Key Points
Question
Are temporal trends in suicidal ideation and attempts among US adolescents different across sex and race/ethnicity from 1991 through 2019?
Findings
In this cross-sectional study of 183 563 adolescents in the US, a decreasing temporal trend in suicidal ideation changed to an increase, with different turning points for female (2009), White (2009), Hispanic (2007), and Black (2005) adolescents. Male and Black youths had nonsignificant changes in suicidal ideation, but the greatest increase in the prevalence of nonfatal suicide attempts.
Meaning
The results of this study suggest that sex and racial/ethnic disparities in temporal trends in adolescents with suicidal ideation and attempts call for greater diversification in suicide prevention.
Abstract
Importance
Disparities by sex and racial/ethnic group in suicide death rates are present in US adolescents. Whether disparities in suicide death extend to groups targeted for suicide prevention efforts, namely, those with suicidal ideation or nonfatal suicide attempts, is unknown.
Objective
To examine differences in temporal trends between suicidal ideation and suicide attempts in US adolescents from 1991 through 2019 by sex and race/ethnicity subgroups.
Design, Setting, and Participants
A cross-sectional analysis of the national Youth Risk Behavior Survey, weighted to represent US adolescents from 1991 to 2019, included 183 563 US high-school students in grades 9 to 12. Data were analyzed from September 16, 2020, through April 12, 2021.
Exposures
Calendar year, sex, race/ethnicity, and interactions of sex and race/ethnicity.
Main Outcomes and Measures
Survey-weighted prevalence estimates, annual percentage changes (APCs) and average APC in the survey-weighted prevalence of suicidal ideation and nonfatal suicide attempts, constructed from self-reported suicidal ideation, plan, and attempts in each survey year, by sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian or Pacific Islander and Native Hawaiian, American Indian/Alaska Native), and their interactions (sex × race/ethnicity).
Results
In 183 563 (unweighted) included adolescents (mean [SD] age, 16.07 [1.23] years; 94 282 females [weighted percentage, 49.4%; 95% CI, 48.8%-50.1%]), the prevalence of suicidal ideation decreased from 1991 to 2019 (from 19.4% to 15.8%; 95% CI, 0.7%-0.9%), whereas the prevalence of nonfatal suicide attempts increased from 1991 to 2019 (from 7.3% to 8.9%; 95% CI, 1.0%-1.4%). Joinpoint regression indicated a −3.1% (95% CI, −3.7% to −2.6%) annual decrease in suicidal ideation between 1991 and 2009, followed by a 3.4% annual increase (95% CI, 1.9% -4.8%) between 2009 and 2019. Decreasing followed by increasing trends in suicidal ideation showed modestly different turning points in female (1991-2009, 2009-2019), White (1991-2009, 2009-2019), Hispanic (1991-2007, 2007-2019), and Black (1991-2005, 2005-2019) adolescents. Although no significant trends were observed in suicide attempts from 1991 through 2019, male (68.4% increase; 95% CI, 0.2% -1.2%) and Black (79.7% increase; 95% CI, 0.1%-1.5%) adolescents had greater increases in the prevalence of suicide attempts. Interaction of sex and race/ethnicity revealed increases in suicidal ideation in White females from 2009 to 2019 (APC, 4.3%; 95% CI, 1.5%-7.1%), Black females from 2005 to 2019 (APC, 3.4%; 95% CI, 1.4%-5.4%), and Hispanic females from 2009 to 2019 (APC, 3.3%; 95% CI, 1.0%-5.6%) and suicide attempts in White females from 2009 to 2019 (APC, 3.1%; 95% CI, 0.3%-6.0%).
Conclusions and Relevance
The findings of this study show apparent sex and racial/ethnic differences in trends in suicidal ideation and suicide attempts. Increases in suicidal ideation since 2009 were observed in female individuals; changes in male and Black adolescents represented the largest increase in the prevalence of suicide attempts between 1991 and 2019. Evidence-based suicide prevention programs need to be tailored by sex and race/ethnicity, calling for greater diversification of health care system, school, and community prevention approaches.
This cross-sectional study analyses temporal trends to assess changes in suicidal ideation and nonfatal suicide attempts among US adolescents from 1991 through 2019.
Introduction
Suicide is the second leading cause of death in youths aged 12 to 18 years in the US.1 In 2019, 2090 (7.1 per 100 000) adolescents in this age group died by suicide.2 Visits to hospital emergency departments due to suicidal ideation or attempts in youths aged 15 to 19 years are increasing,3 with the largest increase observed in Black, Hispanic, and female adolescents between 2008 and 2015.4,5 Monitoring the temporal trends of suicidal behaviors is important to guide development of effective suicide prevention.6,7,8,9 In particular, detecting changes in temporal trends in subgroups and when the risk of suicide is greater in those groups can identify high-risk populations for targeted intervention and guide hypothesis generation and testing.10
Previous studies have reported increasing rates of suicide death,11,12 nonfatal suicidal ideation, plan attempts, and injury due to attempts.12,13,14,15,16 However, most work to date did not separate youths who attempted suicide from those who had suicidal ideation but no attempts.17 This step is needed, because theoretical and empirical evidence suggests that the risk factors associated with suicidal ideation and suicide attempts are likely to differ.18,19 From a public health perspective, knowing whether and how the trends differ between suicidal ideation and attempts is an important component of surveillance.7 Increasing trends in specific suicidal behaviors across demographic groups may signal emerging risk factors or high-risk groups that warrant targeted suicide prevention.20
There are increasing data on sex, racial/ethnic, and intersectionality disparities in suicidal behaviors.12,13,21,22,23 Black adolescents have been reported to be the only racial/ethnic group to show increasing suicide attempts between 1991 and 2017.17 Another study found a narrowing sex gap in youth suicide death between 1975 and 2016.12 Although informative, the existing literature lacks information about any turning points of the trends in suicidal ideation and nonfatal suicide attempts and possible sex and racial/ethnic disparities. Identifying turning points can help in understanding the possible influence of structural inequalities and socioeconomic and political changes on sex- and race/ethnicity-specific suicide trends24 (eFigure 1 in the Supplement).
To our knowledge, the present study provides the first nationally representative analysis of temporal trends to examine changes in suicidal ideation and nonfatal suicide attempts among US adolescents from 1991 through 2019. A secondary objective was to identify the demographic subgroups of adolescents whose trends in terms of suicidal ideation and nonfatal suicide attempts indicate a need to be prioritized for interventions.
Methods
Data and Participants
Since 1991, the national Youth Risk Behavior Survey (YRBS) has been conducted biannually. Each cross-sectional survey cycle uses a 3-stage cluster sampling design to produce a nationally representative sample of high school students in grades 9 to 12 among public and private schools in the 50 states and the District of Columbia. Written informed consent was obtained from the parent or legal guardian of adolescents. Students completed the self-administered, computer-scannable questionnaire anonymously and voluntarily. No compensation was provided. The Centers for Disease Control and Prevention Institutional Review Board approved each independent protocol of the national YRBS.25 This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.
This study pooled data from the 1991-2019 YRBS, across which unweighted sample sizes ranged from 10 904 to 16 410. Data were analyzed from September 16, 2020, through April 12, 2021. School response rates ranged from 75% to 81%; student response rates ranged from 81% to 90%, and overall response rates for the surveys ranged from 60% to 71%. More details regarding sampling strategies and reliabilities of the YRBS survey items are reported elsewhere.26 The analytic sample included 183 563 participants who answered the questions reporting past-year suicide ideation, plan, and/or attempt. Adolescents who had missing information in all 3 suicidal behavior questions were excluded.
