Abstract
Background:
Suicide rates are high in borderline personality disorder (BPD) where interpersonal problems trigger intense affective dysregulation and impulses to act on suicidal thoughts. To date, however, no study has examined how interpersonal stressors contribute to momentary within-person links among affect and impulsivity with suicidal ideation, and how those links vary over time in people’s daily lives.
Methods:
153 individuals diagnosed with BPD and 52 healthy controls completed a 21-day ecological momentary assessment protocol. Of these 153 BPD individuals with BPD, 105 had a history of suicide attempts. Multilevel structural equation modeling (MSEM) was used to examine dynamic links among interpersonal perceptions, affect, state impulsivity, and suicidal intent.
Results:
Aggregated across interactions, lower perceived warmth in others was associated with suicidal ideation. This direct relationship, however, did not extend to momentary within-person associations. Instead, interpersonal conflicts were linked to suicidal ideation indirectly via greater negative affect and lower positive affect. While a robust within-person link between interpersonal perceptions and impulsivity emerged, impulsivity did not account for the relationship between interpersonal perceptions and suicidal ideation.
Conclusion:
This intensive longitudinal study illustrates momentary interpersonal signatures of an emerging suicidal crisis. Among people with BPD at high risk for suicide, interpersonal triggers initiate a cascade of affective dysregulation, which in turn gives rise to suicidal ideation.
Keywords: suicidal ideation, ecological momentary assessment, borderline personality disorder, multilevel structural equation modelling, affective dysregulation, impulsivity
People diagnosed with borderline personality disorder (BPD) are at high risk of dying by suicide: almost all report chronic suicidal ideation, 84% of patients with BPD engage in suicidal behavior, 70% attempt suicide, with a mean of 3.4 lifetime attempts per individual, and 5–10% die by suicide (Black et al., 2004; McGirr et al., 2007; Soloff et al., 1994).
Although correlates of suicidal behavior have been studied extensively in the past 30 years (Turecki et al., 2019), prediction of suicide attempts remains close to chance (Franklin et al., 2017; Nock, 2009). One important reason for this lack of progress is that most studies have focused on between-person differences, or have employed long follow-up intervals, missing the temporal dynamics of suicide risk that require more frequent assessments.
Given the high rate and potential lethality of suicide attempts in BPD, we need a better understanding of proximal and potentially modifiable factors that predict short-term surges in ideation and catalyze suicidal crises (Galynker, 2017). Accordingly, we investigate how interpersonal triggers elicit momentary surges in suicidal ideation - either directly or indirectly via affective or impulsive processes - among people diagnosed with BPD and a history of suicide attempts.
Two key observations emerge from recent studies using ambulatory assessment of the real-time occurrence of suicidal ideation in daily life. First, suicidal ideation severity varies considerably from hour to hour (Ben-Zeev et al., 2012; Hallensleben et al., 2017; Husky et al., 2017; Witte et al., 2006), and covaries with well-known precipitants, which are limited in their ability to predict prospective changes in suicidal ideation (Kleiman et al., 2017; Victor et al., 2019). Second, episodes of suicidal ideation tend to be brief, with participants reporting most episodes to be shorter than an hour (Nock et al., 2009). This descriptive work aligns well with prior theory. The Three Step-Theory, for instance, posits that negative affective states motivate suicidal desire contemporaneously or over seconds to minutes (Klonsky et al., 2017). More specifically, the theory suggests that pain, hopelessness, and suicidal desire are reciprocally influential within a situation, rather than unfolding over longer periods of time. Similarly, Fluid Vulnerability Theory’s concept of a suicidal mode suggests that suicidal crises represent a sudden and intense departure from a baseline state, resulting from complex interactions of mutually influential affective, cognitive, behavioral, and physiological processes (Rudd, 2006).
In BPD, interpersonal stressors often exacerbate emotional instability (Tragesser et al., 2008), yet it is unclear how interpersonal stressors contribute to suicidal crises as they emerge in daily life. On a momentary and daily timescale, interpersonal perceptions of hostility, disaffiliation, and rejection are linked to increases in negative affect (Kaurin et al., 2020; Lazarus et al., 2018; Sadikaj et al. 2013; Sadikaj et al., 2010), aversive tension (Stiglmayr et al., 2005), affective instability, severe anger (Miskewicz et al., 2015), and impulsivity (Coifman et al., 2012; Koenigsberg et al., 2001). Although previous studies have largely suggested that the amplification of affect in BPD is specific to negative affect, some evidence indicates that individuals with BPD also report smaller increases in positive affect in response to agreeable behavior of interaction partners (Sadikaj et al., 2010). Overall, this pattern of reactivity is particularly striking in comparison to healthy controls (Berenson et al., 2011) or depressed patients (Hepp et al., 2017).
Because impulsivity accelerates the transition from thoughts to action, it has long been conceptualized as a central risk factor for suicide attempts in general (Bryan & Rudd, 2006), and in BPD in particular (Brodsky et al., 2006; Soloff et al., 2000). Meta-analytic evidence, however, suggests that the predictive validity of impulsivity for suicide attempts is paradoxically rather modest (Anestis et al., 2014), with little discriminatory value for the differentiation of suicide ideation and attempt (Klonsky & May 2010; May & Klonsky, 2016). However, some evidence derived from a 6-day ecological momentary assessment protocol suggests that impulsivity is related to the likelihood of suicidal behavior and particularly to within-person fluctuations in suicidal ideation, but not to the general tendency to think about suicide (Hadzic et al., 2020). More importantly, previous work has predominantly focused on self-reports of impulsiveness, which are likely relevant to determining long-term suicide risk. State-sensitive indices of impulsivity, in contrast, have the potential to reveal more proximal risk factors for suicidal ideation as it emerges in daily life (Liu et al., 2017).
In contrast, negative affectivity has been more consistently related to the emergence of suicidal ideation (Hallquist & Pilkonis, 2012; Linehan et al., 1993; McGirr et al., 2007; Soloff et al., 2005; Wedig et al., 2012; Yen et al., 2004; 2009). Links et al. (2007) found that in participants with BPD and a history of suicidal behavior, negative mood intensity was significantly related to the intensity of self-reported suicide ideation and to the number of suicidal behaviors during the past year. More recent work further suggests that the within-person link between negative affect and suicidal ideation is enhanced among patients with BPD compared to those without (Mou et al., 2018). These findings are consistent with the notion that suicidal behaviors reflect efforts to escape intense aversive arousal or distress in response to acute stressors (Gratz et al., 2006; Millner et al., 2019), and that the BPD-specific association among both is reinforced by reductions in negative affect (Kleiman et al., 2018; Selby et al., 2009).
Though negative emotions are clearly related to suicidal ideation, positive affect may have incremental predictive value. For instance, Yen et al. (2013) found that over a period of six months low positive affectivity was a stronger prospective predictor for suicidal acts than negative affectivity. Similarly, Hirsch et al.’s (2007) cross-sectional study found that dispositional positive affectivity differentiated older primary care patients with increased levels of suicidal ideation from those without, independently of trait negative affect. In BPD, positive affect may be essential for research on interpersonal precipitants of suicidal ideation, because perceptions of others’ warmth do not necessarily translate to the same amount of increases in positive affect in BPD as in community controls (Sadikaj et al., 2010).
