Abstract
In obese patients, enhanced serum levels of free fatty acids (FFA), such as palmitate (PA) or oleate (OA), are associated with an increase in systemic inflammatory markers. Bacterial infection during periodontal disease also promotes local and systemic low-grade inflammation. How both conditions concomitantly impact tooth movement is largely unknown. Thus, the aim of this study was to address the changes in cytokine expression and the secretion of human periodontal ligament fibroblasts (HPdLF) due to hyperlipidemic conditions, when additionally stressed by bacterial and mechanical stimuli. To investigate the impact of obesity-related hyperlipidemic FFA levels on HPdLF, cells were treated with 200 µM PA or OA prior to the application of 2 g/cm2 compressive force. To further determine the additive impact of bacterial infection, HPdLF were stimulated with lipopolysaccharides (LPS) obtained from Porphyromonas gingivalis. In mechanically compressed HPdLF, PA enhanced COX2 expression and PGE2 secretion. When mechanically stressed HPdLF were additionally stimulated with LPS, the PGE2 and IL6 secretion, as well as monocyte adhesion, were further increased in PA-treated cultures. Our data emphasize that a hyperlipidemic condition enhances the susceptibility of HPdLF to an excessive inflammatory response to compressive forces, when cells are concomitantly exposed to bacterial components.
Keywords: periodontitis, obesity, inflammation, orthodontic tooth movement, periodontal ligament fibroblasts
1. Introduction
Obesity is a common, non-communicable disease, and it is well established that adipose tissue is highly metabolically active [1]. Adipocytes and macrophages, the main cell types of adipose tissue, modulate the secretion of several bioactive molecules [2]. This includes pro-inflammatory cytokines and other inflammatory markers, as well as hormone-like signaling mediators, that have therefore been termed adipokines [2]. They have several functions in different organs and contribute to the regulation of lipid metabolism and inflammatory processes [3]. In obese patients, increased release of pro-inflammatory cytokines such as tumor necrosis factor alpha (TNFα), interleukin 6 (IL6), and IL8, as well as IL1β contributes to the dysregulation of biologically relevant processes and promotes low-grade systemic inflammation [4,5,6].
Studies on the underlying mechanisms of obesity-associated inflammation have focused on alterations in lipid metabolism and the resulting elevated serum levels of free fatty acids (FFA), such as saturated palmitic acid (PA) and monounsaturated oleic acid (OA) [4,7,8,9,10,11,12,13,14]. Although they are relevant for normal cell functions [15], hyperlipidemic conditions of both fatty acids impact inflammatory processes in several cell types [16,17,18,19,20,21,22,23].
Saturated fatty acids (SFA) such as PA have been shown to activate pro-inflammatory genes (TNFα, IL6, IL8, IL1α, IL1β) via multiple pathways [16,17,18,19,20,21,22,24,25]. In a hypothalamic cell line, palmitic acid has been described as an agonist for toll-like receptors (TLR), activating several protein kinases, causing ER stress and increased ROS production, and thus promoting cytokine production and secretion [26]. In addition, culturing cells with palmitic acid was reported to result in the accumulation of palmitoyl-CoA, which serves as a substrate for ceramide production [27]. A high ceramide level is a potent trigger of cell cycle arrest and apoptosis [28], which supports our recent findings of higher cellular senescence and cell death in HPdLF associated with PA [29].
Monosaturated fatty acids (MUFA), such as OA, have mostly been reported to reduce levels of pro-inflammatory cytokines, such as TNFα and IL6, in part by balancing SFA-induced inflammation [8,19,23,30]. However, in dermal fibroblasts, OA appears to be pro-inflammatory, causing increased cyclooxygenase 2 (COX2) expression, higher ROS levels, and oxidative damage [31]. In addition, oleic acid is suspected to predispose obesity and obesity-related disorders by promoting adipogenesis of fibroblast-like 3T3-L1 cells [32]. In vivo, the effects of hyperlipidemia are based on an excess of specific fatty acids and their relation to each other [4,7,8,9,10,11,12,13,14], which complicates in vitro studies.
Similarly to obesity, periodontal inflammation is a global health problem, and patients suffering from severe periodontitis also show low-grade systemic inflammation, with increased levels of pro-inflammatory cytokines [33]. Periodontitis is characterized by the destruction of tooth-supporting soft tissue and alveolar bone through a bacterial-induced inflammatory host response [34]. As the second largest microbial ecosystem, the microbiome of the oral cavity is composed of a variety of different microorganisms including bacteria, fungi, viruses, archaea, and protozoa [35]. Porphyromonas gingivalis (P. gingivalis) has been classified as one of the major gram-negative oral anaerobes affecting periodontal health [36]. A variety of virulence factors, such as lipopolysaccharides (LPS), gingipains, and fimbriae are responsible for the pathogenic mechanism of P. gingivalis [37]. To enable in vitro studies, P. gingivalis or its LPS is often used to mimic periodontitis-causing stimuli. It should be noted, however, that none of these factors or P. gingivalis alone can trigger periodontitis, but that an interplay of a variety of microbial imbalances and a corresponding host susceptibility is necessary for this to occur. In obese mice, a delay in response to infection with P. gingivalis was reported [38]. In addition, P. gingivalis LPS was shown to promote the pro-inflammatory profile of adipokines, possibly contributing to obesity-related inflammation [39,40]. Moreover, changes in gut microbiome due to P. gingivalis swallowing were reported to induce systemic inflammation and metabolic alterations in animal studies [41,42]. However, whether both diseases can subsequently impact orthodontic tooth movement (OTM) is currently poorly understood.
For successful orthodontic treatment, a controlled and non-excessive inflammatory response of the periodontal tissue is necessary in order to foster relevant processes related to remodeling of the alveolar bone [43]. The RANKL/OPG system is involved in alveolar bone remodeling by mechanical forces, with an increase in inflammatory cytokines promoting osteoclast-activating expression and secretion of receptor activator of nuclear factor kappa-β ligand (RANKL), whereas the counteracting osteoprotegerin (OPG) is significantly reduced [44]. The complex inflammatory signaling cascades due to orthodontic treatments are mainly regulated by periodontal ligament fibroblasts (PdLF), which are the main cell type in the periodontium and located between the teeth and alveolar bone [45]. Dysregulation can result in tooth root degradation or even tooth loss, which are major risks of OTM [46,47]. When teeth are mechanically stressed, the triggered aseptic transient inflammation is modulated area-specifically by PdLF. In particular, the expression and secretion of pro-inflammatory cytokines, such as IL6, IL8, prostaglandin E2 (PGE2), and TNFα, are characteristics of the compression side of the PdL, while the release of anti-inflammatory cytokines, such as IL10, is more prominent on the tensile side [43,48]. This area-specific inflammation of the PdL is important for tissue and bone remodeling, by promoting the degradation and reorganization of the extracellular matrix and vascular supply, as well as the activation and differentiation of osteoblasts and osteoclasts [43,49]. Besides that, PdLF also recognize pathogens and their virulence factors through pattern recognition receptors [45], which also induce an inflammatory cellular response.
To date, only a few studies have investigated whether obesity affects tooth movement [50,51,52,53], and none of the studies additionally addressed effects due to periodontitis. Under obese conditions, faster tooth movement was reported in children and adolescents at early stages of tooth movement one week after force application [51]. Although obese patients were mostly reported to have higher levels of osteoclastic activity, due to pro-inflammatory promotion of RANKL levels [54], OTM resulted in prolonged overall treatment duration [50,53] and reduced the numbers of osteoclasts in force-treated obese mice [52]. However, Bremen et al. mainly based the result of their studies on the poorer cooperation of obese patients during orthodontic therapy. The extent to which the force-induced inflammatory response of PdL is impaired under obese conditions has not been investigated so far.
When tooth movement was simulated in rats suffering from periodontitis, an up-regulated expression of several cytokines in the PdL, as well as an increased number of activated osteoclasts and an enhanced extent of dorsal root resorption, was shown [55]. In contrast, in a mouse-model, induction of periodontal inflammation reduced tooth movement by inhibiting osteoclastogenesis [56], whereas oral administration of P. gingivalis in obese mice led to increased alveolar bone loss compared to lean controls [38]. However, to our knowledge, it has not yet been investigated whether periodontitis has an influence on obesity-associated changes in orthodontic force-induced modulation of inflammatory tissue response.
In this context, our aim was: (1) to investigate, whether a fatty acid-simulated hyperlipidemic condition impacts the function of HPdLF in modulating the inflammatory response to a compressive stimulus; and (2) to address changes due to the administration of P. gingivalis LPS. In view of an ever-increasing proportion of obese patients suffering from periodontitis, who nevertheless desire orthodontic treatment, this study should provide initial information on the biological background.
