Abstract
Objective
To evaluate the treatment effectiveness of laser acupuncture (LA) in patients with musculoskeletal pain.
Methods
Major electronic databases, including Medline, PubMed, Embase, Cochrane Library, CINAHL, and Scopus were searched to identify double-blind, randomized controlled trials of LA in musculoskeletal disorders. The primary outcome was the treatment efficacy for pain. The secondary outcomes included the comparison of disability, functional impairment, and dropout rate between LA and sham treatment, as well as the effect of sham treatment for pain. The results from included studies were synthesized with the random effects model.
Results
In total, 20 articles comprising 568 patients receiving LA and 534 patients receiving sham treatment were included in the current study. Our analysis showed LA significantly reduced pain (g=0.88, 95% confidence interval [CI]=0.35 to 1.42, p=0.001), disability (g=0.68, 95% CI=0.29 to 1.08, p<0.001), and functional impairment (g=0.67, 95% CI=0.32 to 1.03, p<0.001). Through meta-regression analysis, we found these effects were not moderated by mean age, the percentage of females, or treatment duration. Additionally, there was no significant difference between the two groups in dropout rate (risk ratio=0.73, p=0.08), and the sham treatment significantly reduced only pain intensity (g=0.54, 95% CI=0.32 to 0.77, p<0.001).
Conclusion
Our findings supported that LA significantly reduced pain, disability, and functional impairment in patients with musculoskeletal disorders. Further researches are required to determine the optimal therapeutic parameters and the suitable patients for receiving LA.
Protocol Registration
CRD42020190919.
Keywords: laser acupuncture, meta-analysis, pain, randomized controlled trial, traditional Chinese medicine
Introduction
Pain is a global public health issue and is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1,2 Almost 20% of adults have suffered from pain, and 10% are newly diagnosed with chronic pain each year.3 Musculoskeletal pain is the most common type of pain and is a significant burden, as it is associated with increased disability and morbidity in patients with chronic diseases.4–6 The prevalence of musculoskeletal pain was 15.4% in Japan in 2010,7 and 36.6% in Taiwan in 2018.8
Musculoskeletal diseases lead to physical impairment and increased medical expenses—burdens that increase with the age of the patient. Acetaminophen, topical non-steroidal anti-inflammatory drugs, antidepressants, and opioids are commonly used conventional treatments for pain; however, they are associated with certain side effects in patients with musculoskeletal diseases.9,10 As a result, specific strategies and adjuvant options may be necessary for musculoskeletal conditions.11 The Centers for Disease Control and Prevention discovered that nearly 40% of adults used some form of complementary medicine.12,13
Acupuncture is the most common complementary therapy used to treat musculoskeletal pain. One study executed in 15 European countries revealed that 13% of participants with pain looked for acupuncture treatment in addition to conventional medication.14 Based on the traditional Chinese medicine (TCM) theory, acupuncture regulates the vitality that flows through the body’s meridians, called qi. Each meridian controls specific functions of the body in correlation with one or a group of organs. It is thought that bringing out this proper flow of qi can promote health, which can be fulfilled by arousing acupoints.15 In 1979, the World Health Organization recognized 43 diseases that may benefit from acupuncture, and in 2003 recommended acupuncture for use in over 100 conditions.16
Nowadays, laser acupuncture (LA) has been practiced in complementary and alternative therapy as well as needle acupuncture. LA has been applied clinically in the 1970s.17,18 LA uses a low-intensity, non-thermal laser irradiation to stimulate the acupoints.19,20 The laser beam can stimulate acupoints by energy deposition with no heat production. This way, the laser beam modulates visceral functions and facilitate metabolism by activating meridians, qi, and blood. LA has the effects of both acupuncture and moxibustion through delivering energy in pulsed wave at acupoints.21
Although articles reviewing LA exist,20,22 its effectiveness on musculoskeletal pain remain controversial.23,24 The efficacy of LA for pain is uncertain, due to inconclusive results from different studies.25–27 The effectiveness of LA regarding both pain reduction and functional outcome improvement were more congruously noted at long-term follow-up compared to promptly after treatment.28 In this study, we provide information from recent articles and perform a meta-analysis of all available randomized controlled trials to assess the effectiveness of LA on pain, disability, and functional impairment in patients with musculoskeletal pain.
Methods
Literature Search and Screening
Eligible articles were identified from PubMed, CINAHL, Cochrane Library, Embase, and Scopus databases. All authors evaluated the eligibility of the trials, and disagreements were resolved by discussion. Literature search was conducted using the search term “(pain OR arthralgia) AND laser acupuncture,” to identify articles published until June 2020, without restrictions on language. The titles and abstracts of articles obtained through the literature search were initially screened by the authors (YC Hung and PY Lin) to decide if they were potentially eligible for inclusion in the analysis. We excluded ineligible articles, including review papers, case reports, non-human studies, and those not mentioning LA. We registered the protocol with PROSPERO (registration number: CRD42020190919).
Study Inclusion Criteria
Studies that passed the screening were included based on the following criteria: (1) the inclusion of patients with musculoskeletal pain; (2) use of LA at meridian points as active treatment; (3) use of a randomized, sham-control study design; and (4) measuring pain intensity, degree of disability, or degree of functional impairment in participants. Trials that included incomplete data that could not be used to calculate effect sizes were excluded. We assessed the quality of each included study using the Cochrane Risk of Bias 2 (RoB2) tool.29
Data Extraction
The following data were obtained for analysis for all included studies: clinical diagnosis, pain location, age, sex, number of subjects, treatment duration, intensity of LA, measurement of pain intensity, disability or degree of functional impairment, and the number of dropout patients. Pain intensity was mainly assessed using the Visual Analog Scale, the McGill Pain Questionnaire, the Western Ontario and McMaster Universities’ Osteoarthritis Index (WOMAC), or the Numerical Pain Rating Scale. The degree of disability was assessed by using the WOMAC, Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, Nottingham Health Profile, or Oswestry Disability Inventory. Function level was assessed by using the WOMAC, DASH questionnaire, Numerical Rating Scale of Limitation of Activities, or Saudi Knee Function Scale.
Meta-Analysis Methods
The primary outcome was the change in pain intensity, comparing the efficacy of LA to sham treatment. The secondary outcomes were the effectiveness of LA vs sham treatment in change of disability and functional impairment, the placebo effect of LA in pain reduction, and the dropout rate between subjects receiving active treatment and sham treatment. For each included study, the effect sizes (ESs) expressing the difference in the effects (reduced pain, disability, or functional impairment) between LA and sham treatment were derived from the standardized mean difference based on Hedges’ adjusted g, where ESs >0 indicate that the effect in the active treatment group was superior to the sham treatment. The ESs expressing the difference in dropout rate between LA and sham treatment were described as risk ratios (RRs), where values <1 indicate a lower dropout rate in the LA treatment group. The ESs of individual studies were synthesized by the random effects model,30 which was chosen because a priori heterogeneity among included studies was expected. When the pooled ES indicated a significant result, we performed a sensitivity analysis to determine whether any of included study was accountable for the significant finding. To perform the sensitivity analysis, each study was individually removed, and the significance of the ES was re-tested.
