Abstract
Background:
The US Food and Drug Administration authorized COVID-19 convalescent plasma (CCP) therapy for hospitalized COVID-19 patients via the Expanded Access Program (EAP) and the Emergency Use Authorization (EUA), leading to use in about 500,000 patients during the first year of the pandemic for the USA.
Methods:
We tracked the number of CCP units dispensed to hospitals by blood banking organizations and correlated that usage with hospital admission and mortality data.
Results:
CCP usage per admission peaked in Fall 2020, with more than 40% of inpatients estimated to have received CCP between late September and early November 2020. However, after randomized controlled trials failed to show a reduction in mortality, CCP usage per admission declined steadily to a nadir of less than 10% in March 2021. We found a strong inverse correlation (r = −0.52, p=0.002) between CCP usage per hospital admission and deaths occurring 2 weeks after admission, and this finding was robust to examination of deaths taking place 1, 2, or 3 weeks after admission. Changes in the number of hospital admissions, SARS-CoV-2 variants, and age of patients could not explain these findings. The retreat from CCP usage might have resulted in as many as 29,000 excess deaths from mid-November 2020 to February 2021.
Conclusions:
A strong inverse correlation between CCP use and mortality per admission in the USA provides population-level evidence consistent with the notion that CCP reduces mortality in COVID-19 and suggests that the recent decline in usage could have resulted in excess deaths.
Funding:
There was no specific funding for this study. AC was supported in part by RO1 HL059842 and R01 AI1520789; MJJ was supported in part by 5R35HL139854. This project has been funded in whole or in part with Federal funds from the Department of Health and Human Services; Office of the Assistant Secretary for Preparedness and Response; Biomedical Advanced Research and Development Authority under Contract No. 75A50120C00096.
Research organism: Human
Introduction
In the Spring of 2020, the USA embarked on a historic and unprecedented deployment of plasma derived from patients who survived COVID-19 (COVID-19 convalescent plasma [CCP]) for treatment of the disease, and 1 year into this effort more than 500,000 individuals have been treated. This development was fueled by the lack of effective alternate therapies, a plentiful supply of plasma from an efficient and high-capacity blood banking network, motivated donors, and strong community partners. US Food and Drug Administration (FDA) regulatory oversight was provided first by its Expanded Access Program (EAP) in partnership with the Mayo Clinic, with first transfusion on early April 2020 (Senefeld et al., 2021), and then by its Emergency Use Authorization (EUA) of August 23, 2020, both of which restricted CCP use to hospitalized patients (Anonymous, 2021b).
The demonstration by the Summer of 2020 that CCP was safe (Joyner et al., 2020a; Joyner et al., 2020b), that antibody concentration in plasma correlated with survival in people treated before mechanical ventilation (Joyner et al., 2021) along with initial suggestions of efficacy (Li et al., 2020; Liu et al., 2020; Salazar et al., 2020), boosted its use. Nonetheless, the use of CCP rose rapidly without the ideal evidence base of efficacy from randomized controlled clinical trials (RCTs), since early RCTs though generally trending positively were inconclusive, mostly due to small size or premature termination as the epidemic abated in the early surge regions (Casadevall et al., 2020). Later in the pandemic, several larger RCTs reported no mortality benefit (Agarwal et al., 2020; Horby et al., 2021; Simonovich et al., 2021), raising doubts as to CCP efficacy. However, these latter trials were undertaken in hospitalized patients treated late in the course of disease and some used plasma with variable antibody levels (Casadevall et al., 2020), and contrasted with a highly successful trial in elderly patients treated within 3 days of illness onset prior to hospitalization (Libster et al., 2021). Despite potential explanations for the negative studies, the results of these studies were sometimes accompanied by editorials that reinforced the message of futility with the British Medical Journal calling CCP ‘ineffective’ (Pathak, 2020), Nature Biotechnology reported that CCP fell ‘flat’ (Sheridan, 2020), and JAMA published a meta-analysis of RCT concluding that there was no evidence of benefit from CCP therapy (Janiaud et al., 2021). On February 17, 2021, the Wall Street Journal reported that Mount Sinai Hospital, which had been a leader in deploying CCP and reported early encouraging results (Liu et al., 2020), had stopped using plasma in patients with COVID-19, and the report specifically mentioned that the negative results from CCP RCTs drove this decision (Marcus, 2021).
On March 13, 2021, the New York Times reported that COVID-19 mortality remained high with nearly 1500 daily deaths despite a drop in the number of new infections since earlier in the year (Leatherby, 2021). Consistent with this report, an analysis of treatment outcomes found that they worsened for the last 2 months of 2020 (Garg et al., 2021). This finding was surprising in light of an apparent reduction in the mortality of hospitalized patients as the epidemic progressed, thought to be from improved management of the disease as clinical experience grew (Ledford, 2020). Analyzing weekly reports from the blood banking industry, we noted that plasma use was on the decline, based on the ratio of units dispensed to hospital relative to hospital admissions. The increase in mortality combined with the reduction in CCP use led us to hypothesize first, that the two phenomena were related, and second, that the decline in CCP use reflected reduced use following the disappointing trial findings. We therefore examined the use of CCP units as a function of time, assessing the relationship of CCP use to COVID-19 mortality, denominating both plasma units and deaths to hospital admissions.
Materials and methods
Convalescent plasma usage
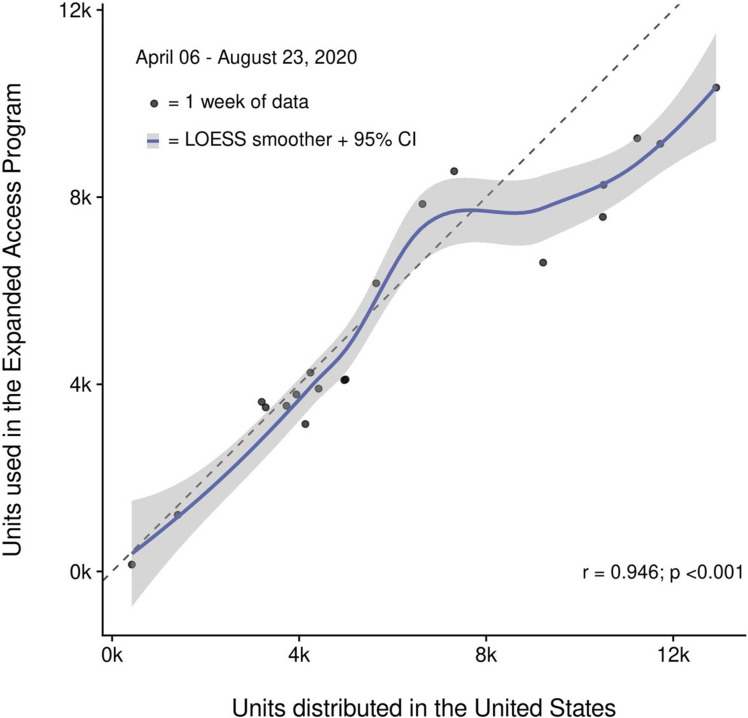
CCP usage was inferred from the distribution of plasma units to hospitals in the USA from data obtained from Blood Centers of America, Inc (BCA, West Warwick, RI). Data fields included collections, distributions to hospitals, distributions to research, or other use. This file consolidated all the reports from regional blood bank reports and provided a total of collected units and units distributed to hospitals. The data file did not have information on whether a unit was actually transfused but BCA can infer usage from hospital re-ordering information and there has been a strong correlation between the total number of units shipped to a hospital and the units transfused by that hospital. Hence, the CCP units dispensed to hospitals represent a reasonable proxy value for the total number of units being transfused to patients. To validate this assumption, we compared the numbers of plasma units dispensed to those used by the EAP. There was a powerful and significant correlation between the weekly counts of units distributed in the USA and those used to treat patients as part of the EAP between April 6 and August 23, 2020 (Spearman’s rho = 0.953, p<0.001) (Figure 1—figure supplement 1). Units transfused in the EAP were reported by providers as part of the official case report forms and each transfusion could comprise one or two units. During both the EAP and EUA epochs of CCP collection and distribution included in this analysis, reimbursement for units collected was provided by the US government. Additionally, most blood products used in the USA including CCP are collected and distributed by a network of regional or national blood banking organizations. In this context, the vast majority (>95%) of all convalescent plasma (CP) administered was likely captured in this analysis (Senefeld et al., 2021).
