Abstract
The COVID-19 pandemic has disproportionately impacted communities of color and highlighted longstanding racial health inequities. Communities of color also report higher rates of medical mistrust driven by histories of medical mistreatment and continued experiences of discrimination and systemic racism. Medical mistrust may exacerbate COVID-19 disparities. This study utilizes the Behavior Model for Vulnerable Populations to investigate predictors of medical mistrust during the COVID-19 pandemic among urban youth of color. Minority youth (N = 105) were recruited from community organizations in Kansas City, Missouri to complete an online survey between May and June 2020. Multiple linear regressions were performed to estimate the effect of personal characteristics, family and community resources, and COVID-19 need-based factors on medical mistrust. Results indicated that loneliness, financial insecurity (e.g., job loss, loss of income) due to the COVID-19 pandemic, and eligibility for free or reduced lunch predicted medical mistrust. Insurance status, neighborhood median household income, social support, and perceived COVID-19 risk were not significantly associated with medical mistrust. Future research and policies are necessary to address systemic factors that perpetuate medical mistrust among youth of color.
Keywords: Medical Mistrust, COVID-19, Loneliness, Youth, Minority Health
Implications.
Practice: Trusted community-based organizations can play an important role in addressing loneliness among youth of color by providing virtual and socially distanced opportunities to connect during the COVID-19 pandemic.
Policy: Polices to mitigate financial hardships among communities of color during the COVID-19 pandemic are crucial to reduce economic disparities which contribute to increased medical mistrust.
Research: Future research is critically needed to develop and evaluate effective and sustainable interventions and polices to dismantle systemic racism and promote health equity.
INTRODUCTION
The novel coronavirus SARS-CoV-2 (COVID-19) pandemic has disproportionately impacted communities of color [1, 2]. In the United States, Black people are at increased risk for COVID-19 incidence, hospitalization, and death compared to Whites [3–5]. Racial disparities in COVID-19 related outcomes are driven by a variety of intersecting factors rooted in institutionalized racism including discrimination, access to quality healthcare, financial inequities, and characteristics related to occupation and housing (e.g., essential work, crowded or unstable living conditions) [5–8]. In addition, communities of color have also been shown to experience higher rates of medical mistrust compared to White communities [9]. Previous research has found that medical mistrust is linked to lower healthcare utilization and poor health outcomes [10–12]. As such, medical mistrust may deter people of color from accessing COVID-19 testing and receipt of adequate medical care. Additionally, a recent study found that Black adults reported greater hesitancy to get vaccinated for COVID-19 compared to non-Hispanic Whites [13]. This is consistent with research showing lower rates of vaccine uptake among racial and ethnic minorities [14, 15]. In order to address the continued disproportionate burden of COVID-19 on communities of color, greater attention and appropriate strategies to mitigate barriers to care, such as medical mistrust, are needed.
Medical mistrust has been defined as “the tendency to distrust medical systems and personnel believed to represent the dominant culture in a given society” [9]. Medical mistrust is distinct from merely a lack of trust between a patient and provider [9, 16]. Instead, medical mistrust is inclusive of broader, often group-based, attitudes and beliefs about health systems. To date, the majority of research on medical mistrust has examined its impacts on health behaviors and outcomes [9, 12]. Previous research has found a strong relationship between demographic factors related to race, ethnicity, and social-economic status and medical mistrust, but the mechanisms and experiences which underly medical mistrust are still relatively understudied [9]. In the United States, experiences of medical mistrust among people of color, particularly among African Americans, are rooted in histories of medical experimentation and mistreatment [17]. The Tuskegee Syphilis Study, in which African American participants were deprived of effective treatment for syphilis, is the most cited historical cause of medical mistrust [18]. However, medical abuses towards African Americans pre-dates the Tuskegee study and can be traced to medical experimentation on slaves in the early 1800s [18, 19]. Historical traumas passed down through generations provide crucial context for understanding medical mistrust among communities of color [20]. Moreover, modern day experiences of discrimination and institutionalized racism continue to cause and perpetuate experiences of medical mistrust among communities of color [21–24]. Prior research has shown patients of color are less likely to be admitted to the hospital after an emergency department visit [25, 26], classified as an immediate/urgent case [25, 26], and treated for pain [27, 28]. Additionally, studies have demonstrated that physician implicit bias impacts clinic decision-making [29, 30]. As such, it is unsurprising that communities of color report high rates of medical mistrust [9]. In addition, institutional factors, including experiences outside of the context of healthcare, such as negative experiences with law enforcement, have also been found to influence medical mistrust. For instance, one study found that experiences of police brutality were predictive of increased medical mistrust [31], suggesting the impact of higher-order, systemic factors on medical mistrust. As such, many scholars have positioned medical mistrust as a crucial social determinant of health which should be studied through a social-ecological lens [32, 33].
