Abstract
Objectives
Sleep deprivation is a common problem in Canada and is associated with many health problems. More than a quarter of Canadians get fewer than the recommended sleep hours (<7 h). This paper examines the prevalence and risk factors for sleep deprivation in two First Nation communities in Saskatchewan, Canada.
Methods
The baseline cross-sectional survey was completed between 2018 and 2019 in collaboration with the two Cree First Nation communities in Saskatchewan, Canada. There were five hundred and eighty-eight participants participated in the survey from two communities. A Multivariate logistic regression model was used for analysis.
Results
The prevalence of sleep deprivation (<7 h of sleep) was 25.4%. The multivariate logistics regression revealed that middle and older age groups, visible mold in the house, and being male with nighttime insomnia symptoms were significantly associated with a higher risk of sleep deprivation among study participants in the study.
Conclusions
In these two First Nation communities, a higher proportion of the participants reported having sleep deprivation. This was a unique study, which evolved from ongoing research collaboration with two First Nation communities in Saskatchewan, Canada. Findings will be helpful in the management of patients with sleep deprivation in these communities; as well as for co-creating policy with the communities and future research priorities.
Keywords: Sleep duration, Sleep deprivation, First nations, Adults
Highlights
-
•
The prevalence sleep deprivation was about 25% in these two First Nation communities.
-
•
Association between sleep deprivation and males with nighttime insomnia observed.
-
•
Another important finding was association between visible mold and sleep deprivation.
1. Introduction
Sleep deprivation is a common problem in Canada. More than a quarter (26%) of Canadians get fewer than seven hours of sleep [1,2]. Sleep deprivation is associated with sociodemographic and socioeconomic risk factors, lifestyle factors, non-communicable diseases/chronic health conditions and factors related to the sleep environment. Socioeconomic positioning was a robust determinant of sleep deprivation [[3], [4], [5], [6], [7]]. In Canada, people aged 18 to 64 with higher household education and income were more likely to report sleeping 7–9 h per night, compared with those with less education and lower incomes [3]. A recent study reported that male gender, older age, low social status, and high coffee intake was associated with objectively determined short sleep duration [4]. Another study reported that short sleep duration was associated with sociodemographic or socioeconomic factors and further described that those with lower levels of education, low household income quartiles and employment status of ‘unemployed’ and ‘disability retirees’ were the most likely to report shorter sleep durations (≤5 h) [5]. The prevalence of short sleep was increased for the lowest household income quintile, those with less than high school education, and among African Americans (compared with Whites) [6]. Ehlers et al. reported that American Indian ethnicity, being older than 30 years, having only a high school diploma were predictive factors for sleep deprivation [7].
Studies have shown an association between lifestyle factors and sleep deprivation. Zhu et al. [4] reported that an inverse ‘U-shaped’ relationship between objective sleep duration and physical activity level and observed that the most physically active slept between 6–7 h. Kline [8] showed that intervening on physical activity levels has been shown to improve sleep efficiency and sleep duration. Another study reported that exercise promoted increased sleep efficiency and duration regardless of the mode and intensity of activity [9]. A meta-analysis investigating the association between portable screen-based media devices and sleep outcomes found that bedtime media usage was associated with insufficient sleep duration and poor sleep quality [10]. However, another meta-analysis found no association between television watching and sleep duration but did find that computer use was associated with a shorter total sleep duration [11]. A report by Hysing et al. [12] indicated that daytime and bedtime use of electronic devices were both related to sleep measures, with an increased risk of short sleep duration, long sleep onset latency and increased sleep deficiency. A dose–response relationship observed between sleep duration and use of electronic devices specifically the association between personal computer use and risk of less than 5 h of sleep compared with the recommended sleep hours [12]. One study reported that short sleepers (≤6 h) were more likely to smoke tobacco than adequate sleepers (≥7 h) [13]. The findings of Hamidovic et al. [14] suggested that sleep loss may increase the likelihood of smoking during abstinence because of the potential of nicotine to reduce subjective sleepiness. Nakata et al. [15] reported that exposure to passive smoking at work was associated with short sleep duration in men and current smoking or non-traditional use of tobacco related to various subtypes of sleep disturbances (difficulty awakening in the morning and difficulty initiating sleep) in both men and women. Angarita et al. [16] reported that acute exposure to substance drug use was associated with sleep disruption by affecting sleep latency, duration, and quality. Evaluating the empirical evidence, Irish et al. [17] presented several common sleep hygiene recommendations, including regular exercise, stress management, noise reduction, sleep timing regularity, and avoidance of caffeine, nicotine, alcohol, and daytime napping.
Sleep deprivation or insufficient sleep duration leads to many health problems [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54]]. Some authors have shown a relationship with short duration of sleep and increased risk of mortality [[19], [20], [21]]. Mullington et al. [22] summarized findings of the effects of insufficient sleep on cardiovascular risk factors including blood pressure, glucose metabolism, hormonal regulation and inflammation. Another study by Hall et al. [23] reported that the prevalence of the metabolic syndrome and its components were elevated in short sleepers.