Though a vast body of work has consistently reported momentary contingencies among interpersonal perceptions and affect or state impulsivity in BPD, no study has illustrated how those processes propel real-life suicidal crises. The evidence reviewed above suggests at least two different pathways through which suicidal ideation in BPD may emerge in daily interpersonal interactions. First, interpersonal perceptions of disaffiliation may be directly linked to increased momentary suicidal ideation (Brodsky et al., 2006). Alternatively, suicidal ideation may arise via a cascade of socio-affective processes, where the effect of interpersonal perceptions on momentary suicidal ideation is indirect, depending on enhanced affective reactivity (both positive and negative) or increased impulsivity in response to interpersonal stressors (Sadikaj et al., 2013; Selby et al., 2009).
We test these pathways from the viewpoint of transactional models of suicidal surges that emphasize within-person links among interpersonal perception, affect, impulsivity, and suicidal ideation. This approach can delineate momentary processes that potentially conduce to suicide. Serious suicidal thoughts are rare, episodic events, and will manifest infrequently during a 21-day EMA protocol, even in a high-risk population, which makes achieving adequate power particularly difficult. Therefore, our analyses are based on a case-control sample enriched for history of high-lethality suicide attempts, which are among the most powerful long-term predictors of lethal suicidal behavior (Christiansen & Jensen, 2007; Gibb et al., 2005; Haw et al., 2007; Suominen et al., 2004). Thus, for the purpose of the current study, healthy controls, non-attempters, and attempters were pooled to represent a range of suicidal ideation severity consistent with dimensional conceptualizations of psychopathology (Stanton et al., 2020).
Methods
All study procedures were approved by the Institutional Review Boards of the University of Pittsburgh (STUDY19050210).
Sample.
Participants were drawn from a longitudinal study (Soloff et al., 2017), and recruited from in- and outpatient clinics or the nearby community by advertisement. At enrollment, participants had to be between 18–45 years. Exclusion criteria included a lifetime diagnosis of any psychotic or bipolar disorder, clinical evidence of organic brain disease, physical disorders or treatments with known psychiatric consequence, and IQ<70 measured by the WTAR (Wechsler, 2001).
The sample comprised 153 individuals diagnosed with BPD and 52 healthy control participants (Mage: 33.71, SD=9.43; 80% female). Of these 153 individuals with BPD, 105 had a history of non-zero lethality suicide attempts; 48 reported no past suicide attempts. To increase the reliability of our EMA measurements, participants with fewer than ten reported interactions (N=19) were excluded. This resulted in a final sample size of 186 participants. The majority of the sample identified as white/Caucasian (76%), followed by Black/African American (15%), Asian (4%), Pacific Islander (3%), or other/did not report racial demographics (2%).
BPD diagnoses were based on the ICD-l0-based International Personality Disorder Examination (Loranger et al., 1994). Non-suicidal participants with BPD had no lifetime history of suicide attempts, healthy control participants had no lifetime history of psychiatric disorders, nor suicide attempts, as determined by the SCID/DSM-IV.
Suicide attempters had a history of a self-injurious act with the intent to die within a one-month period prior to completing the study assessments or had a history of a past suicide attempt with strong current SI at the time of study enrollment. Attempters were required to have medically significant attempts, defined by a score of >1 on the Beck Lethality Scale (Beck et al., 1975). High-lethality attempts were defined by a score of >3. For participants with multiple attempts, data for the highest-lethality attempt were used. High-lethality attempts resulted in coma, need for resuscitation, unstable vital signs, penetrating wounds of abdomen or chest, third-degree burns, or major bleeding.
Power estimations.
Power calculations were based on Monte Carlo simulations of fully specified MSEM models with plausible values taken from previous 21-day studies with similar sampling schemes (Sadikaj et al., 2013; Lazarus et al., 2018). These simulations indicated that power would exceed .80 at an alpha level of .05 for each individual within-person effect with person-level sample sizes of N>50, including tests of main effects and variance components.
Momentary Assessments.
Participants completed a 21-day EMA protocol within predefined time windows, using the MetricWire smartphone application, which reminded them to complete surveys via push notifications. If participants indicated that an interaction occurred, they were asked to report on the behavior of one of their interaction partners along with features of the situation. This resulted in N=9009 reported interactions, with an average number of 48 interactions per participant, ranging from 10 to 116 observations overall. On 12% of days participants reported suicidal ideation at least once during the day, which corresponds to a total of 4% of observations that were characterized by suicidal ideation. Participants rated the behavior of their interaction partner/s regarding dominance or warmth, on a sliding scale from − 50 to +50. The dominance scale ranged from “Accommodating/Submissive/Timid” to “Assertive/Dominant/Controlling” and the warmth scale ranged from “Cold/Distant/Hostile” to “Warm/Friendly/Caring.”
Participants also rated the degree to which they felt negative (i.e., nervous, sad, irritated, angry) or positive emotions (i.e., happy, content, excited) derived from the Positive and Negative Affect Schedule (Watson et al., 1988). Items read “How [ADJECTIVE] did you feel during the interaction?”, and ratings were made on a slider scale from 0 (“Not at All”) to 100 (“Extremely”) for each adjective, and an additional item asking about their impulsivity (i.e., “How would you describe your behavior during the interaction?, 0 (“In Control”) to 100 (“Impulsive”).
Suicidal ideation was assessed with two dichotomous items: “Since the interaction,” “Have you wished you were dead or wished you could go to sleep and not wake up?” and “Have you actually had any thoughts of killing yourself?”, derived from the suicidal ideation subscale of the Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2008).
Data Analysis
Because we repeatedly sampled social interactions from participants, our data had a hierarchical structure, such that interactions (within-person level) were nested within individuals (between-person level). Therefore, we used multilevel structural equation modeling (MSEM), which accommodates this data structure. Variables can be between-person (e.g., gender), which only include variance at the between-person level, or within-person (e.g., interpersonal interaction variables), which include variance at both levels. The total variability in interaction variables are partitioned into the between-person variance, reflecting individual differences in average (or trait-level) responses, and within-person variance, reflecting moment-to-moment fluctuations from an individual’s average level. At each level, MSEM can be used to examine associations among variables (Sadikaj et al., 2019). The between-person portion of the model estimates associations among individual differences in each observed variable. For instance, the correlation or regression path between how suicidal a person tends to be with how much negative affect (NA) they typically tend to experience. In contrast, within-person associations reflect how strongly variables are coupled together as they fluctuate from interaction to interaction. Thus, within-person associations reflect dynamic processes (e.g., how much NA is arises at time of an interpersonal stressor). MSEM also allows for the estimation of random slopes (i.e., slopes that vary across individuals), such that individuals can differ in the strength of their within-person associations among variables that are repeatedly assessed in the EMA protocol. That is, some individuals may have a strong within-person link among variables, but others may have a weaker one, or one of an opposite sign. The fixed effects of these slopes represent the average association in the sample, and at the random effects represent individual differences in the extent to which those situational features co-occur across participants.