Measures
The YRBS assessed 3 self-reported questions related to suicidal behaviors: (1) suicide ideation (During the past 12 months, did you ever seriously consider attempting suicide?), (2) suicide plan (During the past 12 months, did you make a plan about how you would attempt suicide?), and (3) suicide attempts (During the past 12 months, how many times did you actually attempt suicide?). Response options were dichotomized into yes or no. These questions demonstrated substantial reliability in earlier studies.27,28,29
All respondents who reported suicidal ideation or suicide plan but denied suicide attempts were coded as suicidal ideation (n = 24 435). Respondents who reported 1 or more suicide attempts, regardless of their answers to ideation or plan, were coded as suicide attempts (n = 16 497). We focused on nonfatal suicidal behaviors in this study. The suicidal ideation and suicide attempts groups are not mutually exclusive.
The YRBS asks 2 self-report questions about race and Hispanic heritage. Consistent with previous research,30 the 6 categories for race/ethnicity were non-Hispanic White; non-Hispanic Black; non-Hispanic Asian or Pacific Islander and Native Hawaiian (API); Hispanic; American Indian/Alaska Native (AI/AN), and non-Hispanic multiple races. Sex groups were self-reported biological sex. Student grade levels were included as controlled variables. Intersectional terms of sex and race/ethnicity were constructed. Prevalence of suicidal ideation and suicide attempts were calculated for the total sample and by sex, race/ethnicity, and sex × race/ethnicity subgroups, adjusting for survey weights and complex sample design.
Statistical Analysis
Weighted prevalence of suicidal ideation and suicide attempts among the total sample and separately by sex and race/ethnicity from 1991 through 2019 was calculated using Stata, version 16 (StataCorp LLC). To present the magnitude of the changes, the percent differences in the prevalence of suicidal ideation and suicide attempts were calculated using the formula [(rate in 2019 − rate in 1991)/rate in 1991] × 100. Changes in prevalence show the magnitude of changes in the population. Joinpoint, version 4.9.0.0 (National Cancer Institute), was used to estimate piecewise log-linear trends in the survey-weighted prevalence estimates of suicidal ideation and suicide attempts over time. After fitting the regression to the natural logarithm of prevalence using calendar year as a regressor, turning points of change in trends (joinpoints) were identified by a series of Monte Carlo permutation-based tests and model selection.31 Annual percentage change (APC) with 95% CI for each identified trend was estimated. Average APC, a single summary measure, was used to describe the average rate of change over the entire 1991 to 2019 study period. The APC and average APC help identify the time at which the trend in suicidal ideation and attempts changed significantly compared with the trend in previous years. Significant slopes (95% CIs not crossing 0; P < .05) indicated increasing and decreasing trends, whereas nonsignificant APC slopes (95% CIs crossing 0; P > .05) indicated that the prevalence was stable.
Trends were stratified by sex, race/ethnicity, and intersectional terms. Disparities in slopes of suicidal subgroups across sex, race/ethnicity, and intersectionality were tested using parallel pairwise comparisons that detected differences in APCs between 2 models.32 All analyses adjusted for the complex sampling design and survey weight to obtain the US nationally representative estimates, accounting for nonresponse and oversampling of Black and Hispanic students. Trends are presented as a straight line fitted over the full period based on a simple log-linear model if no statistically significant change in trends emerged. If a significant change in the slope of the trend was noted, linear segments connected between 2 years (ie, joinpoints) are presented. Statistical significance was determined by a 2-sided P value <.05 with Wald χ2 tests using design-adjusted coefficient variance-covariance matrices.
Results
Overall Trends and Turning Points
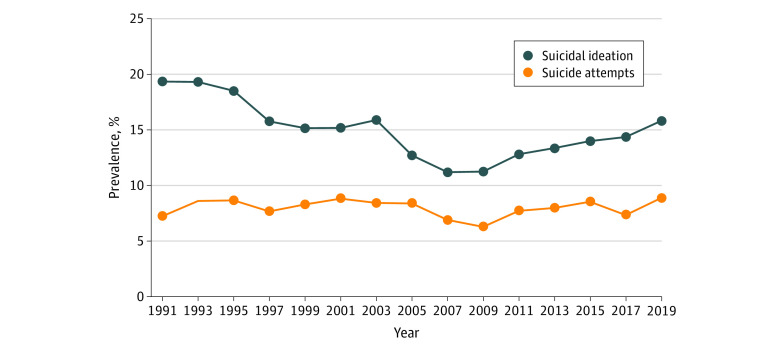
Of 183 563 adolescents (mean [SD] age, 16.07 [1.23] years), 94 282 (unweighted; weighted percentage, 49.4% [95% CI, 48.8%-50.1%]) were female, 89 281 (unweighted; weighted percentage, 50.5% [95% CI, 49.9%-51.2%]) were male, 81 838 (unweighted; weighted percentage, 64.0% [95% CI, 62.3%-65.6%]) were non-Hispanic White adolescents, 37 009 (unweighted; weighted percentage, 12.5% [95% CI, 11.6%-13.4%]) were non-Hispanic Black adolescents, 49 554 (unweighted; weighted percentage, 15.5% [95% CI, 14.4%-16.6%]) were Hispanic adolescents, 7875 (unweighted; weighted percentage, 4.0% [95% CI, 3.5%-4.5%]) were non-Hispanic API adolescents, 1997 (unweighted; weighted percentage, 0.7% [95% CI, 0.6%-0.9%]) were non-Hispanic AI/AN adolescents, and 5290 (unweighted; weighted percentage, 3.3% [95% CI, 3.0%-3.7%]) were non-Hispanic multiple races or other race. In the total sample (Figure 1), the prevalence of suicidal ideation without attempts decreased by 18.2% from 1991 to 2019 (from 19.4% to 15.8%; 95% CI, 0.7%-0.9%). The prevalence of nonfatal suicide attempts increased by 22.5% from 1991 to 2009 (from 7.3% to 8.9%; 95% CI, 1.0%-1.4%).
Figure 1. Prevalence of Suicidal Ideation and Suicide Attempts Among US Adolescents, 1991-2019.
