Abstract
Algerian people largely rely on traditional medicine practices as part of a community’s identity. This first ethnobotanical study aimed to quantify and document the wild medicinal plant taxa from four family and the related traditional knowledge in Naâma province, Algeria. The survey was carried out between 2018 and 2020. The socio-demographic data and the use of medicinal species were recorded and collected randomly from 84 indigenous people using pre-prepared questionnaire. The result was evaluated using quantitative indices. A total of 27 medicinal plant species belonging to 21 genera used in the community were mostly recorded. The most represented families were Lamiaceae and Asteraceae (12 species for each of them). The aerial parts were the most frequently used plant part (73 %), while a decoction (34 %), and infusion (31 %) were the major modes of remedy preparation. The species with high UV were Rosmarinus officinalis L. (0.80), Artemisia herba-alba Asso (0.76), and Juniperus phoenicea L. subsp. phoenicea (0.75). Species with highest FL were: Ephedra alata subsp. alenda (Stapf) Trab (100 %), Teucrium polium L. (60 %), and Ballota hirsuta Benth (57.14.5 %). Atractylis caespitosa Desf and Nepeta nepetella subsp.amethystina (Poir.) Briq were newly cited as medicinal plants and have not been recorded previously in Algeria. Artemisia herba-alba Asso and Thymus algeriensis Boiss. & Reut were reported to treat COVID-19 symptoms. The results obtained indicate the richness of the area with medicinal plants as well as knowledge of alternative medicine. The most cited plants could be contained molecules that can be tested for therapeutic uses.
Keywords: Medicinal plants, Traditional medicine, Ethnobotanical, Naâma
Introduction
In Algeria, traditional medicine practices are linked to the history of Arab-Muslim medicine in the Maghreb (North Africa). These practices are a model of transmission of Arab-Muslim medicine. Some therapeutic uses are transmitted directly from religious texts and are still relevant as hijâma (Cupping therapy), Ruqyah (Reciting Quran), and phytotherapy (Saad and Said 2010).
Phytotherapy is known since antiquity as the most easily accessible resource and the basis of health care; has evolved across the ages to become an important knowledge of drug discovery. However, no official strategic plan (regulatory or legislative) has been developed in the country for the integration of traditional medicine into the health care system. The Algerian Public Health Code of 23 October 1976 (158) rendered the practice of medicine without a license an offense; apart from Sec. 364 on the practice of herbalists, no exceptions were made for the practice of traditional medicine (WHO 2001). On other hand, the production and marketing of herbal drugs are permissible to a small extent. More than twenty herbal drug products are commercialized in the pharmaceutical market of Algeria (Bouzabata 2017). Due to the geographical position in the south Mediterranean basin, Algeria with its spacious area is characterized by several climatic regions and diversified vegetation; more than 3139 species of wild and naturalized plants growing in the country become part of a community’s identity. Algerian people used part of these species for different purposes, which are reflected in the widespread use of medicinal plants by herbalists, healers, and people to treat several diseases (Miara et al. 2018). Nevertheless, many geographical regions and ethnic communities in this country like the province of Naâma (South-West of Algeria) have still not been explored. It has a reserve of medicinal species, a background of practice in traditional medicine for humans. Unfortunately, the indigenous knowledge of plants in Naâma and other provinces is inherited and transmitted orally from one generation to the next which makes them vulnerable to loss; Besides, the new generation is not interested to archive it from the older generation (Bouasla and Bouasla 2017).
Ethnobotany carrying great importance for several fields and the most ethnobotany’s contributions and challenges are to close the gap between researcher and indigenous knowledge, to understanding how humans perceive their standing within nature, to boost methodological methods to explore plants from diverse disciplines, and to promote inter-generational continuity (Rodríguez-Calderón et al. 2019). Many ethnobotanical studies were undertaken in the Mediterranean region, especially in Algeria have warned against losing some traditional medicinal knowledge. In this framework, there is an urgent need for studying, recording, and sharing this heritage using an ethnobotanical approach survey to protect it. (Tuttolomondo et al. 2014; Bouasla and Bouasla 2017; Eddouks et al. 2017).
This study aimed to document the ethnobotanical knowledge focusing on ethnomedicine in Naâma province, a strategic region of southwest Algeria, bordered by Morocco. We inventoried, for the first time, all medicinal plants taxa from Lamiaceae, Asteraceae, Cupressaceae, and Ephedraceae using as medicine. The traditional therapeutics were documenting and analyzing using quantitative indices. Data were compared to historical literature carried out in Algeria and the Mediterranean basin.
