and oral 5‐ASA versus SASP studies, which might therefore imply that this area does not require additional studies. However, the evidence comparing oral 5‐ASA with comparator 5‐ASA is mostly of moderate certainty, and once‐daily with conventional dosing is mostly low‐to‐moderate‐certainty evidence. Additional studies for these comparisons may therefore change the overall results.
Quality of the evidence
We assessed the included studies using the Cochrane 'Risk of bias' tool and GRADE criteria. Five studies were rated at high risk of bias due to incomplete outcome data (Green 1998; Kruis 2003) and lack of blinding (Farup 2001; Flourié 2013; Tursi 2004). Thirty‐two of 54 included studies did not describe the method used for randomization and were rated as unclear for this domain. Twenty‐six studies did not describe methods used for allocation concealment and were rated as unclear for this domain. The methods used for blinding were not described in five studies, and we rated these studies as unclear. Twenty studies were rated as unclear for incomplete outcome data because reasons for withdrawal were either not described or were not attributed to intervention groups. Six studies were rated as unclear for selective reporting.
For the oral 5‐ASA versus placebo comparison clinical remission and AEs were rated as high certainty. The outcomes clinical improvement, endoscopic remission and withdrawal due to AEs were rated as moderate, due to heterogeneity and sparse data, and SAEs were rated as low certainty due to very sparse data (Table 1). For the 5‐ASA versus SASP studies the outcomes induction of remission and clinical improvement were rated as moderate certainty (due to sparse data) and high certainty respectively. The AEs and withdrawal due to AE outcomes were both rated as moderate, due to sparse data, and SAEs were low‐certainty due to very sparse data (Table 2). For the once‐daily compared to conventional‐dosing studies, the overall certainty of the evidence using the GRADE approach was rated as high for the primary outcome (clinical remission) and moderate for the secondary outcomes of clinical improvement and AEs, due to sparse data (Table 3). The studies comparing the various formulations of 5‐ASA indicated that the overall certainty of the evidence for the primary outcome (failure to induce complete global or clinical remission) was moderate, due to a high risk of bias (lack of blinding) in two studies in the pooled analysis (See Table 4).
Potential biases in the review process
A comprehensive literature search helped minimize bias in relation to study selection. In addition two review authors independently screened the studies, extracted the data and assessed the risks of bias. There were limitations to drawing general conclusions. Almost every study used a unique clinical or endoscopic index. Unlike Crohn's disease, the lack of standard indices in UC prevented the collection of consistent treatment efficacy data and makes comparisons across clinical studies difficult. The use of endoscopic remission as an outcome would provide a more rigorous assessment of treatment efficacy in clinical trials. Clinicians should use a standardized approach to assess endoscopic appearance to allow for comparisons across trials. Most of the included studies were not of sufficient duration to permit documentation of endoscopic healing. Results were also periodically obscured in several studies that failed to specify the treatment arm to which certain excluded participants were initially randomized. Despite these and other common factors that must be considered when interpreting meta‐analyses, the data provided strong evidence that pointed towards a number of conclusions.
Agreements and disagreements with other studies or reviews
We have identified two other systematic reviews that have assessed 5‐ASA for the induction of remission in UC (Ford 2011; Kane 2003b). Ford 2011 is a systematic review and meta‐analysis assessing the efficacy of 5‐ASA in people with UC. The review included 37 RCTs with 19 induction studies (nine studies comparing 5‐ASA to placebo and 10 studies comparing different doses of 5‐ASA) and 18 maintenance studies. This review concluded that 5‐ASAs are highly effective for both the induction of remission and prevention of relapse in UC participants.
Kane 2003b is a systematic review on the efficacy of oral 5‐ASA for active UC. Thirty‐one studies were identified and 19 met the inclusion criteria. This review suggested that mesalamine is superior to placebo for treating active UC and that 5‐ASA products appear to be as effective as sulfasalazine, but available data do not suggest a difference in efficacy between any of the 5‐ASA preparations.
Authors' conclusions
Implications for practice.
5‐ASA was superior to placebo and no more effective than SASP. Nonetheless, it is clear that the newer 5‐ASA preparations have yet to be proven to be more clinically beneficial than SASP for the treatment of UC. The decision to use 5‐ASA or SASP should consider tolerance to SASP. Oral 5‐ASA administered once daily is as effective and safe as conventional dosing (twice or three times daily) for induction therapy in mild to moderately‐active UC. There do not appear to be any differences in efficacy or safety between the various formulations of 5‐ASA. Among people with mildly‐active UC a dosage of 4 to 4.8 g/day does not appear to provide any additional benefit over a dosage of 2 to 2.4 g/day. Patients with severe symptoms and moderately‐active disease may benefit from an initial dosage of 4 to 4.8 g/day. When selecting among the various 5‐ASA formulations, physicians and patients should consider dose‐response data, adherence issues related to dose forms (size of dose form and total number of tablets or capsules per day) (Sandborn 2002a).
Implications for research.
Future trials comparing the efficacy of oral 5‐ASA with placebo or SASP do not appear to be justified. There is little evidence to suggest that there is a difference in efficacy between the oral 5‐ASA drugs. Future trials should look at enhancing patient adherence to medication. Adherence to therapy is important for treatment success and may be an important predictor of relapse (Kane 2003a; Kane 2001).
Future trials could assess whether once‐daily dosing regimens improve adherence in the community. There is currently one ongoing study comparing 5‐ASA to placebo. One of the trials (NCT02522767) assessed a 4 g extended‐release once‐daily dosing regimen, but did not assess medication adherence. Future trials may be necessary to identify people who will benefit from varying doses of MMX mesalamine or Salofalk.
What's new
| Date | Event | Description |
|---|---|---|
| 11 June 2019 | New citation required but conclusions have not changed | Updated review with new authors. |
| 11 June 2019 | New search has been performed | We conducted a new literature search on 11 June 2019, and added one study. |
History
Review first published: Issue 4, 1997
| Date | Event | Description |
|---|---|---|
| 14 June 2016 | Amended | Correction of minor error in study flow diagram |
| 9 July 2015 | New citation required but conclusions have not changed | Updated review with new authors |
| 9 July 2015 | New search has been performed | A new literature was conducted on 9 July 2015. New studies added |
Acknowledgements
We would like to thank the following investigators for providing additional information about their studies: Nobuo Hiwatashi, Peter Gibson.
Appendices
Appendix 1. Search strategies
MEDLINE Search Strategy:
1. random$.tw.
2. factorial$.tw.
3. (crossover$ or cross over$ or cross‐over$).tw.
4. placebo$.tw.
5. single blind.mp.
6. double blind.mp.
7. triple blind.mp.
8. (singl$ adj blind$).tw.
9. (double$ adj blind$).tw.
10. (tripl$ adj blind$).tw.
11. assign$.tw.
12. allocat$.tw.
13. randomized controlled trial/
14. or/1‐13
15. (colitis and ulcerat*).mp.
16. ulcerative colitis.mp. or exp ulcerative colitis/
17. (inflammatory bowel disease* or IBD).mp.
18. 19 or 20 or 21
19. 18 and 22
20. 5‐aminosalicylic acid.mp. or exp Mesalamine/
21. Mesalazine.mp. or exp Mesalamine/
22. Sulfasalazine.mp. or exp Sulfasalazine/
23. sulphasalazine.mp. or exp Sulfasalazine/
24. 24 or 25 or 26 or 27
25. 23 and 28
EMBASE Search Strategy:
1. random$.tw.
2. factorial$.tw.
3. (crossover$ or cross over$ or cross‐over$).tw.
4. placebo$.tw.
5. single blind.mp.
6. double blind.mp.
7. triple blind.mp.
8. (singl$ adj blind$).tw.
9. (double$ adj blind$).tw.
10. (tripl$ adj blind$).tw.
11. assign$.tw.
12. allocat$.tw.
13. crossover procedure/
14. double blind procedure/
15. single blind procedure/
16. triple blind procedure/
17. randomized controlled trial/
18. or/1‐17
19. (colitis and ulcerat*).mp.
20. ulcerative colitis.mp. or exp ulcerative colitis/
21. (inflammatory bowel disease* or IBD).mp.
22. 19 or 20 or 21
23. 18 and 22
24. 5‐aminosalicylic acid.mp. or exp Mesalamine/
25. Mesalazine.mp. or exp Mesalamine/
26. Sulfasalazine.mp. or exp Sulfasalazine/
27. sulphasalazine.mp. or exp Sulfasalazine/
28. 24 or 25 or 26 or 27
29. 23 and 28
Cochrane Library Search Strategy:
1. MeSH descriptor: [Colitis, Ulcerative] explode all trees
2. colitis
3. #1 or #2
4. 5‐ASA
5. 5‐aminosalicylic acid
6. Mesalamine
7. Sulfasalazine
8. Salazosulfapyridine
9. Sulphasalazine
10. #4 or #5 or #6 or #7 or #8 or #9
11. #3 and #10
Cochrane IBD Specialized Register:
1. 5‐ASA (ab/ti)
2. 5‐Amino* (ab/ti)
3. Mesala* (ab/ti)
4. Sulfa* (ab/ti)
5. Sulpha* (ab/ti)
6. 1 or 2 or 3 or 4 or 5
7. Colitis (ab/ti)
8. 6 and 7
Clinical Trials. Gov
5‐ASA and Ulcerative Colitis
Data and analyses
Comparison 1. 5‐ASA versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Failure to induce global/clinical remission | 11 | 2387 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.82, 0.89] |
| 1.1.1 Dose of 5‐ASA: < 2 g | 3 | 231 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.84, 1.02] |
| 1.1.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 8 | 956 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.82, 0.94] |
| 1.1.3 Dose of 5‐ASA: ≥ 3 g | 8 | 1200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.77, 0.88] |
| 1.2 Failure to induce global/clinical improvement (including remission) | 14 | 2256 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.61, 0.75] |
| 1.2.1 Dose of 5‐ASA: < 2 g | 3 | 231 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.64, 0.97] |
| 1.2.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 10 | 877 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.67, 0.88] |
| 1.2.3 Dose of 5‐ASA: ≥ 3 g | 9 | 1148 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.51, 0.65] |
| 1.3 Failure to induce endoscopic remission | 4 | 1154 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.67, 0.89] |
| 1.3.1 Dose of 5‐ASA: < 2 g | 1 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.64, 1.14] |
| 1.3.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 3 | 393 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.70, 1.05] |
| 1.3.3 Dose of 5‐ASA: ≥ 3 g | 4 | 639 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.56, 0.87] |
| 1.4 Failure to induce endoscopic improvement (including remission) | 4 | 416 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.59, 0.86] |
| 1.4.1 Dose of 5‐ASA: 2 ‐ 2.9 g | 3 | 265 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.58, 0.92] |
| 1.4.2 Dose of 5‐ASA: ≥ 3 g | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.49, 0.96] |
| 1.5 Adverse events | 8 | 1218 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.85, 1.07] |
| 1.5.1 Dose of 5‐ASA: < 2 g | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.74, 2.13] |
| 1.5.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 5 | 377 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.82, 1.33] |
| 1.5.3 Dose of 5‐ASA: ≥ 3 g | 5 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.80, 1.05] |
| 1.6 Serious adverse events | 4 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.18, 1.56] |
| 1.6.1 Dose of 5‐ASA: 2 ‐ 2.9 g | 3 | 243 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.14, 3.33] |
| 1.6.2 Dose of 5‐ASA: ≥ 3 g | 3 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.10, 1.92] |
| 1.7 Withdrawals due to adverse events | 13 | 2372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.54, 0.97] |
| 1.7.1 Dose of 5‐ASA: < 2 g | 3 | 231 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.19, 1.63] |
| 1.7.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 9 | 926 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.65, 1.94] |
| 1.7.3 Dose of 5‐ASA: ≥ 3 g | 9 | 1215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.41, 0.87] |
| 1.8 Exclusions and withdrawals after study entry | 15 | 2529 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.51, 0.72] |
| 1.8.1 Dose of 5‐ASA: < 2 g | 3 | 231 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.42, 0.98] |
| 1.8.2 Dose of 5‐ASA: 2 ‐ 2.9 g | 11 | 1014 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.53, 0.92] |
| 1.8.3 Dose of 5‐ASA: ≥ 3 g | 10 | 1284 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.41, 0.66] |
Comparison 2. 5‐ASA versus sulfasalazine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Failure to induce global/clinical remission | 8 | 526 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.77, 1.04] |
| 2.1.1 5‐ASA / SASP < 1/2 | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.57, 1.41] |
| 2.1.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 5 | 359 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.77, 1.08] |
| 2.1.3 5‐ASA / SASP ≥ 1/1 | 3 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.59, 1.23] |
| 2.2 Failure to induce global/clinical improvement (including remission) | 14 | 1053 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.76, 1.01] |
| 2.2.1 5‐ASA / SASP < 1/2 | 3 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.47, 1.27] |
| 2.2.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 11 | 804 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.77, 1.05] |
| 2.2.3 5‐ASA / SASP ≥ 1/1 | 3 | 126 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.54, 1.22] |
| 2.3 Failure to induce endoscopic improvement (including remission) | 6 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.65, 1.02] |
| 2.3.1 5‐ASA / SASP < 1/2 | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.58, 1.04] |
| 2.3.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 4 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.53, 1.02] |
| 2.3.3 5‐ASA / SASP ≥ 1/1 | 2 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.72, 1.57] |
| 2.4 Adverse events | 12 | 909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.36, 0.63] |
| 2.4.1 5‐ASA / SASP < 1/2 | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.10, 1.20] |
| 2.4.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 9 | 746 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.41, 0.73] |
| 2.4.3 5‐ASA / SASP ≥ 1/1 | 2 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.05, 0.52] |
| 2.5 Serious adverse events | 2 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.28, 6.52] |
| 2.6 Withdrawals due to adverse events | 10 | 640 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.24, 0.68] |
| 2.6.1 5‐ASA / SASP < 1/2 | 2 | 85 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.41] |
| 2.6.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 5 | 361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.32, 1.39] |
| 2.6.3 5‐ASA / SASP ≥ 1/1 | 4 | 194 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.10, 0.60] |
| 2.7 Exclusions and withdrawals after study entry | 10 | 701 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.58, 0.99] |
| 2.7.1 5‐ASA / SASP < 1/2 | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 1.80] |
| 2.7.2 1/1 > 5‐ASA / SASP ≥ 1/2 | 6 | 478 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.71, 1.34] |
| 2.7.3 5‐ASA / SASP ≥ 1/1 | 4 | 194 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.25, 0.77] |
Comparison 3. Once daily dosing versus conventional dosing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Failure to induce global/clinical remission | 5 | 1761 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.93, 1.06] |
| 3.1.1 MMX once daily (OD) versus twice daily (BID) | 1 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.88, 1.31] |
| 3.1.2 Salofalk granules once daily (OD) versus three times daily (TID) | 1 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.59, 1.25] |
| 3.1.3 MMX once daily (OD) versus Asacol three times daily (TID) | 1 | 171 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.70, 1.12] |
| 3.1.4 Pentasa once daily (OD) versus twice daily (BID) | 1 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.73, 1.17] |
| 3.1.5 Mesalazine once daily (OD) versus twice daily (BID) | 1 | 817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.10] |
| 3.2 Failure to induce global/clinical improvement (including remission) | 3 | 564 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.49, 1.10] |
| 3.2.1 MMX (OD versus BID) | 1 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.26] |
| 3.2.2 MMX (OD) versus Asacol (TID) | 1 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.55, 1.16] |
| 3.2.3 Pentasa (OD versus BID) | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.17, 0.79] |
| 3.3 Failure to induce global/clinical improvement (sensitivity analysis) | 2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.68, 1.10] |
| 3.3.1 MMX (OD versus BID) | 1 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.67, 1.26] |
| 3.3.2 MMX (OD) versus Asacol (TID) | 1 | 171 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.55, 1.16] |
| 3.4 Failure to induce endoscopic remission | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.5 Failure to induce endoscopic improvement (including remission) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.6 Failure to adhere to medication regimen | 2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.64, 2.86] |
| 3.7 Compliance | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.8 Adverse events | 4 | 1586 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.89, 1.18] |
| 3.9 Serious adverse events | 4 | 1586 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.68, 2.66] |
| 3.10 Withdrawals due to adverse events | 5 | 1757 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.54, 1.49] |
| 3.11 Exclusions and withdrawals after study entry | 4 | 944 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.74, 1.39] |
Comparison 4. 5‐ASA versus comparator 5‐ASA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Failure to induce global/clinical remission | 11 | 1968 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.86, 1.02] |
| 4.1.1 Asacol comparator | 6 | 720 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.85, 1.04] |
| 4.1.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.78, 1.17] |
| 4.1.3 Salofalk comparator | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.72, 1.18] |
| 4.1.4 Pentasa comparator | 1 | 227 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.74, 1.10] |
| 4.2 Failure to induce global/clinical remission (sensitivity analysis) | 9 | 1681 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.87, 1.04] |
| 4.2.1 Asacol comparator | 5 | 660 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.86, 1.07] |
| 4.2.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.78, 1.17] |
| 4.2.3 Salofalk comparator | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.72, 1.18] |
| 4.3 Failure to induce global/clinical improvement (including remission) | 8 | 1647 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.77, 1.01] |
| 4.3.1 Asacol comparator | 3 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.73, 1.11] |
| 4.3.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.67, 1.10] |
| 4.3.3 Salofalk comparator | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.74, 1.36] |
| 4.3.4 Pentasa comparator | 1 | 227 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.45, 1.08] |
| 4.4 Failure to induce global/clinical improvement (sensitivity analysis) | 7 | 1420 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.05] |
| 4.4.1 Asacol comparator | 3 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.73, 1.11] |
| 4.4.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.67, 1.10] |
| 4.4.3 Salofalk comparator | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.74, 1.36] |
| 4.5 Adverse events | 9 | 1576 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.92, 1.12] |
| 4.5.1 Asacol comparator | 5 | 556 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.80, 1.03] |
| 4.5.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.01, 1.66] |
| 4.5.3 Salofalk comparator | 2 | 490 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.81, 1.20] |
| 4.6 Serious adverse events | 4 | 677 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.22, 1.56] |
| 4.6.1 Asacol comparator | 2 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.05, 2.11] |
| 4.6.2 Claversal comparator | 1 | 168 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.16, 2.95] |
| 4.6.3 Salofalk comparator | 1 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.14, 6.74] |
| 4.7 Withdrawals due to adverse events | 9 | 1489 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.57, 1.54] |
| 4.7.1 Asacol comparator | 6 | 726 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.04] |
| 4.7.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.70, 3.14] |
| 4.7.3 Salofalk comparator | 1 | 233 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.90 [0.44, 34.35] |
| 4.8 Exclusions and withdrawals after study entry | 9 | 1574 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.22] |
| 4.8.1 Asacol comparator | 5 | 553 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.67, 1.24] |
| 4.8.2 Claversal comparator | 2 | 530 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.74, 1.63] |
| 4.8.3 Salofalk comparator | 2 | 491 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.67, 1.51] |