Importantly, the within-person coefficients reported here represent contemporaneous associations (i.e., within the same wave), although the suicidality items were referenced to “since the interaction.” This modelling decision was based on theoretical and empirical work suggesting that, when the variables assessed fluctuate substantially over the frequency in which they are being monitored, prioritizing lagged associations is not more valuable (Granger, 1969).
Figure 1 provides a schematic overview of the estimated models, along with path annotations as referenced in the results section. Three sets of models were estimated with perceptions of other behavior (i.e., warmth/dominance) predicting suicidal ideation. Model 1 regressed momentary suicidal ideation on perceptions of interaction partner’s behavior at the within-person level (i.e., fluctuations in momentary interpersonal perceptions predicting fluctuations in momentary suicidal ideation) and the between-person level (i.e., individual differences in average perceptions and suicidal ideation). Model 2 introduced negative or positive affect or impulsivity as additional predictors of momentary suicidal ideation at each level, each variable was also regressed on interpersonal perceptions. Finally, Model 3 simultaneously introduced two of the three intermediate variables (i.e., negative and positive affect, impulsivity) as correlated predictors/covariates of momentary suicidal ideation at each level, which permitted the evaluation of unique associations of each predictor with suicidal ideation.
Figure 1.
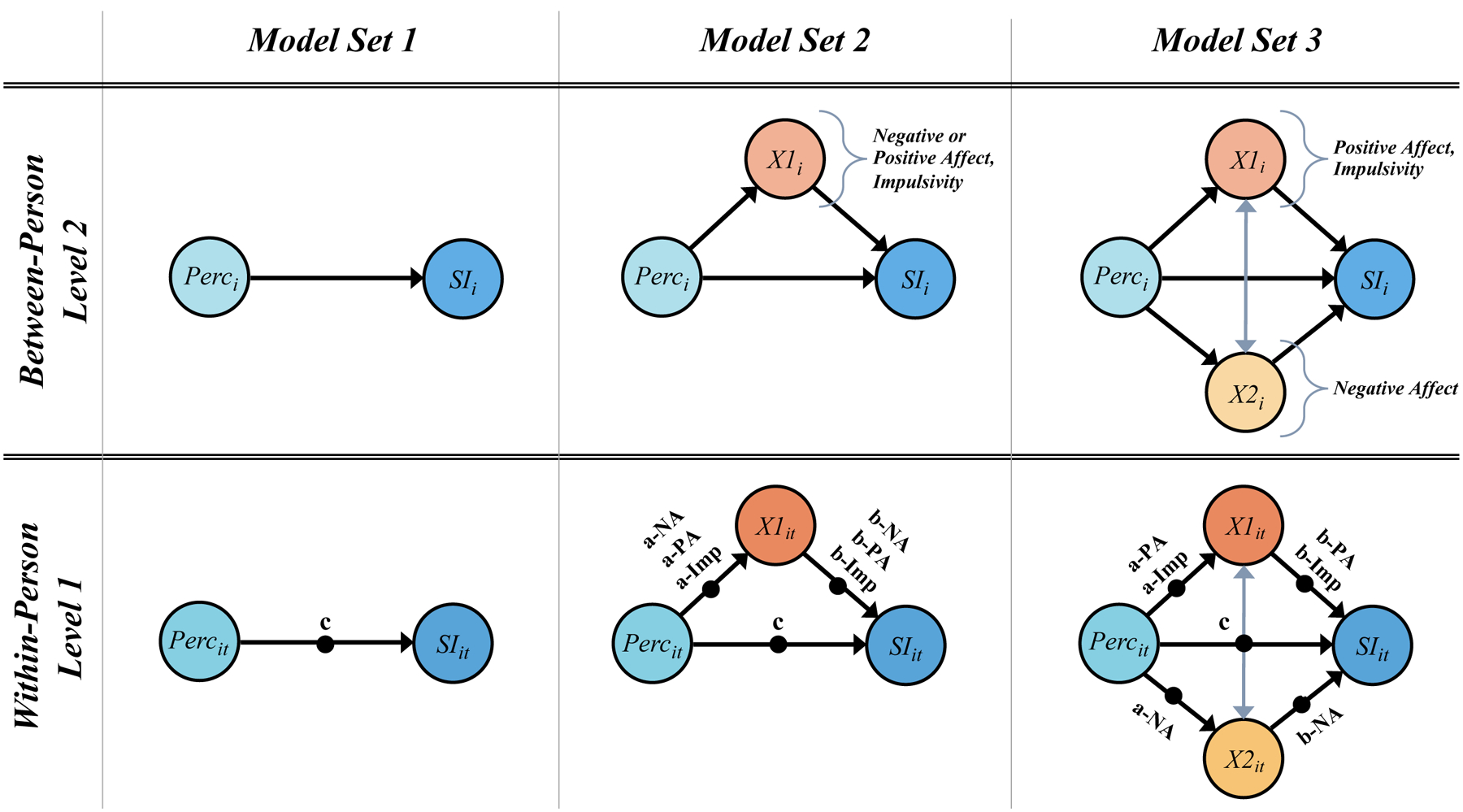
Overview of model sets used for all analyses of suicidal surges including decomposition of observed momentary variables into between-(subscript i) and within-person (subscript t) variance. Note, not all parameters are diagrammed (e.g., residual variances are not depicted). In Model Set 3, at the within-person level, a process was modelled in which perceived warmth or dominance was associated with negative affect and impulsivity or negative and positive affect. In these models, all three variables were independently associated with momentary suicidal ideation, and were allowed to covary. All models controlled for age and gender at the between-person level, and for time and week day at the within-person level. Coefficients for covariates are not presented for parsimony. Single headed arrows indicate regression paths. Filled dots represent random effects. Perc = interpersonal perceptions of warmth or dominance; NA = negative affect; PA = positive affect; Imp = impulsivity; SI = suicidal ideation.
Table 1 summarizes pooled within-person correlations among the variables along with correlations among the random intercepts at the between-person level. Sex (0=female; 1=male) and age (centered on mean age) were also included as covariates in all models at the between-person level. Within-person variables were adjusted for observation number (time centered on mean of observations) and whether the interaction occurred on a weekend to account for possible changes over time and weekly cycles. Along with other parameters not reported in the tables (e.g., residual variances, coefficients for covariates) full specifications and detailed output from all models can be found online at https://osf.io/zpc3u/. All models were estimated in Mplus (version 8.4; Muthén & Muthén, 1998–2019). Bayesian estimation was used because it provides a latent decomposition into within- and between-person variance for both the predictors and outcome variables when random effects are specified. Significance for all model parameters was based on 95% Credibility Intervals (CIs), with CIs that excluded zero indicative of a parameter that differed significantly from zero.
Table 1.