Admission and mortality data
For population-level data on COVID-19 admissions and mortality, we relied on publicly available databases. Specifically, we used information from the Our World in Data (OWID) (https://ourworldindata.org/coronavirus) database. Data used for this analysis were downloaded on March 18, 2021, and are available as Supplementary file 3. We confirmed these findings using Centers for Disease Control (CDC, Atlanta, GA) data on admissions and deaths https://covid.cdc.gov/covid-data-tracker/#new-hospital-admissions and https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendsdeaths. CDC data were downloaded on March 31, 2021, and are available together with other data used in this analysis at: https://github.com/eapPlasma/plasma_hesitancy/tree/main/rawdata.
Statistical analysis
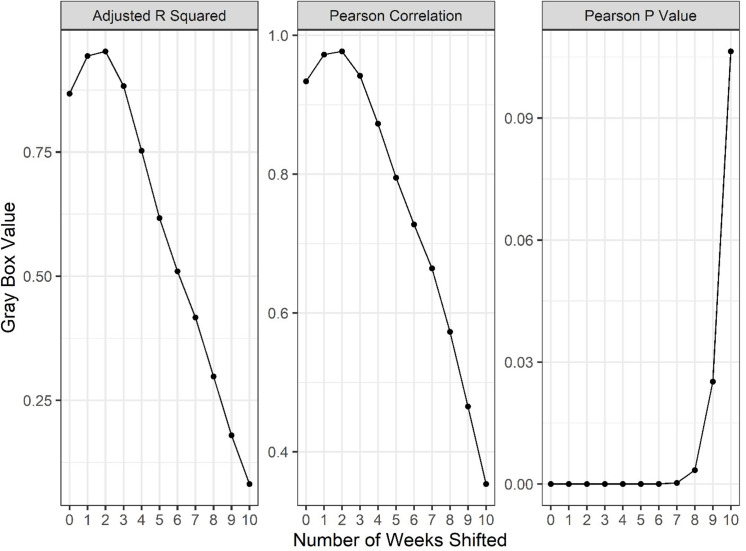
Preliminary descriptive analyses were used to explore the associations of the ratio of number of CCP units dispersed to the number of hospitalizations (CCP utilization ratio) with the ratio of national deaths to national admissions, the latter being a reasonable proxy for the case fatality rate (CFR). No individual-level data were available to link the mortality events directly to the individuals hospitalized to permit a calculation of the true CFR. To address this limitation, the mortality counts reported by the CDC were shifted to better align the deaths with the admitted patients. Since the overwhelming majority of COVID-19 deaths occur in hospitals (Chua et al., 2021; Chuzi et al., 2020), since CCP is only authorized for use in hospitals, and since death generally occurs a few days to weeks after admission, mortality was adjusted for the time lag between admission and death. The median time between admission and death has been reported as 9 days in the USA (Horwitz et al., 2021) and 6.7 days in Belgium (Faes et al., 2020). For the analysis, which was based on weekly aggregated data, a 2-week shift was selected to align the mortality with the median and upper quartile estimates in these reports. The Pearson’s correlation coefficient was used to describe the relationship of the CCP utilization ratio with CFR. To further define this relationship, a linear statistical model was used to regress the utilization ratio onto CFR. This statistical model was weighted by the number of hospitalizations per week. The fit of the model was examined using standard residual-based diagnostic plots and the fit was deemed acceptable using only a linear fit of the CCP utilization ratio.
Three in silico scenarios were created to summarize the effect of alterations to the CCP utilization ratio using the fitted model. In scenario 1, the effect of maintenance of plasma usage was considered. To define maintenance of use, a weighted average of the utilization ratio over the months of August through September 2020 was estimated. This value was then used to estimate the number of deaths that would be expected to occur throughout the study period (admissions starting August 3, 2020 to February 22, 2021). In scenario 2, a constant 50% CCP utilization ratio was set over the entire study period. The utilization rate was approximately the value observed in the early October 2020 period. A final scenario estimated the CFR that may have been observed had CCP not been used at all (i.e., the y-intercept from the model). Model contrasts were used to estimate the change in expected deaths among these scenarios in addition to a fourth condition – the actual number of events reported by the CDC. Values are summarized based on the observed number of hospitalized patients over the study period along with the same values indexed into expected mortality events per 1000 hospitalizations. Pointwise confidence bands for each scenario were obtained by multiplying the model-predicted CFR and its associated 95% confidence interval by the number of hospitalizations per week. Cumulative summations were used to describe the differences in expected deaths over the entire study period. This analysis was repeated independently a third time using a weighted average of utilization ratio of the months October-November on a separate database (OWID) to investigate stability between reporting bodies. As a final method for estimating the overall effect of the changes in CCP utilization, the CDC data were grouped into two time periods representing relative use. The difference in the CFR was used to estimate the expected value for the changes in the expected number of deaths.
Statistical analyses were conducted using R version 3.6.2 (R Development Core Team, 2013); 95% confidence intervals and two-sided p-values were used to summarize association and test for significance at the alpha = 0.05 level of significance, respectively.
Results
CP use
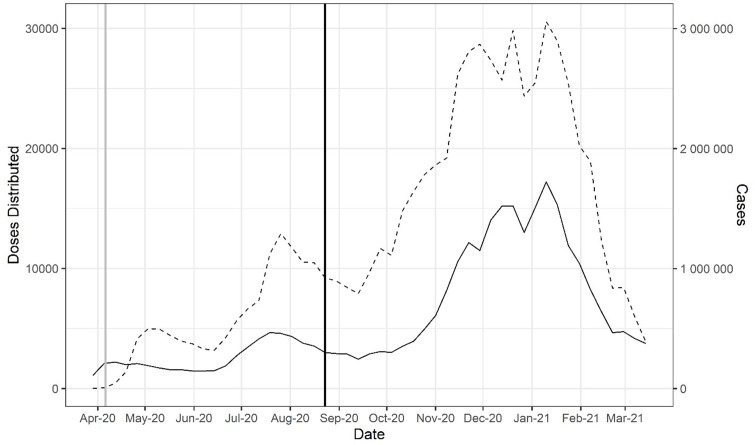
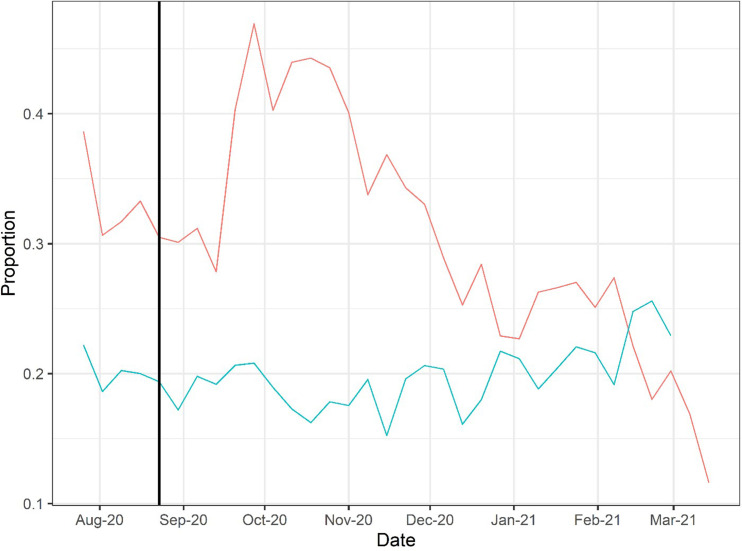
The FDA first allowed compassionate use of CCP on a case-by-case basis in late March 2020, but very quickly initiated the EAP in early April 2020, which was followed by EUA on August 23, 2020, broadening its use. Distribution of CCP to hospitals rose to 25,000–30,000 weekly units by the December 2020 to January 2021 time period, but this rise in plasma distribution largely reflected the great increase in hospital admissions for COVID in those months (Figure 1). When CCP distributions are analyzed as a function of the number of new hospital admissions per week, peak utilization per capita occurred much earlier, in early October 2020 and declined sharply in the following months (Figure 2).