Among-study heterogeneity was assessed by the Q statistic and the I2 statistic, which is the estimated percentage of variability in the effect that is due to heterogeneity rather than random error. Larger I2 values denote a higher heterogeneity. To examine potential sources of among-study heterogeneity, we performed meta-regression and subgroup analysis. Meta-regression was conducted by using the unrestricted maximum likelihood method to examine whether mean age, sex distribution (proportion of females), and the treatment duration of LA in the included studies moderated the pooled ES. Subgroup analysis based on treatment duration (shorter vs longer than one month). In addition, we examined publication bias using visual assessments of the funnel plots and testing their asymmetry via Egger’s regression analysis.31
Comprehensive Meta-Analysis software, version 2 (Biostat, Englewood, NJ, USA) was utilized to perform the statistics in this meta-analysis. Two-sided p-values <0.05 were considered as statistically significant.
We reported the methods, results, and other sections of the meta-analytic study by following the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Supplementary File 1).32 In addition, the quality of evidence of all outcomes in the meta-analysis was assessed using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) guidelines, considering study design, risk of bias, imprecision, inconsistency, indirectness, and magnitude of effect.33
Results
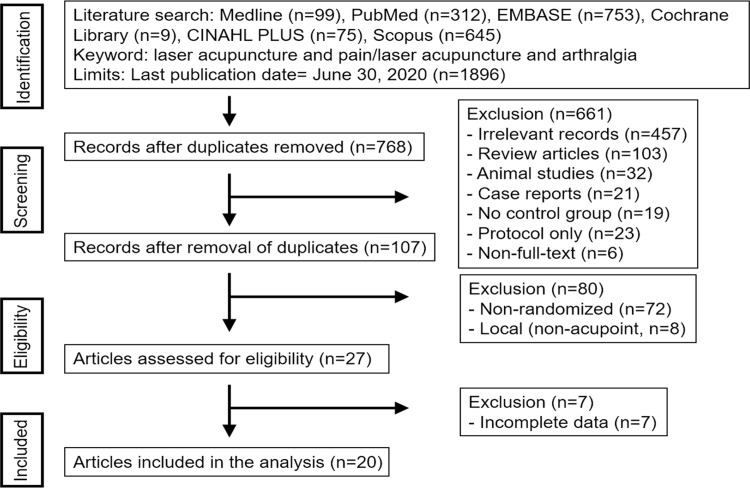
Our literature search found 1896 papers for initial literature search in the meta-analysis. We deleted duplicate citations, screened the results by viewing the titles and abstracts, and excluded studies that did not fulfill the inclusion criteria. Finally, 20 articles were included, comprising 568 patients receiving LA and 534 patients receiving sham treatment.34–53 The process of study search, screening, and selection is shown in Figure 1, and the characteristics of included articles are described in Table 1. The risk of bias of each included study is depicted in Supplementary Figure 2. The risks of all included studies were either “low” or “with some concern.” In addition, the evidence quality assessed using the GRADE system is summarized in Supplementary File 3. The quality of evidence ranged from “low” to “high” among different outcomes.
Figure 1.
Flowchart describing the process of study searching and inclusion.
Table 1.
Characteristics of Laser Acupuncture in Musculoskeletal Disorders
| Study | Condition | Blind | N* | Laser Parameters | Acupoints | Duration (Sessions) | Results |
|---|---|---|---|---|---|---|---|
| Kholoosy et al 202053 | Low back pain | Participants | 20/20 | 808 nm, 160 mW, 0.16 J/cm2 | LI4, ST44, H7 | 3 months (12) | ↓ pain**** Improved spinal ROM, functional status |
| Lin et al 202052 | Knee osteoarthritis | Participants, investigator | 88/55 | 10.6 μm, 160–180 mW, 61.2–68.8 J/cm2 | ST35, EX-LE4, Ashi point | 4 weeks (12) | No significant differences |
| Kibar et al 201751 | Shoulder pain | Participants, therapists | 36/37 | 850 nm, 100 mV, 4 J/cm2 | GB21, LI4, LI11, LI14, LI15, LI16, SI9, SI10, SI11, TE14, TE15 | 3 weeks (15) | ↓ pain**** Improved functional status |
| Lin et al 201750 | Low back pain | Participants, therapists | 25/23 | 808 nm, 40 mW, 15 J/cm2 | BL40, Ashi point | 5 days (5) | ↓ pain** |
| Acosta-Olivo et al 201749 | Wrist pain | Participants | 13/13 | 980 nm, 50 mW | SI5, SJ4, SJ15, LI5,PC7,LI4, VL62,V60,KI3 | 4 weeks (10) | ↓ pain** Improved functional status |
| Adly et al 201748 | Rheumatoid arthritis | Participants | 15/15 | 904 nm, 100 mW, 4 J/cm2 | LR3, ST25, ST36, SI3, SI4, LI4, LI11, SP6, SP9, GB25, GB34, HT7 | 4 weeks (12) | ↓ disease activity score** |
| Helianthi et al 201647 | Knee osteoarthritis | Participants, investigator | 31/31 | 785 nm, 50 mW, 4 J | ST35, ST36, SP9, GB34, EX-LE4 | 5 weeks (10) | ↓ Lequesne index**** |
| Shin et al 201546 | Low back pain | Participants, therapists | 28/28 | 660 nm, 50 mW | GV3–5, BL23–25, BL40, GB30 | 1 week (3) | No significant differences |
| Glazov et al 201445 | Low back pain | Participants, therapists | 48/48 | 840 nm, 20 mW 0.2–0.8 J | GV2–4, BL21–28, BL32–36, BL50–54, GB 25, GB27–32 | 8 weeks (8) | No significant differences |
| Al Rashoud et al 201444 | Knee osteoarthritis | Participants, therapists | 29/29 | 830 nm, 30 mW, 1.2 J | ST35, ST36, SP9, SP10 | 3 weeks (9) | ↓ pain** and ↑ quality of life** |
| Hinman et al 201443 | Knee osteoarthritis | Participants, therapists | 71/70 | 10 mW, 0.2 J | SP9–10, ST34–36, LR7–9, KI10, BL39–40, BL57, GB34–36 | 12 weeks (24) | No significant differences |
| Ferreira et al 201342 | Temporomandibular pain | Participants, | 20/20 | 780 nm, 50 mW, 4.5 J | ST6, SI19, GB20, GB43, LI4, LR3, TE3, EX-HN3 | 3 months (13) | ↓ chronic TMD pain*** |
| Lin et al 201241 | Knee osteoarthritis | Participants, therapists | 28/29 | 650 nm, 36 mW, 43.2 J | ST35 | 2 weeks (6) | ↓ pain**** |
| Katsoulis et al 201040 | Low back pain | Participants, therapists | 3/4 | 808 nm, 40 mW, 15 J/cm2 | BL40 | 5 days (5) | ↓ painNA |
| Zhao et al 201039 | Knee osteoarthritis | Participants, therapists | 20/20 | 650 nm, 36 mW, 43.2 J | ST35 | 2 weeks (6) | ↓ pain** |
| Shen et al 200938 | Knee osteoarthritis | Participants, therapists | 20/20 | 10.6 μm, 200 mW; 650 nm, 36 mW | ST35 | 4 weeks (12) | ↓ pain** |
| Yurtkuran et al 200737 | Knee osteoarthritis | Participants, investigator | 28/27 | 904 nm, 10 mW/cm2, 4 mW, 0.48 J | SP9 | 2 weeks (10) | ↓ periarticular swelling*** |
| Lam and Cheing 200736 | Epicondylitis | Participants, therapists | 21/18 | 904 nm, 25 mW, 0.275 J | Ashi points | 3 weeks (9) | ↓ pain****, ↑grip strength and physical function** |
| Ilbuldu et al 200435 | Trapezius muscle pain | Participants, therapists | 20/20 | 632.8 nm, 2 J | Ashi points | 4 weeks (12) | ↓ pain**, ↑ pain threshold**** |
| Naeser et al 200234 | Carpal tunnel syndrome | Participants, investigator | 4/7 | 632.8 nm, 15 mW, 1J | PC7, TE4, LU11, LI1, PC9, TE1, HT9, SI1 | 4 weeks (12) | ↓ MPQ pain score, Phalen and Tinel sign*** |
Notes: *Laser acupuncture group/control group; **P<0.05; ***P<0.01; ****P<0.001.