Correlations among study variables at within- and between-person levels.
| SI | warmth | dominance | impulsivity | NA | PA | |
|---|---|---|---|---|---|---|
| within-person | ||||||
| suicidal | ||||||
| ideation | 1 | |||||
| warmth | −.14 | 1 | ||||
| dominance | .06 | −.36 | 1 | |||
| impulsivity | .12 | −.23 | .17 | 1 | ||
| NA | .25 | −.49 | .28 | .38 | 1 | |
| PA | −.20 | .43 | −.20 | −.16 | −.43 | 1 |
| Variance | .62 | .73 | .64 | .46 | .60 | .67 |
| between-person | ||||||
| suicidal | 1 | |||||
| ideation | ||||||
| warmth | −.26 | 1 | ||||
| dominance | .11 | −.15 | 1 | |||
| impulsivity | .41 | −.20 | .30 | 1 | ||
| NA | .57 | −.30 | .26 | .51 | 1 | |
| PA | −.41 | .46 | −.15 | −.15 | −.38 | 1 |
| M (SD) / % | 4% | 26.06 | −.74 | 22.72 | 1.53 | 2.36 |
| Variance | .38 | .27 | .36 | .54 | .40 | .34 |
Note. N=189 (between), N=9100 (within); Between-person variance was calculated as the intraclass correlation coefficient (ICC), which can be interpreted as the proportion of total variance accounted for at the between-person level. Within-person variance is therefore calculated as 1.0–ICC. Bolded values indicate the credibility interval does not contain zero. NA = negative affect, PA = positive affect, SI = suicidal ideation.
Results
Model Set 1
For models examining the effects of others’ perceived warmth on suicidal ideation (Model 1), we found no significant fixed effect at the within-person level (c = .187, CI [− .017,.404], but did at the between-person level (βSI.W = −.184, CI −.357, .000]). Similarly, perceiving interaction partners as more dominant was not associated with suicidal ideation at the within-person (c= −.014, CI [−.167,.145]), but was at the between-person level (βSI.D = .185, CI [.029, .331]). Note that for these and all subsequently reported within-person paths, we found significant random effects indicative of individual differences in these associations.
Model Set 2
Next, momentary affect and impulsivity were added as additional intervening predictors of suicidal ideation to our model. Table 2 provides a detailed overview of estimates for models including perceptions of interpersonal warmth, and Table 3 for estimates based on models including perceptions of dominance.
Table 2.
Key estimates from three individual multi-level structural equation models showing associations among suicidal ideation, negative affect, positive affect, or impulsivity, and perceived warmth of others during interactions (Model Set 2).
| (A) Negative Affect | (B) Positive Affect | (C) Impulsivity | ||||
|---|---|---|---|---|---|---|
| Est (CI) | β | Est (CI) | β | Est (CI) | β | |
| within-person estimates | ||||||
| warmth → SI [c] | .007 [.000, .014] | .120 | .001 [−.005, .010] | .062 | −.002 [−.009, .007] | .014 |
| warmth → NA [a-NA] | −.014 [−.016, −.012] | −.402 | - | - | - | - |
| warmth → PA [a-PA] | - | - | .022 [.019, .024] | .422 | - | - |
| warmth → Imp [a-Imp] | - | - | - | - | −.198 [−.242, −.154] | −.188 |
| NA → SI [b-NA] | .466 [.324, .593] | .204 | - | - | - | - |
| PA → SI [b-PA] | - | - | −.294 [−.458, −.181] | −.230 | - | - |
| Imp → SI [b-Imp] | - | - | - | - | .006 [−.001, .013] | .068 |
| indirect Effect [βab] | −.007 [−.009, −.004] | −.006 [−.010, −.004] | −.001 [−.003, .001] | |||
| between-person estimates | ||||||
| warmth → SI | −.006 [−.028, .012] | −.057 | −.004 [−.030, .020] | −.033 | −.021 [−.046, .003] | −.146 |
| warmth → NA | −.014 [−.020, −.008] | −.326 | - | - | - | - |
| warmth → PA | - | - | .025 [.018, .033] | .474 | - | - |
| warmth → Imp | - | - | - | - | −.345 [−.599, −.090] | −.206 |
| NA → SI | 1.262 [.813, 1.664] | .472 | - | - | - | - |
| PA → SI | - | - | −1.037 [−1.489, −.591] | −.418 | - | - |
| Imp → SI | - | - | - | - | .028 [.014, .043] | .323 |
Note. N=186 (between), N=9009 (within); → indicates regression; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; warmth = perceived warmth of interaction partner, NA = negative affect, PA = positive affect, Imp = impulsivity, SI = suicidal ideation.
Table 3.
Key estimates from three individual multi-level structural equation models showing associations among suicidal ideation, negative affect, positive affect, or impulsivity, and perceived dominance of others during interactions (Model Set 2).
| (A) Negative Affect | (B) Positive Affect | (C) Impulsivity | ||||
|---|---|---|---|---|---|---|
| Estimate (CI) | β | Estimate (CI) | β | Estimate (CI) | β | |
| within-person estimates | ||||||
| dominance → SI [c] | −.004 [−.011, .004] | −.034 | −.000 [−.007, .007] | .010 | .002 [−.005, .008] | .028 |
| dominance → NA [a-NA] | .009 [.007, .012] | .228 | - | - | - | - |
| dominance → PA [a-PA] | - | - | −.010 [−.013, −.007] | −.178 | - | - |
| dominance → Imp [a-Imp] | - | - | - | - | .158 [.112, .201] | .133 |
| NA → SI [b-NA] | .423 [.285, .533] | .196 | - | - | - | - |
| PA → SI [b-PA] | - | - | −.331 [−.452, −.228] | −.233 | - | - |
| Imp → SI [b-Imp] | - | - | - | - | .004 [−.003, .011] | .040 |
| indirect Effect [βab] | .004 [.002, .006] | .003 [.002, .005] | .001 [−.001, .002] | |||
| between-person estimates | ||||||
| dominance → SI | −.003 [−.020, .014] | −.031 | .005 [−.014, .026] | .043 | .002 [−.017, .023] | .019 |
| dominance → NA | .009 [.0034 .015] | .251 | - | - | - | - |
| dominance → PA | - | - | −.007 [−.014, .001] | −.138 | - | - |
| dominance → Imp | - | - | - | - | .432 [.210, .625] | .298 |
| NA → SI | 1.281 [.901, 1.669] | .513 | - | - | - | - |
| PA → SI | - | - | −1.078 [−1.48, −.665] | −.449 | - | - |
| Imp → SI | - | - | - | - | .025 [.014, .037] | .347 |
Note. N=186 (between), N=9009 (within); → indicates regression; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; dominance = perceived dominance of interaction partner, NA = negative affect, PA = positive affect, Imp = impulsivity, SI = suicidal ideation.
Negative Affect.
At the within-person level, the fixed effect of perceptions of others’ warmth negatively predicted negative affect (a-NA), and negative affect predicted suicidal ideation (b-NA), while warmth now predicted SI (c; Table 2A). The indirect effect (ab) was also significant, suggesting that negative affect accounted for the link between perceived coldness and momentary suicidal ideation. At the between-person level, lower average perceptions of warmth were associated with experiencing more negative affect on average, and higher average levels of negative affect were associated with an increased likelihood for suicidal ideation; the link between perceptions of warmth and suicidal ideation, however, was no longer significant, suggesting individual differences in negative affect accounted for this association.