Research has shown that when a person sleeps less than 7 h a night there was a dose–response relationship between sleep loss and obesity, that means the shorter the sleep was cause of the greater the obesity [[24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34]]. Also, Taheri et al. [28] reported that sleep insufficiency was associated with lower levels of leptin, a hormone produced by an adipose tissue hormone that suppresses appetite, and higher levels of ghrelin, a peptide that stimulates appetite. Another Canadian study reported that short sleep duration sleepers were 35% more likely to experience a 5 kg weight gain [35]. It is known that people who have a short sleep at night are less able to process glucose compared to those who get enough sleep and have increased chance of developing type 2 diabetes [36,37]. In the Sleep Heart Health Study, which was a community-based cohort, adults who reported 5 h of sleep or less were 2.5 times more likely to have type 2 diabetes, compared with those who slept 7–8 h per night [38]. An experimental study supported the relationship between shorter sleep times and impaired glucose tolerance [39]. Possible mechanisms for how short sleep duration and sleep restriction predispose to obesity and type 2 diabetes have been discussed by McNeil & Chaput et al. [29] and Reutrakul et al. [40]. Authors suggested that short sleepers have may have an increase in insulin release and showed the evidence that short sleep enhances susceptibility to food stimuli for energy-dense, high-carbohydrate foods which may lead to obesity and diabetes.
Sleep deprivation leads to high blood pressure, inflammation, and other bodily stress reactions. Two large epidemiological studies reported that sleep loss and sleep complaints are associated with heart attacks and stroke [41,42]. Adults who sleep less than 6 h a night have a 48% greater chance of developing heart disease and a 15% greater chance having a stroke [37]. Grandner et al. [43] presented the association between long or short sleep durations and cardiovascular disease, via several mechanistic pathways. A review by Nagai et al. [44] reported that the short or long sleep duration is independently associated with an increased likelihood of coronary events.
There was sufficient evidence that short sleep duration acts as a risk factor for hypertension [45]. Sleep durations of 5 h per night was associated with a significantly increased risk of hypertension in participants between the ages of 32 and 59 years, and the increased risk continued to be significant after controlling for obesity and diabetes [46]. Another study by Grandner et al. [47] reported that both short and long sleep duration are associated with increased hypertension risk across most age groups. Faraut et al. [48], Hwang et al. [49] and Kumar et al. [50] reported that compared with the recommended sleep duration of 7 h, a sleep duration of less than 5 h per day/night had an increased prevalence of hypertension.
Several studies reported an association between sleep deprivation and impaired neurobehavioral performance [30,[51], [52], [53], [54]]. Al-Abri [51] reported that there is a strong bi-directional relationship between sleep deprivation/disturbance and depression [51]. Author mentioned that chronic sleep deprivation may lead to depression due to the neurochemical changes that occur in the brain and on reverse, depression may lead to distributed sleep or sleep deprivation. Sun et al. [53] reported that participants with short sleep duration (<5 and 5–6 h) had a higher risk of depression onset and recurrent depression compared to participants with recommended sleep durations (7–8 h). They also reported the bidirectional relationship between sleep duration and depression. That is, conversely, depression induced short sleep durations. A review by Wu et al. [54] reported that potential association between sleep and circadian rhythm with stress granule formation associated with development of the Alzheimer's disease. In addition, there was a link between accidents [55]; injury [[56], [57], [58], [59]]; poor work performance [60,61] and sleep deprivation.
Several studies reported the prevalence of sleep deprivation among American Indian/Alaska Native populations [7,62,63]. Ehlers et al. [7] reported that the sleep deprivation prevalence in American Indian/Alaska Native populations was about 30%. Chapman et al. [62] reported in the 2009–2010 Behavioral Risk Factor Surveillance Survey that insufficient sleep rates were higher among American Indian/Alaska Native peoples compared with non-Hispanic Whites (34.2% vs. 27.4%). A study from the 2014 Behavioral Risk Factor Surveillance System reported that the age-adjusted prevalence of healthy sleep duration (≥a7 h) was lower among American Indians/Alaska Natives (59.6%) compared with non-Hispanic Whites (66.8%) [63].
This information was available for other populations, but little was known about the prevalence of sleep deprivation or insufficient sleep among First Nations peoples in Canada. Also, there were no studies reported in the literature about risk factors and their possible associations with sleep deprivation in First Nations peoples. In this study, we examined prevalence and possible associations between sleep deprivation in two Cree First Nation communities in Saskatchewan using the data from a community-based cross-sectional study. First Nations are one of the three groups of Indigenous peoples in Canada who are the descendants of the original inhabitants of Canada (the other two being Inuit and Métis). First Nations peoples have unique cultures, languages and ceremonies [64,65]. All Indigenous peoples in Canada are impacted by colonization that produces inequities in social and structural determinants of health [66]. The residential school experience in particular negatively impacted the health and wellbeing of survivors as well as their children and grandchildren. This experience attempted to expunge their cultural identity including Indigenous language and cultural customs, their ways of life including consuming traditional foods, and their Indigenous knowledge and family ties linking the youth and Elders [[66], [67], [68]]. Other major impacts from residential school attendance included physical, sexual and emotional abuse, witnessing abuse and isolation from family [67] with intergenerational reverberations. First Nation communities in Canada also frequently report generally poor housing conditions [[69], [70], [71]]. Studies have shown associations between dampness, exposure to visible mould at home and sleep problems [72,73]. To bridge a part of the gap in this current research, this paper examined the prevalence of sleep deprivation and its risk factors and possible associations in two Cree First Nation communities in Saskatchewan, Canada.