Materials and methods
Survey area
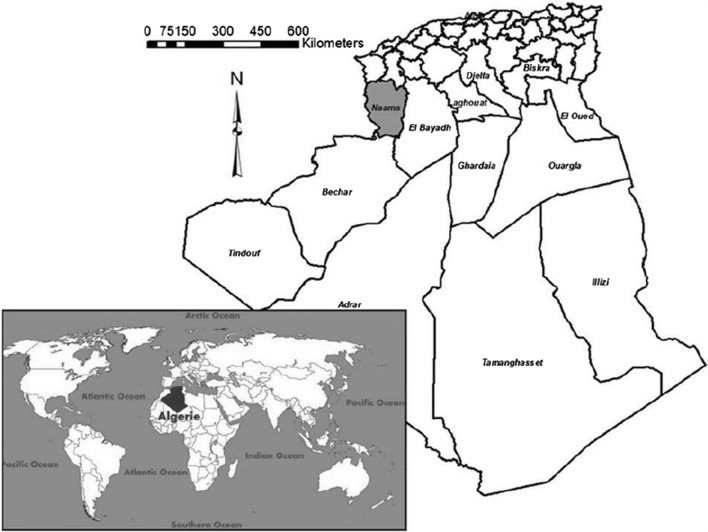
Naâma province is located in the southwest of Algeria (N 33°26′, W 0°54′) (Fig. 1). It is part of the Western Highlands, covers an area of 29.514 Km². It has an estimated population of 192.891 with an average density of about 6.5 Hab/Km2. The area is characterized by an ecological diversity represented by three principal regions: steppe, mountain, and pre-Saharan with 74 %, 12 %, and 14 % of the total area respectively. The climatic year is divided into two main seasons: cold and relatively rainy from November to April, hot and dry from May to October. The rainfall remains weak and irregular in comparison to the north bordering provinces; the temperature ranging from 8 °C in December/January to 31.5 °C in July/August (www.andi.dz/PDF/monographies/NAAMA.pdf).
Fig. 1.
Location map of study area
Data collection
This survey has been done between 2018 and 2020. A total of 84 people were face to face interviews, all people interviewed had been informed about the objective of this study. A semi-structured questionnaire interview was used to record socio-demographic data (gender, age, educational level) and the use of medicinal species (vernacular names, illnesses treated, part used, method of preparation). The plant name has been checked with the plant list database (http://www.theplantlist.org) and the African plant database (http://www.ville-ge.ch/musinfo/bd/cjb/africa/recherche.php). Voucher specimens were confirmed by experimenting botanists and stored in the herbarium of the laboratory of antifungal, antibiotic, Physico-chemical, synthesis, and biological activity, Abou Bekr Belkaid University, Tlemcen, Algeria.
Data analysis
Family use value (FUV)
The FUV was calculated using this formula: FUV = ΣUVs/ns; where ΣUVs is the sum of use value of the species within a family and ns is the total number of species within the same family. The FUV is calculated to identify the importance of plant families (Eddouks et al. 2017).
Use value (UV)
The particular use of UV is to determine the relative significance of the local species. It was used to define the most cited plant species to treat a disease category. UV was calculated using this formula: UV = ΣUi/N; where Ui: number of uses reports per species, and N: total number of informants (Trotter and Logan 1986).
Fidelity level (FL)
The FL value is calculated to estimate the importance of the species for a given purpose. A higher fidelity level (FL) can show that the utilization of plant for specific therapeutic purposes is preferred if respondents cited it frequently. FL was calculated using the following formula: FL= (Np/N)× 100; where Np: is the number of respondents that recommended the use of the plant for a specific disease, and N is the number of respondents that suggested the plant for various illnesses (Phillips 1996).
Results and discussion
Informants’ sociodemographic profile
In this study 84 people were questioned (Table 1), women are more interested in traditional medicine (57.14 %) compared with men. This predominance of women can be explained by their responsibility towards the family in caring for the health of family members, particularly children (Miara et al. 2018). The age range over 60 years is the most frequency range (25 %). Older people have more knowledge and experience than the younger due to the inherent belief that phytotherapy is effective and safe. The younger generation consuming wild species plants as remedies is on the way of extinction due to their interest in modern medicine.
Table 1.
Use of medicinal plants according to socio-demographic factors
| Total | Percentage | |
|---|---|---|
| Gender | ||
| Male | 36 | 42.85 |
| Female | 48 | 57.14 |
| Marital status | ||
| Single | 11 | 13.1 |
| Married | 73 | 86.9 |
| Age groups | ||
| < 20 | 5 | 6 |
| 20–29 | 9 | 11 |
| 30–39 | 14 | 17 |
| 40–49 | 16 | 19 |
| 50–59 | 19 | 23 |
| > 60 | 21 | 25 |
| Educational level | ||
| Illiterate | 34 | 40.48 |
| Primary | 17 | 20.24 |
| Lyceum | 21 | 25 |
| University | 12 | 14.29 |
Part used
The aerial parts (73 %) were more used than the other parts, followed by roots (18 %), and leaves (9 %). Boudjelal et al. (2013) have also registered that the aerial parts are the most used in M’Sila, while other studies reported leaves as the predominant plant part used in surveyed regions of Algeria (Benarba et al. 2015; Bouasla and Bouasla 2017; Miara et al. 2018). It is well known that bioactive principles are contained in the plant’s organs with different concentrations. People in Naâma employ the aerial part based on their traditional heritage which can explain the most uses of this part by the local population.
Method of preparation
The local population uses different forms of preparation. The decoction (34 %) is the most common traditional method described to extract active compounds followed by infusion (31 %), powdering (20 %), maceration (12 %), and cataplasme (3 %). According to Meriem and Hayet (2019), decoction is the method of choice when working with tough and fibrous plants, barks, and roots and with plants that have water-soluble chemicals.
Frequency of families and their use value
Altogether, 27 plant species and 21 genera belonging to plant families Lamiaceae, Asteraceae, Cupressaceae, and Ephedraceae used against several diseases in the community are recorded (Table 2). The most represented families were Lamiaceae and Asteraceae (12 species for each of them), followed by Cupressaceae (2 species), and Ephedraceae (1 species). On the contrary, Ephedraceae (0.56) had a high FUV, followed by Cupressaceae (0.45), Asteraceae (0.36), and Lamiaceae (0.35) (Table 2). Our result indicates that the families which have high FUVs are not necessarily represented by a large number of species in the study area. It confirmed that the use-value of families relies on the preference of the local population to use some plants’ families more than others..