Abbreviation: NA, P value not available.
Pain
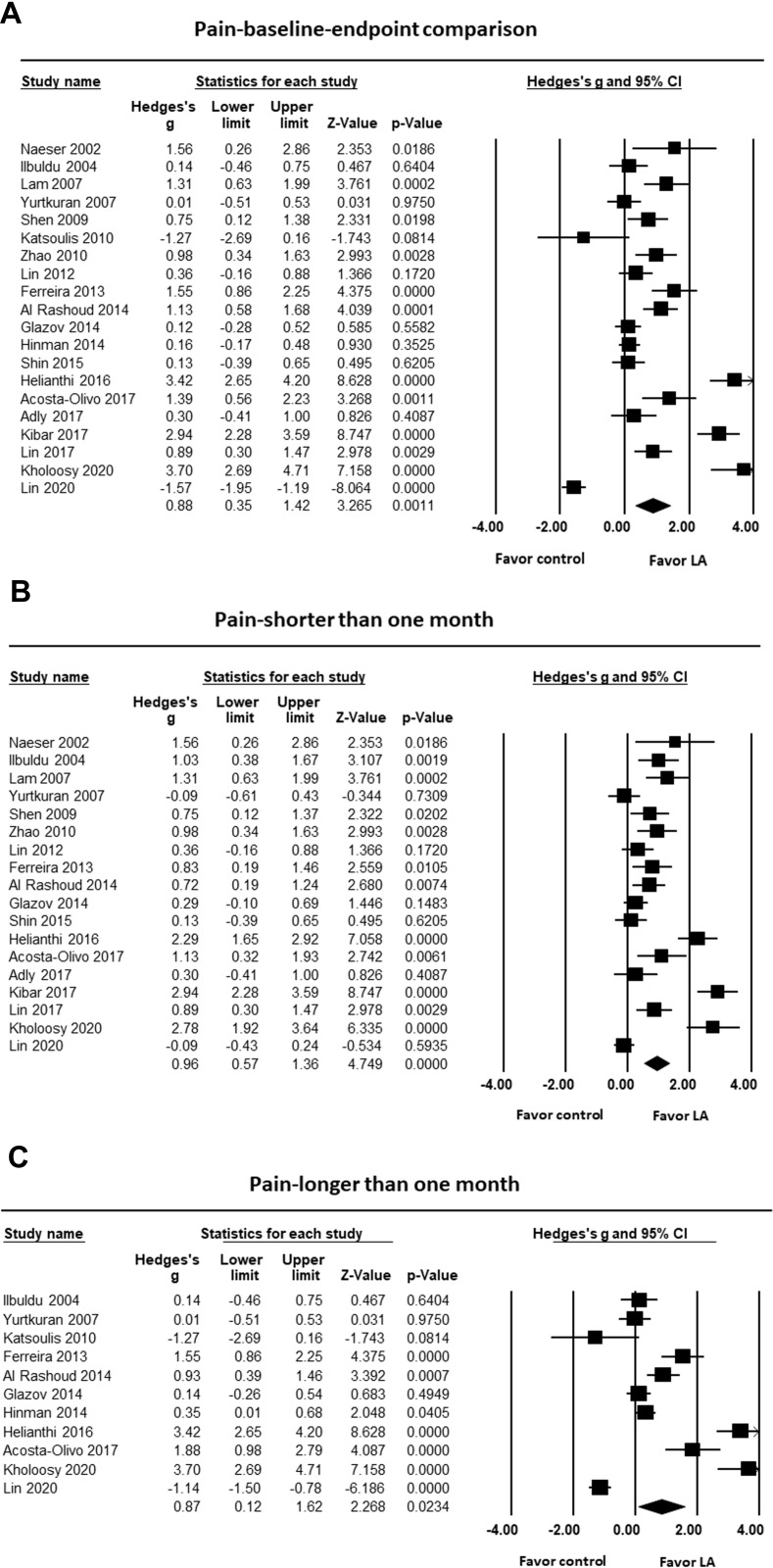
First, we compared the level of pain reduction between patients receiving LA and sham treatment, extracting data from all 20 studies. Our analysis found superior pain reduction in patients receiving LA compared to sham treatment (g=0.88, 95% confidence interval (CI)=0.35 to 1.42, p=0.001; Figure 2). Sensitivity analysis found that the significant effect was not influenced by removal of any individual study. Publication bias was detected, as shown by Egger’s regression test (t=2.92, df=18, p=0.009) and in Supplementary Figure 4. In addition, significant heterogeneity was identified among these studies (Q=309.89, df=19, I2=93.87%, p<0.001).
Figure 2.
Forest plot showing effect sizes (Hedges’ g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing the effect of laser acupuncture (LA) and sham treatment on pain, with (A) overall effect, (B) treatment duration shorter than one month, and (C) treatment duration longer than one month.