The Behavioral Model for Vulnerable Populations offers a theoretical framework to consider how individual-level factors, social determinants of health, and characteristics of health systems influence healthcare utilization [34]. This model, adapted from the Andersen Behavior Model of Health Services Utilization [35], posits that health behaviors are influenced by factors in three domains: (1) predisposing characteristics of individuals, including demographics such as age, sex, and race; (2) enabling factors which influence access to healthcare including family and community resources; and (3) need-based factors which include perceived health status and health risks [35]. The Behavioral Model for Vulnerable Populations builds on the Andersen model by also including specific constructs across each domain that are pertinent to the health of vulnerable populations. For example, the adapted model includes predisposing factors such as childhood characteristics including history of mental illness and substance abuse, and additional enabling factors such as family and community resources related to hunger, transportation, and social services [34]. This model has been previously applied in research with a variety of populations including communities experiencing homelessness [36, 37], co-occurring mental illnesses [38], and previous incarceration [39].
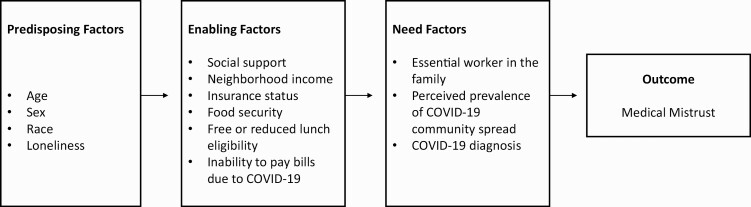
The purpose of the current study is to utilize the Behavioral Model for Vulnerable Populations to examine factors that predict medical mistrust among youth of color during the COVID-19 pandemic. We selected factors in each domain of the model that we thought were relevant to our priority population, urban youth of color, during the COVID-19 pandemic. Our conceptual model is depicted in Figure 1. While this model has been traditionally applied to outcomes such as healthcare utilization, medical mistrust was chosen as the primary proximal outcome of interest not only because it has been shown to be predictive of healthcare utilization [10–12], but also because there is an increasing call to better understand experiences and social determinants of health which influence medical mistrust [9, 31]. We specifically selected factors expected to be pertinent to COVID-19. For example, the Behavioral Model for Vulnerable Populations includes not only demographic characteristics but also factors such as mental illness and psychological resources in the predisposing domain [34]. As such, we specifically selected loneliness as an indicator of mental health to model, given the rise in isolation due to COVID-19. Similarly, for the need-based domain, we selected factors relevant to perceived risk for COVID-19, such as if a family member were an essential worker.
Fig 1.
Conceptual model adapted from the behavioral model for vulnerable populations.
Urban youth of color were the priority population for this study, because few studies have examined medical mistrust among youth [40, 41]. The majority of research focused on medical mistrust has been conducted among adult populations, despite the fact that youth of color report additional barriers to accessing quality healthcare [42, 43]. The COVID-19 pandemic has also led to unique stressors for youth including social distancing practices and remote education [44]). Given the established importance of peer social connections for youth mental health, COVID-19 related isolation may have particularly harmful effects on youth mental health due to their development stage [44, 45]. Furthermore, the shift to remote education has affected the delivery of services normally provided by schools, including food and mental health services [46, 47]. As such, the aim of this study is to utilize the Behavioral Model for Vulnerable Populations to estimate the relationship between predisposing characteristics, enabling factors including social determinants of health, and COVID-19-specific need factors and medical mistrust among urban youth of color.
METHODS
Procedures and Participants
A convenience sample of racial and ethnic minority youth were recruited from community organizations in Kansas City, Missouri to complete an online survey about their experience coping with the COVID-19 pandemic. Survey data collection took place between May and June 2020. We contacted our community partners that serve urban youth regarding an anonymous survey opportunity and provided general background on the purpose of the study. Email addresses of youth were provided to the researchers and interested participants were screened for eligibility using a brief online survey via REDCap. Eligibility criteria required that youth be aged 13–21, identify as a racial or ethnic minority, and be able to read and complete a survey in English. Youth participants then provided consent to participate (parental permission was not necessary per IRB determined minimal risk of the study) and completed all survey questions via REDCap. To keep surveys anonymous and due to IRB determination of minimal risk, parents/guardians were not informed whether their child participated in the survey. Participants were compensated with a $25 gift card. All study procedures were approved by the University of Missouri, Kansas City Institutional Review Board.
Measures
Medical Mistrust
Medical mistrust was measured by the Medical Mistrust Index (MMI), a 7-item self-report scale [48]. This scale has been previously used with diverse populations including with Black and Hispanic adult participants [12, 48, 49]. However, to our knowledge the MMI has not been previously validated with youth of color. Items were measured on a 4-point Likert scale, where higher scores indicated higher levels of mistrust. Cronbach’s alpha in our sample = 0.75.
Predisposing Factors
Predisposing factors measured in this study included age, sex, and loneliness. Loneliness was measured by the UCLA Loneliness Scale, a 20-item self-report measure [50]. This scale has been previously validated for an adolescent population that included minority youth [51]. Items were assessed on a 4-point Likert scale, where higher scores indicated higher levels of loneliness. Cronbach’s alpha in our sample = 0.96.