Table 2.
List of wild medicinal plants and their traditional uses
| References / Species (Voucher specimen no) | Local name (Part used) | Method of use | Recommended uses (FL%) | UV | References representing similar uses |
|---|---|---|---|---|---|
| Asteraceae (0.36) | |||||
| Anvillea garcinii subsp. radiata (Coss. & Durieu) Anderb. (LABSAP-6) | Nogd (Ap) | Mac, Pdr | Eye irritations, gastric pain, diabetes, allergy | 0.29 | (Hammiche and Maiza 2006; Kefifa et al. 2018; Hamza et al. 2019; Miara et al. 2019b) |
| Artemisia arborescens (Vaill.) L. (LABSAP-7) | Chehiba (Ap, R) | Inf٫ Dec | Toothache, gingivitis, depurative, gas | 0.29 | (Tuttolomondo et al. 2014) |
| Artemisia campestris L. (LABSAP-8) | Allel (Ap) | Inf, Dec, Pdr | Menstrual cycle problems, hypertension, brucellosis, diabetes | 0.69 | (Hammiche and Maiza 2006; Boudjelal et al. 2013) |
| Artemisia herba-alba Asso. (LABSAP-9) | Chih (Ap) | Inf, Dec٫ Mac | Gastric disorders, liver problems, wormer, muscle spasm, hypertension, COVID-19 | 0.76 | (Eddouks et al. 2002; Boudjelal et al. 2013; Ouelbani et al. 2016; Kharchoufa et al. 2018) |
| Artemisia atlantica Coss. (LABSAP-10) | Chouihiya (Ap, R) | Inf | Intestinal worms, diarrhea, diabetes, anorexia | 0.15 | (Fakchich and Elachouri 2021) |
| Atractylis caespitosa Desf. (LABSAP-11) | Kanouda (Ap,R) | Inf, Dec٫ Mac | Hepatitis, gas, constipation, obesity, rheumatism, tranquilizer | 0.61 | No data |
| Brocchia cinerea (Delile) Vis. (LABSAP-70) | Gartoufa (Ap) | Dec, Mac, Pdr | Asthma, allergy, inflammation, hypertension, eczema | 0.73 | (Abouri et al. 2012; Kefifa et al. 2018) |
| Echinops bovei Boiss. (LABSAP-12) | Tassekra (R) | Inf, Dec | Digestive disorders, incomplete abortion | 0.13 | (Hammiche and Maiza 2006; Miara et al. 2013) |
| Otoglyphis pubescens (Desf.) Pomel. (LABSAP-13) | Ouazouaza (Ap) | Mac, Pdr | Menstrual cycle problems, cough, otitis, tonsillitis | 0.23 | (Hammiche and Maiza 2006) |
| Rhanterium adpressum Coss. & Durieu.(LABSAP-14) | Arfej (L) | Inf٫ Dec | Antidiuretic, bladder disorders, cyst | 0.14 | No data |
| Santolina rosmarinifolia L. (LABSAP-15) | Jaàda (Ap) | Mac, Pdr | Gastric pain (56.25 %), ulcer, wound | 0.25 | (Boudjelal et al. 2013; Miara et al. 2019a) |
| Warionia saharae Benth. & Coss. (LABSAP-16) | Kebbar miise (L, R) | Inf٫ Dec, Pdr | Brucellosis, cardiac problems, rheumatism | 0.15 | (Abouri et al. 2012; Kharchoufa et al. 2018) |
| Cupressaceae (0.45) | |||||
| Juniperus oxycedrus L. subsp. oxycedrus.(LABSAP-34) | Taga (Ap) | Inf, Dec, Mac | Ulcer, kidney problems, bladder disorders, respiratory complications, asthma | 0.15 | (Ouelbani et al. 2016; Miara et al. 2019a) |
| Juniperus phoenicea L. subsp. phoenicea. (LABSAP-35) | Araàr (L) | Inf٫ Dec, Pdr | Ulcer, diarrhea, gas, eczema, wound, burns, inflammation, food poisonings | 0.75 | (Boudjelal et al. 2013; Benarba 2016; Bouasla and Bouasla 2017; Miara et al. 2018, 2019a) |
| Ephedraceae (0.56) | |||||
| Ephedra alata subsp. alenda (Stapf) Trab.(LABSAP-37) | Alenda (Ap) | Dec | Cancer (100 %), goiter | 0.56 | (Miara et al. 2019c) |
| Lamiaceae (0.35) | |||||
| Ajuga iva (L.) Schreb. (LABSAP-44) | Chendgoura (Ap) | Inf, Dec | Hypertension, diabetes, goiter, intestinal worms | 0.33 | (Boudjelal et al. 2013; Miara et al. 2013, 2019a; Benarba et al. 2015; Benarba 2016) |
| Ballota hirsuta Benth. (LABSAP-45) | Meroukt (Ap) | Cat | Migraine (57.14 %), headache, rheumatism | 0.13 | No data |
| Maropsis deserti (de Noé) Pomel. (LABSAP-46) | Garne el kabche (Ap) | Inf, Dec, Pdr | kidney problems, bladder disorders, diuretic, snakebite and scorpion stings, menstrual cycle problems | 0.15 | (Ould el-Hadj et al. 2003; Abouri et al. 2012) |
| Marrubium vulgare L. (LABSAP-47) | Merioua (Ap, R) | Inf, Dec, Cat | Rheumatism (53.33 %), low back pain, infertility, menstrual cycle problems, cough, toothache | 0.33 | (Miara et al. 2013; Benarba 2016; Ouelbani et al. 2016; Hamza et al. 2019) |
| Mentha suaveolens Ehrh. (LABSAP-48) | Timersît (Ap) | Inf, Dec, Pdr | Gas, diarrhea, allergy, bronchitis, fever | 0.17 | (Lahsissene and Kahouadji 2010; Jamila and Mostafa 2014) |
| Mentha pulegium L. (LABSAP-49) | Flîyo (Ap) | Inf, Dec | Gastric pain, diabetes, cough, hypertension | 0.15 | (Bouasla and Bouasla 2017; Eddouks et al. 2017; Kharchoufa et al. 2018) |