Figure 1. Doses of COVID-19 convalescent plasma (CCP) distributed in the USA by the American Red Cross and American Blood Centers (dashed) and total COVID-19 cases in the USA reported in Our World in Data (OWID) database (solid).
The vertical black line marks August 23, 2020, when the US Food and Drug Administration (FDA) announced that Emergency Use Authorization for CCP in the USA. The vertical gray line marks April 4, 2020, as the start of the Emergency Access Program.
Figure 1—figure supplement 1. Correlation of convalescent plasma distribution and usage within the Expanded Access Program (EAP).
Figure 2. Doses of COVID-19 convalescent plasma (CCP) per hospital admission (red) and mortality calculated as deaths per hospital admission (green) using Our World in Data (OWID) database.
To account for time between admission to death, deaths from 2 weeks after admission are used to calculate mortality. The vertical line marks August 23, 2020, when the US Food and Drug Administration (FDA) announced that Emergency Use Authorization for CCP in the USA.
Correlation between CCP and mortality
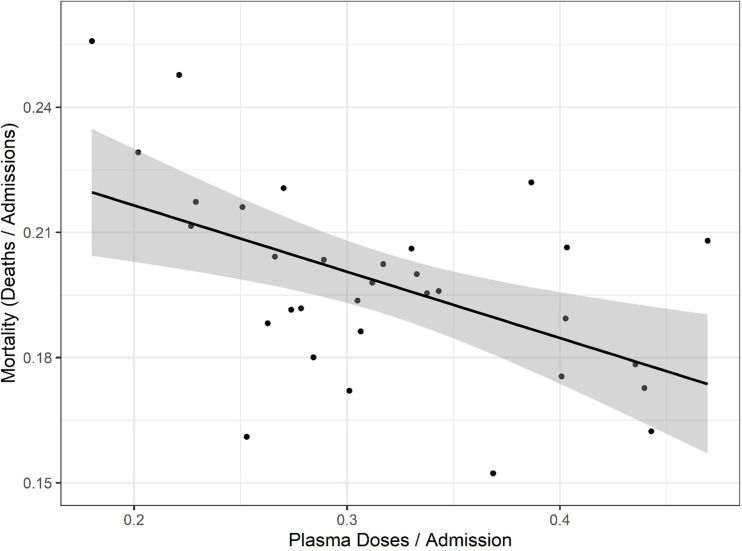
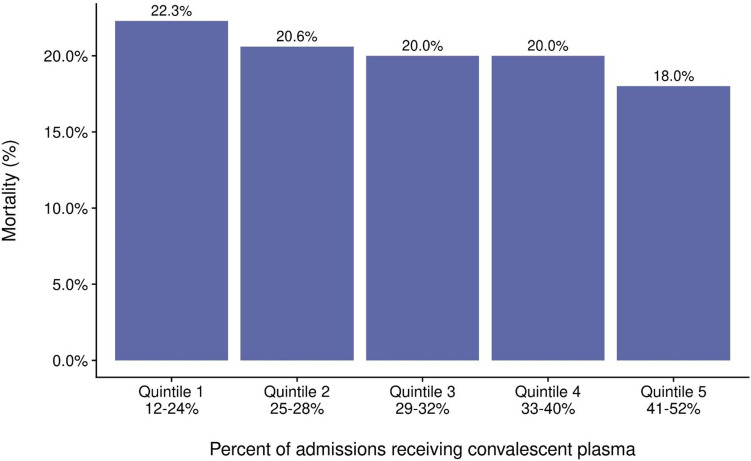
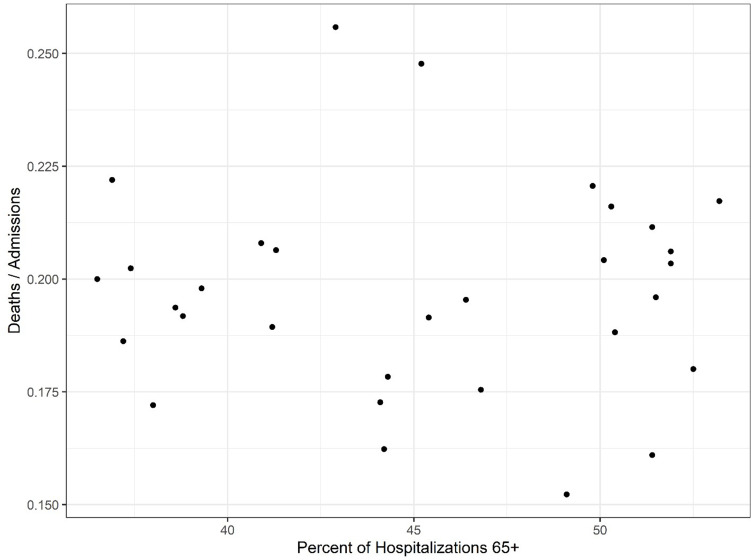
To explore whether there was a relationship between CCP distribution and mortality, we first compared the doses per patient versus reported COVID-19 deaths per hospital admission from publicly available databases (Figure 2). The comparison of curves showed a trough in deaths per admission coinciding with the peak of CCP usage per admission. A plot of mortality versus doses per hospitalized patient using mortality per admission data from the OWID database revealed a strong negative correlation (Pearson’s correlation coefficient of −0.52 with p=0.002) (Figure 3). Similar results were obtained with the CDC database. To account for lags in the reporting of death that vary by state, we also investigated whether this correlation was maintained while adding weeks to the time between admission and death (Figure 3—figure supplement 1). Additionally, if plasma use is divided into quintiles from lowest using weeks to highest using weeks, a graded relationship between use of plasma and mortality is apparent (Figure 3—figure supplement 2). To investigate whether a change in the age demographics of the hospitalized population could account for the observed inverse correlation, we compared the shifted mortality is compared to the percent of hospitalized patients 65+ each week as reported by the CDC and found no significant correlation between these two variables, suggesting changes in mortality are not explainable by an increase in hospitalized high-risk patients (Figure 3—figure supplement 3).
Figure 3. Correlation of mortality (death per admission) and COVID-19 convalescent plasma (CCP) doses per admitted patients using the Our World in Data (OWID) database.
Correlation analysis yields a Pearson’s correlation coefficient of −0.518 (p=0.0024). The black line represents a linear model regression with an R squared of 0.268.
Figure 3—figure supplement 1. A series of linear regressions and Pearson’s correlation tests comparing weekly reported deaths to new weekly hospital admissions, offset by various numbers of weeks to identify the length of lag between admission and death of patients using Our World in Data (OWID) database.