4.2. Analysis.

Comparison 4: 5‐ASA versus comparator 5‐ASA, Outcome 2: Failure to induce global/clinical remission (sensitivity analysis)
Comparison 5. 5‐ASA dose ranging.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Failure to Induce Global/Clinical Remission | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1.1 Salofalk 4.5 g versus 3 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.96, 1.89] |
| 5.1.2 Salofalk 4.5 g versus 1.5 g/day | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.69, 1.22] |
| 5.1.3 Salofalk 3 g versus 1.5 g/day | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.49, 0.95] |
| 5.1.4 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.77, 1.08] |
| 5.1.5 Asacol 3.6 g versus 2.4 g/day | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.61, 1.04] |
| 5.1.6 MMX mesalazine 4.8 g versus 2.4 g/day | 2 | 194 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.82, 1.29] |
| 5.2 Failure to Induce Global/Clinical Remission or Improvement | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.2.1 Asacol 4.8 g versus 1.6 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.19, 0.69] |
| 5.2.2 Asacol 3.6 g versus 1.2 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.29, 1.28] |
| 5.2.3 Asacol 2.4 g versus 1.6 or 1.2 g/day | 2 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.70, 1.21] |
| 5.2.4 Asacol 3.6 g versus 2.4 g/day | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.48, 0.97] |
| 5.2.5 Asacol 4.8 g versus 2.4 g/day | 3 | 1459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.78, 1.01] |
| 5.2.6 MMX mesalazine 4.8 g versus 2.4 g/day | 1 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.61, 1.33] |
| 5.2.7 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.27, 0.71] |
| 5.3 Development of any adverse event | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.3.1 Asacol 4.8 g versus 1.6 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.48, 1.21] |
| 5.3.2 Salofalk 4.5 g versus 3 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.78, 1.20] |
| 5.3.3 Salofalk 4.5 g versus 1.5 g/day | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.77, 1.19] |
| 5.3.4 Salofalk 3 g versus 1.5 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.84, 1.29] |
| 5.3.5 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.78, 1.11] |
| 5.4 Serious adverse events | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.4.1 5.3.2 Salofalk 4.5 g versus 3 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 5.48] |
| 5.4.2 5.3.5 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.25 [0.26, 107.07] |
| 5.5 Withdrawal from study due to adverse event | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.5.1 Asacol 4.8 g versus 2.4 g/day | 1 | 268 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.24, 3.63] |
| 5.5.2 Asacol 4.8 g versus 1.6 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.02, 4.26] |
| 5.5.3 Asacol 2.4 g versus 1.6 g/day | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.00 [0.25, 101.73] |
| 5.5.4 Salofalk 4.5 g versus 3 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.50, 3.36] |
| 5.5.5 Salofalk 4.5 g versus 1.5 g/day | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.34, 1.84] |
| 5.5.6 Salofalk 3 g versus 1.5 g/day | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.25, 1.52] |
| 5.5.7 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.28] |
| 5.6 Exclusions and withdrawals after entry | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.6.1 Salofalk 3 g versus 1.5 g/day | 1 | 210 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.38, 0.99] |
| 5.6.2 Asacol 4.8 g versus 2.4 g/day | 1 | 386 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.40, 1.16] |
| 5.6.3 Asacol 4.8 g versus 1.6 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.04, 1.01] |
| 5.6.4 Asacol 3.6 g versus 2.4 g/day | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.10, 2.48] |
| 5.6.5 Asacol 3.6 g versus 1.2 g/day | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.09, 1.95] |
| 5.6.6 Asacol 2.4 g versus 1.6 or 1.2 g/day | 2 | 155 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.60, 1.92] |
| 5.6.7 Salofalk 4.5 g versus 3 g/day | 1 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.59, 1.74] |
| 5.6.8 Salofalk 4.5 g versus 1.5 g/day | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.38, 0.99] |
| 5.6.9 Pentasa 4 g versus 2.25 g/day | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.24, 1.14] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andreoli 1987.
| Study characteristics | ||
| Methods | Randomized, double‐blind trial comparing 5‐aminosalicylic acid and SASP | |
| Participants | Male and female participants, aged 19 to 63 years, with acute ulcerative colitis (N = 12) | |
| Interventions | 1.5 g/day 5‐ASA or 3 g/day SASP for 2 months | |
| Outcomes | Clinical endoscopic remission within 2 months of start of therapy was considered as a positive indication of remission induction | |
| Notes | Abstract ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation of drugs was performed using a table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Not described |
| Other bias | Unclear risk | Not described |
Bresci 1990.
| Study characteristics | ||
| Methods | Randomized trial comparing 5‐aminosalicylic acid and SASP | |
| Participants | Adults with ulcerative colitis of at least 2 years duration, with mild‐to‐moderate relapse (N = 86) | |
| Interventions | 2.4 g/day 5‐ASA (n = 44) or 3 g/day SASP (n = 42) for 6 weeks | |
| Outcomes | Clinical improvement, endoscopic and histologic appearance, indexes of phlogosis, hematic crasis, hepatic and renal functionality, and adverse events | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Cai 2001.
| Study characteristics | ||
| Methods | Randomized controlled trial | |
| Participants | Adults (aged 18 to 65 years) with active ulcerative colitis (N = 135) | |
| Interventions | Olsalazine 3 g/day (n = 105) or SASP 4 g/day (n = 30) | |
| Outcomes | Clinical improvement and adverse events | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Not described |
| Other bias | Unclear risk | Not described |
D'Haens 2006.
| Study characteristics | ||
| Methods | Randomized, multicenter, double‐blind, parallel‐group, dose‐ranging study | |
| Participants | Adultss (aged > 18 years) with histologically‐confirmed, newly‐diagnosed or relapsing mild to moderately‐active ulcerative colitis (N = 38) | |
| Interventions | MMX mesalazine (SPD476) 1.2 (n = 13), 2.4 (n = 14) or 4.8 g/day (n = 11), given once daily for 8 weeks | |
| Outcomes | Primary outcome: remission defined as a UC‐DAI score < 1 with a score of 0 for rectal bleeding and stool frequency, and at least a 1‐point reduction from baseline in sigmoidoscopy score. Secondary outcomes: change in UC‐DAI score, sigmoidoscopic appearance and histology from baseline to week 8, and the change in symptoms (rectal bleeding and stool frequency) from baseline to weeks 2, 4 and 8 for the 3 dose groups | |
| Notes | Study was funded by Shire Pharmaceuticals Inc. Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: MMX mesalazine and placebo tablets were identical in appearance |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The 1.2 g/day group had 6 withdrawals (6/13) compared to 3 (3/14) in the 2.4 g/day and 1 (1/11) in the 4.8 g/day groups. LOCF was used to address incomplete outcome data |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
D'Haens 2017.
| Study characteristics | ||
| Methods | Randomized, active‐controlled, multicenter, non‐inferiority induction trial | |
| Participants | Adults (18 years and older) diagnosed with mild‐to‐moderate ulcerative colitis (N = 817) | |
| Interventions | Participants received 3.2 g of oral mesalazine administered as 2 x 1600 mg tablets each morning or 4 x 400 mg tablets taken twice daily for 8 weeks | |
| Outcomes | Primary outcome: The proportion of participants in clinical and endoscopic remission at week 8 Secondary outcomes: Endoscopic remission, endoscopic response, clinical remission at week 8, rectal bleeding subscore of 0 at week 8, clinical and endoscopic response at week 8, clinical remission at week 12, clinical response at week 12, rectal bleeding subscore of 0 at week 12, clinical remission at weeks 8 and 10 and 12, clinical response at weeks 8 and 12 |
|
| Notes | Study was funded by Tillotts Pharma, AG. Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomization schedule was generated by computer in permuted blocks of 6 without stratification |
| Allocation concealment (selection bias) | Low risk | An interactive web response system was used to manage randomization and dispense the study drug |
| Blinding (performance bias and detection bias) All outcomes | Low risk | All participants took the same numer of identical‐looking 1600 mg or 400 mg placebo tablets. Investigators, central readers and participants were unaware of the participant assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants involved in the trial were accounted for with reasons |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported in the published study |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Ewe 1988.
| Study characteristics | ||
| Methods | Randomized, double‐blind trial comparing 5‐aminosalicylic acid (olsalazine) and SASP | |
| Participants | Adults with mild‐to‐moderate active chronic ulcerative colitis (N = 40) | |
| Interventions | 1.5 g/day 5‐ASA (olsalazine) for 14 days, and followed by 3 g/day SASP for a further 14 days (n = 20), or vice versa (n = 20) | |
| Outcomes | Clinical improvement: at each study visit a physical examination was performed and a detailed history was taken. In addition, a diary completed daily by the participant was evaluated. The diary was designed to record stool frequency and consistency, and blood staining of stools. Based on these variables investigators rated the efficacy of treatment as “improved”, ”no change” or “worse” | |
| Notes | Cross‐over trial. Data for outcomes were available before cross‐over Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data available for 40 of 41 participants entered in the study |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Farup 2001.
| Study characteristics | ||
| Methods | Randomized, open‐label, non‐inferiority study | |
| Participants | Adults with confirmed diagnosis of active mild‐to‐moderate ulcerative colitis (N = 227). People with proctitis were excluded | |
| Interventions | Pentasa sachet prolonged‐release granules 2 x 1 g packets twice daily (n = 74), 1 packet 4 times daily (n = 76) or pentasa prolonged‐release 500 mg tablets ‐ 2 tablets 4 times daily (n = 77) for 8 weeks | |
| Outcomes | Primary outcome: mean improvement in UC‐DAI Secondary outcomes: remission (UC‐DAI 0 or 1), improvement (reduction in UC‐DAI of > 2 from baseline), satisfaction with regimen, adverse events |
|
| Notes | Study was funded by Ferring Pharmaceuticals, Denmark Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 80 participants did not complete the study. Reasons are provided but are not attributed to individual treatment groups |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes were reported but reporting for withdrawals and adverse events was inadequate |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Feagan 2013.
| Study characteristics | ||
| Methods | Randomized, double‐blind, placebo‐controlled, multicenter, phase 3 study | |
| Participants | Adults (18 years or older) with a documented diagnosis of mild‐to‐moderate UC, defined by a modified UC‐DAI (N = 281) | |
| Interventions | Asacol 4.8 g/day (n = 140) or placebo (n = 141) | |
| Outcomes | Primary outcome: proportion of participants in clinical remission, defined as a score of 0 for stool frequency and rectal bleeding, and absence of fecal urgency at week 6 Secondary outcomes: clinical remission at weeks 6 and 10, endoscopic remission (defined as a sigmoidoscopic score of < 1) at week 6, endoscopic remission at week 10, improvement (defined as a decrease of at least 3 points from baseline in the modified UC‐DAI score) at week 6, improvement at week 10, mean changes in the modified UC‐DAI and UCCS from baseline to week 10, and adverse events |
|
| Notes | Study was funded by Tillotts Pharma, AG. Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated in permutated blocks by computer |
| Allocation concealment (selection bias) | Low risk | An interactive voice/web response system managed the randomization procedure and dispensed the study drug |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and central readers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants involved in the trial were accounted for with reasons |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported in the published study |
| Other bias | Low risk | The study appears to be free of other sources biases |
Feurle 1989.
| Study characteristics | ||
| Methods | Double‐blinded, placebo‐controlled, and centrally‐randomized, with stratification in blocks of 10 for each of the 12 centres | |
| Participants | Outpatients with mild‐to‐moderate ulcerative colitis recruited in West Germany between 1984 and 1986 (N = 105) | |
| Interventions | Olsalazine 2 g/day (4 doses of 2 gelatin capsules each; n = 52) or 8 placebo capsules with identical appearance (n = 53). Participants were advised to start with fewer than 8 pills and reach complete dosage by the third or fourth day and continue for 4 weeks. Compliance was verified by laboratory tests | |
| Outcomes | Clinical and laboratory examinations were performed at recruitment, after 2 weeks, and at the end of 4 weeks. Endoscopy and biopsy were performed on days 0 and 28. Clinical observations were made on days 0, 14, and 28 Endoscopic score was the mean of redness/hyperemia, contact bleeding, spontaneous bleeding and erosions, each graded on a 3‐point scale. Clinical status was based on number of stools, presence of blood in stool, stool consistency, and mucous in stool. The clinical score was considered improved when at least 3 of the 4 parameters increased. Occurrence of withdrawals and side effects was also tabulated |
|
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: identical placebo capsule |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Fleig 1988.
| Study characteristics | ||
| Methods | Prospective, randomized, double‐blind comparison of benzalazine (SAB) and SASP. | |
| Participants | Consecutive patients were randomized. Participants, aged 18 to 75 years, with histologically‐ and endoscopically‐diagnosed ulcerative colitis for 16 months with an acute episode defined as the occurrence of diarrhea with at least 5 stools daily for at least 3 days. Endoscopic appearance was graded according to a 4‐point scale (N = 43) | |
| Interventions | Equimolar, identical‐appearing doses of either SASP (2 tablets, 3 times/day; 0.5 g per tablet; n = 21) or SAB (2 tablets, 3 times/day; 0.36 g per tablet; n = 22) for 6 weeks, except for the first week when dosage of either was 2 tablets, 4 times daily | |
| Outcomes | Laboratory and clinical evaluations were performed once a week, in addition to participant diaries to record number and consistency of stools, and occurrence of rectal bleeding. Endoscopy was performed at entry and after 6 weeks to determine severity of inflammation and to obtain a biopsy which was evaluated on a 4‐point scale Efficacy was evaluated in terms of positive changes in major clinical (number and consistency of stools), sigmoidoscopic, and morphological (histologic grading of inflammation) criteria. Occurrence of side effects and withdrawals were also reported | |
| Notes | Study was funded by Henning Berlin GmbH Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Participants received the medication assigned to their patient number according to the sequence of entry into the trial. Treatment was randdomly assigned to patient numbers |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: tablets of identical appearance. Assignment was blind to both participants and treating physicians |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two participants in 5‐ASA group were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Flourié 2013.
| Study characteristics | ||
| Methods | Multicenter, controlled, randomized, investigator‐blinded, comparative, non‐inferiority study | |
| Participants | Adults (18 years or older) with newly‐diagnosed or relapsing mild‐to‐moderate ulcerative colitis, with disease extension beyond the rectum (N = 206) | |
| Interventions | Mesalazine (4 g/day), either once daily with 2 sachets of 2 g mesalazine granules in the morning (n = 102), or twice daily with 1 x 2 g sachet in the morning and one in the evening (n = 104) for 8 weeks | |
| Outcomes | Primary outcome: percentage of participants in clinical and endoscopic remission after 8 weeks (defined as UC‐DAI score < 1) Secondary outcomes: complete remission at week 8 (clinical and endoscopic UC‐DAI = 0), clinical and endoscopic improvement at week 8 (decrease in UC‐DAI by at least 2 points), clinical remission at weeks 4, 8 and 12, determined by normal stool frequency, no bloody stools and no active disease by physician’s assessment, time to remission (based on participant’s diary with normal stool frequency and cessation of bleeding; estimated using Kaplan–Meier methodology), mucosal healing at 8 weeks (defined as a UC‐DAI endoscopic subscore of 0 or 1, or alternatively a Rachmilewitz endoscopic index of < 4), adherence, global patient’s acceptability and adverse events |
|
| Notes | Study was funded by Ferring Pharmaceuticals Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized centrally by a computer‐generated randomization system |
| Allocation concealment (selection bias) | Low risk | To maintain the investigator‐blind trial design, sealed treatment boxes were identical in size and weight, and contained written instruction about the dosing arm to which the participant was assigned; investigators were unaware of this information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Only investigators were blinded in this trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants involved with the study are accounted for |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Unclear risk | The study appeared to be free of other sources of biases |
Forbes 2005.