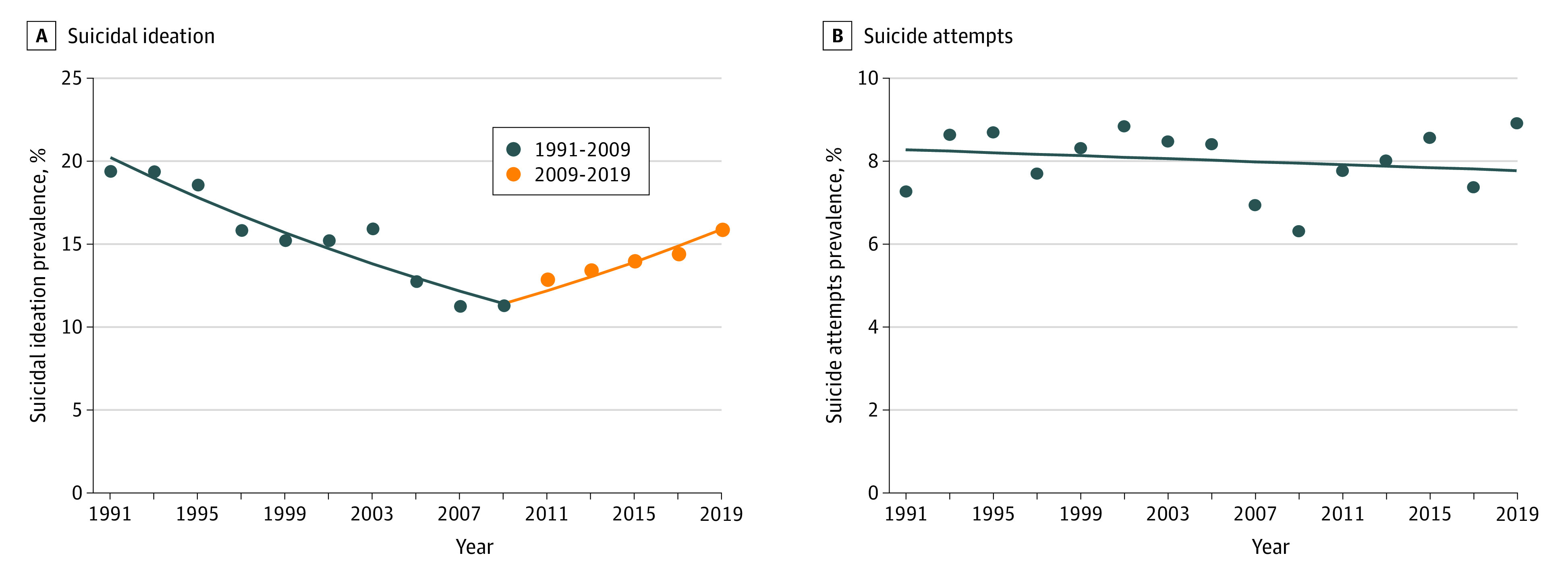
Joinpoint regression identified a decreasing trend in suicidal ideation from 1991 to 2019 among the total sample (average APC, −0.9%; 95% CI, −1.4% to −0.3%), with 2009 the turning point of a decreasing-increasing trend observed in suicidal ideation (Table, Figure 2). In the total sample, the prevalence of suicidal ideation decreased from 1991 to 2009 (APC, −3.1%; 95% CI, −3.7% to −2.6%), followed by an increase from 2009 to 2019 (APC, 3.4%; 95% CI, 1.9%-4.8%). Trends in nonfatal suicide attempts in the total sample were not significant and no turning points were observed (APC, −0.2%; 95% CI, −0.9% to 0.5%) (Table, Figure 2).
Table. Annual Percentage Changes in Suicidal Ideation and Suicide Attempts Among US Adolescents, 1991-2019a.
| Demographic characteristic | Average APC, % (95% CI) | Segment 1 | APC, % (95% CI) | Segment 2 | APC, % (95% CI) | Segment 3 | APC, % (95% CI) |
|---|---|---|---|---|---|---|---|
| Total | |||||||
| Suicidal ideation | −0.9 (−1.4 to −0.3) | 1991-2009 | −3.1 (−3.7 to −2.6) | 2009-2019 | 3.4 (1.9 to 4.8) | NA | NA |
| Suicide attempts | −0.2 (−0.9 to 0.5) | 1991-2019 | −0.2 (−0.9 to 0.5) | NA | NA | NA | NA |
| Sex | |||||||
| Suicidal ideation | |||||||
| Female | −0.7 (−1.3 to −0.1) | 1991-2009 | −3.2 (−3.8 to −2.7) | 2009-2019 | 4.0 (2.5 to 5.6) | NA | NA |
| Male | −1.3 (−2.6 to 0.0) | 1991-2007 | −3.3 (−4.9 to −1.6) | 2007-2019 | 1.4 (−1.2 to 4.0) | NA | NA |
| Suicide attempts | |||||||
| Female | −0.6 (−1.3 to 0.1) | 1991-2019 | −0.6 (−1.3 to 0.1) | NA | NA | NA | NA |
| Male | 0.6 (−0.2 to 1.5) | 1991-2019 | 0.6 (−0.2 to 1.5) | NA | NA | NA | NA |
| Race/ethnicity | |||||||
| Suicidal ideation | |||||||
| White | −1.0 (−1.8 to −0.2) | 1991-2009 | −3.4 (−4.2 to −2.7) | 2009-2019 | 3.6 (1.3 to 5.9) | NA | NA |
| Black | −0.1 (−1.4 to 1.2) | 1991-2005 | −3.3 (−5.2 to −1.3) | 2005-2019 | 3.1 (1.0 to 5.4) | NA | NA |
| Hispanic | −0.7 (−1.7 to 0.3) | 1991-2007 | −2.6 (−4.1 to −1.2) | 2007-2019 | 1.9 (0.2 to 3.6) | NA | NA |
| API | −1.1 (−1.9 to −0.2) | 1991-2019 | −1.1 (−1.9 to −0.2) | NA | NA | NA | NA |
| AI/AN | 1.2 (−0.5 to 2.9) | 1991-2019 | 1.2 (−0.5 to 2.9) | NA | NA | NA | NA |
| Suicide attempts | |||||||
| White | −0.5 (−1.4 to 0.4) | 1991-2019 | −0.5 (−1.4 to 0.4) | NA | NA | NA | NA |
| Black | 0.6 (−0.1 to 1.4) | 1991-2019 | 0.6 (−0.1 to 1.4) | NA | NA | NA | NA |
| Hispanic | −1.1 (−2.1 to −0.1) | 1991-2019 | −1.1 (−2.1 to −0.1) | NA | NA | NA | NA |
| API | −1.1 (−2.7 to 0.5) | 1991-2019 | −1.1 (−2.7 to 0.5) | NA | NA | NA | NA |
| AI/AN | −1.4 (−3.4 to 0.7) | 1991-2019 | −1.4 (−3.4 to 0.7) | NA | NA | NA | NA |
| Sex × race/ethnicity | |||||||
| Suicidal ideation | |||||||
| Female | |||||||
| White | −0.9 (−1.9 to 0.1) | 1991-2009 | −3.6 (−4.5 to −2.8) | 2009-2019 | 4.3 (1.5 to 7.1) | NA | NA |
| Black | 0.1 (−1.1 to 1.3) | 1991-2005 | −3.1 (−4.9 to −1.2) | 2005-2019 | 3.4 (1.4 to 5.4) | NA | NA |
| Hispanic | −0.2 (−1.1 to 0.7) | 1991-2009 | −2.1 (−3.1 to −1.1) | 2009-2019 | 3.3 (1.0 to 5.6) | NA | NA |
| API | −1.5 (−2.7 to −0.2) | 1991-2019 | −1.5 (−2.7 to −0.2) | NA | NA | NA | NA |
| AI/AN | 2.4 (−0.6 to 5.6) | 1991-2019 | 2.4 (−0.6 to 5.6) | NA | NA | NA | NA |
| Male | |||||||
| White | −1.5 (−2.5 to −0.4) | 1991-2007 | −3.5 (−4.7 to −2.2) | 2007-2019 | 1.3 (−0.9 to 3.5) | NA | NA |
| Black | −0.5 (−2.2 to 1.3) | 1991-2019 | −0.5 (−2.2 to 1.3) | NA | NA | NA | NA |
| Hispanic | −1.0 (−1.9 to 0.0) | 1991-2019 | −0.5 (−2.2 to 1.3) | NA | NA | NA | NA |
| API | −0.2 (−1.6 to 1.1) | 1991-2019 | −1.0 (−1.9 to 0.0) | NA | NA | NA | NA |
| AI/AN | 0.1 (−2.2 to 2.5) | 1991-2019 | −0.2 (−1.6 to 1.1) | NA | NA | NA | NA |
| Suicide attempts | |||||||
| Female | |||||||
| White | −0.4 (−2.8 to 1.9) | 1991-2003 | −0.5 (−2.5 to 1.5) | 2003-2009 | −6 (−16.4 to 5.8) | 2009-2019 | 3.1 (0.3 to 6.0) |
| Black | 0.5 (−0.4 to 1.4) | 1991-2019 | 0.5 (−0.4 to 1.4) | NA | NA | NA | NA |
| Hispanic | −1.5 (−2.5 to −0.5) | 1991-2019 | −1.5 (−2.5 to −0.5) | NA | NA | NA | NA |
| API | −1.4 (−3.2 to 0.5) | 1991-2019 | −1.4 (−3.2 to 0.5) | NA | NA | NA | NA |
| AI/AN | −0.2 (−2.9 to 2.6) | 1991-2019 | −0.2 (−2.9 to 2.6) | NA | NA | NA | NA |
| Male | |||||||
| White | 0.9 (−0.3 to 2.2) | 1991-2019 | 0.9 (−0.3 to 2.2) | NA | NA | NA | NA |
| Black | 0.7 (−0.5 to 2.0) | 1991-2019 | 0.7 (−0.5 to 2.0) | NA | NA | NA | NA |
| Hispanic | 1.6 (−0.9 to 4.2) | 1991-1995 | 0.7 (−0.5 to 2.0) | 1995-2019 | −0.8 (−2.1 to 0.5) | NA | NA |
| API | −1.2 (−3.3 to 1.0) | 1991-2019 | 17.7 (−2.0 to 41.4) | NA | NA | NA | NA |
| AI/AN | −0.6 (−4.4 to 3.5) | 1991-2019 | −1.2 (−3.3 to 1.0) | NA | NA | NA | NA |
Abbreviations: AI/AN, non-Hispanic American Indian/Alaska Native; APC, annual percentage change; API, non-Hispanic Asian or Pacific Islander and Native Hawaiian; NA, not applicable.