Figure 3—figure supplement 2. Mortality from COVID-19 by quintile of percent of admissions receiving COVID-19 convalescent plasma (CCP).
Figure 3—figure supplement 3. Investigation of high age group mortality.
Estimates of excess deaths
The linear model using the CCP utilization ratio to predict the CFR fits the data well in that this model explained 25% (R2 = 0.254) of the variance of CFR using only the CCP utilization ratio. The model estimated that the CFR decreased by 1.8 percentage points for every 10 percentage point increase in the rate of utilization of CCP (p=0.004). The linear regression analysis yielded a mortality in patients not receiving CCP of 25.2% as the y-intercept. A comparison of this number with that from US studies shows reasonable agreement between with the average mortality of 23.5% in patients not receiving CCP (Supplementary file 1). This percentage also closely matches the 24% mortality for COVID-19 patients for the large RECOVERY trial in the UK (Horby et al., 2021) and the 30% mortality of patients receiving late CCP in analysis from the EAP (Joyner et al., 2021). An extrapolation of the linear model to the situation where every patient is treated with CCP yields a mortality of 7.6%, which is lower than the average mortality in US studies, but still within the range reported (Supplementary file 1). However, this extrapolation to maximal use is much less reliable given the absence of points in the y-axis region above an CCP utilization ratio of 0.6 and uncertainty as to whether the relationship is linear in those ranges. Hence, we caution the reader about making any strong inference from this estimate while noting that it is close to the 6.2% mortality reported for COVID-19 patients treated with high titer CCP very early upon hospitalization (Salazar et al., 2021). Nevertheless, it is possible to use these efficacy numbers to estimate what the effect on deaths would have been had the USA continued to use CCP at the height of its usage in early Fall 2020, when more than 40% of all patients received plasma therapy.
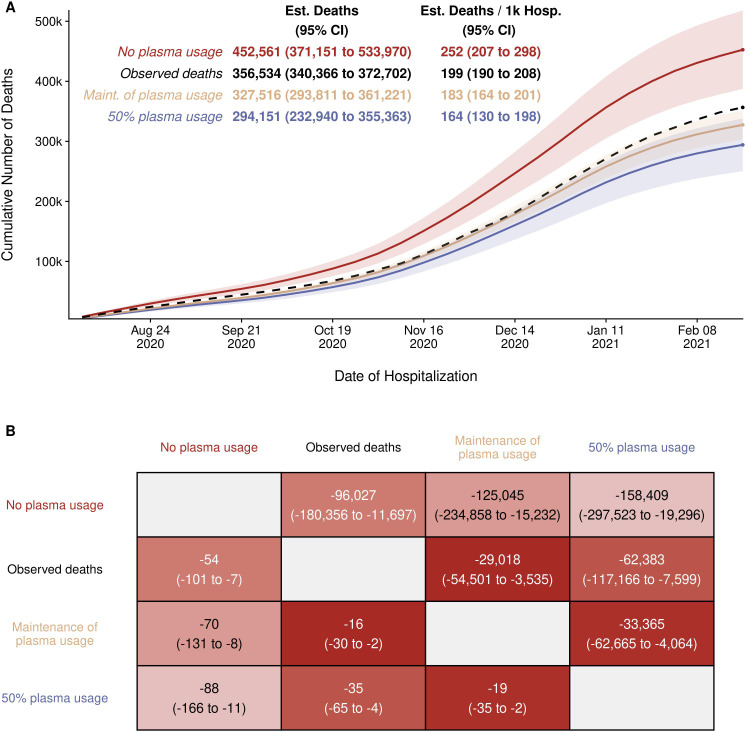
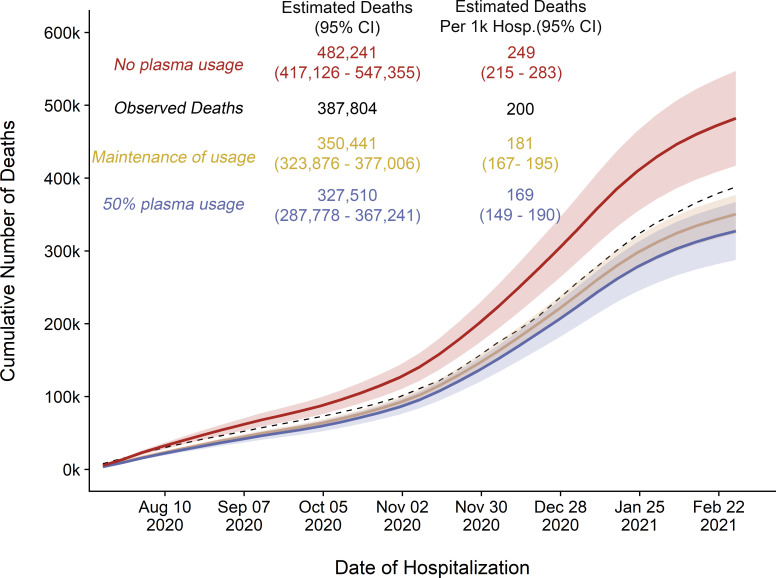
With this model as a framework for estimating the excess number of deaths, the results of three scenarios were obtained (Figure 4). The total observed deaths over the study period was 356,534. Had the rate of CCP utilization observed during August through October 2002 carried over for the remaining months, the expected number of deaths was 327,516 (95% CI: 293,811–361,221), which might result in 29,018 (95% CI: 3535–54,501) fewer deaths than observed. This excess death, in comparison, was small relative to the estimate that results from assuming plasma utilization was as high as it was after the EUA was issued. Had 50% utilization of plasma been continued, 62,383 (95% CI: 7599–117,166) fewer deaths may have been observed. Under the most extreme scenario comparing no plasma use to the highest observed use, a difference of 158,409 (95% CI: 19,296–297,523) deaths is estimated. We repeated this analysis independently for each of the databases used (CDC versus OWID) with concordant results (Figure 4; Figure 4—figure supplement 1; Supplementary file 2; Supplementary file 3). The models also estimate that between 94,436 (Figure 4—figure supplement 1; Supplementary file 3) and 95,026 (Figure 4) excess deaths might have occurred in the USA had CP never been deployed using the OWID and CDC databases, respectively.
Figure 4. Estimated (Est.) deaths under modeled scenarios of COVID-19 convalescent plasma (CCP) using Centers for Disease Control (CDC) database.
Panel A presents the longitudinal observed (dashed line) and modeled number of deaths under three scenarios for CCP over the study period (August 3, 2020 to February 22, 2021) that included 356,534 deaths in 1,793,502 hospitalized patients. Over the entire study period, the CCP utilization ratio was 29.1%. In the scenario labeled maintenance (Maint.) of plasma, the CCP utilization ratio was set to 39.5%. With the no plasma and 50% plasma usage scenarios, the CCP utilization ratio was set at 0% and 50%, respectively. Panel B provides the pairwise comparisons of these scenarios to estimate the difference in expected number of deaths among the scenarios for the entire hospitalized patients (upper right triangle) and re-indexed to events per 1000 patients (lower left triangle). The rows represent the comparator or reference scenario, columns indicate the altered CCP use scenario. For example, the cell that intersects the observed deaths and the maintenance of plasma column shows that 29,018 fewer deaths would result had plasma use remained at the 39.5% level.
Figure 4—figure supplement 1. Replicated cumulative excess deaths analysis per Our World in Data (OWID) database for scenario 1 (orange).
