Abstract
BACKGROUND & AIMS:
Depression and anxiety can have negative effects on patients and are important to treat. There have been few studies of their prevalence among patients with cirrhosis. We aimed to characterize the prevalence and risk factors for depression and anxiety in a large multi-center cohort of patients with cirrhosis.
METHODS:
We conducted a telephone-based survey of patients with cirrhosis at 3 health systems in the United States (a tertiary-care referral center, a safety net system, and a Veterans hospital) from April through December 2018. Of 2871 patients approached, 1021 (35.6%) completed the survey. Depression and anxiety were assessed using the PHQ-9 (range 0–25) and STAI (range 20–80) instruments, with clinically significant values defined as PHQ-9 ≥15 and STAI ≥40. We performed multivariate logistic regression analysis to identify factors associated with significant depression and anxiety.
RESULTS:
The median PHQ-9 score was 7 (25th percentile–75th percentile, 3–12) and the median STAI score was 33 (25th percentile–75th percentile, 23–47); 15.6% of patients had moderately severe to severe depression and 42.6% of patients had high anxiety. In multivariable analyses, self-reported poor health (odds ratio [OR], 4.08; 95% CI, 1.79–9.28), being widowed (OR, 2.08; 95% CI, 1.07–4.05), fear of hepatocellular carcinoma (OR, 1.89; 95% CI, 1.04–3.42), higher household income (OR, 0.30; 95% CI, 0.10–0.95), and Hispanic ethnicity (OR, 0.57; 95% CI, 0.33–0.97) were associated with moderately severe to severe depression. Male sex (OR, 0.71; 95% CI, 0.51–0.98), self-reported poor health (OR, 2.73; 95% CI, 1.73–4.32), and fear of hepatocellular carcinoma (OR, 2.24; 95% CI, 1.33–3.78) were associated with high anxiety.
CONCLUSIONS:
Nearly 1 in 6 patients with cirrhosis have moderately severe to severe depression and nearly half have moderate–severe anxiety. Patients with cirrhosis should be evaluated for both of these disorders.
Keywords: Psychiatric Illness, Liver Disease, Comorbidity, Cirrhosis, Depression, Anxiety
Cirrhosis is a common cause of morbidity and mortality, ranking as the 12th leading cause of death overall in the United States.1 Irrespective of cause, chronic liver damage can lead to the development of cirrhosis—a major risk factor for hepatocellular carcinoma and need for liver transplantation.1 Viral hepatitis, nonalcoholic steatohepatitis (NASH), and alcohol use are major causes of chronic liver disease in the United States and Europe.2 Worldwide, 2 billion people are either overweight or obese,3 over 400 million suffer from diabetes,4 and harmful use of alcohol results in 5.3% of all global deaths5—all of which are risk factors for chronic liver disease and cirrhosis.6
These predisposing risk factors are frequently associated with mental health disorders. For example, anxiety and depression are reported in 11.1% and 33% of patients with alcohol use disorders, respectively7; similarly, intravenous drug use is associated with depression in 7.3% and anxiety in 2.9% of patients.8 Depression and anxiety not only play a crucial role in a decreased health-related quality of life in patients with chronic diseases,9 but also can affect many aspects of care, including adherence to medical appointments, medications, and engagement with social risk behaviors (alcohol and drugs).10–12 Estimates for the prevalence of depression and anxiety are best known in patients with decompensated cirrhosis and liver transplant candidates13,14; however, the burden of these mental health disorders in a broad cirrhosis patient population, particularly across different health care settings, is lacking. Therefore, we aimed to study the prevalence and risk factors associated with the presence of depression and anxiety in a diverse, outpatient cohort with well-compensated cirrhosis followed in 3 different types of health systems in the United States.15
Materials And Methods
Study Population
We included adult patients, ≥18 years of age, with cirrhosis of any etiology from any of the 3 participating centers: Parkland Health and Hospital System (Parkland), University of Texas Southwestern Medical Center (UTSW), and Michael E. DeBakey Veterans Affairs (VA) Medical Center (MEDVAMC). Parkland is an integrated county health system that offers a sliding-fee scale program, providing access to primary and subspecialty medical services, including hepatocellular carcinoma (HCC) screening and treatment for Dallas County residents. UTSW is an academic tertiary care referral health system, with a large liver transplantation program. The MEDVAMC is one of the largest VA medical centers, with hepatology subspecialty clinics and serves as a liver transplantation center for veterans in the United States. All 3 sites have a comprehensive electronic medical record (EMR) system for inpatient and outpatient visits and have access to subspecialty care, including hepatology and mental health services.
Patients were identified by a validated EMR case identification algorithm based on International Classification of Diseases–Ninth Revision (ICD-9) or International Classification of Diseases–Tenth Revision (ICD-10) codes for cirrhosis (571.2 or 571.5; K70.30 or K74.6) or cirrhosis complications (456.0, 456.1, 456.2, 456.21, 567.23, 572.2, 572.3, 572.4; K65.2, K72.9, K72.91, K76.6, K76.7, I85.0, I85.1).16–18 In addition, we included patients with an aspartate aminotransferase-to-platelet ratio ≥1.5, which has been shown to have an area under the receiver-operating curve of 0.94 to predict cirrhosis.19 All cases with cirrhosis were confirmed with chart-validation by 2 transplant hepatologists (R.H., A.G.S.) and disagreements were resolved by consensus. We excluded patients with a history of HCC, liver transplantation, presence of active cancer, enrolled in palliative care, Child-Turcotte-Pugh class C cirrhosis, or incarceration. We also excluded patients without known physical address or phone number and those with language other than English or Spanish. The study was approved by the UTSW and VA/Baylor College of Medicine institutional review boards.
