Abstract
Objective:
Latinx populations are rapidly growing and aging in the US. There is a critical need to accurately and efficiently detect those at risk for dementia, particularly those with Mild Cognitive Impairment (MCI). MCI diagnosis often relies on neuropsychological assessment, although cultural, demographic, and linguistic characteristics may impact test scores. This study provides a scoping review of neuropsychological studies on MCI in Hispanic/Latinx populations to evaluate how studies report and account for these factors in diagnosis of MCI.
Method:
Studies were identified utilizing Web of Science, PubMed, and Scopus, using search terms “(Hispanic* OR Latin* OR “Mexican American* OR “Puerto Ric*” OR Caribbean)” and (“Mild Cognitive Impairment” OR MCI). Studies utilizing neuropsychological tests in diagnosis of MCI for Latinx individuals in the US were identified. Sample characterization (e.g., country of origin, literacy, language preference and proficiency), neuropsychological testing methods (e.g., test selection and translation, normative data source), and method of MCI diagnosis were reviewed.
Results:
Forty-four manuscripts met inclusion criteria. There was considerable variability in reporting of demographic, cultural and linguistic factors across studies of MCI in Latinx individuals. For example, only 5% of studies reported nativity status, 52% reported information on language preference and use, and 34% reported the method and/or source of test translation and adaptation.
Conclusions:
Future studies of diagnosis of MCI in Latinx individuals should report culturaldetails and use of appropriate neuropsychological assessment tools and normative data. This is important to accurately estimate the prevalence of MCI in Latinx individuals.
Keywords: neuropsychological assessment, mild cognitive impairment, Hispanics, Latinos, Latinx, Mexican Americans
Individuals of Hispanic ethnicity represent a rapidly growing demographic in the US population, with projections that they will represent 26% of the US population by 2050 (Vincent & Velkoff, 2010). Individuals self-identifying as of Hispanic ethnicity represent considerable cultural, linguistic, and demographic diversity. The Census Bureau’s code list contains more than 30 Hispanic or Latino subgroups (US Census Bureau.); in 2010, 63% of this group identified as Mexican American, 9.2% as Puerto Rican, 3.5% as Cuban, and 24% as another country of origin. Of the 53.7 million Hispanics aged 5 and older living in the US in 2017, 72% reported speaking a language other than English, and (28%) reported speaking only English Individuals of Hispanic ethnicity in the US represent a broad spectrum with regard to the degree of identification with the majority US culture versus a heritage culture, ranging from recent US immigrants to families living in the US for several generations (Flores, 2017). These factors, for example, relate to disparities with regard to access to and quality of education, with Hispanic adults disproportionately impacted by limited or no access to education relative to non-Hispanics (Judd et al., 2009; Musu-Gillette et al., 2017). Of note, although the US Census and the research literature has traditionally used the term “Hispanic” or “Latino/a” to describe this population, the term “Latinx” has been proposed as a more inclusive term. We will thus use the term “Latinx” for the remainder of this manuscript.
Cultural, linguistic, and demographic factors have a known impact on neuropsychological test performance, which has been summarized comprehensively elsewhere (Cagigas & Manly, 2014; Fujii, 2017; Loewenstein, Argüelles, Argüelles, & Linn-fuentes, 1994; Rivera Mindt, Byrd, Saez, & Manly, 2010a) including their considerations in neuropsychological assessment of older adults (e.g., Rivera Mindt et al., 2019). Education has a clear and pervasive impact on neuropsychological test performance (Lezak et al., 2012). Although educational experience is typically quantified as number of years of education, disparities in educational quality are known to contribute to differences in neuropsychological test scores (Sisco et al., 2015). Literacy has been used as a proxy for educational quality (Manly, Jacobs, Touradji, Small, & Stern, 2002), and illiteracy impacts performance across all neuropsychological domains (Ardila et al., 2010). Of relevance to Latinx immigrants, educational systems provide educational content and skills (e.g., test-taking) that are culturally relevant. As such, individuals living and educated in the US may be more likely, relative to individuals living and educated in other countries, to have been exposed to culturally-salient information that aligns with items and constructs being evaluated in North American neuropsychological tests. For example, cultural factors have been shown to impact approach to speeded tests (e.g., (Agranovich, Panter, Puente, & Touradji, 2011) and cognitive abilitites associated with tests of intellectual functioning (Fasfous, Hidalgo-Ruzzante, Vilar-Lopez, Catena-Martinez, & Perez-Garcia, 2013). Indeed, several studies have reported relationships between the number of years educated outside of the US and neuropsychological test performance (Krch et al., 2015; Razani, Burciaga, Madore, & Wong, 2007). In addition, diagnostic errors (i.e., false identification of impairment) have been demonstrated in healthy populations during use of North American neuropsychological tests for diverse populations (e.g., Daughterty et al., 2017).
The neuropsychological testing experience is impacted by cultural identity and values (Rivera-Mindt et al., 2019; Cagigas & Manly, 2014; Fujii, 2017). Acculturation, or the degree to which one identifies with the dominant versus heritage culture, has been associated with neuropsychological test performance (Razani et al., 2007), with higher performance in those with higher dominant culture acculturation (Arentoft et al., 2012) and number of years lived in the US (Gasquoine, 1999). However, operationalization of this construct has proven challenging, may be multidimensional (Huynh, Howell, & Benet-Martínez, 2009), and may not explain additional variance beyond education and language use (Mungas, Reed, Haan, & Gonzalez, 2005). Given the cultural, demographic, linguistic, and socioeconomic diversity amongst Latin American countries, it is not surprising that differences have been reported in neuropsychological test performance in healthy individuals across these countries, despite equivalent inclusion and exclusion criteria (Arango-Lasprilla et al., 2015; Rivera & Arango-Lasprilla, 2017). These findings may be particularly relevant to consider for relatively recent immigrants to the US from Latin America. Differences in neuropsychological test performance by region of origin has also been shown in an HIV+ Latinx sample (Marquine et al., 2018). Taken together, it is unclear whether and when it is appropriate to combine individuals from various countries of origin into an ostensibly homogenous group.
Language use is an important consideration in neuropsychological assessment of Latinx individuals. In bilinguals, some studies have found lower performance on some language-based neuropsychological tests relative to monolinguals (Gasquoine & Gonzalez, 2012), such as confrontation naming (e.g., Gollan, Fennema-Notestine, Montoya, & Jernigan, 2007), and higher performance on measures of attention, particularly inhibitory control (Rivera Mindt et al., 2008). Bilingualism is a possible protective factor in onset of dementia diagnosis (Bialystok, Abutalebi, Bak, Burke, & Kroll, 2016), although these findings have been inconsistent (Zahodne, Schofield, Farrell, Stern, & Manly, 2014) and may be moderated by education level (Estanga et al., 2017; Gollan, Salmon, Montoya, & Galasko, 2011). Determination of the most appropriate language for neuropsychological assessment can be complex, particularly in the context of bilinguals with comparable proficiency in both languages, and bilingual individuals may be best assessed through a combination of languages (Judd et al., 2009; Rivera Mindt et al., 2008). Guidelines for determining best language for testing are limited; studies suggest that self-rating of language proficiency can be inaccurate (Judd et al., 2009), leading some to recommend objective methods of measuring language proficiency (Miranda et al., 2016; Rivera Mindt et al., 2008). For individuals evaluated in Spanish, selection of neuropsychological tests that have been appropriately translated, culturally adapted, and sufficiently equivalent to the English-language version is a challenging endeavor, and the field has been faced by a dearth of such instruments (Rivera-Mindt et al., 2019).
In light of these complex factors, it is clear that the creation, selection, and implementation of culturally appropriate normative data is difficult, and ethnicity alone clearly does not fully capture the numerous factors impacting neuropsychological test performance in cognitively healthy individuals in these populations. Use of culturally appropriate normative data can be critical so as to reduce the risk of false-positive errors (i.e., designation of cognitively normal as impaired; e.g., Manly et al., 2005), although use of demographically corrected normative data is complex and requires nuanced decision-making (Romero et al., 2009). Differential false-positive errors by ethnicity has important and widespread research and clinical implications, ranging from policy decisions derived from prevalence estimates to conclusions drawn from investigation of mechanisms of disease process.
The above challenges may be particularly relevant to diagnostic accuracy for Mild Cognitive Impairment (MCI), given that one of the core components of this diagnosis is evidence of cognitive impairment, with generally preserved functional independence. Whereas early iterations of the criteria for this diagnosis (Petersen et al., 2001) required impairment in one or more cognitive domains, greater than expected given the patient’s age and educational background, newer criteria (Albert et al., 2011) specify that cognitive decline should be observed relative to culturally appropriate norms. Similarly, the DSM-5’s inclusion of the minor neurocognitive disorder diagnosis (American Psychiatric Association, 2013) notes an expectation of cognitive impairment around 1–2 standard deviations (SD) below expectation based on culturally appropriate norms. Despite the mandate to utilize culturally appropriate normative data, there does not exist a consensus regarding normative data or neuropsychological assessment tools that are appropriate for all Latinx older adults (Rivera-Mindt et al., 2019).