As an alternative method to estimating the excess deaths, which alleviates the need for a model, the data were summarized into two time periods characterized by high and low utilization of CCP (Table 1). In each of the 7 weeks from September 21 to November 8, 2020, the estimated proportion of inpatients transfused with CP exceeded 40% (average 42.6%). We refer to this period as ‘high utilization’. In the period immediately following – from November 9, 2021, to the week starting March 22, 2021 – utilization was lower; transfusion rates declined steadily, averaging 27.4% and we refer to this as the ‘low utilization’ period. The 2-week lagged mortality ratio for 257,424 patients hospitalized in the high utilization period was 18.16% and rose to 20.08% for the 1,344,463 patients admitted in the 18-week period of low utilization. Table 1 shows that if the mortality rate in the low utilizing 18 weeks had been the same as during the high transfusion period, 25,871 fewer deaths might have taken place.
Table 1. Estimated number of excess deaths due to transfusion hesitancy.
| Time period | Transfusion rate | Number of admissions | Deaths | Mortality rate | Expected deaths if mortality had remained at 18.16% | Excess deaths in the low transfusion period | Excess deaths per 1000 admissions |
|---|---|---|---|---|---|---|---|
| High utilization ( September 21, 2021 to November 8, 2021) | 42.59% | 257,424 | 46,747 | 18.16% | 46,747 | – | – |
| Low Utilization (November 9, 2021 to March 22, 2021) | 27.43% | 1,344,463 | 270,019 | 20.08% | 244,148 | 25,871 | 19.2 |
Discussion
The use of CCP in hospitalized patients rose steadily after the FDA EUA of late August 2020, and from mid-September to the end of October, we estimate that CCP was provided to more than 40% of admissions. This rise occurred despite opinion pieces arguing that evidence of efficacy was insufficient for the authorization (Baden et al., 2020; Pau et al., 2021) . However, RCTs from India (Agarwal et al., 2020), Argentina (Simonovich et al., 2021), and the UK (Horby et al., 2021) reporting that CCP use did not reduce mortality in hospitalized patients were followed by a substantial decline in use that began in November. The American Association of Blood Banks reported a 50% increase in the number of institutions planning to stop offering CCP between February and March 2021 (Anonymous, 2021a). By March 2021, no more than 10% of hospitalized patients were receiving CCP.
The drop in per capita CCP utilization was strongly associated with an increase in mortality among hospitalized COVID-19 patients. It is notable that mortality from COVID-19 among hospitalized patients decreased substantially over most of 2020, consistent with worldwide trends (Ledford, 2020), but then began to rise in late November and early December 2020, a period that coincided with reduction in CCP use. If the association we describe is truly causal, we estimate that reduced use of CCP resulted in 29,000–36,000 excess deaths over the past year in the USA.
Concluding that a causal relationship exists between CCP use and mortality requires excluding the contribution of other variables that can affect mortality, a challenging task during an ongoing pandemic when information about the pathophysiology and clinical course of COVID-19 is accruing rapidly. All possible confounders are not available to us to include in this analysis. However, five factors can reasonably be excluded. We excluded that variation in age of hospitalized patients explained the findings since the mean age of the hospitalized population with COVID-19 was actually older during peak use of CCP than later, implying that the association might be even higher if age of admissions was taken into account. Similarly, we considered whether the winter surge in hospital admissions that stretched staff to the utmost could have affected the death rate, but excluded this possibility since the number of hospital admissions per week was not associated with mortality (r = −0.02). A delay in recording of death certificate information could not account for the findings since our findings are robust when deaths are considered from 2 to 5 weeks after admission. We considered whether the emergence of new variants accounted for our findings but excluded this possibility since this concern would apply largely to the most recent months. Only 76 isolations of the UK B.1.1.7 variant, which is associated with higher contagiousness and perhaps, mortality (Challen et al., 2021), were identified by January, an estimated 0.5% or less of COVID infections at that time (Galloway et al., 2021). Even as late as mid-March 2021, a time beyond the analyses of this paper, the B.1.1.17 variant comprised only 25% of US isolates (Anonymous, 2021c); increased mortality from these infections, if present, would not manifest itself until times later than our analysis included. In addition, limiting the end-time of our analysis to January 2021 did not change the findings. Finally, we note that interventions associated with efficacy against COVID-19 such as corticosteroids, Remdesivir, and prone positioning were introduced into clinical practice before the decline in CP use that began in late fall and that no new effective therapy was introduced or withdrawn during the October 2020 to March 2021 period, except for the decline in CP use documented here.
Our findings should be interpreted with caution but several aspects of the evidentiary landscape point to CPP efficacy in reducing mortality when used appropriately. First, an analysis of several dozen studies associated the administration of CCP with reduced mortality, with an overall effect size of ~35% (Klassen et al., 2021). These studies include a powerful RCT in elderly outpatients that halved progression to severe disease. In the USA, the two completed RCTs each show a reduction of mortality with CPP usage (Bennett-Guerrero et al., 2021; O'Donnell et al., 2021). Second, CP has proven effective in individuals with defective humoral immunity and B cell defects (Senefeld et al., 2020; Thompson et al., 2021). Third, the active agent in plasma, specific antibody to SARS-CoV-2, is strongly related to mortality in transfused patients (Joyner et al., 2021; Libster et al., 2021; Maor et al., 2020). Fourth, the active agent of CCP, specific antibody to SARS-CoV-2, has powerful antiviral activity and has been shown to reduce the viral load in patients with COVID-19, thus providing a mechanistic explanation for its therapeutic effect (Kim et al., 2020). Fifth, human CP is protective in murine models of COVID-19 (Sun et al., 2020). Sixth, patients treated with CCP manifest reduced inflammatory markers (Bandopadhyay et al., 2021; Tremblay et al., 2020; Wu et al., 2021) that can lead to host damage (Pirofski and Casadevall, 2020). Seventh, research has identified nine places where plasma affects the cascade of inflammation to the benefit of treated patients (Acosta-Ampudia et al., 2021).
The clinical evidence on CP and mortality is mixed. Three randomized trials have failed to show a reduction in mortality (Agarwal et al., 2020; Horby et al., 2021; Simonovich et al., 2021), another RCT found a 40% reduction in mortality (O'Donnell et al., 2021), as other smaller trials and comparative studies (reviewed in Klassen et al., 2021). Unfortunately, many trials treated patients with advanced disease. For example, while the overall findings of the RECOVERY trial were null (Horby et al., 2021), all four categories of patients treated early in the course of illness (before antibody conversion, in the first 7 days, not receiving steroids, not on oxygen) showed lower mortality in the CPP arm. Late use of plasma, or use in people with advanced illness, is not likely to be effective, because at that time the inflammatory response itself is the major pathophysiologic pathway to severe illness and death, and added antibody is likely powerless to change the course of illness (Casadevall et al., 2021b).
While we agree that RCTs are the ideal source of information on treatments, if trials are done in a patient population unlikely to benefit from the intervention because of late disease, they cannot fully contribute to understanding. We argue for taking a more holistic look at the available data on CP, which, as noted above, is consistent with benefit of treatment in early disease and with adequate antibody in the plasma. Our population-level analysis is analogous to the observational studies that linked smoking and lung cancer, a finding universally accepted by the weight of evidence from many sources, in spite of the absence of any RCT demonstrating the finding (Smoking and Health, 1964).
Taking a page from the reluctance of citizens to accept vaccines against SARS-CoV-2, a phenomenon that has been termed ‘vaccine hesitancy’ (Pullan and Dey, 2021), we call the reduced use of CCP ‘plasma hesitancy’. Plasma hesitancy may be a result of health care providers overvaluing and overemphasizing negative results from RCT findings while dismissing other evidence that CCP reduces mortality. Physicians have relatively little recent experience with treating infectious diseases with antibody therapies (Casadevall et al., 2021b). Chemical agents, however, are more familiar, and the success of antiviral drugs against human immunodeficiency and hepatitis C viruses is well known.