2. Material and methods
2.1. Study sample
The baseline survey of the First Nations Sleep Health Project (FNSHP) collaboration was completed between 2018 and 2019 in collaboration with the two Cree First Nation communities (Community A and Community B) in Saskatchewan, Canada. The overall goal of the FNSHP was to study the relationships between sleep disorders and risk factors and co-morbidities, and to evaluate local diagnosis and treatment. Ethics approval was obtained from the University of Saskatchewan's Biomedical Research Ethics Board (Certificate No. Bio #18–110) and followed Chapter 9 (Research Involving the First Nations, Inuit, and Metis Peoples of Canada) in the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans [74]. Individual participants gave their written consent in this research collaboration with the two Saskatchewan First Nation communities.
2.2. Data collection
Research assistants were hired from these communities and trained to conduct the baseline surveys in their respective community. Adults 18 years and older were invited to the Community Health/Youth Centre to participate in baseline survey. Data were collected via interviewer-administered questionnaires and clinical assessments. A pamphlet describing the study and an invitation to participate in the baseline survey were distributed by the research assistants by door-to-door canvassing and also during local community events such as ‘Treaty Days’. Simultaneously, the community members were invited through a social media campaign to participate in the survey. The survey collected information on demographic variables, individual and contextual determinants of sleep health, self-reported height and weight, and objective clinical measurements. This manuscript is based on data from the questionnaires. Demographic information about participants including age, sex, body mass index, education level, money left at the end of the month, life-style factors, sleeping environment, medical history, and sleep health information was obtained from the survey questionnaire.
Information collected on ever diagnosed non-communicable diseases/chronic conditions were: diabetes; high blood pressure; heart problems; stroke; atrial fibrillation; chronic obstructive pulmonary disease/emphysema; asthma; chronic bronchitis; sleep apnea; acid reflux; hypothyroidism; depression, anxiety, post-traumatic stress disorder; Parkinson's disease; chronic pain; kidney disease and restless legs syndrome. Other factors considered were: prescription medication use; sleep medication; and traditional medicines which are used to assist with sleeping.
2.3. Definitions
2.3.1. Sleep duration and sleep deprivation
Sleep duration was calculated using questions about the participant's usual sleep habits during the past month: “When have you usually gone to bed?”; When have you usually gotten up in the morning?”; “How long has it taken to fall asleep each night?”. Taking the difference of the first two questions, the time in bed at night was calculated and then time to falling asleep was subtracted to obtain the actual sleep duration. Recommendations of optimal sleep duration hours were based on those from the National Sleep Foundation [75]. Sleep deprivation was defined as the participants with sleep duration of less than 7 h per night (less than the recommended optimal sleep duration per night).
2.4. Statistical analysis
Statistical analyses were conducted using SPSS software (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp.). Descriptive statistics, mean and standard deviation (SD) were reported for continuous variables and p-values of t-tests were reported for comparing the means of two samples. For categorical variables, frequency and percentage (%) were reported. Chi-square tests were used to determine the bivariable association of sleep deprivation prevalence with the independent variables of interest. Logistic regression models were used to predict the relationship between a binary outcome of sleep deprivation (yes or no) and a set of explanatory variables. A series of logistic regression models were fitted to determine whether potential risk factors, confounders, and interactive effects contributed significantly to the prevalence of sleep deprivation. Based on bivariable analysis, variables with p < 0.20 and less than 25% missing variables were included in the multivariate model. All variables that were statistically significant (p < 0.05), as well as important clinical factors (sex, age and body mass index (BMI)), were retained in the final multivariable model. Interactions between potential effect modifiers were examined and were retained in the final model if the p-value was <0.05. The strength of associations were presented by odds ratios (OR) and their 95% confidence intervals (CI) [76].
3. Results
There were five hundred and eighty-eight participants participated in the baseline survey, 418 individuals from Community A and 170 individuals from Community B. The mean age ±SD of the 588 study participants was 40.0 ± 15.3 years with a range being from 18 to 78 years. There were 44.2% male and 55.8% females that participated in this study. Sleep duration was available for 567 individuals. The mean sleep duration was 8.18 ± 2.28 h. The prevalence of sleep deprivation was 25.4% (144/567).