Relationships with perceived dominance were similar but somewhat weaker (Table 3A): interpersonal perceptions predicted negative affect (a-NA), and negative affect predicted suicidal ideation (b-NA). Although the total of the c path was not significant, an indirect effect (ab) emerged, suggesting that negative affect accounted for the link between perceived dominance and momentary suicidal ideation. The same pattern emerged at the between-person level.
Positive Affect.
A very similar pattern with opposing signs emerged for the model including positive affect (Table 2B), such that at the within-person level interpersonal warmth was positively associated with positive affect (a-PA), and positive affect negatively with suicidal ideation (b-PA). Again, the indirect effect (ab) was significant, while the c path did not reach significance. The same pattern emerged at the between-person level.
Models including perceived dominance (Table 3B) revealed a similar pattern of results, with the only exceptions being an expectedly negatively association with positive affect (a-PA), and no between-person level association between perceived dominance and positive affect.
Impulsivity.
For models that included impulsivity (Table 2C), we found a significant negative within-person link between perceptions of warmth and impulsivity (a-Imp), while the effects for the b-Imp path and the c path were not significant. At the between-person level, lower average perceptions of warmth were associated with feeling more impulsive on average, and that higher average levels of impulsivity were associated with an increased likelihood for suicidal ideation.
In models where impulsivity was included to account for the link between dominance and suicidal ideation (Table 3C), only a significant link between interpersonal perceptions and impulsivity emerged (a-Imp). At the between-person level, however, higher average perceptions of dominance were associated with experiencing more impulsivity, and higher average levels of impulsivity were associated with an increased likelihood for suicidal ideation.
Model Set 3
Finally, to test the robustness of our indirect effects, we added negative affect and impulsivity (and negative with positive affect, respectively) simultaneously as covarying predictors of suicidal ideation to our models. Table 4 provides estimates for models including negative affect and impulsivity, and Table 5 summarizes estimates for models including negative and positive affect.
Table 4.
Key estimates from multi-level structural equation models simultaneously estimating associations among suicidal ideation, negative affect and impulsivity, and perceptions of others during interactions (Model Set 3).
| Negative Affect ↔ Impulsivity | ||||
|---|---|---|---|---|
| (A) warmth | (B) dominance | |||
| Estimate (CI) | β | Estimate (CI) | β | |
| within-person estimates | ||||
| perception → SI [c] | .005 [−.002, .013] | .116 | −.003 [−.011, .006] | −.016 |
| perception → NA [a-NA] | −.014 [−.016, −.012] | −.407 | .009 [.007, .012] | .230 |
| perception → Imp [a-Imp] | −.199 [−.244,−.155] | −.188 | .159 [.114, .204] | .133 |
| NA → SI [b-NA] | .467 [.305, .660] | .194 | .470 [.323, .621] | .199 |
| Imp → SI [b-Imp] | .000 [−.009, .007] | .000 | .001 [−.008, .008] | −.011 |
| NA ↔ Imp | 2.640 [2.45, 2.83] | .301 | 3.27 [3.06, 3.50] | .331 |
| between-person estimates | ||||
| perception → SI | −.010 [−.031, .016] | −.073 | −.007 [−.028, .017] | −.054 |
| perception → NA | −.014 [−.020, −.007] | −.316 | .009 [.004, .015] | .248 |
| perception → Imp | −.362 [−.606, −.101] | −.219 | .432 [.213, .642] | .296 |
| NA → SI | 1.264 [.701, 1.809] | .416 | 1.31 [.67, 1.97] | .403 |
| Imp → SI | .007 [−.005, .022] | .095 | .014 [−.006, .030] | .160 |
| NA ↔ Imp | 4.60 [3.19, 6.25] | .494 | 4.50 [3.12, 6.22] | .482 |
Note. N=186 (between), N=9009 (within); → indicates regression, ↔ indicates correlation between variables; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; perception = degree to which interaction partners’ behavior is perceived to be warm / dominant, NA = negative affect, Imp = impulsivity, SI = suicidal ideation.
Table 5.
Key estimates from multi-level structural equation models simultaneously estimating associations among suicidal ideation, negative and positive affect, and perceptions of others during interactions (Model Set 3).
| Negative Affect ↔ Positive Affect | ||||
|---|---|---|---|---|
| (A) warmth | (B) dominance | |||
| Estimate (CI) | β | Estimate (CI) | β | |
| within-person estimates | ||||
| perception → SI [c] | .007 [.000, .015] | .136 | −.003 [−.011, .004] | −.032 |
| perception → NA [a-NA] | −.014 [−.016, −.013] | −.402 | .009 [.007, .012] | .228 |
| perception → PA [a-PA] | .022 [.019, .024] | .422 | −.010 [−.013, −.007] | −.177 |
| NA → SI [b-NA] | .376 [.241, .514] | .178 | .361 [.221, .487] | .168 |
| PA → SI [a-PA] | −.188 [−.333, .−.056] | −.163 | −.177 [−.328, −.021] | −.127 |
| NA ↔ PA | −.119 [−.127, −.110] | −.299 | −.189 [−.200, −.178] | −.389 |
| between-person estimates | ||||
| perception → SI | .007 [−.016, .031] | .052 | −.007 [−.025, .012] | −.060 |
| perception → NA | −.014 [−.021, −.008] | −.322 | .010 [.004, .015] | .249 |
| perception → PA | .026 [.018, .033] | .477 | −.007 [−.014, .000] | −.142 |
| NA → SI | 1.248 [.778, 1.74] | .405 | 1.304 [.854, 1.796] | .430 |
| PA → SI | −.770 [−1.257, −.306] | −.310 | −.695 [−1.20, −.302] | −.288 |
| NA ↔ PA | −.075 [−.123, −.035] | −.278 | −.112 [−.170, −.066] | −.360 |
Note. N=186 (between), N=9009 (within); → indicates regression, ↔ indicates correlation between variables; β parameter estimates are standardized. 95% credibility intervals of unstandardized parameter estimates are in parentheses. Bolded values indicate the credibility interval does not contain zero; perception = degree to which interaction partners’ behavior is perceived to be warm / dominant, NA = negative affect, PA = positive affect, SI = suicidal ideation.
Negative Affect and Impulsivity.
At the within-person level, perceptions of others’ warmth negatively predicted negative affect (a-NA), and impulsivity (a-Imp). Moreover, negative affect (b-NA), but not impulsivity (b-Imp), was related to suicidal ideation. The path between perceived warmth and suicidal ideation, however, was not significant (c). At the between person level, the same pattern of results emerged, and impulsivity and negative affect were positively associated with each other (Table 4A).
Perceptions of others’ dominance were positively related to negative affect (a-NA), and impulsivity (a-Imp) at the within-person level (Table 4B). Again, negative affect (b-NA), but not impulsivity (b-Imp), was related to suicidal ideation, while the path between perceived dominance and suicidal ideation was not significant (c). At the between-person level, the same pattern of results emerged, and impulsivity and negative affect were positively associated with each other.
Negative and Positive Affect.