| Nepeta nepetella subsp. amethystina (Poir.) Briq. (LABSAP-50) | Napta (Ap) | Inf٫ Dec | Gas (52.94 %), digestive disorders, diuretic, diaphoretic, muscle spasm | 0.33 | No data |
| Rosmarinus officinalis L. (LABSAP-51) | Azir eljabel (Ap) | Inf, Dec, Pdr | Cough, influenza, cold, rheumatism, muscle spasm, cholelithiasis, cholagogue, fever | 0.80 | (Benarba 2016; Bouasla and Bouasla 2017; Eddouks et al. 2017; Kharchoufa et al. 2018) |
| Saccocalyx satureioides Coss. & Durieu. (LABSAP-52) | Azir ermal (Ap) | Inf٫ Dec٫ Pdr | Hypertension, cardiac problems, diabetes, gastritis, hyperglycemia | 0.57 | (Benarba et al. 2015; Hamza et al. 2019) |
| Teucrium polium L. (LABSAP-53) | Jaàda (Ap) | Dec, Mac, Pdr | Digestive disorders (60 %), hypertension, diabetes | 0.17 | (Benarba 2016; Bouasla and Bouasla 2017; Kharchoufa et al. 2018; Miara et al. 2019a) |
| Thymus algeriensis Boiss. & Reut. (LABSAP-54) | Zaàtar (Ap) | Inf, Dec, Pdr | Cold, hypercholesterolemia, inflammation, menstrual cycle problems, COVID-19 | 0.68 | No data |
| Thymus munbyanus subsp. ciliatus (Desf.) Greuter & Burdet. (LABSAP-55) | Djertil (Ap, R) | Inf, Dec | Cough, cold, influenza, inflammation, diabetes | 0.46 | (Boudjelal et al. 2013; Miara et al. 2013, 2018) |
Inf infusion, Dec decoction, cat cataplasm, Mac maceration, Pwd powder, Ap aerial part, L leaves, R root
Medicinal plants used
Species with high used values (UV) were Rosmarinus officinalis L. (0.80), Artemisia herba-alba Asso (0.76), Juniperus phoenicea L. subsp. phoenicea (0.75). This means that these species are the most important medicinal plants used in folk medicine by the population of Naâma to treat ailments, which might be due to their vast distribution in the area study.
In our research area, the use of R. officinalis L. was recorded especially to treat respiratory system problems such as cough, influenza, cold; it is also used for rheumatism, muscle spasm, cholelithiasis, cholagogue, and fever. In the traditional pharmacopeia of Algeria, the same species was recorded as an anti-diabetic, antitumoral, antihypertension, and for treating hepatic diseases (Boudjelal et al. 2013). The most effective bio-active secondary metabolites of R. officinalis L. were phenolic acids, diterpenes, and triterpenes phenolic. Among the isolated phenolic compounds, carnosic acid, carnosol acid, ursolic acid, and rosmarinic acid have been recorded to have major pharmacological effects (Tomi et al. 2016). These compounds except rosmarinic acid increased hPXR (human Pregnane X receptor) target gene expression, transactivated the ligand-binding domain of hPXR and recruited steroid receptor coactivator (SRC)-1, SRC-2, and SRC-3 to the ligand-binding domain of hPXR. The hPXR plays important role in the control of many gene expression linked to inflammatory processes (Seow and Lau 2017).
The most important therapeutic uses of Artemisia herba-alba Asso were those of gastric disorders, liver problems, wormer, muscle spasm, cardiac problems, and hypertension. In Algeria, it is reported to treat digestive system problems (Boudjelal et al. 2013; Miara et al. 2018, 2019a), diabetes (Bouasla and Bouasla 2017), cancer, and respiratory system diseases (Ouelbani et al. 2016). The properties of this plant may be due to its chemical compounds as monoterpenoids, sesquiterpenoids (largely in essential oils), flavonoids, and phenolic compounds (Khlifi et al. 2013; Mohamed et al. 2019) Several studies studied the antispasmodic activity of the essential oil extracted from the plant’s aerial parts. It was found that the administration of this oil relaxed the spontaneous tonus of the rabbit jejunum and reversed the tonic contraction of rat jejunum induced by carbachol (Aziz et al. 2012). Another published study has found that the aqueous extract of this plant has increased the time of gastrointestinal transit in alloxan-treated rabbits and mice (Marrif et al. 1995), and improves insulin sensitivity and hepatic steatosis in rodents-induced metabolic syndrome (Réggami et al. 2019). The same extract at a dose of 150 mg/kg for 20 days significantly reduced the systolic blood pressure in spontaneously hypertensive rats (Zeggwagh et al. 2008).