2. Results
2.1. Palmitic Acid Induces an Increased Inflammatory State in HPdLF
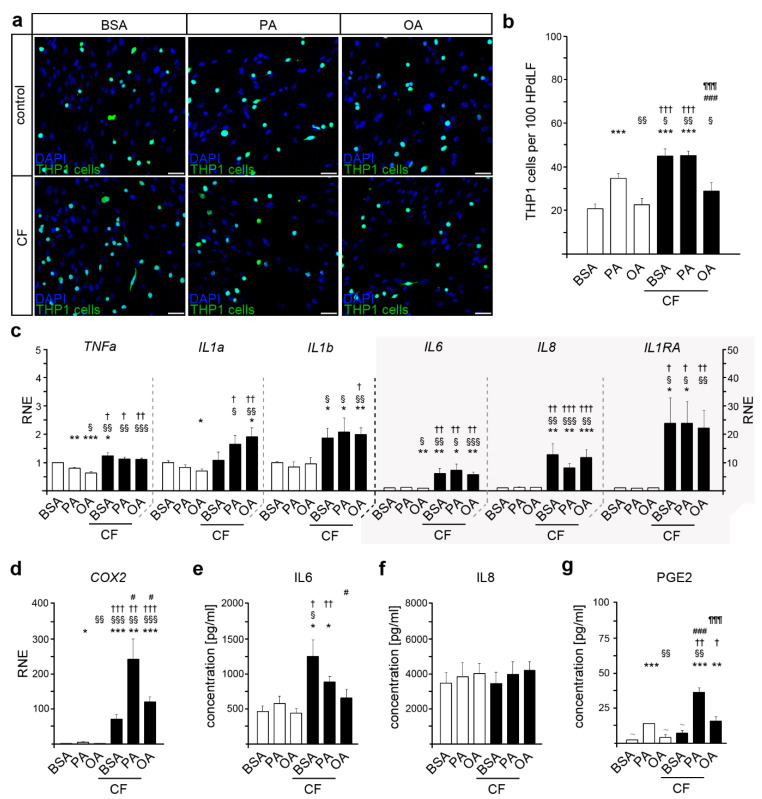
To investigate the impact of hyperlipidemic palmitic and oleic acid levels on the regulatory function of HPdLF, we performed a THP1 cell adhesion assay (Figure 1a,b). Non-adherent THP1 monocyte-like cells are attracted by the cytokines secreted by stimulated HPdLF and can differentiate into functional adherent macrophages [57]. We analyzed the number of adherent Alexa488-labeled THP1 cells on HPdLF cultured in palmitic or oleic acid. Cells incubated with BSA only were used as a control, since BSA functions as a carrier for fatty acids. We detected an increased number of THP1 cells on PA-incubated HPdLF (Figure 1a,b). Cultivation with OA resulted in similar amounts of attracted THP1 monocytic cells compared to the BSA controls. This suggests that palmitic acid in particular promotes an inflammatory response in HPdLF.
Figure 1.
Palmitic and oleic acid influence the inflammatory response of human periodontal ligament fibroblasts (HPdLF) to compressive force of six hours (CF). (a,b) Analysis of the number of adherent THP1 monocytic cells (green) on HPdLF (blue), stimulated either with palmitic or oleic acid in comparison to BSA control (a). THP1 cells were stained with CellTracker™ and the nuclei of all cells were stained with DAPI. The relative number of THP1 cells is displayed per 100 HPdLF (b). (c,d) Quantitative expression analysis of genes coding for inflammatory markers TNFα, IL1α, IL1β, IL6, IL8, IL1RA (c), and COX2 (d) in fatty acid-cultured HPdLF stimulated with 6 h of compressive force in comparison to BSA controls. Results are normalized to unstimulated BSA controls. (e–g) Analysis of secreted cytokines IL6 (e), IL8 (f), and PGE2 (g) in HPdLF cultures stimulated with palmitic or oleic acid and six hours of compressive force compared to BSA controls. * p < 0.05; ** p < 0.01; *** p < 0.001 in relation to BSA, § p < 0.05; §§ p < 0.01; §§§ p < 0.001 in relation to PA, † p < 0.05; †† p < 0.01; ††† p < 0.001 in relation to OA, # p < 0.05; ### p < 0.001 in relation to BSA+CF, ¶¶¶ p < 0.001 in relation to PA + CF; one-way ANOVA and post hoc test (Tukey). Scale bars: 50 μm in (a). BSA, bovine serum albumin; CF, compressive force; OA, oleic acid; PA, palmitic acid; RNE, relative normalized expression; ~, below detection limit.
2.2. Oleic Acid Impacts THP1 Adhesion due to Mechanical Compression in HPdLF
The compressive forces associated with orthodontic procedures promote inflammatory processes that are modulated by periodontal ligament cells [43,45]. Therefore, we investigated whether culturing with fatty acids affects the response of HPdLF to six hours of mechanical compression, at which time the expression and secretion of several cytokines are already increased [58]. While compression induced increased THP1 cell adhesion in the BSA controls and PA-treated HPdLF (Figure 1a,b), OA supplementation hindered the force-induced increase in THP1 attraction. Thus, our data suggest that oleic acid limits the inflammatory response to a compressive stimuli of six hours.
2.3. COX2 Expression and PGE2 Secretion Are Altered in Mechanically Stimulated HPdLF in Relation to Fatty Acid Stimulation
To further analyze the inflammatory response of HPdLF cultured in fatty acids, we performed quantitative PCR of genes coding for the cytokines and inflammatory markers, TNFα, IL1α, IL1β, IL1RA, IL6, IL8, and COX2 (Figure 1c,d). We detected no changes in the baseline levels of IL1β, IL1RA, and IL8, whereas TNFα was reduced under both fatty acid conditions (Figure 1c). Moreover, OA cultures showed significantly lower levels of IL1α and IL6 (Figure 1c). In PA-treated HPdLF, we detected increased expression of COX2 compared to BSA controls (Figure 1d).
As a result of the six-hour compressive stimuli, the expression of most genes was increased regardless of the culture condition (Figure 1c,d). However, the force-induced increase in COX2 expression was significantly higher in PA and OA cultures compared to BSA controls (Figure 1d). This increase was still significantly lower in OA-treated HPdLF than in the respective PA cultures.
Analysis of cytokine secretion in the supernatant revealed no significant changes of basic IL6 levels with fatty acid treatment. However, mechanical stimulation promoted IL6 secretion in the BSA controls, as well as in PA cultures, but not in OA-treated HPdLF (Figure 1e). In contrast, IL8 secretion was not altered, neither by fatty acid treatment nor mechanical compression (Figure 1f).
In contrast to the BSA controls, whose PGE2 levels were below the detection limit, we detected PGE2 secretion by HPdLF treated with PA (Figure 1g). In addition, mechanical compression increased the PGE2 levels in PA cultures and raised PGE2 levels slightly above the detection limit in OA cultures.
Since IL6, rather than PGE2, is highly important for monocytes for differentiating into macrophages [59,60], our analysis of inflammatory markers supported the previous results of the THP1 assay.
2.4. Stimulation with Lipopolysaccharides from P. gingivalis Resulted in an Excessive Inflammatory Response of HPdLF Exposed to Palmitic Acid
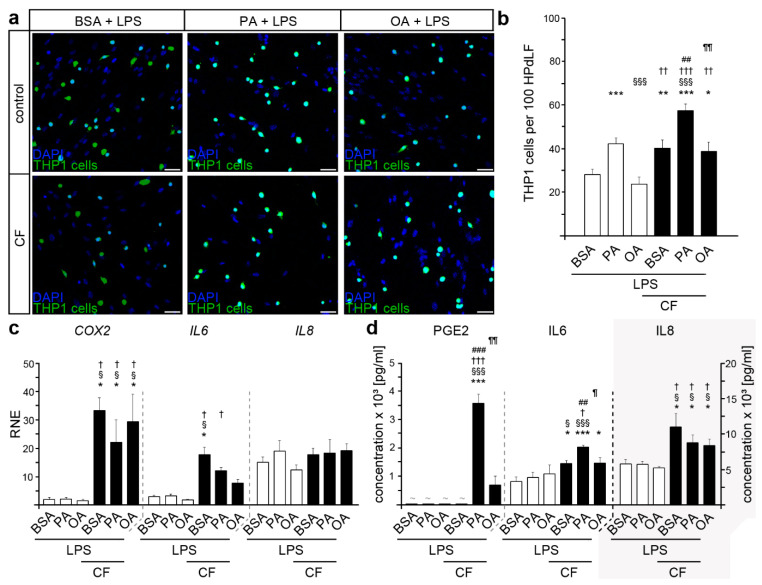
In order to simulate an infection with P. gingivalis, HPdLF were stimulated for 24 h with the appropriate lipopolysaccharides. In comparison to the unstimulated BSA controls, LPS stimulation resulted in an increased THP1 cell adhesion (compare with Figure 1b, Figure 2a,b; p-value = 0.03473, *). This was also detectable in the LPS-stimulated PA cultures (p-value = 0.04951, *). Additionally, higher numbers of adherent THP1 cells were evident in LPS-stimulated PA cultures compared to the respective BSA controls (Figure 2a,b).