In summary, there are multiple cultural, linguistic, and demographic factors that are known to impact neuropsychological test scores in Latinx populations, and may also impact the prevalence, expression, course of age-related cognitive impairment in older adults. To our knowledge, there has been only one review published on the diagnosis of MCI in Hispanics (Rose, 2005), which did not focus on neuropsychological assessment. In light of the importance of neuropsychological assessment in diagnosis of MCI, the present study aimed to conduct a scoping review of the existing literature on the diagnosis of MCI in Latinx individuals. Specifically, we aimed to evaluate: 1) whether relevant demographic, cultural and linguistic factors were reported in studies on MCI in Latinx individuals, and 2) whether these factors were considered in MCI diagnostic methodology, particularly with regard to selection of normative data. We hypothesized that we would find variability in the reporting of relevant cultural, linguistic, and demographic information, and with regard to the extent to which neuropsychological data used for MCI diagnosis incorporated these factors. A scoping review was selected as the methodology for this research question given the methodological focus of our research questions (Peters et al., 2015). More specifically, whereas systematic reviews often seek to synthesize the strength and quality of the evidence for a particular research question, scoping reviews seek to provide an overview of a particular literature (e.g., Pham et al., 2014). The scoping review framework is often recommended when a topic has not been extensively reviewed, is complex and heterogeneous, and to address questions regarding how research on a particular topic is conducted (Munn et al., 2018; Pham et al., 2014). Similar to systematic reviews, scoping reviews include rigorous, systematic methodology, with recent publication of PRISMA guidelines (i.e., Preferred Reporting Items for Systematic reviews and Meta-Analyses; (Tricco et al., 2018) for this approach.
Method
We follow the PRISMA guidelines in design and reporting of our scoping review (Tricco et al., 2018). We developed an a priori protocol after pilot testing of the literature.
Identification of relevant studies
We conducted a search of three scientific databases: Web of Science, PubMed, and Scopus (final search date: 4/30/2019). We used the following search criteria for all databases: (“Mild Cognitive Impairment” OR MCI) AND (Hispanic* OR Latin* OR “Mexican American*” OR (Puerto Ric*) OR Caribbean).
Selection criteria
We utilized the following selection criteria for studies: 1) research manuscript (e.g., excluded editorials, reviews) 2) abstract included search terms (when relevance was ambiguous based on abstract, full article text was accessed); 3) clinical/behavioral focus (e.g., excluded studies reporting exclusively biomarker analyses) 4) manuscript written in English or Spanish; and 5) study utilized neuropsychological assessment as component of MCI diagnosis (e.g., studies in which MCI diagnosis was based on cognitive screening were excluded). Neuropsychological assessment was defined as administration of greater than two neuropsychological tests and sampling at least two cognitive domains (given that the focus was on neuropsychological assessment, we did not include studies that administered 1–2 cognitive screening instruments); 6) study sample included Latinx individuals in the US; 7) analyses and/or reported outcomes included ethnicity and MCI diagnosis (e.g., we excluded papers that included Latinx individuals in the sample, but did not describe analyses or results by ethnicity). We did not limit by publication year.
Procedure
After removal of duplicates, each study was reviewed. We extracted information regarding the samples’ cultural, demographic, and linguistic characteristics, in addition to MCI diagnostic methods. We extracted the following data items. With regard to sample characteristics, we identified whether the manuscript described: 1) the Latinx sample’s countries of origin; 2) the proportion of the sample that was US-born, 3) the number of years lived in the US (when sample was not described as entirely US-born); 4) country of education, 5) assessment of literacy; and 6) assessment of acculturation. With regard to language functioning and use, we identified: 1) whether any information was provided with regard to language use (i.e., English and/or Spanish-speaking); 2) whether and how assessment of language proficiency and/or preference was completed; 3) language used for neuropsychological assessment and proportion of sample tested in each language; 4) method used to determine language of assessment; 5) method of test translation/adaptation for neuropsychological assessments completed in Spanish. With regard to MCI diagnostic methods, we identified: 1) method of MCI diagnosis (i.e., clinical consensus, algorithm, or single clinician/other method); 2) whether a specific normative cut-off was reported for MCI diagnosis; 3) whether the source of the normative data was reported; and 4) whether the normative data source included a meaningful number of Latinx individuals (i.e., >10% of normative sample). Data charting was completed by one reviewer (EMB).
Procedure for charting results:
For each variable of interest, the text of each manuscript was scanned. Of note, many studies utilized data from a parent cohort study and cited a prior manuscript that described procedural details pertaining to MCI diagnostic methods. When these manuscripts were referenced, the referenced study was reviewed. We also performed this additional review for charting of region of origin, but not for other sample characteristics or linguistic functioning, as the composition of the specific analytic sub-sample may have varied from previously published cohort subsamples.
Synthesis of results
For each paper reviewed, we determined whether each data item was included, categorized the included data items, then tallied the number and proportion of included papers that reported each data item.
Results
Studies identified
Figure 1 displays number of studies identified from each source. After removal of studies that did not meet inclusion criteria and duplicates, 44 manuscripts were identified for inclusion.
Figure 1.
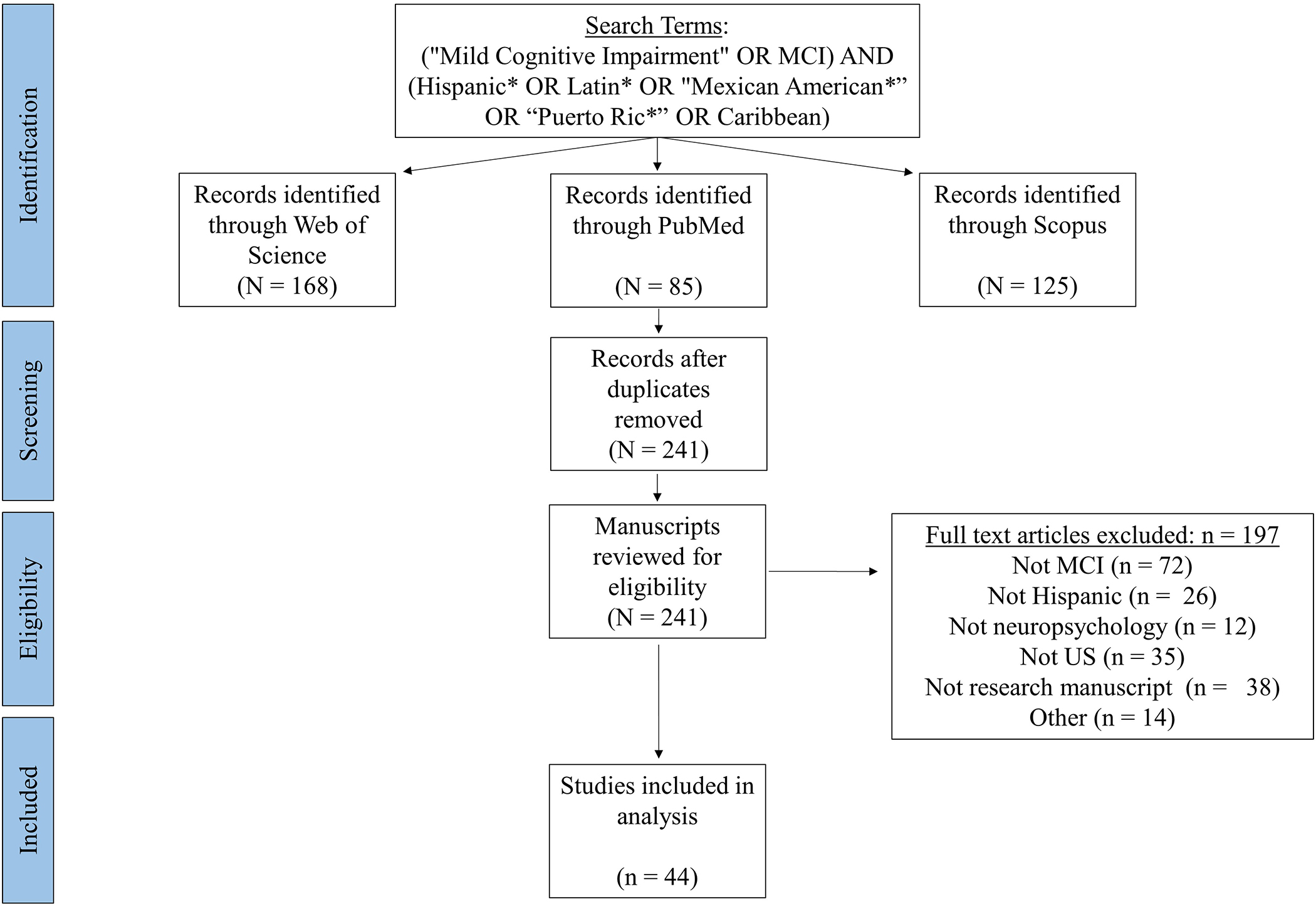
Flow diagram of article identification, screening, eligibility, and inclusion. MCI = mild cognitive impairment.
Characteristics of sources of evidence
Tables 1 and 2 provide information on sample characterization and linguistic functioning (Table 1) and neuropsychological assessment and MCI diagnostic methods (Table 2) for each included study. Table 3 summarizes these findings.
Table 1.