Depression and Anxiety
As previously described,20 participants eligible for the study were invited via letter and called thereafter to inquire their willingness to participate and conduct the baseline survey between April and December 2018, with a maximum of 6 call attempts. We assessed depressive symptoms with the Patient Health Questionnaire-9 (PHQ-9),21 which is accurate for grading depression severity and sensitive to changes over time, including in patients with cirrhosis.22,23 PHQ-9 scores range from 0 to 25, with moderately severe depression defined as a PHQ-9 score of 15–19 and severe depression defined as a PHQ-9 score ≥20. We used a threshold of a PHQ-9 score ≥15 (ie, moderately severe to severe depression) as our outcome of interest, as treatment evaluation is recommended for this degree of depression, independent of duration and functional impairment. Anxiety was assessed using State–Trait Anxiety Inventory (STAI), which has been used in breast, colon, and lung cancer screening programs24–26 and in patients with cirrhosis.27 The STAI ranges from 20 to 80, with moderate–severe anxiety defined as score ≥40.
We collected demographics and clinical history through the EMR. Patient age, sex, race and ethnicity, preferred language, and type of insurance were obtained. Liver disease etiology was classified using laboratory data and ICD-9 and ICD–10 codes into the following categories: hepatitis C virus, hepatitis B virus, alcohol-related liver disease, NASH, and other. Ascites and hepatic encephalopathy were ascertained using ICD-9 and ICD-10 codes and medications using a validated algorithm and classified as none, mild or controlled, and severe or uncontrolled.28
Statistical Analyses
We compared baseline characteristics across the 3 different sites and used parametric and nonparametric tests depending on the normality distribution of the data. For survey questions with missing data, we performed single imputation using the mean of the patient’s responses from similar survey items. To characterize variables independently associated with moderately severe to severe depression and moderate–severe anxiety, we used multivariable logistic regression to estimate prevalence odds ratios and 95% confidence intervals. Models were adjusted for study site and clinically meaningful factors that could act as confounders (eg, age, sex, language). For all analyses, statistical significance was defined as P < .05. All data analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Results
Patient Population
Of 2875 patients with cirrhosis who met inclusion criteria, 1021 (35.5%) completed the baseline survey: 629 at Parkland, 155 at UTSW, and 237 at MEDVAMC (Table 1). The median age was 61 years, and 63.9% (n = 649) were men. The cohort was racially and ethnically diverse, with 35.2% non-Hispanic White, 28.6% non-Hispanic Black, and 33.4% Hispanic White. The most common etiologies for cirrhosis were hepatitis C virus at Parkland and the MEDVAMC (60.9% and 76.9%, respectively) and NASH at UTSW (30.3%). Over three-fourths of participants at each site had Child-Pugh-Turcotte A cirrhosis. Health status was reported as excellent in 11.9%, 16.8%, and 17.4% at Parkland, UTSW, and MEDVAMC respectively, and reported as fair/poor in 58.5% at Parkland, compared with 44.5% at the MEDVAMC and 38.7% at UTSW. As previously published,20 survey respondents had similar clinical characteristics compared with survey nonrespondents, although respondents had a higher proportion of women and Hispanics (Supplementary Table 1).
Table 1.
Baseline Characteristics of Patients With Cirrhosis, Stratified by Site (N = 1021)
| Parkland (n = 629) | UTSW (n = 155) | MEDVAMC (n = 237) | P value | |
|---|---|---|---|---|
| Age category | ||||
| 21–50y | 105 (16.7) | 23 (14.8) | 15 (6.4) | <.0001 |
| 51–60 y | 260 (41.3) | 37 (23.9) | 37 (15.7) | |
| 61–90 y | 264 (42.0) | 95 (61.3) | 184 (78.0) | |
| Sex | ||||
| Female | 265 (42.1) | 90 (58.1) | 16 (6.8) | <.0001 |
| Male | 364 (57.9) | 65 (41.9) | 220 (93.2) | |
| Race/ethnicity | ||||
| White | 113 (18.0) | 102 (65.8) | 144 (61.0) | <.0001 |
| Black | 219 (34.8) | 16 (10.3) | 57 (24.2) | |
| Hispanic | 10 (1.6) | 11 (7.1) | 7 (3.0) | |
| Other | 287 (45.6) | 26 (16.8) | 28 (11.9) | |
| Health status | ||||
| Excellent/very good | 75 (11.9) | 26 (16.8) | 41 (17.4) | <.0001 |
| Good | 184 (29.3) | 69 (44.5) | 88 (37.3) | |
| Fair/poor | 368 (58.5) | 60 (38.7) | 105 (44.5) | |
| Refused/don’t know | 2 (0.3) | 0 (0.0) | 2 (0.9) | |
| Marital Status | ||||
| Married | 169 (26.9) | 83 (53.6) | 96 (40.7) | <.0001 |
| Living with partner | 48 (7.6) | 6 (3.9) | 17 (7.2) | |
| Widowed | 62 (9.9) | 21 (13.6) | 20 (8.5) | |
| Separated | 68 (10.8) | 5 (3.2) | 9 (3.8) | |
| Divorced | 119 (18.9) | 23 (14.8) | 38 (16.1) | |
| Single, never married | 163 (25.9) | 17 (11.0) | 52 (22.0) | |
| Don’t know/refused | 0 (0.0) | 0 (0.0) | 4 (1.7) | |
| Etiology | ||||
| HCV | 383 (60.9) | 41 (26.5) | 179 (75.9) | <.0001 |
| HBV | 20 (3.2) | 7 (4.5) | 1 (0.4) | |
| Alcohol | 123 (19.6) | 30 (19.4) | 26 (11.0) | |
| NASH | 74 (11.8) | 47 (30.3) | 15 (6.4) | |
| Other | 29 (4.6) | 30 (19.4) | 15 (6.4) | |
| Child-Turcotte-Pugh class | ||||
| A | 443 (70.4) | 126 (81.3) | 185 (78.4) | |
| B/C | 186 (29.6) | 29 (18.7) | 51 (21.6) | |
| Household income | ||||
| <$15,000 | 340 (54.1) | 18 (11.6) | 42 (17.8) | <.0001 |
| $15,000–$25,000 | 93 (14.8) | 11 (7.1) | 33 (14.0) | |
| $25,000–$50,000 | 55 (8.7) | 32 (20.7) | 32 (13.6) | |
| $50,000+ | 11 (1.8) | 75 (48.4) | 28 (11.9) | |
| Don’t know/refused | 130 (20.7) | 19 (12.3) | 101 (42.8) | |
NOTE. Values are n (%).