Finally, when both positive and negative affect were simultaneously added as predictors of suicidal ideation (Table 5A), we found that perceptions of others’ warmth negatively predicted negative affect (a-NA), and positively positive affect (a-PA). Both were uniquely related to suicidal ideation (b-NA; b-PA), albeit in different directions, and positive and negative affect were negatively associated with each other. The path between perceived warmth and suicidal ideation, was not significant. At the between person level, the same pattern of results emerged. For the a-NA and a-PA paths, a converse pattern emerged for our model including perceptions of dominance (Table 5B).
Discussion
We administered intensive longitudinal assessments to BPD patients, many of whom had a history of high-lethality suicide attempts, over several weeks to evaluate relationships between interpersonally stressful encounters, and suicidal surges (i.e., within-person links of affective dysregulation and suicidal ideation) in the moment-to-moment stream of individuals’ daily lives. When aggregated across all interactions, an association between perceived coldness and suicidal ideation emerged, supporting the notion that interpersonal experiences are meaningfully related to suicidal ideation in BPD (Brodsky et al., 2006; Brown et al., 2002). However, this between-person association did not extend to the within-person momentary timescale. Instead, the triggering effect of interpersonal conflicts was indirect, such that greater NA or lower PA in the context of perceived conflict or withdrawal was associated with suicidal ideation. The present study suggests that in people diagnosed with BPD at high risk for suicide, situational interpersonal triggers do not directly elicit suicidal thoughts. Instead, the effect of negative interpersonal experiences on suicidal ideation unfolds indirectly via affective dysregulation.
Moreover, positive and negative affect each uniquely accounted for the link between interpersonal stressors and suicidal ideation, even after adjusting for their covariation, both at the within- and between-person level. This pattern of incremental effects supports theoretical assumptions that affective manifestations of BPD encompass positive as well as negative mood states (Linehan et al., 1993; Russel et al., 2007). It also underlines the notion that suicidal ideation in BPD is driven not only by distress (NA) giving rise to escape motivations (Millner et al., 2019), but also by low PA, which may undermine a persons’ ability to find alternative solutions or put the current crisis in perspective (Baumeister, 1990).
Ratings of impulsivity were unassociated with ideation within-person, and as such they did not explain the indirect effect of negative affect. However, impulsivity did exhibit a momentary relationship with interpersonal perception, consistent with previous work (Coifman et al., 2012). Average impulsivity was associated with average suicidal ideation, but not after adjusting for negative affect consistent with a vast body of work indicating that maladaptive interpersonal behaviors and impulsive coping are related to affective instability among individuals with BPD (Bradley et al., 2007) though longitudinally affective instability is a stronger predictor of suicidal behavior than impulsivity (Yen et al., 2004). Although widely in line with previous work, we note that characteristics of our sample (e.g., mean age) may have attenuated the effect, because impulsive suicidal acts become less common as BPD patients transition into midlife (Wedig et al., 2012; Zanarini et al., 2016).
Additional considerations of our study include that, the direct link between interpersonal perceptions and suicidal ideation was not significant at the within-person level, though the indirect effect through affect was. Although this circumstance has traditionally been discussed to preclude indirect-effect models, more recent writings note that inferences on intervening relationships are justified if the indirect effect carried by the X→M and M→Y paths is significant (MacKinnon et al., 2007), regardless of whether the bivaraite association between X and Y was significant.
Additionally, our study primarily included people diagnosed with BPD, and follow-up studies replicating our findings of the socio-affective dysregulation-suicidal ideation nexus in clinically more diverse samples are needed to corroborate our findings. Yet, BPD is a particularly informative population for the study of suicidal ideation, because it reflects a confluence of internalizing and externalizing psychopathology (Eaton et al., 2011; Crowell et al., 2009; James & Taylor, 2008): Diagnostic criteria such as affective instability relate more strongly to internalizing, while others, such as marked impulsivity, relate more strongly to externalizing forms of psychopathology. Such heterogeneity may imply generalizability to other clinical disorders.
A key question arising from our analyses is whether suicidal surges are a cause, in and of themselves, of suicide attempts. High negative and low positive affect could provide the emotional substrate for suicidal ideation as a proximal risk factor, potentially informing treatment. Alternatively, affective dysregulation may represent a reliable correlate, but not a causal component of suicidal ideation. It could be, for example, that both suicidal ideation and negative affect share risks. For instance, a growing literature suggests that Pavlovian escape biases (from negative affect) invigorate suicidal behavior (Millner et al., 2019) while disrupted decision processes undermine the consideration of deterrents and alternatives (Dombrovski et al., 2013; Brown et al., 2020). Future computational studies could help disentangle the role of affective states from dispositional deficits.
Future intensive longitudinal research on suicidal processes should also consider both the assessment schedule and statistical modeling alternatives. Suicidal ideation is infrequent and episodic, severely complicating its assessment. Although EMA-based sampling strategies seem uniquely capable of capturing meaningful variation in suicidal thought and behavior (Gratch et al., 2020), how best to balance intensity and duration of assessment to capture this meaningful variation is challenging. Relatedly, a recurring debate is whether lagged associations should be prioritized over contemporaneous associations. Although contemporaneous and cross-sectional associations are often treated as the same, in intensive longitudinal data contemporaneous associations imply dynamic processes, which refer to the systematic covariation of variables as they fluctuate from measurement occasion to occasion. Contemporaneous associations capture processes that are assumed to be shorter than the time between assessments, while lagged associations provide a statistical model for processes that are likely ot be longer than the sampling frequency (Granger, 1969). If the process assessed is faster than the assessment interval, prioritizing lagged associations may not be inherently more valuable, particularly when measurements were not evenly spaced in time (e.g., when assessments are randomized throughout the day). Thus, the choice of an assessment and data analytic approach requires theoretical justification, and should be based on estimates of how long episodes of suicidal thinking may last. Research has just begun to estimate the true timescale of an emergent suicidal crisis, and future studies should, therefore, systematically examine theoretically informed real-time sampling and modeling strategies of suicidal ideation.
This is the first reported study using EMA to characterize differential associations among affect and impulsivity with suicidal ideation, contextualized within stressful interpersonal interactions. Our study uncovers how momentary links among socio-affective processes and suicidal thoughts may drive the progression of suicidal crises in daily life: In people diagnosed with BPD at high risk for suicide, situational triggers do not directly elicit suicidal thoughts, but unfold indirectly via affective dysregulation.
Acknowledgements
We are grateful to the patients who took part in this study and to the clinical and research teams who made this work possible.
Financial Support
The study was supported by the National Institute of Mental Health (R01 MH048463).