Segments were chosen by joinpoint regression.
Figure 2. Trends in Suicidal Ideation and Suicide Attempts Among the Total Sample, 1991-2019.
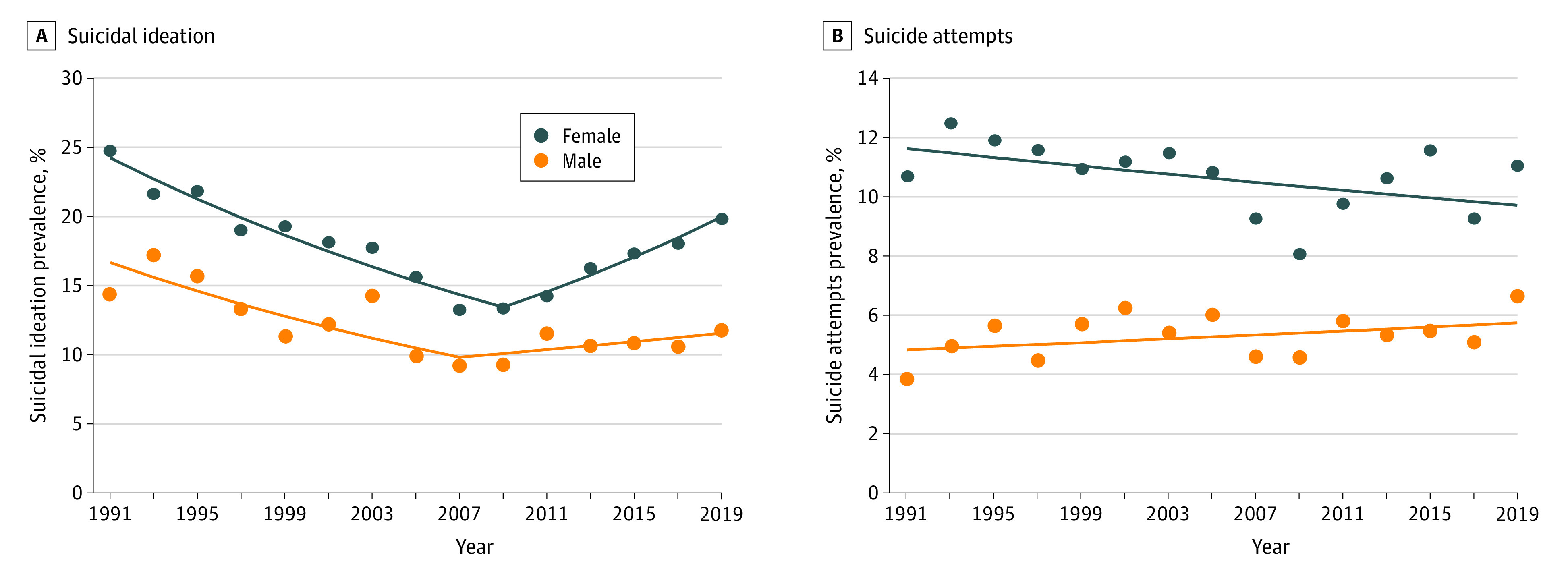
Differences by Sex
The prevalence of suicidal ideation in females and males decreased comparably between 1991 and 2019 (18.5% for females, 21.8% for males) (eFigure 2 in the Supplement). Joinpoint regression (Table) estimated that suicidal ideation in females decreased from 1991 to 2009 (APC, −3.2%; 95% CI, −3.8% to −2.7%) and increased from 2009 to 2019 (APC, 4.0%; 95% CI, 2.5%-5.6%). Suicidal ideation in males decreased from 1991 to 2007 (APC, −3.3%; 95% CI, −4.9% to −1.6%) and remained stable thereafter (APC, 1.4%; 95% CI, −1.2% to 4.0%) (Figure 3). APCs of suicidal ideation in males and females were parallel, but there were statistically significant differences in APCs in nonfatal suicide attempts by sex (eFigure 2 in the Supplement). Between 1991 and 2019, the APC in female adolescents was −0.6% (95% CI, −1.3% to 0.1%) and, in male adolescents, 0.6% (95% CI, −0.2% to 1.5%). The increasing prevalence of nonfatal suicide attempts was largely attributable to male adolescents (68.4%; 95% CI, 0.2%-1.2%), with the rate 20 times greater compared with females (3.4%; 95% CI, −0.1% to 0.2%) between 1991 and 2019 (eFigure 2 in the Supplement).
Figure 3. Trends in Suicidal Ideation and Suicide Attempts by Sex, 1991-2019.
Differences by Race/Ethnicity
Suicidal ideation in Black (9.5%) and AI/AN (98.1%) adolescents has increased from 1991 through 2019 compared with a decreasing prevalence in other races/ethnicities (White, −23.8%; Hispanic, −1.2%; API, −23.1%) (eFigure 3 in the Supplement). Suicidal ideation in White, Black, and Hispanic adolescents showed decreasing and increasing trends over the study period but with different turning points: 2009 for White adolescents (from APC, −3.4%; 95% CI, −4.2% to −2.7% to APC, 3.6%; 95% CI, 1.3%-5.9%), 2005 for Black adolescents (from APC, −3.3%; 95% CI, −5.2% to −1.3% to APC, 3.1%; 95% CI, 1.0%-5.4%), and 2007 for Hispanic adolescents (from APC, −2.6%; 95% CI, −4.1% to −1.2% to APC, 1.9%; 95% CI, 0.2%-3.6%). Suicidal ideation in API adolescents decreased from 1991 to 2019 (APC, −1.1%; 95% CI, −1.9% to −0.2%). There were statistically significant differences in APCs in suicidal ideation across racial/ethnic groups (eFigure 2 in the Supplement; Table, Figure 4).