Table 1 depicts the bivariate associations with sleep deprivation and determinants. Significantly more males were sleep deprived compared to females. Adults who attended residential school were more likely to report sleep deprivation compared to those that did not attend residential school. The same significant association was not observed between if study participant's parents and grandparents had attended residential school and sleep deprivation. Individuals that engaged in non-traditional use of tobacco/current smokers had a higher prevalence of sleep deprivation than those that did not use/smoke. There was a significantly lower risk of sleep deprivation amongst those who consumed one drink per week compared with those that did not drink. There was a higher prevalence of sleep deprivation in individuals who had sleep apnea compared with those that reported not having diagnosis of sleep apnea. Participants exposed to adverse housing conditions such as visible mold and moldy smell were significantly associated with a higher prevalence of sleep deprivation compared to individuals not exposed to these housing conditions. In addition, “afraid to sleep in your home”, “waking up during the night due to terrifying dreams or nightmares or flashback to a traumatic event” and “trouble going to sleep or stay asleep (nighttime insomnia symptoms)” were significantly associated with sleep deprivation. No associations were observed between use of prescription medications, sleep medication or traditional medicines and sleep deprivation.
Table 1.
Bivariable associations between sleep deprivation and risk factors (n = 567).
| Variables | Total |
Sleep Deprivation |
Unadjusted OR (95% CI) | P value | |
|---|---|---|---|---|---|
| n (%) | Yes n (%) | No n (%) | |||
| Demographics | |||||
| Sex (n = 567) | |||||
| Male | 248 (43.7) | 76 (52.8) | 172 (40.7) | 1.63 (1.12,2.39) | 0.012 |
| Female | 319 (56.3) | 68 (47.2) | 251 (59.3) | 1.00 | |
| Age group, in years (n = 567) | |||||
| 18-29 | 170 (30.0) | 36 (25.0) | 134 (31.7) | 1.00 | |
| 30-39 | 139 (24.5) | 35 (24.3) | 104 (24.6) | 1.25 (0.74, 2.13) | 0.406 |
| 40-49 | 94 (16.6) | 29 (20.1) | 65 (15.4) | 1.66 (0.94, 2.94) | 0.082 |
| 50-59 | 98 (17.3) | 23 (16.0) | 75 (17.7) | 1.14 (0.63, 2.07) | 0.663 |
| 60+ | 66 (11.6) | 21 (14.6) | 45 (10.6) | 1.74 (0.92, 3.28) | 0.088 |
| Body Mass Index (BMI) (n = 529) | |||||
| Obese | 247 (46.7) | 66 (49.6) | 181 (45.7) | 1.32 (0.80, 2.17) | 0.275 |
| Overweight | 148 (28.0) | 38 (28.6) | 110 (27.8) | 1.25 (0.72, 2.17) | 0.427 |
| Neither obese or nor overweight | 134 (25.3) | 29 (21.8) | 105 (26.5) | 1.00 | |
| Education level (n = 561) | |||||
| Less than secondary school graduation | 209 (37.3) | 50 (35.5) | 159 (37.9) | 0.91 (0.58, 1.44) | 0.687 |
| Secondary school graduation | 169 (30.1) | 44 (31.2) | 125 (29.8) | 1.02 (0.63, 1.64) | 0.940 |
| Some university/completed university/technical school | 183 (32.6) | 47 (33.3) | 136 (32.4) | 1.00 | |
| Employment status (n = 553) | |||||
| Social assistance/unemployment insurance | 129 (23.3) | 35 (25.2) | 94 (22.7) | 1.01 (0.60, 1.71) | 0.954 |
| Unemployed | 143 (25.9) | 29 (20.9) | 114 (27.5) | 0.69 (0.41, 1.18) | 0.180 |
| Other including retired or home makers | 117 (21.2) | 31 (22.3) | 86 (20.8) | 0.98 (0.57, 1.68) | 0.950 |