HBV, hepatitis B virus; HCV, hepatitis C virus; MEDVAMC, Michael E. DeBakey VA Medical Center; NASH, nonalcoholic steatohepatitis; PHQ-9, Patient Health Questionnaire-9; UTSW, UT Southwestern Medical Center; VA, Veterans Affairs.
Prevalence of Depression and Anxiety
The median PHQ-9 score for the cohort was 7 (P25th–P75th, 3–12), with moderately severe (PHQ-9 score 15–19) and severe (PHQ-9 score ≥20) depression present in 11.3% and 4.3% of the population, respectively (Table 2, Figure 1). PHQ-9 scores were lower in patients from UTSW (median 5 [P25th–P75th, 2–9]) compared with those from Parkland or MEDVAMC (median 7 [P25th–P75th, 3–12] for both). UTSW also had fewer patients with moderately severe to severe depression than Parkland MEDVAC as well (6.5% vs 17.3% and 16.9%, respectively). The median STAI score was 33.3 (IQR, 23.3–46.7), with moderate–severe anxiety being present in 42.6% of the cohort. Patients at Parkland had higher STAI scores than did those followed at UTSW or the MEDVAMC (median 36.7 vs 33.3 and 33.3), including a higher proportion of patients classified as having moderate–severe anxiety (46.7% vs 38.7% and 34.2%, respectively) (Table 2, Figure 1). Overall, half (55.0%) of the cohort had neither depression nor anxiety, 29.4% had anxiety alone, 2.5% had depression alone, and 13.1% had both depression and anxiety.
Table 2.
Prevalence of Depression and Anxiety in Patients With Cirrhosis, Stratified by Site
| Parkland (n = 629) | UTSW (n = 155) | MEDVAMC (n = 237) | Total (N = 1021) | P Value | |
|---|---|---|---|---|---|
| Depression measured by PHQ-9 score | |||||
| No-minimal depression (0–4) | 238 (37.8) | 72 (46.5) | 86 (36.3) | 396 (38.8) | .03 |
| Mild depression (5–9) | 153 (24.3) | 45 (29.0) | 64 (27.0) | 262 (25.7) | |
| Moderate depression (10–14) | 129 (20.5) | 28 (18.1) | 47 (19.8) | 204 (20.0) | |
| Moderately severe depression (15–19) | 82 (13.0) | 8 (5.2) | 25 (10.6) | 115 (11.3) | |
| Severe depression (20–25) | 27 (4.3) | 2 (1.3) | 15 (6.3) | 44 (4.3) | |
| Anxiety measured by STAI score | |||||
| Mild anxiety (<40) | 335 (53.3) | 95 (61.3) | 156 (65.8) | 586 (57.4) | .002 |
| Moderate-severe anxiety (≥40) | 294 (46.7) | 60 (38.7) | 81 (34.2) | 435 (42.) | |
MEDVAMC, Michael E. DeBakey VA Medical Center; PHQ-9, Patient Health Questionnaire-9; STAI, State–Trait Anxiety Inventory; UTSW, University of Texas Southwestern Medical Center.
Figure 1.