Figure 2.
Stimulation with LPS obtained from P. gingivalis led to an excessive immune response in palmitate-cultured HPdLFs undergoing compressive stress. (a,b) Analysis of the number of adherent THP1 monocytic cells (green) on HPdLF (blue) stimulated either with palmitic or oleic acid in comparison to BSA controls and stimulated for six hours with compressive force (CF) (a). THP1 cells were stained with CellTracker™ and the nuclei of all cells were stained with DAPI. The relative number of THP1 cells is displayed per 100 HPdLF (b). (c) Quantitative expression analysis of genes coding for inflammatory markers IL6, IL8, and COX2 in fatty acid-cultured HPdLF stimulated with 6 h compressive force in comparison to BSA controls. Results are normalized to unstimulated BSA controls. (d) Analysis of secreted cytokines PGE2, IL6, and IL8 in HPdLF stimulated with palmitic or oleic acid and 6 h of compressive force compared to BSA controls. * p < 0.05; ** p < 0.01; *** p < 0.001 in relation to BSA, § p < 0.05; §§§ p < 0.001 in relation to PA, † p < 0.05; †† p < 0.01; ††† p < 0.001 in relation to OA, ## p < 0.01; ### p < 0.001 in relation to BSA+CF, ¶ p < 0.05; ¶¶ p < 0.01 in relation to PA + CF; one-way ANOVA and post-hoc test (Tukey). Scale bars: 50 μm in (a). BSA, bovine serum albumin; CF, compressive force; LPS, lipopolysaccharides of P. gingivalis; OA, oleic acid; PA, palmitic acid; RNE, relative normalized expression; ~, below detection limit.
After applying a compressive stimuli, a significant increase in THP1 cell adhesion was detected in all LPS-stimulated HPdLF (Figure 2a,b). However, the force-induced increase in adherent THP1 cells was significantly higher in LPS-primed PA cultures. In addition, the LPS stimulation of compressed PA-cultures led to significantly higher numbers of adherent TPH1 cells, when compared to those not stimulated with LPS (compare with Figure 1b; BSA CF: p-value = 0.28094; PA CF: p-value = 0.00483, **; OA CF: p-value = 0.11800).
A quantitative analysis of COX2 expression showed no fatty acid-related differences when stimulated with LPS (Figure 2c). Nevertheless, the transcriptional levels were significantly higher compared to those of non-LPS-stimulated HPdLF (compare with Figure 1d; BSA p-value = 0.03516, *; PA: p-value = 0.01895, *; OA: p-value = 0.01001, *). Similar changes in expression were also found for IL6 and IL8 (Figure 2c). Compared to their respective unstimulated conditions (compare with Figure 1c), the application of LPS led to a significantly up-regulated expression in BSA controls (IL6 p-value = 0.00310, **; IL8 p-value = 4.29214 × 10−8, ***), in PA cultures (IL6 p value = 0.00368; **; IL8 p value = 6.02460 × 10−5; ***), and in OA-cultured HPdLF (IL6 p-value = 0.02475, *; IL8 p-value = 2.21541 × 10−6; ***). In response to compressive forces, increased values were detected for COX2 and IL6 transcription, but not for IL8 (Figure 2c). Moreover, IL6 levels showed significant differences regarding fatty acid stimulation, with reduced expression in OA cultures.
Further analysis of the secreted proteins in the culture media revealed a profound increase of PGE2 in the mechanically stressed and LPS-stimulated PA cultures (Figure 2d) that was significantly higher compared to the non-LPS-stimulated PA cultures (compare with Figure 1g; p-value = 0.00042, ***). Under all other conditions, PGE2 levels were below the detection limit. In addition, we detected a force-induced enhancement of IL6 but not of IL8 secretion levels for LPS-stimulated BSA controls (Figure 2d). The increase in IL6 cytokine release was even higher when cells were additionally exposed to PA, which further supports the modulatory impact of PA on the inflammatory response of HPdLF to mechanical, as well as bacterial, stress. Moreover, we detected significantly higher levels of IL6 and IL8 secretion in LPS-stimulated PA and OA cultures compared to the HPdLF that were not challenged by P. gingivalis LPS (compare with Figure 1e,f; IL6 PA p-value = 3.18950 × 10−5, ***; OA p-value = 0.02287, *; IL8 PA p-value = 0.00142, **; OA p-value = 0.00103, **). For IL8, this was also detected for BSA controls (p-value = 2.06347 × 10−5, ***).
In summary, our data point to an increased inflammatory response in mechanical HPdLF treated with palmitic acid. Furthermore, our data strongly suggest that the inflammatory stress response is even more pronounced when the cells are additionally stimulated with periodontitis-causing bacterial compounds.
3. Discussion
In this study we investigated the possible impact of a fatty acid-stimulated hyperlipidemic condition, typically seen in obese patients, on the function of human periodontal ligament fibroblast, in terms of their inflammatory response to compressive forces when additionally challenged with P. gingivalis LPS. Exposition to palmitate resulted in enhance inflammatory state, even when not additionally stressed. Mechanical forces increased COX2/PGE2 levels in fatty-acid cultures and additional LPS administration further increased PGE2 and IL6 secretion in PA-primed HPdLF.
The causes and mechanisms of obesity-induced inflammatory processes are not fully understood. However, the important role of fatty acids in the activation and modulation of inflammatory signaling pathways is suggested. The applied concentration of both fatty acids, PA and OA, has previously been used in other in vitro studies, and the used BSA concentration relates to serum albumin and is characteristic for obesity and hypertriglyceridemia [9,10,11,12,13,14,29]. The investigated cytokines play important roles in the defense against pathogens in periodontal diseases, as well as in the regulation of orthodontic force-induced alveolar bone remodeling [43,61]. Dysregulation by hyperlipidemic conditions could affect inflammation, which is important for both processes, and a basic investigation of the underlying biological changes of inflammatory markers would be relevant for further studies in obese patients with periodontal inflammation.
We detected increased COX2 expression and PGE2 secretion in HPdLF that were stimulated with palmitic acid. This is in line with recent studies in which PA-related increased COX2 transcription levels were reported in several cells types [20,62,63]. Catalyzing a rate-limiting step in prostaglandin synthesis, COX2 overexpression could lead to increased production of PGE2, which was also shown to induce fibroblast apoptosis by multiple pathways [64]. Moreover, intracrine COX2/PGE2 signaling was also reported to contribute to the establishment and maintenance of cellular senescence [65]. Therefore, our recently reported higher numbers of apoptotic and senescent HPdLF cultured in palmitate may have been due to, at least partially, increases in COX2/PGE2 signaling [29]. In contrast to our results, de Souza et al. [20] also showed enhanced expression of IL6 in response to PA treatment in human endothelial cells. However, the cell cultures were simultaneously stimulated with TNFα, which could have influenced the expression pattern of several cytokines. In orbital fibroblasts, comparable concentrations of palmitate promoted the secretion of IL6 and monocyte chemotactic protein 1 (MCP1) [66]. It should be noted that the preparation of the corresponding palmitate concentration was done with ethanol, rather than heated water, and thus could potentially have impacted the cytokine levels. Higher concentrations of PA also resulted in increased levels of the pro-inflammatory cytokines IL6 and TNFα in cardiac fibroblasts [16]. However, these high concentrations were shown to be toxic in HPdLF (data not shown). In cultured HPdLF, reduced expression levels of TNFα, IL1α, and IL6 were detected due to oleate treatment. Comparable observations were also made in other cell types stimulated with OA alone [22,23], which underline the anti-inflammatory potential of oleate. However, in murine dermal fibroblasts, OA induced pro-inflammatory cellular responses via increased COX2 levels [31]. Therefore, it can be assumed that fatty acids evoke a specific cellular reaction depending on cell type and their ratio to other fatty acids, as well as additional intrinsic and extrinsic stimuli. However, for simulating an obesity-related pro-inflammatory state, hyperlipidemic culturing with PA seems to be favorable for HPdLF.
