Abstract
Objectives
Whether the Affordable Care Act (ACA) insurance expansions improved access to care and health for adults aged 51–64 years has not been closely examined. This study examined longitudinal changes in access, utilization, and health for low-socioeconomic status adults aged 51–64 years before and after the ACA Medicaid expansion.
Methods
Longitudinal difference-in-differences (DID) study before (2010–2014) and after (2016) Medicaid expansion, including N = 2,088 noninstitutionalized low-education adults aged 51–64 years (n = 633 in Medicaid expansion states, n = 1,455 in nonexpansion states) from the nationally representative biennial Health and Retirement Study. Outcomes included coverage (any, Medicaid, and private), access (usual source of care, difficulty finding a physician, foregone care, cost-related medication nonadherence, and out-of-pocket costs), utilization (outpatient visit and hospitalization), and health status.
Results
Low-education adults aged 51–64 years had increased rates of Medicaid coverage (+10.6 percentage points [pp] in expansion states, +3.2 pp in nonexpansion states, DID +7.4 pp, p = .001) and increased likelihood of hospitalizations (+9.2 pp in expansion states, −1.1 pp in nonexpansion states, DID +10.4 pp, p = .003) in Medicaid expansion compared with nonexpansion states after 2014. Those in expansion states also had a smaller increase in limitations in paid work/housework over time, compared to those in nonexpansion states (+3.6 pp in expansion states, +11.0 pp in nonexpansion states, DID −7.5 pp, p = .006). There were no other significant differences in access, utilization, or health trends between expansion and nonexpansion states.
Discussion
After Medicaid expansion, low-education status adults aged 51–64 years were more likely to be hospitalized, suggesting poor baseline access to chronic disease management and pent-up demand for hospital services.
Keywords: Affordable Care Act, Hospitalization, Medicaid, Retirement
Low-socioeconomic status (SES) Americans approaching retirement face a crisis of poor health and increasing mortality (Case & Deaton, 2015, 2017). Between 2001 and 2014, while high-SES Americans gained 3 years of life expectancy, low-SES Americans did not experience these gains (Chetty et al., 2016). Between 2010 and 2017, when overall U.S. life expectancy declined, Americans with a college degree gained up to 1.7 years of life expectancy, whereas those with a high school degree or less experienced up to 1 year of decline in life expectancy (Sasson & Hayward, 2019). These declines in life expectancy occurred across racial groups (Woolf & Schoomaker, 2019). During the critical period before age 65, low-SES adults in their 50s and 60s have exhibited signs of accelerated aging, characterized by greater numbers of chronic conditions and declining health, compared with prior cohorts of Americans (Case & Deaton, 2015; Heiss et al., 2014; Soldo et al., 2006). However, until the passage of the Affordable Care Act (ACA), low-SES adults aged 51–64 years had few health insurance options before reaching Medicare eligibility at age 65.
The ACA’s coverage expansions for adults younger than age 65 went into effect in 2014. This benefit change represented a significant departure from past insurance expansions for children, disabled individuals, and older adults, as the target group gaining coverage involved working-age adults. Low-SES adults aged 51–64 years became eligible for new coverage options, including Medicaid expansion for those with incomes less than or equal to 138% of the federal poverty level (FPL) in participating states and subsidized health insurance exchange (a.k.a. “Marketplace”) plans for those with incomes 100%–400% FPL.
Previous research found evidence of improved health and lower mortality with insurance expansions for the general population (Miller & Wherry, 2017; Simon et al., 2017; Sommers et al., 2012, 2014, 2015; Van Der Wees et al., 2013; Wherry & Miller, 2016), and mixed health effects among adults older than age 65 gaining Medicare coverage (Card et al., 2007, 2008, 2009; McWilliams et al., 2007a; Polsky et al., 2009). But research has paid less attention to the unique circumstances of adults approaching retirement age, and much of this work predated recent increases in morbidity and mortality for this group (McWilliams et al., 2004). However, Miller et al. (2019) conducted a rigorous study, which found decreased all-cause mortality for low-SES adults aged 55–64 years after the ACA Medicaid expansion. The authors note that this reduction appears to be driven by disease-related deaths, including those considered potentially preventable with adequate health care. This suggests that the use of health care services, including diagnosis and treatment of health conditions (Fedewa et al., 2019; Hendryx & Luo, 2018), may prevent premature death among adults aged 51–64 years who gain Medicaid coverage.
Although factors such as access to care and health care utilization could drive the observed effect of Medicaid coverage on health and mortality, studies have not closely examined these factors among this vulnerable age group since the implementation of the ACA. The objective of this study was to examine the impact of the ACA Medicaid expansion on health care access, utilization, and health, in a nationally representative cohort of low-SES adults aged 51–64 years.
Method
Study Design
We conducted a longitudinal difference-in-differences (DID) study of U.S. adults aged 51–64 years in the Health and Retirement Study (HRS), assessing changes in coverage, access to care, health care utilization, and health status before (2010–2014) and after (2016) implementation of the ACA Medicaid expansion. The institutional review board deemed the study exempt, because it involved the use of publicly available deidentified data, except for state identifiers which were accessed through a secure data enclave.
Data Source
The HRS is a nationally representative panel study that surveys approximately 20,000 individuals older than age 50 about their health and economic well-being. The survey includes in-person or telephone surveys with participants biennially. Since 1998, response rates have ranged from 70% to 90% (Health and Retirement Study, 2017; Sonnega et al., 2014). All HRS participants provide informed consent.
Study Cohort
We identified a cohort of HRS respondents aged 51–59 years in 2010 (birth years 1951–1959) and thus younger than age 65 (56–64 years) in the final year of our analysis in 2016 (N = 14,173). We defined low SES as less than or equal to high school graduation (n = 6,500). We selected the sample by education rather than income to avoid the expected year-to-year variability in income. This approach enriched the sample for individuals with incomes that would be eligible for ACA coverage (Supplementary Table 1).