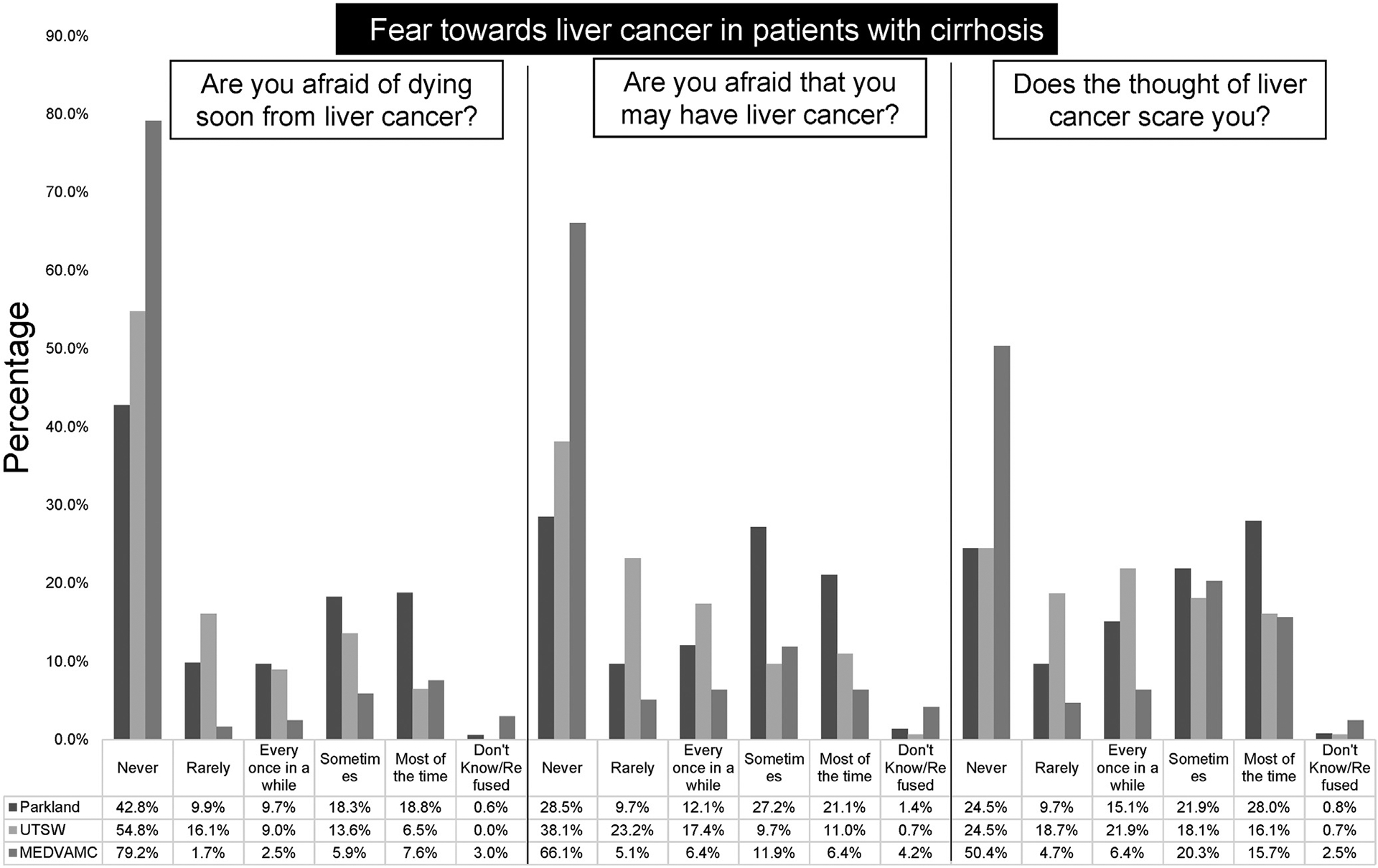
Distribution of depression and anxiety scores in a cohort of patients with cirrhosis.
Specific HCC-related fears were reported by patients, although there continued to be notable differences across the 3 sites. Over one-fourth (28.0%) of patients from Parkland reported fear of HCC most of the time, compared with 16.1% and 15.7% of those at UTSW and MEDVAMC, respectively. Similarly, fear of having and dying from HCC most of the time was reported in 16.2% and 14.3% of the cohort, with the highest proportions among Parkland patients for both (Figure 2).
Figure 2.
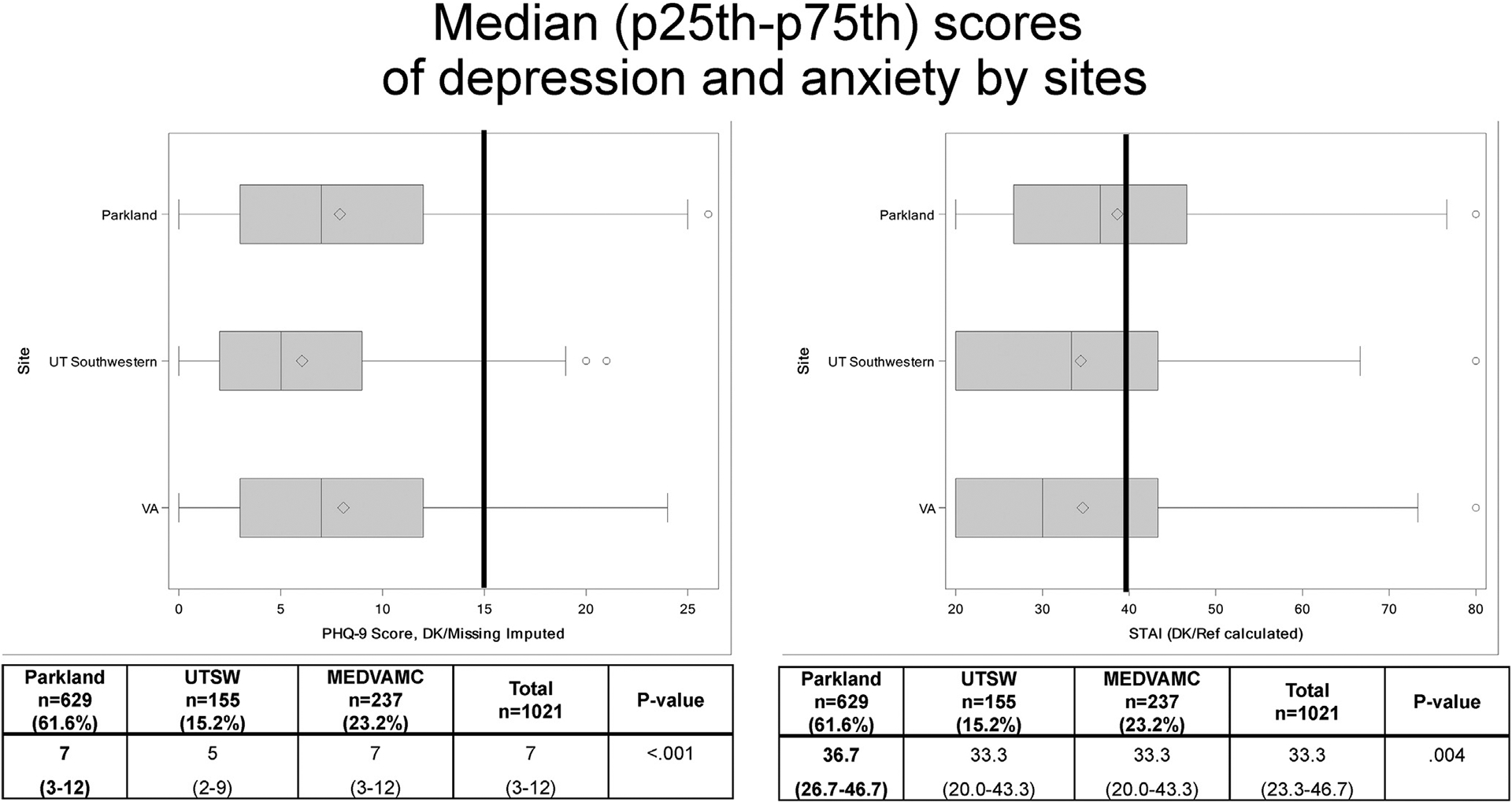
Percentages of participants with cirrhosis World Health Organization reports.