Figure 4. Trends in Suicidal Ideation and Suicide Attempts by Race/Ethnicity, 1991-2019.
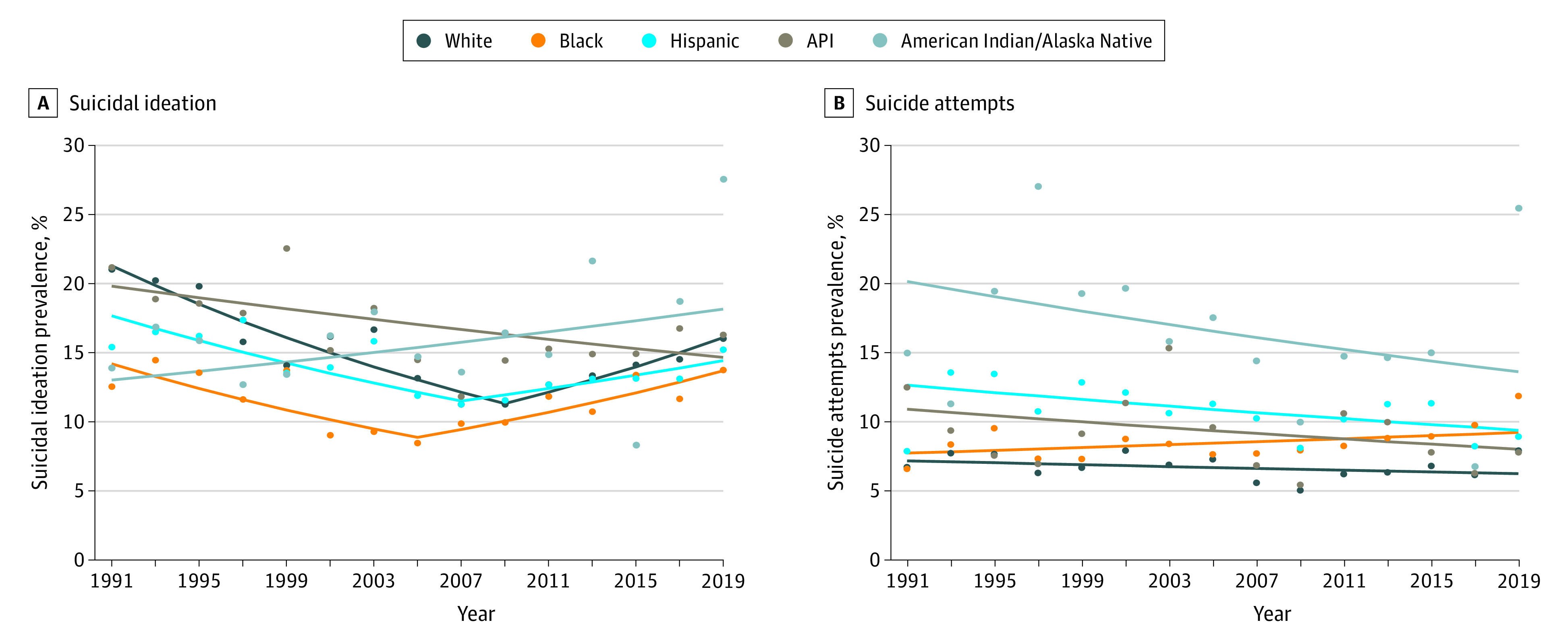
API indicates non-Hispanic Asian or Pacific Islander and Native Hawaiian.
Black adolescents had the highest increase in the prevalence of suicide attempts between 1991 and 2019 (79.7%; 95% CI, 0.1%-1.5%) compared with all other races/ethnicities (White, 17.8%; Hispanic, 13.4%; API, −37.6%; AI/AN, 70.0%). Joinpoint regression estimated a downward trend in suicide attempts in Hispanic adolescents from 1991 to 2019 (APC, −1.1%; 95% CI, −2.1% to −0.1%). No changes were detected in other racial/ethnic groups, despite the only positive APC (0.6%; 95% CI, −0.1% to 1.4%) observed in Black adolescents (White: APC, −0.5%; 95% CI, −1.4% to 0.4%; API: APC, −1.1%; 95% CI, −2.7% to 0.5%; AI/IN: APC, −1.4%; 95% CI, −3.4% to 0.7%) (Table, Figure 4). Parallel comparisons in trends in suicide attempts indicated different APCs between White and Black adolescents and Black and Hispanic adolescents.
Differences by Sex and Race/Ethnicity
Stratifying by both sex and race/ethnicity revealed further subgroup differences. During 1991-2019, Black (13.4%) and AI/AN (32.6%) females showed an increasing prevalence of suicidal ideation and other female subgroups had decreasing rates. In addition, AI/AN (204.0%) and Black (20.8%) males had higher increasing rates in nonfatal suicide attempts compared with other male racial/ethnic groups (eFigure 4 in the Supplement). Suicidal ideation in White females decreased during 1991-2009 (APC, −3.6%; 95% CI, −4.5% to −2.8%) and increased during 2009-2019 (APC, 4.3%; 95% CI, 1.5%-7.1%). Similar decreasing and increasing trends were observed in suicidal ideation in Black and Hispanic females with different turning points. Suicidal ideation in API females (APC, −1.5%; 95% CI, −2.7% to −0.2%) decreased over the entire study period (Table; eFigure 5 in the Supplement).
Black males had the highest increase in suicide attempts (162.4%) compared with all other sex and racial/ethnic subgroups (White females, −9.3%; Black females, 62.1%; Hispanic females, 3.0%; API females, −43.2%; AI/AN females, 65.2%; White males, 92.7%; Hispanic males, 50.3%; API males, 30.0%; AI/AN males, 86.7%) from 1991 to 2019. In the past decade (2009 to 2019), suicide attempts increased by 3.1% annually (95% CI, 0.3%-6.0%) among White females, whereas there was a consistent decrease in suicide attempts among Hispanic females from 1991 to 2019 (APC, −1.5%; 95% CI, −2.5% to −0.5%). The prevalence of suicide attempts remained stable among other sex and racial/ethnic subgroups.
Discussion
To our knowledge, this is the first study to examine and compare the temporal trends in suicidal ideation and nonfatal suicide attempts across sex and race/ethnicity during 1991-2019 using a nationally representative sample of US adolescents. The core finding is the sex and race/ethnic disparities in the 22.5% increase in the prevalence of US adolescent suicide attempts from 1991 to 2019, and the 18.2% decrease in prevalence of suicidal ideation over the same period. We detected the largest percentage increase in suicide attempts in male and Black adolescents. Trends in suicidal ideation among females, particularly among non-Hispanic Black, non-Hispanic White, and Hispanic females, showed a V-shape (decreasing-increasing) change across the entire study period (1991-2019), with different turning points (2005 in non-Hispanic Black, 2007 in non-Hispanic White, 2009 in Hispanic females). Trends in suicide attempts were stable, except for a significant increasing trend among non-Hispanic White female adolescents from 2009 to 2019. Our findings highlight emerging sex and racial/ethnic disparity in the epidemiologic factors associated with US adolescent suicide.