| Study characteristics | ||
| Methods | Randomized non‐inferiority trial | |
| Participants | Adults with ulcerative colitis with mild‐to‐moderate relapse (N = 88) | |
| Interventions | Asacol 2 x 400 mg tablets 3 times/day (2.4 g/day, n = 42) or ipocol 2 x 400 mg tablets 3 times/day (2.4 g/day, n = 46) for 8 weeks | |
| Outcomes | Outcomes included clinical remission (investigator’s overall clinical assessment), modified St Mark’s Colitis Activity score, macroscopic and microscopic appearance of the rectum, and adverse events. Outcomes were evaluated at entry and weeks 2, 4, and 8. Tablet counts were performed by pharmacy departments to check compliance | |
| Notes | Lagap Pharmaceuticals Ltd provided all the drugs used for the study, and arranged the blinded packaging and the telephone randomization service. The company also monitored the conduct of the trials and appropriate documentation in the various centres to comply with Good Clinical Practice, together with providing modest running
expenses. Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Low risk | Centralized telephone randomization by Lagap Pharmaceuticals Ltd |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Study drug was provided in an anonymous blister package with instructions to take 2 x 400 mg tablets 3 times a day. The tablets themselves were not identical as they are somewhat different in shape. Participants were advised that they might find that they were prescribed a tablet shaped differently from those they had received before, but not that this was or was not Asacol or ipocol. Clinical investigators took care neither to see nor to enquire about the nature of the tablets |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | During the course of the study, 11 participants withdrew from the Asacol group, and 9 withdrew from the Ipocol group: reasons for withdrawal were not provided |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Gibson 2006.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy parallel‐group trial | |
| Participants | Adults (19 to 70 years) with mild to moderately‐active ulcerative colitis confirmed by standard endoscopic and histopathological criteria (N = 258) | |
| Interventions | Eudragit‐L‐coated mesalazine tablets (Salofalk 3 g/day, n = 131) or ethylcellulose‐coated mesalazine tablets (Pentasa 3 g/day, n = 127) for 8 weeks | |
| Outcomes |
Primary outcome: clinical remission (CAI < 4) Secondary outcomes: CAI; clinical improvement (clinical remission or improved CAI of > 3 from baseline), number of stools per week; number of bloody stools per week; time to first symptomatic remission; endoscopic remission (EI < 4); endoscopic improvement; histological remission; histological improvement; physician's global assessment; and adverse events |
|
| Notes | LOCF if participants withdrew early. Participants were assumed to be treatment failures if no CAI score was available. Adherence checked by tablet count The study was sponsored by Dr Falk Pharma GmbH (Freiburg, Germany) Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated using the program "Rancode +" |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, sealed, non‐transparent envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 43 participants were excluded from the per protocol analysis but it is not clear which groups they came from. ITT analysis was presented for the primary outcome |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Good 1992.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, randomized comparison of SASP and mesalamine. Each site was independently randomized in blocks of 6 | |
| Participants | People with endoscopically‐confirmed active ulcerative colitis (N = 117) | |
| Interventions | Mesalamine, 1 g/day (n = 27), 2 g/day (n = 31), or 4 g/day (n = 30) or SASP, 4 g/day (n = 29). Drugs were dispensed in blister packs according to a double‐dummy technique | |
| Outcomes | Clinical assessments were performed at entry, 4 weeks, and at 8 weeks Efficacy was rated according to positive changes in disease activity index and a physician's overall assessment | |
| Notes | Abstract ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Green 1998.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | Adults (18 to 80 years) with moderate‐to‐severely active ulcerative colitis confirmed by flexible sigmoidoscopy (N = 99) | |
| Interventions | Balsalazide (2.25 g 3 times daily: 6.75 g/day, n = 50) or Asacol (0.8 g 3 times daily: 2.4 g/day, n = 49) for 12 weeks | |
| Outcomes | Primary outcome: The proportion of participants achieving complete remission (based on diary card) by 12 weeks. Participants left the study at weeks 4 or 8 if they achieved complete remission. Complete remission was defined as none or mild symptoms, sigmoidoscopic grade of 0 or 1 and no use of rectal steroid foam. Other outcomes included participant and investigator satisfaction, laboratory assessments, median time to relief of symptoms, cumulative days free of symptoms, study dropouts, dropouts due to treatment failure and adverse events. Outcomes were evaluated at entry and weeks 2, 4, 8 and 12. Adherence was assessed at follow‐up visits | |
| Notes | Participants were provided with rectal steroid foam as relief medication for use as required Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: placebos of identical appearance to the Balsalazide capsules and mesalamine tablets were provided. Participants received 3 capsules (Balsalazide/placebo) and 2 tablets (mesalamine/placebo) 3 times daily |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 38% of the participants (38 of 101) did not complete the study (15 Balsalazide; 23 mesalamine), the main reason being treatment failure, which was more common in the mesalamine group (6 Balsalazide; 16 mesalamine; P = 0.015). Other reasons for withdrawal included noncompliance with the study protocol (6 Balsalazide, 3 mesalamine), unacceptable adverse events (1 Balsalazide, 1 mesalamine), and treatment with excluded medication (1 Balsalazide, 1 mesalamine). 3 participants (1 Balsalazide, 2 mesalamine) who were erroneously admitted into the study were also withdrawn; 1 receiving Balsalazide did not have UC, 1 receiving mesalamine was not using adequate contraception, and 1 receiving mesalamine was included into the study after the recruitment deadline had passed |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Green 2002.
| Study characteristics | ||
| Methods | Double‐blind and randomized | |
| Participants | Patients with acute relapse of ulcerative colitis and newly‐diagnosed patients (N = 57) | |
| Interventions | Sulfasalazine, 3 g daily (n = 29), or Balsalazide, 6.75 g daily (n = 28), according to a double‐dummy protocol for 12 weeks. Some participants were receiving concomitant oral or topical steroids | |
| Outcomes | 1. Remission rates at the end of the study or withdrawal 2. Treatment success or failure at the end of the study or withdrawal |
|
| Notes | This study was sponsored by Biorex Laboratories Limited Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number table |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant from the SASP group was lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Expected outcome were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hanauer 1993.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, placebo‐controlled, randomized, dose‐response trial conducted at 20 sites | |
| Participants | Adults, over 18 years old, with mild‐to‐moderate active ulcerative colitis confirmed by clinical and colonoscopic evidence with a score ≥ 5 on a 15‐point index, were selected from 06 March 1987 to 04 August 1988. Participants were stratified according to extent of disease. Therapies of steroids, SASP, or other mesalamine formulations were stopped at least 7 days before trial. Immunosuppressives were stopped at least 90‐days before study (N = 374) | |
| Interventions | Mesalamine (pentasa) 1 g (n = 92), 2 g (n = 97) or 4 g per day (n = 95), or placebo (n = 90), in 250 mg capsules in identical blister cards for 8 weeks. Loperamide (2 mg) was dispensed to participants when absolutely necessary for control of diarrhea | |
| Outcomes | In addition to daily patient diaries, clinical assessments and sigmoidoscopy were performed at weeks 1, 4, 8 or upon withdrawal Clinical improvement was assessed using the physician's global assessment, assessment of treatment failure, sigmoidoscopic index, biopsy score, participants' perceptions, and trips to the toilet. Induction of remission was assessed by more stringent criteria for physician's assessment, sigmoidoscopic index and biopsy score |
|
| Notes | Study was funded by Marion Merrell Dow Inc. Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered drug containers of identical appearance |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: study drug was supplied in 250 mg capsules in identical blister cards to ensure blinding of both the investigator and the participant |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 participants were lost to follow‐up. More participants withdrew from the placebo group due to insufficient therapeutic effect |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hanauer 1996.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, placebo‐controlled, randomized, dose‐ranging trial | |
| Participants | Patients from 24 centers with mild to moderately‐active ulcerative colitis. No anti‐diarrheals were allowed (N = 273) | |
| Interventions | Olsalazine, 2 g (n = 92) or 3 g per day (n = 91), or placebo (n = 90) for 12 weeks. Full dosage was reached after 1 week | |
| Outcomes | Assessments were performed at entry, 6 and 12 weeks (or upon termination) End points included induction of clinical remission (according to number of bowel movements and amount of blood in stool) and induction of endoscopic remission or endoscopic improvement (evaluated on a 5‐pt scale, where 0 or 1 indicated remission) |
|
| Notes | Abstract ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Expected outcomes were reported, Post hoc rescoring of endoscopic reports were reported for endoscopic remission |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hanauer 2005.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study (ASCEND II) | |
| Participants | Adults (aged 18 to 75 years) with moderately‐active ulcerative colitis confirmed by endoscopy or radiography (N = 386) | |
| Interventions | Asacol 2.4 g/day (400 mg tablet; n = 139) or 4.8 g/day of mesalamine (Asacol 800 mg tablet; n = 129) for 6 weeks | |
| Outcomes | Primary outcome: treatment success at 6 weeks defined as either complete remission or a clinical response to therapy. Complete remission was defined as complete resolution of: (i) stool frequency (normal stool frequency); (ii) rectal bleeding (no rectal bleeding); (iii) PFA score (generally well); (iv) endoscopy findings (normal), and a PGA score of 0. A clinical response to therapy was defined as improvement in the baseline PGA score and improvement in at least one other clinical assessment (stool frequency, rectal bleeding, PFA, endoscopy findings) and no worsening in any other clinical assessment Secondary outcomes: overall improvement at week 3, improvement from baseline in each of the clinical assessment subscores at weeks 3 and 6, overall improvement at week 6 in the subgroup of participants with ulcerative colitis limited to the left side of the colon (proctitis, proctosigmoiditis, or left‐sided colitis), time to normalization of stool frequency (based on the participant’s daily diary), time to resolution of rectal bleeding (based on the participant’s daily diary), and change from baseline in the UC‐DAI, and adverse events |
|
| Notes | The study was funded by Procter & Gamble Pharmaceuticals, Inc. (Cincinnati, OH), who also provided study drug for the investigation Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permutated block randomization scheme |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: identical placebos were used. Both participants and investigative staff were blinded to treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 18.7% of participants in 2.4 g/day group withdrew (26/139) compared to 12.4% of the 4.8 g/day group (16/129). More participants withdrew from the 2.4 g/day group due to lack of treatment effect |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hanauer 2007.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study (ASCEND I) | |
| Participants | Adults (aged 18 to 75 years) with mild to moderately‐active ulcerative colitis confirmed by endoscopy or radiography (N = 301) | |
| Interventions | Asacol 2.4 g/day (400 mg tablet; n = 154) or 4.8 g/day of Asacol (800 mg tablet; n = 147) for 6 weeks | |
| Outcomes | Primary outcome: treatment success at week 6. Secondary efficacy end points included the proportion of participants who improved from baseline at week 3 and the percentage of participants whose clinical assessment scores (stool frequency, rectal bleeding, sigmoidoscopy scores, PFA scores and PGA scores) improved from baseline scores at weeks 3 and 6, improvement in QOL from baseline to weeks 3 and 6, and time to symptom relief (stool frequency, rectal bleeding or both) and adverse events. Overall improvement or treatment success was defined as either complete remission or a clinical response to therapy. Complete remission was defined as normal stool frequency, no rectal bleeding, a PFA score of 0 (generally healthy), normal endoscopy findings and a PGA score of 0 (quiescent disease activity). A clinical response to therapy was defined as a decrease in the PGA score of at least one point from baseline, plus improvement in at least one other clinical assessment parameter (stool frequency, rectal bleeding, PFA or endoscopy findings) and no worsening in any of the other clinical assessments | |
| Notes | This study was supported by Procter & Gamble Pharmaceuticals Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permutated block randomization scheme |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: identical placebos were used. Both investigators and participants were blinded to treatment assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hetzel 1986.
| Study characteristics | ||
| Methods | Random, double‐blinded allocation of placebo or ADS. Participants were seen 1 week before trial, and weekly during treatment, and 6 weeks after completion of treatment | |
| Participants | People with mild‐to‐moderate exacerbation of ulcerative proctitis or left‐sided colitis (N = 30). None had evidence of a severe attack of colitis (i.e. no fever, tachycardia, hemoglobin < 10 g/l or ESR > 30 mm/h). Diagnosis confirmed by sigmoidoscopy, histology of rectal biopsies, radiological or colonoscopic appearance, and negative stool samples (for salmonella, shigella, campylobacter, Clostridium difficile). People known to be intolerant of SASP were included to determine whether their sensitivity extended to olsalazine sodium (ADS) | |
| Interventions | Disodium azodisalicylate (ADS, olsalazine sodium; n = 15), 2 g/day (1 g twice a day; 4 gelatin capsules; n = 15), or matching placebo with meals for 6 weeks | |
| Outcomes | Sigmoidoscopic appearances at weeks 0 and 6 were graded according to a 4‐point scale (Grade 0‐ normal mucosa; grade 1‐ mild mucosal hyperemia; grade 2 ‐moderately‐severe proctitis with granularity of mucosa; grade 3‐ severe proctitis with spontaneous bleeding and/or ulceration and/or pus). Rectal biopsies (also at weeks 0 and 6) were assessed by a single experienced observer. Comparisons between samples were classified as 'much improved', 'improved', 'unchanged' or 'worse' | |
| Notes | This study was supported by Pharmacia (Australia) Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number code |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: matching placebo |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hiwatashi 2011.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, parallel‐group study | |
| Participants | Patients (aged 15 to 64 years) with moderately‐active ulcerative colitis (modified Mayo score 6 to 8 points) (N = 123) | |
| Interventions | 2.25 g/day mesalazine (3 round 250 mg tablets, 3 times a day; n = 63) or 4.0 g/day mesalazine (4 oval 500 mg tablets, 2 times a day; n = 60) | |
| Outcomes | Primary outcome: Mean change in UC‐DAI Secondary outcomes: Mean change in each UC‐DAI variable (stool frequency, rectal bleeding, mucosal appearance, and physician’s overall assessment of disease), clinical remission, clinical improvement and adverse events |
|
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Biased‐coin minimization algorithm |
| Allocation concealment (selection bias) | Low risk | Centralized randomization by independent CRO |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: Study medication consisted of a round tablet containing 250 mg of mesalazine, an oval tablet containing 500 mg of mesalazine and placebo tablets identical in size and appearance to the study drugs |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 participants dropped out from the 2.25 g/day group and 1 participant dropped out from the 4.0 g/day group |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Ito 2010.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, placebo‐controlled trial | |
| Participants | Patients (aged > 16 to < 65 years) with mild to moderately‐active ulcerative colitis. Disease activity was assessed using the UC‐DAI (Sutherland 1987). Patients with mild‐to‐moderate active ulcerative colitis who had a score of 3 to 8 on the UC‐DAI with a bloody stool score of > 1 were eligible for the study (N = 229) | |
| Interventions | The objective of the study was to demonstrate the superiority of Asacol 3.6 g/day and non‐inferiority of Asacol 2.4 g/day against pentasa 2.25 g/day. Participants were randomized to Asacol 3.6 g/day (n = 65), Asacol 2.4 g/day (n = 66), pentasa 2.25 g/day (n = 65) or placebo (n = 33) for 8 weeks | |
| Outcomes | Participants were evaluated at baseline and week 8 or at early withdrawal Primary outcome: Reduction in UC‐DAI score from baseline Secondary outcomes: Reduction in each UC‐DAI item score, the proportion of participants achieving remission (a UC‐DAI score of < 2 and zero points for bloody stool score); the proportion of participants achieving efficacy (remission or participant who did not achieve remission but whose reduction of UC‐DAI score is > 2) |
|
| Notes | Study was supported by ZERIA Pharmaceutical Co., Ltd., Research and Development
Division Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Biased‐coin minimization algorithm |
| Allocation concealment (selection bias) | Low risk | Centralized randomization: A person independent from the study was in charge of the random allocation. The randomization code was sealed and stored until the blind was removed |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: the appearance of the medication was identical |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Jiang 2004.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy comparison of olsalazine and SASP | |
| Participants | Male and female patients (average age 32.6 years) with acute relapse of ulcerative colitis (N = 42) | |
| Interventions | Olsalazine 2 g/day (n = 21) or SASP 4 g/day (n = 21) for 8 weeks. Lopermide (1 to 2 pills/day) was given to participants unable to tolerate diarrhea but not for more than 10 days | |
| Outcomes | Clinical and laboratory examinations were performed at entry and after 1, 2, 4, 6 and 8 weeks of treatment. Colonoscopy and biopsy were performed 3 days before treatment and within 3 days of completion Outcomes included induction of complete remission (subsidence of clinical symptoms with a relatively normal mucous membrane on colonoscopy), induction of clinical remission (0 to 2 stools a day with no gross blood or red cells in stool), colonoscopic remission (evaluated on a 2‐ or 5‐point scale) and histological remission (evaluated on a 5‐point scale) |
|
| Notes | Study was supported by Youth Research Foundation of the PublicHealthBureau
of Shandong Province, No. 2001CA2EFB2 Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation of drugs was performed using a table of random numbers |
| Allocation concealment (selection bias) | Low risk | Participant |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number of participants who completed the trial was not reported |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kamm 2007.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, placebo‐controlled trial with an Asacol reference group | |
| Participants | Adults (aged > 18 years) with mild to moderately‐active ulcerative colitis (N = 341). New or relapsing cases of ulcerative colitis were included in the study. Ulcerative colitis was defined by symptomatic, radiographic and endoscopic criteria. Disease activity was assessed using a modified UC‐DAI (Sutherland 1987). People with mild‐to‐moderate active ulcerative colitis with a score of 4 to 10 on the UC‐DAI and a sigmoidoscopy score > 1 and a physician’s global assessment score < 2 with comparable histology were eligible for the study. To increase stringency, patients showing any mucosal friability were given a sigmoidoscopy score of at least 2. During the screening period patients were permitted to continue receiving a stable dose of mesalamine (< 2.0 g/day) if they were receiving this treatment prior to screening. This was withdrawn at baseline if the patient was found to be eligible for inclusion | |
| Interventions | MMX mesalamine 2.4 g/day (n = 84) or 4.8 g/day (n = 85) given once daily, Asacol 2.4 g/day (n = 86) given in 3 divided doses, or placebo (n = 86) | |
| Outcomes | Outcomes were evaluated at entry and week 8 or at early withdrawal. Primary outcome: the proportion of participants at week 8 in clinical and endoscopic remission (modified UC‐DAI of < 1 with rectal bleeding and stool frequency scores of 0, no mucosal friability, and a > 1 point reduction in sigmoidoscopy score from baseline) Secondary outcomes: the proportion of participants achieving clinical remission (a score of zero points for stool frequency and rectal bleeding); clinical improvement (a decrease > 3 points from baseline in modified UC‐DAI), changes in modified UC‐DAI score (baseline to week 8); changes in sigmoidoscopic appearance (baseline to week 8); and changes in rectal bleeding and stool frequency (from baseline to any study visit). Other secondary outcomes included an analysis of treatment failure rate, a comparison of time to withdrawal and adverse events |
|
| Notes | This study was supported by Shire Pharmaceuticals Inc. Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization: Participants were randomized centrally by an interactive voice response system |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kruis 1998.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | Adults (18 to 75 years) with a mild‐to‐moderate (endoscopic score < 4) attack of ulcerative colitis (N = 168) | |
| Interventions | Olsalazine 3 g/day (n = 88) or mesalazine (claversal) 3 g/day (n = 80) for 12 weeks | |
| Outcomes | Primary outcome: Endoscopic remission (defined as a score of 0 or 1 on the Rachmilewitz index) Secondary outcomes: Clinical remission (< 1 on modified Rachmilewitz index), physician's global assessment on 4‐point scale |
|
| Notes | This study was supported by a grant from Pharmacia & Upjohn AB, Uppsala, Sweden Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 25% dropout rate, but dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kruis 2003.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind trial | |
| Participants | Adults (aged 18 to 70 years) with mild‐to‐moderate (CAI 6 to 12; EI > 4) attack of UC with at least 1 previous episode or persistently bloody diarrhea at least 14 days preceding entry (N = 316) | |
| Interventions | Mesalamine (Salofalk pellets) 1.5 g/day (0.5 g 3 times daily; n = 103); 3.0 g/day (1.0 g 3 times daily; n = 107) or 4.5 g/day (1.5 g 3 times daily; n = 106) for 8 weeks | |
| Outcomes | Primary outcome: Clinical remission (CAI < 4) Secondary outcomes: Endoscopic remission (EI < 4); endoscopic improvement (reduction of EI by at least 1 point); clinical improvement (CAI decreased by at least 3 points), life quality index; physician's global assessment; and adverse events |
|
| Notes | This study was supported by Dr. Falk Pharma GmbH, Freiburg, Germany Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The drug was dispensed by sachets containing mesalamine pellets or a mixture of mesalamine and placebo pellets. The pellets with active drug and placebo pellets were identical in outward appearance. To ensure blindness, the sachets of the 3 different dose groups contained the same number and volume of pellets. In the sachets with the highest dose all pellets consisted of the active drug |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout rate in 1.5 g/day group was 32.0% (33/103) compared to 19.6% (21/107) in the 3.0 g/day group and 19.8% (21/106) in the 4.5 g/day group. The most frequent reason for premature termination was inefficiency of treatment (23%, 17%, and 13%, respectively). No other reasons for withdrawal were provided |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kruis 2009.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy, parallel‐group, multicenter, phase III non‐inferiority study assessing the efficacy and safety of mesalazine (Salofalk granules) 3.0 g once‐daily dosing versus 1 g 3 times daily dosing for the treatment of active ulcerative colitis | |
| Participants | Adults (aged 18 to 75 years) with active ulcerative colitis (CAI ≥ 6 and EI ≥ 4; Rachmilewitz criteria) were recruited from 54 centers in 13 countries for an 8‐week induction trial (N = 380) | |
| Interventions | Mesalazine 3.0 g once daily (n = 191) or 1 g three times daily (n = 189) Adherence with study medication was checked by counting the medication returned at study visits |
|
| Outcomes | Primary outcome: Clinical remission at the end of the study (defined by CAI < 4) Secondary outcomes: Clinical improvement (decrease in CAI by at least 1 point baseline), disease activity index (DAI) , EI, histological index (HI, based on Riley), time to first resolution of clinical symptoms, PGA and participant preference |
|
| Notes | This study was funded in full by Dr Falk Pharma, Freiburg, Germany Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Levine 2002.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, dose‐response, parallel‐group study | |
| Participants | Adults (aged 18 to 80 years) with mild to moderately‐active ulcerative colitis confirmed by flexible sigmoidoscopy (N = 154) | |
| Interventions | Balsalazide 6.75 g/day (n = 35), Balsalazide 2.25 g/day (n = 35) or Asacol 2.4 g/day (n = 36) for 8 weeks | |
| Outcomes | Primary outcome: Difference between treatment groups in rectal bleeding and in at least one other symptom. Improvement was defined as improvement in at least one category of the disease activity scale (i.e. normal, mild, moderate, severe) Secondary outcomes: Remission status (normal stool frequency and no blood in stool for 48 hours before visit, physician’s global assessment score of quiescent and a sigmoidoscopy score of mild or normal), rectal biopsy score, and IBDQ score |
|
| Notes | For the purposes of this review we used only the comparison between Balsalazide 6.75 g and Asacol 2.4 g (i.e. equimolar doses) Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: Placebos were identical in appearance to the Balsalazide capsules and mesalamine (Asacol) tablets |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 31% dropout rate. Dropouts appear to be balanced across intervention groups. More participants withdrew from the low‐dose Balsalazide and mesalamine groups due to lack of therapeutic effect than the high‐dose Balsalazide group |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Lichtenstein 2007.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, placebo‐controlled trial | |
| Participants | People with newly‐diagnosed or relapsing (relapsed < 6 weeks prior to entry) mild to moderately‐active ulcerative colitis (modified UC‐DAI score of 4 ‐ 10, with a sigmoidoscopy score > 1 and a PGA score < 2 with compatible histology) (N = 262) | |
| Interventions | Participants were randomized to MMX mesalamine 4.8 g/day (n = 94) given once daily, 2.4 g twice daily (n = 93), or placebo (n = 93) for 8 weeks | |
| Outcomes | Outcomes were evaluated at the screening visit (week –1) baseline (week 0), week 2, week 4 and week 8 or at early withdrawal Primary outcome: Clinical and endoscopic remission at week 8 (modified UC‐DAI of < 1 with rectal bleeding and stool frequency scores of 0, no mucosal friability, and a > 1 point reduction in sigmoidoscopy score from baseline) Secondary outcomes: Clinical remission (a score of zero points for stool frequency and rectal bleeding); clinical improvement (a decrease > 3 points from baseline in modified UC‐DAI), changes in modified UC‐DAI score (baseline to week 8); changes in sigmoidoscopic appearance (baseline to week 8); and changes in rectal bleeding and stool frequency (from baseline to any study visit). Other secondary outcomes included an analysis of treatment failure rate, a comparison of time to withdrawal and adverse events |
|
| Notes | This study was supported by Shire Pharmaceuticals Inc. Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Participants were randomized centrally by an interactive voice response system |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. MMX mesalamine and placebo tablets were identical in appearance |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal. There were a higher number of withdrawals in the placebo group due to lack of efficacy |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Maier 1985.