Correlates of Depression and Anxiety
In multivariable analysis, self-reported poor health, being widowed, and fear of having HCC were positively associated with having moderately severe to severe depression, while higher household income and Hispanic ethnicity were inversely associated with depression (Table 3). Female sex, self-reported poor health, fear of HCC and dying from HCC was associated with moderate–severe anxiety in multivariable analyses (Table 4). Age, liver disease etiology, and severity of liver dysfunction were not risk factors for either depression or anxiety in multivariable analyses. The prevalence depression and anxiety, stratified by Child-Turcotte-Pugh class, are presented in Supplementary Table 2. The prevalence of moderately severe to severe depression was 14.1% among Child-Turcotte-Pugh class A patients and 19.9% among patients with Child-Turcotte-Pugh class B or C cirrhosis, whereas moderate–severe depression was reported in 40.5% of patients with Child-Turcotte-Pugh class A cirrhosis and 48.5% of Child-Turcotte-Pugh class B patients.
Table 3.
Multivariable Logistic Regression for Correlates of Moderately Severe to Severe Depression (PHQ-9 Score ≥15)
| Prevalence odds ratio | 95% Confidence interval | P value | |
|---|---|---|---|
| Age category | |||
| 21–50 y | Reference | Reference | Reference |
| 51–60 y | 0.96 | 0.53–1.75) | .90 |
| 61–90 y | 0.90 | 0.49–1.68 | .74 |
| Sex | |||
| Female | Reference | Reference | Reference |
| Male | 0.72 | 0.47–1.12 | .14 |
| Race/ethnicity | |||
| White | Reference | Reference | Reference |
| Black | 0.65 | 0.38–1.11 | .11 |
| Hispanic | 0.57 | 0.33–0.97 | .04 |
| Other | 0.91 | 0.28–2.95 | .88 |
| Are you afraid of dying soon from liver cancer? | |||
| Never | Reference | Reference | Reference |
| Rarely | 1.04 | 0.50–2.15 | .92 |
| Every once in a while | 0.43 | 0.16–1.13 | .09 |
| Sometimes | 0.91 | 0.49–1.69 | .77 |
| Most of the time | 1.41 | 0.73–2.71 | .31 |
| Are you afraid that you may have liver cancer? | |||
| Never | Reference | Reference | Reference |
| Rarely | 0.87 | 0.38–2.02 | .75 |
| Every once in a while | 2.16 | 1.10–4.22 | .03 |
| Sometimes | 1.89 | 1.04–3.42 | .04 |
| Most of the time | 1.43 | 0.73–2.81 | .30 |
| Does the thought of liver cancer scare you? | |||
| Never | Reference | Reference | Reference |
| Rarely | 1.14 | 0.50–2.60 | .75 |
| Every once in a while | 0.82 | 0.37–1.78 | .61 |
| Sometimes | 1.44 | 0.77–2.69 | .25 |
| Most of the time | 1.61 | 0.82–3.17 | .17 |
| Health status | |||
| Excellent/very good | Reference | Reference | Reference |
| Good | 1.59 | 0.66–3.80 | .30 |
| Fair/poor | 4.08 | 1.79–9.28 | .001 |
| Marital status | |||
| Single, never married | Reference | Reference | Reference |
| Divorced | 1.24 | 0.69–2.25 | .47 |
| Living with partner | 0.92 | 0.41–2.05 | .83 |
| Married | 1.14 | 0.65–2.01 | .64 |
| Separated | 1.32 | 0.63–2.78 | .46 |
| Widowed | 2.08 | 1.07–4.05 | .03 |
| Child-Turcotte-Pugh class | |||
| A (5–6) | Reference | Reference | Reference |
| B (7–9) | 1.19 | 0.79–1.813 | .40 |
| Etiology | |||
| HCV | Reference | Reference | Reference |
| Alcohol | 1.40 | 0.82–2.39 | .22 |
| HBV | 1.20 | 0.38–3.78 | .76 |
| NASH | 0.90 | 0.47–1.75 | .76 |
| Other | 0.92 | 0.40–2.11 | .84 |
| Household income | |||
| <$15,000 | Reference | Reference | Reference |
| $15,000–$25,000 | 1.10 | 0.61–1.96 | .76 |
| $25,000–$50,000 | 0.89 | 0.45–1.76 | .74 |
| $50,000+ | 0.30 | 0.10–0.95 | .04 |
| Site | |||
| Parkland | Reference | Reference | Reference |
| UTSW | 0.52 | 0.23–1.20 | .13 |
| VA | 1.37 | 0.77–2.46 | .29 |
HBV, hepatitis B virus; HCV, hepatitis C virus; NASH, nonalcoholic steatohepatitis; PHQ-9, Patient Health Questionnaire-9; UTSW, UT Southwestern Medical Center; VA, Veterans Affairs.