Enabling Factors
Enabling factors measured in this study included social support, insurance status, free or reduced lunch eligibility, food insecurity, neighborhood income, and inability to pay bills due to COVID-19. Social support was measured by the Multidimensional Perceived Support Scale, a 12-item self-report measure [52]. This scale has been previously validated among a population of urban adolescents who were primarily Black. [53] Items were assessed on a 7-point Likert scale, where higher scores indicated higher levels of social support. Cronbach’s alpha in our sample = 0.95. Neighborhood income was based on median household income by zip code. Zip codes with a household mean income below $43,000 were categorized as low-income, and those above the $43,000 threshold were categorized as high-income. The $43,000 cut-point was chosen because it approximated the median neighborhood income in our sample. All other enabling variables were single-item measures. Financial insecurity due to COVID-19 was measured by the following question drawn from the Centers for Disease Control and Prevention (CDC) COVID-19 Community Survey Question Bank [54]: “In the past two weeks, has your family experienced the following as a result of COVID-19?” Answer options included, “Not enough money to pay rent,” “Not enough money to pay for gas,” and “Not enough money to pay for food.” If participants answered “yes” to any of these three questions, they were categorized as reporting financial insecurity due to COVID-19.
COVID-19 Need-Based Factors
COVID-19 need-based factors were measured by single-items also drawn from the CDC COVID-19 Community Survey Question Bank [54]. Variables included reporting if a family member was an essential worker, if a family member had been diagnosed with COVID-19, and perceived COVID-19 community spread in the participant’s area.
Statistical Analyses
Descriptive analyses (means, standard deviations, and frequencies) were performed to characterize the sample. Histograms were created for all continuous variables to examine distributions. All models were assessed for missing data. Missingness rates varied across sets of models: less than 4% for all predisposing models, 3.8%–11.4% for enabling models, and 16.3%-20% for models including both enabling and need-based factors. No individual item was missing more than 8.6%. The higher level of missingness for the two need-based models is primarily driven by the following variables: worry over food insecurity (N-missing = 9), neighborhood median income (N-missing = 7), and essential worker status (N-missing = 5). Given the relatively low missingness across the majority of models, complete case analyses were performed. The aim of this study was to estimate if personal characteristics, social determinants of health, and COVID-19 related need-based factors predicted medical mistrust. Analyses followed the study’s conceptual model (see Figure 1) which was adapted from the Behavioral Model for Vulnerable Populations [34]. Due to limited variance, variables for race and COVID-19 diagnosis were excluded from models. Simple linear regressions were conducted to assess the crude association between predisposing, enabling and COVID-19 need-based variables with medical mistrust. To minimize potential bias due to the study’s small sample size, adjusted models were sequentially developed in which we controlled for the theoretically most proximal layer (e.g., the association between enabling factors and medical mistrust was assessed, controlling for all predisposing factors, and the association between need factors and medical mistrust was assessed, controlling for all enabling factors). All models were estimated with SAS version 9.4.
RESULTS
One hundred five participants completed the survey. Respondents were primarily African American (n = 87, 83.7%), and the majority of respondents were female (n = 69, 65.7%). Of the enabling factors examined, half of the sample was eligible for free or reduced lunch, and 27% of participants reported food insecurity in last the 12 months. One third of the sample (34.3%) reported that they either did not have health insurance or did not know if they had health insurance. Approximately 20% of participants reported family financial strain due to the pandemic including the inability to pay rent, gas, or food bills in the previous two weeks. With respect to COVID-19 need-based characteristics, the majority of participants (59.0%) reported that they had at least one family member employed as an essential worker (e.g., healthcare employee, grocery store worker, postal service). Only three participants (3.0%) reported that they had a family member who had been diagnosed with COVID-19. About half of the sample (49.5%) reported that they “didn’t know” if there was COVID-19 community spread in their area. See complete summary of descriptive statistics in Table 1.
Table 1.
Participant characteristics
| Total (N = 105) | |
|---|---|
| Predisposing Factors | |
| Gender, n (%) | |
| Female | 69 (65.7%) |
| Male | 36 (34.3%) |
| Age, mean (SD) | 16.47 (1.60) |
| Race, n (%) | |
| African American/Black | 87 (83.7%) |
| Hispanic American | 7 (6.7%) |
| Asian American | 3 (2.9%) |
| Native Hawaiian/Other Pacific Islander | 3 (2.9%) |
| White | 3 (2.9%) |
| Other | 1 (1.0%) |
| Ethnicity, n (%) | |
| Non-Hispanic | 90 (86.5%) |
| Hispanic or Latino Origin | 14 (13.5%) |
| Loneliness, mean (SD) | 20.54 (15.01) |
| Enabling Factors | |
| Insurance status, n (%) | |
| No Insurance/Don’t Know | 36 (34.3%) |
| Public Health Insurance | 38 (36.2%) |
| Private Insurance | 31 (29.5%) |
| Zip code, n (%) | |
| Low Income (Household income, $43,000) | 49 (50.0%) |
| High Income | 49 (50.0%) |
| Worry of possible food insecurity (in past 12 months), n (%) | |
| Never True | 62 (64.6%) |
| Sometimes/Always True | 34 (35.4%) |
| Food insecurity (in past 12 months), n (%) | |
| Never True | 73 (73.0%) |
| Sometimes/Always True | 27 (27.0%) |
| Free and reduced lunch, n (%) | |
| No | 50 (50.0%) |
| Yes | 50 (50.0%) |
| Inability to pay rent/gas/food in the last 2 weeks as a result of COVID-19, n (%) | |
| No | 83 (79.1%) |
| Yes | 22 (21.0%) |
| Social support, mean (SD) | 63.21 (14.70) |
| Need Factors | |
| Family member who is an essential worker, n (%) | |
| No | 41 (41.0%) |
| Yes | 59 (59.0%) |
| Family member who has been diagnosed with COVID-19, n (%) | |
| No | 93 (92.1%) |
| Yes | 3 (3.0 %) |
| Don’t Know | 5 (5.0 %) |
| Perception of community COVID-19 spread | |
| No | 40 (38.1%) |
| Yes | 13 (12.4%) |
| Don’t Know | 52 (49.5%) |
| Outcome | |
| Medical mistrust, mean (SD) | 19.42 (3.08) |
Categories that do not add up to N = 105 indicate that missing values have been omitted.