| Study characteristics | ||
| Methods | Randomized controlled trial | |
| Participants | People with active inflammatory bowel disease (ulcerative colitis n = 30, or Crohn's disease n = 30) | |
| Interventions | Oral 5‐ASA, 0.5 g 3 times daily (n = 15) or oral SASP, 1.0 g 3 times daily (n = 15) for 8 weeks | |
| Outcomes | Remission and clinical improvement | |
| Notes | Study also enrolled 30 participants with Crohn's disease Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | Not described |
| Other bias | Unclear risk | Not described |
Mansfield 2002.
| Study characteristics | ||
| Methods | Randomized, multicenter, double‐blind, parallel‐group study. Clinical and laboratory examinations were performed at recruitment, and weeks 2, 4 and 8 | |
| Participants | Adults with newly‐diagnosed or recently‐relapsed ulcerative colitis confirmed by sigmoidoscopy in conjunction with a negative stool culture (N = 50) | |
| Interventions | Sulfasalazine, 3 g daily (n = 24), or Balsalazide, 6.75 g daily (n = 26) according to a double‐dummy protocol for 8 weeks | |
| Outcomes | Clinical and sigmoidoscopic remission. Remission was defined as a stool frequency ≤ 2 a day without blood and with a sigmoidoscopic appearance of normal rectal mucosa or minimal erythema | |
| Notes | The study was initially sponsored by Biorex Laboratories Ltd Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy, identical gelatine capsules |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up. More participants were withdrawn from the SASP group due to adverse events than the Balsalazide group. Othe dropouts were balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Marakhouski 2005.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | Adults (18 to 70 years) with mild to moderately‐active ulcerative colitis (N = 233) | |
| Interventions | Mesalazine pellets (Salofalk; n = 115) or mesalazine tablets (n = 118) at an initial dose of 1.5 g/day. In case of inadequate response the dose could be increased up to 3 g/day after the first follow‐up visit at 2 weeks. Participants were treated for 8 weeks |
|
| Outcomes | Primary outcome: Complete response (clinical remission) defined as CAI < 4 at individual study end Secondary outcomes: Time to first response; endoscopic remission (defined as EI < 4) and improvement; histological improvement; and PGA |
|
| Notes | This study was supported by a grant from Dr. Falk Pharma GmbH, Freiburg, Germany Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: placebos of identical appearance to 5‐ASA tablets and pellets were used to ensure double‐blind performance of the trial |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 13.5% dropout rate. Dropouts were balanced across groups. Reasons for dropping out were summarized across both groups |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Miglioli 1990.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel dose‐response study | |
| Participants | Adults (aged 18 to 65 years) with clinically mild active ulcerative colitis based on Truelove and Witts criteria (Truelove 1955) (N = 73) | |
| Interventions | Mesalazine (Asacol 400 mg tablets) at daily doses of 1.2 g (n = 25), 2.4 g (n = 24) or 3.6 g (n = 24) for 4 weeks | |
| Outcomes | Clinical remission or improvement, endoscopic and histological improvement. Clinical remission was defined as no more than 2 bowel movements a day with no visible blood in the stool in the symptomless participant. Clinical improvement defined as a clear decrease in severity of symptoms and signs not satisfying remission criteria | |
| Notes | The study was supported by Giuliani SpA and Bracco, SpA, Italy Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: identical placebo tablets |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 11 participants did not complete the study (5 in 1.2 g/day group; 4 in 2.4 g/day group; and 2 in 3.6 g/day group because of worsening of disease in 5, lack of improvement in 4 and loss to follow‐up and intercurrent disease in 1). It is not clear which reasons apply to each group |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Mihas 1988.
| Study characteristics | ||
| Methods | A prospective, controlled, double‐blind trial | |
| Participants | Adults (18 year or older) with exacerbated ulcerative colitis (N = 19) | |
| Interventions | Oral 5‐ASA 0.8 g 3 times a day (2.4g/day, n = 7) vs sulfasalazine 1g 3 times a day (3g/day, n = 12) for 4 weeks | |
| Outcomes | Response to treatment was based on endoscopic appearance, subjective symptoms, objective criteria and laboratory findings | |
| Notes | Abstract publication only ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | A prospective double‐blind trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2/12 participants from sulfasalazine group were unable to complete the study because of adverse events |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Munakata 1995.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, double‐dummy comparison of SASP and mesalazine | |
| Participants | Patients, 16 years and older, with mild to moderately‐active ulcerative colitis were enrolled from July 1992 to March 1994 (N = 109) | |
| Interventions | Controlled‐release mesalazine, 1.5 g/day plus SASP‐matched placebo (n = 52) or active SASP, 3 g/day, with mesalazine‐matched placebo (n = 57), for 4 weeks | |
| Outcomes | Clinical and endoscopic assessment was performed at entry, and after 2 and 4 weeks Improvement was assessed as changes in clinical status based on disease activity and severity of symptoms, compared to baseline findings Improvement was also measured by endoscopic findings |
|
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization Randomization was under the direction of a central controller |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 9 participants dropped out of the study |
| Selective reporting (reporting bias) | Unclear risk | Not described |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Pontes 2014.
| Study characteristics | ||
| Methods | Randomized, double‐blind, placebo‐ and active‐controlled proof‐of‐concept study | |
| Participants | Adults (18 to 65 years) with mild‐to‐moderate active ulcerative colitis (Total Mayo score (TMS) >5 and <10, ) confirmed by endoscopy (N = 34) | |
| Interventions | Dersalazine 3 x 400 mg twice a day (2.4 g/day, n = 13), mesalazine 3 x 400 mg twice a day (2.4 g/day, n = 8), or placebo (n = 13) for 4 weeks | |
| Outcomes | Primary safety outcome: Proportion of participants with AEs of severe intensity or treatment withdrawal Secondary safety outcomes: proportion of participants with AEs, AEs with suspected relationship to study medication, and with clinically relevant abnormalities in laboratory tests or physical examination Secondary efficacy outcomes: Change in TMS from baseline to week 4, change in partial Mayo score (PMS) from baseline to weeks 2 and 4, complete remission, clinical remission, TMS clinical response and mucosal healing rates by week 4, and PMS clinical response by weeks 2 and 4 |
|
| Notes | Study was supported by Palau Pharma S.A. Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list in blocks of 4 with a ratio of 2:1:1 (dersalazine sodium:mesalazine:placebo) |
| Allocation concealment (selection bias) | Low risk | Centrally randomized |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The treatments had indistinguishable appearance and were uniquely identified with a randomization number according to a computer‐generated randomization list |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants did not complete the 4‐week treatment (3 from placebo group, and 2 from dersalazine group) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | They study appears to be free of other sources of bias |
Pruitt 2002.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | People (aged 12 to 80 years) with mild to moderately‐active ulcerative colitis confirmed by flexible sigmoidoscopy (N = 173) | |
| Interventions | Balsalazide 6.75 g/day (n = 84) or Asacol 2.4 g/day (n = 89) for 8 weeks | |
| Outcomes | Primary outcome: Proportion of participants in symptomatic remission (based on diary card) at the end of week 8 or at early completion of treatment. Symptomatic remission was defined as PFA rating of normal or mild and absence of rectal bleeding Secondary outcomes: Time to symptomatic remission, proportion of participants in complete remission (symptomatic remission plus sigmoidoscopic evaluation score of normal or mild), improvement in sigmoidoscopic evaluation score, change from baseline in PGA of disease activity at week 8 or early completion and adverse events |
|
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: each study drug treatment was administered 3 times daily as 3 capsules (Balsalazide active drug or placebo) and 2 tablets (Asacol active drug or placebo) to maintain blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Qian 2004.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | Adults (aged 18 to 70 years) with active ulcerative colitis (N = 56) | |
| Interventions | Olsalazine (250 mg capsules: 4 capsules twice daily; n = 31) or SASP (250 mg tabletss, 4 tablets 4 times daily; n = 25) for 8 weeks | |
| Outcomes | Clinical improvement and adverse events | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐stratified randomization |
| Allocation concealment (selection bias) | Low risk | Pharmaceuticals were packed and encoded according to random numbers. The encoding process was monitored by the staff from Shanghai Pharmaceutical Affairs Bureau |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants from SASP group were unable to complete the study |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Rachmilewitz 1989.
| Study characteristics | ||
| Methods | Randomized, double‐blind parallel‐group comparison of mesalazine versus SASP. Drugs were centrally packaged and labelled. Entry assessment involved physical exam, history, colonoscopy, and lab tests. In addition to participant diaries, assessments, including lab test, urine analysis, blood counts and liver/kidney function tests, were performed at bi‐weekly follow‐ups. Mandatory repeat colonoscopy was performed after week 8 | |
| Participants | Outpatients, aged 18 to 70 years, at 46 centres in 7 countries, with active mild‐to‐moderate ulcerative colitis (N = 220) | |
| Interventions | Coated mesalazine (Mesasal), 1.5 g/day (n = 115), or SASP 3 g/day (n = 105) for 8 weeks in a double‐dummy manner. Compliance was monitored by pill counts | |
| Outcomes | Clinical/endoscopic remission was defined as a clinical/endoscopic activity index score < 4. Improvement was also assessed as changes in frequency and consistency of stools, and blood in stools The incidence of adverse effects was also tabulated | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated Participants were randomised in groups of 4 according to a predetermined list generated by a computer |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Raedler 2004.
| Study characteristics | ||
| Methods | Phase 2, multicenter, randomized, double‐blind, double‐dummy, parallel‐group study | |
| Participants | Adults (18 to 75 years) with recurrent mild to moderately‐active ulcerative colitis (N = 362) | |
| Interventions | 3 g/day mesalazine in sachets of micropellets (1.5 g sachet taken twice daily with liquid, n = 181) or tablets (Claversal 500 mg; 2 tablets taken 3 times daily, n = 181) for 8 weeks Adherence assessed by tablet and sachet counts |
|
| Outcomes | Primary outcome: Clinical remission (sum of CAI components 1 to 4 based on Rachmilewitz was CAI < 2) within 8 weeks of treatment Secondary outcomes: Complete clinical remission (sum of CAI components 1 to 7 was < 4), endoscopic remission (EI based on Rachmilewitz was < 2) |
|
| Notes | This study was funded by a grant from Merckle Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: active drug and the matching placebo were identical in appearance, form, smell and taste. Medication labels were identical for both treatments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Rao 1989.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy, multicenter comparison of Olsalazine and SASP. At entry and at 4 weeks, participants were assessed clinically, by sigmoidoscopy, rectal biopsy, blood tests, stool samples and urine analysis. Participants also kept stool diary records | |
| Participants | Outpatients with a first attack of mild to moderately‐severe ulcerative colitis, confirmed by sigmoidoscopic and histologic evidence and negative stool cultures (N = 37) | |
| Interventions | Olsalazine, 2 g/day (n = 20), or enteric‐coated SASP, 3 g/day (n = 17), provided in sealed blister packs, administered 4 times a day. Full dosage was reached after 7 days and continued for 4 weeks. Double‐dummy technique required each participant to take a physically indistinguishable dummy containing mainly potato starch. Compliance was confirmed by pill counts | |
| Outcomes | Changes in daily stool frequency and consistency, sigmoidoscopic and histological appearance, and clinical assessments were defined as 'improved' (an increase by at least 1 point), 'unchanged' or 'worsened'. Remission was defined as the lack of blood in stool, no more than 2 bowel movements a day, and no systemic disturbance. Overall improvement was defined as a positive change in at least 2 of the above criteria | |
| Notes | Pharmacia Limited supplied the double dummy packs containing olsalazine
capsules and sulphasalazine tablets Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. Participants received Olsalazine or sulphasalazine along with physically‐indistinguishable dummies. The drugs were provided in sealed blister packs |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 participants in the Olsalazine group did not complete the study, compared with 4 participants in the SASP group. Reasons for withdrawal were not given |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Rijk 1991.
| Study characteristics | ||
| Methods | Prospective, double‐blinded, multicenter trial comparing Olsalazine and Sulfasalazine. Participants were centrally randomized | |
| Participants | People with active ulcerative colitis (N = 55) | |
| Interventions | 6 g/day SASP (n = 28) or 3 g/day Olsalazine (n = 27) in externally‐indistinguishable capsules, for 6 weeks | |
| Outcomes | Remission was assessed on the basis of clinical and endoscopic criteria. Withdrawals and occurrence of adverse events were also measured | |
| Notes | Abstract ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: externally‐indistinguishable capsules |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 participants from each group were withdrawn because of adverse events or increasing severity of disease |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Riley 1988.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy comparison of mesalamine and SASP. History, physical, blood counts, urine samples, sigmoidoscopy and biopsy were performed upon entry | |
| Participants | Adult outpatients with mild‐to‐moderate ulcerative colitis relapse or first attack, recruited from 3 hospitals in close geographical proximity. All were passing blood at least once a day and all had hemorrhagic rectal mucosa (N = 60) | |
| Interventions | SASP 2 g/day (n = 20), delayed‐release mesalazine (Asacol), 800 mg/day (n = 20), or Asacol 2.4 g/day (n = 21). Each participant received 3 sets of tablets (2 placebo and 1 active) in a double‐dummy method | |
| Outcomes | In addition to daily diaries, participants were assessed at 2 and 4 weeks and any other time they wished. At 4 weeks, clinical assessment, biopsy and sigmoidoscopy were repeated Stool frequency, rectal bleeding, sigmoidoscopic, and histologic measures were used for comparison of groups. Withdrawals and adverse events were also measured |
|
| Notes | Financial support for this study was provided by Tillotts Laboratories, UK Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization Medications were centrally prepackaged and randomly distributed to each centre |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant dropped out of the SASP group |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Robinson 1994.