Table 4.
Multivariable Logistic Regression for Correlates of Moderate–Severe Anxiety (STAI score >40)
| Prevalence odds ratio | 95% Confidence interval | P value | |
|---|---|---|---|
| Age category | |||
| 21–50 y | Reference | Reference | Reference |
| 51–60 y | 1.02 | 0.66–1.59 | .93 |
| 61–90 y | 0.71 | 0.45–1.11 | .14 |
| Sex | |||
| Female | Reference | Reference | Reference |
| Male | 0.71 | 0.51–0.98 | .04 |
| Race/ethnicity | |||
| White | Reference | Reference | Reference |
| Black | 0.90 | 0.60–1.34 | .60 |
| Hispanic | 0.97 | 0.64–1.45 | .87 |
| Other | 0.67 | 0.28–1.62 | .37 |
| Are you afraid of dying soon from liver cancer? | |||
| Never | Reference | Reference | Reference |
| Rarely | 1.41 | 0.84–2.39 | .19 |
| Every once in a while | 1.31 | 0.75–2.28 | .35 |
| Sometimes | 1.61 | 1.01–2.54 | .04 |
| Most of the time | 2.24 | 1.33–3.78 | .003 |
| Are you afraid that you may have liver cancer? | |||
| Never | Reference | Reference | Reference |
| Rarely | 1.60 | 0.97–2.66 | .07 |
| Every once in a while | 1.40 | 0.85–2.32 | .19 |
| Sometimes | 1.15 | 0.74–1.78 | .54 |
| Most of the time | 1.08 | 0.66–1.79 | .75 |
| Does the thought of liver cancer scare you? | |||
| Never | Reference | Reference | Reference |
| Rarely | 0.96 | 0.55–1.68 | .89 |
| Every once in a while | 1.37 | 0.82–2.30 | .23 |
| Sometimes | 1.78 | 1.13–2.80 | .01 |
| Most of the time | 2.13 | 1.29–3.51 | .003 |
| Health status | |||
| Excellent/very good | Reference | Reference | Reference |
| Good | 1.35 | 0.84–2.19 | .22 |
| Fair/poor | 2.73 | 1.73–4.31 | <.0001 |
| Marital status | |||
| Single, never married | Reference | Reference | Reference |
| Divorced | 1.05 | 0.67–1.63 | .84 |
| Don’t know/refused | 2.08 | 0.16–26.54 | .57 |
| Living with partner | 1.14 | 0.63–2.05 | .67 |
| Married | 0.76 | 0.50–1.14 | .18 |
| Separated | 1.22 | 0.70–2.15 | .48 |
| Widowed | 1.02 | 0.60–1.73 | .95 |
| Child-Turcotte-Pugh score | |||
| Class A (5–6) | Reference | Reference | Reference |
| Class B (7–9) | 1.10 | 0.79–1.52 | .59 |
| Etiology | |||
| HCV | Reference | Reference | Reference |
| Alcohol | 1.01 | 0.67–1.52 | .97 |
| HBV | 1.34 | 0.56–3.18 | .51 |
| NASH | 0.86 | 0.54–1.37 | .53 |
| Other | 1.05 | 0.59–1.87 | .88 |
| Household income | |||
| <$15,000 | Reference | Reference | Reference |
| $15,000–$25,000 | 0.98 | 0.63–1.54 | .94 |
| $25,000–$50,000 | 1.00 | 0.61–1.64 | .99 |
| $50,000+ | 0.71 | 0.38–1.30 | .26 |
| Site | |||
| Parkland | Reference | Reference | Reference |
| UTSW | 1.23 | 0.73–2.08 | .43 |
| VA | 1.21 | 0.78–1.88 | .39 |
HBV, hepatitis B virus; HCV, hepatitis C virus; NASH, nonalcoholic steatohepatitis; STAI, State–Trait Anxiety Inventory; UTSW, UT Southwestern Medical Center; VA, Veterans Affairs.
Discussion
In this large, diverse cohort of 1021 patients with cirrhosis, we found moderately severe to severe depression and anxiety were both common, with over 15% having depression and over 40% having anxiety. Anxiety and depression were both associated with fear of HCC and self-reported poor health. There were notable site-level differences in the prevalence of depression and anxiety, with higher proportions among patients at the county and VA health systems than at the academic tertiary care referral center. However, these differences were no longer significant in multivariable models, suggesting that these differences were explained by patient-level differences.
Our study extends the prior literature of depression and anxiety in patients with cirrhosis, which have largely focused on patients with more advanced liver dysfunction.27,29,30 Prior studies have reported depression and anxiety in 15% to >50% of patients with Child-Turcotte-Pugh class B or C and liver cancer. High levels of anxiety and depression are expected in these populations given high morbidity, with frequent complications, hospitalizations, caregiver dependency, and high risk of mortality. Interestingly, we found similar proportions of depression and anxiety despite most patients in our cohort having compensated cirrhosis. In our cohort, moderately severe to severe depression was also not associated with degree of liver dysfunction or comorbidity. Although our study did not conduct in-depth analyses for reasons underlying depression and anxiety, this finding suggests that depression and anxiety may contribute to behaviors leading to chronic liver disease (eg, substance abuse, unhealthy eating habits, and lack of physical exercise) rather than cirrhosis causing depression and anxiety, we note that depression and anxiety were both associated with fear of HCC. HCC is a common cause of death in patients with cirrhosis, and prior studies have similarly suggested patients express fear of developing or dying from HCC.31,32 It is unclear if improved surveillance effectiveness and increased patient engagement would help mitigate HCC-related fears.