CCP remains one of few options available for treating COVID-19 early in the disease. It is readily available wherever there are recovered patients, requires no complex manufacturing, is inexpensive, and has an excellent safety profile (Joyner et al., 2020a). Interim guidelines for the American Association of Blood Banks (Cohn et al., 2021) and from Brazil (De Santis et al., 2021) emphasize both of these principles – early treatment and high antibody content in plasma. We hope that physicians policymakers, regulators, and guideline committees consider the totality of the available evidence, including our findings, when making decisions for CCP use in individual patients (Casadevall et al., 2021a).
Acknowledgements
We are grateful to Bill Block and Jennifer Kapral from BCA (West Warwick, RI) and Kate Fry from America Blood Centers (Washington, DC) for their help in obtaining the plasma usage data. Disclaimer: The views and opinions expressed in this publication are those of the authors and do not reflect the official policy or position of the US Department of Health and Human services and its agencies including the Biomedical Research and Development Authority and the Food and Drug Administration, as well as any agency of the US government. Assumptions made within and interpretations from the analysis are not reflective of the position of any US government entity.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Arturo Casadevall, Email: acasade1@jhu.edu.
Jameel Iqbal, James J Peters Veterans Affairs Medical Center, United States.
Mone Zaidi, Icahn School of Medicine at Mount Sinai, United States.
Funding Information
This paper was supported by the following grants:
National Institute of Allergy and Infectious Diseases AI1520789 to Arturo Casadevall.
Biomedical Advanced Research and Development Authority 75A50120C00096 to Michael J Joyner.
Additional information
Competing interests
No competing interests declared.
Author contributions
Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Project administration.
Formal analysis, Investigation, Methodology, Writing - original draft.
Formal analysis, Investigation, Methodology.
Investigation, Writing - review and editing.
Investigation, Writing - review and editing.
Conceptualization, Project administration, Writing - review and editing.
Conceptualization, Investigation, Writing - original draft, Project administration.
Conceptualization, Formal analysis, Investigation, Methodology, Writing - original draft.
Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft.
Additional files
Summarized data of hospitalizations and deaths, from CDC data.
Data availability
All data generated or analysed during this study are included in the manuscript and supporting files.
References
- Acosta-Ampudia Y, Monsalve DM, Rojas M, Rodríguez Y, Gallo JE, Salazar-Uribe JC, Santander MJ, Cala MP, Zapata W, Zapata MI, Manrique R, Pardo-Oviedo JM, Camacho B, Ramírez-Santana C, Anaya JM, CP-COVID-19 group COVID-19 convalescent plasma composition and immunological effects in severe patients. Journal of Autoimmunity. 2021;118:102598. doi: 10.1016/j.jaut.2021.102598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal A, Mukherjee A, Kumar G, Chatterjee P, Bhatnagar T, Malhotra P, PLACID Trial Collaborators Convalescent plasma in the management of moderate covid-19 in adults in India: open label phase II multicentre randomised controlled trial (PLACID trial) BMJ. 2020;371:m3939. doi: 10.1136/bmj.m3939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous AABB survey: ccp usage reevaluation march. 2021a. [April 1, 2021]. https://www.aabb.org/docs/default-source/default-document-library/resources/ccp-usage-re-evaluation-survey-report-ii-march-2021.pdf?sfvrsn=3db80c8e_0
- Anonymous Investigational COVID-19 convalescent plasma, Guidance for Industry. 2021b. [April 1, 2021]. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/investigational-covid-19-convalescent-plasma
- Anonymous Variant proportions in the united states. 2021c. [April 1, 2021]. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/variant-proportions.html
- Baden LR, Solomon CG, Greene MF, D’Agostino RB, Harrington D. The FDA and the Importance of Trust. New England Journal of Medicine. 2020;383:e148. doi: 10.1056/NEJMe2030687. [DOI] [PubMed] [Google Scholar]
- Bandopadhyay P, Rozario R, Lahiri A, Sarif J, Ray Y, Paul SR, Roy R, Maiti R, Chaudhuri K, Bagchi S, Maiti A, Perwez MM, Sharma Sarkar B, Roy D, Chakraborty R, Vasudevan JS, Sharma S, Biswas D, Maiti C, Saha B, Bhattacharya P, Pandey R, Chatterjee S, Paul S, Ganguly D. Nature and dimensions of the systemic hyper-inflammation and its attenuation by convalescent plasma in severe COVID-19. The Journal of Infectious Diseases. 2021 doi: 10.1093/infdis/jiab010. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett-Guerrero E, Romeiser JL, Talbot LR, Ahmed T, Mamone LJ, Singh SM, Hearing JC, Salman H, Holiprosad DD, Freedenberg AT, Carter JA, Browne NJ, Cosgrove ME, Shevik ME, Generale LM, Andrew MA, Nachman S, Fries BC, Stony Brook Medicine COVID Plasma Trial Group Severe acute respiratory syndrome coronavirus 2 convalescent plasma versus standard plasma in coronavirus disease 2019 infected hospitalized patients in New York: a Double-Blind randomized trial. Critical Care Medicine. 2021 doi: 10.1097/CCM.0000000000005066. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A, Grossman BJ, Henderson JP, Joyner MJ, Shoham S, Pirofski LA, Paneth N. The assessment of convalescent plasma efficacy against COVID-19. Med. 2020;1:66–77. doi: 10.1016/j.medj.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casadevall A, Joyner M, Paneth N. A victory or scientific pragmatism. the new atlantis. 2021a. [April 1, 2021]. https://www.thenewatlantis.com/publications/a-victory-for-scientific-pragmatism