Outcome Measures
Measures included health insurance coverage, both whether the individual had any source of insurance coverage and also whether they specifically had Medicaid or private insurance (including employer-sponsored, group, and nongroup insurances). Access measures included usual source of care (“Is there a place that you usually go to when you are sick or need advice about your health?”), difficulty finding a physician (“In the last two years, did you have any trouble finding a general doctor or provider who would see you?”), foregone care (“In the last two years, was there any time when you needed medical care, but did not get it because you couldn’t afford it?”), cost-related medication nonadherence (“At any time in the last two years have you ended up taking less medication than was prescribed for you because of the cost?”), and out-of-pocket costs (“About how much did you pay out-of-pocket for [medical] expenses in the last two years?”). Out-of-pocket medical expenses included expenses for hospitalization, nursing home, outpatient, dental, medications, home health care, specialty health care facility, adult day care, social work, outpatient rehabilitation, physical therapy, and transportation, adjusted for 2014 dollars (RAND Corporation, 2019).
Utilization measures included outpatient visits (“How many times have you seen or talked to a medical doctor about your health, including emergency room, clinic visits, or house calls in the last two years?”) and hospitalizations (“In the last two years, have you been a patient in a hospital overnight?”). Because the interview question pertaining to outpatient visits in the HRS combines emergency room visits with other types of visits, we could not examine these two types of visits separately.
General health status was assessed with the item, “Would you say your health is excellent, very good, good, fair, or poor?,” and dichotomized as excellent/very good versus good/fair/poor. Self-reported depressive symptoms were measured by the eight-item version of the Center for Epidemiological Studies Depression scale (Radloff, 1977; Zivin et al., 2010). We also looked at self-reported health impairments that limited paid work or housework as an additional health outcome (“Do you have any impairment or health problem that limits the kind or amount of [paid work you can do/work you can do around the house]?”).
Note that three access measures (usual source of care, difficulty finding a physician, and foregone care) were introduced into the HRS in 2012, so do not have data in previous waves.
Exposure: State Medicaid Expansion
Our exposure of interest was state Medicaid expansion status as of 2016, as this was the first full HRS wave after Medicaid expansion implementation in 2014 (The Henry J. Kaiser Family Foundation, n.d.). In our primary analyses, we excluded 11 states that expanded Medicaid prior to the main ACA Medicaid expansion in 2014 (Supplementary Table 2 and Supplementary Figure 1), in a manner similar to prior studies of the ACA coverage expansion (Levy et al., 2018; Miller & Wherry, 2017; Wherry & Miller, 2016). These 11 states included some states that took the option to expand Medicaid early under the ACA (so-called “early expander” states; Supplementary Figure 1). Four of the six “early expander” states significantly expanded coverage eligibility before 2014 and, thus, were excluded from analysis, while two “early expander” states did not have significant changes in coverage eligibility until after 2014 so remained in the analysis. This left 40 states in the primary analysis (as we considered the District of Columbia a state).
Covariates
Covariates included age, gender, race/ethnicity, marital status, number of self-reported functional limitations (measured by limitations in the activities of daily living and instrumental activities in daily living), and the total number of self-reported chronic conditions (hypertension, diabetes, cancer, lung conditions, heart conditions, stroke, psychological conditions, and arthritis), employment, and wealth (a measure of assets, categorized as quartiles for the analysis). We used the early release version of the 2016 RAND-HRS file to estimate income and wealth (RAND Corporation, 2019).
Statistical Analysis
A total of N = 2,088 respondents were included in the final analysis after all the inclusion and exclusion criteria. We used a longitudinal DID approach, a quasi-experimental method for isolating the impact of an intervention from concurrent secular trends, comparing trends among respondents in Medicaid expansion states to those in nonexpansion states as follows:
where, = the jth outcome for the ith individual at time t, = a binary variable indicating whether the respondent resides in an expansion or nonexpansion state at time t, the HRS year of observation, = additional covariates including age, gender, race/ethnicity, marital status, number of functional limitations, number of chronic conditions, employment status, wealth (contains both time-invariant and time-variant variables), and = error term.
We considered 2010 the base year for all variables except for the three access variables that were introduced in 2012. For these access variables, 2012 was used as the base year. Study year 2016 was chosen as the postexpansion change year, as most of the interview questions in HRS are framed to capture respondents’ experiences in the approximately 2 years since the prior interview. As a result, interviews conducted during the 2014 wave also documented respondents’ experiences from before 2014. Using 2016 as the change year allowed us to more effectively separate between the pre- and postperiod in Medicaid expansion states.
We used generalized estimating equations (GEEs), applying a logit approach for dichotomous outcomes, with Huber–White robust standard errors clustered at the respondent level. All analyses are adjusted for the complex survey design with repeated measures to estimate standard errors that account for the design effects. The out-of-pocket costs variable was log-transformed to approximate a normal distribution; after analyses, estimates were transformed back from the logarithmic scale to present results in the original dollar measurement. The depressive symptoms variable was estimated using a negative binomial approach.
The DID design assumes that trends across expansion and nonexpansion groups are parallel in the “pretreatment” period prior to 2014, so that any differences afterward may be attributable to the “treatment effect” of ACA Medicaid expansion. We considered health and economic trends during the 2010–2016 study period and found no reasonable shocks that would have differentially affected expansion and nonexpansion states. We also adjusted our analyses to control for economic indicators, such as employment, income, and wealth. In addition, we empirically assessed the equality of the preexpansion time trends (2010–2012) in expansion and nonexpansion states by testing the interaction of time (quarter) with a dummy variable for expansion versus nonexpansion state, followed by a Wald test to jointly test the null hypothesis that the interaction terms were equal to zero. These showed a nonsignificant interaction term for each of the outcomes, assuring that the parallel trends assumption was satisfied (Dimick & Ryan, 2014). Regression-adjusted plots from parallel trends testing are shown in Supplementary Figure 2.
Sensitivity Analyses
While our main models focused on respondents with low education, excluding individuals in the 11 states with pre-2014 Medicaid expansions, we conducted sensitivity analyses with alternative sample definitions of low SES (i.e., income ≤138% FPL). Additional sensitivity analyses focused on using alternative state sampling: (a) examining all 50 states, (b) another set of models excluding only the 6 “early expander” states that opted to expand Medicaid under the ACA prior to 2014, and (c) excluding late-expanding states that expanded their Medicaid programs after 2014 (Alaska—9/15, Indiana—2/15, Louisiana—7/16, Montana—1/16, and Pennsylvania—1/15), in addition to excluding the 11 states with pre-2014 Medicaid expansions as done in the main analyses. See Supplementary Table 2 for our classification of states.