Recently, the use of Artemisia herba-alba Asso extract to treat the symptom of COVID-19 is under-discussed. Our informants found the effective use of the plant combined with Thymus algeriensis Boiss.& Reut against COVID-19 in the early stage. It is necessary to emphasize that no published data based on clinical experience are supporting the use of these plants, and their effectiveness against coronavirus is unknown. the beneficial effects of Artemisia herba-alba Asso are probably due to its flavonoids as Artemisinin and others. The safe toxicity profile of artemisinin and its immunomodulatory properties on inflammatory diseases and viral infection encourage trying it against COVID-19. Artemisinin, an effective anti-malarial drug, reduces tumor necrosis factor (TNF)-α and interleukin (IL)-6 which are key mediators of acute respiratory distress syndrome (Cheong et al. 2020). In vitro, artemisinin-based combination therapy exerted antiviral activity against clinically isolated SARS-CoV-2 strain (IHUMI-3) in Vero E6 cells; among these, Mefloquine-artesunate showed the best inhibition with 72.1 ± 18.3 % (Gendrot et al. 2020). A clinical study in China showed that a Hemi-synthetic derivative of artemisinin (artesunate) was accompanied by a shorter duration of COVID-19 symptoms than a standard of care (Cheong et al. 2020; Li et al. 2021) found that the treatment with artemisinin-piperaquine could significantly shorten the time to reach undetectable SARS-CoV-2..
Our survey indicated that Juniperus phoenicea L. subsp.phoenicea is used especially to treat ulcer, diarrhea, gas, eczema, wound, burns, inflammation, and food poisonings. Previous surveys in Algeria have shown that this plant is widely used to treat ulcers, intoxication, inflammation, and digestive disorders (Boudjelal et al. 2013; Bouasla and Bouasla 2017; Miara et al. 2018). Various studies have shown that Amentoflavone isolated from Juniperus phoenicea L exhibit a wide range of pharmacological functions (Yu et al. 2017). Administration of amentoflavone in Wistar rats induced ulcerative colitis reduces the extent of the inflammatory colonic injury by decreased mucosal injury score, vascular permeability, and diminished myeloperoxidase and lactate dehydrogenase activity. Furthermore, amentoflavone inhibits colitis by increased superoxide dismutase, glutathione, and decreased lipid peroxidation and nitric oxide. The treatment with this biflavonoid compound reduces the colonic TNF-α, IL-1β, and IL-6 levels as well as the expression of inducible nitric oxide synthase and cyclooxygenase-2. Also, this compound inhibits the activation and translocation of nuclear factor (NF)-κB subunits (p65/p50) (Sakthivel and Guruvayoorappan 2013; Yu et al. 2017).
Our respondents have reported that Brocchia cinerea (Delile) Vis could be utilized in the treatment of asthma, allergy, inflammation, hypertension, and eczema. However, the same species was used by the local population and healers in Algeria to treat pharyngitis, cold, stomach ache, kidney diseases, systemic healing, and migraine (Benarba et al. 2015; Benarba 2016). Recent studies revealed that this plant exhibits various biological activities such as analgesic, cytotoxic, and effect on diabetes. These are related to the presence of chemical substances such as flavonoids, terpenes, and essential oils which are predominated by thujone, eucalyptol, and santolinatriene (Amssayef and Eddouks 2020; Guaouguaou et al. 2020). It have been reported that a single and repeated oral administration of Brocchia cinerea (Delile) Vis aqueous extract at the dose of 20 mg/kg for 15 days, reduced significantly blood glucose and plasma triglycerides levels in both normal and diabetic rats (Amssayef and Eddouks 2020). Other ethnopharmacological uses of the most cited plants by the local population are represented in Table 2.
Fidelity level (FL)
FL of species was determined and we considered those plants whose FL were superior to 50 as important and significant. The plants with less than 5 use reports were excluded. Ephedra alata subsp. alenda (Stapf) Trab having the highest FL (100 %) was used for treating cancer. The same result was found in the study of Illizi in Algerian Sahara (Miara et al. 2019c). Calculation of FL indicated that Teucrium polium L. is the wide species used for treating digestive disorders with an FL of 60 %. Ballota hirsuta Benth has been reported to be used in the treatment of migraine with an FL of (57.14.5 %). Santolina rosmarinifolia L was used for gastric pain having an FL of 56.25 % (Table 2).
Comparison with national and regional ethnobotanical surveys:
Comparative analysis results from 21 previous ethnobotanical surveys are shown in Table 2; in which they reported at minimum one similar therapeutic use from the inventoried plants. Among the 21 works of literature; 13 can give full data of national surveys or herbal practices in Algeria, the other literature can give the most cited data of ethnobotanical studies or herbal practices in surrounding areas such as Morocco and Italy. The number of medicinal plants listed in different provinces of Algeria ranged from 37 to 141 species. 141 species were recorded in Mascara province (Benarba et al.2015), 118 medicinal herbs were recorded in the Tuareg community in the region of Illizi (Miara et al. 2019c), and 102 medicinal plants were recorded in the two provinces of Constantine and Mila (Ouelbani et al. 2016). While the 37 medicinal plants were recorded in Ouargla province (Ould el-Hadj et al. 2003). Our results inventoried 27 medicinal plants belonged to the four botanical families in Naâma. Two species were newly cited as medicinal plants in our study, and their therapeutic use is not cited in the 21 literature above. The plants were Atractylis caespitosa Desf and Nepeta nepetella subsp.amethystina (Poir.) Briq. In Algeria, only one study has investigated the antimicrobial activity and chemical composition of essential oil and hydrosol extract of Nepeta nepetella subsp. amethystina (Poir.) Briq (Bellahsene et al. 2015). These results can contribute to new research for further biological and pharmacological studies..