Possible scores for loneliness range from 0 to 60, where higher scores indicate higher levels of loneliness. Possible scores for social support range from 12 to 84, where higher scores indicate higher levels of social support. Possible scores for medical mistrust range from 7 to 28 where higher scores indicate higher levels of mistrust.
For the study’s main analyses, crude and adjusted model estimates are reported in Tables 2 & 3. Loneliness was the only predisposing factor significantly associated with medical mistrust in the crude model (β = 0.04, SE = 0.02, 95% CI [0.001, 0.08]). However, when controlling for age and gender, the effect of loneliness was no longer statistically significant (p = .054), though, the effect size and standard error remained the same in the adjusted model. With respect to enabling factors, inability to pay bills due to the COVID-19 pandemic was significantly associated with medical mistrust in both the crude model (β = 1.713, SE = 0.72, 95% CI [0.31, 3.12]) and adjusted model (β = 1.337, SE = 0.62, 95% CI [0.11, 2.40]). Free and reduced lunch eligibility was also significantly associated with medical mistrust in the adjusted model (β = 1.63, SE = 0.76, 95% CI [0.15, 3.12]) when controlling for predisposing factors. No additional enabling factors or any need-based factors were significantly associated with medical mistrust in any of the models reported in Tables 2 & 3.
Table 2.
Crude models indicating the association between predisposing, enabling, and need-based factors and medical mistrust
| Medical Mistrust | |||
|---|---|---|---|
| β | SE | 95% CI | |
| Predisposing | |||
| Gender | −0.215 | 0.63 | [−1.45,1.02] |
| Age | 0.181 | 0.19 | [−0.19,0.55] |
| Loneliness | 0.040 | 0.02 | [0.001,0.08] |
| Depression | −0.048 | 0.05 | [−0.15,0.05] |
| Enabling | |||
| Insurance status | −0.25 | 0.63 | [−1.48,0.98] |
| Zip code | −1.082 | 0.62 | [−2.30, 0.14] |
| Worry of food insecurity | −0.047 | 0.58 | [−1.19, 1.10] |
| Food insecurity | 0.313 | 0.67 | [−0.99,1.62] |
| Free and reduced lunch | 1.040 | 0.60 | [−0.13,2.21] |
| Inability to pay bills due to COVID-19 | 1.713 | 0.72 | [0.31, 3.12] |
| Social support | −0.026 | 0.02 | [−0.07,0.01] |
| Need | |||
| Essential worker | 0.788 | 0.63 | [−0.44, 2.02] |
| Prevalence of community spread | |||
| Yes | 1.715 | 0.96 | [−0.17, 3.61] |
| Don’t know | 0.619 | 0.64 | [−0.63, 1.86] |
Table 3.
Adjusted models indicating the association between predisposing, enabling, and need-based factors and medical mistrust
| Medical Mistrust | |||
|---|---|---|---|
| β | SE | 95% CI | |
| Predisposing adjusting for other predisposing factors | |||
| Gender | −0.124 | −1.37 | [−1.37, 1.12] |
| Age | 0.084 | 0.29 | [−0.30,0.46] |
| Loneliness | 0.040 | 0.02 | [−0.0008, 0.12] |
| Enabling factors adjusting for predisposing factors (gender, age, loneliness) | |||
| Insurance status | −0.330 | 0.65 | [−1.60, 0.94] |
| Zip code | −1.023 | 0.63 | [−2.26, 0.21] |
| Worry of food insecurity | −0.032 | 0.62 | [−1.24, 1.18] |
| Food insecurity | 0.295 | 0.70 | [−1.09, 1.67] |
| Free and reduced lunch | 1.337 | 0.62 | [0.11, 2.40] |
| Inability to pay bills due to COVID-19 | 1.636 | 0.76 | [0.15, 3.12] |
| Social support | −0.007 | 0.02 | [−0.05, 0.04] |
| Need-factors adjusting for enabling factors | |||
| Essential worker | 0.569 | 0.60 | [−0.60, 1.74] |
| Prevalence of community spread | |||
| Yes | 1.243 | 1.09 | [−0.89, 3.37] |
| Don’t know | 0.360 | 0.63 | [−0.87, 1.59] |
DISCUSSION
The COVID-19 pandemic has not only led to increased morbidity and mortality, but also financial hardships and increased isolation resulting from social distancing recommendations. Our study found that unique stressors from the COVID-19 pandemic are associated with medical mistrust among urban youth of color. Loneliness was the only predisposing factor significantly positively associated with medical mistrust in our crude model. This effect lost statistical significance (p = .054) when controlling for gender and age, but this is likely due to limited power as a result of the study sample size. While the effect of loneliness should be interpreted with caution, it may still have meaningful implications. There is prior evidence that loneliness has increased more among adolescents relative to other age groups during the COVID-19 pandemic [55], and it appears that increased loneliness may be associated with greater medical mistrust. Prior research has shown that those who have others in their support network who engage in a medical treatment or health behavior (e.g., uptake of pre-exposure prophylaxis [PrEP]) tend to have less hesitancy in engaging in the health-related behavior themselves [56]. As such, if youth of color feel isolated from their social network during the COIVD-19 pandemic, they are presumably less likely to share information and support related to medical care access and decision making.