Sample characterization and linguistic functioning in studies of MCI in Latinx individuals
| Cohort | Study | Sample description | Nativity; Number of years in US | Country of education | Language use | Literacy | Acculturation |
|---|---|---|---|---|---|---|---|
| 1Florida ADRC | Duara et al., 2019 | Hispanic (in discussion: primarily from countries such as Cuba, Colombia, Venezuela) | NR | NR | Tested in English or Spanish (72% in Spanish) | NR | NR |
| Florida ADRC, Miami Beach | Rosselli et al., 2019 | Immigrants to US from Latin-American countries | All immigrants; Reported mean age of immigratio n, number of years in US | NR | Measured bilingualism with self-report questionnaire; Tested in preferred language (62% in Spanish) | NR | NR |
| FRONTIER | Johnson et al., 2013 | Hispanic1 | NR | NR | NR | NR | NR |
| Johnson et al., 2014 | Mexican American | NR | NR | NR | NR | NR | |
| FRONTIER, HABLE, TARCC | Johnson et al., 2015 | Mexican American | NR | NR | NR | AMNART/WAT | NR |
| FRONTIER, TARCC | O’Bryant, Johnson, Reisch, et al., 2013 | Mexican American | NR | NR | NR | NR | NR |
| FRONTIER, TARCC | O’Bryant, Johnson, Balldin, et al., 2013 | Mexican American | NR | NR | 39% tested in Spanish | NR | NR |
| HABLE | Johnson et al., 2016 | Mexican American | NR | NR | NR | NR | NR |
| Johnson et al., 2017 | Mexican American | NR | NR | Tested in English or Spanish; proportion NR | NR | NR | |
| Johnson, Large, Izurieta Munoz, Hall, & O’Bryant, 2019 | Mexican American | NR | NR | Tested in English or Spanish; proportion NR | NR | NR | |
| Szerlip et al., 2015 | Mexican American | NR | NR | Tested in English or Spanish; proportion NR | NR | NR | |
| NACC | (cclendon, Hernandez, Smyth, & Lerner, 2009 | Hispanic | NR | NR | NR | NR | NR |
| Milani, Marsiske, Cottler, Chen, & Striley, 2018 | Hispanic | NR | NR | NR | NR | NR | |
| Pandya, Lacritz, Deschner, Woon, & Weiner, 2017 | Hispanic | NR | NR | NR | NR | NR | |
| NYU ADC | Guerrero-Berroa et al., 2014 | Countries of origin specified (US/Latin America) | Reported number US-born; number of years in US NR | NR | All Spanish primary language; all tested in Spanish | NR | NR |
| Predictors 3 | Stem, Gu, Cosentino, Azar, & Lawless, 2017 | Hispanic2 | NR | NR | NA (methods paper) | NR | NR |
| SPS3 | Dhamoon et al., 2015 | Hispanic (note: participants from Spain were classified as nonHispanic white) | NR | NR | NR | NR | NR |
| Jacova et al., 2015 | Hispanics living in US were a subset of Hispanic sample. Countries of origin NR | NR | NR | Selected only monolingual (>90% Spanish) and bilingual (>50% Spanish) speakers; All tested in Spanish | NR | NR | |
| Pearce et al., 2014 | Hispanics living in US were a subset of Hispanic sample | NR | NR | Reported proportion that spoke English and Spanish | NR | NR | |
| SPRINT | Williamson et al., 2019 | Hispanic | NR | NR | Reported tests available in Spanish | NR | NR |
| TARCC | O’Bryant, Johnson, Edwards, Soares, & Devous, 2013 | Mexican American | NR | NR | NR | NR | NR |
| Royall & Palmer, 2013 | Mexican American | NR | NR | Reported tests available in Spanish, proportion tested in Spanish NR | NR | NR | |
| Royall & Palmer, 2014 | Hispanic1 | NR | NR | NR | NR | NR | |
| Royall & Palmer, 2016 | Mexican American | NR | NR | Reported tests available in Spanish, proportion tested in Spanish NR | NR | NR | |
| Royall & Palmer, 2017 | Mexican American | NR | NR | NR | NR | NR | |
| (Salazar, Velez, & Royall, 2014) | Mexican American | NR | NR | 55% tested in Spanish | AMNART | NR | |
| Salazar, Dwivedi, & Royall, 2016 | 99% Mexican American | NR | NR | English or Spanish speaking; language of testing NR | AMNART | NR | |
| UC Davis ADC | DeCarli et al., 2008 | Hispanic | NR | NR | Reported proportion fluent in English (36%); number tested in Spanish (64%) | AMNART (subset) | NR |
| Early et al., 2013 | Hispanic (primarily Mexican descent) | NR | NR | Reported proportion tested in Spanish (54%) | AMNART (subset) | NR | |
| Farias, Mungas, & Jagust, 2005 | Hispanic | NR | NR | Reported proportion tested in Spanish (46%) | NR | NR | |
| Farias, Mungas, Reed, Harvey, & Decarli, 2009 | Hispanic | NR | NR | NR | AMNART | NR | |
| Hinton et al., 2010 | Hispanic | NR | NR | NR | NR | NR | |
| Miller et al., 2015 | Region of ancestry reported (i.e., primarily North, Central, or South American ancestry; most commonly Mexico) | NR | NR | 19% were monolingual Spanish speakers; proportion tested in Spanish NR | NR | NR | |
| WHICAP | Blum et al., 2012 | Hispanic2 | NR | NR | NR | NR | NR |
| Devanand et al., 2010 | Caribbean Hispanic | NR | NR | Reported number that completed smell test in Spanish (n = 373 of 1092 participants) | NR | NR | |
| Gu et al., 2015 | Hispanic2 | NR | NR | Tested in English or Spanish; proportion not reported | NR | NR | |
| Luchsinger et al., 2007 | Caribbean Hispanic | NR | NR | NR | NR | NR | |
| Manly et al., 2005 | Caribbean Hispanic, from several countries of origin | NR | NR | 28.7% of sample was Hispanic; 25% of full sample was Spanishspeaking; 93% of Hispanic sample tested in Spanish | NR | NR | |
| Manly et al., 2008 | Caribbean Hispanic, from several countries of origin | NR | NR | 92% tested in Spanish | NR | NR | |
| Manly et al., 2011 | Caribbean Hispanic | NR | NR | Tested in English or Spanish; proportion not reported | NR | NR | |
| Rizvi et al., 2018 | Hispanic2 | NR | NR | English or Spanish speaking; language of testing NR | NR | NR | |
| Scarmeas et al., 2009 | Hispanic2 | NR | NR | NR | NR | NR | |
| Zahodne et al., 2013 | Hispanic2 | NR | NR | Sample was 36% Hispanic; 33% of sample tested in Spanish | WRAT-3/WAT | NR | |
| Women's Health Initiative-Memory Study | Goveas et al., 2016 | Hispanic | NR | NR | NR | NR | NR |
Note: ADC = Alzheimer’s Disease Center. ADRC = Alzheimer’s Disease Research Center. AMNART = American National Adult Reading Test. FRONTIER = Facing Rural Obstacles to Healthcare Now Through Intervention, Education & Research. HABLE =Health & Aging Brain among Latino Elders. NA = not applicable. NACC = National Alzheimer’s Disease Coordinating Center. NR = Not reported. NYU ADC = New York University Alzheimer’s Disease Center. SPS3 = The Secondary Prevention of Small Subcortical Strokes study. TARCC = Texas Alzheimer’s Research and Care Consortium. UC = University of California. WAT = Word Accentuation Test. WHICAP = Washington Heights-Inwood Columbia Aging Project (WHICAP). WRAT = Wide Range Achievement Test.
Cited previous paper describing cohort as Mexican American.
Cited previous paper describing cohort as Caribbean Hispanic.
Table 2.
Neuropsychological assessment and MCI diagnostic methods in Latinx individuals
| Cohort | Study | Method for selection of language of assessment | Translation/adaptation | MCI diagnosis method | Normative data source | Normative data included Hispanics |
|---|---|---|---|---|---|---|
| 1Florida ADRC | Duara et al. 2019 | Patient preference | Cited published Spanish translations | Consensus with NACC D1 classification protocol | Cited normative data for Spanish translations | Yes |
| Florida ADRC, Miami Beach | Rosselli et al., 2019 | Patient preference | NR | Clinician diagnosis. Impaired scores ≥ 1.5 SD below normal | NR | Assumed yes; reported that norms were corrected by age, education, and language |
| FRONTIER | Johnson et al., 2013 | NR | NR | Clinical consensus | NR | No |
| Johnson et al., 2014 | NR | NR | Clinical consensus assumed but not specified in this paper. MCI generally considered when test scores were ≥ 1.5 SD below the mean. | Publisher's norms NHW; unpublished local norms for English- and Spanish-speaking Hispanics | Yes | |
| FRONTIER, HABLE, TARCC | Johnson et al., 2015 | NR | NR | Clinical consensus | NR | NR |
| FRONTIER, TARCC | O’Bryant, Johnson, Reisch, et al., 2013 | Patient preference | NR | Clinical consensus | (Ivnik et al., 1992) | No |
| FRONTIER, TARCC | O’Bryant, Johnson, Balldin, et al., 2013 | Patient preference | NR | Clinical consensus | Ivnik et al. (1992) | No |
| HABLE | Johnson et al., 2016 | NR | NR | Clinical consensus. MCI generally considered when test scores were ≥ 1.5 SD below the mean. | NR | NR |
| Johnson et al., 2017 | Patient preference | NR | Clinical consensus | Unpublished local norms for English and Spanish-speaking Hispanics | Yes | |
| Johnson et al., 2019 | Patient preference | NR | Clinical consensus. Impairment considered if test was ≥ 1.5 SD below age- and education-adjusted norms. | (O’Bryant et al., 2018) | Yes | |
| Szerlip et al., 2015 | Patient preference | NR | Clinical consensus. Impairment considered if test was ≥ 1.5 SD below age- and education-adjusted norms. | Unpublished local norms for English and Spanish-speaking Hispanics | Yes | |
| NACC | Mcclendon et al., 2009 | NR | NR | Clinician diagnosis | NR | NR |
| Milani et al., 2018 | NR | NR | Clinician diagnosis | NR | NR | |
| Pandya et al., 2017 | NR | NR | Clinician diagnosis | (Shirk et al., 2011) | No (4.2% Hispanic in normative sample) | |
| NYU ADC | Guerrero-Berroa et al., 2014 | Patient preference | NR | Clinical consensus | Unclear; referenced (De Santi et al., 2008)(89% White, ethnicity NR); also referenced normative data for Wechsler for Spanish speakers | Y, reported as available for WAIS only (EIWA-III, Spain); referenced US validation study |
| Predictors 3 | Stern et al., 2017 | Patient opinion of best performance | Translated and back-translated by a committee of Spanish speakers from Cuba, Puerto Rico, Spain, and the Dominican Republic. | Clinical consensus | Source NR; describes age-, education-, ethnicity, and sex-corrected scores from WHICAP (Manly et al. (2005) assumed). | Yes |
| SPS3 | Dhamoon et al. 2015 | NR | NR | Algorithm; Impairment z ≤ −1·5 in at least 1 test domain; per Jacova et al. (2012) | Unclear; references methods from Jacova et al. (2012); (Englishspeaking sample) | No (if consistent with Jacova et al. (2012) |