Our finding of the substantial increase in suicide attempts parallels the increase in emergency department visits for nonfatal self-inflicted injuries among youths and young adults.4,5,33,34 We detected a larger increase in male adolescents attempting suicide than in their female counterparts from 1991 through 2019, which is consistent with previous studies on suicide death rates among male children and youths aged 5 to 18 years between 1991 and 2017.14,23,35 Possible male-specific risk factors include greater access to firearms at home,36 less predisposition to seek help,37 and a greater tendency to adopt avoidance strategies to cope with emotional problems.38 Other studies, however, have revealed greater increases in emergency department visits for suicide attempts among females than males between 2001-2015,4 2008-2015,33 and 2011-2015.5 Owing to the self-reported nature of the suicide attempt questions in our data, we cannot rule out the possibility of male youths becoming more willing to self-disclose in more recent cohorts. More research is warranted to examine emerging risk factors for these groups.
Of public health concern, suicide attempts among Black adolescents have increased rapidly, accelerating by 79.7% from 1991 to 2019. This finding is consistent with prior research on increasing self-reported suicidal behaviors between 1991 and 2018,17 emergency department visits for suicide attempts,39 and suicide deaths between 1993-2012,40 2001-2015,23 and 1999-2015.15 Our results expand on previous reports of a disproportionate increase in suicide attempts among Black adolescents relative to other racial/ethnic groups with more updated data, investigation of turning points, and comparisons with trends in suicidal ideation.
Although few studies have examined the mechanisms underlying suicide attempts in Black adolescents,41 existing findings suggest structural inequalities and social determinants of health factors as plausible explanations.41,42,43 Black adolescents were more likely to experience long-standing socioeconomic inequalities (eg, poverty, racial segregation), living in families with financial hardships, and reporting other behavioral challenges.15,44,45,46,47 Such experiences could disproportionately precipitate greater disparities in untreated mental illness, levels of hopelessness, and risks of suicidal behaviors among Black youths.35 Notably, Black adolescents had higher adverse childhood experience (eg, abuse, neglect) exposures than their White and Hispanic counterparts,48 and adverse childhood experiences had a strong and dose-responsive association with attempted suicide among adolescents.49 Black adolescents also experienced greater online race-related traumatic events that may increase their risks of attempting suicide.50,51 More research on the race-specific risk and protective factors for suicide attempts among Black youths is needed.
The higher prevalence of suicidal ideation and suicide attempts in female compared with male adolescents indicates the need for the sex gaps to be addressed. Specifically, even with the observed decrease, prevalence rates in suicidal ideation and suicide attempts among female adolescents remained high in 2019 (Figure 3). Narrowing sex gaps were consistently observed in emergency department visits for suicidal ideation or nonfatal suicide attempts,4,5,13,33 suicide death,12,52 and self-reported suicidal ideation,21,22,53 with female adolescents aged 10 years or older more represented than males. The female-specific upward trends mirrored the trajectories of depression, with increasing depressive symptoms observed only among females since 2005.22,37,54 The post-2009 increasing trend in suicidal ideation among White female youths paralleled an increasing trend in mental health service use for suicidal ideation or suicide attempts among White female youths aged 12 to 17 years from 2009 to 2018.55
Adolescents in recent decades are experiencing rapid change in technology with behavioral consequences (eg, disrupted sleep, increased obesity) and evolving cultural norms associated with mental health discourse (eg, more suicide-related lyrics in popular rap music).21,22,53,56 Increasing suicidal ideation among female youths after 2007 calls for the need for suicide interventions addressing female-specific risks, particularly given their greater vulnerability to school bullying, cyberbullying, and peer victimization than male adolescents.11,57,58,59 Our results lend support to previous studies35,60 suggesting the need to consider both individual stress-diathesis risks and societal-contextual factors at large.
Previous suicide prevention efforts may contribute to short-term decreases in suicide attempts but are inefficient to prevent the upward trends that started in 2007 (eFigure 1 in the Supplement),61,62 especially among male and Black adolescents.14 Our study suggests that more funding support and policy advocacy are warranted to develop more comprehensive and culturally appropriate suicide prevention programs targeting different risks of ideation and attempts across sex and racial/ethnic groups. Future suicide risk assessments should avoid generalized solutions.63 Growing risks, such as adverse childhood experiences, systematic racism, discrimination, neighborhood violence, and socioeconomic disparities, need to be included in youth suicide prevention programs in general and for males and Black youths in particular.12,23,40,41 Barriers associated with access and adherence to mental health treatment at structural (eg, transportation, costs, availability of school-based mental health services), social (eg, stigma), and interpersonal (eg, implicit and explicit bias among clinicians toward racial minorities) levels should be addressed through interventions targeting access to mental health care and social determinants of health.42 Prevention approaches, including health promotion campaigns to increase the awareness of suicidal ideation, the intention to seek help from mental health professionals, coping skills, and the policies that strengthen financial stability, may improve suicide literacy and prevent youth suicide.64 Relative contributions of suicide prevention strategies (eg, risk assessment, public awareness, postvention), policies (eg, addressing the opioid crisis, bullying), and macrolevel societal factors (eg, economic context, structural racism) deserve attention.24,65
Strengths and Limitations
A strength of this study is our use of large, nationally representative, most recent YRBS data across 1991-2019, which offers a unique opportunity to examine distinct trends in suicidal ideation and suicide attempts across sex and race/ethnicity among US adolescents. This study has limitations. First, the cross-sectional nature of YRBS limits the determination of causality in the trends. Second, YRBS only surveyed students who attend schools; thus, the data are not representative of all adolescents in the age group. Third, the measurement of suicidal behaviors and demographic characteristics are self-reported. Despite the good test-retest reliability66 and wide use in previous studies,60 there is a potential for self-reporting bias (eg, reluctance to disclose ideation and attempt history). The questions cannot capture short-term changes in suicidal thoughts and behaviors (eg, less than weekly). Future research that uses validated assessment instruments (eg, Columbia–Suicide Severity Rating Scale)67 or ecological momentary assessment technology that delivers questions on smartphones will increase understanding of more-imminent risks associated with suicide attempts among adolescents. Suicide deaths and underreporting of nonfatal suicide attempts may influence the results. Fourth, given the possible age-related racial/ethnic disparities observed in previous literature,23 further investigation on whether the trends in suicidal ideation and suicide attempts varied by grade levels is warranted to guide more targeted interventions for younger and older adolescents.