Two of the measured enabling factors – the inability to pay bills due to COVID-19 and free or reduced lunch eligibility – were also significantly positively associated with medical mistrust when controlling for predisposing factors, indicating the influence of family social economic status on medical mistrust. The COVID-19 pandemic has led to increased financial insecurity due to increased rates of unemployment, and there is evidence that COVID-19 has disproportionately impacted minority unemployment [57]. Previous research suggests that job loss and financial insecurity during the COVID-19 pandemic is associated with greater risk for depression [58]. Our study results add to this literature by indicating that COVID-19-related financial hardships are associated with medical mistrust. Prior research has found that distrust in one institution, such as experiences with police, breeds distrust in other institutions including healthcare [23, 31, 59]. As such, one possible explanation for our finding is that financial hardships due to COVID-19 may well impact trust in government, employers, or schools to provide equitable educational and economic opportunities, and distrust in these institutions could carry over to increased distrust of healthcare institutions.
Furthermore, the finding regarding free or reduced lunch eligibility is also potentially of particular importance for youth during the COVID-19 pandemic, because youth are frequently unable to attend in-person school where they may receive services such as free or reduced lunch [47]. There are examples of many school systems and organizations that have developed programs during the COIVD-19 pandemic to ensure continued services such as pick-up and delivery meal options [60]. Innovations such as these are critical to support the nutritional needs of youth and families during the COVID-19 pandemic, and may potentially offer broader benefit including mitigating mistrust of public institutions.
Contrary to the study hypotheses, none of the COVID-19 need-based factors (e.g., family measures of who is an essential worker, perception of community spread) measured in our study were significantly associated with medical mistrust. However, there was too little variance in our sample to estimate the effect of having a family member diagnosed with COVID-19. Future research should examine the impact of COVID-19 diagnosis on medical mistrust. While not significantly associated with medical mistrust, it was of note that almost half the sample reported that they did not know if there was COVID-19 community spread in their area. This finding is consistent with another nationally representative survey which found racial disparities in knowledge about COVID-19 risk and transmission, with African American participants reporting significantly lower knowledge compared to non-Hispanic White participants [61]. A recent randomized control trial did find, however, that physician-delivered prevention messaging led to increased COVID-19 knowledge among Black and Latinx participants. For Black participants, information seeking behaviors increased when the messaging had come from a racial/ethnically concordant physician [62]. This research underscores the importance of diversifying the healthcare work force as a long-term strategy toward mitigating medical mistrust and promoting health equity.
To our knowledge, this is the first paper to examine predictors of medical mistrust among youth during the COVID-19 pandemic. This paper is subject to notable strengths and limitations. The study is enhanced by the use of Behavioral Model for Vulnerable Populations to guide study analyses, especially given the novel and exploratory nature of the data. This study was limited, however, by the small sample size. Future research should examine predictors of medical mistrust during the ongoing COVID-19 pandemic among a larger sample of youth of color. Missing data could have led to increased bias in our estimates, though, the two models with the highest degree of missingness were the need-based models which were not the primary focus of this study. This study was also limited by the cross-sectional design wherein we were unable to investigate temporal changes due to the onset of the COVID-19 pandemic. In an effort to reduce participant burden, many of the enabling and need-based factors were assessed by single-item measures which are inherently subject to lower validity and reliability compared to a validated scale. In addition, adolescents may be less likely to accurately report on family economic status compared with adults [63, 64]. Prior research finds that adolescents may under-report characteristics like food insecurity due to parental buffering [65]. Nevertheless, when trying to understand indicators of medical mistrust among youth, perceptions of financial insecurity are likely an important stressor in and of itself. Lastly, the relationship between factors in each domain (e.g., predisposing, enabling, and need-based factors) may be more nuanced than we were able to capture through our modeling. Future research should examine issues of cumulative risk between factors in each domain, as well as consider additional factors pertinent to these domains such as housing insecurity. In addition, it would be useful for future research to examine predictors of medical mistrust among youth of color living in rural areas, who have been found to have higher rates of poverty compared to national rates [66, 67].