Even though depression and anxiety are common, with significant implications for patient adherence and satisfaction, these comorbidities unfortunately often go unnoticed in clinical practice. Screening for depression and anxiety should be encouraged in all patients with cirrhosis to identify those in need of mental health counseling. Doing so can improve patient quality of life, improve compliance with medical recommendations, and may reduce unhealthy behaviors such as alcohol or drug abuse that can exacerbate underlying liver dysfunction.33,34 Once identified, the creation of either co-located clinics or multidisciplinary care in which mental health or social workers are embedded could tailor the needs for patients with high anxiety or depression scores, as they already exist in other fields.35 Screening in subsets of patients, such as those with alcohol-related cirrhosis, may be ineffective, given that this was not a major correlate of depression or anxiety in our study. Notably, we did not capture granular information on alcohol use via validated measures such as Alcohol Use Disorders Identification Test-Concise in all patients, nor other substance abuse behaviors.
We acknowledge that our study had several limitations. First, our survey was limited by nonresponse bias, although our response rate is similar to those of similar mailed efforts.36,37 Characteristics of respondents and nonrespondents appeared similar overall, although respondents had a higher proportion of women and Hispanics than nonrespondents. It is possible that our results may underestimate the prevalence of depression and overestimate anxiety based on associations seen in multivariable analysis. Further, unmeasured differences, such as social withdrawal, may also lead to differential prevalence estimates in non-respondents. Second, our results may not be generalizable to all patients and settings, particularly those outside the United States, although we examined patients across 3 major types of US health systems. Although we included patients with Child-Turcotte-Pugh class A or B cirrhosis, we excluded those with Child-Turcotte-Pugh class C cirrhosis, who may have increased depression and anxiety, given the increased risk of liver-related mortality. Third, we were unable to determine reasons for the depression and anxiety in this study, and the associations with HCC-related concerns and poor overall health status may not be causal. Finally, the present study only assessed these symptoms at a single time point, so we could not determine if these mental health symptoms would persist or change over time. However, we feel that these weaknesses are outweighed by several strengths, including the large sample size, the largest in the field of depression and anxiety and cirrhosis to our knowledge, including a high proportion of patients with compensated cirrhosis, manual chart review of all patients to confirm the presence of cirrhosis, and the use of validated symptom scales (PHQ-9 and STAI).
In conclusion, we found that moderately severe to severe depression and anxiety were both common among patients with cirrhosis. Providers should consider screening for these conditions and initiate early referral to mental health providers as needed.
Supplementary Material
What You Need to Know.
Background
Depression and anxiety can have negative effects on patients and are important to treat. There have been few studies of prevalence of these disorders among patients with cirrhosis.
Findings
A telephone-based survey of patients with cirrhosis at 3 health systems in the United States found that almost 1 in 6 patients with cirrhosis have moderately severe to severe depression and nearly half have moderate–severe anxiety.
Implications for patient care
Patients with cirrhosis should be evaluated for depression and anxiety.
Funding
This work was conducted with support from National Cancer Institute R01 CA212008 and Cancer Prevention Research Institute of Texas RP150587. The work is also supported in part by the Center for Gastrointestinal Development, Infection and Injury (National Institute of Diabetes and Digestive and Kidney Diseases P30 DK 56338). Ruben Hernaez and Jennifer R. Kramer are investigators at the Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413), Michael E. DeBakey VA Medical Center, Houston, TX. This material is based upon work supported (or supported in part) by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and the Michael E. DeBakey VA Medical Center Health Services Research and Development Center of Excellence (HFP90-020). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institute of Health, Department of Veterans Affairs, or the U.S. government.
Abbreviations used in this paper:
- EMR
electronic medical record
- HCC
hepatocellular carcinoma
- ICD-9
International Classification of Diseases–Ninth Revision
- ICD-10
International Classification of Diseases–Tenth Revision
- IQR
interquartile range
- MEDVAMC
Michael E. DeBakey Veterans Affairs Medical Center
- NASH
nonalcoholic steatohepatitis
- PHQ-9
Patient Health Questionnaire-9
- STAI
State–Trait Anxiety Inventory
- UTSW
UT Southwestern Medical Center
- VA
Veterans Affairs
Footnotes
Conflicts of Interest
The authors disclose no conflicts.
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at https://doi.org/10.1016/j.cgh.2020.08.045.