| Jacova et al., 2015 | NR | Reported published and validated Spanish test versions with references. | Algorithm: Impairment on each test identified with z-score ≤ −1·5. Tests grouped into domains using PCA. MCI designation if impairment in ≥1 domain. | Yes; varied | Yes, for most tests | |
| Pearce et al., 2014 | NR | NR | Algorithm: impairment defined as score of ≥1.5 SD below the mean. | Cited Jacova et al. (2012) | No, if consistent with Jacova et al. (2012) | |
| SPRINT | Williamson et al., 2019 | NR | Reported that validated Spanish translations were used when available; otherwise translated and back-translated | Expert adjudication panel | NR | NR |
| TARCC | Bryant et al., 2013 | NR | NR | Clinical consensus | Ivnik et al. (1992) | No (0.2% Hispanic in normative sample) |
| Royall & Palmer, 2013 | NR | NR | NR in this paper (clinical consensus reported in other TARCC papers) | NR | NR | |
| Royall et al., 2014 | NR | NR | NR in this paper (clinical consensus reported in other TARCC papers) | NR | NR | |
| Royall & Palmer, 2016 | NR | NR | NR in this paper (clinical consensus reported in other TARCC papers) | NR | NR | |
| Royall & Palmer, 2017 | NR | NR | Clinical consensus | NR; notes that norms for MA are not available for many tests | NR | |
| Salazar et al., 2014 | Patient opinion of best performance | NR | Clinical consensus | NR | NR | |
| Salazar et al., 2016 | Patient opinion of best performance | NR | Clinical consensus | Ivnik et al. (1992) | No (0.2% Hispanic in normative sample) | |
| UC Davis ADC | DeCarli et al., 2008 | NR | NR | Clinical consensus. Must perform <10th percentile (age and education adjusted) in at least 1 cognitive domain. | NR | NR |
| Early et al., 2013 | Patient opinion of best performance | NR | Clinical consensus. Must perform <10th percentile (age and education adjusted) in at least 1 cognitive domain. | NR | NR | |
| Farias et al., 2005 | Patient preference if bilingual | Psychometric ally matched with IRT (SENAS) | Clinical consensus; test score < 10th percentile (demographically adjusted) | (Mungas et al., 2004) | Yes | |
| Farias et al., 2009 | NR | NR | Clinical consensus. impairment considered as approximately 1.5 SD below age- corrected norms; considering education and occupational background. | NR | NR | |
| Hinton et al., 2010 | NR | NR | Clinical consensus | NR | NR | |
| Miller et al., 2015 | NR | NR | “Standard criteria” | NR, but (Weintraub et al., 2009) referenced (non-Hispanic norms). | NR | |
| WHICAP | Blum et al., 2012 | Patient’s opinion of best performance (per Stern et al., 1992) | Translated & back-translated | NR; Manly et al. (2005) assumed | NR | NR |
| Devanand et al., 2010 | Patient’s opinion of best performance (per Manly et al., 2005) | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | Yes | |
| Gu et al., 2015 | Patient’s opinion of best performance (per Manly et al., 2005) | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | yes | |
| Luchsinger et al., 2007 | Patient’s opinion of best performance (per Manly et al., 2005) | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | Yes | |
| Manly et al., 2005 | Patient’s opinion of best performance | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Local, robust norms, based on age, education, sex, and ethnicity | Yes | |
| Manly et al., 2008 | Patient’s opinion of best performance | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | Yes | |
| Manly et al., 2011 | Patient’s opinion of best performance | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | Yes | |
| Rizvi et al., 2018 | Patient preference | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al. (2005) | Yes | |
| Scarmeas et al., 2009 | NR | Translated & back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment) | Manly et al. (2005) | Yes | |
| Zahodne et al., 2013 | NR | Translated and back-translated | Clinical consensus*; 1.5 SD normative cut-off for impairment | Manly et al., (2005) | Yes | |
| Women's Health Initiative- Memory Study | Goveas et al., 2016 | NR | NR | Neurologist diagnosis | NR | NR |
Note: ADC = Alzheimer’s Disease Center. ADRC = Alzheimer’s Disease Research Center. AMNART = American National Adult Reading Test. FRONTIER = Facing Rural Obstacles to Healthcare Now Through Intervention, Education & Research. HABLE =Health & Aging Brain among Latino Elders. NA = not applicable. NACC = National Alzheimer’s Disease Coordinating Center. NR = Not reported. NYU ADC = New York University Alzheimer’s Disease Center. SENAS = Spanish and English Neuropsychological Assessment Scales. SPS3 = The Secondary Prevention of Small Subcortical Strokes study. TARCC = Texas Alzheimer’s Research and Care Consortium. WAT = Word Accentuation Test. WHICAP = Washington Heights-Inwood Columbia Aging Project (WHICAP). WRAT = Wide Range Achievement Test.
Cited previous paper describing cohort as Mexican American.
Cited previous paper describing cohort as Caribbean Hispanic.
Diagnosis of dementia was ruled out through consensus conference
MCI classification was then performed through algorithm
Table 3.
Summary of results from 44 included manuscripts
| Variable | N (%) reported |
|---|---|
| Latinx sample characteristics | |
| Provided any information on region of origin | 25 (57%) |
| Mexican American | 14 (32%) |
| Specified countries of origin of combined sample | 3 (7%) |
| “Hispanic” only | 19 (43%) |
| “Hispanic” only; cited prior study describing region of origin | 8 (18%) |
| Nativity status | 2 (5%) |
| Number of years in US | 1 (2%) |
| Country of education | 0 (0%) |
| Reported literacy assessment - English | 7 (16%) |
| Reported literacy assessment- Spanish | 2 (5%) |
| Reported acculturation assessment | 0 (0%) |
| Linguistic functioning and language of testing | |
| Any information regarding language use/preference | 23 (52%) |
| Any assessment of language proficiency/preference | 1 (2%) |
| Reported proportion tested in English/Spanish | 13 (30%)a |
| Reported method to determine language for testing | 22 (50%) |
| Patient preference | 22 (100%)b |
| Method of test translation/adaptation | 15 (3%) |
| MCI Diagnosis method | |
| Clinical consensus method | 35 (80%) |
| Algorithm (no clinician diagnosis) | 3 (7%) |
| Otherc | 6 (14%) |
| Referenced specific normative cut-off for MCI | 20 (45%) |
| Reported source of normative data | 25 (57%) |
| Normative data included Latinx/validated in Latinx sample | 18 (72%)d |
Note:
43 studies considered; 1 study was methods paper.
considered the 22 studies that reported method of selection of testing language.
Other category was composed of clinician diagnosis.
considered the 25 studies that reported normative data source.
Synthesis of Results
Sample characteristics:
Less than two thirds (57%; n = 25 of 44) of studies provided any information on the region of origin of their Latinx sample, with the remaining studies (43%; n=19 of 44) of studies providing no information beyond the description of “Hispanic.” Of note, of the studies that described their sample as “Hispanic” (n = 19), a subset of these (n = 8) cited a prior study that provided additional information on the cohort’s region of origin. With regard to studies that did provide information on region of origin, 32% of all included studies (n = 14 of 44) described their sample as Mexican American, 7% (n = 3 of 44) described a sample with combined, specified countries of origin, and the remainder (18%; n = 8 of 44) provided information on region of origin but did not describe the specific countries of origin. Only two studies (5%; n = 2 of 44) provided information on the nativity status of Latinx participants, only 1 study reported number of years living in the US, and no studies described the countries of education of their sample. A minority (16%; n = 7 of 44) of studies reported completion of a literacy assessment in English, and only 2 of 44 (5%) reported completion of a literacy assessment in Spanish. No studies in this sample reported use of an acculturation assessment.
Linguistic functioning:
Half (52%; 23 of 44) of studies provided any information on language preference and use for their Latinx sample, and only one study reported use of an assessment of language proficiency or preference. Few studies (30%; n = 13 of 44) reported the proportion of their sample tested in English or Spanish. When a method was specified for determining the language to be used for testing (50% of studies; n = 22 of 44), all studies described using patient preference, and no studies reported use of an objective method. Thirty-four percent (n = 15 of 44) of included studies reported information regarding the method and/or source of neuropsychological test translation and/or adaptation.
MCI diagnostic method:
Most (80%; n = 35 of 44) of the studies reported use of clinical consensus method for MCI diagnosis, and the remainder reported use of an algorithm (7%; n = 3 of 44)) or other clinical assessment method (14%; n = 6 of 44). Nearly half of the studies (45%; n = 20 of 44) reported use of a specific normative cut-off for diagnosis of MCI. However, only 57% of studies (n = 25 of 44) reported the source of the normative data used to interpret neuropsychological data. Of the studies that reported the source of normative data, most(72%; n = 18 of 25) reported use of normative data that included Latinx individuals.
Exploratory analysis by publication year:
To investigate whether our findings differed by publication year, particularly in light of updates to MCI diagnostic criteria (DSM-5, Albert et al., 2011), we plotted each of our data items by publication year as an exploratory, qualitative analysis (Supplemental Figures 1 through 3). This analysis did not identify discernible trends by publication year for our data elements, particularly in light of the variable and limited number of studies published each year.