We cannot underestimate the importance of mitigating medical mistrust during the ongoing COVID-19 pandemic. Medical mistrust among people of color is rooted in longstanding histories of medical abuse and poor-quality medical care [17], and it is more important than ever to address the systemic factors which continue to perpetuate mistrust. Medical mistrust may impact individuals’ willingness to adhere to evidence-based public health guidelines to reduce risk of COVID-19 exposure and access to COVID-19 testing and medical care [33]. There is evidence from the HIV epidemic that mistrust among social networks was associated with a decrease in HIV antiretroviral adherence among African American men [68]. Though, some research has found that while Black people have significantly higher fear around participating in biomedical research compared to Whites, that they are just as likely to ultimately participate in biomedical research [69]. Emerging data does indicate, however, that young adults, Black adults, Hispanic adults, and those living in urban areas are the most likely groups to report that they want to “wait and see” how the COVID-19 vaccine works for others before getting vaccinated themselves [70]. As such, efforts to mitigate medical mistrust among youth of color is especially critical to promote uptake of the COVID-19 vaccine. There is prior evidence indicating that partnering with community-based or faith-based organizations to provide vaccinations and other health services is effective in improving knowledge and utilization among minority communities [71–75]. More work on this front is critically needed, however, as current national data shows that the COVID-19 vaccination rate among White people is significantly higher than rates for Hispanic and Black people [76]. Therefore, we recommend integrating COIVD-19 testing and vaccination services in community-based settings that have already established trusting relationships with communities of color.
In conclusion, our study found that loneliness, financial insecurity, and free or reduced lunch eligibility are associated with increased medical mistrust. In the short term, steps should be taken to promote social connections among youth of color in ways that are in keeping with COVID-19 public health guidelines. Prior research indicates that youth participation in out-of-school programs leads to improvement in a host of wellbeing indicators, including social cohesion and prosocial behavior [77]. As such, efforts by community-based organizations to support youth social engagement through virtual or socially-distanced means may be especially useful at this time. Our study findings also contribute to the literature highlighting the crucial role systemic and economic-driven inequalities have on medical mistrust perspectives among youth of color. Given the wealth of prior evidence indicating that systemic racism is a driver of racial economic inequality and disproportionate COVID-19 burden, we conclude that to address determinants of medical mistrust, public health research, practice, and policy must do a better job in addressing factors which perpetuate poverty and systemic racism [33, 78–80].
Acknowledgements
The authors are grateful to the community-based organizations who supported this study, and we would specifically like to acknowledge Paige O’Connor, the Founder and Former Director of Youth Ambassadors.
Funding Sources: This research was supported by the Robert Wood Johnson Foundation (Grant No. 76141).
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All procedures performed were approved by the Institutional Review Board at the University of Missouri-Kansas City.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Transparency Statement
1. Study registration. This study was not formally registered.
2. Analytic plan pre-registration. The analysis plan was not formally pre-registered.
3. Data availability. De-identified data from this study are not available in a pubic archive. Requests to access de-identified data can be sent to the corresponding author, but will require approval from IRB and community partners.
4. Analytic Code. Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author.
5. Materials availability. Materials used to conduct the study are not publicly available.
References
- 1. Jones J, Sullivan PS, Sanchez TH, et al. Similarities and differences in COVID-19 awareness, concern, and symptoms by race and ethnicity in the United States: Cross-Sectional Survey. J Med Internet Res. 2020;22(7):e20001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. Eclinicalmedicine. 2020;29:100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rodriguez F, Solomon N, de Lemos JA, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry. Circulation. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black Patients and White Patients with COVID-19. N Engl J Med. 2020;382(26):2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cordes J, Castro MC. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spatial Spatio-temporal Epidemiol. 2020;34:100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. [DOI] [PubMed] [Google Scholar]
- 8. Egede LE, Walker RJ. Structural racism, social risk factors, and COVID-19 — A dangerous convergence for Black Americans. N Engl J Med. 2020;383(12):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Benkert R, Cuevas A, Thompson HS, Dove-Meadows E, Knuckles D. Ubiquitous yet unclear: a systematic review of medical mistrust. Behav Med. 2019;45(2):86–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57 Suppl 1:146–161. [DOI] [PubMed] [Google Scholar]
- 11. Kalichman SC, Eaton L, Kalichman MO, Grebler T, Merely C, Welles B. Race-based medical mistrust, medication beliefs and HIV treatment adherence: test of a mediation model in people living with HIV/AIDS. J Behav Med. 2016;39(6):1056–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Williamson LD, Bigman CA. A systematic review of medical mistrust measures. Patient Educ Couns. 2018;101(10):1786–1794. [DOI] [PubMed] [Google Scholar]
- 13. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann Intern Med. 2020;173(12):964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Amboree TL, Darkoh C. Barriers to human Papillomavirus Vaccine uptake among racial/ethnic minorities: a systematic review. J Racial Ethnic Health Disparities. 2020;1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Almario CV, May FP, Maxwell AE, Ren W, Ponce NA, Spiegel BM. Persistent racial and ethnic disparities in flu vaccination coverage: Results from a population-based study. Am J Infect Control. 2016;44(9):1004–1009. [DOI] [PubMed] [Google Scholar]