Some new therapeutic uses that did not mention to those in the previous studies are recorded in our study. Species used to treat brucellosis such as Artemisia campestris L.; species used as anti-inflammatories like Brocchia cinerea (Delile) Vis, Thymus algeriensis Boiss. & Reut, and Thymus munbyanus subsp. ciliatus (Desf.) Greuter & Burdet; and species used to manage hypercholesterolemia included Thymus algeriensis Boiss. & Reut. Other new practices were described for Maropsis deserti (de Noé) Pomel as a diuretic while Rhanterium adpressum Coss. & Durieu as antidiuretic; Otoglyphis pubescens (Desf.) Pomel to treat otitis and tonsillitis; Saccocalyx satureioides Coss. & Durieu as antihypertensive; Ballota hirsuta Benth to heal rheumatism. For skin diseases; the new uses referred to Brocchia cinerea (Delile) Vis to treat eczema. The same plant with Anvillea garcinii subsp. radiata (Coss. & Durieu) Anderb acts as an anti-allergic plant; Ephedra alata subsp. alenda (Stapf) Trab using as an anti-goiter; Juniperus oxycedrus L. subsp.oxycedrus and Santolina rosmarinifolia L. as anti-ulcer agents. Also, the new traditional therapeutics that did not cite any in the previous literature included Artemisia herba-alba Asso, and Thymus algeriensis Boiss. & Reut to manage COVID-19 symptoms. These botanical species should be evaluated phytochemically and pharmaceutically.
Conclusions
The current study is the first survey that records the indigenous knowledge of the use of medicinal plants in the province of Naâma. The results obtained indicate the richness and diversity of the area with medicinal plants. Moreover, local people possess precious quantities of knowledge confirmed by the large number of species cited with their mode of preparation and different part used for manifold therapeutic uses. Some of this heritage was being lost. That is why; this study supports the importance of the preservation of local knowledge and indigenous practices of transferring it to other communities and scientists. It became necessary that the pharmaceutical industry must collaborate with the indigenous traditional people’s possessed collective knowledge of alternative medicine as a source of new drugs.
Acknowledgements
The authors are grateful to the peoples of Naâma for accepting to share their knowledge and practices. Without their contribution, this study would have been impossible.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Miloud Bouafia, Email: miloudbio@gmail.com.
Fouzia Amamou, Email: amamoufouzia@gmail.com.
Mohamed Gherib, Email: gmnaama64@gmail.com.
Mohammed Benaissa, Email: ben_forets@yahoo.fr.
Rachid Azzi, Email: rachidbio@yahoo.fr.
Saïd Nemmiche, Email: snemiche@hotmail.com.
References
- Abouri M, El Mousadik A, Msanda F, et al. An ethnobotanical survey of medicinal plants used in the Tata Province, Morocco. Int J Med Plant Res. 2012;1:99–123. [Google Scholar]
- Amssayef A, Eddouks M. Antihyperglycemic, antihyperlipidemic and antioxidant effects of cotula cinerea (del) in normal and streptozotocin-induced diabetic rats. Endocr Metab Immune Disord Drug Targets. 2020;20:1. doi: 10.2174/1871530320666200513081312. [DOI] [PubMed] [Google Scholar]
- Aziz M, Karim A, El-Ouariachi EM, et al. Relaxant effect of essential oil of Artemisia herba-alba Asso. on rodent jejunum contractions. Sci Pharm. 2012;80:457–467. doi: 10.3797/scipharm.1106-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellahsene C, Bendahou M, Khadir A, et al. Antimicrobial activity and chemical composition of essential oil and hydrosol extract of Nepeta nepetella subsp. amethystina (Poir.) Briq. from Algeria. J Appl Pharm Sci. 2015;5:21–25. doi: 10.7324/JAPS.2015.50904. [DOI] [Google Scholar]
- Benarba B. Medicinal plants used by traditional healers from south-west Algeria: an ethnobotanical study. J Intercult Ethnopharmacol. 2016;5:320–330. doi: 10.5455/jice.20160814115725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benarba B, Belabid L, Righi K, et al. Ethnobotanical study of medicinal plants used by traditional healers in Mascara (North West of Algeria) J Ethnopharmacol. 2015;175:626–637. doi: 10.1016/j.jep.2015.09.030. [DOI] [PubMed] [Google Scholar]
- Bouasla A, Bouasla I. Ethnobotanical survey of medicinal plants in northeastern of Algeria. Phytomedicine. 2017;36:68–81. doi: 10.1016/j.phymed.2017.09.007. [DOI] [PubMed] [Google Scholar]
- Boudjelal A, Henchiri C, Sari M, et al. Herbalists and wild medicinal plants in M’Sila (North Algeria): an ethnopharmacology survey. J Ethnopharmacol. 2013;148:395–402. doi: 10.1016/j.jep.2013.03.082. [DOI] [PubMed] [Google Scholar]