During OTM, the compressive force acts as a strong extrinsic stimulus to HPdLF. Here, we could show that hyperlipidemic fatty acid levels influence the force-induced increase in COX2 expression in mechanically stimulated HPdLF. Accordingly, the PGE2 secretion of compressed HPdLF was also increased in response to different fatty acids. In general, the PGE2 secretion of HPdLF is promoted by mechanical stimulation in vitro and in vivo and it is responsible, among other cytokines, for the initiation of osteoclastic activity [67,68]. Some studies reported a rather moderate increase in PGE2 after OA supplementation [69,70], which is also supported by our findings.
Too high levels of PGE2 could be problematic for tissue homeostasis and bone remodeling. In animal model systems, submucosal as well as intraligamentous PGE2 administration significantly accelerated tooth movement with increased root resorption [67,71,72]. Moreover, high PGE2 levels were also associated with enhanced transformation of monocytes into osteoclasts and the inhibition of PdL fibroblast proliferation [73]. Contrary to these results, other studies showed that elevated PGE2 levels inhibited osteoclast formation and function [74,75]. We recently hypothesized that mechanically compressed HPdLF that were exposed to palmitic acid would fail to sufficiently activate immature osteoclasts, due to enhanced cellular senescence and cell death [29]. Our data now suggest that a high level of PGE2 secretion by compressed PA-stimulated HPdLF could directly inhibit the differentiation of immature osteoclasts. This would support the results of Yan et al. [52], who demonstrated reduced numbers of osteoclasts in obese mice, correlating with attenuated experimental tooth movement. Further studies on patient PGE2 levels could prove whether this theory is relevant to the increased duration of orthodontic treatment in obese adolescents [50]. However, it should be taken into account that higher levels of several cytokines are also present in senescent cells, as well as in cell death [76,77]. Although cell survival is generally not affected by compressive stimulation with 2g/cm² [78], fatty acid primed HPdLF might be more sensitive to the applied forces.
In contrast to several studies that showed enhanced IL6 levels due to palmitic acid exposition [24,79,80], we could not detect increased levels of either IL6 expression or secretion in PA-treated HPdLF. In nondiabetic peripheral blood mononuclear cells, palmitic acid also failed to increase IL6 secretion [81]. However, a force-induced increase in IL6 secretion was observed in BSA controls and evident in PA-treated compressed HPdLF. Interestingly, compressed HPdLF exposed to OA did not show increased IL6 levels. Our data support the findings of Rodrigues et al. [82], who detected reduced IL6 concentrations in the skin wounds of rats fed with higher amounts of oleic acid. As an important osteotropic cytokine, force-released IL6 directly or indirectly interacts with bone-modulating cells, thereby promoting bone resorption on the compressive side of affected teeth [43]. As a result, reduced IL6 levels, as found in OA-treated HPdLF cultures, could lead to decreased bone resorption, which would hamper tooth movement and probably increase treatment duration. It should be taken into account that hyperlipidemia in obese patients is not represented only by the increase of a particular fatty acid, but is based on a composition of several SFA, MUFA, and polyunsaturated fatty acids (PUFA). In the context of our study, we can only speculate how obesity-related hyperlipidemia might affect osteoclastogenesis. However, in vitro preliminary studies can help in the targeted analysis of limited patient material.
Since a controlled inflammation contributes to the regulation of force-induced alveolar bone remodeling, several studies have focused on the impact of periodontal disease, an uncontrollable inflammatory stimulus when left untreated during OTM. P. gingivalis, a major periodontal pathogen, induces an inflammatory response in HPdLF via increased expression and secretion of IL6 and IL8, respectively [83,84]. We detected elevated levels of these cytokines in LPS-stimulated HPdLF, which, interestingly, were independent of the presence of fatty acids. For IL8, this appears to be consistent with the study of Fadel et al. [85], who detected no differences in IL8 levels between obese and normal weight patients suffering from periodontitis. In the case of IL6, however, this seems to be different from other studies reporting that P. gingivalis augmented palmitate-induced cytokine secretion in gingival fibroblasts and osteoclasts [86,87]. In these studies, different cell types were investigated and a lower palmitate concentration [86] or direct bacterial infection [87] was used for stimulation.
Based on our data, we speculate that palmitic acid in combination with P. gingivalis LPS stimulation makes HPdLF susceptible to an excessive immune response to compressive forces. This is based on the detection of excessive PGE2 secretion, as well as increased IL6 amounts and higher levels of adherent THP1 monocytic cells on palmitate-treated HPdLF that were LPS and force-stimulated. In this context, Sokolova et al. [16] reported that cardiac fibroblast exposed to palmitate and additionally challenged with LPS from Escherichia coli (E. coli) showed an increased expression and secretion of the pro-inflammatory cytokine IL1β, which was fatty acid dose- and time-dependent. In the same study, they revealed that stimulation with oleic acid and E. coli LPS did not induce comparable changes in IL1β levels.
The results of our study are limited by their experimental design. First, we examined only a certain amount of PA and OA as well as P. gingivalis LPS, and second, the compressive force was applied only for the specific duration of six hours. Thus, we cannot exclude the possibility that changes in the experimental setup could cause further changes in the expression and secretion of the cytokines studied, which are not obvious under our experimental design. However, this requires further investigation. Furthermore, it is important to note that periodontitis is not caused by overexposure to the LPS of one bacterium, but by a variety of virulence factors of different pathogens, as well as the specific host immune system. However, our studies provide some first ideas for the possible biological mechanisms of how obesity-related hyperlipidemia and periodontitis concomitantly affect orthodontic tooth movement, which can be further addressed in future studies.
4. Materials and Methods
4.1. Cell Culture
Commercially acquired human periodontal ligament fibroblast (HPdLF, Lonza, Basel, Switzerland) were grown in culture medium consisting of Dulbecco’s modified Eagle medium (DMEM; Thermo Fisher Scientific, Carlsbad, CA, USA) containing 4.5 g/L glucose, 10% heat-inactivated fetal bovine serum (Thermo Fisher Scientific, Carlsbad, CA, USA), 100 U/mL penicillin, 100 µg/mL streptomycin, and 50 µg/mL L-ascorbic acid at 37 °C, 5% CO2 and 95% humidity. Cells were passaged when reaching a confluency of 75% with 0.05% Trypsin/EDTA (Thermo Fisher Scientific, Carlsbad, CA, USA). For experiments, HPdLF of passage four to eight were used.
THP1 monocytic cells (DMSZ, Braunschweig, Germany) were cultured in RPMI 1640 medium (Thermo Fisher Scientific, Carlsbad, CA, USA) containing 10% FBS, 100 U/mL penicillin, and 100 µg/mL streptomycin at 37 °C, 5% CO2, and 95% humidity. The non-adherent cells were passaged regularly after seven days and seeded at a density of 1 × 106 cells in 20 mL medium in T175 culture flask (Thermo Fisher Scientific, Carlsbad, CA, USA). For this, cells were pelleted by centrifugation for 5 min at 1000× g and diluted in 1 mL RPMI culture medium prior to cell counting in a hemocytometer (Neubauer Chamber Improved, Avantor, Radnor, PA, USA).
4.2. Fatty Acid and P. gingivalis LPS Stimulation
For the analysis of RNA expression and cytokine secretion, 2.5 × 104 HPdLF were seeded into each well of a 6-well plate. For TPH1 cell adherence assay, 5 × 10³ cells were plated onto coverslips into each well of a 24-well-plate. Prior to fatty acid stimulation, cells were cultured in DMEM culture medium for 24 h. The stimulation with 200 µM palmitic or 200 µM oleic acid was performed as described previously [29]. Briefly, fatty acids were dissolved at 70 °C in sterile water containing 50 mM NaOH, complexed with 37 °C preheated bovine serum albumin (BSA, Seqens IVD, Limoges, France) and diluted in culture medium. As control, 0.66% BSA in DMEM culture medium was used. Fatty acid treatment was performed for six days resulting in a cell confluence of 65–75% before a compressive force was applied. For bacterial stimulation, 10 µg/mL lipopolysaccharides of P. gingivalis (InvivoGen, San Diego, CA, USA) were added to the culture medium 24 h before mechanical stimulation. To control for LPS application, HPdLF were stimulated with LPS but not mechanically loaded.
4.3. Mechanical Compression
Application of compressive force in 6-well plates was performed on the basis of the protocol of Kirschneck et al. [88] and as previously described [29]. Briefly, a compressive stimuli of 2 g/cm2 was applied with sterile glass plates for six hours at 37 °C, 5% CO2, and 95% humidity. Then, cells were either directly isolated with TRIzol Reagent (Thermo Fisher Scientific, Carlsbad, CA, USA) for expression analysis or medium was collected 24 h later for protein analysis.