- 16. Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45(2):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14(2):56–60. [PubMed] [Google Scholar]
- 18. Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87(11):1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Savitt TL. The use of blacks for medical experimentation and demonstration in the Old South. J South Hist. 1982;48(3):331–348. [PubMed] [Google Scholar]
- 20. Alsan M, Wanamaker M, Hardeman RR. The Tuskegee study of untreated Syphilis: a case study in peripheral trauma with implications for health professionals. J Gen Intern Med. 2020;35(1):322–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. López‐Cevallos DF, Harvey SM, Warren JT. Medical mistrust, perceived discrimination, and satisfaction with health care among young‐adult rural Latinos. The Journal of Rural Health. 2014;30(4):344–351. [DOI] [PubMed] [Google Scholar]
- 22. Hammond WP. Psychosocial correlates of medical mistrust among African American men. Am J Community Psychol. 2010;45(1-2):87–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williamson LD, Smith MA, Bigman CA. Does discrimination breed mistrust? Examining the role of mediated and non-mediated discrimination experiences in medical mistrust. J Health Commun. 2019;24(10):791–799. [DOI] [PubMed] [Google Scholar]
- 24. Bajaj SS, Stanford FC. Beyond Tuskegee — Vaccine distrust and everyday racism. N Engl J Med. 2021;384(5):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhang X, Carabello M, Hill T, He K, Friese CR, Mahajan P. Racial and ethnic disparities in emergency department care and health outcomes among children in the United States. Front Pediatr. 2019;7:525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang X, Carabello M, Hill T, Bell SA, Stephenson R, Mahajan P. Trends of racial/ethnic differences in emergency department care outcomes among adults in the United States from 2005 to 2016. Front Med (Lausanne). 2020;7:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4(3):277–294. [DOI] [PubMed] [Google Scholar]
- 29. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alang S, McAlpine DD, Hardeman R. Police brutality and mistrust in medical institutions. J Racial Ethnic Health Disparits. 2020;7(4):760–768. [DOI] [PubMed] [Google Scholar]
- 32. Jaiswal J. Whose responsibility is it to dismantle medical mistrust? Future directions for researchers and health care providers. Behav Med. 2019;45(2):188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jaiswal J, LoSchiavo C, Perlman DC. Disinformation, misinformation and inequality-driven mistrust in the time of COVID-19: lessons unlearned from AIDS denialism. AIDS Behav. 2020;24(10):2776–2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 35. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124. [PubMed] [Google Scholar]
- 36. Stein JA, Andersen R, Gelberg L. Applying the Gelberg-Andersen Behavioral Model for vulnerable populations to health services utilization in homeless women. J Health Psychol. 2007;12(5):791–804. [DOI] [PubMed] [Google Scholar]
- 37. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Andersen Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Small LFF. Use of mental health services among people with co-occurring disorders and other mental health co-morbidities: employing the Behavioral Model of Vulnerable Populations. Mental Health Substance Use. 2010;3(2):81–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Oser CB, Bunting AM, Pullen E, Stevens-Watkins D. African American Female Offender’s use of alternative and traditional health services after re-entry: examining the behavioral model for vulnerable populations. J Health Care Poor Underserved. 2016;27(2A):120–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Arrington-Sanders R, Hailey-Fair K, Wirtz AL, et al. Role of structural marginalization, HIV Stigma, and mistrust on HIV prevention and treatment among young Black Latinx Men who have sex with men and transgender women: perspectives from youth service providers. AIDS Patient Care STDS. 2020;34(1):7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Oakley LP, López-Cevallos DF, Harvey SM. The association of cultural and structural factors with perceived medical mistrust among Young Adult Latinos in rural Oregon. Behav Med. 2019;45(2):118–127. [DOI] [PubMed] [Google Scholar]
- 42. Elster A, Jarosik J, VanGeest J, Fleming M. Racial and ethnic disparities in health care for adolescents: a systematic review of the literature. Arch Pediatr Adolesc Med. 2003;157(9):867–874. [DOI] [PubMed] [Google Scholar]
- 43. Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. 2010;19(4):759–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of CoViD-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(22):8479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wiguna T, Anindyajati G, Kaligis F, et al. Brief research report on adolescent mental well-being and school closures during the COVID-19 Pandemic in Indonesia. Front Psychiatry. 2020;11:598756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. [DOI] [PubMed] [Google Scholar]
- 47. Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Health. 2020;5(5):e243–e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sheppard VB, Huei-Yu Wang J, Hurtado-de-Mendoza A, Sutton AL, LaVeist TA. Psychometric properties of the Medical Mistrust Index (MMI) in Latina Immigrants. Behav Med. 2019;45(2):128–133. [DOI] [PubMed] [Google Scholar]
- 50. Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39(3):472–480. [DOI] [PubMed] [Google Scholar]
- 51. Mahon NE, Yarcheski TJ, Yarcheski A. Validation of the revised UCLA Loneliness Scale for adolescents. Res Nurs Health. 1995;18(3):263–270. [DOI] [PubMed] [Google Scholar]
- 52. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Personality Assess. 1998;52(1):30–41. [Google Scholar]
- 53. Canty-Mitchell J, Zimet GD. Psychometric properties of the multidimensional scale of perceived social support in urban adolescents. Am J Community Psychol. 2000;28(3):391–400. [DOI] [PubMed] [Google Scholar]
- 54. CDC. 2020. COVID-19 Community response survey guidance. Available at https://www.nlm.nih.gov/dr2/JHU_COVID-19_Community_Response_Survey_v1.3.pdf. Accessibility verified May 1, 2021.