In the primary analyses of respondents with low education in the 40 states without pre-2014 Medicaid expansion, we also examined our study outcomes in the subgroup of individuals with self-reported chronic diseases (eight conditions noted above, in the section describing covariates). In addition to the main GEE analyses, we also examined alternative analytic approaches including individual fixed effects models, mixed models, and a model including state fixed effects.
Lastly, we conducted a falsification test focused on individuals aged 65 and older who had low education and were in the primary 40-state sample (n = 1,963 in expansion states and n = 3,330 in nonexpansion states). As these individuals were eligible for Medicare throughout the study period, we would expect to observe no significant changes in coverage or health care associated with Medicaid expansion; therefore, this group serves as a useful comparison.
Results
Respondent Characteristics
Low-education respondents in expansion states (n = 633) had similar age and gender distributions compared to respondents in nonexpansion states (n = 1,455) at baseline (N = 2,088; Table 1). However, there was a greater proportion of non-Hispanic black (17.3% vs. 11.3%) and Hispanic (17.7% vs. 8.7%) individuals in nonexpansion states compared with expansion states. Individuals in nonexpansion states also had lower levels of baseline income (30.9% vs. 23.2% in the lowest income category with ≤138% FPL) and excellent or very good health status (33.5% vs. 41.1%) than those in expansion states. The 2010 baseline uninsured rate was higher in nonexpansion states than in expansion states (27.4% vs. 17.1%; Supplementary Table 3).
Table 1.
Baseline Characteristics of HRS Respondents Aged 51–64 Years With High School Education or Less, 2010
| Characteristics | Mean or % of HRS respondents | |
|---|---|---|
| Expansion states (n = 633; population weighted N = 3,430,425) | Nonexpansion states (n = 1,455; population weighted N = 6,412,975) | |
| Age (years) | 54.3 | 54.2 |
| Female | 50.7% | 50.2% |
| Race/ethnicity | ||
| White/Non-Hispanic | 75.7% | 61.7% |
| Black/Non-Hispanic | 11.3% | 17.3% |
| Hispanic | 8.7% | 17.7% |
| Other | 4.3% | 3.4% |
| Income, % FPL | ||
| ≤138 | 23.2% | 30.9% |
| 139–250 | 18.1% | 19.1% |
| 251–400 | 16.1% | 18.9% |
| >400 | 42.6% | 31.1% |
| Wealth, total assets (2014 dollars) | ||
| Quartile 1 | 34.4% | 36.7% |
| Quartile 2 | 29.3% | 38.9% |
| Quartile 3 | 24.7% | 17.7% |
| Quartile 4 | 11.6% | 6.7% |
| Married | 68.3% | 67.1% |
| Employed | 66.9% | 60.7% |
| Health excellent or very good | 41.1% | 33.5% |
| Chronic health conditions | ||
| Diabetes | 18.5% | 18.4% |
| Hypertension | 47.7% | 46.5% |
| Cardiovascular disease | 14.8% | 13.6% |
| Stroke | 3.9% | 3.9% |
| Chronic lung disease | 10.3% | 9.7% |
| Cancer | 7.8% | 7.8% |
| Arthritis | 36.8% | 40.1% |
| Depression | 27.3% | 26.4% |
Notes: HRS = Health and Retirement Study; FPL = federal poverty level. Estimates incorporate survey weights. Respondents in 11 states with pre-2014 expansions of Medicaid eligibility are excluded.
Unadjusted Trends in Access, Health Care, and Health
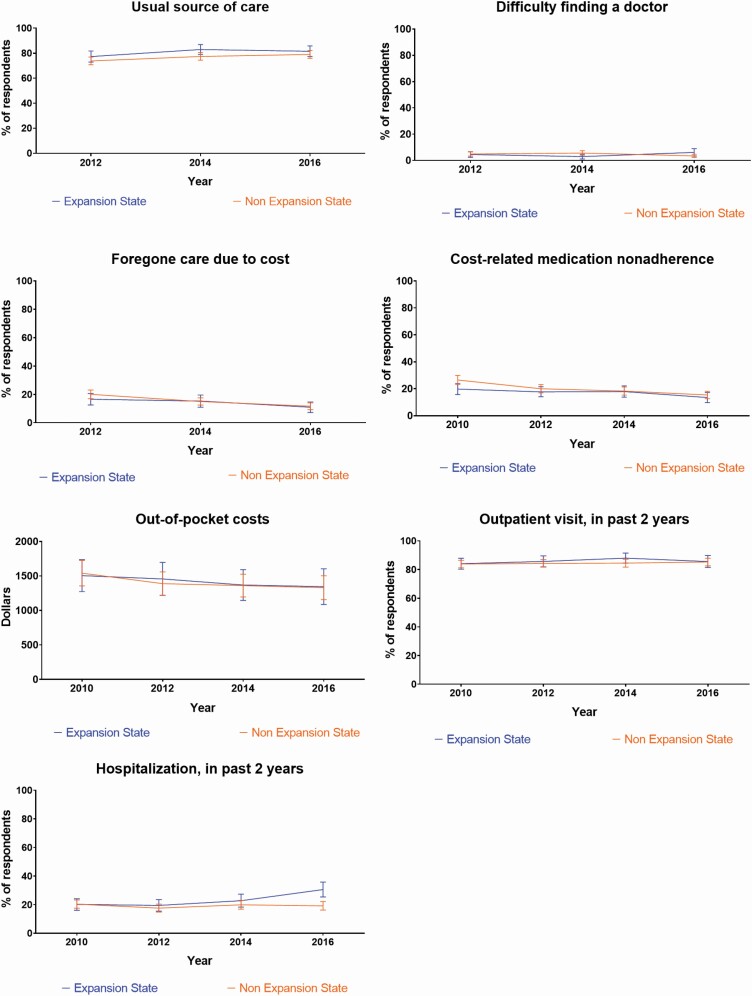
Figures 1 and 2 display trends in study outcomes that are adjusted for the complex survey design without covariates. In general, rates of coverage increased over time in both expansion and nonexpansion states for low-education adults aged 51–64 years (Figure 1). Rates of foregone care and cost-related medication nonadherence appeared to decline over time in both expansion and nonexpansion states for low-education respondents (Figure 2).
Figure 1.