Discussion
The present scoping review sought to evaluate how relevant demographic, linguistic, and cultural factors are considered in neuropsychological diagnostic procedures for MCI in Latinx populations. This is the first scoping review of the literature on neuropsychological assessment of MCI in Latinx individuals, and the first paper to systematically evaluate how demographic, linguistic, and cultural factors are reported and considered when using neuropsychological assessment for as part of diagnosis of MCI in Latinx populations. Our analysis revealed considerable variability across studies with regard to reporting of Latinx sample characteristics, linguistic functioning, and methods for translation/adaptation and interpretation of neuropsychological tests for MCI diagnosis in Latinx individuals. Approximately half of studies reported the source of normative data used for determination of cognitive impairment, despite common use of a specific normative cut-off for classification of impairment for MCI diagnosis. Based upon these findings, it is difficult to ascertain the most important gaps in the science of MCI in Latinx individuals, the extent to which extant studies will generalize to various growing Latinx populations, and whether the neuropsychological assessment tools used for diagnosis result in differential diagnostic precision across ethnic groups.
Sample characteristics
We found that studies varied considerably in descriptions of their Latinx samples, with inconsistent reporting of relevant information such as immigration status, country of origin, country of education, literacy and acculturation. These Latinx populations may vary with regard to factors such as environmental and medical risk factors and associated resource needs for dementia risk reduction, symptom management, and caregiver support. Combining Latinx groups from various countries of origin, with different levels of acculturation and educational experience, may lead to unmeasured variance in neuropsychological test performance. This unmeasured variance may lead to erroneous attributions regarding ethnic differences in study outcomes, limiting hypothesis generation that may more precisely address research questions pertaining to cognitive health disparities (e.g., (Glymour & Manly, 2008). This may also lead to within-group variability in samples that tend to be differentially impacted by limited sample size. Finally, omission of this information limits feasibility to compare and synthesize findings across studies, particularly with methodologies such as systematic reviews and meta-analyses, and to identify knowledge gaps with regard to specific Latinx populations and/or specific contextual factors that are in need of further inquiry.
Linguistic functioning
Given that only 28% of Latinx individuals living in the US identify as monolingual English speakers, linguistic functioning in Latinx populations is of particular relevance. Bilinguals and monolinguals may also differ along other dimensions that may impact neuropsychological test performance, such as acculturation, length of time in the US, and SES. Although the question of whether and how bilingualism impacts the nature and trajectory of cognitive decline is unclear, many studies have found an impact of bilingualism on cross-sectional neuropsychological test performance (Zahodne et al., 2014), although this has not been entirely consistent (Early et al., 2018). If longitudinal data are not available for interpretation of neuropsychological tests for MCI diagnosis, the use of normative data is often the primary method used to infer cognitive decline. As such, bilingualism may impact MCI diagnostic validity when cross-sectional test performance is interpreted based on normative data for monolinguals (e.g., Gasquoine & Gonzalez, 2012).
Knowledge about bilingualism is also important for determining the language of neuropsychological test administration. Language of test administration is a relatively easy decision for those that are monolingual or strongly dominant in one language, although this determination becomes more complex for balanced bilinguals (Rivera Mindt et al., 2008). We found that individual preference was overwhelmingly reported as the method used for determining the language of testing. It is unclear whether self-reported preference is ideal, particularly when individuals present with age-related cognitive decline. Future research will be important to further clarify the most appropriate methods for determining language of test administration and their potential impact on cognitive test performance.
There are many challenges that may lead to barriers in the collection and reporting of Latinx sample characteristics. Time constraints often limit the amount of information that can be collected from each individual. Information about immigration status can be sensitive and thus may not be asked. Sample sizes of minority groups or sub-groups are often small, and it may be thus impossible to recruit sufficient numbers of individuals in order to appropriately analyze the impact of variables such as nativity status or country of origin. Due to limitations of neuropsychological assessment tools, information on specific demographic, educational, and cultural characteristics may not impact decisions on methodology (e.g., test selection) or analysis (due to limited sample size). Manuscript space limitations may also lead researchers to make difficult decisions regarding inclusion of this information. However, dissemination of this information from individual studies is important for generation of hypotheses, to facilitate synthesis of available evidence, and to continue to identify gaps in our knowledge of this population.
Neuropsychological assessment methods
Fewer than half of studies reported their method or source of test translation or cultural adaptation of tests. The method of translation and adaptation is a critical aspect of study design for readers to evaluate, as translations that were developed for individuals from different countries of origin may not be universally appropriate, particularly those developed in Spain versus Latin America. Methods of translation/adaptation may vary from publisher’s translations to local translations adapted specifically for the study population of interest. For example, there are several published Spanish language versions of the WAIS (e.g., Wechsler, 2001, 2003, 2008), with different adaptations and normative data. Selection of a test created for a different Latinx population may result in bias, or varying difficulty that is unrelated to the underlying cognitive ability being assessed. For example, words from test stimuli may be of differentially low frequency or have different meanings across different countries, and instructions adapted for a different Spanish-speaking country may be difficult to understand (e.g., Rivera Mindt et al., 2019). These factors may have a critical impact on test performance, and when the method of translation/adaptation is not reported, this aspect of the science remains unclear.
MCI diagnostic methods
Most studies used a clinical consensus method for diagnosis of MCI, whereas the remainder utilized algorithm or non-consensus-based clinical decisions. Less than two-thirds of studies reported the source of their normative data, despite relatively common use of a specific normative cut-off for diagnosis. When the source of normative data is not reported, readers cannot evaluate the appropriateness of these data and potential risk for false-positive errors. Of encouragement, most of the studies that reported use of normative data did report use of norms that included Latinx, and several have developed local demographically-corrected normative data (e.g., Manly et al., 2005; O’Bryant et al., 2018).
The neuropsychology literature has pointed to the importance of consideration of multivariate base rates of low scores in improving accuracy in classification of cognitive impairment. Studies have demonstrated that it is common, in the cognitively healthy older adult population, to obtain at least one cognitive test score in the impaired range when completing a comprehensive neuropsychological assessment (Brooks et al., 2017). The probability of obtaining at least one low score is impacted by education and culture (Brooks, Iverson, & White, 2007), and is common in some Spanish-speaking populations (e.g., (Diego Rivera et al., 2019). Attending to multivariate base rates of low scores may improve diagnostic precision in MCI (Oltra-Cucarella et al., 2018). As such, future work should consider the use of multivariate base rates of low scores in Latinx populations toward improved diagnostic precision for MCI. Taken together, each of these issues point to the complexity of accurately classifying MCI in minority populations. Diagnosis of MCI should incorporate the diverse cultural, sociodemographic, and linguistic characteristics of an individual. The diagnostic criteria for MCI have evolved since their inception to require consideration of cultural factors in interpreting neuropsychological data. It is unknown whether diagnostic approach (i.e., consensus-based versus algorithm) is of superior diagnostic accuracy for minority populations. When MCI is diagnosed with consensus conferences, consideration of cultural factors in rendering diagnosis is dependent upon the cultural competence of the clinicians performing the diagnosis. Similarly, the precision of an algorithm approach will be dependent upon the appropriateness of methods used to derive the algorithm. This may be a fruitful avenue for future work.
Clinical and research implications and future directions
Our findings have important implications for future clinical and research endeavors. More specific characterization of Latinx samples in research studies will aid clinicians in better evaluating whether particular research findings are relevant to their individual patient. Continued identification of the impact of contextual factors, including those identified in the present review, in addition to other factors (e.g., wealth/income, attitudes and beliefs about the assessment process and age-related cognitive changes) can aid clinicians working with minority populations in providing culturally appropriate care and improved diagnostic precision. These contextual factors should represent a critical component of the clinical conceptualization process, as has been summarized comprehensively elsewhere (Fujii, 2017, Fujii, 2018).
It is important to note that Latinx populations can be considered a vulnerable population, as they are at increased risk for poor health outcomes associated with social factors such as reduced access to health care (e.g., related to SES disparities, language barrier; Waisel, 2013). They may also be at increased risk for poorer quality of care related to a dearth of culturally competent health care providers (Rivera Mindt, Byrd, Saez, & Manly, 2010b). As such, it is critically important to better understand the expression and course of age-related cognitive disorders so as to better serve them. Future work can also be directed toward exploration of whether our findings generalize to assessment of MCI in other minority groups (e.g., Asian Americans) also with heterogeneous cultural and linguistic characteristics.
Our scoping review lays the groundwork for future systematic reviews and meta-analytic efforts focused on MCI in Latinx populations. Specifically, future systematic reviews addressing research questions regarding MCI in Latinx populations should now consider the absence of this important demographic and cultural information in the literature when considering the implications and generalizability of specific findings. In addition, future synthesis efforts may be thwarted by limited ability to understand to whom particular findings are applicable.
Limitations
We may have missed studies that are relevant to this area of inquiry. However, our search terms were broad and we feel that the present analysis reflects a representative sample of studies on MCI in Latinx individuals. Second, we did not include studies that utilized cognitive screening instruments to evaluate MCI in Latinx individuals. It is unclear whether our findings would generalize to studies that utilized cognitive screenings, although given that interpretation of cognitive screening instruments would also be impacted by the factors that we reviewed, we think that the implications of our findings would generalize to the use of cognitive screens. We also did not include studies on Latinx populations living outside of the US, so it is not clear whether our findings would generalize to those populations. This scoping review protocol was not pre-registered and a single reviewer performed the data extraction process. Finally, we analyzed the reporting of many of the most widely-reported factors that impact neuropsychological test interpretation, although there are other important contextual factors relevant to Latinx populations (e.g., income/wealth, attitudes/beliefs about testing) that were not included in this review.