- Bouzabata A. Les médicaments à base de plantes en Algérie: réglementation et enregistrement. Phytothérapie. 2017;15:401–408. doi: 10.1007/s10298-016-1089-5. [DOI] [Google Scholar]
- Cheong DHJ, Tan DWS, Wong FWS, Tran T. Anti-malarial drug, artemisinin and its derivatives for the treatment of respiratory diseases. Pharmacol Res. 2020;158:104901. doi: 10.1016/j.phrs.2020.104901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddouks M, Maghrani M, Lemhadri A, Ouahidi M-L, Jouad H. Ethnopharmacological survey of medicinal plants used for the treatment of diabetes mellitus, hypertension and cardiac diseases in the south-east region of Morocco (Tafilalet) J Ethnopharmacol. 2002;82:97–103. doi: 10.1016/S0378-8741(02)00164-2. [DOI] [PubMed] [Google Scholar]
- Eddouks M, Ajebli M, Hebi M. Ethnopharmacological survey of medicinal plants used in Daraa-Tafilalet region (Province of Errachidia), Morocco. J Ethnopharmacol. 2017;198:516–530. doi: 10.1016/j.jep.2016.12.017. [DOI] [PubMed] [Google Scholar]
- Fakchich J, Elachouri M (2021) An overview on ethnobotanico-pharmacological studies carried out in Morocco from 1991 to 2015: Systematic review (part 1). J Ethnopharmacol 267:113200. 10.1016/j.jep.2020.113200 [DOI] [PubMed]
- Gendrot M, Duflot I, Boxberger M, et al. Antimalarial artemisinin-based combination therapies (ACT) and COVID-19 in Africa: in vitro inhibition of SARS-CoV-2 replication by mefloquine-artesunate. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guaouguaou FE, Bebaha MAA, Taghzouti K, Es-Safi NE. Phytochemical investigation, acute toxicity, central analgesic and antioxidant activities of extracts and essential oil of Cotula cinerea Del (Asteraceae) Curr Bioact Compd. 2020;16:164–173. doi: 10.2174/1573407214666180821115826. [DOI] [Google Scholar]
- Hammiche V, Maiza K. Traditional medicine in Central Sahara: pharmacopoeia of Tassili N’ajjer. J Ethnopharmacol. 2006;105:358–367. doi: 10.1016/j.jep.2005.11.028. [DOI] [PubMed] [Google Scholar]
- Hamza N, Berke B, Umar A, et al. A review of Algerian medicinal plants used in the treatment of diabetes. J Ethnopharmacol. 2019;238:111841. doi: 10.1016/j.jep.2019.111841. [DOI] [PubMed] [Google Scholar]
- Jamila F, Mostafa E. Ethnobotanical survey of medicinal plants used by people in Oriental Morocco to manage various ailments. J Ethnopharmacol. 2014;154:76–87. doi: 10.1016/j.jep.2014.03.016. [DOI] [PubMed] [Google Scholar]
- Kefifa A, Saidi A, Hachem K, Mehalhal O. An ethnobotanical survey and quantitative study of indigenous medicinal plants used in the Algerian semi-arid region. Phytothérapie. 2018 doi: 10.3166/phyto-2018-0077. [DOI] [Google Scholar]
- Kharchoufa L, Merrouni IA, Yamani A, Elachouri M. Profile on medicinal plants used by the people of north Eastern Morocco: toxicity concerns. Toxicon. 2018;154:90–113. doi: 10.1016/j.toxicon.2018.09.003. [DOI] [PubMed] [Google Scholar]
- Khlifi D, Sghaier RM, Amouri S, et al. Composition and anti-oxidant, anti-cancer and anti-inflammatory activities of Artemisia herba-alba, Ruta chalpensis L. and Peganum harmala L. Food Chem Toxicol. 2013;55:202–208. doi: 10.1016/j.fct.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Lahsissene H, Kahouadji A. Analyse ethnobotanique des plantes médicinales et aromatiques de la flore marocaine: cas de la région de Zaër 1. Phytothérapie. 2010;8:202–209. doi: 10.1007/s10298-010-0569-2. [DOI] [Google Scholar]
- Li G, Yuan M, Li H, et al. Safety and efficacy of artemisinin-piperaquine for treatment of COVID-19: an open-label, non-randomised and controlled trial. Int J Antimicrob Agents. 2021;57:106216. doi: 10.1016/j.ijantimicag.2020.106216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrif HI, Ali BH, Hassan KM. Some pharmacological studies on Artemisia herba-alba (Asso.) in rabbits and mice. J Ethnopharmacol. 1995;49:51–55. doi: 10.1016/0378-8741(95)01302-4. [DOI] [PubMed] [Google Scholar]
- Meriem E, Hayet E. Are the plants used in Algerian traditional medicine effective?: Assessment of the antibacterial, anti-inflammatory and anti-oxidative effects of three plants used in Algerian traditional medicine; Olea europaea, Glycyrrhiza glabra and Ocimum basilicum. Med Technol J. 2019;3:443–452. doi: 10.26415/2572-004X-vol3iss3p443-452. [DOI] [Google Scholar]
- Miara MD, Hammou MA, Aoul SH. Phytothérapie et taxonomie des plantes médicinales spontanées dans la région de Tiaret (Algérie) Phytotherapie. 2013;11:206–218. doi: 10.1007/s10298-013-0789-3. [DOI] [Google Scholar]