Next, to examine the sources of the among-study heterogeneity, we examined the effect of variables by using subgroup meta-analysis and meta-regression. In the subgroup analysis, we found that LA was more effective in reducing pain than sham treatment, for duration with both shorter (g=0.96, 95% CI=0.57 to 1.36, p<0.001; Figure 2) and longer (g=0.87, 95% CI=0.12 to 1.62, p=0.02; Figure 2) than one month. In addition, meta-regression was conducted to examine whether the effect of LA on pain reduction was moderated by mean age, sex distribution of subjects, total dose of LA, or treatment duration. We found that the effect size was not moderated by mean age (slope=0.02, p=0.40), the percentage of females (slope=-1.43, p=0.30), or treatment duration (slope=−0.02, p=0.38; see Supplementary Figure 5, which shows the regressions for mean age, the percentage of females, and treatment duration in terms of their effect on pain).
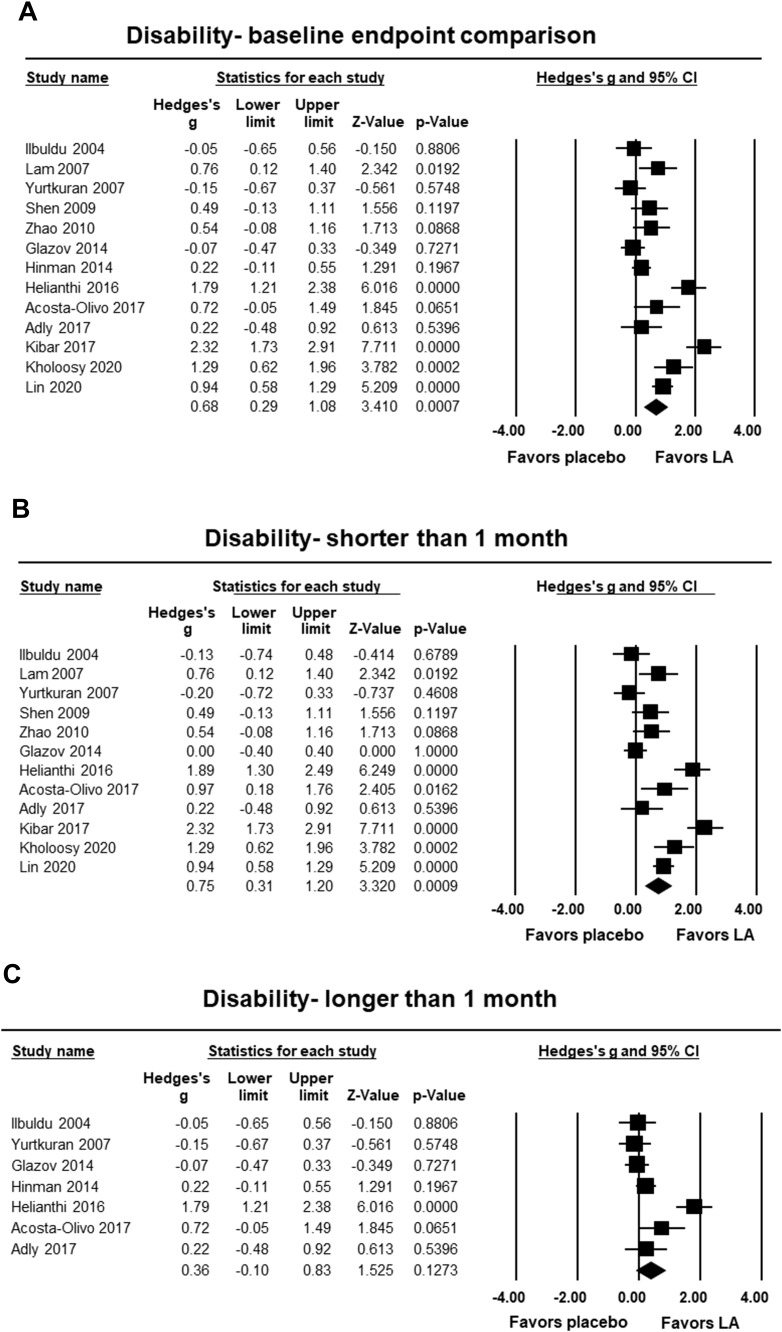
Disability
We compared the change in the level of disability between patients receiving LA and sham treatment with data extracted from 13 studies. Our analysis found a significant reduction in the level of disability in patients receiving LA compared to those receiving sham treatment (g=0.68, 95% CI=0.29 to 1.08, p<0.001; Figure 3). Sensitivity analysis illustrated that the significant effect was not influenced by removing any single study. No publication bias was detected in the analysis (t=0.96, df=11, p=0.36), as shown in Supplementary Figure 6. Significant heterogeneity was found among these studies (Q=86.40, df =12, I2=86.11%, p<0.001).
Figure 3.
Forest plot showing effect sizes (Hedges’ g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing the effect of laser acupuncture (LA) and sham treatment on disability levels, with (A) overall effect, (B) treatment duration shorter than one month, and (C) treatment duration longer than one month.
In the subgroup analysis, we found that LA was significantly more effective at reducing disability in treatments shorter than one month in duration (g=0.75, 95% CI=0.31 to 1.20, p<0.001; Figure 3); however, not in treatments longer than one month in duration (g=0.36, 95% CI=−0.10 to 0.83, p=0.13; Figure 3). In addition, through the meta-regression analysis, we found that the effect was not moderated by mean age (slope=0.03, p=0.08), the percentage of females (slope=−0.60, p=0.62), or treatment duration (slope=−0.02, p=0.07; see Supplementary Figure 7, which shows the meta-regression analyses for mean age, the percentage of females, and treatment duration in terms of their effect on disability).