Conclusions
Although Latinx populations are diverse along many dimensions important for interpretation of neuropsychological data (e.g., language use, nativity status), we found wide variability in the reporting of these factors in studies of MCI in Latinx populations. Increased detail is needed in reporting of neuropsychological assessment methodology for Latinx individuals, as this will lead to better identification of knowledge gaps in our understanding of MCI in these populations. Neuropsychological assessment for diagnosis of MCI in Latinx individuals is complex and complicated by a dearth of culturally appropriate neuropsychological assessment tools and normative data. As such, researchers must make difficult decisions about how to ascertain MCI diagnosis with tools that have generally not been developed and validated for this diverse and growing population. Efforts to develop psychometrically equivalent neuropsychological assessment tools (e.g., Mungas, Reed, Crane, Haan, & González, 2004) and generate local, robust normative data (e.g., Manly et al., 2005) are critical steps in continuing to develop culturally sound methods of cognitive assessment in these populations. We also recommend that future studies offer more detailed information regarding their Latinx samples and assessment methodology, and that manuscript space is allotted to report this information.
Supplementary Material
Key Points:
Question: Have studies described methods for accounting for demographic, cultural, and linguistic diversity when using neuropsychological assessment for mild cognitive impairment in Latinx populations?
Findings: Studies often do not report their methods for accounting for demographic, linguistic, and cultural diversity in assessment of MCI in Latinx individuals.
Importance: Increased detail is needed in reporting of neuropsychological assessment methodology for Latinx individuals, as this will lead to better identification of knowledge gaps in our understanding of MCI in these populations.
Next Steps: Future work is needed to further develop culturally appropriate neuropsychological assessment methods in Latinx populations.
Acknowledgments
Funded by:
National Institutes of Health
References
- Agranovich AV, Panter AT, Puente AE, & Touradji P (2011). The culture of time in neuropsychological assessment: Exploring the effects of culture-specific time attitudes on timed test performance in Russian and American samples. Journal of the International Neuropsychological Society, 17, 692–701. 10.1017/S1355617711000592 [DOI] [PubMed] [Google Scholar]
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, … Phelps CH (2011). The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s and Dementia. 10.1016/j.jalz.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Arango-Lasprilla JC, Rivera D, Aguayo A, Rodríguez W, Garza MT, Saracho CP, … Perrin PB (2015). Trail Making Test: Normative data for the Latin American Spanish speaking adult population. NeuroRehabilitation, 37, 639–661. 10.3233/NRE-151284 [DOI] [PubMed] [Google Scholar]
- Ardila A (2005). Cultural values underlying psychometric cognitive testing. Neuropsychology Review, 15, 185–195. 10.1007/s11065-005-9180-y [DOI] [PubMed] [Google Scholar]
- Ardila A, Bertolucci PH, Braga LW, Castro-Caldas A, Judd T, Kosmidis MH, … Rosselli M (2010). Illiteracy: The neuropsychology of cognition without reading. Archives of Clinical Neuropsychology, 25, 689–712. 10.1093/arclin/acq079 [DOI] [PubMed] [Google Scholar]
- Arentoft A, Byrd D, Robbins RN, Monzones J, Miranda C, Rosario A, … Rivera Mindt M (2012). Multidimensional effects of acculturation on English-language neuropsychological test performance among HIV+ Caribbean Latinas/os. Journal of Clinical and Experimental Neuropsychology, 34, 814–825. 10.1080/13803395.2012.683856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bialystok E, Abutalebi J, Bak TH, Burke DM, & Kroll JF (2016). Aging in two languages: Implications for public health. Ageing Research Reviews, 27, 56–60. 10.1016/j.arr.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum S, Luchsinger JA, Manly JJ, Schupf N, Stern Y, Brown TR, … Brickman AM (2012). Memory after silent stroke: Hippocampus and infarcts both matter. Neurology, 78, 38–46. 10.1212/WNL.0b013e31823ed0cc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks BL, Iverson GL, & White T (2007). Substantial risk of “Accidental MCI” in healthy older adults: Base rates of low memory scores in neuropsychological assessment. Journal of the International Neuropsychological Society, 13, 490–500. 10.1017/S1355617707070531 [DOI] [PubMed] [Google Scholar]
- Cagigas XE, & Manly JJ (2014). Cultural neuropsychology: The new norm. In Clinical neuropsychology: A pocket handbook for assessment (3rd ed.). (pp. 132–156). Washington DC: American Psychological Association. 10.1037/14339-008 [DOI] [Google Scholar]
- De Santi S, Pirraglia E, Barr W, Babb J, Williams S, Rogers K, … de Leon MJ (2008). Robust and Conventional Neuropsychological Norms: Diagnosis and Prediction of Age-Related Cognitive Decline. Neuropsychology, 22, 469–484. 10.1037/0894-4105.22.4.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeCarli C, Reed BR, Jagust W, Martinez O, Ortega M, & Mungas D (2008). Brain behavior relationships among African Americans, whites, and Hispanics. Alzheimer Disease and Associated Disorders, 22, 382–391. 10.1097/WAD.0b013e318185e7fe [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devanand DP, Tabert MH, Cuasay K, Manly JJ, Schupf N, Brickman AM, … Mayeux R (2010). Olfactory identification deficits and MCI in a multi-ethnic elderly community sample. Neurobiology of Aging, 31, 1593–1600. 10.1016/j.neurobiolaging.2008.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhamoon MS, McClure LA, White CL, Lakshminarayan K, Benavente OR, & Elkind MSV (2015). Long-term disability after lacunar stroke: Secondary prevention of small subcortical strokes. Neurology, 84, 1002–1008. 10.1212/wnl.0000000000001331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duara R, Loewenstein DA, Lizarraga G, Adjouadi M, Barker WW, Greig-Custo MT, … ST DK (2019). Effect of age, ethnicity, sex, cognitive status and APOE genotype on amyloid load and the threshold for amyloid positivity. NeuroImage: Clinical, 22. 10.1016/j.nicl.2019.101800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Early DR, Widaman KF, Harvey D, Beckett L, Park LQ, Farias ST, … Mungas D (2013). Demographic predictors of cognitive change in ethnically diverse older persons. Psychology and Aging, 28, 633–645. 10.1037/a0031645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estanga A, Ecay-Torres M, Ibañez A, Izagirre A, Villanua J, Garcia-Sebastian M, … Martinez-Lage P (2017). Beneficial effect of bilingualism on Alzheimer’s disease CSF biomarkers and cognition. Neurobiology of Aging, 50, 144–151. 10.1016/j.neurobiolaging.2016.10.013 [DOI] [PubMed] [Google Scholar]
- Flores Antonio. (2017). Facts on Latinos in America | Pew Research Center. Retrieved July 25, 2019, from https://www.pewhispanic.org/2017/09/18/facts-on-u-s-latinos/#hispanic-pop [Google Scholar]
- Farias ST, Mungas D, & Jagust W (2005). Degree of discrepancy between self and other-reported everyday functioning by cognitive status: Dementia, mild cognitive impairment, and healthy elders. International Journal of Geriatric Psychiatry, 20, 827–834. 10.1002/gps.1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias ST, Mungas D, Reed BR, Harvey D, & Decarli C (2009). Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Archives of Neurology, 66, 1151–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasfous AF, Hidalgo-Ruzzante N, Vilar-Lopez R, Catena-Martinez A, & Perez-Garcia M (2013). Cultural differences in neuropsychological abilities required to perform intelligence tasks. Archives of Clinical Neuropsychology, 28, 784–790. 10.1093/arclin/act074 [DOI] [PubMed] [Google Scholar]
- Fujii D (2017). Conducting a culturally-informed neuropsychological assessment. Washington DC: American Psychological Association. [Google Scholar]
- Fujii D (2018). Developing a cultural context for conducting a neuropsychological evaluation with a culturally diverse client: the ECLECTIC framework. The Clinical Neuropsychologist, 32, 1356–1392. 10.1080/13854046.2018.1435826 [DOI] [PubMed] [Google Scholar]
- Gasquoine Philip G. (1999). Variables moderating cultural and ethnic differences in neuropsychological assessment: The case of Hispanic Americans. The Clinical Neuropsychologist, 13, 376–383. 10.1076/clin.13.3.376.1735 [DOI] [PubMed] [Google Scholar]
- Gasquoine Philip Gerard, & Gonzalez CD (2012). Using monolingual neuropsychological test norms with bilingual Hispanic Americans: Application of an individual comparison standard. Archives of Clinical Neuropsychology, 27, 268–276. 10.1093/arclin/acs004 [DOI] [PubMed] [Google Scholar]
- Glymour MM, & Manly JJ (2008). Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review, 18, 223–254. 10.1007/s11065-008-9064-z [DOI] [PubMed] [Google Scholar]
- Gollan TH, Fennema-Notestine C, Montoya RI, & Jernigan TL (2007). The bilingual effect on Boston Naming Test performance. Journal of the International Neuropsychological Society, 13, 197–208. 10.1017/S1355617707070038 [DOI] [PubMed] [Google Scholar]
