On May 19, 2021, the Delta Variant of Concern (VOC), formerly known as the Indian VOC or B 1.617.2, became the dominant strain of SARS-CoV-2 in Scotland. The Alpha VOC (formerly known as the Kent VOC, B.1.1.7, or S gene negative) had been the dominant strain previously, but it has rapidly been replaced (appendix p 1).
Samples were analysed using ThermoFisher's TaqPath RT-PCR, which tests for the presence of three target genes from SARS-CoV-2. S gene-negative samples had a deletion in S gene of B.1.1.7 (Alpha VOC) at position 69-70, with cycle threshold (Ct) values less than 30 for at least one of the OR and N genes. S gene-positive samples had Ct values less than 30 for the S gene and valid Ct values for the other two genes. In contrast, a weak S gene-positive sample had a Ct of 30 or less for S. Sequencing data from Scotland has found that for April 1 to May 28, 2021, the latest date until which data were available, 97% of S gene positive cases sequenced in Scotland were the Delta variant and that 99% of Delta variants were S gene positive.
EAVE II is a Scotland-wide COVID-19 surveillance platform that has been used to track and forecast the epidemiology of COVID-19, inform risk stratification, and investigate vaccine effectiveness and safety.1, 2, 3, 4 It comprises national health-care datasets on 5·4 million people (about 99% of the Scottish population) linked through Scotland's unique Community Health Index number.
We used the EAVE II platform to undertake a cohort analysis to describe the demographic profile of COVID-19 patients, investigate the risk of hospital admission for COVID-19, and estimate vaccine effectiveness in preventing COVID-19 hospital admissions in S gene-positive cases. We also employed a test-negative design to estimate vaccine effectiveness against risk of SARS-CoV-2 infection.5 This analysis was based upon all individuals who have a PCR test for SARS-CoV-2 in the study period, and it compares the proportions positive among individuals vaccinated at the time of the swab test with those unvaccinated when they are tested, adjusting for demographic and temporal covariates.
Building on methods that have previously been described in detail, we defined a COVID-19 hospital admission as being within 14 days of testing positive for SARS-CoV-2.3, 5 Individuals who tested positive within 2 days after a hospital admission were also included. Individuals tested during a hospital stay from day 3 onwards were excluded. Hospital-acquired COVID-19 infections were excluded.
Our analysis covered the period from April 1 to June 6, 2021, for the demographic distribution of cases. By April 1, 2021, 44·7% of the population in Scotland had received one dose of the COVID-19 vaccine, and 7·6% had received two doses. Among people aged 65 years or older, the percentages were 91·2% and 15·9%, respectively. By the end of the study period (ie, June 6, 2021), 59·4% had received one dose and 39·4% two doses; the corresponding proportions were 91·7% and 88·8%, respectively for those aged 65 years or older. Distributions of first dose vaccine uptakes by age, deprivation, and vaccine type are shown in the appendix (p 1–2).
There were 19 543 confirmed SARS-CoV-2 infections over the period of interest, of whom 377 were admitted to hospital for COVID-19; 7723 (39·5%) of these cases and 134 (35·5%) hospital admissions were in those who were S gene-positive (appendix p 3).
S gene-positive cases occurred in all ages, with a greater proportion of those S gene-positive aged 5–9 years compared to S gene-negative cases (appendix p 2). There was a slight inverse deprivation gradient with S gene-positive cases disproportionally seen in the most socioeconomically affluent quintile. Most cases (70%) had no underlying relevant comorbidities. 70% of S gene-positive cases had not had any COVID-19 vaccination doses, compared to 75% of S gene-negative cases.
The Cox regression analysis for time to hospital admission found that S gene-positive cases were associated with an increased risk of COVID-19 hospital admission: hazard ratio (HR) 1·85 (95% CI 1·39–2·47) when compared to S gene-negative cases, after adjusting for age, sex, deprivation, temporal trend, and comorbidities. A greater number of COVID-19 relevant comorbidities increased the risk of COVID-19 hospital admission (appendix p 3).
Overall, a strong vaccine effect did not clearly manifest until at least 28 days after the first vaccine dose (HR 0·32, 95% CI 0·22–0·46; appendix p 3). Among S gene-negative cases, the effect of vaccination (at least 28 days after first or second dose) was to reduce the risk of hospital admission (HR 0·28, 95% CI 0·18–0·43) compared to unvaccinated. The corresponding hazard ratio for risk of hospital admission for S gene-positive cases was 0·38 (95% CI 0·24–0·58), with an interaction test p value of 0·19, suggesting that there was no evidence of a differential vaccine effect on hospital admissions among those first testing positive (appendix p 4).