Footnotes
Conflict of Interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Anestis MD, Soberay KA, Gutierrez PM, Hernández TD, & Joiner TE (2014). Reconsidering the link between impulsivity and suicidal behavior. Personality and Social Psychology Review, 18(4), 366–386. [DOI] [PubMed] [Google Scholar]
- Baumeister RF (1990). Suicide as escape from self. Psychological Review, 97(1), 90–113. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, & Kovacs M (1975). Classification of suicidal behaviors: I. Quantifying intent and medical lethality. The American Journal of Psychiatry, 132(3), 285–287. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Young MA, & Depp CA (2012). Real-time predictors of suicidal ideation: mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1–2), 55–59. [DOI] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafaeli E, Coifman KG, & Paquin NL (2011). The rejection–rage contingency in borderline personality disorder. Journal of Abnormal Psychology, 120(3), 681–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DW, Blum N, Pfohl B, & Hale N (2004). Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. Journal of Personality Disorders, 18(3), 226–239. [DOI] [PubMed] [Google Scholar]
- Bradley R, Conklin CZ, & Westen D (2007). Borderline personality disorder. In O’Donohue W, Fowler KA, & Lilienfeld SO (Eds.), Personality disorders: Toward the DSM-V (p. 167–201). Sage Publications, Inc. [Google Scholar]
- Brodsky BS, Groves SA, Oquendo MA, Mann JJ, & Stanley B (2006). Interpersonal precipitants and suicide attempts in borderline personality disorder. Suicide and Life-Threatening Behavior, 36(3), 313–322. [DOI] [PubMed] [Google Scholar]
- Brown MZ, Comtois KA, & Linehan MM (2002). Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology, 111(1), 198–202. [DOI] [PubMed] [Google Scholar]
- Brown VM, Wilson J, Hallquist MN, Szanto K, & Dombrovski AY (2020). Ventromedial prefrontal value signals and functional connectivity during decision-making in suicidal behavior and impulsivity. Neuropsychopharmacology, 45(6), 1034–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, & Rudd MD (2006). Advances in the assessment of suicide risk. Journal of Clinical Psychology, 62(2), 185–200. [DOI] [PubMed] [Google Scholar]
- Christiansen E, & Frank Jensen B (2007). Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. Australian and New Zealand Journal of Psychiatry, 41(3), 257–265. [DOI] [PubMed] [Google Scholar]
- Coifman KG, Berenson KR, Rafaeli E, & Downey G (2012). From negative to positive and back again: Polarized affective and relational experience in borderline personality disorder. Journal of Abnormal Psychology, 121(3), 668. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan MM (2009). A biosocial developmental model of borderline personality: Elaborating and extending linehan’s theory. Psychological Bulletin, 135(3), 495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Clark L, Reynolds CF, & Siegle GJ (2013). Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry, 70(10), 1020–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, & Hasin DS (2011). Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine, 41(5), 1041–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. [DOI] [PubMed] [Google Scholar]
- Galynker I, Yaseen ZS, Cohen A, Benhamou O, Hawes M, & Briggs J (2017). Prediction of suicidal behavior in high risk psychiatric patients using an assessment of acute suicidal state: The suicide crisis inventory. Depression and anxiety, 34(2), 147–158. [DOI] [PubMed] [Google Scholar]
- Gibb SJ, Beautrais AL, & Fergusson DM (2005). Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. Australian & New Zealand Journal of Psychiatry, 39(1–2), 95–100. [DOI] [PubMed] [Google Scholar]
- Granger CW (1969). Investigating causal relations by econometric models and cross-spectral methods. Econometrica: Journal of the Econometric Society, 424–438. [Google Scholar]
- Gratch I, Choo TH, Galfalvy H, Keilp JG, Itzhaky L, Mann JJ, … & Stanley B (2020). Detecting suicidal thoughts: The power of ecological momentary assessment. Depression and Anxiety, 1–9. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115(4), 850–855. [DOI] [PubMed] [Google Scholar]
- Hadzic A, Spangenberg L, Hallensleben N, Forkmann T, Rath D, Strauß M, … & Glaesmer H (2020). The association of trait impulsivity and suicidal ideation and its fluctuation in the context of the Interpersonal Theory of Suicide. Comprehensive Psychiatry, 98, 152158. [DOI] [PubMed] [Google Scholar]
- Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, & Spangenberg L (2019). Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. European Psychiatry, 56(1), 43–50. [DOI] [PubMed] [Google Scholar]
- Hallquist MN, & Pilkonis PA (2012). Refining the phenotype of borderline personality disorder: Diagnostic criteria and beyond. Personality Disorders: Theory, Research, and Treatment, 3(3), 228–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haw C, Bergen H, Casey D, & Hawton K (2007). Repetition of deliberate self-harm: a study of the characteristics and subsequent deaths in patients presenting to a general hospital according to extent of repetition. Suicide and Life-Threatening Behavior, 37(4), 379–396. [DOI] [PubMed] [Google Scholar]
- Hepp J, Lane SP, Wycoff AM, Carpenter RW, & Trull TJ (2018). Interpersonal stressors and negative affect in individuals with borderline personality disorder and community adults in daily life: A replication and extension. Journal of Abnormal Psychology, 127(2), 183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein PR, Chapman B, & Lyness JM (2007). Positive affect and suicide ideation in older adult primary care patients. Psychology and Aging, 22(2), 380–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky M, Swendsen J, Ionita A, Jaussent I, Genty C, & Courtet P (2017). Predictors of daily life suicidal ideation in adults recently discharged after a serious suicide attempt: a pilot study. Psychiatry research, 256, 79–84. [DOI] [PubMed] [Google Scholar]
- James LM, & Taylor J (2008). Associations between symptoms of borderline personality disorder, externalizing disorders, and suicide-related behaviors. Journal of Psychopathology and Behavioral Assessment, 30(1), 1–9. [Google Scholar]
- Kaurin A, Wright AG, Pilkonis PA, Scott L, Woods WC, Stepp S, & Beeney JE (Manuscript Submitted for Publication). Attachment and Borderline Personality Disorder: Differential Effects on Daily Socio-Affective Processes. 10.31234/osf.io/fncjg [DOI] [PMC free article] [PubMed]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Coppersmith DD, Millner AJ, Franz PJ, Fox KR, & Nock MK (2018). Are suicidal thoughts reinforcing? A preliminary real-time monitoring study on the potential affect regulation function of suicidal thinking. Journal of Affective Disorders, 232, 122–126. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Saffer BY, & Bryan CJ (2018). Ideation-to-action theories of suicide: a conceptual and empirical update. Current Opinion in Psychology, 22, 38–43. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, & May A (2010). Rethinking impulsivity in suicide. Suicide and Life-Threatening Behavior, 40(6), 612–619. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, New AS, Goodman M, Silverman J, … & Siever LJ (2001). Are the interpersonal and identity disturbances in the borderline personality disorder criteria linked to the traits of affective instability and impulsivity?. Journal of Personality Disorders, 15(4), 358–370. [DOI] [PubMed] [Google Scholar]
- Lazarus S, Scott L, Beeney J, Wright AGC, Stepp S, & Pilkonis P (2018). Borderline Personality Disorder Symptoms and Affective Responding to Perceptions of Rejection and Acceptance From Romantic Versus Nonromantic Partners. Personality Disorders: Theory, Research, and Treatment, 9(3), 197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Heard HL, & Armstrong HE (1993). Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of General Psychiatry, 50(12), 971–974. [DOI] [PubMed] [Google Scholar]