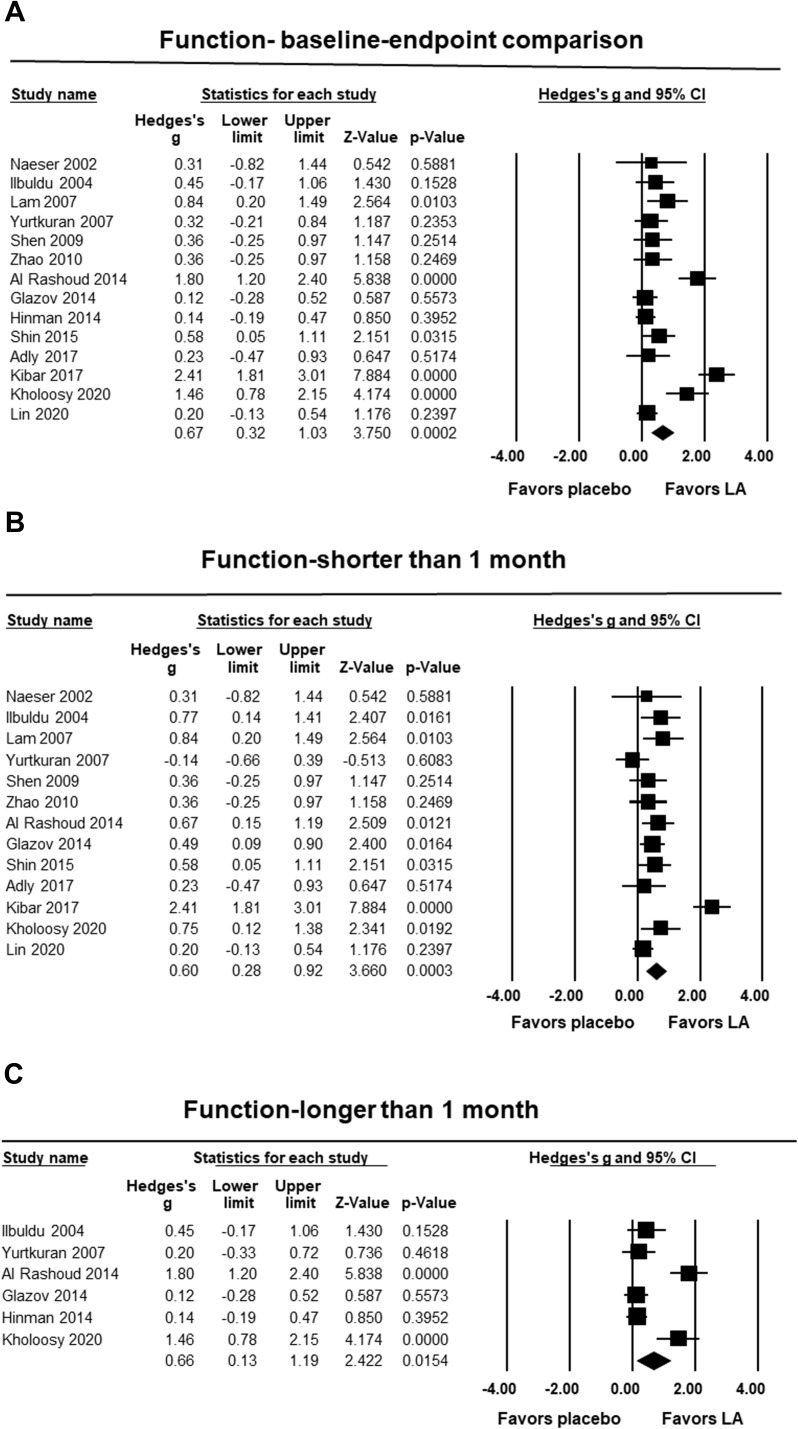
Functional Impairment
We also compared the change in the level of functional impairment between patients receiving LA and sham treatment, with data derived from 14 studies. Our results showed a significant decrease in the level of functional impairment in patients receiving LA compared to sham treatment (g=0.67, 95% CI=0.32 to 1.03, p<0.001; Figure 4). Sensitivity analysis revealed that the significant effect was not influenced by removal of any single study. However, publication bias was detected in the analysis (t=1.82, df=12, p=0.09) and in Supplementary Figure 8. Significant heterogeneity was found among these studies (Q=78.07, df=13, I2=83.35%, p<0.001).
Figure 4.
Forest plot showing effect sizes (Hedges’ g) and 95% confidence intervals (CIs) from individual studies and pooled results comparing the effect of effect of laser acupuncture (LA) and sham treatment on the recovery of functional impairment, with (A) overall effect, (B) treatment duration shorter than one month, and (C) treatment duration longer than one month.
In the subgroup analysis, we found that LA was significantly more effective in reducing functional impairment in treatments shorter than one month in duration (g=0.60, 95% CI=0.28 to 0.92, p=0.001; Figure 4), as well as in treatments longer than one month in duration (g=0.66, 95% CI=0.13 to 1.19, p=0.02; Figure 4). In addition, through the meta-regression analysis, we found that the effect was not moderated by mean age (slope=0.00, p=0.97), the percentage of females (slope=−0.05, p=0.96), or treatment duration (slope=−0.01, p=0.58; see Supplementary Figure 9, which shows the regressions for mean age, the percentage of females, and treatment duration in terms of their effect on function).
Dropout Rate
We found that the dropout rate was not significantly different when comparing patients receiving LA to those receiving sham treatment (RR=0.73, p=0.08; see Supplementary Figure 10, which shows a forest plot incorporating data from previous studies). No publication bias was found (t=0.33, df=18, p=0.74), as shown in Supplementary Figure 11. Additionally, no significant heterogeneity was found among studies (Q=9.47, df=19, I2=0.00%, p=0.95).
Placebo Effect
Finally, we examined the placebo effect of sham treatment on pain intensity, based on data from the 20 included studies. We found sham treatment significantly reduced pain intensity (g=0.54, 95% CI=0.32 to 0.77, p<0.0001; see Supplementary Figure 12, which shows a forest plot comparing the degree of pain reduction associated with laser acupuncture and placebo treatment). Sensitivity analysis showed that the significant effect was not influenced by removal of any single study. Publication bias was detected in the analysis (t=2.44, df=18, p=0.03; see Supplementary Figure 13). In addition, significant heterogeneity was noted among these studies (Q=104.49, df =19, I2=81.82%, p<0.001).
Discussion
This study revealed that the positive effects of LA are most pronounced for pain reduction and functional impairment, following treatments of both shorter and longer than one month in duration. In treatments shorter than one month, LA also appears to improve disability; however, in treatments longer than one month, its effect is not significant. Disability is a physical condition that renders a person unable to act in a manner considered usual for the majority of people. Disability caused by a musculoskeletal disorder that lasts for longer than one month may require physical rehabilitation therapy in addition to LA. We found that these effects were not moderated by mean age, sex distribution, or treatment duration. There was no significant difference between LA and sham groups in dropout rates. The main strength of this study is that LA ameliorates pain, disability, and functional impairment in patients with musculoskeletal pain.
Law et al revealed that LA was efficacious in ameliorating musculoskeletal pain and functional outcomes after 6 to 26 weeks of treatment,28 while the findings of this study revealed improvement after 5 days to 3 months of treatment (Table 1). Randomized trials offer the best evidence for assessing the occurrence of events with enough frequency. If the trial designs are similar, the insight can be improved by combining the evidence from each trial. Such meta-analyses are best executed by statistically synthesizing results from a series of studies. Advantages of meta-analyses include: the potential for a more thorough, larger population analysis of outcomes (eg, time to event); inconsistencies of individual results can be pooled and quantified, increasing the statistical power; precision and accuracy; the ability to explore patient subgroups; and the ability to verify data quality as well as implementation of sensitivity analyses on main results. Following a vast search, we excluded more than 98% of the identified articles due to them not meeting the inclusion criteria. We believe that our results, according to statistically synthesizing the data, provide the best obtainable evidence on LA for pain management.