Conclusions
The findings of this study suggest that addressing suicide disparities is a priority in research, clinical practice, and policy. We found large increases in the prevalence of suicide attempts in male and Black adolescents from 1991 through 2019. Female adolescents, particularly among White, Black, and Hispanic groups, experienced increasing suicidal ideation since 2009, but not nonfatal suicide attempts. From a policy perspective, our results highlight the need to implement evidence-based, structural, and suicide prevention programs involving collaboration between health systems and communities. Males, particularly Black male adolescents, appear to have the greatest need in terms of prevention of suicidal behaviors. Both groups have underperformed in help-seeking capacity and there may be stigma and racial barriers to getting psychiatric treatment for young Black males. Strategies that prioritize monitoring the trends in risk factors for suicidal behaviors in racial/ethnic subgroups, design culturally appropriate prevention programs, alleviate structural inequality, reduce mental health stigma and barriers to health care, and promote help-seeking should be ethnically and sexually diversified for effective suicide prevention.
eFigure 1. Turning Points in Temporal Trends in Suicidal Subgroups and Possible Associated Policy and Societal Factors, 1991-2019
eFigure 2. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex, 1991-2019
eFigure 3. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Race/ethnicity, 1991-2019
eFigure 4. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex and Race/ethnicity, 1991-2019
eFigure 5. Trends in Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex and Race/ethnicity, 1991-2019
References
- 1.Centers for Disease Control and Prevention . Injury Prevention & Control. Fatal injury and violence data. 2021. Accessed April 9, 2021. https://www.cdc.gov/injury/wisqars/fatal.html
- 2.Centers for Disease Control and Prevention . CDC WONDER. About multiple cause of death, 1999-2019. Accessed October 6, 2020. https://wonder.cdc.gov/mcd-icd10.html
- 3.Ting SA, Sullivan AF, Boudreaux ED, Miller I, Camargo CA Jr. Trends in US emergency department visits for attempted suicide and self-inflicted injury, 1993-2008. Gen Hosp Psychiatry. 2012;34(5):557-565. doi: 10.1016/j.genhosppsych.2012.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mercado MC, Holland K, Leemis RW, Stone DM, Wang J. Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10 to 24 years in the United States, 2001-2015. JAMA. 2017;318(19):1931-1933. doi: 10.1001/jama.2017.13317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4):e20182192. doi: 10.1542/peds.2018-2192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mann JJ, Rizk MM. A brain-centric model of suicidal behavior. Am J Psychiatry. 2020;177(10):902-916. doi: 10.1176/appi.ajp.2020.20081224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064-2074. doi: 10.1001/jama.294.16.2064 [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293(20):2487-2495. doi: 10.1001/jama.293.20.2487 [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. Office of the Surgeon General and National Action Alliance for Suicide Prevention . 2012 National strategy for suicide prevention: goals and objectives for action. 2012. Accessed December 12, 2020. https://www.ncbi.nlm.nih.gov/books/NBK109917/ [PubMed]
- 10.Xiao Y, Lindsey MA. Racial/ethnic, sex, sexual orientation, and socioeconomic disparities in suicidal trajectories and mental health treatment among adolescents transitioning to young adulthood in the USA: a population-based cohort study. Adm Policy Ment Health. 2021;1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luby J, Kertz S. Increasing suicide rates in early adolescent girls in the United States and the equalization of sex disparity in suicide: the need to investigate the role of social media. JAMA Netw Open. 2019;2(5):e193916-e193916. doi: 10.1001/jamanetworkopen.2019.3916 [DOI] [PubMed] [Google Scholar]
- 12.Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open. 2019;2(5):e193886-e193886. doi: 10.1001/jamanetworkopen.2019.3886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006 to 2015. JAMA Psychiatry. 2020;77(7):684-693. doi: 10.1001/jamapsychiatry.2020.0596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishara BL, Stijelja S. Trends in US suicide deaths, 1999 to 2017, in the context of suicide prevention legislation. JAMA Pediatr. 2020;174(5):499-500. doi: 10.1001/jamapediatrics.2019.6066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan SQ, Berrington de Gonzalez A, Best AF, et al. Infant and youth mortality trends by race/ethnicity and cause of death in the United States. JAMA Pediatr. 2018;172(12):e183317-e183317. doi: 10.1001/jamapediatrics.2018.3317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miron O, Yu K-H, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000-2017. JAMA. 2019;321(23):2362-2364. doi: 10.1001/jama.2019.5054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. 2019;144(5):e20191187. doi: 10.1542/peds.2019-1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.May AM, Klonsky ED. What distinguishes suicide attempters from suicide ideators? a meta-analysis of potential factors. Clinical Psychology: Science and Practice. 2016;23(1):5-20. doi: 10.1111/cpsp.12136 [DOI] [Google Scholar]
- 19.Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. 2016;12:307-330. doi: 10.1146/annurev-clinpsy-021815-093204 [DOI] [PubMed] [Google Scholar]
- 20.Gunnell D, Appleby L, Arensman E, et al. ; COVID-19 Suicide Prevention Research Collaboration . Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468-471. doi: 10.1016/S2215-0366(20)30171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci. 2018;6(1):3-17. doi: 10.1177/2167702617723376 [DOI] [Google Scholar]
- 22.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. 2019;128(3):185-199. doi: 10.1037/abn0000410 [DOI] [PubMed] [Google Scholar]
- 23.Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA Pediatr. 2018;172(7):697-699. doi: 10.1001/jamapediatrics.2018.0399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steelesmith DL, Fontanella CA, Campo JV, Bridge JA, Warren KL, Root ED. Contextual factors associated with county-level suicide rates in the United States, 1999 to 2016. JAMA Netw Open. 2019;2(9):e1910936-e1910936. doi: 10.1001/jamanetworkopen.2019.10936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Underwood JM, Brener N, Thornton J, et al. Overview and methods for the youth risk behavior surveillance system: United States, 2019. MMWR Suppl. 2020;69(1):1-10. doi: 10.15585/mmwr.su6901a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brener ND, Kann L, Shanklin S, et al. ; Centers for Disease Control and Prevention (CDC); Centers for Disease Control and Prevention (CDC) . Methodology of the Youth Risk Behavior Surveillance System—2013. MMWR Recomm Rep. 2013;62(RR-1):1-20. [PubMed] [Google Scholar]
- 27.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31(4):336-342. doi: 10.1016/S1054-139X(02)00339-7 [DOI] [PubMed] [Google Scholar]
- 28.Underwood JM, Brener N, Halpern-Felsher B. Tracking adolescent health behaviors and outcomes: strengths and weaknesses of the Youth Risk Behavior Surveillance System. National Academy of Medicine. October 5, 2020. Accessed April 26, 2021. https://nam.edu/tracking-adolescent-health-behaviors-and-outcomes-strengths-and-weaknesses-of-the-youth-risk-behavior-surveillance-system/ [DOI] [PMC free article] [PubMed]
- 29.May A, Klonsky ED. Validity of suicidality items from the Youth Risk Behavior Survey in a high school sample. Assessment. 2011;18(3):379-381. doi: 10.1177/1073191110374285 [DOI] [PubMed] [Google Scholar]
- 30.Silverman JG, Raj A, Mucci LA, Hathaway JE. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA. 2001;286(5):572-579. doi: 10.1001/jama.286.5.572 [DOI] [PubMed] [Google Scholar]
- 31.Kim H-J, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 32.Kim HJ, Fay MP, Yu B, Barrett MJ, Feuer EJ. Comparability of segmented line regression models. Biometrics. 2004;60(4):1005-1014. doi: 10.1111/j.0006-341X.2004.00256.x [DOI] [PubMed] [Google Scholar]