- Gollan TH, Salmon DP, Montoya RI, & Galasko DR (2011). Degree of bilingualism predicts age of diagnosis of Alzheimer’s disease in low-education but not in highly educated Hispanics. Neuropsychologia, 49, 3826–3830. 10.1016/j.neuropsychologia.2011.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goveas JS, Rapp SR, Hogan PE, Driscoll I, Tindle HA, Smith JC, … Resnick SM (2016). Predictors of Optimal Cognitive Aging in 80 + Women : The Women’s Health Initiative Memory Study. 71, 62–71. 10.1093/gerona/glv055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y, Brickman AM, Stern Y, Habeck CG, Razlighi QR, Luchsinger JA, … Scarmeas N (2015). Mediterranean diet and brain structure in a multiethnic elderly cohort. Neurology, 85, 1744–1751. 10.1212/WNL.0000000000002121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero-Berroa E, Kluger A, Schmeidler J, Sailor K, Lizardi H, Golomb J, … Reisberg B (2014). Neuropsychological and neuropsychiatric prediction of global cognitive status among older Spanish-speaking Hispanics and English-speaking whites. Journal of Geriatric Psychiatry and Neurology, 27, 266–275. 10.1177/0891988714532020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton L, Carter K, Reed BR, Beckett L, Lara E, Decarli C, & Mungas D (2010). Recruitment of a community-based cohort for research on diversity and risk of dementia. Alzheimer Disease and Associated Disorders, 24, 234–241. 10.1097/WAD.0b013e3181c1ee01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh Q-L, Howell RT, & Benet-Martínez V (2009). Reliability of bidimensional acculturation scores: A meta-analysis. Journal of Cross-Cultural Psychology, 40, 256–274. 10.1177/0022022108328919 [DOI] [Google Scholar]
- Ivnik RJ, Malec JF, Smith GE, Tangalos EG, Petersen RC, Kokmen E, & Kurland LT (1992). Mayo’s older americans normative studies: WAIS-R norms for ages 56 to 97. Clinical Neuropsychologist, 6(sup001), 1–30. 10.1080/13854049208401877 [DOI] [Google Scholar]
- Jacova C, Pearce LA, Roldan AM, Arauz A, Tapia J, Costello R, … Benavente OR (2015). Cognitive performance following lacunar stroke in Spanish-speaking patients : results from the SPS3 trial. International Journal of Stroke, 10, 519–528. 10.1111/ijs.12511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson LA, Cushing B, Rohlfing G, Edwards M, Davenloo H, D’Agostino D, … O’Bryant SE (2014). The Hachinski Ischemic Scale and cognition: The influence of ethnicity. Age and Ageing, 43, 364–369. 10.1093/ageing/aft189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson LA, Edwards M, Gamboa A, Hall J, Robinson M, & O’Bryant SE (2017). Depression, inflammation, and memory loss among Mexican Americans: Analysis of the HABLE cohort. International Psychogeriatrics, 29, 1693–1699. 10.1017/S1041610217001016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson LA, Gamboa A, Vintimilla R, Cheatwood AJ, Grant A, Trivedi A, … O’Bryant SE (2015). Comorbid depression and diabetes as a risk for Mild Cognitive Impairment and Alzheimer’s disease in elderly Mexican Americans. Journal of Alzheimer’s Disease, 47, 129–136. 10.3233/JAD-142907 [DOI] [PubMed] [Google Scholar]
- Johnson LA, Gamboa A, Vintimilla R, Edwards M, Hall J, Weiser B, … O’Bryant SE (2016). A depressive endophenotype for predicting cognitive decline among Mexican American adults and elders. Journal of Alzheimer’s Disease, 54, 201–206. 10.3233/JAD-150743 [DOI] [PubMed] [Google Scholar]
- Johnson LA, Mauer C, Jahn D, Song M, Wyshywaniuk L, Hall JR, … O’Bryant SE (2013). Cognitive differences among depressed and non-depressed MCI participants: A project FRONTIER study. International Journal of Geriatric Psychiatry, 28, 377–382. 10.1002/gps.3835 [DOI] [PubMed] [Google Scholar]
- Johnson Leigh Ann, Large SE, Izurieta Munoz H, Hall JR, & O’Bryant SE (2019). Vascular depression and cognition in Mexican Americans. Dementia and Geriatric Cognitive Disorders, 47, 68–78. 10.1159/000494272 [DOI] [PubMed] [Google Scholar]
- Judd T, Capetillo D, Carrión-Baralt J, Mármol LM, San Miguel-Montes L, Navarrete MG, … Committee NP and P. (2009). Professional considerations for improving the neuropsychological evaluation of Hispanics: A National Academy of Neuropsychology Education Paper. Archives of Clinical Neuropsychology, 24, 127–135. 10.1093/arclin/acp016 [DOI] [PubMed] [Google Scholar]
- Krch D, Lequerica A, Arango-Lasprilla JC, Rogers HL, Deluca J, & Chiaravalloti ND (2015). The multidimensional influence of acculturation on Digit Symbol-Coding and Wisconsin Card Sorting Test in Hispanics. Clinical Neuropsychologist, 29, 624–638. 10.1080/13854046.2015.1063696 [DOI] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Bigler ED, & Tranel D (2012). Neuropsychological assessment (5th Edition). New York: Oxford University Press. [Google Scholar]
- Loewenstein DA, Argüelles T, Argüelles S, & Linn-fuentes P (1994). Potential cultural bias in the neuropsychological assessment of the older adult. Journal of Clinical and Experimental Neuropsychology, 16, 623–629. 10.1080/01688639408402673 [DOI] [PubMed] [Google Scholar]
- Luchsinger JA, Patel B, Tang M-X, Manly JJ, Mayeux R, & Reitz C (2007). Relation of diabetes to mild cognitive impairment. Archives of Neurology, 64, 570–575. 10.1001/archneur.64.4.570 [DOI] [PubMed] [Google Scholar]
- Manly JJ, Bell-McGinty S, Tang MX, Schupf N, Stern Y, & Mayeux R (2005). Implementing diagnostic criteria and estimating frequency of mild cognitive impairment in an urban community. Archives of Neurology, 62, 1739–1746. 10.1001/archneur.62.11.1739 [DOI] [PubMed] [Google Scholar]
- Manly JJ, Jacobs DM, Touradji P, Small SA, & Stern Y (2002). Reading level attenuates differences in neuropsychological test performance between African American and White elders. Journal of the International Neuropsychological Society, 8, 341–348. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11939693 [DOI] [PubMed] [Google Scholar]
- Manly JJ, Schupf N, Stern Y, Brickman AM, Tang MX, & Mayeux R (2011). Telephone-based identification of mild cognitive impairment and dementia in a multicultural cohort. Archives of Neurology, 68, 607–614. 10.1001/archneurol.2011.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JPG, & Mayeux R (2008). Frequency and course of mild cognitive impairment in a multiethnic community. Annals of Neurology, 63, 494–506. 10.1002/ana.21326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcclendon MJ, Hernandez S, Smyth KA, & Lerner AJ (2009). Memantine and Acetylcholinesterase Inhibitor Treatment in Cases of CDR 0.5 or Questionable Impairment. Journal of Alzheimer’s Disease, 16, 577–583. 10.3233/JAD-2009-0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milani SA, Marsiske M, Cottler LB, Chen X, & Striley CW (2018). Optimal cutoffs for the Montreal Cognitive Assessment vary by race and ethnicity. Alzheimer’s and Dementia: Diagnosis, Assessment and Disease Monitoring, 10, 773–781. 10.1016/j.dadm.2018.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JW, Harvey DJ, Beckett LA, Green R, Farias ST, Reed BR, … De Carli C (2015). Vitamin D status and rates of cognitive decline in a multiethnic cohort of older adults. JAMA Neurology, 72, 1295–1303. 10.1001/jamaneurol.2015.2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda C, Rentería MA, Fuentes A, Coulehan K, Arentoft A, Byrd D, … Arce Rentería M (2016). The relative utility of three English language dominance measures in predicting the neuropsychological performance of HIV+ bilingual Latino/a adults. The Clinical Neuropsychologist, 30, 185–200. 10.1080/13854046.2016.1139185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mungas D, Reed BR, Crane PK, Haan MN, & González H (2004). Spanish and English Neuropsychological Assessment Scales (SENAS): Further development and psychometric characteristics. Psychological Assessment, 16, 347–359. 10.1037/1040-3590.16.4.347 [DOI] [PubMed] [Google Scholar]
- Mungas D, Reed BR, Haan MN, & Gonzalez H (2005). Spanish and English Neuropsychological Assessment Scales: Relationship to demographics, language, cognition, and independent function. Neuropsychology, 19, 466–475. 10.1037/0894-4105.19.4.466 [DOI] [PubMed] [Google Scholar]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, & Aromataris E (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18, 143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musu-Gillette L, de Brey C, McFarland J, Hussar W, Sonnenberg W, & Wilkinson-Flicker S (2017). Status and Trends in the Education of Racial and Ethnic Groups 2017. Retrieved from https://nces.ed.gov/pubs2017/2017051.pdf
- O’Bryant SE, Edwards M, Johnson L, Hall J, Gamboa A, & O’jile J (2018). Texas Mexican American adult normative studies: Normative data for commonly used clinical neuropsychological measures for English- and Spanish-speakers. Developmental Neuropsychology, 43, 1–26. 10.1080/87565641.2017.1401628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Bryant SE, Johnson L, Balldin V, Edwards M, Barber R, Williams B, … Hall J (2013). Characterization of Mexican Americans with mild cognitive impairment and Alzheimer’s disease. Journal of Alzheimer’s Disease, 33, 373–379. 10.3233/JAD-2012-121420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Bryant SEO, Johnson L, Edwards M, Soares H, & Devous MD (2013). The Link Between C-Reactive Protein and Alzheimer ‘ s Disease Among Mexican Americans. Journal of Alzheimer’s Disease, 34, 701–706. 10.3233/JAD-122071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Bryant SE, Johnson L, Reisch J, Edwards M, Hall J, Barber R, … Singh M (2013). Risk factors for mild cognitive impairment among Mexican Americans. Alzheimer’s and Dementia, 9, 622–631.e1. 10.1016/j.jalz.2012.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oltra-Cucarella J, Sánchez-SanSegundo M, Lipnicki DM, Sachdev PS, Crawford JD, Pérez-Vicente JA, … Ferrer-Cascales R (2018). Using base rate of low scores to identify progression from amnestic Mild Cognitive Impairment to Alzheimer’s Disease. Journal of the American Geriatrics Society, 66, 1360–1366. 10.1111/jgs.15412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandya SY, Lacritz LH, Deschner M, Woon FL, & Weiner MF (2017). Predictors of Reversion from Mild Cognitive Impairment to Normal Cognition. Dementia and Geriatric Cognitive Disorders, 42, 204–214. 10.1159/000456070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce LA, McClure LA, Anderson DC, Jacova C, Sharma M, Hart RG, & Benavente OR (2014). Effects of long-term blood pressure lowering and dual antiplatelet treatment on cognitive function in patients with recent lacunar stroke: A secondary analysis from the SPS3 randomised trial. The Lancet Neurology, 13, 1177–1185. 10.1016/S1474-4422(14)70224-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, & Soares CB (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13, 141–146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, … Winblad B (2001). Current concepts in Mild Cognitive Impairment. Archives of Neurology, 58(12), 1985. 10.1001/archneur.58.12.1985 [DOI] [PubMed] [Google Scholar]