Considering the whole population cohort (rather than just hospital cases), the test-negative analysis to estimate vaccine effectiveness in preventing RT-PCR-confirmed SARS-CoV-2 infection showed that, compared to those unvaccinated, at least 14 days after the second dose, BNT162b2 (Pfizer–BioNTech vaccine) offered very good protection: 92% (95% CI 90–93) S gene-negative, 79% (75–82) S gene-positive. Protection associated with ChAdOx1 nCoV-19 (Oxford–AstraZeneca vaccine) was, however, substantial but reduced: 73% (95% CI 66–78) for S gene-negative cases versus 60% (53–66) for those S gene-positive (appendix p 6). These estimates were obtained from a generalised additive logistic model adjusting for age, temporal trend when the swab was taken, and number of previous tests using splines plus sex and deprivation. As there was a trend in vaccine uptake and a trend to increasing Delta variant, the temporal adjustment with a general trend might not fully account for these changes. Also, no formal significance test to compare the vaccines was done. Similar changes in the vaccine effects for at least 14 days post second dose were seen for the Pfizer–BioNTech vaccine when restricting the analysis to those reporting symptoms at the time of test, but with wider confidence intervals associated with the reduced sample size. For the Oxford–AstraZeneca vaccine, the change was greater as the S gene-negative vaccine effect was higher (appendix p 7). These results are consistent with the Delta VOC vaccine effects published by Public Health England.6
In summary, we show that the Delta VOC in Scotland was found mainly in younger, more affluent groups. Risk of COVID-19 hospital admission was approximately doubled in those with the Delta VOC when compared to the Alpha VOC, with risk of admission particularly increased in those with five or more relevant comorbidities. Both the Oxford–AstraZeneca and Pfizer–BioNTech COVID-19 vaccines were effective in reducing the risk of SARS-CoV-2 infection and COVID-19 hospitalisation in people with the Delta VOC, but these effects on infection appeared to be diminished when compared to those with the Alpha VOC. We had insufficient numbers of hospital admissions to compare between vaccines in this respect. The Oxford–AstraZeneca vaccine appeared less effective than the Pfizer–BioNTech vaccine in preventing SARS-CoV-2 infection in those with the Delta VOC. Given the observational nature of these data, estimates of vaccine effectiveness need to be interpreted with caution.
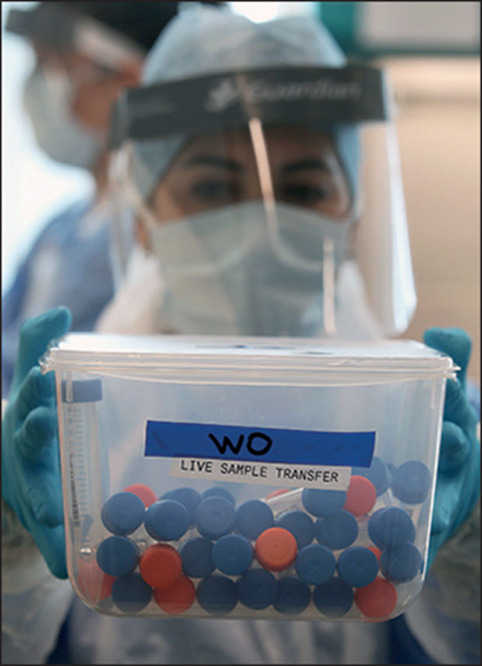
© 2021 Andrew Milligan/Getty Images
AS, JM, and CR are members of the Scottish Government's COVID-19 Advisory Group. AS and CR are members of the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) risk stratification subgroup. JM is a member of NERVTAG. CR is a member of the Scientific Pandemic Influenza Group on Modelling. AS is a member of AstraZeneca's Thrombotic Thrombocytopenic Advisory Group. All roles are unremunerated. JM, BT, and CR are employed by Public Health Scotland. Acknowledgments are listed in the appendix.
Supplementary Material
References
- 1.Simpson CR, Robertson C, Vasileiou E, et al. Early Pandemic Evaluation and Enhanced Surveillance of COVID-19 (EAVE II): protocol for an observational study using linked Scottish national data. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-039097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mulholland RH, Vasileiou E, Simpson CR, et al. Cohort profile: early pandemic evaluation and enhanced surveillance of COVID-19 (EAVE II) database. Int J Epidemiol. 2021 doi: 10.1093/ije/dyab028. published online April 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasileiou E, Simpson CR, Shi T, et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet. 2021;397:1646–1657. doi: 10.1016/S0140-6736(21)00677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simpson CR, Shi T, Vasileiou E, et al. First dose ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic and haemorrhagic events in Scotland. Nat Med. 2021 doi: 10.1038/s41591-021-01408-4. published online June 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373 doi: 10.1136/bmj.n1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernal JL, Andrews N, Gower C, et al. Effectiveness of COVID-19 vaccines against the B.1.617.2 variant. KHub. 2021 doi: 10.1101/2021.05.22.21257658. published online May 24. (preprint). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