Sixteen articles revealed that LA had superior effects to the control group in terms of pain management, improvement of disability, and functional improvement (Table 1). The laser parameters used for LA in these studies were as follows: wavelength, 632.8–980 nm; power, 4–200 mW; and energy, 0.275–43.2 J. Four studies43,45,46,52 revealed negative results for LA; two of these studies43,45 applied 0.2 J of energy to acupoints, and one study52 applied 61.2–68.8 J. A power density and energy that is too low or high can result in an ineffective response.54 One study46 treated patients three times weekly for only one week. The improper choice of acupoints, low frequencies, inadequate energy, infrequent treatments, and unskilled therapists can all lead to a negative effect following LA therapy.21
On the basis of TCM theory, qi stagnation and blood stasis cause pain (a pathological change in which a long-term or serious stagnation of qi obstructs blood flow, a disease with features of simultaneous qi stagnation and blood stasis).55,56 Based on the gate-control theory of pain and the endorphin-and-neurotransmitter model, acupuncture has the ability to modulate certain pain signals related to endogenous neurotransmitters.57
The de-qi sensation felt by the patient after acupuncture needling is associated with the therapeutic effect of acupuncture, according to the TCM theory.21,58,59 LA is not associated with de-qi sensations such as distension, soreness, heaviness, or numbness. However, LA could activate blood and move qi, providing anti-inflammatory and analgesic effects. The re-adjustment of qi and blood flow recovers internal homeostasis and improves disease symptoms.60 Low-level laser therapy has anti-inflammatory effects, influences neural modulation, and has cellular effects through the dissociation of nitric oxide from cytochrome C oxidase.20 It seems to play the same role as needle acupuncture at the skin level, by means of an inhibitory mechanism associated with nerve block.61 Low-level laser therapy can decrease inflammation by lowering the quantity of biochemical markers (prostaglandin E2, messenger ribonucleic acid cyclooxygenase-2, interleukin-1β, and tumor necrosis factor-α), neutrophil influx, oxidative stress, edema, and hemorrhage.62 LA combines the therapeutic effects of traditional acupuncture and low-level lasers. The analgesic effect of low-level laser therapy is mediated by peripheral opioid receptors,63 whereas traditional acupuncture has local and remote analgesia that may be mediated by various mechanisms.
Invasive acupuncture needling is associated with potential complications, including pneumothorax, central nervous system or spinal cord injury, cardiac tamponade or heart injury, subarachnoid or intracranial hemorrhage, broken needles, local bruising, swelling, tenderness, infection or cellulitis, dizziness, syncope, nausea, and vomiting.64–67 By combining traditional acupuncture and modern laser medicine, noninvasive LA is a low-intensity, nonthermal laser irradiation method to stimulate acupuncture points. LA does not include the pain sensation and risk of complications associated with acupuncture needling. It focuses on acupoint treatment, as opposed to ordinary laser therapy which focuses on local non-acupoints. Noninvasive and pain-free, LA could be an alternative therapy to traditional acupuncture for needle-phobic patients.
In this study, it was noted that pain intensity might have been influenced by the placebo effect. The placebo effect is not a medical effect; however, it benefits a patient’s health status due to the perception that the placebo treatment is effective.68,69 There are several possible mechanisms of the placebo effect, including the expectation model and the reflex conditioning model. A subject’s thoughts and beliefs may respond positively to the health state in the expectation model; their previous experiences will produce a positive conditioned stimulus in the reflex conditioning model. Some neurobiological studies have shown that placebo analgesia mechanisms may be associated with endogenous opioids, dopamine, endocannabinoids, oxytocin, or vasopressin.70–73 However, the analgesic effect of neuromodulation with LA is significantly superior to the placebo effect in this study.
Meta-analysis is a statistical method and quantitative technique to pool the results of several individual studies. Pooling the results from individual clinical trials provides more precise and accurate information on the effect of LA for musculoskeletal pain. However, several limitations of meta-analysis exist, including: little information provided about the mechanism of action, imperfect literature data collection, the presence of publication bias, over-estimating the treatment effect size, lower quality research methods, lack of TCM syndrome differentiation, and heterogeneity. In some studies, randomization is not performed with a computer-generated random number list, a coin toss, or well-intermixed envelopes. Some trials were incompletely masked or blinded and did not use identical tablets or vials. In order to reduce the above limitations, we selected more than 14 well-randomized, double-blind clinical trials conducted in different countries. Finally, some non-English articles might have been missed from our search results.
Conclusion
This meta-analysis has shown that LA may improve pain, disability, and functional levels in musculoskeletal disorders. Further researches are necessary to better determine optimal therapeutic parameters, including wavelength, dose, and intensity, and to reach the maximal physiological benefit and cost-effectiveness of therapy.
Abbreviations
CI, confidence interval; DASH, the Disabilities of the Arm, Shoulder and Hand; ES, effect size; LA, laser acupuncture; RR, risk ratio; TCM, traditional Chinese medicine; WOMAC, the Western Ontario and McMaster Universities’ Osteoarthritis Index.
Ethical Publication Statement
We have read and understood the journal’s policies, and we believe that neither the manuscript nor the study violates any of these.
Disclosure
The authors report no conflicts of interest.
References
- 1.Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health. 2011;11:770. doi: 10.1186/1471-2458-11-770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–1982. doi: 10.1097/j.pain.0000000000001939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Association for the Study of Pain. Unrelieved pain is a major global healthcare problem. Available from: https://www.iasp-pain.org/files/Content/ContentFolders/GlobalYearAgainstPain2/20042005RighttoPainRelief/factsheet.pdf. Accessed June 4, 2021.
- 4.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656. [PMC free article] [PubMed] [Google Scholar]
- 5.Blyth FM, Briggs AM, Schneider CH, et al. The global burden of musculoskeletal pain-where to from here? Am J Public Health. 2019;109(1):35–40. doi: 10.2105/AJPH.2018.304747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams A, Kamper SJ, Wiggers JH, et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. doi: 10.1186/s12916-018-1151-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakamura M, Nishiwaki Y, Ushida T, et al. Prevalence and characteristics of chronic musculoskeletal pain in Japan. J Orthop Sci. 2011;16(4):424–432. doi: 10.1007/s00776-011-0102-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health and Welfare. National health insurance annual statistical report; 2018. Available from: https://www.mohw.gov.tw/cp-4574-49817-2.html. Accessed September12, 2020.