- 33.Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008-2015. Pediatrics. 2018;141(6):e20172426. doi: 10.1542/peds.2017-2426 [DOI] [PubMed] [Google Scholar]
- 34.Burstein B, Agostino H, Greenfield B. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. 2019;173(6):598-600. doi: 10.1001/jamapediatrics.2019.0464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fontanella CA, Hiance-Steelesmith DL, Phillips GS, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatr. 2015;169(5):466-473. doi: 10.1001/jamapediatrics.2014.3561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simonetti JA, Mackelprang JL, Rowhani-Rahbar A, Zatzick D, Rivara FP. Psychiatric comorbidity, suicidality, and in-home firearm access among a nationally representative sample of adolescents. JAMA Psychiatry. 2015;72(2):152-159. doi: 10.1001/jamapsychiatry.2014.1760 [DOI] [PubMed] [Google Scholar]
- 37.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):e20161878. doi: 10.1542/peds.2016-1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gould MS, Velting D, Kleinman M, Lucas C, Thomas JG, Chung M. Teenagers’ attitudes about coping strategies and help-seeking behavior for suicidality. J Am Acad Child Adolesc Psychiatry. 2004;43(9):1124-1133. doi: 10.1097/01.chi.0000132811.06547.31 [DOI] [PubMed] [Google Scholar]
- 39.Rubin R. Rising rates of ED visits for suicidal ideation, suicide attempt. JAMA. 2020;324(16):1598-1598. [DOI] [PubMed] [Google Scholar]
- 40.Bridge JA, Asti L, Horowitz LM, et al. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatr. 2015;169(7):673-677. doi: 10.1001/jamapediatrics.2015.0465 [DOI] [PubMed] [Google Scholar]
- 41.Congressional Black Caucus . Ring the alarm: The crisis of Black youth suicide in America. 2019. Accessed December 12, 2020. https://watsoncoleman.house.gov/uploadedfiles/full_taskforce_report.pdf
- 42.Brent DA, Goldstein TR, Benton TD. Bridging gaps in follow-up appointments after hospitalization and youth suicide: mental health care disparities matter. JAMA Netw Open. 2020;3(8):e2013100. doi: 10.1001/jamanetworkopen.2020.13100 [DOI] [PubMed] [Google Scholar]
- 43.Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. 2010;19(4):759-774. doi: 10.1016/j.chc.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lindsey MA, Xiao Y. Depression, trauma, and suicide among adolescent and young adult males. In: Griffith DM, Bruce MA, Thorpe RJ Jr, eds. Men’s Health Equity: A Handbook. Routledge/Taylor & Francis Group; 2019:288-303. [Google Scholar]
- 45.Mann JJ, Metts AV. The Economy and Suicide. Hogrefe Publishing; 2017. doi: 10.1027/0227-5910/a000487 [DOI] [PubMed] [Google Scholar]
- 46.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195-1201. doi: 10.1001/jamapediatrics.2016.2154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alegría M, Araneta MR, Rivers B. The National Advisory Council on Minority Health and Health Disparities Reflection. Am J Public Health. 2019;109(S1):S14-S15. doi: 10.2105/AJPH.2019.304961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011-2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatr. 2018;172(11):1038-1044. doi: 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089-3096. doi: 10.1001/jama.286.24.3089 [DOI] [PubMed] [Google Scholar]
- 50.Fitzpatrick KM, Piko BF, Miller E. Suicide ideation and attempts among low-income African American adolescents. Suicide Life Threat Behav. 2008;38(5):552-563. doi: 10.1521/suli.2008.38.5.552 [DOI] [PubMed] [Google Scholar]
- 51.Tynes BM, Willis HA, Stewart AM, Hamilton MW. Race-related traumatic events online and mental health among adolescents of color. J Adolesc Health. 2019;65(3):371-377. doi: 10.1016/j.jadohealth.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 52.Yu B, Chen X. Age and birth cohort–adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Netw Open. 2019;2(9):e1911383-e1911383. doi: 10.1001/jamanetworkopen.2019.11383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keyes KM, Gary D, O’Malley PM, Hamilton A, Schulenberg J. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol. 2019;54(8):987-996. doi: 10.1007/s00127-019-01697-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Keyes KM, Hamilton A, Patrick ME, Schulenberg J. Diverging trends in the relationship between binge drinking and depressive symptoms among adolescents in the U.S. from 1991 through 2018. J Adolesc Health. 2020;66(5):529-535. doi: 10.1016/j.jadohealth.2019.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mojtabai R, Olfson M. National trends in mental health care for US adolescents. JAMA Psychiatry. 2020;77(7):703-714. doi: 10.1001/jamapsychiatry.2020.0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kresovich A, Reffner Collins MK, Riffe D, Carpentier FRD. A content analysis of mental health discourse in popular rap music. JAMA Pediatr. 2021;175(3):286-292. doi: 10.1001/jamapediatrics.2020.5155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim S, Colwell SR, Kata A, Boyle MH, Georgiades K. Cyberbullying victimization and adolescent mental health: evidence of differential effects by sex and mental health problem type. J Youth Adolesc. 2018;47(3):661-672. doi: 10.1007/s10964-017-0678-4 [DOI] [PubMed] [Google Scholar]
- 58.Li R, Lian Q, Su Q, Li L, Xie M, Hu J. Trends and sex disparities in school bullying victimization among U.S. youth, 2011-2019. BMC Public Health. 2020;20(1):1583. doi: 10.1186/s12889-020-09677-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.O’Keeffe GS, Clarke-Pearson K; Council on Communications and Media . The impact of social media on children, adolescents, and families. Pediatrics. 2011;127(4):800-804. doi: 10.1542/peds.2011-0054 [DOI] [PubMed] [Google Scholar]
- 60.Xiao Y, Romanelli M, Lindsey MA. A latent class analysis of health lifestyles and suicidal behaviors among US adolescents. J Affect Disord. 2019;255:116-126. doi: 10.1016/j.jad.2019.05.031 [DOI] [PubMed] [Google Scholar]
- 61.Godoy Garraza L, Kuiper N, Goldston D, McKeon R, Walrath C. Long-term impact of the Garrett Lee Smith Youth Suicide Prevention Program on youth suicide mortality, 2006-2015. J Child Psychol Psychiatry. 2019;60(10):1142-1147. doi: 10.1111/jcpp.13058 [DOI] [PubMed] [Google Scholar]
- 62.Godoy Garraza L, Walrath C, Goldston DB, Reid H, McKeon R. Effect of the Garrett Lee Smith Memorial Suicide Prevention Program on suicide attempts among youths. JAMA Psychiatry. 2015;72(11):1143-1149. doi: 10.1001/jamapsychiatry.2015.1933 [DOI] [PubMed] [Google Scholar]
- 63.Cramer RJ, Kapusta ND. A social-ecological framework of theory, assessment, and prevention of suicide. Front Psychol. 2017;8:1756. doi: 10.3389/fpsyg.2017.01756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stanley B, Mann JJ. The need for innovation in health care systems to improve suicide prevention. JAMA Psychiatry. 2020;77(1):96-98. doi: 10.1001/jamapsychiatry.2019.2769 [DOI] [PubMed] [Google Scholar]
- 65.Mann JJ, Michel CA, Auerbach RP. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry. 2021;p202020060864. Published online February 18, 2021. doi: 10.1176/appi.ajp.2020.20060864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.US Department of Education National Center for Education Statistics . Trends in high school dropout and completion rates in the United States. Accessed March 21, 2019. https://nces.ed.gov/programs/dropout/ind_03.asp
- 67.Posner K, Brown GK, Stanley B, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266-1277. doi: 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Turning Points in Temporal Trends in Suicidal Subgroups and Possible Associated Policy and Societal Factors, 1991-2019
eFigure 2. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex, 1991-2019
eFigure 3. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Race/ethnicity, 1991-2019
eFigure 4. Prevalence of Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex and Race/ethnicity, 1991-2019
eFigure 5. Trends in Suicidal Ideation and Suicide Attempts among US Adolescents, by Sex and Race/ethnicity, 1991-2019