The application of compressive forces in 24-well plates was performed by centrifugation for six hours at 30 °C. A force of 7.13 g/cm² was applied, as this was the minimal conditions of the centrifuge. Control cells were cultured at 30 °C for the time of the mechanical stimulation.
4.4. THP1 Cell Adherence assay
To visualize the inflammatory response of HPdLF to fatty acid stimulation, as well as to mechanical and bacterial stress, a THP1 cell adhesion assay was performed. For this, non-adherent THP1 monocytic cells were first stained with 15 µM Celltracker CMFDA (Thermo Fisher Scientific, Carlsbad, CA, USA) in sterile phosphate buffered saline (PBS, Thermo Fisher Scientific, Carlsbad, CA, USA) for 30 min at 37 °C, 5% CO2, and 95% humidity. Cells were then pelleted by centrifugation (5 min, 1000× g), resuspended in RPMI medium, and 50 × 10³ cells were added to each well of cultured HPdLF. Cell adhesion was carried out for 30 min before non-adhered THP1 cells were removed by two washing steps with prewarmed sterile PBS. After treatment, cells were fixated in 4% paraformaldehyde for 10 min, washed in PBS, and nuclei were stained for 5 min with DAPI (1:10,000 in PBS). Coverslips were embedded with Mowiol® 4–88 (Carl Roth, Karlsruhe, Germany) on glass object slides for microscopic imaging. The experiment was repeated three times, with two coverslips per condition.
4.5. RNA Extraction and Quantitative PCR
For expression analysis, the RNA of treated HPdLF was isolated with TRIzol Reagent (Thermo Fisher Scientific, Carlsbad, CA, USA)/1-bromo-3-chloropropane and purified with an RNA Clean and Concentrator-5 kit (Zymo Research, Freiburg, Germany) according to the manufacture’s guidelines. RNA quantity and quality was tested with Nanodrop 2000 (Avantor, Radnor, PA, USA). SuperScript IV Reverse Transcriptase (Thermo Fisher Scientific, Carlsbad, CA, USA) was used for cDNA synthesis using Oligo(dt)18 primers (Thermo Fisher Scientific, Carlsbad, CA, USA), according to the manufacture’s protocol. Quantitative PCR was performed with Luminaris Color HiGreen qPCR Master Mix (Thermo Fisher Scientific, Carlsbad, CA, USA), according to the manufacture’s protocol and analyzed with qTOWER3 (Analytik Jena, Jena, Germany). Primer sequences for all analyzed genes are displayed in Table 1. RPL22 and TBP were used as reference genes. Melting curve analysis and agarose gel electrophoresis was performed to assess primer quality and specificity. A dilution series was used to calculate primer efficiency. Data were analyzed with the efficiency corrected ΔΔCT method [89]. Each condition was analyzed at least in biological triplicate, with technical duplicates per sample.
Table 1.
qPCR primer sequences of human genes indicated in 5’-3’ direction. bp, base pairs. Length, amplicon length.
| Gene | Gene Symbol | NCBI Gene ID | Primer Sequence | Length |
|---|---|---|---|---|
| C-X-C motif chemokine ligand 8 | IL8 | 3576 | fw TTGGCAGCCTTCCTGATTTCTrew GGTCCACTCTCAATCACTCTCA | 149 bp |
| Interleukin 1 alpha | IL1α | 3552 | fw GACTGCCCAAGATGAAGACCArev CCAAGCACACCCAGTAGTCT | 185 bp |
| Interleukin 1 beta | IL1β | 3553 | fw CGAATCTCCGACCACCACTArev AGCCTCGTTATCCCATGTGT | 186 bp |
| Interleukin-1 receptor antagonist | IL1RN (IL1RA) | 3557 | fw GATGTGCCTGTCCTGTGTCArev ACTCAAAACTGGTGGTGGGG | 146 bp |
| Interleukin 6 | IL6 | 3569 | fw CATCCTCGACGGCATCTCAGrew TCACCAGGCAAGTCTCCTCA | 164 bp |
| Prostaglandin-endoperoxide synthase 2 | PTGS2 (COX2) | 5743 | fw GATGATTGCCCGACTCCCTTrew GGCCCTCGCTTATGATCTGT | 185 bp |
| Ribosomal protein L22 | RPL22 | 6146 | fw TGATTGCACCCACCCTGTAGrev GGTTCCCAGCTTTTCCGTTC | 98 bp |
| TATA-box binding protein | TBP | 6908 | fw CGGCTGTTTAACTTCGCTTCCrev TGGGTTATCTTCACACGCCAAG | 86 bp |
| Tumor necrosis factor | TNFα | 7124 | fw CACGCTCTTCTGCCTGCTGrev AGGCTTGTCACTCGGGGTT | 130 bp |
4.6. Enzyme-Linked Immunosorbent Assay (ELISA)
To analyze cytokine secretion, IL6 (R&D Systems, Minneapolis, MN, USA), IL8 (R&D Systems, Minneapolis, MN, USA), and prostaglandin E2 (PGE2; Thermo Fisher Scientific, Carlsbad, CA, USA) ELISA were performed on medium isolated from HPdLF, according to the manufacturer’s guidelines. Each individual condition was tested at least in biological triplicate, with technical duplicates per sample.
4.7. Microscopy, Image Analysis, and Statistics
The THP1 cell adhesion assay was imaged with an inverted confocal laser scanning microscope TCS SP5 (Leica), and Fiji software (https://imagej.net/Fiji, accessed on 1 April 2017) was used for cell number analysis. Graph Pad Prism (https://www.graphpad.com, accessed on 1 February 2021) was used for statistical analysis, in addition to Adobe Photoshop CS5 (https://adobe.com, accessed on 1 February 2013) for figure illustration. One-way ANOVA and post hoc test (Tukey) were used as statistical tests. Significance levels: p value < 0.05 *; p value < 0.01 **; p value < 0.001 ***.
5. Conclusions
Our study provides new information on how obesity-related hyperlipidemia affects the function of periodontal ligament fibroblasts in modulating the inflammatory response to compressive forces in vitro. Force-induced inflammation is enhanced by palmitate and further increased when cells were additionally challenged with LPS from P. gingivalis. Thus, this study provides the first information on changes in the regulation of cytokines that may be relevant during orthodontic tooth movement in an ever-increasing proportion of obese patients who also suffer from periodontitis.
Acknowledgments
The authors thank Katrin von Brandenstein for excellent technical support.