Unadjusted trends in coverage and health measures for 51- to 64-year-old low-education respondents before and after Medicaid expansion. Expansion states are those that expanded Medicaid under the Affordable Care Act as of 2016 and include Alaska, Arkansas, Colorado, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Michigan, Montana, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Washington, and West Virginia. Eleven states (Arizona, California, Connecticut, District of Columbia, Delaware, Hawaii, Massachusetts, Minnesota, New York, Vermont, and Wisconsin) that expanded Medicaid prior to 2014 were excluded from the analysis. Nonexpansion states are those that did not expand Medicaid under the Affordable Care Act as of 2016 and include Alabama, Florida, Georgia, Idaho, Kansas, Maine, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, and Wyoming.
Figure 2.
Unadjusted trends in access and health care utilization measures for 51- to 64-year-old low-education respondents before and after Medicaid expansion. Expansion states are those that expanded Medicaid under the Affordable Care Act as of 2016 and include Alaska, Arkansas, Colorado, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Michigan, Montana, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Washington, and West Virginia. Eleven states (Arizona, California, Connecticut, District of Columbia, Delaware, Hawaii, Massachusetts, Minnesota, New York, Vermont, and Wisconsin) that expanded Medicaid prior to 2014 were excluded from the analysis. Nonexpansion states are those that did not expand Medicaid under the Affordable Care Act as of 2016 and include Alabama, Florida, Georgia, Idaho, Kansas, Maine, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, and Wyoming.
DID Analysis
In DID regression analyses for low-education adults aged 51–64 years adjusted for covariates, insurance coverage rates increased in both expansion (+9.0 percentage points) and nonexpansion (+11.7 percentage points) states but the difference between the two was nonsignificant (p = .40; Table 2). With regard to types of coverage, low-education adults aged 51–64 years had greater increases in Medicaid coverage in expansion (+10.6 percentage points) than in nonexpansion (+3.2 percentage points) states (DID +7.4 percentage points, p = .001). Trends in private insurance show the converse pattern, with nonsignificantly greater increases in nonexpansion states than expansion states after 2014 for low-education respondents (DID −6.0 percentage points, p = .05; Table 2).
Table 2.
DID Regression Analysis for 51- to 64-Year-Old Low-Education Respondents in Medicaid Expansion Versus Nonexpansion States
| Outcomes | Expansion states | Nonexpansion states | Adjusted DID (95% CI) | DID, p value | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Postexpansion | ∆ After expansion | Baseline | Postexpansion | ∆ After expansion | |||
| Coverage | ||||||||
| Any insurance (%) | 80.2 | 89.2 | +9.0 | 75.5 | 87.2 | +11.7 | −2.6 (−8.7 to 3.5) | .40 |
| Medicaid (%) | 10.3 | 20.9 | +10.6 | 8.6 | 11.8 | +3.2 | +7.4 (3.1 to 11.7) | .001 |
| Private insurance (%) | 61.7 | 59.1 | −2.6 | 59.3 | 62.7 | +3.4 | −6.0 (−12.2 to 0.1) | .05 |
| Access | ||||||||
| Usual source of care (%) | 76.5 | 80.5 | +4.0 | 74.4 | 79.7 | +5.3 | −1.2 (−8.0 to 5.7) | .74 |
| Difficulty finding a physician (%) | 4.5 | 6.1 | +1.6 | 4.9 | 3.4 | −1.5 | +3.1 (−0.9 to 7.0) | .13 |
| Foregone care due to cost (%) | 17.6 | 11.5 | −6.1 | 19.6 | 11.2 | −8.4 | +2.3 (−3.4 to 7.9) | .43 |
| Cost-related medication nonadherence (%) | 20.8 | 13.7 | −7.1 | 25.9 | 15.1 | −10.8 | +3.6 (−1.9 to 9.2) | .20 |
| Out-of-pocket costsa ($) | 1,620.6 | 1,425.4 | −195.2 | 1,709.1 | 1,497.4 | −211.7 | +16.5 (−426.8 to 459.8) | .94 |
| Utilization | ||||||||
| Outpatient visitb, in past 2 years (%) | 83.9 | 84.9 | +1.0 | 84.0 | 85.6 | +1.6 | −0.6 (−6.5 to 5.3) | .84 |
| Hospitalization, in past 2 years (%) | 20.7 | 29.9 | +9.2 | 20.2 | 19.1 | −1.1 | +10.4 (3.6 to 17.2) | .003 |
| Health | ||||||||
| Health, excellent or very good (%) | 37.7 | 30.9 | −6.8 | 34.3 | 27.9 | −6.4 | −0.5 (−6.7 to 5.7) | .88 |
| Depressive symptomsc | 1.9 | 1.7 | −0.2 | 2.0 | 1.6 | −0.4 | +0.2 (−0.1 to 0.5) | .21 |
| Health limits paid/house/any work (%) | 37.3 | 40.9 | +3.6 | 35.4 | 46.4 | +11.0 | −7.5 (−12.8 to −2.2) | .006 |
Notes: CI = confidence interval; DID = difference-in-differences. Baseline year is 2010, except for variables introduced in 2012 (usual source of care, difficulty finding a physician, and foregone care due to cost). Generalized estimating equations with Huber–White robust standard errors clustered at the respondent level for longitudinal analyses, adjusting for age, gender, race/ethnicity, wealth, employment, and marital status.
aOut-of-pocket costs were log-transformed to approximate a normal distribution in analyses; estimates were transformed back from the logarithmic scale to present mean dollar amounts and confidence intervals.
bOutpatient visits include visits to the clinic, physician’s office, or emergency room.
cDepressive symptoms were measured using the Center for Epidemiological Studies Depression scale.
Low-education adults aged 51–64 years experienced an increased likelihood of hospitalizations in Medicaid expansion (+9.2 percentage points) compared with nonexpansion states (−1.1 percentage points; DID +10.4 percentage points, p = .003; Table 2). While low-education respondents in both groups experienced an increased likelihood of reporting limitations in paid work/housework over time, likely due to aging, the increase in Medicaid expansion states (+3.6 percentage points) was significantly smaller than the increase in the nonexpansion states (+11.0 percentage points; DID −7.5 percentage points, p = .006; Table 2). There were no other significant differences in access, utilization, or health trends between expansion and nonexpansion states in 2010–2016 (Table 2).