| Study characteristics | ||
| Methods | Double‐blind, randomized, single‐center trial. | |
| Participants | People with acute attacks of mild‐to‐moderate ulcerative colitis. No concomitant medications for UC were allowed (N = 98) | |
| Interventions | Olsalazine, 3 g/day, or placebo for 28 days | |
| Outcomes | Participant evaluations were performed at days 14 and 28 for clinical and laboratory parameters Efficacy was based on evaluations of diarrhea, rectal bleeding, mucorrhea, sigmoidoscopic score, nausea, abdominal tenderness, stool consistency, and global disease severity rating compared to baseline status |
|
| Notes | Abstract ‐ funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Sandborn 2009.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, active‐controlled trial (ASCEND III) | |
| Participants | Adults (aged 18 to 75 years) with moderately‐active ulcerative colitis that extended proximally beyond 15 cm from the anal verge, as confirmed by flexible sigmoidoscopy or colonoscopy (N = 772) | |
| Interventions | Asacol 2.4 g/day (400 mg tablet; n = 383) or 4.8 g/day of mesalamine (Asacol 800 mg tablet; n = 389) for 6 weeks | |
| Outcomes | Primary outcome: treatment success (overall improvement) at week 6, defined as improvement in the PGA (based on clinical assessments of rectal bleeding, stool frequency, and sigmoidoscopy), with no worsening in any individual clinical assessment Secondary outcomes: clinical remission at weeks 3 and 6; improvement in stool frequency, rectal bleeding, and PFA assessments at weeks 3 and 6; improvement in the sigmoidoscopy with CFT, PGA, and UC‐DAI assessments at week 6; and treatment success in participants with left‐sided disease at week 6 |
|
| Notes | This study was supported by Procter & Gamble Pharmaceuticals Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The investigator or designated representative telephoned the Interactive Voice Response System for patient randomization and allocation of study medication once the patient was determined to be eligible for the study |
| Allocation concealment (selection bias) | Low risk | Interactive Telephone Voice Response System |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy, identical placebos |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Sandborn 2012.
| Study characteristics | ||
| Methods | Phase 3, multicenter, randomized, double‐blind, double dummy, placebo‐controlled trial | |
| Participants | Adults (18 to 75 years of age) with active, mild‐to‐moderate ulcerative colitis for at least 6 months, with UC‐DAI score of 4 ‐ 10 points (N = 489) | |
| Interventions | Budesonide MMX 9 mg/day (n = 123), budesonide MMX 6 mg/day (n = 121), mesalamine (Asacol 2.4 g/day, as reference, n = 124), or placebo (n = 121) for 8 weeks | |
| Outcomes | Primary outcome: Combined clinical and endoscopic remission at week 8. Remission was defined as combined clinical and endoscopic remission with a UC‐DAI score < 1 point, with subscores of 0 for both rectal bleeding and stool frequency, no mucosal friability on colonoscopy, and a > 1‐point reduction from baseline in the endoscopic index score Secondary outcomes: Clinical improvement (> 3‐point reduction in UC‐DAI), endoscopic improvement (> 1‐point reduction in the UC‐DAI mucosal appearance subscore), symptom resolution (score of 0 for both rectal bleeding and stool frequency subscores from the UC‐DAI), histologic healing (histologic score of < 1 (corresponding to a histologic activity grade of 0) according to the Saverymuttu scale, and adverse events |
|
| Notes | This study was supported by Santarus, Inc, and Cosmo Pharmaceuticals SpA Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization for this study was developed by an external contractor and administered centrally |
| Allocation concealment (selection bias) | Low risk | The interactive voice response system was used to centrally randomize participants to study drug |
| Blinding (performance bias and detection bias) All outcomes | Low risk | A double‐dummy procedure was used to maintain blinding, with participants in each treatment group receiving their blinded study drug 3 times daily |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 140 participants were unable to complete the study (34 from budesonide 9 mg daily, 32 from budesonide 6 mg daily, 29 from Asacol 2.4 g/day, and 45 from placebo group) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported in the published study |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Scherl 2009.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, placebo‐controlled trial | |
| Participants | Acute are of mild‐to‐moderate active UC; baseline Modified Mayo Disease Activity Index (MMDAI) score between 6 and 10 (Table 1), inclusive (e.g., mild to moderately‐active UC) with an individual subscale score = 2 for rectal bleeding and mucosal appearance; disease extending at least 20 cm from the rectum on screening endoscopy /sigmoidoscopy; had not taken = 6.75 g / day of Balsalazide, or greater than 2.4 g / day of mesalamine or equivalent daily dose of any other 5‐ASA product during the 14 days before the initiation of study medication (n = 250) Participants assessment included MMDAI (deletion of friability from endoscopy score equal to 1), and physical exam, laboratory tests and participant diary cards |
|
| Interventions | Balsalazide 3.3 g/day (n = 167) or matching placebo (n = 83) | |
| Outcomes | Participants were assessed at screening visit, baseline, day 7, day 14, day 28 and day 56 and follow‐up Primary outcome: Clinical improvement (≥ 3‐point improvement in MMDAI) and improvement in the rectal bleeding (≥ 1 point improvement) at week 8 or end of treatment. Clinical improvement was defined as a ≥ 3 point improvement from baseline in the total MMDAI score and a ≥ 1 point improvement from baseline in the rectal bleeding subscale of the MMDAI Secondary outcomes: Clinical remission, defined as a score of 0 for rectal bleeding and a combined score of ≤ 2 for bowel frequency and physician's assessment using the MMDAI subscales, at week 8 or end of treatment; proportion of participants who experienced mucosal healing, defined as an endoscopy or sigmoidoscopy score of 0 or 1 at week 8 or end of treatment; proportion of participants with improvement ( ≥ 1 point improvement) from baseline to week 8 or end of treatment in the MMDAI subscale of mucosal appearance, bowel frequency, rectal bleeding, and physician's assessment; proportion of participants achieving complete remission, defined as a MMDAI score of ≤ 1, at week 8 or end of treatment; and mean change from baseline to week 8 or end of treatment for the MMDAI score |
|
| Notes | The study was funded by Salix Pharmaceuticals Author conflicts of interest are reported in the manuscript |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized, automated, validated interactive voice response system |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: All tablets were identical in appearance. Both the investigator and participant were blinded to assigned treatment throughout the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Schroeder 1987.
| Study characteristics | ||
| Methods | Placebo‐controlled, double‐blinded, and randomized | |
| Participants | People, age 15 to 70 years, with mild‐to‐moderate ulcerative colitis seen at the Mayo Clinic (Rochester, Minn.) from 01 September 1984 to 28 February 1986 (N = 87). UC was defined by symptomatic, radiographic, endoscopic criteria. Colonic involvement was determined by flexible proctosigmoidoscopy with double‐contrast x‐ray films of colon or complete colonoscopy, or both. Newly‐ or previously‐diagnosed cases were included. Participants receiving corticosteroids or SASP were required to stop such therapy at least 1 week prior to start of study. Pre‐entry evaluations included history, physical, blood count, chemistry screening, urinalysis, stool sample (had to be negative for ova, parasites, enteric pathogens) Participant population was stratified into 4 strata: 1‐ previous treatment, left‐sided disease; 2‐ previous treatment, universal disease; 3‐ no previous treatment, left‐sided disease; 4‐ no previous treatment, universal disease |
|
| Interventions | Asacol tablets (400 mg of 5‐ASA, coated with pH‐sensitive polymer Eudragit‐S which dissolves at pH 7 or higher) or matching placebo (500 mg microcellulose with identical pH‐sensitive coating, n = 38) 4.8 g/day (n = 38) or 1.6 g/day (latter dose only used in stratum 1, n = 11), 12 tablets daily for 6 weeks. No pill count, but participants were asked about compliance |
|
| Outcomes | Evaluation occurred at 3 weeks and 6 weeks Clinical response, described as 'complete', 'partial', or 'no response', was determined on the basis of stool frequency, amount of rectal bleeding, and PGA (which included sigmoidoscopic appearance) on 4‐point scales, compared to baseline data. 'Complete response' indicated resolution of all symptoms. Occurences of adverse reactions was also tabulated | |
| Notes | Early termination of treatment for any reason was deemed to constitute treatment failure This study was supported by Tillotts Laboratories, UK Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization sequence was developed by the Section of Medical Research Statistics, Rochester Methodist Hospital |
| Allocation concealment (selection bias) | Low risk | Centralized randomization according to a sequence used by the dispensing pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: matching placebo |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | More placebo participants (n = 16) did not complete the study than 5‐ASA participants (n = 5). Placebo participants were more likely to drop out due to flare of UC or no improvement |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Sninsky 1991.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, placebo‐controlled, computer‐randomized trial involving 5 university‐based medical centers, 1 IBD center, and 3 private‐practice sites. | |
| Participants | Adults, ages 18 to 75 years, with mildly‐ to moderately‐active ulcerative colitis were enrolled from November 1988 to June 1989 (N = 158). Diagnosis by symptomatic, radiographic, and endoscopic criteria had to have been confirmed by colonoscopy, proctosigmoidoscopy or barium enema within 24 months of start of study. Cases of both newly‐ and previously‐diagnosed disease showing continued active signs, despite SASP therapy were included. Steroid therapy had to be stopped at least 1 month before start of study; SASP and topical rectal therapies were discontinued at least 1 week before start. Concomitant use of corticosteroids, aspirin, NSAIDs, metronidazole, 6‐mercaptopurine, azathioprine, cyclosporine, or other investigational drugs was not permitted Participants were not stratified according to clinical characteristics. Initial participant evaluation and follow‐up exams consisted of lab tests, flexible proctosigmoidoscopy and radiographic films or colonoscopy at entry, followed by sigmoidoscopy at 3 and 6 weeks |
|
| Interventions | 1.6 g/day (n = 53) or 2.4 g/day (n = 53) oral mesalamine (Asacol) in 400 mg tablets coated with pH‐sensitive polymer (Eudragit‐S) or matching placebo tablets (n = 52) containing microcellulose. Compliance was checked by pill count at each visit and by review of participant diaries |
|
| Outcomes | Clinical grading was based on stool frequency, rectal bleeding, sigmoidoscopic findings, and PFA, each on 4‐point scale, which together gave the PGA, also on a 4‐point scale. The change in this clinical grade was indicated by classifying each participant as being 'in remission', 'improved', 'maintained', or 'worsened'. Withdrawals and adverse events were also reported | |
| Notes | This study was supported by a clinical grant from Norwich Eaton Pharmaceuticals Inc., Norwich, New York Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: matching placebo |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Sutherland 1990.
| Study characteristics | ||
| Methods | Double‐blind, placebo‐controlled, multicenter, parallel trial with random allocation of placebo or drug | |
| Participants | Patients were initially screened with a baseline history, physical exam, and flexible sigmoidoscopy or colonoscopy in order to calculate the activity index Men and non‐pregnant women, at least 18 years of age, with ulcerative colitis of variable extent, from 5 American and 2 Canadian centers and all enrolled between July 1985 and September 1986 (n = 136). Ulceration had to extend at least 20 cm proximal to the anus. Participants had to have a minimum score of 4 measured by DAI (4 subgroups for each of bowel frequency, presence of blood, sigmoidoscopic appearance, and physician's assessment of severity for a maximum score of 12) | |
| Interventions | Random allocation of Rowasa (250 mg tablets) taken as 4 tablets, 4 times a day, for a total of either 4 g/day (n = 47) or 2 g/day (n = 45), and an identical‐appearing placebo (n = 44) for 6 weeks. Compliance was measured by pill counts | |
| Outcomes | Follow‐up was assessed by telephone contact at end of week 1, 2, 4 and 5 and by clinical exam at the ends of weeks 3 and 6. Each clinic visit included flexible sigmoidoscopy and a PGA Efficacy was assessed by changes in the DAI and PGA. The change in PGA was described as 'much or somewhat improved', 'unchanged', or 'somewhat worse or much worse'. The change in the DAI score was evaluated by end‐of‐study score minus 'baseline' | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | All assignments to treatment and subsequent assessments of response to treatment were under double‐blind conditions |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: identical placebo |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 34% dropout rate, but dropouts appear to be balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Tursi 2004.
| Study characteristics | ||
| Methods | Multicenter, randomized trial | |
| Participants | Adults (19 to 69 years) with mild‐to‐moderate active ulcerative colitis confirmed by endoscopic evaluation (N = 90) | |
| Interventions | Balsalazide 4.5 g/day (n = 30) or Balsalazide 2.25 g/day + VSL#3 (n = 30) or Asacol 2.4 g/day (n = 30) for 8 weeks | |
| Outcomes | Primary outcome: Symptomatic remission based on clinical evaluation and diary card at 2, 4 and 8 weeks. Symptomatic remission was defined as PFA ratings of normal bowel movements and absence of rectal bleeding Secondary outcomes: Time to symptomatic remission, the proportion of participants achieving improvement in endoscopic evaluation score at 8 weeks, change in CAI from baseline at 8 weeks, improvement in histology at 8 weeks, and adverse events |
|
| Notes | For the purposes of this review we used only the comparison between Balsalazide 4.5 g/day and Asacol 2.4 g/day (n = 60) This study was supported by departmental sources Conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label. Physicians and participants were not blinded. Histological specimens were examined and graded for inflammation by 1 histopathologist blind to the treatment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4 participants withdrew from the Balsalazide group (13%) compared to 8 from the Asacol group (26%). Reasons for withdrawal are similar, except that 2 participants from the Asacol group withdrew for adverse events |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Willoughby 1988.
| Study characteristics | ||
| Methods | Randomized, double‐dummy, multicenter comparison of SASP and Olsalazine | |
| Participants | Out‐patients with mild to moderately‐active ulcerative colitis, either first attack or relapse (N = 56) | |
| Interventions | Oral sulphasalazine, 3 g/day (n = 30), or oral olsalazine, 3 g/day (n = 26), each in divided doses. Dose escalation schedule was used for first week of treatment after which full‐dose therapy continued for further 4 weeks. Tablets were counted to monitor compliance | |
| Outcomes | As well as diary cards, participants were clinically assessed upon entry, after 2 weeks, and after 5 weeks. Biopsy, sigmoidoscopy, and lab tests were performed at entry and after week 5 Clinical response was evaluated as changes in stool frequency and loss of blood and mucus from stools. Sigmoidoscopic and histological assessments were considered to have improved if score on a standard scale increased by at least 1 point (Dick 1964). Withdrawals and adverse effects were also tabulated | |
| Notes | Prarmacia UK Ltd. supplied the active and placebo drugs used in this study Funding support and conflicts of interest were not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomization was not described Randomization was restricted in blocks of four to ensure approximately equal numbers of patients allocated to each form of treatment |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts appear to be balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Zinberg 1990.
| Study characteristics | ||
| Methods | Double‐blind, placebo‐controlled trial | |
| Participants | Men and women, 18 to 75 years of age, with mild‐to‐moderate ulcerative colitis ‐ visible blood in the stool and disease involvement of 15 cm or more above the anal verge as defined by flexible sigmoidoscopy or colonoscopy (N = 15). The exacerbation could be a first instance or relapse of established disease. At least 3 days prior to participation, SASP, antidiarrheal agents, antispasmodics, and anticholinergics were discontinued. Oral or rectal steroids were not permitted within 1 week of study entry and other immunosuppressants were not permitted within 1 month of study. Concomitant medications not permitted during the study included NSAIDs, salicylates, digitalis derivatives, tranquilizers, and anti‐depressants At initial patient interview, history and physical exam were performed including baseline laboratory studies. Urine analysis for enteric pathogens was also performed |
|
| Interventions | Olsalazine (Pharmacia) in opaque gelatin capsules, each of 250 mg (n = 7) or indistinguishable placebo capsules (n = 8) in identical containers, 12 capsules/day (3 with each meal and 3 at bedtime) for 28 days Compliance was assessed by interview as well as by pill count | |
| Outcomes | Evaluations were performed at the end of the 2nd and 4th weeks. Endoscopic evaluation was performed at entry and after 4 weeks Clinical evaluation included participant recordings of number of daily bowel movements, stool consistency, presence of blood and mucus, urgency, and incontinence. Endoscopic evaluation assessed the severity of ulceration, friability, erythema, and exudate, each on a 3‐point scale. The sum of these 3 scores gave a total endoscopic score. Improvement was assessed in terms of the changes in both clinical and endoscopic evaluations | |
| Notes | Funding support and conflicts of interest were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Centralized randomization Randomization was on an alternate basis between drug and placebo and allocated by pharmaceutical manufacturer |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: physically‐indistinguishable placebo capsules were provided in identical containers |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across intervention groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Expected outcomes were reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
AE: adverse event; CAI: clinical activity index; CFT: contact friability test; EI: endoscopy index; ESR: erythrocyte sedimentation rate; IBD: inflammatory bowel disease; LOCF: last observation carried forward; MMDAI: modified Mayo disease activity index; PFA: patient functional assessment; PGA: physician global assessment; QOL: quality of life; SASP: sulfasalazine; UCCS: ulcerative colitis clinical score; UC‐DAI: ulcerative colitis disease activity index;
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adrizzone 2006 | Ineligible comparator group (AZA) |
| Ahluwalia 1992 | Not a randomized control trial |
| Behrens 2013 | No control group |
| Dignass 2018 | No control group (both groups received 1000 mg mesalamine a day) |
| Fiorino 2019 | The study drug was not pure 5‐ASA, but also contained sodium hyaluronate |
| Gross 2011 | Ineligible comparator group (Budesonide) |
| Irvine 2008 | Not a randomized control trial |
| Kamm 2009 | Not a randomized control trial |
| Levine 2017 | Not an oral 5‐ASA formulation |
| Mahmood 2005 | Not an oral 5‐ASA formulation |
| Paoluzi 2002 | No control group |
| Park 2018 | Maintenance study |
| Pruitt 1991 | Not a randomized control trial |
| Rubin 2017 | Compares once‐daily budesonide to placebo in people who are refractory to 5‐ASA treatment |
| Safdi 1997 | Not an oral 5‐ASA formulation |
| Suzuki 2017 | Not an induction trial |
| Turner 2017 | A pediatric study |
| Vecchi 2001 | Not an oral 5‐ASA formulation |
| Vernia 2000 | No control group |
| Ye 2018 | No control group (both groups received same oral regimen) |
| Yoshimura 2018 | No control group |
Characteristics of ongoing studies [ordered by study ID]
NCT02522767.
| Study name | A randomized, double‐blind, placebo‐controlled, multicenter study investigating the efficacy and safety of mesalamine 4 g extended release granules (sachet) for the induction of clinical and endoscopic remission in active, mild to moderate ulcerative Colitis |
| Methods | Participants were randomized to 1 of 2 groups:
|
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | 4g extended release granules of Mesalamine and placebo |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | October 2015 |
| Contact information | Clinical Development Support: DK0-Disclosure@ferring.com |
| Notes | This study is currently recruiting participants The estimated completion date is 28 February 2018 |
Differences between protocol and review
We added in SAEs as a secondary outcome for this review. SAEs were not reported in the previously published version.