Author Contributions
Conceptualization, J.S. and M.W.; Investigation, J.S., S.A., J.A.B., I.K., J.M., C.-L.H. and A.D.; Project administration, J.S. and M.W.; Supervision, U.S.-S., C.J. and M.W.; Visualization, J.S.; Writing—original draft, J.S. and S.A.; Writing—revised draft, J.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Medical Faculty of Jena and by a grant from the Interdisciplinary Centre for Clinical Research within the faculty of Medicine at the RWTH Aachen University (IZKF OC1-2).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets of this study are available from the corresponding author on reasonable request. The data are not publicly available due to very large size of microscopy images.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Khan S., Barrington G., Bettiol S., Barnett T., Crocombe L. Is overweight/obesity a risk factor for periodontitis in young adults and adolescents? A systematic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2018;19:852–883. doi: 10.1111/obr.12668. [DOI] [PubMed] [Google Scholar]
- 2.Zorena K., Jachimowicz-Duda O., Slezak D., Robakowska M., Mrugacz M. Adipokines and obesity. Potential link to metabolic disorders and chronic complications. Int. J. Mol. Sci. 2020;21:3570. doi: 10.3390/ijms21103570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ouchi N., Parker J.L., Lugus J.J., Walsh K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boden G. Obesity and free fatty acids. Endocrinol. Metab. Clin. N. Am. 2008;37:635–646. doi: 10.1016/j.ecl.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suganami T., Tanimoto-Koyama K., Nishida J., Itoh M., Yuan X., Mizuarai S., Kotani H., Yamaoka S., Miyake K., Aoe S., et al. Role of the toll-like receptor 4/nf-kappab pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler. Thromb. Vasc. Biol. 2007;27:84–91. doi: 10.1161/01.ATV.0000251608.09329.9a. [DOI] [PubMed] [Google Scholar]
- 6.Cooke A.A., Connaughton R.M., Lyons C.L., McMorrow A.M., Roche H.M. Fatty acids and chronic low grade inflammation associated with obesity and the metabolic syndrome. Eur. J. Pharmacol. 2016;785:207–214. doi: 10.1016/j.ejphar.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 7.Ebbert J.O., Jensen M.D. Fat depots, free fatty acids, and dyslipidemia. Nutrients. 2013;5:498–508. doi: 10.3390/nu5020498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drosatos-Tampakaki Z., Drosatos K., Siegelin Y., Gong S., Khan S., Van Dyke T., Goldberg I.J., Schulze P.C., Schulze-Spate U. Palmitic acid and dgat1 deficiency enhance osteoclastogenesis, while oleic acid-induced triglyceride formation prevents it. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2014;29:1183–1195. doi: 10.1002/jbmr.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bierman E.L., Dole V.P., Roberts T.N. An abnormality of nonesterified fatty acid metabolism in diabetes mellitus. Diabetes. 1957;6:475–479. doi: 10.2337/diab.6.6.475. [DOI] [PubMed] [Google Scholar]
- 10.Taskinen M.R., Bogardus C., Kennedy A., Howard B.V. Multiple disturbances of free fatty acid metabolism in noninsulin-dependent diabetes. Effect of oral hypoglycemic therapy. J. Clin. Investig. 1985;76:637–644. doi: 10.1172/JCI112016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prisby R.D., Swift J.M., Bloomfield S.A., Hogan H.A., Delp M.D. Altered bone mass, geometry and mechanical properties during the development and progression of type 2 diabetes in the zucker diabetic fatty rat. J. Endocrinol. 2008;199:379–388. doi: 10.1677/JOE-08-0046. [DOI] [PubMed] [Google Scholar]
- 12.Soares E.A., Nakagaki W.R., Garcia J.A., Camilli J.A. Effect of hyperlipidemia on femoral biomechanics and morphology in low-density lipoprotein receptor gene knockout mice. J. Bone Miner. Metab. 2012;30:419–425. doi: 10.1007/s00774-011-0345-x. [DOI] [PubMed] [Google Scholar]
- 13.Cistola D.P., Small D.M. Fatty acid distribution in systems modeling the normal and diabetic human circulation. A 13c nuclear magnetic resonance study. J. Clin. Investig. 1991;87:1431–1441. doi: 10.1172/JCI115149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kissebah A.H., Alfarsi S., Adams P.W., Wynn V. Role of insulin resistance in adipose tissue and liver in the pathogenesis of endogenous hypertriglyceridaemia in man. Diabetologia. 1976;12:563–571. doi: 10.1007/BF01220632. [DOI] [PubMed] [Google Scholar]
- 15.Ferreri C., Masi A., Sansone A., Giacometti G., Larocca A.V., Menounou G., Scanferlato R., Tortorella S., Rota D., Conti M., et al. Fatty acids in membranes as homeostatic, metabolic and nutritional biomarkers: Recent advancements in analytics and diagnostics. Diagnostics. 2016;7:1. doi: 10.3390/diagnostics7010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sokolova M., Vinge L.E., Alfsnes K., Olsen M.B., Eide L., Kaasboll O.J., Attramadal H., Torp M.K., Fosshaug L.E., Rashidi A., et al. Palmitate promotes inflammatory responses and cellular senescence in cardiac fibroblasts. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2017;1862:234–245. doi: 10.1016/j.bbalip.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Pillon N.J., Azizi P.M., Li Y.E., Liu J., Wang C., Chan K.L., Hopperton K.E., Bazinet R.P., Heit B., Bilan P.J., et al. Palmitate-induced inflammatory pathways in human adipose microvascular endothelial cells promote monocyte adhesion and impair insulin transcytosis. Am. J. Physiol. Endocrinol. Metab. 2015;309:E35–E44. doi: 10.1152/ajpendo.00611.2014. [DOI] [PubMed] [Google Scholar]
- 18.Nemecz M., Constantin A., Dumitrescu M., Alexandru N., Filippi A., Tanko G., Georgescu A. The distinct effects of palmitic and oleic acid on pancreatic beta cell function: The elucidation of associated mechanisms and effector molecules. Front. Pharmacol. 2018;9:1554. doi: 10.3389/fphar.2018.01554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gillet C., Spruyt D., Rigutto S., Dalla Valle A., Berlier J., Louis C., Debier C., Gaspard N., Malaisse W.J., Gangji V., et al. Oleate abrogates palmitate-induced lipotoxicity and proinflammatory response in human bone marrow-derived mesenchymal stem cells and osteoblastic cells. Endocrinology. 2015;156:4081–4093. doi: 10.1210/en.2015-1303. [DOI] [PubMed] [Google Scholar]
- 20.de Souza C.O., Valenzuela C.A., Baker E.J., Miles E.A., Rosa Neto J.C., Calder P.C. Palmitoleic acid has stronger anti-inflammatory potential in human endothelial cells compared to oleic and palmitic acids. Mol. Nutr. Food Res. 2018;62:e1800322. doi: 10.1002/mnfr.201800322. [DOI] [PubMed] [Google Scholar]
- 21.Carrillo C., Cavia Mdel M., Alonso-Torre S. Role of oleic acid in immune system; mechanism of action; a review. Nutr. Hosp. 2012;27:978–990. doi: 10.3305/nh.2012.27.4.5783. [DOI] [PubMed] [Google Scholar]
- 22.de Lima-Salgado T.M., Alba-Loureiro T.C., do Nascimento C.S., Nunes M.T., Curi R. Molecular mechanisms by which saturated fatty acids modulate tnf-alpha expression in mouse macrophage lineage. Cell Biochem. Biophys. 2011;59:89–97. doi: 10.1007/s12013-010-9117-9. [DOI] [PubMed] [Google Scholar]
- 23.Al-Shudiefat A.A., Sharma A.K., Bagchi A.K., Dhingra S., Singal P.K. Oleic acid mitigates tnf-alpha-induced oxidative stress in rat cardiomyocytes. Mol. Cell. Biochem. 2013;372:75–82. doi: 10.1007/s11010-012-1447-z. [DOI] [PubMed] [Google Scholar]
- 24.Korbecki J., Bajdak-Rusinek K. The effect of palmitic acid on inflammatory response in macrophages: An overview of molecular mechanisms. Inflamm. Res. 2019;68:915–932. doi: 10.1007/s00011-019-01273-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou H., Urso C.J., Jadeja V. Saturated fatty acids in obesity-associated inflammation. J. Inflamm. Res. 2020;13:1–14. doi: 10.2147/JIR.S229691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sergi D., Morris A.C., Kahn D.E., McLean F.H., Hay E.A., Kubitz P., MacKenzie A., Martinoli M.G., Drew J.E., Williams L.M. Palmitic acid triggers inflammatory responses in n42 cultured hypothalamic cells partially via ceramide synthesis but not via tlr4. Nutr. Neurosci. 2020;23:321–334. doi: 10.1080/1028415X.2018.1501533. [DOI] [PubMed] [Google Scholar]
- 27.Novgorodov S.A., Wu B.X., Gudz T.I., Bielawski J., Ovchinnikova T.V., Hannun Y.A., Obeid L.M. Novel pathway of ceramide production in mitochondria: Thioesterase and neutral ceramidase produce ceramide from sphingosine and acyl-coa. J. Biol. Chem. 2011;286:25352–25362. doi: 10.1074/jbc.M110.214866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hannun Y.A. Functions of ceramide in coordinating cellular responses to stress. Science. 1996;274:1855–1859. doi: 10.1126/science.274.5294.1855. [DOI] [PubMed] [Google Scholar]