| Employed (full-time, part-time, self-employed) | 164 (29.7) | 44 (31.7) | 120 (29.0) | 1.00 | |
| Shift Worker (n = 567) | |||||
| Yes | 56 (9.9) | 14 (9.7) | 42 (9.9) | 0.98 (0.52, 1.85) | 0.943 |
| No | 511 (90.1) | 130 (90.3) | 381 (90.1) | 1.00 | |
| Money left at the end of the month (n = 561) | |||||
| Not enough money | 324 (57.8) | 91 (64.1) | 233 (55.6) | 1.30 (0.79, 2.13) | 0.295 |
| Just enough money | 120 (21.4) | 24 (16.9) | 96 (22.9) | 0.83 (0.45, 1.55) | 0.565 |
| Some money | 117 (20.9) | 27 (19.0) | 90 (21.5) | 1.00 | |
| Attend residential school (n = 567) | |||||
| Yes | 190 (33.5) | 58 (40.3) | 132 (31.2) | 1.49 (1.01, 2.20) | 0.047 |
| No | 377 (66.5) | 86 (59.7) | 291 (68.8) | 1.00 | |
| Parents or grandparents attended a residential school (n = 567) | |||||
| Yes | 488 (86.0) | 122 (84.8) | 366 (86.5) | 1.13 (0.54, 2.36) | 0.738 |
| No | 35 (6.2) | 12 (8.3) | 23 (5.5) | 1.77 (0.66, 4.78) | 0.257 |
| Do not know |
44 (7.8) |
10 (6.9) |
34 (8.0) |
1.00 |
|
| Life-style factors | |||||
| Smoking Status/Non-Traditional Use (n = 561) | |||||
| Current smoker | 402 (71.7) | 119 (82.6) | 283 (67.9) | 1.75 (1.00, 3.06) | 0.049 |
| Ex-smoker | 66 (11.8) | 7 (4.9) | 59 (14.1) | 0.49 (0.19, 1.26) | 0.141 |
| Never smoker | 93 (16.6) | 18 (12.5) | 75 (18.0) | 1.00 | |
| Marijuana Use (n = 562) | |||||
| Regularly | 162 (28.8) | 43 (30.3) | 119 (28.3) | 1.16 (0.75, 1.79) | 0.512 |
| Occasionally | 85 (15.2) | 24 (16.9) | 61 (14.5) | 1.26 (0.73, 2.16) | 0.402 |
| No use | 315 (56.0) | 75 (52.8) | 240 (57.2) | 1.00 | |
| Alcohol consumption per week (n = 397) | |||||
| More than 1 per week | 149 (37.5) | 42 (41.2) | 107 (36.3) | 0.92 (0.55, 1.55) | 0.752 |
| One-per week | 121 (30.5) | 22 (21.6) | 99 (33.6) | 0.52 (0.29, 0.95) | 0.032 |
| Non-drinker | 127 (32.0) | 38 (37.3) | 89 (30.2) | 1.00 | |
| Non-medical drugs (n = 563) | |||||
| Yes | 36 (6.4) | 9 (6.3) | 27 (6.4) | 0.99 (0.45, 2.15) | 0.975 |
| No | 527 (93.6) | 133 (93.7) | 394 (93.6) | 1.00 | |
| Physical activities at least 3 weeks (n = 528) | |||||
| Yes | 290 (54.9) | 75 (57.3) | 215 (54.2) | 1.13 (0.76, 1.69) | 0.537 |
| No | 238 (45.1) | 56 (42.7) | 182 (45.8) | 1.00 | |
| Screen time-2 hours or more (n = 431) | |||||
| Yes | 284 (65.9) | 73 (64.0) | 211 (66.6) | 0.89 (0.57, 1.40) | 0.626 |
| No |
147 (34.1) |
41 (36.0) |
106 (33.4) |
1.00 |
|
| Non-Communicable Diseases/Chronic Conditions | |||||
| Diabetes (n = 534) | |||||
| Yes | 98 (18.4) | 28 (20.6) | 70 (17.6) | 1.21 (0.74, 1.98) | 0.436 |
| No | 436 (81.6) | 108 (79.4) | 328 (82.4) | 1.00 | |
| High blood pressure (n = 513) | |||||
| Yes | 161 (31.4) | 48 (37.5) | 113 (29.4) | 1.44 (0.95, 2.20) | 0.086 |
| No | 352 (68.6) | 80 (62.5) | 272 (70.6) | 1.00 | |
| Heart problems (n = 531) | |||||
| Yes | 59 (11.1) | 17 (12.8) | 42 (10.6) | 1.24 (0.68, 2.27) | 0.479 |
| No | 472 (88.9) | 116 (87.2) | 356 (89.4) | 1.00 | |
| Stroke (n = 548) | |||||
| Yes | 16 (2.9) | 3 (2.2) | 13 (3.2) | 0.69 (0.19, 2.47) | 0.571 |
| No | 532 (97.1) | 133 (97.8) | 399 (96.8) | 1.00 | |
| Atrial fibrillation (n = 524) | |||||
| Yes | 12 (2.3) | 3 (2.3) | 9 (2.3) | 1.03 (0.27, 3.87) | 0.963 |
| No | 512 (97.7) | 125 (97.7) | 387 (97.7) | 1.00 | |
| Chronic obstructive pulmonary disease/emphysema (n = 530) | |||||
| Yes | 17 (3.2) | 5 (3.8) | 12 (3.0) | 1.25 (0.43, 3.63) | 0.677 |