Contributions of authors
Alistair Murray (AM) was involved in the search and selection of studies for inclusion in the review, collection of data for the review, assessment of the risks of bias, analysis of data, interpretation of data and writing the review.
Tran M Nguyen (TMN) was involved in the co‐ordination of the review, search and selection of studies for inclusion in the review, collection of data for the review, assessment of the certainty of the body of evidence, analysis of data, interpretation of data and writing the review.
Claire E Parker (CEP) was involved in the design of the review and interpretation of data.
Brian G Feagan (BGF) was involved in the conception of the review, design of the review and interpretation of data.
John K MacDonald (JKM) was involved in assessment of the certainty of the body of evidence, interpretation of data and writing the review.
Declarations of interest
AM: no known conflicts of interest.
TMN: no known conflicts of interest.
CEP: no known conflicts of interest.
BGF has received fees from Abbott/AbbVie, Amgen, Astra Zeneca, Avaxia Biologics Inc., Bristol‐Myers Squibb, Celgene, Centocor Inc., Elan/Biogen, Ferring, JnJ/Janssen, Merck, Nestles, Novartis, Novonordisk, Pfizer, Prometheus Laboratories, Protagonist, Salix Pharma, Takeda, Teva, TiGenix, Tillotts Pharma AG and UCB Pharma for Scientific Advisory Board membership; fees from Abbott/AbbVie, Actogenix, Akros, Albireo Pharma, Amgen, Astra Zeneca, Avaxia Biologics Inc., Avir Pharma, Axcan, Baxter Healthcare Corp., Biogen Idec, Boehringer‐Ingelheim, Bristol‐Myers Squibb, Calypso Biotech, Celgene, Elan/Biogen, EnGene, Ferring Pharma, Roche/Genentech, GiCare Pharma, Gilead, Given Imaging Inc., GSK, Ironwood Pharma, Janssen Biotech (Centocor), JnJ/Janssen, Kyowa Kakko Kirin Co Ltd., Lexicon, Lilly, Lycera BioTech, Merck, Mesoblast Pharma, Millennium, Nektar, Nestles, Novonordisk, Pfizer, Prometheus Therapeutics and Diagnostics, Protagonist, Receptos, Salix Pharma, Serono, Shire, Sigmoid Pharma, Synergy Pharma Inc., Takeda, Teva Pharma, TiGenix, Tillotts, UCB Pharma, Vertex Pharma, VHsquared Ltd., Warner‐Chilcott, Wyeth, Zealand, and Zyngenia for consultancy; payment for lectures from Abbott/AbbVie, JnJ/Janssen, Takeda, Warner‐Chilcott, UCB Pharma; his institution has received grants/grants pending from Abbott/AbbVie, Amgen, Astra Zeneca, Bristol‐Myers Squibb (BMS), Janssen Biotech (Centocor), JnJ/Janssen, Roche/Genentech, Millennium, Pfizer, Receptos, Santarus, Sanofi, Tillotts, and UCB Pharma. Dr Feagan was the author of one study that was included in this review.
JKM: no known conflicts of interest.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Andreoli 1987 {published data only}
- Andreoli A, Cosintino R, Trotti R, Berri F, Prantera C. 5-aminosalicylic acid versus salazopirin (SASP) in the oral treatment of active ulcerative colitis (UC) and in remission. In: Clinical Controversies in Inflammatory Bowel Disease. 1987:170.
Bresci 1990 {published data only}
- Bresci G, Carrai M, Venturini G, Gambardella L. Therapeutic effectiveness and tolerance of 5-aminosalicylic acid in short term treatment of patients with ulcerative colitis at a low or medium phase of activity. International Journal of Tissue Reactions 1990;12(4):243-6. [PubMed] [Google Scholar]
Cai 2001 {published data only}
- Cai JT, Wu LF, Du Q, Qian KD. Olsalazine versus sulfasalazine in the treatment of ulcerative colitis: randomized controlled clinical trial. Chinese Journal of Digestion 2001;21(10):593-5. [Google Scholar]
D'Haens 2006 {published data only}
- D'Haens G, Hommes D, Engels L, Baert F, Van der Waaij L, Connor P, et al. Once daily MMX mesalazine for the treatment of mild-to-moderate ulcerative colitis: a phase II, dose-ranging study. Alimentary Pharmacology and Therapeutics 2006;24(7):1087-97. [DOI] [PubMed] [Google Scholar]
D'Haens 2017 {published data only}
- D'Haens GR, Sandborn WJ, Zou G, Stitt LW, Rutgeerts PJ, Gilgen D, et al. Randomised non-inferiority trial: 1600mg versus 400mg tablets of mesalazine for the treatment of mild-to-moderate ulcerative colitis. Alimentary Pharmacology & Therapeutics 2017;46(3):292-302. [DOI] [PubMed] [Google Scholar]
Ewe 1988 {published data only}
- Ewe K, Eckhardt V, Kanzler G. Treatment of ulcerative colitis with olsalazine and sulfasalazine: efficacy and side effects. Scandinavian Journal of Gastroenterology 1988;23(Suppl 148):70-5. [DOI] [PubMed] [Google Scholar]
Farup 2001 {published data only}
- *.Farup PG, Hinterleitner TA, Lukás M, Hébuterne X, Rachmilewitz D, Campieri M, et al. Mesalazine 4 g daily given as prolonged-release granules twice daily and four times daily is at least as effective as prolonged-release tablets four times daily in patients with ulcerative colitis. Inflammatory Bowel Diseases 2001;7(3):237-42. [DOI] [PubMed] [Google Scholar]
- Farup PG, Oddsson E, Hinterleitner T. Mesalamine 4 g prolonged release granules BID and QID versus tablets QID for mild/moderate UC. Gastroenterology 1999;116(4 Part 2):A713. [Google Scholar]
Feagan 2013 {published data only}
- Feagan B, Sandborn W, D'Haens G, McDonald J, Rutgeerts P, Munkholm P, et al. The value of a central image management system (CIMS) in the conduct of randomized controlled trials of therapy for ulcerative colitis (UC). American Journal of Gastroenterology 2012;107:S579-80. [Google Scholar]
- *.Feagan BG, Sandborn WJ, D’Haens G, Pola S, McDonald JW, Rutgeerts P, et al. The role of centralized reading of endoscopy in a randomized controlled trial of mesalamine for ulcerative colitis. Gastroenterology 2013;145(1):149-57. [DOI] [PubMed] [Google Scholar]
Feurle 1989 {published data only}
- *.Feurle GE, Theuer D, Velasco S, Barry BA, Wordehoff D, Sommer A, et al. Olsalazine versus placebo in the treatment of mild to moderate ulcerative colitis: a randomised double-blind trial. Gut 1989;30(10):1354-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feurle GE, Theuer D, Velasco S, Barry BA, Wordehoff D, Sommer A, et al. Olsalazine versus placebo in the treatment of mild to moderate ulcerative colitis: a randomized double-blind trial. Gastroenterology 1988;94(5 Part 2):A126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fleig 1988 {published data only}
- Fleig WE, Laudage G, Sommer H, Wellman W, Stange EF, Riemann J. Prospective, randomized, double-blind comparison of benzalazine and sulfasalazine in the treatment of active ulcerative colitis. Digestion 1988;40(3):173-80. [DOI] [PubMed] [Google Scholar]
Flourié 2013 {published data only}
- *.Flourié B, Hagège H, Tucat G, Maetz D, Hébuterne X, Kuyvenhoven JP, et al. Randomised clinical trial: once- vs. twice-daily prolonged-release mesalazine for active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2013;37(8):767-75. [DOI] [PubMed] [Google Scholar]
- Flourié B, Hagège H, Tucat G, Masclee A, Dewit O, Probert C, et al. Once-daily versus twice-daily mesalazine for active ulcerative colitis: Efficacy results from MOTUS, a multicentre, controlled, randomised, investigator-blinded study. Journal of Crohn's & Colitis 2012;6:S82. [Google Scholar]
- Flourié B, Hagège H, Tucat G, Masclee A, Dewit O, Probert C, et al. Once-daily versus twice-daily mesalazine for active ulcerative colitis: efficacy results from motus, a multicentre, controlled, randomised, investigator-blinded study. Gastroenterology 2012;142(5 suppl 1):S197. [Google Scholar]
- Flourié B, Kuyvenhoven J, Probert C, Dewit O. Comparing the efficacy of once-daily or twice-daily mesalazine dosing in the treatment of left-sided ulcerative colitis versus the overall MOTUS study population. Journal of Crohn's & Colitis 2013;7:S236. [Google Scholar]
- Pierik M, Hagège H, Tucat G, Masclee A, Dewit O, Probert C, et al. Once-daily versus twice-daily mesalazine for mild to moderately active ulcerative colitis: Mucosal healing and early response data from MOTUS, a multicentre, controlled, randomised, investigator-blinded study. Journal of Crohn's & Colitis 2012;6:S82-3. [Google Scholar]
Forbes 2005 {published data only}
- Forbes A, Al-Damluji A, Ashworth S, Bramble M, Herbert K, Ho J, et al. Multicentre randomized-controlled clinical trial of Ipocol, a new enteric-coated form of mesalazine, in comparison with Asacol in the treatment of ulcerative colitis. Alimentary Pharmacology & Therapeutics 2005;21(9):1099-104. [DOI] [PubMed] [Google Scholar]
Gibson 2006 {published data only}
- Gibson PR, Fixa B, Pekárková B, Bátovský M, Radford-Smith G, Tibitanzl J, et al. Comparison of the efficacy and safety of Eudragit-L-coated mesalazine tablets with ethylcellulose-coated mesalazine tablets in patients with mild to moderately active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2006;23(7):1017-26. [DOI] [PubMed] [Google Scholar]
Good 1992 {published data only}
- Good L, Nester T, Borgen L. A double-blind comparison of controlled release mesalamine tablets and sulfasalazine in the treatment of ulcerative colitis. Gastroenterology 1992;102:A630. [Google Scholar]
Green 1998 {published data only}
- Green JR, Holdsworth CD, Lobo AJ, Leicester R, Gibson JA, Kerr GD, et al. Balsalazide is more effective and better tolerated than mesalazine in acute ulcerative colitis. In: Digestive Disease Week Abstract Book. 1997. [DOI] [PubMed]
- *.Green JR, Lobo AJ, Holdsworth CD, Leicester RJ, Gibson JA, Kerr GD, et al. Balsalazide is more effective and better tolerated than mesalazine in the treatment of acute ulcerative colitis. Gastroenterology 1998;114(1):15-22. [DOI] [PubMed] [Google Scholar]
Green 2002 {published data only}
- *.Green JR, Mansfield JC, Gibson JA, Kerr GD, Thornton PC. A double-blind comparison of balsalazide, 6.75 g daily, and sulfasalazine, 3g daily, in patients with newly diagnosed or relapsed active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2002;16(1):61-8. [DOI] [PubMed] [Google Scholar]
- Green JR, Swan CH, Rowlinson AE, Gibson JA, Brown P, Kerr GD, et al. Sulphasalazine or high dose balsalazide to treat acute relapse in ulcerative colitis? Results of a randomized trial. Gastroenterology 1993;104(4 Part 2):709. [Google Scholar]
Hanauer 1993 {published data only}
- Hanauer S, Beshears L, Wilkinson C. Induction of remission in a dose-ranging study of oral mesalamine capsules (Pentasa). Gastroenterology 1990;98(5 Part 2):A174. [Google Scholar]
- *.Hanauer S, Schwartz J, Robinson M, Roufail W, Arora S, Cello J, et al. Mesalamine capsules for treatment of active ulcerative colitis: results of a controlled trial. American Journal of Gastroenterology 1993;88(8):1188-97. [PubMed] [Google Scholar]
- Hanauer S, Schwartz J, Roufail W, Robinson M, Cello J, Safdi M, et al. Dose-ranging study of oral mesalamine capsule (Pentasa) for active ulcerative colitis. Gastroenterology 1989;96:A195. [PubMed] [Google Scholar]
- Miner P, Nostrant T, Wruble L, Hines C, Johnson S, Wilkinson C, et al. Multicenter trial of Pentasa for active ulcerative colitis. Gastroenterology 1991;100(5 Part 2):A231. [Google Scholar]
- Robinson M, Cello J, Safdi M, Schwartz J, Roufail W, Hoop R, et al. Mesalamine (Pentasa) enhances quality of life (QofL) for ulcerative colitis (UC) patients. Gastroenterology 1991;100(5 Part 2):A243. [Google Scholar]
- Robinson M, Hanauer S, Hoop R, Zbrozek A, Wilkinson C. Mesalamine capsules enhance the quality of life for patients with ulcerative colitis. Alimentary Pharmacology & Therapeutics 1994;8(1):27-34. [DOI] [PubMed] [Google Scholar]
Hanauer 1996 {published data only}
- Hanauer SB, Barish C, Pambianco D, Sigmon R, Gannan R, Koval G, et al. A multi-center, double-blind, placebo-controlled, dose-ranging trial of olsalazine for mild-moderately active ulcerative colitis. Gastroenterology 1996;110:A921. [Google Scholar]
Hanauer 2005 {published data only}
- Hanauer SB, Sandborn WJ, Kornbluth A, Katz S, Safdi M, Woogen S, et al. Delayed-release oral mesalamine at 4.8 g/day (800 mg tablet) for the treatment of moderately active ulcerative colitis: the ASCEND II trial. American Journal of Gastroenterology 2005;100(11):2478-85. [DOI] [PubMed] [Google Scholar]
Hanauer 2007 {published data only}
- Hanauer SB, Sandborn WJ, Dallaire C, Archambault A, Yacyshyn B, Yeh C, et al. Delayed-release oral mesalamine 4.8 g/day (800 mg tablets) compared to 2.4 g/day (400 mg tablets) for the treatment of mildly to moderately active ulcerative colitis: The ASCEND I trial. Canadian Journal of Gastroenterology 2007;21(12):827-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hetzel 1986 {published data only}
- Hetzel DJ, Bochner F, Imhoff DM, Gibson GE, Fitch RJ, Hecker R, et al. Azodisacylate (ADS) in the treatment of ulcerative colitis (UC): a controlled trial and assessment of drug disposition. Gastroenterology 1985;88:A1418. [DOI] [PubMed] [Google Scholar]
- *.Hetzel DJ, Shearman DJ, Bochner F, Imhoff DM, Gibson GE, Fitch RJ, et al. Azodisalicylate (Olsalazine) in the treatment of active ulcerative colitis. A placebo controlled clinical trial and assessment of drug disposition. Journal of Gastroenterology and Hepatology 1986;1:257-66. [DOI] [PubMed] [Google Scholar]
- Hetzel DJ, Shearman DJ, Labrooy J, Bochner F, Imhoff DM, Gibson GE, et al. Olsalazine in the treatment of active ulcerative colitis: a placebo controlled clinical trial and assessment of drug disposition. Scandinavian Journal of Gastroenterology Supplement 1988;23(148):61-9. [DOI] [PubMed] [Google Scholar]
Hiwatashi 2011 {published data only}
- Hiwatashi N, Suzuki Y, Mitsuyama K, Munakata A, Hibi T. Clinical trial: effects of an oral preparation of mesalazine at 4 g/day on moderately active ulcerative colitis. A phase III parallel-dosing study. Journal of Gastroenterology 2011;46(1):46-56. [DOI] [PubMed] [Google Scholar]
Ito 2010 {published data only}
- Ito H, Iida M, Matsumoto T, Suzuki Y, Koyama H, Yoshida T, et al. A direct comparative study of two different mesalamine formulations revealed appropriate use of mesalamine for patients with active ulcerative colitis depending on the characteristics of disease. Gastroenterology 2010;1:S166. [Google Scholar]
- *.Ito H, Iida M, Matsumoto T, Suzuki Y, Sasaki H, Yoshida T, et al. Direct comparison of two different mesalamine formulations for the induction of remission in patients with ulcerative colitis: a double-blind, randomized study. Inflammatory Bowel Diseases 2010;16(9):1567-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jiang 2004 {published data only}
- Jiang XL, Cui HF. Different therapy for different types of ulcerative colitis. World Journal of Gastroenterology 2004;10(10):1513-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamm 2007 {published data only}
- Hanauer S, Sandborn W, Lichtenstein G, Kamm M, Barrett K, Joseph R. MMX mesalamine for providing remission of active mild-to-moderate ulcerative colitis: an evidence-based medicine analysis. Inflammatory Bowel Diseases 2007;13(S5):663. [Google Scholar]
- *.Kamm MA, Sandborn WJ, Gassull M, Schreiber S, Jackowski L, Butler T, et al. Once-daily, high-concentration MMX mesalamine in active ulcerative colitis. Gastroenterology 2007;132(1):66-75. [DOI] [PubMed] [Google Scholar]
Kruis 1998 {published data only}
- *.Kruis W, Brandes JW, Schreiber S, Theuer D, Krakamp B, Schutz E, et al. Olsalazine versus mesalazine in the treatment of mild to moderate ulcerative colitis. Alimentary Pharmacology & Therapeutics 1998;12(8):707-15. [DOI] [PubMed] [Google Scholar]
- Kruis W, Schreiber S, Theuer D, Schutz E, Krakamp B, Otto P, et al. Comparison of an azoboundamino salicylate (olsalazine) vs. a coated aminosalicylate (mesalamine) for active ulcerative colitis. Gastroenterology 1996;110(4):942. [Google Scholar]
Kruis 2003 {published data only}
- *.Kruis W, Bar-Meir S, Feher J, Mickisch O, Mlitz H, Faszczyk M, et al. The optimal dose of 5-aminosalicylic acid in active ulcerative colitis: a dose-finding study with newly developed mesalamine. Clinical Gastroenterology and Hepatology 2003;1(1):36-43. [DOI] [PubMed] [Google Scholar]
- Kruis W, Meir SB, Feher J, Stolte M. Dose finding study of the efficacy and safety of newly developed 5-ASA containing pellets in patients with active ulcerative colitis. Gastroenterology 2000;118(4 Suppl 2):A780. [Google Scholar]
Kruis 2009 {published data only}
- Kruis W, Gorelov A, Kiudelis G, Rácz I, Pokrotnieks J, Horynski M, et al. Once daily dosing of 3g mesalamine (Salofalk® Granules) is therapeutic equivalent to a three-times daily dosing of 1g mesalamine for the treatment of active ulcerative colitis. Gastroenterology 2007;132(4 Suppl 1):A130-1. [Google Scholar]
- *.Kruis W, Kiudelis G, Rácz I, Gorelov IA, Pokrotnieks J, Horynski M, et al. Once daily versus three times daily mesalazine granules in active ulcerative colitis: a double-blind, double-dummy, randomised, non-inferiority trial. Gut 2009;58(2):233-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levine 2002 {published data only}
- Levine DS, Pruitt R, Riff D, Koval G, Sales D, Wruble L, et al. A multi-center, double-blind dose-response trial of Colazide (balsalazide disodium) and Asacol (mesalamine) for mild-moderately active ulcerative colitis. Gastroenterology 1997;112:A1026. [Google Scholar]
- *.Levine DS, Riff DS, Pruitt R, Wruble L, Koval G, Sales D, et al. A randomized, double blind, dose-response comparison of balsalazide (6.75 g), balsalazide (2.25 g), and mesalamine (2.4 g) in the treatment of active, mild-to-moderate ulcerative colitis. American Journal of Gastroenterology 2002;97(6):1398-407. [DOI] [PubMed] [Google Scholar]
Lichtenstein 2007 {published data only}
- Lichtenstein GR, Kamm MA, Boddu P, Gubergrits N, Lyne A, Butler T, et al. Effect of once- or twice-daily MMX mesalamine (SPD476) for the induction of remission of mild to moderately active ulcerative colitis. Clinical Gastroenterology and Hepatology 2007;5(1):95-102. [DOI] [PubMed] [Google Scholar]
Maier 1985 {published data only}
- Maier K, Fruhmorgen P, Bode JC, Heller T, Von Gaisberg U, Klotz U. Successful acute treatment of chronic inflammatory intestinal diseases with oral 5-aminosalicylic acid [Erfolgreiche akutbehandlung chronisch-entzundlicher darmerkrankungen mit oraler 5-aminosalicylsaure]. Deutsche Medizinische Wochenschrift 1985;110(10):363-8. [DOI] [PubMed] [Google Scholar]
Mansfield 2002 {published data only}