- 29.Symmank J., Chorus M., Appel S., Marciniak J., Knaup I., Bastian A., Hennig C.L., Doding A., Schulze-Spate U., Jacobs C., et al. Distinguish fatty acids impact survival, differentiation and cellular function of periodontal ligament fibroblasts. Sci. Rep. 2020;10:15706. doi: 10.1038/s41598-020-72736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ravaut G., Legiot A., Bergeron K.F., Mounier C. Monounsaturated fatty acids in obesity-related inflammation. Int. J. Mol. Sci. 2020;22:330. doi: 10.3390/ijms22010330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Romana-Souza B., Saguie B.O., Pereira de Almeida Nogueira N., Paes M., Dos Santos Valenca S., Atella G.C., Monte-Alto-Costa A. Oleic acid and hydroxytyrosol present in olive oil promote ros and inflammatory response in normal cultures of murine dermal fibroblasts through the nf-kappab and nrf2 pathways. Food Res. Int. 2020;131:108984. doi: 10.1016/j.foodres.2020.108984. [DOI] [PubMed] [Google Scholar]
- 32.Malodobra-Mazur M., Cierzniak A., Dobosz T. Oleic acid influences the adipogenesis of 3t3-l1 cells via DNA methylation and may predispose to obesity and obesity-related disorders. Lipids Health Dis. 2019;18:230. doi: 10.1186/s12944-019-1173-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cecoro G., Annunziata M., Iuorio M.T., Nastri L., Guida L. Periodontitis, low-grade inflammation and systemic health: A scoping review. Medicina. 2020;56:272. doi: 10.3390/medicina56060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kinane D.F., Stathopoulou P.G., Papapanou P.N. Periodontal diseases. Nat. Reviews. Dis. Primers. 2017;3:17038. doi: 10.1038/nrdp.2017.38. [DOI] [PubMed] [Google Scholar]
- 35.Deo P.N., Deshmukh R. Oral microbiome: Unveiling the fundamentals. J. Oral Maxillofac. Pathol. 2019;23:122–128. doi: 10.4103/jomfp.JOMFP_304_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nakayama M., Ohara N. Molecular mechanisms of porphyromonas gingivalis-host cell interaction on periodontal diseases. Jpn. Dent. Sci. Rev. 2017;53:134–140. doi: 10.1016/j.jdsr.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulhall H., Huck O., Amar S. Porphyromonas gingivalis, a long-range pathogen: Systemic impact and therapeutic implications. Microorganisms. 2020;8:869. doi: 10.3390/microorganisms8060869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amar S., Zhou Q., Shaik-Dasthagirisaheb Y., Leeman S. Diet-induced obesity in mice causes changes in immune responses and bone loss manifested by bacterial challenge. Proc. Natl. Acad. Sci. USA. 2007;104:20466–20471. doi: 10.1073/pnas.0710335105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cani P.D., Amar J., Iglesias M.A., Poggi M., Knauf C., Bastelica D., Neyrinck A.M., Fava F., Tuohy K.M., Chabo C., et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–1772. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 40.Le Sage F., Meilhac O., Gonthier M.P. Porphyromonas gingivalis lipopolysaccharide induces pro-inflammatory adipokine secretion and oxidative stress by regulating toll-like receptor-mediated signaling pathways and redox enzymes in adipocytes. Mol. Cell. Endocrinol. 2017;446:102–110. doi: 10.1016/j.mce.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 41.Kato T., Yamazaki K., Nakajima M., Date Y., Kikuchi J., Hase K., Ohno H., Yamazaki K. Oral administration of porphyromonas gingivalis alters the gut microbiome and serum metabolome. mSphere. 2018;3:e00460-18. doi: 10.1128/mSphere.00460-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arimatsu K., Yamada H., Miyazawa H., Minagawa T., Nakajima M., Ryder M.I., Gotoh K., Motooka D., Nakamura S., Iida T., et al. Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci. Rep. 2014;4:4828. doi: 10.1038/srep04828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamaguchi M., Fukasawa S. Is inflammation a friend or foe for orthodontic treatment?: Inflammation in orthodontically induced inflammatory root resorption and accelerating tooth movement. Int. J. Mol. Sci. 2021;22:2388. doi: 10.3390/ijms22052388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yamaguchi M. Rank/rankl/opg during orthodontic tooth movement. Orthod. Craniofacial Res. 2009;12:113–119. doi: 10.1111/j.1601-6343.2009.01444.x. [DOI] [PubMed] [Google Scholar]
- 45.Jonsson D., Nebel D., Bratthall G., Nilsson B.O. The human periodontal ligament cell: A fibroblast-like cell acting as an immune cell. J. Periodontal Res. 2011;46:153–157. doi: 10.1111/j.1600-0765.2010.01331.x. [DOI] [PubMed] [Google Scholar]
- 46.Weltman B., Vig K.W., Fields H.W., Shanker S., Kaizar E.E. Root resorption associated with orthodontic tooth movement: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. discussion 412A. [DOI] [PubMed] [Google Scholar]
- 47.Wishney M. Potential risks of orthodontic therapy: A critical review and conceptual framework. Aust. Dent. J. 2017;62(Suppl. 1):86–96. doi: 10.1111/adj.12486. [DOI] [PubMed] [Google Scholar]
- 48.Garlet T.P., Coelho U., Silva J.S., Garlet G.P. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur. J. Oral Sci. 2007;115:355–362. doi: 10.1111/j.1600-0722.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- 49.Li Y., Jacox L.A., Little S.H., Ko C.C. Orthodontic tooth movement: The biology and clinical implications. Kaohsiung J. Med Sci. 2018;34:207–214. doi: 10.1016/j.kjms.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 50.von Bremen J., Wagner J., Ruf S. Correlation between body mass index and orthodontic treatment outcome. Angle Orthod. 2013;83:371–375. doi: 10.2319/070612-555.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saloom H.F., Papageorgiou S.N., Carpenter G.H., Cobourne M.T. Impact of obesity on orthodontic tooth movement in adolescents: A prospective clinical cohort study. J. Dent. Res. 2017;96:547–554. doi: 10.1177/0022034516688448. [DOI] [PubMed] [Google Scholar]
- 52.Yan B., Liu D., Zhang C., Zhang T., Wang X., Yang R., Liu Y., He D., Zhou Y. Obesity attenuates force-induced tooth movement in mice with the elevation of leptin level: A preliminary translational study. Am. J. Transl. Res. 2018;10:4107–4118. [PMC free article] [PubMed] [Google Scholar]
- 53.von Bremen J., Lorenz N., Ruf S. Impact of body mass index on oral health during orthodontic treatment: An explorative pilot study. Eur. J. Orthod. 2016;38:386–392. doi: 10.1093/ejo/cjv074. [DOI] [PubMed] [Google Scholar]
- 54.Cao J.J. Effects of obesity on bone metabolism. J. Orthop. Surg. Res. 2011;6:30. doi: 10.1186/1749-799X-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kirschneck C., Fanghanel J., Wahlmann U., Wolf M., Roldan J.C., Proff P. Interactive effects of periodontitis and orthodontic tooth movement on dental root resorption, tooth movement velocity and alveolar bone loss in a rat model. Ann. Anat. Anat. Anz. Off. Organ Anat. Ges. 2017;210:32–43. doi: 10.1016/j.aanat.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 56.Okamoto A., Ohnishi T., Bandow K., Kakimoto K., Chiba N., Maeda A., Fukunaga T., Miyawaki S., Matsuguchi T. Reduction of orthodontic tooth movement by experimentally induced periodontal inflammation in mice. Eur. J. Oral Sci. 2009;117:238–247. doi: 10.1111/j.1600-0722.2009.00625.x. [DOI] [PubMed] [Google Scholar]
- 57.Bosshart H., Heinzelmann M. Thp-1 cells as a model for human monocytes. Ann. Transl. Med. 2016;4:438. doi: 10.21037/atm.2016.08.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li Y., Li M., Tan L., Huang S., Zhao L., Tang T., Liu J., Zhao Z. Analysis of time-course gene expression profiles of a periodontal ligament tissue model under compression. Arch. Oral Biol. 2013;58:511–522. doi: 10.1016/j.archoralbio.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 59.Chomarat P., Banchereau J., Davoust J., Palucka A.K. Il-6 switches the differentiation of monocytes from dendritic cells to macrophages. Nat. Immunol. 2000;1:510–514. doi: 10.1038/82763. [DOI] [PubMed] [Google Scholar]