| No | 513 (96.8) | 128 (96.2) | 385 (97.0) | 1.00 | |
| Asthma (n = 540) | |||||
| Yes | 66 (12.2) | 19 (14.0) | 47 (11.6) | 1.23 (0.70, 2.19) | 0.472 |
| No | 474 (87.8) | 117 (86.0) | 357 (88.4) | 1.00 | |
| Chronic Bronchitis (n = 541) | |||||
| Yes | 33 (6.1) | 10 (7.4) | 23 (5.7) | 1.33 (0.62, 2.88) | 0.465 |
| No | 508 (93.9) | 125 (92.6) | 383 (94.3) | 1.00 | |
| Sleep apnea (n = 513) | |||||
| Yes | 36 (7.0) | 14 (11.2) | 22 (5.7) | 2.09 (1.04, 4.24) | 0.039 |
| No | 477 (93.0) | 111 (88.8) | 366 (94.3) | 1.00 | |
| Acid Reflux (n = 545) | |||||
| Yes | 51 (31.0) | 51 (37.0) | 118 (29.0) | 1.44 (0.96, 2.16) | 0.081 |
| No | 376 (69.0) | 87 (63.0) | 289 (71.0) | 1.00 | |
| Hypothyroidism (n = 530) | |||||
| Yes | 43 (8.1) | 9 (6.8) | 34 (8.5) | 0.78 (0.36, 1.68) | 0.530 |
| No | 487 (91.9) | 123 (93.2) | 364 (91.5) | 1.00 | |
| Depression (n = 524) | |||||
| Yes | 162 (30.9) | 50 (36.8) | 112 (28.9) | 1.43 (0.95, 2.16) | 0.087 |
| No | 362 (69.1) | 86 (63.2) | 276 (71.1) | 1.00 | |
| Anxiety (n = 525) | |||||
| Yes | 168 (32.0) | 45 (33.8) | 123 (31.4) | 1.12 (0.74, 1.70) | 0.600 |
| No | 357 (68.0) | 88 (66.2) | 269 (68.6) | 1.00 | |
| Post-traumatic stress disorder (n = 529) | |||||
| Yes | 57 (10.8) | 16 (11.9) | 41 (10.4) | 1.17 (0.63, 2.16) | 0.615 |
| No | 472 (89.2) | 118 (88.1) | 354 (89.6) | 1.00 | |
| Parkinson's disease (n = 541) | |||||
| Yes | 7 (1.3) | 2 (1.5) | 5 (1.2) | 1.18 (0.23, 6.16) | 0.843 |
| No | 534 (98.7) | 135 (98.5) | 399 (98.8) | 1.00 | |
| Chronic pain (n = 544) | |||||
| Yes | 128 (23.5) | 38 (28.1) | 90 (22.0) | 1.39 (0.89, 2.16) | 0.146 |
| No | 416 (76.5) | 97 (71.9) | 319 (78.0) | 1.00 | |
| Kidney disease (n = 545) | |||||
| Yes | 23 (4.2) | 3 (2.2) | 20 (4.9) | 0.44 (0.13, 1.50) | 0.189 |
| No | 522 (95.8) | 133 (97.8) | 389 (95.1) | 1.00 | |
| Restless legs syndrome (RLS) (n = 542) | |||||
| Yes | 189 (34.9) | 56 (41.5) | 133 (32.7) | 1.46 (0.98, 2.18) | 0.064 |
| No |
353 (65.1) |
79 (58.5) |
274 (67.3) |
1.00 |
|
| Sleep environment | |||||
| Dampness (n = 562) | |||||
| Yes | 313 (55.7) | 84 (58.3) | 229 (54.8) | 1.15 (0.79, 1.69) | 0.460 |
| No | 249 (44.3) | 60 (41.7) | 189 (45.2) | 1.00 | |
| Visible mold (n = 561) | |||||
| Yes | 291 (51.9) | 89 (62.2) | 202 (48.3) | 1.76 (1.19, 2.60) | 0.004 |
| No | 270 (48.1) | 54 (37.8) | 216 (51.7) | 1.00 | |
| Moldy smell (n = 563) | |||||
| Yes | 281 (49.9) | 84 (58.3) | 197 (47.0) | 1.58 (1.08, 2.31) | 0.020 |
| No | 282 (50.1) | 60 (41.7) | 222 (53.0) | 1.00 | |
| Smoke inside house (n = 560) | |||||
| Yes | 242 (43.2) | 70 (49.0) | 172 (41.2) | 1.37 (0.93, 2.00) | 0.109 |
| No | 318 (56.8) | 73 (51.0) | 245 (58.8) | 1.00 | |
| Crowding (n = 556) | |||||
| >1 person/bedroom | 406 (73.0) | 106 (74.1) | 300 (72.6) | 1.08 (0.70, 1.66) | 0.730 |
| ≤ 1 person/bedroom |
150 (27.0) |
37 (25.9) |
113 (27.4) |
1.00 |
|
| Place of sleep (n = 435) | |||||
| Bedroom | 326 (74.9) | 83 (72.8) | 243 (75.7) | 0.77 (0.23, 2.56) | 0.668 |
| Living room | 52 (12.0) | 13 (11.4) | 39 (12.1) | 0.75 (0.19, 2.85) | 0.673 |
| Basement | 44 (10.1) | 14 (12.3) | 30 (9.3) | 1.05 (0.28, 4.00) | 0.943 |
| Other | 13 (3.0) | 4 (3.5) | 9 (2.8) | 1.00 | |
| Sleeping arrangement shared with (n = 558) | |||||
| Child | 114 (20.4) | 31 (21.8) | 83 (20.0) | 0.87 (0.45, 1.68) | 0.682 |