- Casadevall A, Pirofski LA, Joyner MJ. The principles of antibody therapy for infectious diseases with relevance for COVID-19. mBio. 2021b;12:e03372-20. doi: 10.1128/mBio.03372-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. 2021;372:n579. doi: 10.1136/bmj.n579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua IS, Shi SM, Levine DM. Place of death and End-of-Life care utilization among COVID-19 decedents in a Massachusetts health care system. Journal of Palliative Medicine. 2021;24:322–323. doi: 10.1089/jpm.2020.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuzi S, Molsberry R, McCabe ME, Yancy CW, Ogunseitan A, Allen NB, Khan SS. Distribution in place of death for COVID-19-Related mortality in the united states. Journal of the American Geriatrics Society. 2020;68:1917–1918. doi: 10.1111/jgs.16721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn CS, Estcourt L, Grossman BJ, Pagano MB, Allen ES, Bloch EM, Tobian AAR. COVID-19 convalescent plasma: interim recommendations from the AABB. Transfusion. 2021;61:1313–1323. doi: 10.1111/trf.16328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Santis GC, Mendrone A, Langhi D, Covas DT, Fabron A, Cortez AJP, Dinardo CL, Ubiali EMA, Marques JFC, Bordin JO, Rugani MA. Suggested guidelines for convalescent plasma therapy for the treatment of COVID-19. Hematology, Transfusion and Cell Therapy. 2021 doi: 10.1016/j.htct.2021.03.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faes C, Abrams S, Van Beckhoven D, Meyfroidt G, Vlieghe E, Hens N, Belgian Collaborative Group on COVID-19 Hospital Surveillance Time between symptom onset, hospitalisation and recovery or death: statistical analysis of belgian COVID-19 patients. International Journal of Environmental Research and Public Health. 2020;17:7560. doi: 10.3390/ijerph17207560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway SE, Paul P, MacCannell DR, Johansson MA, Brooks JT, MacNeil A, Slayton RB, Tong S, Silk BJ, Armstrong GL, Biggerstaff M, Dugan VG. Emergence of SARS-CoV-2 b.1.1.7 lineage - United states, December 29, 2020-January 12, 2021. MMWR. Morbidity and Mortality Weekly Report. 2021;70:95–99. doi: 10.15585/mmwr.mm7003e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg S, Patel K, Pham H, Kirley PD, Kawasaki B, Yousey-Hindes K, Havers F. Clinical trends among U.S. adults hospitalized with COVID-19, March-December 2020. medRxiv. 2021 doi: 10.1101/2021.04.21.21255473. [DOI] [PMC free article] [PubMed]
- Horby PW, Estcourt L, Peto L, Emberson JR, Staplin N, Spata E, Landray MJ. Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. medRxiv. 2021 doi: 10.1101/2021.03.09.21252736. [DOI]
- Horwitz LI, Jones SA, Cerfolio RJ, Francois F, Greco J, Rudy B, Petrilli CM. Trends in COVID-19 Risk-Adjusted mortality rates. Journal of Hospital Medicine. 2021;16:90–92. doi: 10.12788/jhm.3552. [DOI] [PubMed] [Google Scholar]
- Janiaud P, Axfors C, Schmitt AM, Gloy V, Ebrahimi F, Hepprich M, Smith ER, Haber NA, Khanna N, Moher D, Goodman SN, Ioannidis JPA, Hemkens LG. Association of convalescent plasma treatment with clinical outcomes in patients with COVID-19: a systematic review and Meta-analysis. Jama. 2021;325:1185–1195. doi: 10.1001/jama.2021.2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyner MJ, Bruno KA, Klassen SA, Kunze KL, Johnson PW, Lesser ER, Wiggins CC, Senefeld JW, Klompas AM, Hodge DO, Shepherd JRA, Rea RF, Whelan ER, Clayburn AJ, Spiegel MR, Baker SE, Larson KF, Ripoll JG, Andersen KJ, Buras MR, Vogt MNP, Herasevich V, Dennis JJ, Regimbal RJ, Bauer PR, Blair JE, van Buskirk CM, Winters JL, Stubbs JR, van Helmond N, Butterfield BP, Sexton MA, Diaz Soto JC, Paneth NS, Verdun NC, Marks P, Casadevall A, Fairweather D, Carter RE, Wright RS. Safety update: covid-19 convalescent plasma in 20,000 hospitalized patients. Mayo Clinic Proceedings. 2020a;95:1888–1897. doi: 10.1016/j.mayocp.2020.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyner MJ, Wright RS, Fairweather D, Senefeld JW, Bruno KA, Klassen SA, Carter RE, Klompas AM, Wiggins CC, Shepherd JRA, Rea RF, Whelan ER, Clayburn AJ, Spiegel MR, Johnson PW, Lesser ER, Baker SE, Larson KF, Ripoll JG, Andersen KJ, Hodge DO, Kunze KL, Buras MR, Vogt MNP, Herasevich V, Dennis JJ, Regimbal RJ, Bauer PR, Blair JE, Van Buskirk CM, Winters JL, Stubbs JR, Paneth NS, Verdun NC, Marks P, Casadevall A. Early safety indicators of COVID-19 convalescent plasma in 5000 patients. Journal of Clinical Investigation. 2020b;130:4791–4797. doi: 10.1172/JCI140200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyner MJ, Carter RE, Senefeld JW, Klassen SA, Mills JR, Johnson PW, Theel ES, Wiggins CC, Bruno KA, Klompas AM, Lesser ER, Kunze KL, Sexton MA, Diaz Soto JC, Baker SE, Shepherd JRA, van Helmond N, Verdun NC, Marks P, van Buskirk CM, Winters JL, Stubbs JR, Rea RF, Hodge DO, Herasevich V, Whelan ER, Clayburn AJ, Larson KF, Ripoll JG, Andersen KJ, Buras MR, Vogt MNP, Dennis JJ, Regimbal RJ, Bauer PR, Blair JE, Paneth NS, Fairweather D, Wright RS, Casadevall A. Convalescent plasma antibody levels and the risk of death from Covid-19. New England Journal of Medicine. 2021;384:1015–1027. doi: 10.1056/NEJMoa2031893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MS, An MH, Kim WJ, Hwang TH. Comparative efficacy and safety of pharmacological interventions for the treatment of COVID-19: a systematic review and network meta-analysis. PLOS Medicine. 2020;17:e1003501. doi: 10.1371/journal.pmed.1003501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klassen SA, Senefeld JW, Johnson PW, Carter RE, Wiggins CC, Shoham S, Salazar E. The effect of convalescent plasma therapy on COVID-19 patient mortality: systematic review and Meta-analysis. medRxiv. 2021 doi: 10.1101/2020.07.29.20162917. [DOI] [PMC free article] [PubMed]
- Leatherby L. Despite encouraging downward trend, US. covid deaths remain high. New York times. 2021. [March 13, 2021]. https://www.nytimes.com/interactive/2021/03/13/us/coronavirus-march-summer-peak.html
- Ledford H. Why do COVID death rates seem to be falling? Nature. 2020;587:190–192. doi: 10.1038/d41586-020-03132-4. [DOI] [PubMed] [Google Scholar]
- Li L, Zhang W, Hu Y, Tong X, Zheng S, Yang J, Kong Y, Ren L, Wei Q, Mei H, Hu C, Tao C, Yang R, Wang J, Yu Y, Guo Y, Wu X, Xu Z, Zeng L, Xiong N, Chen L, Wang J, Man N, Liu Y, Xu H, Deng E, Zhang X, Li C, Wang C, Su S, Zhang L, Wang J, Wu Y, Liu Z. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and Life-threatening COVID-19: a randomized clinical trial. Jama. 2020;324:460–470. doi: 10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libster R, Pérez Marc G, Wappner D, Coviello S, Bianchi A, Braem V, Esteban I, Caballero MT, Wood C, Berrueta M, Rondan A, Lescano G, Cruz P, Ritou Y, Fernández Viña V, Álvarez Paggi D, Esperante S, Ferreti A, Ofman G, Ciganda A, Rodriguez R, Lantos J, Valentini R, Itcovici N, Hintze A, Oyarvide ML, Etchegaray C, Neira A, Name I, Alfonso J, López Castelo R, Caruso G, Rapelius S, Alvez F, Etchenique F, Dimase F, Alvarez D, Aranda SS, Sánchez Yanotti C, De Luca J, Jares Baglivo S, Laudanno S, Nowogrodzki F, Larrea R, Silveyra M, Leberzstein G, Debonis A, Molinos J, González M, Perez E, Kreplak N, Pastor Argüello S, Gibbons L, Althabe F, Bergel E, Polack FP. Early High-Titer plasma therapy to prevent severe Covid-19 in older adults. New England Journal of Medicine. 2021;384:610–618. doi: 10.1056/NEJMoa2033700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu STH, Lin HM, Baine I, Wajnberg A, Gumprecht JP, Rahman F, Rodriguez D, Tandon P, Bassily-Marcus A, Bander J, Sanky C, Dupper A, Zheng A, Nguyen FT, Amanat F, Stadlbauer D, Altman DR, Chen BK, Krammer F, Mendu DR, Firpo-Betancourt A, Levin MA, Bagiella E, Casadevall A, Cordon-Cardo C, Jhang JS, Arinsburg SA, Reich DL, Aberg JA, Bouvier NM. Convalescent plasma treatment of severe COVID-19: a propensity score–matched control study. Nature Medicine. 2020;26:1708–1713. doi: 10.1038/s41591-020-1088-9. [DOI] [PubMed] [Google Scholar]