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, & McEwen SA (2014). A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Research Synthesis Methods, 5, 371–385. 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razani J, Burciaga J, Madore M, & Wong J (2007). Effects of acculturation on tests of attention and information processing in an ethnically diverse group. Archives of Clinical Neuropsychology, 22, 333–341. 10.1016/j.acn.2007.01.008 [DOI] [PubMed] [Google Scholar]
- Rivera D, & Arango-Lasprilla JC (2017). Methodology for the development of normative data for Spanish-speaking pediatric populations. NeuroRehabilitation, 41, 581–592. 10.3233/NRE-172275 [DOI] [PubMed] [Google Scholar]
- Rivera Diego, Olabarrieta-Landa L, Brooks BL, Ertl MM, Benito-Sánchez I, Quijano MC, … Arango-Lasprilla JC (2019). Multivariate Base Rates of Low Scores on Tests of Learning and Memory among Latino Adult Populations. Journal of the International Neuropsychological Society, 25, 834–844. 10.1017/S135561771900050X [DOI] [PubMed] [Google Scholar]
- Rivera Mindt M, Arentoft A, Coulehan K, Summers AC, Tureson K, Aghvinian M, & Byrd DA (2019). Neuropsychological Evaluation of Culturally/Linguistically Diverse Older Adults. In Ravdin L & Katzen H (Eds.), Handbook on the Neuropsychology of Aging and Dementia, Second Edition (pp. 25–48). New York: Springer. 10.1007/978-3-319-93497-6_3 [DOI] [Google Scholar]
- Rivera Mindt M, Arentoft A, Kubo Germano K, D’Aquila E, Scheiner D, Pizzirusso M, … Gollan TH (2008). Neuropsychological, cognitive, and theoretical considerations for evaluation of bilingual individuals. Neuropsychology Review, 18, 255–268. 10.1007/s11065-008-9069-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera Mindt M, Byrd D, Saez P, & Manly J (2010a). Increasing Culturally Competent Neuropsychological Services for Ethnic Minority Populations: A Call to Action. The Clinical Neuropsychologist, 24, 429–453. 10.1080/13854040903058960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera Mindt M, Byrd D, Saez P, & Manly J (2010b). Increasing Culturally Competent Neuropsychological Services for Ethnic Minority Populations: A Call to Action. The Clinical Neuropsychologist, 24, 429–453. 10.1080/13854040903058960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi B, Narkhede A, Last BS, Budge M, Tosto G, Manly JJ, … Brickman AM (2018). The effect of white matter hyperintensities on cognition is mediated by cortical atrophy. Neurobiology of Aging, 64, 25–32. 10.1016/j.neurobiolaging.2017.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero HR, Lageman SK, Kamath VV, Sim A, Suarez P, Manly JJ, … Attix DK (2009). Challenges in the Neuropsychological Assessment of Ethnic Minorities : Summit Proceedings. The Clinical Neuropsychologist, 23, 761–779. 10.1080/13854040902881958 [DOI] [PubMed] [Google Scholar]
- Rose KM (2005). Mild cognitive impairment in Hispanic Americans: An overview of the state of the science. Archives of Psychiatric Nursing, 19, 205–209. 10.1016/j.apnu.2005.07.002 [DOI] [PubMed] [Google Scholar]
- Rosselli M, Loewenstein DA, Curiel RE, Penate A, Torres VL, Lang M, … Duara R (2019). Effects of bilingualism on verbal and nonverbal memory measures in mild cognitive impairment. Journal of the International Neuropsychological Society, 25, 15–28. 10.1017/S135561771800070X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royall DR, Palmer RF (2014). Does ethnicity moderate dementia’s biomarkers? Neurobiology of Aging, 35, 336–344. 10.1016/j.neurobiolaging.2013.08.006 [DOI] [PubMed] [Google Scholar]
- Royall DR, & Palmer RF (2013). Validation of a latent construct for dementia case-finding in Mexican-Americans. Journal of Alzheimer’s Disease, 37, 89–97. 10.3233/JAD-130353 [DOI] [PubMed] [Google Scholar]
- Royall Donald R, & Palmer RF (2016). Thrombopoietin is associated with d ‘ s intercept, and only in Non-Hispanic Whites. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 3, 35–42. 10.1016/j.dadm.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royall Donald R, & Palmer RF (2017). d scores predict mild cognitive impairment and Alzheimer’s disease conversions from nondemented states. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 6, 214–221. 10.1016/j.dadm.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar R, Dwivedi AK, & Royall DR (2016). Cross-Ethnic Differences in the Severity of Neuropsychiatric Symptoms in Persons With Mild Cognitive Impairment and Alzheimer’s Disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 29, 13–21. 10.1176/appi.neuropsych.15120423 [DOI] [PubMed] [Google Scholar]
- Salazar R, Velez CE, & Royall DR (2014). Telephone screening for mild cognitive impairment in hispanics using the Alzheimers Questionnaire. Experimental Aging Research, 40, 129–139. 10.1080/0361073X.2014.882189 [DOI] [PubMed] [Google Scholar]
- Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, & Luchsinger JA (2009). Mediterranean diet and mild cognitive impairment. Archives of Neurology, 66, 216–225. 10.1001/archneurol.2008.536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirk S, Mitchell M, Shaughnessy L, Sherman J, Locascio J, Weintraub S, & Atri A (2011). A web-based normative calculator for the uniform data set (UDS) neuropsychological test battery. Alzheimer’s Research and Therapy, 3, 32. 10.1186/alzrt94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisco S, Gross AL, Shih RA, Sachs BC, Glymour MM, Bangen KJ, … Manly JJ (2015). The role of early-life educational quality and literacy in explaining racial disparities in cognition in late life. Journals of Gerontology - Series B Psychological Sciences and Social Sciences, 70, 557–567. 10.1093/geronb/gbt133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern Y, Gu Y, Cosentino S, Azar M, & Lawless S (2017). The Predictors study : Development and baseline characteristics of the Predictors 3 cohort. Alzheimer’s & Dementia, 13, 20–27. 10.1016/j.jalz.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szerlip HM, Edwards ML, Williams BJ, Johnson LA, Vintimilla RM, & O’Bryant SE (2015). Association between cognitive impairment and chronic kidney disease in Mexican Americans. Journal of the American Geriatrics Society, 63(10), 2023–2028. 10.1111/jgs.13665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, … Straus SE (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine, 169, 467. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- US Census Bureau. About Hispanic Origin. Retrieved July 25, 2019, from https://www.census.gov/topics/population/hispanic-origin/about.html
- Vincent GK, & Velkoff VA (2010). The Older Population in the United States : 2010 to 2050, population estimates and projections. In Current population reports: Population estimates and projections (Vol. P25–1138, pp. 1–16). Retrieved from http://www.census.gov/content/dam/Census/library/publications/2010/demo/p25-1138.pdf [Google Scholar]
- Waisel DB (2013). Vulnerable populations in healthcare. Current Opinion in Anaesthesiology, 26, 186–192. 10.1097/ACO.0b013e32835e8c17 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2001). WAIS–III: Escala de Inteligencia Wechsler Para Adultos—III. (Ediciones T, Ed.). Madrid, Spain. [Google Scholar]
- Wechsler D (2003). Escala Wechsler de Inteligencia para Adultos-III. Mexico City: Manual Moderno. [Google Scholar]
- Wechsler D (2008). Escala de Inteligencia Wechsler Para Adultos— Tercera Edicion (EIWA–III). San Antonio, TX: Pearson. [Google Scholar]
- Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, … Morris JC (2009). The Alzheimer’s Disease Centers’ Uniform Data Set (UDS): The neuropsychologic test battery. Alzheimer Disease and Associated Disorders, 23, 91–101. 10.1097/WAD.0b013e318191c7dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, … Wright CB (2019). Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA - Journal of the American Medical Association, 321, 553–561. 10.1001/jama.2018.21442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Manly JJ, Brickman AM, Siedlecki KL, Decarli C, & Stern Y (2013). Quantifying cognitive reserve in older adults by decomposing episodic memory variance: Replication and extension. Journal of the International Neuropsychological Society, 19, 854–862. 10.1017/S1355617713000738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Schofield PW, Farrell MT, Stern Y, & Manly JJ (2014). Bilingualism does not alter cognitive decline or dementia risk among Spanish-speaking immigrants. Neuropsychology, 28, 238–246. 10.1037/neu0000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