References
- 1.Peng JK, Hepgul N, Higginson IJ, et al. Symptom prevalence and quality of life of patients with end-stage liver disease: a systematic review and meta-analysis. Palliat Med 2019; 33:24–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ko FY, Yang AC, Tsai SJ, et al. Physiologic and laboratory correlates of depression, anxiety, and poor sleep in liver cirrhosis. BMC Gastroenterol 2013;13:18–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global Report on Diabetes. Geneva, Switzerland: WHO Press, 2020. [Google Scholar]
- 5.World Health Organization. Global Status Report on Alcohol and Health 2018: Executive Summary. Geneva, Switzerland: WHO Press, 2018. [Google Scholar]
- 6.Asrani SK, Devarbhavi H, Eaton J, et al. Burden of liver diseases in the world. J Hepatol 2019;70:151–171. [DOI] [PubMed] [Google Scholar]
- 7.McHugh RK, Weiss RD. Alcohol use disorder and depressive disorders. Alcohol Res 2019;40. 10.35946/arcr.v40.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004;61:807–816. [DOI] [PubMed] [Google Scholar]
- 9.Gerontoukou EI, Michaelidoy S, Rekleiti M, et al. Investigation of anxiety and depression in patients with chronic diseases. Health Psychol Res 2015;3:2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke JD, Burke KC, Rae DS. Increased rates of drug abuse and dependence after onset of mood or anxiety disorders in adolescence. Hosp Commun Psychiatry 1994;45:451–455. [DOI] [PubMed] [Google Scholar]
- 11.Conner KR, Sorensen S, Leonard KE. Initial depression and subsequent drinking during alcoholism treatment. J Stud Alcohol 2005;66:401–406. [DOI] [PubMed] [Google Scholar]
- 12.Spak L, Spak F, Allebeck P. Alcoholism and depression in a Swedish female population: co-morbidity and risk factors. Acta Psychiatr Scand 2000;102:44–51. [DOI] [PubMed] [Google Scholar]
- 13.Stine JG, Stukenborg GJ, Wang J, et al. Liver transplant candidates have impaired quality of life across health domains as assessed by computerized testing. Ann Hepatol 2020;19:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bajaj JS, Thacker LR, Wade JB, et al. PROMIS computerised adaptive tests are dynamic instruments to measure health-related quality of life in patients with cirrhosis. Aliment Pharmacol Ther 2011;34:1123–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feng Z, Marrero JA, Khaderi S, et al. Design of the Texas Hepatocellular Carcinoma Consortium Cohort Study. Am J Gastroenterol 2019;114:530–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nehra MS, Ma Y, Clark C, et al. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol 2013;47:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol 2012;107:247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rakoski MO, McCammon RJ, Piette JD, et al. Burden of cirrhosis on older Americans and their families: analysis of the health and retirement study. Hepatology 2012; 55:184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003;38:518–526. [DOI] [PubMed] [Google Scholar]
- 20.Singal AG, Hernaez R. Patient-reported barriers are associated with HCC surveillance receipt in a multi-center cohort of patients with cirrhosis. Clin Gastroenterol Hepatol 2020. July 3 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reyes-Gibby CC, Anderson KO, Morrow PK, et al. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health (Larchmt) 2012;21:311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee K, Otgonsuren M, Younoszai Z, et al. Association of chronic liver disease with depression: a population-based study. Psychosomatics 2013;54:52–59. [DOI] [PubMed] [Google Scholar]
- 24.Laing SS, Bogart A, Chubak J, et al. Psychological distress after a positive fecal occult blood test result among members of an integrated healthcare delivery system. Cancer Epidemiol Biomarkers Prev 2014;23:154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tosteson AN, Fryback DG, Hammond CS, et al. Consequences of false-positive screening mammograms. JAMA Intern Med 2014;174:954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Byrne MM, Weissfeld J, Roberts MS. Anxiety, fear of cancer, and perceived risk of cancer following lung cancer screening. Med Decis Mak 2008;28:917–925. [DOI] [PubMed] [Google Scholar]
- 27.Nardelli S, Pentassuglio I, Pasquale C, et al. Depression, anxiety and alexithymia symptoms are major determinants of health related quality of life (HRQoL) in cirrhotic patients. Metab Brain Dis 2013;28:239–243. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan DE, Dai F, Aytaman A, Baytarian M, et al. Development and performance of an algorithm to estimate the Child-Turcotte-Pugh score from a National Electronic Healthcare Database. Clin Gastroenterol Hepatol 2015;13:2333–2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buganza-Torio E, Mitchell N, Abraldes JG, et al. Depression in cirrhosis - a prospective evaluation of the prevalence, predictors and development of a screening nomogram. Aliment Pharmacol Ther 2019;49:194–201. [DOI] [PubMed] [Google Scholar]
- 30.Bianchi G, Marchesini G, Nicolino F, et al. Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis 2005;37:593–600. [DOI] [PubMed] [Google Scholar]
- 31.Singal AG, Volk ML, Rakoski MO, et al. Patient involvement in healthcare is associated with higher rates of surveillance for hepatocellular carcinoma. J Clin Gastroenterol 2011;45:727–732. [DOI] [PubMed] [Google Scholar]
- 32.Farvardin S, Patel J, Khambaty M, et al. Patient-reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology 2017;65:875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ho SB, Brau N, Cheung R, et al. Integrated care increases treatment and improves outcomes of patients with chronic hepatitis C virus infection and psychiatric illness or substance abuse. Clin Gastroenterol Hepatol 2015;13:2005–3. [DOI] [PubMed] [Google Scholar]
- 34.Khan A, Tansel A, White DL, et al. Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: a systematic review. Clin Gastroenterol Hepatol 2016;14:191–194; quiz e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breitbart WS, Alici Y. Psycho-oncology. Harv Rev Psychiatry 2009;17:361–376. [DOI] [PubMed] [Google Scholar]
- 36.Younossi ZM, Stepanova M, Afendy M, Lam BP, Mishra A. Knowledge about infection is the only predictor of treatment in patients with chronic hepatitis C. J Viral Hepat 2013;20:550–555. [DOI] [PubMed] [Google Scholar]
- 37.Singal AG, Tiro JA, Murphy CC, Marrero JA, et al. Mailed outreach invitations significantly improve HCC surveillance rates in patients with cirrhosis: a randomized clinical trial. Hepatology 2019;69:121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