- Maor Y, Cohen D, Paran N, Israely T, Ezra V, Axelrod O, Shinar E, Izak M, Rahav G, Rahimi-Levene N, Bazofin BM, Gelman R, Dicker D, Brosh-Nissimov T, Megged O, Dahan D, Benov A, Paz A, Edward K, Moran A, Rogowski O, Sorkine P, Mayo A, Zimhony O, Chen J. Compassionate use of convalescent plasma for treatment of moderate and severe pneumonia in COVID-19 patients and association with IgG antibody levels in donated plasma. EClinicalMedicine. 2020;26:100525. doi: 10.1016/j.eclinm.2020.100525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus A. New York's Mount Sinai Ends Blood-Plasma Treatment for Hospitalized Covid-19 Patients, The Wall Street Journal. 2021. [April 1, 2021]. https://www.wsj.com/livecoverage/covid-2021-02-17/card/cGbDcQrNi5UetgXrjbwz
- O'Donnell MR, Grinsztejn B, Cummings MJ, Justman JE, Lamb MR, Eckhardt CM, Philip NM, Cheung YK, Gupta V, João E, Pilotto JH, Diniz MP, Cardoso SW, Abrams D, Rajagopalan KN, Borden SE, Wolf A, Sidi LC, Vizzoni A, Veloso VG, Bitan ZC, Scotto DE, Meyer BJ, Jacobson SD, Kantor A, Mishra N, Chauhan LV, Stone EF, Dei Zotti F, La Carpia F, Hudson KE, Ferrara SA, Schwartz J, Stotler BA, Lin W-HW, Wontakal SN, Shaz B, Briese T, Hod EA, Spitalnik SL, Eisenberger A, Lipkin WI. A randomized double-blind controlled trial of convalescent plasma in adults with severe COVID-19. medRxiv. 2021 doi: 10.1101/2021.03.12.21253373. [DOI] [PMC free article] [PubMed]
- Pathak EB. Convalescent plasma is ineffective for covid-19. BMJ. 2020;371:m4072. doi: 10.1136/bmj.m4072. [DOI] [PubMed] [Google Scholar]
- Pau AK, Aberg J, Baker J, Belperio PS, Coopersmith C, Crew P, Grund B, Gulick RM, Harrison C, Kim A, Lane HC, Masur H, Sheikh V, Singh K, Yazdany J, Tebas P. Convalescent plasma for the treatment of COVID-19: perspectives of the national institutes of health COVID-19 treatment guidelines panel. Annals of Internal Medicine. 2021;174:93–95. doi: 10.7326/M20-6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirofski LA, Casadevall A. Pathogenesis of COVID-19 from the perspective of the Damage-Response framework. mBio. 2020;11:e01175. doi: 10.1128/mBio.01175-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullan S, Dey M. Vaccine hesitancy and anti-vaccination in the time of COVID-19: a google trends analysis. Vaccine. 2021;39:1877–1881. doi: 10.1016/j.vaccine.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team . Vienna, Austria: R Foundation for Statistical Computing; 2013. http://www.r-project.org [Google Scholar]
- Salazar E, Christensen PA, Graviss EA, Nguyen DT, Castillo B, Chen J, Lopez BV, Eagar TN, Yi X, Zhao P, Rogers J, Shehabeldin A, Joseph D, Leveque C, Olsen RJ, Bernard DW, Gollihar J, Musser JM. Treatment of coronavirus disease 2019 patients with convalescent plasma reveals a signal of significantly decreased mortality. The American Journal of Pathology. 2020;190:2290–2303. doi: 10.1016/j.ajpath.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar E, Christensen PA, Graviss EA, Nguyen DT, Castillo B, Chen J, Lopez BV, Eagar TN, Yi X, Zhao P, Rogers J, Shehabeldin A, Joseph D, Masud F, Leveque C, Olsen RJ, Bernard DW, Gollihar J, Musser JM. Significantly decreased mortality in a large cohort of coronavirus disease 2019 (COVID-19) Patients transfused early with convalescent plasma containing High-Titer Anti-Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Spike protein IgG. The American Journal of Pathology. 2021;191:90–107. doi: 10.1016/j.ajpath.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senefeld JW, Klassen SA, Ford SK, Wiggins CC, Bostrom BC, Thompson MA, Joyner MJ. Therapeutic use of convalescent plasma in COVID-19 patients with immunodeficiency. medRxiv. 2020 doi: 10.1101/2020.11.08.20224790. [DOI]
- Senefeld JW, Johnson PW, Kunze KL, van Helmond N, Klassen SA, Wiggins CC, Joyner MJ. Program and patient characteristics for the united states expanded access program to COVID-19 convalescent plasma. medRxiv. 2021 doi: 10.1101/2021.04.08.21255115. [DOI]
- Sheridan C. Convalescent plasma falls flat in first randomized trial. Nature Biotechnology. 2020 doi: 10.1038/d41587-020-00020-0. In press. [DOI] [PubMed] [Google Scholar]
- Simonovich VA, Burgos Pratx LD, Scibona P, Beruto MV, Vallone MG, Vázquez C, Savoy N, Giunta DH, Pérez LG, Sánchez M, Gamarnik AV, Ojeda DS, Santoro DM, Camino PJ, Antelo S, Rainero K, Vidiella GP, Miyazaki EA, Cornistein W, Trabadelo OA, Ross FM, Spotti M, Funtowicz G, Scordo WE, Losso MH, Ferniot I, Pardo PE, Rodriguez E, Rucci P, Pasquali J, Fuentes NA, Esperatti M, Speroni GA, Nannini EC, Matteaccio A, Michelangelo HG, Follmann D, Lane HC, Belloso WH. A randomized trial of convalescent plasma in Covid-19 severe pneumonia. New England Journal of Medicine. 2021;384:619–629. doi: 10.1056/NEJMoa2031304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoking and Health . Report of the Advisory Committee to the Surgeon General of the United States. Department of Health, Education. andAnd Welfare, Public Health Service; 1964. [Google Scholar]
- Sun J, Zhuang Z, Zheng J, Li K, Wong RL, Liu D, Huang J, He J, Zhu A, Zhao J, Li X, Xi Y, Chen R, Alshukairi AN, Chen Z, Zhang Z, Chen C, Huang X, Li F, Lai X, Chen D, Wen L, Zhuo J, Zhang Y, Wang Y, Huang S, Dai J, Shi Y, Zheng K, Leidinger MR, Chen J, Li Y, Zhong N, Meyerholz DK, McCray PB, Perlman S, Zhao J. Generation of a broadly useful model for COVID-19 pathogenesis, vaccination, and treatment. Cell. 2020;182:734–743. doi: 10.1016/j.cell.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MA, Henderson JP, Shah PK, Rubinstein SM, Joyner MJ, Choueiri TK, Warner JL. Convalescent plasma and improved survival in patients with hematologic malignancies and COVID-19. medRxiv. 2021 doi: 10.1101/2021.02.05.21250953. [DOI]
- Tremblay D, Seah C, Schneider T, Bhalla S, Feld J, Naymagon L, Wang B, Patel V, Jun T, Jandl T, Rahman F, Liu STH, Aberg JA, Bouvier N, Mount Sinai Health System Convalescent Plasma Team Convalescent plasma for the treatment of severe COVID-19 infection in Cancer patients. Cancer Medicine. 2020;9:8571–8578. doi: 10.1002/cam4.3457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Shen J, Han Y, Qiao Q, Dai W, He B, Pang R, Zhao J, Luo T, Guo Y, Yang Y, Wu Q, Jiang W, Zhang J, Zhang M, Li N, Li W, Xia X. Upregulated IL-6 Indicates a Poor COVID-19 Prognosis: A Call for Tocilizumab and Convalescent Plasma Treatment. Frontiers in Immunology. 2021;12:598799. doi: 10.3389/fimmu.2021.598799. [DOI] [PMC free article] [PubMed] [Google Scholar]