- Mansfield JC, Giaffer MH, Cann PA, McKenna D, Thornton PC. A double-blind comparison of balsalazide, 6.75 g, and sulfasalazine, 3 g, as sole therapy in the management of ulcerative colitis. Alimentary Pharmacology & Therapeutics 2002;16(1):69-77. [DOI] [PubMed] [Google Scholar]
Marakhouski 2005 {published data only}
- *.Marakhouski Y, Fixa B, Holoman J, Hulek P, Lukas M, Batovsky M, et al. A double-blind dose-escalating trial comparing novel mesalazine pellets with mesalazine tablets in active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2005;21(2):133-40. [DOI] [PubMed] [Google Scholar]
- Marakhouski Y, Fixa B, Holoman J. Erratum: a double-blind dose-escalating trial comparing novel mesalazine pellets with mesalazine tablets in active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2005;21(6):793. [DOI] [PubMed] [Google Scholar]
Miglioli 1990 {published data only}
- *.Miglioli M, Bianchi Porro G, Brunetti G, Sturniolo GC, and the Italian IBD group. Oral delayed-release mesalazine in the treatment of mild ulcerative colitis: a dose ranging study. European Journal of Gastroenterology and Hepatology 1990;2:229-34. [Google Scholar]
- Miglioli M, Brunetti G, Sturniolo GC, Bianchi Porro G, Campieri M, Cottone M, et al. Oral 5-ASA (Asacol) in mild ulcerative colitis. a randomized double blind dose ranging trial. Italian Journal of Gastroenterology 1989;21(1 Suppl):7-8. [Google Scholar]
Mihas 1988 {published data only}
- Mihas AA, Xynopoulos D, Mihas TA. A prospective trial of oral 5-aminosalicylic acid vs sulfasalazine in ulcerative colitis.. Gastroenterology 1988;94(5 Part 2):A303. [Google Scholar]
Munakata 1995 {published data only}
- *.Munakata A, Yoshida Y, Muto T, Tsuchiya S, Fukushima T, Hiwatashi N, et al. Double-blind comparative study of sulfasalazine and controlled-release mesalazine tablets in the treatment of active ulcerative colitis. Journal of Gastroenterology 1995;30(Suppl 8):108-11. [PubMed] [Google Scholar]
- Munakata A, Yoshida Y, Muto T. Clinical efficacy of oral controlled-release mesalazine, N-5ASA on ulcerative colitis: double-blind comparative study in comparison with salazosulphapyridineu. Yakuri to Chiryo (Japanese Pharmacology and Therapeutics) 1994;22(Suppl 10):S2555-83. [Google Scholar]
Pontes 2014 {published data only}
- Pontes C, Vives R, Torres F, Panes J. Safety and activity of dersalazine sodium in patients with mild-to-moderate active colitis: double-blind randomized proof of concept study. Inflammatory Bowel Diseases 2014;20(11):2004-12. [DOI] [PubMed] [Google Scholar]
Pruitt 2002 {published data only}
- *.Pruitt R, Hanson J, Safdi M, Wruble L, Hardi R, Johanson J, et al. Balsalazide is superior to mesalamine in the time to improvement of signs and symptoms of acute mild-to-moderate ulcerative colitis. American Journal of Gastroenterology 2002;97(12):3078-86. [DOI] [PubMed] [Google Scholar]
- Pruitt R, Hanson J, Safdi M, Wruble L, Hardi R, Johanson JF, et al. Balsalazide is superior to mesalamine in the time to improvement of signs and symptoms of acute ulcerative colitis. Gastroenterology 2000;118(4 Suppl 2):A120-1. [DOI] [PubMed] [Google Scholar]
- Pruitt RE, Rosen AA, Wruble LD, Sedghi S, Shepard RD, Mareya SM. Safety and tolerability of twice-daily balsalazide tablets: Results from 2 randomized, double-blind, multicenter, phase 3 studies and 1 open-label, multicenter, phase 3 study. Gastroenterology 2009;136(5 Suppl 1):A523. [Google Scholar]
Qian 2004 {published data only}
- Qian LP, Lin GJ, Xu SR, Ding WQ. Clinical effect of olsalazine sodium capsule in the treatment of ulcerative colitis. Fudan University Journal of Medical Sciences 2004;31(4):421-4. [Google Scholar]
Rachmilewitz 1989 {published data only}
- Rachmelewitz D. Mesalazine (5-ASA) is as effective as sulfasalazine (SZ) in the treatment of active ulcerative colitis (UC). Gastroenterology 1988;94(5 Part 2):A362. [Google Scholar]
- *.Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ 1989;298(6666):82-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raedler 2004 {published data only}
- Behrens C, Bias P, Malchow H, Raedler A. Mesalazine (5-ASA) micropellets show comparable efficacy and tolerability as mesalazine tablets in patients with ulcerative colitis. A prospective, multi-national, randomised, double-blind, active-controlled clinical phase II study. Gastroenterology 2003;124(4 Suppl 1):A379. [Google Scholar]
- *.Raedler A, Behrens C, Bias P. Mesalazine (5-aminosalicylic acid) micropellets show similar efficacy and tolerability to mesalazine tablets in patients with ulcerative colitis -- results from a randomized-controlled trial. Alimentary Pharmacology & Therapeutics 2004;20(11-12):1353-63. [DOI] [PubMed] [Google Scholar]
Rao 1989 {published data only}
- *.Rao SS, Dundas SA, Holdsworth CD, Cann PA, Palmer KR, Corbett CL. Olsalazine or sulphasalazine in first attacks of ulcerative colitis? A double-blind study. Gut 1989;30(5):675-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao SS, Holdsworth CD, Palmer KL, Cann PA, Dundas SA, Corbett CL. Olsalazine versus sulphasalazine (SASP) in first attacks of ulcerative colitis (UC): a double blind study. Gut 1988;29:A705. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rijk 1991 {published data only}
- Rijk MCM, Tongerson JH. The efficacy and safety of sulphasalazine and olsalazine in patients with active ulcerative colitis. Gastroenterology 1991;100:A243. [Google Scholar]
Riley 1988 {published data only}
- *.Riley SA, Mani V, Goodman MJ, Herd ME, Dutt S, Turnberg A. Comparison of delayed release 5-aminosalicylic acid (mesalazine) and sulphasalazine in the treatment of mild to moderate ulcerative colitis relapse. Gut 1988;29(5):669-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley SA, Mani V, Goodman MJ, Turnberg LA. Delayed-release 5-aminosalicylic acid (5-ASA) and sulphasalazine (SSZ) in the treatment of mild to moderate ulcerative colitis (UC) relapse. Gut 1987;28:A1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robinson 1994 {published data only}
- Robinson M, Gitnick G, Balart L, Das K, Turkin D. Olsalazine in the treatment of mild to moderate ulcerative colitis. Gastroenterology 1988;84:A381. [Google Scholar]
- *.Robinson M, Hanauer S, Hoop R, Zbrozek A, Wilkinson C. Mesalamine capsules enhance the quality of life for patients with ulcerative colitis. Alimentary Pharmacology & Therapeutics 1994;8(1):27-34. [DOI] [PubMed] [Google Scholar]
Sandborn 2009 {published data only}
- Sandborn WJ, Regula J, Feagan B, Belousova EA, Jojic NV, Lukas M, et al. Efficacy and safety of delayed-release oral mesalamine at 4.8g/d (800mg tablet) in the treatment of moderately active ulcerative colitis: results of the ASCEND III study. Gastroenterology 2008;134(4 Suppl 1):A99. [Google Scholar]
- *.Sandborn WJ, Regula J, Feagan BG, Belousova E, Jojic N, Lukas M, et al. Delayed-release oral mesalamine 4.8 g/day (800-mg tablet) is effective for patients with moderately active ulcerative colitis. Gastroenterology 2009;137(6):1934-43. [DOI] [PubMed] [Google Scholar]
Sandborn 2012 {published data only}
- Sandborn WJ, Travis S, Moro L, Jones R, Gautille T, Bagin R, et al. Once-daily budesonide MMX® extended-release tablets induce remission in patients with mild to moderate ulcerative colitis: results from the CORE I study. Gastroenterology 2012;143(5):1218-26. [DOI] [PubMed] [Google Scholar]
Scherl 2009 {published data only}
- Pruitt RE, Rosen AA, Wruble L, Sedghi S, Shepard RD, Mareya SM, et al. Safety and tolerability of twice-daily balsalazide tablets: results of a phase 3, randomized, double-blind, placebo-controlled, multicenter study. Gastroenterology 2008;134(4 Suppl 1):A494. [Google Scholar]
- Rubin DT, Rosen AA, Sedghi S, Shepard RD, Mareya SM, Huang S, et al. Twice-daily balsalazide tablets improve patient quality of life after 2 and 8 weeks of treatment: results of a phase 3, randomized, double-blind, placebo-controlled, multicenter study. Gastroenterology 2008;134(4 Suppl 1):A494. [Google Scholar]
- *.Scherl EJ, Pruitt R, Gordon GL, Lamet M, Shaw A, Huang S, et al. Safety and efficacy of a new 3.3 g b.i.d. tablet formulation in patients with mild-to-moderately-active ulcerative colitis: a multicenter, randomized, double-blind, placebo-controlled study. American Journal of Gastroenterology 2009;104(6):1452-9. [DOI] [PubMed] [Google Scholar]
- Scherl EJ, Pruitt RE, Gordon GL, Lamet M, Shaw AL, Huang S, et al. Twice-daily dosing of balsalazide tablets 3.3 g is safe and effective in the treatment of mild-to-moderate ulcerative colitis. Gastroenterology 2009;1:A520. [Google Scholar]
Schroeder 1987 {published data only}
- Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. New England Journal of Medicine 1987;317(26):1625-9. [DOI] [PubMed] [Google Scholar]
Sninsky 1991 {published data only}
- Sninsky CA, Cort DH, Shanahan F, Powers BJ, Sessions JT, Pruitt RE, et al. Oral mesalamine (Asacol) for mildly to moderately active ulcerative colitis. A multicenter study. Annals of Internal Medicine 1991;115(5):350-5. [DOI] [PubMed] [Google Scholar]
Sutherland 1990 {published data only}
- Sutherland LR, Robinson M, Onstad G, Peppercorn M, Greenberger N, Goodman M, et al. A double-blind, placebo-controlled, multicentre study of the efficacy and safety of 5-aminosalicylic acid tablets in the treatment of ulcerative colitis. Canadian Journal of Gastroenterology 1990;4:463-7. [Google Scholar]
Tursi 2004 {published data only}
- Tursi A, Brandimarte G, Giorgetti GM, Forti G, Modeo ME, Elisei W. Low-dose balsalazide plus high-potency probiotic preparation is more effective than balsalazide alone or mesalazine in the treatment of acute mild-to-moderate ulcerative colitis. Gastroenterology 2005;128((4 Suppl 2)):A17. [PubMed] [Google Scholar]
- *.Tursi A, Brandimarte G, Giorgetti GM, Forti G, Modeo ME, Gigliobianco A. Low-dose balsalazide plus a high-potency probiotic preparation is more effective than balsalazide alone or mesalazine in the treatment of acute mild-to-moderate ulcerative colitis. Medical Science Monitor 2004;10(11):126-31. [PubMed] [Google Scholar]
Willoughby 1988 {published data only}
- Willoughby CP, Cowan RE, Gould SR, Machell RJ, Stewart JB. Double-blind comparison of olsalazine and sulfasalazine in active ulcerative colitis. Scandinavian Journal of Gastroenterology 1988;148:40-4. [DOI] [PubMed] [Google Scholar]
Zinberg 1990 {published data only}
- Zinberg J, Molinas S, Das KM. A double-blinded, placebo-controlled clinical study of azodisalicylate sodium (olsalazine) in the treatment of ulcerative colitis. Gastroenterology 1987;92:A1711. [PubMed] [Google Scholar]
- *.Zinberg J, Molinas S, Das KM. Double-blind placebo-controlled study of olsalazine in the treatment of ulcerative colitis. American Journal of Gastroenterology 1990;85(5):562-6. [PubMed] [Google Scholar]
References to studies excluded from this review
Adrizzone 2006 {published data only}
- Ardizzone S, Maconi G, Russo A, Imbesi V, Colombo E, Bianchi Porro G. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut 2006;55(1):47-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahluwalia 1992 {published data only}
- Ahluwalia NK, Thompson DG, Goodman MJ, Mani V, McIntyre J, Dane G. Double-blind randomized trial of 4.8 g vs. 2.4 g of mesalazine for 4 weeks in the treatment of acute ulcerative colitis. Gastroenterology 1992;102:A588. [Google Scholar]
Behrens 2013 {published data only}
- Behrens C, Bias P, Malchow H, Raedler A. Mesalazine (5-ASA) micropellets show comparable efficacy and tolerability as mesalazine tablets in patients with ulcerative colitis. A prospective, multi-national, randomised, double-blind, active-controlled clinical phase II study. Gastroenterology 2013;124(4 Suppl 1):A379. [Google Scholar]
Dignass 2018 {published data only}
- Dignass A, Schnabel R, Romatowski J, Pavlenko V, Dorofeyev A, Dorova J, et al. Efficacy and safety of novel high-dose mesalazine tablet in mild to moderate active ulcerative colitis: a double-blind, multicentre, randomised trial. United European Gastroenterology Journal 2018;6(1):138-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fiorino 2019 {published data only}
- Fiorino G, Sturniolo GC, Bossa F, Cassinotti A, Sabatino AD, Giuffrida P, et al. A phase 2a, multicenter, randomized, double-blind,parallel-group, placebo-controlled trial of IBD98-M delayed-release capsules to induce remission in patients with active and mild to moderate ulcerative colitis. Cells 2019;8(6):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 2011 {published data only}
- Gross V, Bunganic I, Belousova EA, Mikhailova TL, Kupcinskas L, Kiudelis G, et al. 3g mesalazine granules are superior to 9mg budesonide for achieving remission in active ulcerative colitis: a double-blind, double-dummy, randomised trial. Journal of Crohn's & Colitis 2011;5(2):129-38. [DOI] [PubMed] [Google Scholar]
Irvine 2008 {published data only}
- Irvine EJ, Yeh CH, Ramsey D, Stirling AL, Higgins PD. The effect of mesalazine therapy on quality of life in patients with mildly and moderately active ulcerative colitis. Alimentary Pharmacology & Therapeutics 2008;28(11-12):1278-86. [DOI] [PubMed] [Google Scholar]
Kamm 2009 {published data only}
- Kamm MA, Lichtenstein GR, Sandborn WJ, Schreiber S, Lees K, Barrett K, et al. Effect of extended MMX mesalamine therapy for acute, mild-to-moderate ulcerative colitis. Inflammatory Bowel Diseases 2009;15(1):1-8. [DOI] [PubMed] [Google Scholar]
Levine 2017 {published data only}
- Levine A, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R, et al. Mesalamine enemas for induction of remission in pediatric ulcerative colitis refractory to oral Mesalamine: A prospective cohort study. Journal of Pediatric Gastroenterology and Nutrition 2017;64(Suppl 1):49. [DOI] [PubMed] [Google Scholar]
- *.Levine A, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R, et al. Mesalamine enemas for induction of remission in pediatric ulcerative colitis refractory to oral mesalamine: A prospective cohort study. Journal of Crohn's & Colitis 2017;11(Suppl 1):S285. [DOI] [PubMed] [Google Scholar]
Mahmood 2005 {published data only}
- Mahmood A, Melley L, Fitzgerald AJ, Ghosh S, Playford RJ. Trial of trefoil factor 3 enemas, in combination with oral 5-aminosalicylic acid, for the treatment of mild-to-moderate left-sided ulcerative colitis. Alimentary Pharmacology & Therapeutics 2005;21(11):1357-64. [DOI] [PubMed] [Google Scholar]
Paoluzi 2002 {published data only}
- Paoluzi P, D'Albasio G, Pera A, Bianchi Porro G, Paoluzi OA, Pica R, et al. Oral and topical 5-aminosalicylic acid (mesalazine) in inducing and maintaining remission in mild-moderate relapse of ulcerative colitis: one-year randomised multicentre trial. Digestive and Liver Disease 2002;34(11):787-93. [DOI] [PubMed] [Google Scholar]
Park 2018 {published data only}
- Park SK, Eun CS, Seo GS, Lim J, Kim TO, Park DI. The effects and adherence of Asacol comparing 2.4 g once daily with 800 mg three times or 1200 mg twice daily for maintain therapy in the ulcerative colitis: prospective multicentre randomised study. Journal of Crohn's & Colitis 2018;12(Suppl 1):S367. [Google Scholar]
Pruitt 1991 {published data only}
- Pruitt RE, Gremillion DE, Herring RW, Bailey AH, Faust TW, Potter M, et al. Oral Asacol in the treatment of mild to moderate ulcerative colitis: the Nashville experience. Journal of the Tennessee Medical Association 1991;84(5):237. [PubMed] [Google Scholar]
Rubin 2017 {published data only}
- Rubin DT, Cohen RD, Sandborn WJ, Lichtenstein GR, Axler J, Riddell RH, et al. Budesonide multimatrix is efficacious for mesalamine-refractory, mild to moderate ulcerative colitis: A randomised, placebo-controlled trial. Journal of Crohn's & Colitis 2017;11(7):785-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Safdi 1997 {published data only}
- Safdi M, DeMicco M, Sninsky C, Banks P, Wruble L, Deren J, et al. A double-blind comparison of oral versus rectal mesalamine versus combination therapy in the treatment of distal ulcerative colitis. American Journal of Gastroenterology 1997;92(10):1867-71. [PubMed] [Google Scholar]
Suzuki 2017 {published data only}
- Suzuki Y, Iida M, Ito H, Nishino H, Ohmori T, Arai T, et al. 2.4 g Mesalamine (Asacol 400 mg tablet) once daily is as effective as three times daily in maintenance of remission in ulcerative colitis: A randomized, noninferiority, multi-center trial. Inflammatory Bowel Diseases 2017;23(5):822-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2017 {published data only}
- Turner D, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R, et al. Once- versus twice-daily mesalazine to induce remission in paediatric ulcerative colitis: A randomised controlled trial. Journal of Crohn's & Colitis 2017;11(5):527-33. [DOI] [PubMed] [Google Scholar]
Vecchi 2001 {published data only}
- Vecchi M, Meucci G, Gionchetti P, Beltrami M, Di Maurizio P, Beretta L, et al. Oral versus combination mesalazine therapy in active ulcerative colitis: A double-blind, double-dummy, randomized multicentre study. Alimentary Pharmacology & Therapeutics 2001;15(2):251-6. [DOI] [PubMed] [Google Scholar]
Vernia 2000 {published data only}
- Vernia P, Monteleone G, Grandinetti G, Villotti G, Di Giulio E, Frieri G, et al. Combined oral sodium butyrate and mesalazine treatment compared to oral mesalazine alone in ulcerative colitis: randomized, double-blind, placebo-controlled pilot study. Digestive Diseases and Sciences 2000;45(5):976-81. [DOI] [PubMed] [Google Scholar]
Ye 2018 {published data only}
- Ye LN, Huang YB, Chen CX, Lv W, Fan YH, Yang HH, et al. Combined oral and suppository treatment with Pentasa (mesalazine) is superior to oral therapy alone in patients with mild/moderate extensive or left-sided active ulcerative colitis: a randomized multi-center controlled study. Journal of Digestive Diseases 2018;19(1):35. [Google Scholar]
Yoshimura 2018 {published data only}
- Yoshimura N, Okano S, Sako M, Takazoe M. Efficacy of once a day multi matrix mesalamine formulation, lialda in patients with active mild to moderate ulcerative colitis after inadequate response to the pH-dependent release mesalamine formulation, asacol. Journal of Crohn's & Colitis 2018;12(1):S300. [Google Scholar]
References to ongoing studies
NCT02522767 {published data only}
- NCT02522767. Mesalamine 4 g sachet for the induction of remission in active, mild to moderate ulcerative colitis (UC) (Ferring Pharmaceuticals). clinicaltrials.gov/show/NCT02522767 (first received 13 August 2015).