| Spouse or partner | 174 (31.2) | 42 (29.6) | 132 (31.7) | 0.74 (0.40, 1.38) | 0.345 |
| Alone | 200 (35.8) | 48 (33.8) | 152 (36.5) | 0.74 (0.40, 1.35) | 0.323 |
| Other family member/Other | 70 (12.5) | 21 (14.8) | 49 (11.8) | 1.00 | |
| Afraid to sleep in your home (n = 566) | |||||
| Yes | 58 (10.2) | 24 (16.8) | 34 (8.0) | 2.31 (1.32, 4.04) | 0.004 |
| No | 508 (89.8) | 119 (83.2) | 389 (92.0) | 1.00 | |
| Waking up during the night due to terrifying dreams or nightmares or flashback to a traumatic event (n = 564) | |||||
| Yes | 263 (46.6) | 80 (56.3) | 183 (43.4) | 1.68 (1.15, 2.47) | 0.008 |
| No | 301 (53.4) | 62 (43.7) | 239 (56.6) | 1.00 | |
| Trouble going to sleep or stay asleep (n = 562) | |||||
| Sometimes/most of the time/all of the time | 391 (69.6) | 115 (80.4) | 276 (65.9) | 2.13 (1.34, 3.37) | 0.001 |
| Never/Rarely | 171 (30.4) | 28 (19.6) | 143 (34.1) | 1.00 | |
| Prescription medication use (n = 559) | |||||
| Yes | 253 (45.3) | 67 (46.5) | 186 (44.8) | 1.07 (0.73, 1.57) | 0.723 |
| No | 306 (54.7) | 77 (53.5) | 229 (55.2) | 1.00 | |
| Medication use for sleep (n = 558) | |||||
| Yes | 66 (11.8) | 20 (13.9) | 46 (11.1) | 1.29 (0.73, 2.27) | 0.375 |
| No | 492 (88.2) | 124 (86.1) | 368 (88.9) | 1.00 | |
| Traditional medication use for sleep (n = 559) | |||||
| Yes | 30 (5.4) | 7 (4.9) | 23 (5.5) | 0.87 (0.37, 2.07) | 0.755 |
| No | 137 (95.1) | 392 (94.5) | 1.00 | ||
Odds ratios that are significantly different from zero (p < 0.05) are shown in bold.
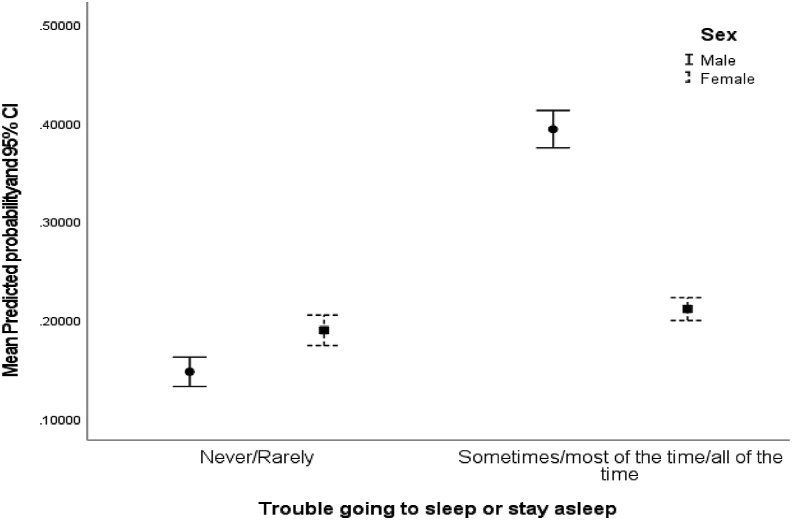
Multivariate logistic regression results are presented in Table 2. It was observed that those in the middle age group (age group 40–49: OR = 2.21; 95% CI (1.16, 4.23)) and older age group (age group 60+: OR = 2.53; 95% CI (1.24, 5.17)), had visible mold in the house (OR = 1.72; 95% CI (1.12, 2.64)), and males with nighttime insomnia symptoms were associated significantly with a higher prevalence of sleep deprivation compared to without nighttime insomnia symptoms (Fig. 1) after adjusting for other factors.
Table 2.
Adjusted odds ratios for associations between sleep deprivation and covariates.
| Variable | Multivariate Logistic Regression |
|
|---|---|---|
| Adjusted odds ratio (95% CI) | p value | |
| Demographics | ||
| Sex | ||
| Male | 0.76 (0.32, 1.83) | 0.539 |
| Female | 1.00 | |
| Age group, in years | ||
| 18-29 | 1.00 | |
| 30-39 | 1.69 (0.93, 3.07) | 0.085 |
| 40-49 | 2.21 (1.16, 4.23) | 0.016 |
| 50-59 | 1.63 (0.84, 3.17) | 0.151 |
| 60+ | 2.53 (1.24, 5.17) | 0.011 |
| Body Mass Index (BMI) | ||
| Obese | 1.32 (0.78, 2.25) | 0.298 |
| Overweight | 1.08 (0.59, 1.95) | 0.795 |
| Neither obese or nor overweight |
1.00 |
|
| Sleep environment | ||
| Visible mold | ||
| Yes | 1.72 (1.12, 2.64) | 0.013 |
| No | 1.00 | |
| Trouble going to sleep or stay asleep | ||
| Sometimes/most of the time/all of the time | 1.12 (0.57, 2.22) | 0.741 |
| Never/Rarely | 1.00 | |
| Interaction: Trouble going to sleep or stay asleep and Sex (SeeFig. 1) | ||
| Male X Sometimes/most of the time/all of the time (Ref: Never/Rarely) | 4.50 (2.17, 9.32) | 0.001 |
| Female X Sometimes/most of the time/all of the time (Ref: Never/Rarely) | 1.41 (0.57, 2.22) | 0.741 |
Odds ratios that are significantly different from zero (p < 0.05) are shown in bold.