- 9.Derry S, Wiffen PJ, Kalso EA, et al. Topical analgesics for acute and chronic pain in adults - an overview of cochrane reviews. Cochrane Database Syst Rev. 2017;5:CD008609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yabuki S, Ip AKK, Tam CK, et al. Evidence-based recommendations on the pharmacological management of osteoarthritis and chronic low back pain: an Asian consensus. Asian J Anesthesiol. 2019;57(2):37–54. doi: 10.6859/aja.201906_57(2).0003 [DOI] [PubMed] [Google Scholar]
- 11.Lewis R, Gómez Álvarez CB, Rayman M, et al. Strategies for optimising musculoskeletal health in the 21(st) century. BMC Musculoskelet Disord. 2019;20(1):164. doi: 10.1186/s12891-019-2510-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes PM, Bloom B, Nahin R. CDC national health statistics report #12. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 13.Simpson CA. Complementary medicine in chronic pain treatment. Phys Med Rehabil Clin N Am. 2015;26(2):321–347. doi: 10.1016/j.pmr.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 14.Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 15.Wu JN. A short history of acupuncture. J Altern Complement Med. 1996;2(1):19–21. doi: 10.1089/acm.1996.2.19 [DOI] [PubMed] [Google Scholar]
- 16.Zhang X. Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials. Geneva: World Health Organization; 2002:23–26. [Google Scholar]
- 17.Hill S. Letter: acupuncture research in the USSR. Am J Chin Med. 1976;4:204–205. [PubMed] [Google Scholar]
- 18.Miklánek J, Kriz V. 1st experiences with the utilization of lasers for acupuncture. The Akuplas device. Fysiatr Revmatol Vestn. 1978;56(1):36–40. [PubMed] [Google Scholar]
- 19.Whittaker P. Laser acupuncture: past, present, and future. Lasers Med Sci. 2004;19(2):69–80. doi: 10.1007/s10103-004-0296-8 [DOI] [PubMed] [Google Scholar]
- 20.Chon TY, Mallory MJ, Yang J, et al. Laser acupuncture: a concise review. Med Acupunct. 2019;31(3):164–168. doi: 10.1089/acu.2019.1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu WL, Hung IL, Hung YC. Explore laser acupuncture’s role. In: Chen LL, Cheng TO, editors. Acupuncture in Modern Medicine. IntechOpen; 2013. doi: 10.5772/55092 [DOI] [Google Scholar]
- 22.Wu SY, Kuo CE, Hung YC, et al. Managing pain with laser acupuncture. In: Prostran M, editor. Pain Management. InTechOpen; 2016. doi: 10.5772/62863 [DOI] [Google Scholar]
- 23.Fleckenstein J, Niederer D, Auerbach K, et al. No effect of acupuncture in the relief of delayed-onset muscle soreness: results of a randomized controlled trial. Clin J Sport Med. 2016;26(6):471–477. doi: 10.1097/JSM.0000000000000259 [DOI] [PubMed] [Google Scholar]
- 24.Abbasoglu A, Cabioglu MT, Tugcu AU, et al. Laser acupuncture before heel lancing for pain management in healthy term newborns: a randomised controlled trial. Acupunct Med. 2015;33(6):445–450. doi: 10.1136/acupmed-2015-010765 [DOI] [PubMed] [Google Scholar]
- 25.Chang WD, Wu JH, Yang WJ, et al. Therapeutic effects of low-level laser on lateral epicondylitis from differential interventions of Chinese-Western medicine: systematic review. Photomed Laser Surg. 2010;28(3):327–336. doi: 10.1089/pho.2009.2558 [DOI] [PubMed] [Google Scholar]
- 26.Chow RT, Johnson MI, Lopes-Martins RAB, et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897–1908. doi: 10.1016/S0140-6736(09)61522-1 [DOI] [PubMed] [Google Scholar]
- 27.Jang H, Lee H. Meta-analysis of pain relief effects by laser irradiation on joint areas. Photomed Laser Surg. 2012;30(8):405–417. doi: 10.1089/pho.2012.3240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Law D, McDonough S, Bleakley C, et al. Laser acupuncture for treating musculoskeletal pain: a systematic review with meta-analysis. J Acupunct Meridian Stud. 2015;8(1):2–16. doi: 10.1016/j.jams.2014.06.015 [DOI] [PubMed] [Google Scholar]
- 29.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 30.Shadish WR, Haddock CK. Combining estimates of effect size. In: Cooper H, Hedges LV, editors. The Handbook of Research Synthesis. New York: Russell Sage foundation; 1994:261–281. [Google Scholar]
- 31.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 34.Naeser MA, Hahn KA, Lieberman BE, et al. Carpal tunnel syndrome pain treated with low-level laser and microamperes transcutaneous electric nerve stimulation: a Controlled Study. Arch Phys Med Rehabil. 2002;83(7):978–988. doi: 10.1053/apmr.2002.33096 [DOI] [PubMed] [Google Scholar]
- 35.Ilbuldu E, Cakmak A, Disci R, et al. Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomed Laser Surg. 2004;22(4):306–311. doi: 10.1089/pho.2004.22.306 [DOI] [PubMed] [Google Scholar]
- 36.Lam LK, Cheing GL. Effects of 904-nm low-level laser therapy in the management of lateral epicondylitis: a randomized controlled trial. Photomed Laser Surg. 2007;25(2):65–71. doi: 10.1089/pho.2006.2047 [DOI] [PubMed] [Google Scholar]
- 37.Yurtkuran M, Alp A, Konur S, et al. Laser acupuncture in knee osteoarthritis: a Double-Blind, Randomized Controlled Study. Photomed Laser Surg. 2007;25(1):14–20. doi: 10.1089/pho.2006.1093 [DOI] [PubMed] [Google Scholar]
- 38.Shen X, Zhao L, Ding G, et al. Effect of combined laser acupuncture on knee osteoarthritis: a Pilot Study. Lasers Med Sci. 2009;24(2):129–136. doi: 10.1007/s10103-007-0536-9 [DOI] [PubMed] [Google Scholar]
- 39.Zhao L, Shen X, Cheng K, et al. Validating a nonacupoint sham control for laser treatment of knee osteoarthritis. Photomed Laser Surg. 2010;28(3):351–356. doi: 10.1089/pho.2009.2511 [DOI] [PubMed] [Google Scholar]
- 40.Katsoulis J, Ausfeld-Hafter B, Windecker-Gétaz I, et al. Laser acupuncture for myofascial pain of the masticatory muscles. A Controlled Pilot Study. Schweiz Monatsschr Zahnmed. 2010;120(3):213–225. [PubMed] [Google Scholar]
- 41.Lin ML, Wu HC, Hsieh YH, et al. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evid Based Complement Alternat Med. 2012;2012:521612. doi: 10.1155/2012/521612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ferreira LA, de Oliveira RG, Guimarães JP, et al. Laser acupuncture in patients with temporomandibular dysfunction: a randomized controlled trial. Lasers Med Sci. 2013;28(6):1549–1558. doi: 10.1007/s10103-013-1273-x [DOI] [PubMed] [Google Scholar]
- 43.Hinman RS, McCrory P, Pirotta M, et al. Acupuncture for chronic knee pain: a randomized clinical trial. JAMA. 2014;312(13):1313–1322. doi: 10.1001/jama.2014.12660 [DOI] [PubMed] [Google Scholar]
- 44.Al Rashoud AS, Abboud RJ, Wang W, et al. Efficacy of low-level laser therapy applied at acupuncture points in knee osteoarthritis: a randomised double-blind comparative trial. Physiotherapy. 2014;100(3):242–248. doi: 10.1016/j.physio.2013.09.007 [DOI] [PubMed] [Google Scholar]