Sensitivity/Subgroup Analyses
Restricting the analysis to respondents with low incomes less than or equal to 138% of FPL (N = 994) rather than low education yielded similar findings with respect to greater Medicaid coverage in expansion compared with nonexpansion states (DID +13.8 percentage points, p = .003; Table 3). We also saw similar increases in hospitalization in expansion versus nonexpansion states for low-income respondents but the findings were nonsignificant in this sensitivity analysis (DID +8.0 percentage points, p = .16; Table 3). However, we saw notable differences with regard to access measures, demonstrating greater difficulty finding a physician (DID +8.3 percentage points, p = .04), and lesser improvements in cost-related medication nonadherence (DID +11.5 percentage points, p = .04) for low-income adults aged 51–64 years in expansion compared with nonexpansion states (Table 3).
Table 3.
DID Regression Analysis for 51- to 64-Year-old Low-Income Respondents in Medicaid Expansion Versus Nonexpansion States
| Outcomes | Expansion states | Nonexpansion states | Adjusted DID (95% CI) | DID, p value | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Postexpansion | ∆ After expansion | Baseline | Postexpansion | ∆ After expansion | |||
| Coverage | ||||||||
| Any insurance (%) | 63.8 | 86.3 | +22.5 | 65.0 | 81.5 | +16.5 | +5.9 (−4.8 to 16.7) | .28 |
| Medicaid (%) | 30.8 | 46.5 | +15.7 | 24.6 | 26.4 | +1.8 | +13.8 (4.8 to 22.9) | .003 |
| Private insurance (%) | 22.0 | 23.0 | +1.0 | 30.1 | 39.7 | +9.6 | −8.5 (−18.7 to 1.6) | .10 |
| Access | ||||||||
| Usual source of care (%) | 63.3 | 76.1 | +12.8 | 67.8 | 69.9 | +2.1 | +10.6 (−1.4 to 22.6) | .08 |
| Difficulty finding a physician (%) | 8.7 | 12.4 | +3.7 | 10.1 | 5.5 | −4.6 | +8.3 (0.2 to 16.3) | .04 |
| Foregone care due to cost (%) | 29.7 | 22.2 | −7.5 | 28.0 | 18.3 | −9.7 | +2.1 (−10.2 to 14.5) | .73 |
| Cost-related medication nonadherence (%) | 26.6 | 24.2 | −2.4 | 35.0 | 21.1 | −13.9 | +11.5 (0.3 to 22.6) | .04 |
| Out-of-pocket costsa ($) | 1105.7 | 1125.1 | +19.4 | 1571.0 | 1264.5 | −306.5 | +325.9 (−261.1 to 912.9) | .28 |
| Utilization | ||||||||
| Outpatient visitb, in past 2 years (%) | 76.1 | 76.5 | +0.4 | 81.5 | 81.3 | −0.2 | +0.5 (−11.1 to 12.2) | .93 |
| Hospitalization, in past 2 years (%) | 34.1 | 38.9 | +4.8 | 27.8 | 24.7 | −3.1 | +8.0 (−3.2 to 19.2) | .16 |
| Health | ||||||||
| Health, excellent or very good (%) | 22.5 | 20.2 | −2.3 | 18.7 | 21.9 | +3.2 | −5.5 (−13.7 to 2.8) | .19 |
| Depressive symptomsc | 2.7 | 2.7 | 0.0 | 2.7 | 2.7 | 0.0 | 0.0 (−0.7 to 0.7) | .96 |
| Health limits paid/house/any work (%) | 60.5 | 66.2 | +5.7 | 57.2 | 62.9 | +5.7 | 0.0 (−8.1 to 8.1) | .995 |
Notes: CI = confidence interval; DID = difference-in-differences. Baseline year is 2010, except for variables introduced in 2012 (usual source of care, difficulty finding a physician, and foregone care due to cost). Generalized estimating equations with Huber–White robust standard errors clustered at the respondent level for longitudinal analyses, adjusting for age, gender, race/ethnicity, wealth, employment, and marital status.
aOut-of-pocket costs were log-transformed to approximate a normal distribution in analyses; estimates were transformed back from the logarithmic scale to present mean dollar amounts and confidence intervals.
bOutpatient visits include visits to the clinic, physician’s office, or emergency room.
cDepressive symptoms were measured using the Center for Epidemiological Studies Depression scale.
In subgroup analyses focused on low-education adults aged 51–64 years with chronic diseases, we found similar results to the main findings in the overall low-education sample (Supplementary Table 4). In other sensitivity analyses with alternative sample selection by respondent SES definition (low education vs. low income) or states selected (35, 40, 45, or all 51 states), or alternative analytic approaches (individual fixed effects, mixed models, or state fixed effects), findings remained largely similar to the primary analyses given in Table 2 (Supplementary Tables 5–14).
Falsification Test
We also conducted a falsification test with low-education adults aged 65 and older who were eligible for Medicare and thus would not be expected to experience significant changes due to Medicaid expansion. Aside from a small difference in trends in having a usual source of care, we found no significant differences between trends in expansion and nonexpansion states for coverage, hospitalizations, or any other study outcomes for this group of older adults (Supplementary Table 15).
Discussion
In this longitudinal DID study conducted before and after the ACA Medicaid expansion, rates of coverage increased similarly for low-education adults aged 51–64 years in both expansion and nonexpansion states, with a greater increase in rates of Medicaid coverage in expansion states. Low-education adults aged 51–64 years also experienced greater increases in hospitalization in expansion states compared with nonexpansion states. However, there were no significant differential improvements in access to care or outpatient visits in the 2 years after the Medicaid expansion in 2014. Likewise, low-education adults aged 51–64 years did not report greater overall health improvements associated with Medicaid expansion, though they did have lesser declines in functioning that limited work and other activities compared to individuals in nonexpansion states.
Regarding insurance coverage, this study replicated findings from previous studies of adults aged 51–64 years (Levy et al., 2018). Rates of coverage increased in both expansion and nonexpansion states, with greater increases in Medicaid in expansion states and greater increases in private insurance in nonexpansion states (Levy et al., 2018). Thus, as Levy et al. noted, the “treatment effect” of Medicaid expansion on overall rates of coverage appeared minimal, but the type of insurance gained (public vs. private) differs between expansion and nonexpansion states (Levy et al., 2018). Hospital payer mix shifted from uninsured to Medicaid accordingly in Medicaid expansion states (Admon et al., 2019; Barakat et al., 2017, 2020; Freedman et al., 2017; Mondesir et al., 2019; Nikpay et al., 2016). Overall, our coverage findings likely reflect not just expansion of Medicaid in expansion states, but also other ACA coverage expansions including the expansion of private health insurance exchange plans in both expansion and nonexpansion states.