- 55. Luchetti M, Lee JH, Aschwanden D, et al. The trajectory of loneliness in response to COVID-19. Am Psychol. 2020;75(7):897–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nydegger LA, Dickson-Gomez J, Ko Ko T. A longitudinal, qualitative exploration of perceived HIV Risk, healthcare experiences, and social support as facilitators and barriers to PrEP adoption among Black Women. Aids Behav. 2021;25:582–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Couch KA, Fairlie RW, Xu H. Early evidence of the impacts of COVID-19 on minority unemployment. J Public Econ. 2020;192:104287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 Pandemic are associated with worse mental health. J Occup Environ Med. 2020;62(9):686–691. [DOI] [PubMed] [Google Scholar]
- 59. Alang S, McAlpine D, McClain M, Hardeman R. Police brutality, medical mistrust and unmet need for medical care. Prev Med Rep. 2021;22:101361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kinsey EW, Hecht AA, Dunn CG, et al. School closures during COVID-19: opportunities for innovation in meal service. Am J Public Health. 2020;110(11):1635–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in Coronavirus 2019 reported incidence, knowledge, and behavior among US Adults. JAMA Netw Open. 2020;3(6):e2012403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Alsan M, Stanford FC, Banerjee A, et al. Comparison of knowledge and information-seeking behavior after general COVID-19 public health messages and messages tailored for Black and Latinx Communities: a randomized controlled trial. Ann Intern Med. 2021;174(4):484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: development and evaluation of a new indicator. Pediatrics. 2001;108(2):E31. [DOI] [PubMed] [Google Scholar]
- 64. Ensminger ME, Forrest CB, Riley AW, et al. The validity of measures of socioeconomic status of adolescents. J Adolescent Res. 2000;15(3):392–419. [Google Scholar]
- 65. Nalty CC, Sharkey JR, Dean WR. Children’s reporting of food insecurity in predominately food insecure households in Texas border colonias. Nutr J. 2013;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Crockett LJ, Carlo G, Temmen C. Ethnic and racial minority youth in the rural United States: an overview. In Crockett LJ, Carlo G, eds. Rural Ethnic Minority Youth and Families in the United States: Theory, Research, and Applications. Switzerland: Springer International Publishing; 2016:1–12. [Google Scholar]
- 67. Lichter DT, Johnson KM. The changing spatial concentration of America’s rural poor population*. Rural Sociol. 2007;72(3):331–358. [Google Scholar]
- 68. Bogart LM, Wagner GJ, Green HD, et al. Medical mistrust among social network members may contribute to antiretroviral treatment nonadherence in African Americans living with HIV. Soc Sci Med. 2016;164:133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Katz RV, Kegeles SS, Kressin NR, et al. The Tuskegee Legacy Project: willingness of minorities to participate in biomedical research. J Health Care Poor Underserved. 2006;17(4):698–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Hamel L, Kirzinger A, Lopes L, Kearney A, Sparks G, Bodie M. KFF COVID-19 Vaccine Monitor: January 2021. Available at https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-january-2021/. Accessibility verified April 9, 2021.
- 71. LeBaron CW, Starnes D, Dini EF, Chambliss JW, Chaney M. The impact of interventions by a community-based organization on inner-city vaccination coverage: Fulton County, Georgia, 1992-1993. Arch Pediatr Adolesc Med. 1998;152(4):327–332. [DOI] [PubMed] [Google Scholar]
- 72. Daniels NA, Juarbe T, Moreno-John G, Pérez-Stable EJ. Effectiveness of adult vaccination programs in faith-based organizations. Ethn Dis. 2007;17(1 Suppl 1):S15–S22. [PubMed] [Google Scholar]
- 73. Quinn SC, Andrasik MP. Addressing vaccine hesitancy in BIPOC Communities — Toward trustworthiness, partnership, and reciprocity. N Engl J Med. [DOI] [PubMed] [Google Scholar]
- 74. Berkley-Patton J, Thompson CB, Martinez DA, et al. Examining church capacity to develop and disseminate a religiously appropriate HIV tool kit with African American churches. J Urban Health. 2013;90(3):482–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Berkley-Patton J, Bowe-Thompson C, Bradley-Ewing A, et al. Taking It to the Pews: a CBPR-guided HIV awareness and screening project with black churches. AIDS Educ Prev. 2010;22(3):218–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ndugga N, Pham O, Hill L, Artiga S, Alam R, Parker N. Latest Data on COVID-19 Vaccinations Race/Ethnicity. KFF. Available at https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/. Accessibility verified April 9, 2021.
- 77. Durlak JA, Weissberg RP. The impact of after-school programs that promote personal and social skills. Chicago, IL: Collaborat Acad Soc Emot Learning (Nj1). 2007. Available at https://casel.org/wp-content/uploads/2016/06/the-impact-of-after-school-programs-that-promote-personal-and-social-skills.pdf. [Google Scholar]
- 78. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting black lives—the role of health professionals. N Engl J Med. 2016;375(22):2113–2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Pirtle WNL. Racial capitalism: a fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Educat Behav. 2020;47(4):504–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Gravlee CC. Systemic racism, chronic health inequities, and COVID‐19: A syndemic in the making? Am J Human Biol. 2020;32(5):e23482. [DOI] [PMC free article] [PubMed] [Google Scholar]