Additional references
Andrade 1995
- Andrade SE, Walker AM, Gottlieb LK, Hollenberg NK, Testa MA, Saperia GM, et al. Discontinuation of antihyperlipidemic drugs – do rates reported in clinical trials reflect rates in primary care settings? New England Journal of Medicine 1995;332(17):1125-31. [DOI] [PubMed] [Google Scholar]
Arend 2004
- Arend LJ, Springate JE. Interstitial nephritis from mesalazine: case report and literature review. Pediatric Nephrology 2004;19(5):550-3. [DOI] [PubMed] [Google Scholar]
Azad Khan 1977
- Azad Khan AK, Piris J, Truelove SC. An experiment to determine the active therapeutic moiety of sulfasalazine. Lancet 1977;2(8044):892-5. [DOI] [PubMed] [Google Scholar]
Beaulieu 2009
- Beaulieu DB, Schwartz DA. Medication persistence in patients with ulcerative colitis: meeting the challenges and improving patient outcomes. Medscape CME Gastroenterology 2009. Available from www.medscape.org/viewarticle/713895.
Brixner 2007
- Brixner D, Magowan S, Accortt N. Evaluation of prescription refill patterns based on daily dosing regimen and pill load for calcium channel blockers. In: Academy of Managed Care Pharmacy Annual Meeting. San Diego, CA, 2007.
Chan 1983
- Chan RP, Pope DJ, Gilbert AP, Sacra PJ, Baron JH, Lennard-Jones JE. Studies of two novel sulfasalazine analogs, ipsalazide and balsalazide. Digestive Diseases and Sciences 1983;28(7):609-15. [DOI] [PubMed] [Google Scholar]
Conrad 2014
- Conrad K, Roggenbuck D, Laass MW. Diagnosis and classification of ulcerative colitis. Autoimmunity Reviews 2014;13(4-5):463-6. [DOI] [PubMed] [Google Scholar]
Danese 2011
- Danese S, Fiocchi C. Ulcerative colitis. New England Journal of Medicine 2011;365(18):1713-25. [DOI] [PubMed] [Google Scholar]
Das 1973
- Das KM, Eastwood MA, McManus JP, Sircus W. Adverse reactions during salicylazosulfapyridine therapy and the relation with drug metabolism and acetylator phenotype. New England Journal of Medicine 1973;289(10):491-5. [DOI] [PubMed] [Google Scholar]
Dew 1982
- Dew MJ, Hughes PJ, Lee MG, Evans BK, Rhodes J. An oral preparation to release drugs in the human colon. British Journal of Clinical Pharmacology 1982;14(3):405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dick 1964
- Dick AP, Grayson MJ, Carpenter RG, Petrie A. Controlled trial of sulphasalazine in the treatment of ulcerative colitis. Gut 1964;5(5):437-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ediger 2007
- Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, et al. Predictors of medication adherence in inflammatory bowel disease. American Journal of Gastroenterology 2007;102(7):1417-26. [DOI] [PubMed] [Google Scholar]
Elseviers 2004
- Elseviers MM, D'Haens G, Lerebours E, Plane C, Stolear JC, Riegler G, et al. Renal impairment in patients with inflammatory bowel disease: association with aminosalicylate therapy? Clinical Nephrology 2004;61(2):83-9. [DOI] [PubMed] [Google Scholar]
Feuerstein 2014
- Feuerstein JD, Cheifetz AS. Ulcerative colitis. Mayo Clinic Proceedings 2014;89(11):1553-63. [DOI] [PubMed] [Google Scholar]
Ford 2011
- Ford AC, Achkar JP, Khan KJ, Kane SV, Talley NJ, Marshall JK, et al. Efficacy of 5-aminosalicylates in ulcerative colitis: systematic review and meta-analysis. American Journal of Gastroenterology 2011;106(4):601-16. [DOI] [PubMed] [Google Scholar]
Frandsen 2002
- Frandsen NE, Saugmann S, Marcussen N. Acute interstitial nephritis associated with the use of mesalazine in inflammatory bowel disease. Nephron 2002;92(1):200-2. [DOI] [PubMed] [Google Scholar]
Greenfield 1993
- Greenfield SM, Punchard NA, Teare JP, Thompson RP. Review article: The mode of action of the aminosalicylates in inflammatory bowel disease. Alimentary Pharmacology & Therapeutics 1993;7(4):369-83. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardy 1987
- Hardy JG, Healey JN, Reynolds JR. Evaluation of an enteric-coated delayed-release 5-aminosalicylic acid tablet in patients with inflammatory bowel disease. Alimentary Pharmacology & Therapeutics 1987;1(4):273-80. [DOI] [PubMed] [Google Scholar]
Hayllar 1991
- Hayllar J, Bjarnason I. Sulphasalazine in ulcerative colitis: In memoriam? Gut 1991;32(5):462-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Altman DG. Measuring inconsistency in meta-analysis. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Ireland 1987
- Ireland A, Jewell DP. Olsalazine in patients intolerant of sulphasalazine. Scandinavian Journal of Gastroenterology 1987;22(9):1038-40. [DOI] [PubMed] [Google Scholar]
Jarnerot 1996
- Järnerot G. Withdrawal rates because of diarrhea in Dipentum-treated patients with ulcerative colitis are low when Dipentum is taken with food and dose-titrated. Gastroenterology 1996;110:A932. [Google Scholar]
Kane 2001
- Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. American Journal of Gastroenterology 2001;96(10):2929-33. [DOI] [PubMed] [Google Scholar]
Kane 2003a
- Kane S, Huo D, Aikens J, Hanauer S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. American Journal of Medicine 2003;114(1):39-43. [DOI] [PubMed] [Google Scholar]
Kane 2003b
- Kane SV, Bjorkman DJ. The efficacy of oral 5-ASAs in the treatment of active ulcerative colitis: A systematic review. Reviews in Gastroenterological Disorders 2003;3:210. [PubMed] [Google Scholar]
Kane 2006
- Kane SV. Systematic review: adherence issues in the treatment of ulcerative colitis. Alimentary Pharmacology & Therapeutics 2006;23(5):577-85. [DOI] [PubMed] [Google Scholar]
Kane 2008
- Kane SV, Brixner D, Rubin DT, Sewitch MJ. The challenge of compliance and persistence: focus on ulcerative colitis. Journal of Managed Care Pharmacy 2008;14(1 Suppl A):S2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klotz 1980
- Klotz U, Maier K, Fischer C, Heinkel K. Therapeutic efficacy of sulfasalazine and its metabolites in patients with ulcerative colitis and Crohn's disease. New England Journal of Medicine 1980;303(26):1499-502. [DOI] [PubMed] [Google Scholar]
Levy 1999
- Levy RL, Feld AD. Increasing patient adherence to gastroenterology treatment and prevention regimens. American Journal of Gastroenterology 1999;94(7):1733-42. [DOI] [PubMed] [Google Scholar]
Loftus 2004
- Loftus EJ. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology 2004;126(6):1504-17. [DOI] [PubMed] [Google Scholar]
Maeda 2001
- Maeda S, Nomura S, Tahara M, Haneda M, Kikkawa R. Interstitial nephritis after treatment with mesalazine in the patient with ulcerative colitis. Nihon Naika Gakkai Zasshi 2001;90(5):872-3. [DOI] [PubMed] [Google Scholar]
Magowan 2006
- Magowan S, Kane S, Lange JL. 5-ASA prescription refill rates for ulcerative colitis are independent of formulation and dosing regimens. American Journal of Gastroenterology 2006;101:S447. Abstract 1144. [Google Scholar]
Misiewitz 1965
- Misiewitz JJ, Lennard-Jones JE, Connell AM, Baron JH, Jones FA. Controlled trial of sulfasalazine in maintenance therapy for ulcerative colitis. Lancet 1965;1:185-8. [Google Scholar]
Myers 1987
- Myers B, Evans DN, Rhodes J, Evans BK, Hughes BR, Lee MG, et al. Metabolism and urinary excretion of 5-aminosalicylic acid in healthy volunteers when given intravenously or released for absorption at different sites in the gastrointestinal tract. Gut 1987;28(2):196-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nielsen 1982
- Nielsen OH. Sulfasalazine intolerance: a retrospective study of the reasons for discontinuing treatment with sulfasalazine in patients with chronic inflammatory bowel disease. Scandinavian Journal of Gastroenterology 1982;17(3):389-93. [DOI] [PubMed] [Google Scholar]
Nielsen 1983
- Nielsen OH, Bondesen S. Kinetics of 5-aminosalicylic acid after jejunal instillation in man. British Journal of Clinical Pharmacology 1983;16(6):738-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ordás 2012
- Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Ulcerative colitis. Lancet 2012;380(9853):1606-19. [DOI] [PubMed] [Google Scholar]
Peppercorn 1972
- Peppercorn MA, Goldman P. The role of intestinal bacteria in the metabolism of salicylazo-sulfapyridine. Journal of Pharmacology and Experimental Therapeutics 1972;181(3):555-62. [PubMed] [Google Scholar]
Ponder 2013
- Ponder A, Long MD. A clinical review of recent findings in the epidemiology of inflammatory bowel disease. Clinical Epidemiology 2013;5:237-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rao 1987
- Rao SS, Cann PA, Holdsworth CD. Clinical experience of the tolerance of mesalazine and olsalazine in patients intolerant of sulphasalazine. Scandinavian Journal of Gastroenterology 1987;22(3):332-6. [DOI] [PubMed] [Google Scholar]
Rasmussen 1982
- Rasmussen SN, Bondesen S, Hvidberg EF, Hansen SH, Binder V, Halskou S, et al. 5-aminosalicylic acid in a slow-release preparation: bioavailability, plasma level, and excretion in humans. Gastroenterology 1982;83(5):1062-70. [PubMed] [Google Scholar]
Rothfuss 2006
- Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World Journal of Gastroenterology 2006;12(30):4819-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sandborn 2002a
- Sandborn WJ. Rational selection of oral 5-aminosalicylate formulations and prodrugs for the treatment of ulcerative colitis. American Journal of Gastroenterology 2002;97(12):2939-41. [DOI] [PubMed] [Google Scholar]
Sandborn 2002b
- Sandborn WJ, Hanauer SB, Buch A. Comparable systemic absorption of 5-ASA and N-AC-5-ASA from U.S. Asacol and Colazal. American Journal of Gastroenterology 2002;97:S263. [Google Scholar]
Sandborn 2002c
- Sandborn WJ, Hanauer SB. The pharmacokinetic profiles of oral 5ASA formulations used in the management of ulcerative colitis: a systematic review. American Journal of Gastroenterology 2002;97:S269. [Google Scholar]
Sandborn 2003
- Sandborn WJ, Hanauer SB. Systematic review: the pharmacokinetic profiles of oral mesalazine formulations and mesalazine pro-drugs used in the management of ulcerative colitis. Alimentary Pharmacology & Therapeutics 2003;17(1):29-42. [DOI] [PubMed] [Google Scholar]
Schroeder 1972
- Schroeder H, Campbell DE. Absorption, metabolism, and excretion of salicylazosulfapyridine in man. Clinical Pharmacology and Therapeutics 1972;13(4):539-51. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Shale 2003
- Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Alimentary Pharmacology & Therapeutics 2003;18(2):191-8. [DOI] [PubMed] [Google Scholar]
Staerk Laursen 1990
- Staerk Laursen L, Stokholm M, Bukhave K, Rask-Madsen J, Lauritsen K. Disposition of 5-aminosalicylic acid by olsalazine and three mesalazine preparations in patients with ulcerative colitis: comparison of intraluminal colonic concentrations, serum values, and urinary excretion. Gut 1990;31(11):1271-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sutherland 1987
- Sutherland LR, Martin F, Greer S, Robinson M, Greenberger N, Saibil F, et al. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology 1987;92(6):1894-8. [DOI] [PubMed] [Google Scholar]
Sutherland 2006a
- Sutherland LR, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD000544. [DOI: 10.1002/14651858.CD000544.pub2] [DOI] [PubMed] [Google Scholar]
Svartz 1942
- Svartz N. Salazyopyrin, a new sulfanilamide preparation: A. Therapeutic results in rheumatic polyarthritis. B. Therapeutic results in ulcerative colitis. C. Toxic manifestations in treatment with sulfanilamide preparation. Acta Medica Scandinavia 1942;110:557-90. [Google Scholar]
Truelove 1955
- Truelove SC, Witts LJ. Cortisone in ulcerative colitis: Final report on a therapeutic trial. British Medical Journal 1955;2(4947):1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Truelove 1959
- Truelove SC, Witts LJ. Cortisone and corticotrophin in ulcerative colitis. British Medical Journal 1959;1(5119):387-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Hees 1980
- Van Hees PA, Bakker JH, Tongeren JH. Effect of sulfapyridine, 5-aminosalicylic acid, and placebo in patients with idiopathic proctitis: a study to determine the active therapeutic moiety of sulfasalazine. Gut 1980;21(7):632-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Willoughby 1982
- Willoughby CP, Aronson JK, Agback H, Bodin NO, Truelove SC. Distribution and metabolism in healthy volunteers of disodium azodisalicylate, a potential therapeutic agent for ulcerative colitis. Gut 1982;23(12):1081-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Feagan 2012
- Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No: CD000543. [DOI: 10.1002/14651858.CD000543.pub3] [DOI] [PubMed] [Google Scholar]
Sutherland 1993
- Sutherland LR, May GR, Shaffer EA. Sulfasalazine revisited: a meta-analysis of 5-aminosalicylic acid in the treatment of ulcerative colitis. Annals of Internal Medicine 1993;118:540-9. [DOI] [PubMed] [Google Scholar]
Sutherland 1997
- Sutherland LR, Roth DE, Beck PL. Alternatives to sulfasalazine: A meta-analysis of 5-ASA in the treatment of ulcerative colitis. Inflammatory Bowel Diseases 1997;3:65-78. [PubMed] [Google Scholar]
Sutherland 2006b
- Sutherland LR, MacDonald JK. Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD000543. [DOI: 10.1002/14651858.CD000543.pub2] [DOI] [PubMed] [Google Scholar]
Wang 2016
- Wang Y, Parker CE, Bhanji T, Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2016, Issue 4. Art. No: CD000543. [DOI: 10.1002/14651858.CD000543.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


