Kawasaki disease (KD) is an acute febrile vasculitis of childhood of unknown cause.1 As the coronavirus disease 2019 (COVID-19) pandemic continues, many countries have implemented nonpharmaceutical interventions (NPIs) to mitigate the spread of the virus. In Korea, NPIs such as mandatory mask wearing, school closure, and testing and isolation of symptomatic individuals were implemented in February 2020, with good compliance.2 On-site school reopening was postponed until May 20, 2020, and schools were reopened gradually until June 6, maintaining strict policies such as physical distancing and restrictions on private education and group activities.2 This nationwide intervention provided a unique opportunity for us to investigate the collateral effect of NPIs on the incidence of other diseases. We aimed to investigate whether NPIs were associated with a change in KD incidence in Korea, the country with the second-highest KD incidence rate worldwide.
In this retrospective, ecologic study, data on all KD cases among children 0 to 19 years of age from January 2010 to September 2020 were collected using the National Health Insurance Service database. The NPI period was defined as February through September 2020. The KD incidence rate in the NPI period was compared with the annual mean incidence rate during the same months in the pre-NPI period and with the incidence rate predicted by the autoregressive integrated moving average model. KD was defined as a case where the International Classification of Diseases–10 diagnostic code for KD (M30.3) and the prescription code for intravenous immunoglobulin (IVIg) were claimed together. IVIg-resistant KD was defined as recrudescent or persistent fever 24 to 48 hours after the first IVIg infusion, requiring an IVIg prescription nonconsecutively for at least 3 days. These data are licensed for this analysis only, and the institutional review board approved the study.
A total of 53 424 cases of KD were identified; among these, 83% occurred in children <5 years of age, and 17% were resistant to IVIg. In the pre-NPI period, the annual mean incidence was 48.1 per 100 000 persons and the monthly mean incidence was 4.1/100 000 (Figure [A]). After NPI implementation, KD incidence declined sharply; from April onward, it plateaued (Figure [B]). KD incidence is typically seasonal, with a minor peak in the late spring and summer and a larger one in the winter; however, this seasonal pattern was absent in the NPI period. When considering the months from February to September, the incidence in the NPI period was 18.8/100 000, corresponding to 60% of the mean incidence (31.5/100 000) in the pre-NPI period (P=0.085) and 58% of the predicted incidence (32.2/100 000 [95% CI, 46.6–77.9%]). The incidence in children between 0 and 4 years of age, the group with the highest incidence rate, was 80.0/100 000, significantly lower than the mean incidence in the pre-NPI period (123.0/100 000; P=0.003) and the predicted incidence (123.3/100 000 [95% CI, 51.9–86.7%]; Figure [C]). In the 5 to 9 years of age group, the incidence (10.6/100 000) was also significantly lower than the mean incidence (23.8/100 000) in the pre-NPI period (P=0.04) and the predicted incidence (24.7/100 000 [95% CI, 30.9–70.6%]; Figure [D]). However, there was no difference in the incidence before and after NPI implementation in the 10 to 19 years of age group, the group with the lowest incidence (Figure [E]).
Figure.
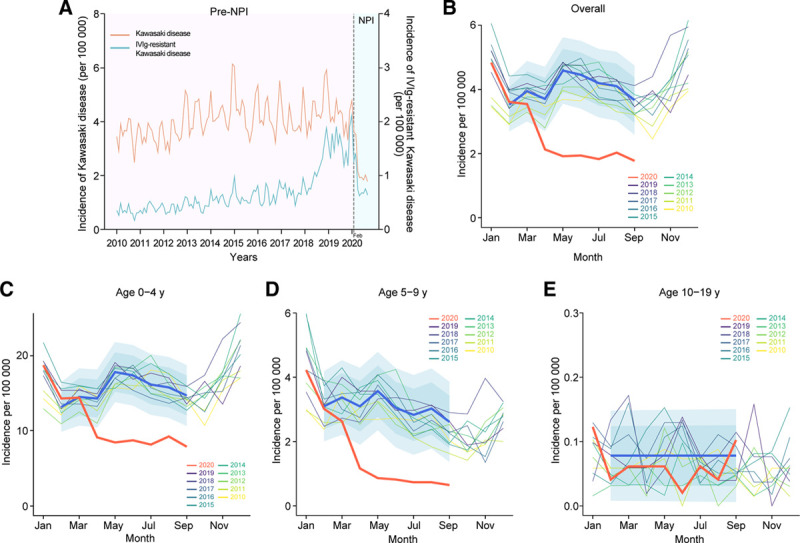
Kawasaki disease (KD) incidence in Korea. A, Yearly incidence of KD from 2010 to 2020. The red line denotes the age-specific incidence of KD, and the blue line denotes the age-specific incidence of intravenous immunoglobulin (IVIg)–resistant KD. The dotted line represents February 2020, when nonpharmaceutical interventions (NPIs) were implemented in Korea owing to coronavirus disease 2019 (COVID-19). B through E, Monthly incidence of KD and incidence predicted by an autoregressive integrated moving average model. The thick red line denotes the observed incidence during the NPI period, the thick blue line denotes the predicted incidence in the NPI period, and blue shades represent 80% and 95% CIs of the predicted incidence in the NPI period.