- 60.Zaslona Z., Serezani C.H., Okunishi K., Aronoff D.M., Peters-Golden M. Prostaglandin e2 restrains macrophage maturation via e prostanoid receptor 2/protein kinase a signaling. Blood. 2012;119:2358–2367. doi: 10.1182/blood-2011-08-374207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramadan D.E., Hariyani N., Indrawati R., Ridwan R.D., Diyatri I. Cytokines and chemokines in periodontitis. Eur. J. Dent. 2020;14:483–495. doi: 10.1055/s-0040-1712718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu J., Hu S., Cui Y., Sun M.K., Xie F., Zhang Q., Jin J. Saturated fatty acids up-regulate cox-2 expression in prostate epithelial cells via toll-like receptor 4/nf-kappab signaling. Inflammation. 2014;37:467–477. doi: 10.1007/s10753-013-9760-6. [DOI] [PubMed] [Google Scholar]
- 63.Coll T., Palomer X., Blanco-Vaca F., Escola-Gil J.C., Sanchez R.M., Laguna J.C., Vazquez-Carrera M. Cyclooxygenase 2 inhibition exacerbates palmitate-induced inflammation and insulin resistance in skeletal muscle cells. Endocrinology. 2010;151:537–548. doi: 10.1210/en.2009-0874. [DOI] [PubMed] [Google Scholar]
- 64.Huang S.K., White E.S., Wettlaufer S.H., Grifka H., Hogaboam C.M., Thannickal V.J., Horowitz J.C., Peters-Golden M. Prostaglandin e(2) induces fibroblast apoptosis by modulating multiple survival pathways. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2009;23:4317–4326. doi: 10.1096/fj.08-128801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martien S., Pluquet O., Vercamer C., Malaquin N., Martin N., Gosselin K., Pourtier A., Abbadie C. Cellular senescence involves an intracrine prostaglandin e2 pathway in human fibroblasts. Biochim. Et Biophys. Acta. 2013;1831:1217–1227. doi: 10.1016/j.bbalip.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 66.Paik J.S., Cho W.K., Oh E.H., Lee S.B., Yang S.W. Palmitate induced secretion of il-6 and mcp-1 in orbital fibroblasts derived from patients with thyroid-associated ophthalmopathy. Mol. Vis. 2012;18:1467–1477. [PMC free article] [PubMed] [Google Scholar]
- 67.Seifi M., Eslami B., Saffar A.S. The effect of prostaglandin e2 and calcium gluconate on orthodontic tooth movement and root resorption in rats. Eur. J. Orthod. 2003;25:199–204. doi: 10.1093/ejo/25.2.199. [DOI] [PubMed] [Google Scholar]
- 68.Saito M., Saito S., Ngan P.W., Shanfeld J., Davidovitch Z. Interleukin 1 beta and prostaglandin e are involved in the response of periodontal cells to mechanical stress in vivo and in vitro. Am. J. Orthod. Dentofac. Orthop. 1991;99:226–240. doi: 10.1016/0889-5406(91)70005-H. [DOI] [PubMed] [Google Scholar]
- 69.Cheng Z., Abayasekara D.R., Elmes M., Kirkup S., Wathes D.C. Effect of oleic acid supplementation on prostaglandin production in maternal endometrial and fetal allantochorion cells isolated from late gestation ewes. Placenta. 2015;36:1011–1017. doi: 10.1016/j.placenta.2015.07.128. [DOI] [PubMed] [Google Scholar]
- 70.Hageman J.R., McCulloch K., Hunt C.E., Cobb M., Quade B., Crussi F., Pachman L. Oleic acid lung injury increases plasma prostaglandin levels. Prostaglandins Leukot. Essent. Fat. Acids. 1989;35:157–164. doi: 10.1016/0952-3278(89)90118-X. [DOI] [PubMed] [Google Scholar]
- 71.Yamasaki K., Shibata Y., Fukuhara T. The effect of prostaglandins on experimental tooth movement in monkeys (macaca fuscata) J. Dent. Res. 1982;61:1444–1446. doi: 10.1177/00220345820610121401. [DOI] [PubMed] [Google Scholar]
- 72.Caglaroglu M., Erdem A. Histopathologic investigation of the effects of prostaglandin e2 administered by different methods on tooth movement and bone metabolism. Korean J. Orthod. 2012;42:118–128. doi: 10.4041/kjod.2012.42.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chao C.F., Shih C., Wang T.M., Lo T.H. Effects of prostaglandin e2 on alveolar bone resorption during orthodontic tooth movement. Acta Anat. 1988;132:304–309. doi: 10.1159/000146592. [DOI] [PubMed] [Google Scholar]
- 74.Mano M., Arakawa T., Mano H., Nakagawa M., Kaneda T., Kaneko H., Yamada T., Miyata K., Kiyomura H., Kumegawa M., et al. Prostaglandin e2 directly inhibits bone-resorbing activity of isolated mature osteoclasts mainly through the ep4 receptor. Calcif. Tissue Int. 2000;67:85–92. doi: 10.1007/s00223001102. [DOI] [PubMed] [Google Scholar]
- 75.Take I., Kobayashi Y., Yamamoto Y., Tsuboi H., Ochi T., Uematsu S., Okafuji N., Kurihara S., Udagawa N., Takahashi N. Prostaglandin e2 strongly inhibits human osteoclast formation. Endocrinology. 2005;146:5204–5214. doi: 10.1210/en.2005-0451. [DOI] [PubMed] [Google Scholar]
- 76.Vernot J.P. Senescence-associated pro-inflammatory cytokines and tumor cell plasticity. Front. Mol. Biosci. 2020;7:63. doi: 10.3389/fmolb.2020.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Galluzzi L., Vitale I., Aaronson S.A., Abrams J.M., Adam D., Agostinis P., Alnemri E.S., Altucci L., Amelio I., Andrews D.W., et al. Molecular mechanisms of cell death: Recommendations of the nomenclature committee on cell death 2018. Cell Death Differ. 2018;25:486–541. doi: 10.1038/s41418-017-0012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Janjic Rankovic M., Docheva D., Wichelhaus A., Baumert U. Effect of static compressive force on in vitro cultured pdl fibroblasts: Monitoring of viability and gene expression over 6 days. Clin. Oral Investig. 2020;24:2497–2511. doi: 10.1007/s00784-019-03113-6. [DOI] [PubMed] [Google Scholar]
- 79.Zhou B.R., Zhang J.A., Zhang Q., Permatasari F., Xu Y., Wu D., Yin Z.Q., Luo D. Palmitic acid induces production of proinflammatory cytokines interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha via a nf-kappab-dependent mechanism in hacat keratinocytes. Mediat. Inflamm. 2013;2013:530429. doi: 10.1155/2013/530429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bunn R.C., Cockrell G.E., Ou Y., Thrailkill K.M., Lumpkin C.K., Jr., Fowlkes J.L. Palmitate and insulin synergistically induce il-6 expression in human monocytes. Cardiovasc. Diabetol. 2010;9:73. doi: 10.1186/1475-2840-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Volpe C.M., Abreu L.F., Gomes P.S., Gonzaga R.M., Veloso C.A., Nogueira-Machado J.A. The production of nitric oxide, il-6, and tnf-alpha in palmitate-stimulated pbmncs is enhanced through hyperglycemia in diabetes. Oxidative Med. Cell. Longev. 2014;2014:479587. doi: 10.1155/2014/479587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rodrigues H.G., Vinolo M.A., Magdalon J., Vitzel K., Nachbar R.T., Pessoa A.F., dos Santos M.F., Hatanaka E., Calder P.C., Curi R. Oral administration of oleic or linoleic acid accelerates the inflammatory phase of wound healing. J. Investig. Dermatol. 2012;132:208–215. doi: 10.1038/jid.2011.265. [DOI] [PubMed] [Google Scholar]
- 83.Yamamoto T., Kita M., Oseko F., Nakamura T., Imanishi J., Kanamura N. Cytokine production in human periodontal ligament cells stimulated with porphyromonas gingivalis. J. Periodontal Res. 2006;41:554–559. doi: 10.1111/j.1600-0765.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 84.Liu J., Tang X., Li C., Pan C., Li Q., Geng F., Pan Y. Porphyromonas gingivalis promotes the cell cycle and inflammatory cytokine production in periodontal ligament fibroblasts. Arch. Oral Biol. 2015;60:1153–1161. doi: 10.1016/j.archoralbio.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 85.Fadel H.T., Pliaki A., Gronowitz E., Marild S., Ramberg P., Dahlen G., Yucel-Lindberg T., Heijl L., Birkhed D. Clinical and biological indicators of dental caries and periodontal disease in adolescents with or without obesity. Clin. Oral Investig. 2014;18:359–368. doi: 10.1007/s00784-013-0972-9. [DOI] [PubMed] [Google Scholar]
- 86.Shikama Y., Kudo Y., Ishimaru N., Funaki M. Possible involvement of palmitate in pathogenesis of periodontitis. J. Cell. Physiol. 2015;230:2981–2989. doi: 10.1002/jcp.25029. [DOI] [PubMed] [Google Scholar]
- 87.Muluke M., Gold T., Kiefhaber K., Al-Sahli A., Celenti R., Jiang H., Cremers S., Van Dyke T., Schulze-Spate U. Diet-induced obesity and its differential impact on periodontal bone loss. J. Dent. Res. 2016;95:223–229. doi: 10.1177/0022034515609882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kirschneck C., Batschkus S., Proff P., Kostler J., Spanier G., Schroder A. Valid gene expression normalization by rt-qpcr in studies on hpdl fibroblasts with focus on orthodontic tooth movement and periodontitis. Sci. Rep. 2017;7:14751. doi: 10.1038/s41598-017-15281-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative pcr and the 2(-delta delta c(t)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets of this study are available from the corresponding author on reasonable request. The data are not publicly available due to very large size of microscopy images.