In terms of health care access, this age group had high baseline rates of access, so they may have had less room for improvement compared with younger adults. More than 75% of the low-education study sample already had a usual source of care and fewer than 5% had difficulty finding a physician before Medicaid expansion. However, other measures of access had greater potential for improvement. For example, approximately 20% of low-education respondents reported foregone care and cost-related medication nonadherence at baseline. These access measures improved for low-education adults aged 51–64 years in both expansion and nonexpansion states, and we found no significant differential effects associated with Medicaid expansion.
However, there was a trend toward greater difficulty finding a physician and lesser improvements in cost-related medication adherence among low-education adults aged 51–64 years in expansion states compared with nonexpansion states, and this differential worsening was significant in analyses among low-income individuals. While the low-income sample was smaller, it was also the group more likely to experience changes in insurance under the ACA and thus may explain larger effect sizes seen in low-income compared with low-education respondents. Overall, the access findings signal concern that increased rates of Medicaid coverage in expansion states may not completely translate to improved access and, thus, may lead to pent-up demand for routine care that could result in acute care utilization.
For utilization, the study’s key finding showed that low-education adults aged 51–64 years in expansion states experienced an increased likelihood of hospitalization after Medicaid expansion. Several prior studies have found no increases in hospitalization after Medicaid expansion, though these studies focused on the total non-older adult population aged 19–64 years (Admon et al., 2019; Freedman et al., 2017; Pickens et al., 2018). Another study of all non-older adults using a different data source found that rates of hospitalization increased in the first year after Medicaid expansion, but that there was no longer a significant difference between expansion and nonexpansion states by 2 years after expansion (Miller & Wherry, 2017).
As low-SES (whether low-education or low-income) adults aged 51–64 years are more likely to have chronic health conditions, they may have had greater pent-up demand for health care services before Medicaid expansion and greater deterrents to seek care due to copays and other cost sharing associated with private plans or a lack of insurance. A study of HRS participants conducted before the ACA followed adults with chronic conditions before and after reaching age 65 and found increases in health care utilization and costs after adults became eligible for Medicare coverage (McWilliams et al., 2007b). As many adults were newly diagnosed with diabetes, cancer, and other serious health conditions after Medicaid expansion (Kaufman et al., 2015; Soni et al., 2018; Torres et al., 2017; Winkelman & Chang, 2018), it may take time for these individuals to engage with outpatient care and control their chronic conditions to reduce the need for hospitalization. More recent studies have found that individuals with diabetes and other chronic conditions have experienced decreases in hospitalizations associated with these chronic conditions after Medicaid expansion (Barakat et al., 2020; Freedman et al., 2017; Mondesir et al., 2019).
Our observation of increased hospitalization rates in the setting of similar coverage rates suggests that the type of coverage—Medicaid versus private insurance—may contribute to 51- to 64-year olds’ decision making about when and where to seek care. As Medicaid provides generous coverage with little or no cost sharing, it is possible that it presents a lower bar to obtaining many health care services, including hospitalizations. This pattern suggests potential pent-up demand for hospital care that is similar to prior research on uninsured adults with chronic conditions who gain Medicare coverage at age 65 (Card et al., 2008; McWilliams et al., 2007b). For example, in Card et al.’s study, hospitalizations increased sharply after age 65, but in differential patterns for high- versus low-SES individuals—high-SES individuals were more likely to have a supplemental private plan in addition to Medicare and more likely to have hospitalizations for elective procedures such as joint replacements, while low-SES individuals were more likely to be hospitalized for ambulatory care sensitive conditions such as congestive heart failure after age 65 (Card et al., 2008). It is possible that we may see future declines in hospitalizations as low-SES adults aged 51–64 years have chronic conditions diagnosed and treated effectively. It is also possible that effective chronic disease management may lead to improved health, though our study may have been underpowered to detect changes in health observed in studies with larger samples (Miller et al., 2019).
The study has several potential limitations. First, we used self-reported measures, which may be limited by social desirability or recall bias, though the HRS is a robust longitudinal study and such effects are unlikely to affect respondents in expansion and nonexpansion states differentially. Second, the study’s low-education 51- to 64-year-old adult sample was relatively small, limiting the power to identify small changes associated with Medicaid expansion. Third, we were limited to a 2-year look-back period for certain HRS interview questions (difficulty finding a physician, foregone care, cost-related medication nonadherence, out-of-pocket costs, outpatient visits, and hospitalizations). Fourth, the selection of the low-SES sample by educational attainment may also bias estimates toward the null, as approximately a third of the sample had incomes greater than 400% FPL and may not have been eligible for Medicaid or subsidized individual private insurance plans. However, sensitivity analyses conducted with individuals who had incomes less than 138% FPL showed overall similar trends. In addition, our falsification test showed no changes in hospitalization for adults aged 65 and older who would be eligible for Medicare, supporting the specificity of the study’s finding for adults aged 51–64 years in Medicaid expansion states.
Despite these limitations, the study has important implications for the health care of adults aged 51–64 years after Medicaid expansion. The increase in hospitalizations for this age group highlights the need to assess for potential drivers of hospitalization, such as poorly controlled chronic conditions or social needs that affect health care utilization. To improve the diagnosis and management of chronic conditions in adults aged 51–64 years, states that have not expanded Medicaid should consider policies to expand health insurance coverage. Such policies may include Medicaid expansion, expansion of eligibility for financial assistance on state-based exchanges, or options for younger adults to buy into Medicare, such as the recently introduced Medicare at 50 Act (S. 470, 2019). The findings also suggest that other policy solutions beyond coverage expansion are needed to improve access to ambulatory care and health outcomes among low-SES adults in this age group. Implementation and appropriate evaluation of care management and care coordination programs will be essential to addressing navigation challenges and social drivers of poor health outcomes that drive acute care utilization. Several care management demonstration programs are currently being tested by states and the federal government (Center for Medicare & Medicaid Innovation, n.d.). Lessons learned from these endeavors might inform optimal strategies for improving the care experience and overall health of low-SES adults approaching retirement.