- Links PS, Eynan R, Heisel MJ, Barr A, Korzekwa M, McMain S, & Ball JS (2007). Affective instability and suicidal ideation and behavior in patients with borderline personality disorder. Journal of Personality Disorders, 21(1), 72–86. [DOI] [PubMed] [Google Scholar]
- Liu RT, Trout ZM, Hernandez EM, Cheek SM, & Gerlus N (2017). A behavioral and cognitive neuroscience perspective on impulsivity, suicide, and non-suicidal self-injury: Meta-analysis and recommendations for future research. Neuroscience & Biobehavioral Reviews, 83, 440–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, … & Jacobsberg LB (1994). The international personality disorder examination: The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration international pilot study of personality disorders. Archives of General Psychiatry, 51(3), 215–224. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AM, & Klonsky ED (2016). “Impulsive” suicide attempts: What do we really mean? Personality Disorders: Theory, Research, and Treatment, 7(3), 293–302. [DOI] [PubMed] [Google Scholar]
- McGirr A, Paris J, Lesage A, Renaud J, & Turecki G (2007). Risk factors for suicide completion in borderline personality disorder: a case-control study of cluster B comorbidity and impulsive aggression. The Journal of Clinical Psychiatry. [DOI] [PubMed] [Google Scholar]
- Millner AJ, den Ouden HEM, Gershman SJ, Glenn CR, Kearns JC, Bornstein AM, Marx BP, Keane TM, & Nock MK (2019). Suicidal thoughts and behaviors are associated with an increased decision-making bias for active responses to escape aversive states. Journal of Abnormal Psychology, 128(2), 106–118. [DOI] [PubMed] [Google Scholar]
- Miskewicz K, Fleeson W, Arnold EM, Law MK, Mneimne M, & Furr RM (2015). A contingency-oriented approach to understanding borderline personality disorder: Situational triggers and symptoms. Journal of Personality Disorders, 29(4), 486–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mou D, Kleiman EM, Fedor S, Beck S, Huffman JC, & Nock MK (2018). Negative affect is more strongly associated with suicidal thinking among suicidal patients with borderline personality disorder than those without. Journal of Psychiatric Research, 104, 198–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (2019). Mplus User’s Guide (1998–2019). Muthén & Muthén: Los Angeles, CA. [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, … & De Graaf R (2009). Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Medicine, 6(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba SK (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, … & Mann J (2008). Columbia-suicide severity rating scale (C-SSRS). New York, NY: Columbia University Medical Center, 2008. [Google Scholar]
- Rudd MD (2006). Fluid vulnerability theory: A cognitive approach to understanding the process of acute and chronic risk. In Ellis TE (Ed.), Cognition and suicide: Theory, research, and therapy (pp. 355–368). Washington, DC: American Psychological Association. [Google Scholar]
- Russell JJ, Moskowitz DS, Zuroff DC, Sookman D, & Paris J (2007). Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology, 116(3), 578. [DOI] [PubMed] [Google Scholar]
- Sadikaj G, Wright AG, Dunkley D, Zuroff D, & Moskowitz D (2019, October 8). Multilevel Structural Equation Modeling for Intensive Longitudinal Data: A Practical Guide for Personality Researchers. 10.31234/osf.io/hwj9r [DOI]
- Sadikaj G, Moskowitz DS, Russell JJ, Zuroff DC, & Paris J (2013). Quarrelsome behavior in borderline personality disorder: Influence of behavioral and affective reactivity to perceptions of others. Journal of Abnormal Psychology, 122(1), 195–207. [DOI] [PubMed] [Google Scholar]
- Sadikaj G, Russell JJ, Moskowitz DS, & Paris J (2010). Affect dysregulation in individuals with borderline personality disorder: Persistence and interpersonal triggers. Journal of Personality Assessment, 92(6), 490–500. [DOI] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, & Joiner TE Jr. (2009). An exploration of the emotional cascade model in borderline personality disorder. Journal of Abnormal Psychology, 118(2), 375–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soloff PH, & Chiappetta L (2017). Suicidal behavior and psychosocial outcome in borderline personality disorder at 8-year follow-up. Journal of Personality Disorders, 31(6), 774–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soloff PH, Fabio A, Kelly TM, Malone KM, & Mann JJ (2005). High-lethality status in patients with borderline personality disorder. Journal of Personality Disorders, 19(4), 386–399. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lis JA, Kelly T, Cornelius JR, & Ulrich R (1994). Risk factors for suicidal behavior in borderline personality disorder. The American Journal of Psychiatry, 151(9), 1316–1323. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lynch KG, Kelly TM, Malone KM, & Mann JJ (2000). Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. American Journal of Psychiatry, 157(4), 601–608. [DOI] [PubMed] [Google Scholar]
- Stanton K, McDonnell CG, Hayden EP, & Watson D (2020). Transdiagnostic approaches to psychopathology measurement: Recommendations for measure selection, data analysis, and participant recruitment. Journal of Abnormal Psychology, 129(1), 21–28. [DOI] [PubMed] [Google Scholar]
- Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, & Bohus M (2005). Aversive tension in patients with borderline personality disorder: A computer-based controlled field study. Acta Psychiatrica Scandinavica, 111(5), 372–379. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, & Lönnqvist J (2004). Completed suicide after a suicide attempt: a 37-year follow-up study. American Journal of Psychiatry, 161(3), 562–563. [DOI] [PubMed] [Google Scholar]
- Tragesser SL, Lippman LG, Trull TJ, & Barrett KC (2008). Borderline personality disorder features and cognitive, emotional, and predicted behavioral reactions to teasing. Journal of Research in Personality, 42(6), 1512–1523. [Google Scholar]
- Turecki G, Brent DA, Gunnell D, O’Connor RC, Oquendo MA, Pirkis J, & Stanley BH (2019). Suicide and suicide risk. Nature Reviews Disease Primers, 5(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Victor SE, Scott LN, Stepp SD, & Goldstein TR (2019). I Want You to Want Me: Interpersonal Stress and Affective Experiences as Within-Person Predictors of Nonsuicidal Self-Injury and Suicide Urges in Daily Life. Suicide and Life-Threatening Behavior, 49(4), 1157–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wechsler D (2001). Wechsler Test of Adult Reading (WTAR). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wedig MM, Silverman MH, Frankenburg FR, Reich DB, Fitzmaurice G, & Zanarini MC (2012). Predictors of suicide attempts in patients with borderline personality disorder over 16 years of prospective follow-up. Psychological medicine, 42(11), 2395–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, … & Morey LC (2004). Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry, 161(7), 1296–1298. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Skodol AE, Grilo CM, Edelen MO, et al. Personality traits as prospective predictors of suicide attempts. (2009). Acta Psychiatrica Scandinavica, 120(3):222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S, Weinstock LM, Andover MS, Sheets ES, Selby EA, & Spirito A (2013). Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychological Medicine, 43(5), 983–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, & Fitzmaurice GM (2016). Fluidity of the subsyndromal phenomenology of borderline personality disorder over 16 years of prospective follow-up. American Journal of Psychiatry, 173(7), 688–694. [DOI] [PMC free article] [PubMed] [Google Scholar]