The incidence of IVIg-resistant KD had been increasing since 2018 in the pre-NPI period (Figure [A]), whereas the overall KD incidence did not change significantly (post/pre-NPI slope coefficient=0.04, P<0.0001). There was no significant change in the incidence of IVIg-resistant KD during the NPI period (6.8/100 000) compared with the annual mean of the previous 10 years (5.1/100 000; P>0.99).
The reasons for the association of NPI-related factors and KD incidence decrease are unclear. A reduction in respiratory viral infections and climate change, which have been cited as potential external triggers, were also associated with our findings.2–4 The incidence of KD-like diseases such as adenovirus infection and measles, which cause febrile rashes that can mimic KD, decreased after implementation of NPIs; this association may have created a bias.2 However, the proportion of IVIg-resistant KD, a severe form of KD, did not change in 2020 compared with that in 2019 (37.7% and 36.2%, respectively; P=0.28). This finding suggests that the decrease of KD-like diseases, generally milder than KD, had little effect on the overall decrease in the incidence of KD. Nevertheless, the KD incidence rate in Korea (80/100 000 children <5 years of age) is 3 to 16 times higher than that in Western countries (5 to 25/100 000 children <5 years of age), even after NPI implementation.1,5 This difference suggests that other variables, such as genetic and ethnic factors, are important in the pathogenesis of KD, regardless of the effect of NPIs.5
This nationwide study reveals that the KD incidence decreased significantly after the implementation of NPIs in Korea. Further long-term research is needed to determine whether the decrease in incidence of KD is solely attributable to the effects of NPIs.
Acknowledgments
This study used the National Health Information Database (NHIS-2020-1-572) from the National Health Insurance Service. Drs Kang, Y.-E. Kim, J. Jung, and Ahn had full access to the study data and take responsibility for its integrity and accuracy of the analysis. Drs Kang and Y.-E. Kim contributed equally to this study. Drs Ahn, J. Jung, and Kang contributed to study concept and design. Drs Y.-E. Kim, Huh, J.-H. Kim, S.Y. Jung, J. Jung, Ahn, and Kang and M.Y. Kim and J. Hong contributed to acquisition, analysis, and interpretation of data. Drs Ahn, J. Jung, and Kang contributed to drafting of the manuscript. Drs Huh and J. Jung and J. Hong contributed to statistical analysis.
Sources of Funding
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education (grant number 2019032869) and Gachon University Gil Medical Center (grant number 2019-11). The sponsor of the study was not involved in the study design, analysis, and interpretation of data; writing of the report; or the decision to submit the study results for publication.
Disclosures
None.
Footnotes
J.-M. Kang and Y.-E. Kim contributed equally to this article.
For Sources of Funding and Disclosures, see page 2510.
References
- 1.McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, et al. ; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135:e927–e999. doi: 10.1161/CIR.0000000000000484 [DOI] [PubMed] [Google Scholar]
- 2.Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, Kang JM. Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021;72:e184–e191. doi: 10.1093/cid/ciaa1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burns JC, Cayan DR, Tong G, Bainto EV, Turner CL, Shike H, Kawasaki T, Nakamura Y, Yashiro M, Yanagawa H. Seasonality and temporal clustering of Kawasaki syndrome. Epidemiology. 2005;16:220–225. doi: 10.1097/01.ede.0000152901.06689.d4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodó X, Curcoll R, Robinson M, Ballester J, Burns JC, Cayan DR, Lipkin WI, Williams BL, Couto-Rodriguez M, Nakamura Y, et al. Tropospheric winds from northeastern China carry the etiologic agent of Kawasaki disease from its source to Japan. Proc Natl Acad Sci U S A. 2014;111:7952–7957. doi: 10.1073/pnas.1400380111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elakabawi K, Lin J, Jiao F, Guo N, Yuan Z. Kawasaki disease: global burden and genetic background. Cardiol Res. 2020;11:9–14. doi: 10.14740/cr993 [DOI] [PMC free article] [PubMed] [Google Scholar]