In summary, low-education adults aged 51–64 years had increased rates of Medicaid coverage and increased likelihood of hospitalization after Medicaid expansion, suggesting poor baseline access to chronic disease management and pent-up demand for health care services.
Supplementary Material
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (NIH; grant number K08AG056591 to R. Tipirneni and grant numbers P30 AG024824, P30 AG053760, and R01 AG053972 to K. M. Langa). The Health and Retirement Study is funded by the National Institute on Aging (grant number U01 AG009741) and performed at the Institute for Social Research, University of Michigan. The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation of the manuscript; and decision to submit the manuscript for publication. The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Previous Presentation
This work was presented at the Gerontological Society of America Annual Scientific Meeting, Austin, TX, November 13, 2019.
Conflict of Interest
The authors have no financial, personal, or any other conflict of interest for this article.
Author Contributions
R. Tipirneni, H. G. Levy, K. M. Langa, R. J. McCammon, K. Zivin, and J. Z. Ayanian conceptualized and designed the study. R. Tipirneni, R. J. McCammon, and M. Karmakar analyzed and interpreted the data. R. Tipirneni, H. G. Levy, K. M. Langa, R. J. McCammon, K. Zivin, J. Luster, M. Karmakar, and J. Z. Ayanian prepared the manuscript.
References
- Admon, A J, Valley, T S, Ayanian, J Z, Iwashyna, T J, Cooke, C R, & Tipirneni, R. (2019). Trends in hospital utilization after Medicaid expansion. Medical Care, 57(4), 312–317. doi: 10.1097/MLR.0000000000001082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barakat, M T, Mithal, A, Huang, R J, Mithal, A, Sehgal, A, Banerjee, S, & Singh, G. (2017). Affordable Care Act and healthcare delivery: A comparison of California and Florida hospitals and emergency departments. PLoS One, 12(8), e0182346. doi: 10.1371/journal.pone.0182346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barakat, M T, Mithal, A, Huang, R J, Sehgal, A, Sehgal, A, Singh, G, & Banerjee, S. (2020). Recent trends and the impact of the Affordable Care Act on emergency department visits and hospitalizations for gastrointestinal, pancreatic, and liver diseases. Journal of Clinical Gastroenterology, 54(3), e21–e29. doi: 10.1097/MCG.0000000000001102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card, D, Dobkin, C, & Maestas, N. (2007). The impact of health insurance status on treatment intensity and health outcomes. RAND Corporation.https://www-rand-org.proxy.lib.umich.edu/pubs/working_papers/WR505.html [Google Scholar]
- Card, D, Dobkin, C, & Maestas, N. (2008). The impact of nearly universal insurance coverage on health care utilization: Evidence from Medicare. The American Economic Review, 98(5), 2242–2258. doi: 10.1257/aer.98.5.2242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card, D, Dobkin, C, & Maestas, N. (2009). Does Medicare save lives? The Quarterly Journal of Economics, 124(2), 597–636. doi: 10.1162/qjec.2009.124.2.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case, A, & Deaton, A. (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15078–15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case, A, & Deaton, A. (2017). Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity, 2017, 397–476. doi: 10.1353/eca.2017.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicare & Medicaid Innovation. (n.d.). [Website].U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. Retrieved January 5, 2020 from https://innovation.cms.gov/ [Google Scholar]
- Chetty, R, Stepner, M, Abraham, S, Lin, S, Scuderi, B, Turner, N, Bergeron, A, & Cutler, D. (2016). The association between income and life expectancy in the United States, 2001–2014. Journal of the American Medical Association, 315(16), 1750–1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimick, J B, & Ryan, A M. (2014). Methods for evaluating changes in health care policy: The difference-in-differences approach. Journal of the American Medical Association, 312(22), 2401–2402. doi: 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- Fedewa, S A, Yabroff, K R, Smith, R A, Goding Sauer, A, Han, X, & Jemal, A. (2019). Changes in breast and colorectal cancer screening after Medicaid expansion under the Affordable Care Act. American Journal of Preventive Medicine, 57(1), 3–12. doi: 10.1016/j.amepre.2019.02.015 [DOI] [PubMed] [Google Scholar]
- Freedman, S, Nikpay, S, Carroll, A, & Simon, K. (2017). Changes in inpatient payer-mix and hospitalizations following Medicaid expansion: Evidence from all-capture hospital discharge data. PLoS One, 12(9), e0183616. doi: 10.1371/journal.pone.0183616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study. (2017). Sample sizes and response rates. Retrieved from https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf
- Heiss, F, Venti, S F, & Wise, D A. (2014). The persistence and heterogeneity of health among older Americans (NBER Working Paper No. 20306). National Bureau of Economic Research. https://www.nber.org/papers/w20306. doi: 10.3386/w20306 [DOI] [Google Scholar]
- Hendryx, M, & Luo, J. (2018). Increased cancer screening for low-income adults under the Affordable Care Act Medicaid expansion. Medical Care, 56(11), 944–949. doi: 10.1097/MLR.0000000000000984 [DOI] [PubMed] [Google Scholar]
- Kaufman, H W, Chen, Z, Fonseca, V A, & McPhaul, M J. (2015). Surge in newly identified diabetes among Medicaid patients in 2014 within Medicaid expansion states under the Affordable Care Act. Diabetes Care, 38(5), 833–837. doi: 10.2337/dc14-2334 [DOI] [PubMed] [Google Scholar]
- Levy, H, Buchmueller, T C, & Nikpay, S. (2018). Health reform and retirement. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(4), 713–722. doi: 10.1093/geronb/gbw115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McWilliams, J M, Meara, E, Zaslavsky, A M, & Ayanian, J Z (2007a). Health of previously uninsured adults after acquiring Medicare coverage. Journal of the American Medical Association, 298(24), 2886–2894. doi: 10.1001/jama.298.24.2886 [DOI] [PubMed] [Google Scholar]
- McWilliams, J M, Meara, E, Zaslavsky, A M, & Ayanian, J Z (2007b). Use of health services by previously uninsured Medicare beneficiaries. The New England Journal of Medicine, 357(2), 143–153. doi: 10.1056/NEJMsa067712 [DOI] [PubMed] [Google Scholar]
- McWilliams, J M, Zaslavsky, A M, Meara, E, & Ayanian, J Z. (2004). Health insurance coverage and mortality among the near-elderly. Health Affairs (Project Hope), 23(4), 223–233. doi: 10.1377/hlthaff.23.4.223 [DOI] [PubMed] [Google Scholar]
- Medicare at 50 Act, S. 470, 116th Congress (2019–2020). https://www.congress.gov/bill/116th-congress/senate-bill/470.