- 45.Glazov G, Yelland M, Emery J. Low-dose laser acupuncture for non-specific chronic low back pain: a double-blind randomised controlled trial. Acupunct Med. 2014;32(2):116–123. doi: 10.1136/acupmed-2013-010456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shin JY, Ku B, Kim JU, et al. Short-term effect of laser acupuncture on lower back pain: a randomized, placebo-controlled, double-blind trial. Evid Based Complement Alternat Med. 2015;2015:808425. doi: 10.1155/2015/808425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Helianthi DR, Simadibrata C, Srilestari A, et al. Pain reduction after laser acupuncture treatment in geriatric patients with knee osteoarthritis: a randomized controlled trial. Acta Med Indones. 2016;48(2):114–121. [PubMed] [Google Scholar]
- 48.Adly AS, Adly AS, Adly MS, et al. Laser acupuncture versus reflexology therapy in elderly with rheumatoid arthritis. Lasers Med Sci. 2017;32(5):1097–1103. doi: 10.1007/s10103-017-2213-y [DOI] [PubMed] [Google Scholar]
- 49.Acosta-Olivo C, Siller-Adame A, Tamez-Mata Y, et al. Laser treatment on acupuncture points improves pain and wrist functionality in patients undergoing rehabilitation therapy after wrist bone fracture. a Randomized, Controlled, Blinded Study. Acupunct Electrother Res. 2017;42(1):11–25. doi: 10.3727/036012917x14908026365007 [DOI] [PubMed] [Google Scholar]
- 50.Lin ML, Wu JH, Lin CW, et al. Clinical effects of laser acupuncture plus chinese cupping on the pain and plasma cortisol levels in patients with chronic nonspecific lower back pain: a randomized controlled trial. Evid Based Complement Alternat Med. 2017;2017:3140403. doi: 10.1155/2017/3140403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kibar S, Konak HE, Evcik D, et al. Laser acupuncture treatment improves pain and functional status in patients with subacromial impingement syndrome: a Randomized, Double-Blind, Sham-Controlled Study. Pain Med. 2017;18(5):980–987. doi: 10.1093/pm/pnw197 [DOI] [PubMed] [Google Scholar]
- 52.Lin L, Cheng K, Tan MT, et al. Comparison of the effects of 10.6-μm infrared laser and traditional moxibustion in the treatment of knee osteoarthritis. Lasers Med Sci. 2020;35(4):823–832. doi: 10.1007/s10103-019-02863-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kholoosy L, Elyaspour D, Akhgari MR, et al. Evaluation of the therapeutic effect of low level laser in controlling low back pain: a randomized controlled trial. J Lasers Med Sci. 2020;11(2):120–125. doi: 10.34172/jlms.2020.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bjordal J, Couppé C, Ljunggreen A. Low level laser therapy for tendinopathy. Evidence of a dose-response pattern. Phys Ther Rev. 2001;6(2):91–99. doi: 10.1179/ptr.2001.6.2.91 [DOI] [Google Scholar]
- 55.Shi DB. The Encyclopedia of Traditional Chinese Medicine [e-Book in Chinese]. Version 1.0 For PC. Taipei: Yuan-Liou; 2002. [Google Scholar]
- 56.World Health Organization Regional Office for the Western Pacific (WPRO). WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region. Manila: WPRO; 2007:56. [Google Scholar]
- 57.Chon TY, Lee MC. Acupuncture. Mayo Clin Proc. 2013;88:1141–1146. doi: 10.1016/j.mayocp.2013.06.009 [DOI] [PubMed] [Google Scholar]
- 58.Yang XY, Shi GX, Li QQ, et al. Characterization of deqi sensation and acupuncture effect. Evid Based Complement Alternat Med. 2013;2013:319734. doi: 10.1155/2013/319734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Park JE, Ryu YH, Liu Y, et al. A literature review of de qi in clinical studies. Acupunct Med. 2013;31(2):132–142. doi: 10.1136/acupmed-2012-010279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hu WL, Chang CH, Hung YC, et al. Laser acupuncture therapy in patients with treatment-resistant temporomandibular disorders. PLoS One. 2014;9(10):e110528. doi: 10.1371/journal.pone.0110528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Silberstein M. Is acupuncture stimulation a misnomer? A case for using the term blockade. BMC Complement Altern Med. 2013;13:68. doi: 10.1186/1472-6882-13-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bjordal JM, Johnson MI, Iversen V, et al. Photoradiation in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg. 2006;24(2):158–168. doi: 10.1089/pho.2006.24.158 [DOI] [PubMed] [Google Scholar]
- 63.Perese Serra A, Ashmawi HA. Influence of naloxone and methysergide on the analgesic effects of low-level laser in an experimental pain model. Rev Bras Anestesiol. 2010;60(3):302–310. doi: 10.1016/S0034-7094(10)70037-4 [DOI] [PubMed] [Google Scholar]
- 64.Chan M, Wu XY, Wu J, et al. Safety of acupuncture: overview of systematic reviews. Sci Rep. 2017;7(1):3369. doi: 10.1038/s41598-017-03272-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ullah W, Ahmad A, Mukhtar M, et al. Acupuncture-related cardiac complications: a systematic review. J Invasive Cardiol. 2019;31(4):E69–E72. [PubMed] [Google Scholar]
- 66.Lin SK, Liu JM, Wang PH, et al. Incidence of cellulitis following acupuncture treatments in Taiwan. Int J Environ Res Public Health. 2019;16(20):3831. doi: 10.3390/ijerph16203831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wu J, Hu Y, Zhu Y, et al. Systematic review of adverse effects: a further step towards modernization of acupuncture in China. Evid Based Complement Alternat Med. 2015;2015:432467. doi: 10.1155/2015/432467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Colloca L, Barsky AJ, Ropper AH. Placebo and nocebo effects. N Engl J Med. 2020;382(6):554–561. doi: 10.1056/NEJMra1907805 [DOI] [PubMed] [Google Scholar]
- 69.Brody H. Meaning and an overview of the placebo effect. Perspect Biol Med. 2018;61(3):353–360. doi: 10.1353/pbm.2018.0048 [DOI] [PubMed] [Google Scholar]
- 70.Hashmi JA. Placebo effect: theory, mechanisms and teleological roots. Int Rev Neurobiol. 2018;139:233–253. doi: 10.1016/bs.irn.2018.07.017 [DOI] [PubMed] [Google Scholar]
- 71.Girach A, Aamir A, Zis P. The neurobiology under the placebo effect. Drugs Today (Barc). 2019;55(7):469–476. doi: 10.1358/dot.2019.55.7.3010575 [DOI] [PubMed] [Google Scholar]
- 72.Peciña M, Zubieta J-K. Molecular mechanisms of placebo responses in humans. Mol Psychiatry. 2015;20(4):416–423. doi: 10.1038/mp.2014.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kjær SW, Rice A, Wartolowska K, et al. Neuromodulation: more than a placebo effect? Pain. 2020;161(3):491–495. doi: 10.1097/j.pain.0000000000001727 [DOI] [PubMed] [Google Scholar]