- Miara MD, Bendif H, Ait Hammou M, Teixidor-Toneu I. Ethnobotanical survey of medicinal plants used by nomadic peoples in the Algerian steppe. J Ethnopharmacol. 2018;219:248–256. doi: 10.1016/j.jep.2018.03.011. [DOI] [PubMed] [Google Scholar]
- Miara MD, Bendif H, Rebbas K, et al. Medicinal plants and their traditional uses in the highland region of Bordj Bou Arreridj (Northeast Algeria) J Herb Med. 2019;16:100262. doi: 10.1016/j.hermed.2019.100262. [DOI] [Google Scholar]
- Miara MD, Bendif H, Ouabed A et al (2019b) Ethnoveterinary remedies used in the Algerian steppe: Exploring the relationship with traditional human herbal medicine. J Ethnopharmacol 244:112–164. 10.1016/j.jep.2019.112164 [DOI] [PubMed]
- Miara MD, Teixidor-Toneu I, Sahnoun T, Bendif H, Ait Hammou M (2019c) Herbal remedies and traditional knowledge of the Tuareg community in the region of Illizi (Algerian Sahara). J Arid Environ 167:65–73. 10.1016/j.jaridenv.2019.04.020
- Mohamed HRH, Amer M, Faky ASAE. Growth retardation and apoptotic death of tumor cells by Artemisia herba-alba oral administration in Ehrlich solid carcinoma bearing mice. Rev Bras Farmacogn. 2019;29:763–772. doi: 10.1016/j.bjp.2019.06.007. [DOI] [Google Scholar]
- Ouelbani R, Bensari S, Mouas TN, Khelifi D. Ethnobotanical investigations on plants used in folk medicine in the regions of Constantine and Mila (North-East of Algeria) J Ethnopharmacol. 2016;194:196–218. doi: 10.1016/j.jep.2016.08.016. [DOI] [PubMed] [Google Scholar]
- Ould el-Hadj M, Hadj-Mahammed M, Zabeirou H. Place des plantes spontanées dans la médicine traditionnelle de la région de Ouargla (Sahara septentrional est) Courr du Savoir. 2003;3:47–51. [Google Scholar]
- Phillips OL. Advances in economic botany. Berlin: JSTOR; 1996. Some quantitative methods for analyzing ethnobotanical knowledge; pp. 171–197. [Google Scholar]
- Réggami Y, Benkhaled A, Boudjelal A, et al. Artemisia herba-alba aqueous extract improves insulin sensitivity and hepatic steatosis in rodent model of fructose-induced metabolic syndrome. Arch Physiol Biochem. 2019 doi: 10.1080/13813455.2019.1659825. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Calderón Á, Muñoz JA, Moreno D, Celis M. Describing and diffusing the ethnobotanical knowledge of Bogotá D.C. (Colombia) through an online tool focused on common names of plants. Acta Bot Bras. 2019;33:303–314. doi: 10.1590/0102-33062018abb0337.. [DOI] [Google Scholar]
- Saad B, Said O. Tradition and Perspectives of Greco-Arab and Islamic Herbal Medicine. Herb Suppl. 2010 doi: 10.1002/9780470910108.ch10. [DOI] [Google Scholar]
- Sakthivel KM, Guruvayoorappan C. Amentoflavone inhibits iNOS, COX-2 expression and modulates cytokine profile, NF-κB signal transduction pathways in rats with ulcerative colitis. Int Immunopharmacol. 2013;17:907–916. doi: 10.1016/j.intimp.2013.09.022. [DOI] [PubMed] [Google Scholar]
- Seow CL, Lau AJ. Differential activation of pregnane X receptor by carnosic acid, carnosol, ursolic acid, and rosmarinic acid. Pharmacol Res. 2017;120:23–33. doi: 10.1016/j.phrs.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Tomi K, Kitao M, Konishi N, et al. Enantioselective GC–MS analysis of volatile components from rosemary (Rosmarinus officinalis L.) essential oils and hydrosols. Biosci Biotechnol Biochem. 2016;80:840–847. doi: 10.1080/09168451.2016.1146066. [DOI] [PubMed] [Google Scholar]
- Trotter RT, Logan MH. Informant consensus: a new approach for identifying potentially effective medicinal plants. In: Etkin NL, editor. Plants and indigenous medicine and diet, biobehavioral approaches. New York: Routledge; 1986. pp. 91–112. [Google Scholar]
- Tuttolomondo T, Licata M, Leto C, et al. Ethnobotanical investigation on wild medicinal plants in the Monti Sicani Regional Park (Sicily, Italy) J Ethnopharmacol. 2014;153:568–586. doi: 10.1016/j.jep.2014.02.032. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization) Legal status of traditional medicine and complementary/alternative medicine: a worldwide review. Geneva: No.WHO/EDM/TRM/2001.2; 2001. [Google Scholar]
- Yu S, Yan H, Zhang L, et al. A review on the phytochemistry, pharmacology, and pharmacokinetics of amentoflavone, a naturally-occurring biflavonoid. Molecules. 2017;22:299. doi: 10.3390/molecules22020299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeggwagh NA, Farid O, Michel JB, Eddouks M. Cardiovascular effect of Artemisia herba alba aqueous extract in spontaneously hypertensive rats. Methods Find Exp Clin Pharmacol. 2008;30:375. doi: 10.1358/mf.2008.30.5.1186081. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.