- Miller, S, Altekruse, S, Johnson, N, & Wherry, L R. (2019). Medicaid and mortality: New evidence from linked survey and administrative data (NBER Working Paper No. 26081). National Bureau of Economic Research. https://www.nber.org/papers/w26081. doi: 10.3386/w26081 [DOI] [Google Scholar]
- Miller, S, & Wherry, L R. (2017). Health and access to care during the first 2 years of the ACA Medicaid expansions. The New England Journal of Medicine, 376(10), 947–956. doi: 10.1056/NEJMsa1612890 [DOI] [PubMed] [Google Scholar]
- Mondesir, F L, Kilgore, M L, Shelley, J P, Levitan, E B, Huang, L, Riggs, K R, Pisu, M, Li, Y, Bronstein, J M, Agne, A, & Cherrington, A L. (2019). Medicaid expansion and hospitalization for ambulatory care-sensitive conditions among nonelderly adults with diabetes. The Journal of Ambulatory Care Management, 42(4), 312–320. doi: 10.1097/JAC.0000000000000280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikpay, S, Buchmueller, T, & Levy, H G. (2016). Affordable Care Act Medicaid expansion reduced uninsured hospital stays in 2014. Health Affairs (Project Hope), 35(1), 106–110. doi: 10.1377/hlthaff.2015.1144 [DOI] [PubMed] [Google Scholar]
- Pickens, G, Karaca, Z, Cutler, E, Dworsky, M, Eibner, C, Moore, B, Gibson, T, Iyer, S, & Wong, H S. (2018). Changes in hospital inpatient utilization following health care reform. Health Services Research, 53(4), 2446–2469. doi: 10.1111/1475-6773.12734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky, D, Doshi, J A, Escarce, J, Manning, W, Paddock, S M, Cen, L, & Rogowski, J. (2009). The health effects of Medicare for the near-elderly uninsured. Health Services Research, 44(3), 926–945. doi: 10.1111/j.1475-6773.2009.00964.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- RAND Corporation. (2019). Data products of the center for the study of aging. Retrieved from https://www.rand.org/well-being/social-and-behavioral-policy/centers/aging/dataprod.html
- Sasson, I, & Hayward, M D. (2019). Association between educational attainment and causes of death among white and black US adults, 2010–2017. Journal of the American Medical Association, 322(8), 756–763. doi: 10.1001/jama.2019.11330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon, K, Soni, A, & Cawley, J. (2017). The impact of health insurance on preventive care and health behaviors: Evidence from the first two years of the ACA medicaid expansions. Journal of Policy Analysis and Management, 36(2), 390–417. doi: 10.1002/pam.21972 [DOI] [PubMed] [Google Scholar]
- Soldo, B J, Mitchell, O S, Tfaily, R, & McCabe, J F. (2006). Cross-cohort differences in health on the verge of retirement (NBER Working Paper No. 12762). National Bureau of Economic Research. https://www.nber.org/papers/w12762. doi: 10.3386/w12762 [DOI] [Google Scholar]
- Sommers, B D, Baicker, K, & Epstein, A M. (2012). Mortality and access to care among adults after state Medicaid expansions. The New England Journal of Medicine, 367(11), 1025–1034. doi: 10.1056/NEJMsa1202099 [DOI] [PubMed] [Google Scholar]
- Sommers, B D, Gunja, M Z, Finegold, K, & Musco, T. (2015). Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. Journal of the American Medical Association, 314(4), 366–374. doi: 10.1001/jama.2015.8421 [DOI] [PubMed] [Google Scholar]
- Sommers, B D, Long, S K, & Baicker, K. (2014). Changes in mortality after Massachusetts health care reform: A quasi-experimental study. Annals of Internal Medicine, 160(9), 585–593. doi: 10.7326/M13-2275 [DOI] [PubMed] [Google Scholar]
- Soni, A, Simon, K, Cawley, J, & Sabik, L. (2018). Effect of Medicaid expansions of 2014 on overall and early-stage cancer diagnoses. American Journal of Public Health, 108(2), 216–218. doi: 10.2105/AJPH.2017.304166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega, A, Faul, J D, Ofstedal, M B, Langa, K M, Phillips, J W, & Weir, D R. (2014). Cohort profile: The health and retirement study (HRS). International Journal of Epidemiology, 43(2), 576–585. doi: 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Henry J. Kaiser Family Foundation. (n.d.). Status of state action on the Medicaid expansion decision. Retrieved January, 5, 2020 from https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- Torres, H, Poorman, E, Tadepalli, U, Schoettler, C, Fung, C H, Mushero, N, Campbell, L, Basu, G, & McCormick, D. (2017). Coverage and access for Americans with chronic disease under the Affordable Care Act: A quasi-experimental study. Annals of Internal Medicine, 166(7), 472–479. doi: 10.7326/M16-1256 [DOI] [PubMed] [Google Scholar]
- Van Der Wees, P J, Zaslavsky, A M, & Ayanian, J Z. (2013). Improvements in health status after Massachusetts health care reform. The Milbank Quarterly, 91(4), 663–689. doi: 10.1111/1468-0009.12029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wherry, L R, & Miller, S. (2016). Early coverage, access, utilization, and health effects associated with the Affordable Care Act Medicaid expansions: A quasi-experimental study. Annals of Internal Medicine, 164(12), 795–803. doi: 10.7326/M15-2234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkelman, T N A, & Chang, V W. (2018). Medicaid expansion, mental health, and access to care among childless adults with and without chronic conditions. Journal of General Internal Medicine, 33(3), 376–383. doi: 10.1007/s11606-017-4217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, S H, & Schoomaker, H. (2019). Life expectancy and mortality rates in the United States, 1959–2017. Journal of the American Medical Association, 322(20), 1996–2016. doi: 10.1001/jama.2019.16932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin, K, Llewellyn, D J, Lang, I A, Vijan, S, Kabeto, M U, Miller, E M, & Langa, K M. (2010). Depression among older adults in the United States and England. The American Journal of Geriatric Psychiatry, 18(11), 1036–1044. doi: 10.1097/JGP.0b013e3181dba6d2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.