Fig. 1.
Mean Predicted probability of sleep deprivation and trouble going to sleep or stay asleep by sex.
Mean predicted probability of sleep deprivation and trouble going to sleep or staying asleep (nighttime insomnia symptoms) by sex is presented in Fig. 1. Mean predicted probability was higher for males who had nighttime insomnia symptoms compared with those who did not have nighttime insomnia symptoms. There was no significant difference for females with and without nighttime insomnia symptoms.
4. Discussion
Sleep deprivation occurs when a person is not able to get the recommended number of hours of sleep. The prevalence of sleep deprivation among participants in two Cree First Nation communities in Saskatchewan was 25.4%. This prevalence of sleep deprivation was lower (25.4%) when compared with North American Indians/Alaska Native populations reported by Ehlers et al. (30%) [7] and Chapman et al. (34.2%) [62], but very close (26%) to the general population in Canada [1,2]. The results of this study demonstrated that those in the middle and older age groups, visible mold in the house, and males with nighttime insomnia symptoms were associated significantly with a higher prevalence of sleep deprivation after adjusting for other factors.
The amount of sleep needed to feel refreshed, and function well depends upon the individual and varies across the age groups [37]. In Canada, 1 in 4 adults aged 18–34 years; 1 in 3 adults aged 35–64 years and 1 in 4 adults aged 65–79 years are not getting the recommended sleep hours [2], which implies that compared to the middle aged groups, the older age group has a lower risk of sleep deprivation. One study suggests that older adults may actually be more tolerant of sleep deprivation than younger age groups [77]. However, the authors commented that further research was needed to clarify whether older adults were actually more resistant to the effects of sleep loss than younger adults. In this study, presented herein, it was observed that the middle age groups (30–39 years and 40–49 years) and older age group (60+ years) had an increased prevalence of sleep deprivation. There was a linear dose-dependent relationship between age and prevalence of sleep deprivation except for the age group 50–59 years. The preponderance of evidence showed that sleep quality and duration decreased with age [78,79].
As mentioned in the Introduction, housing conditions were poor in First Nation communities in Canada [[69], [70], [71]]. In the current study, 55.7% reported dampness, 51.9% reported visible mold and 49.9% reported moldy smell in the house in the two First Nation communities. Several studies suggest that living in damp or mouldy home environments in the house may be associated with sleep problems. In a cross-sectional study among adults in England, participants living in damp buildings were more likely to report sleep problems [72]. Another study of children reported increased risk for sleep problems in children exposed to visible mould or dampness in the house. Results were significant for any sleep problems (OR = 1.77 (1.21, 2.60)), and short sleep time (OR = 1.68 (1.09, 2.61)) [73]. In this study, it was found that there was an increased prevalence for sleep deprivation in adults exposed to visible mold (OR = 1.72 (1.12, 2.64)). This finding is very important, and points to further public health interventions on poor quality housing stock in First Nation communities. Housing in these communities is funded through federal transfer and has long been considered to be underfunded [80].
Several suggestions have been made by other authors for the possible mechanisms related to exposure to mold and sleep deprivation or disruption. One possible explanation is that damp and moldy environments (which contain beta-glucan) may cause fatigue [81,82], irritation and inflammation in mucus membranes or airways [83]. Another explanation is that moldy environments with higher levels of microbial volatile organic compounds (MVOCs) [[84], [85], [86]] can cause nasal inflammation [82,84,85,87,88], a well-known risk factor for sleep disturbances [89,90]. In addition, mold odors or unpleasant smells that are related to humid environments can impair sleep [82,91].
Finally, the multivariate results revealed that males who had nighttime insomnia symptoms compared to without nighttime insomnia symptoms were associated with significantly higher prevalence of sleep deprivation. The observed sex differences in sleep deprivation outcome is compelling, but not surprising in light of these associations. Other studies, did not report a sex effect on sleep-related outcomes in adults from Indigenous communities residing in the United States [7,92] or Canada [93]. Sabanayagam et al. [92] reported no significant difference in the reported average sleep duration between older (aged ≥ 55 years) Indigenous adult men and women. A few studies have reported a relationship between sleep deprivation and insomnia [94,95]. It has been suggested that objective measured short sleep duration was a risk factor for development of chronic insomnia from poor sleep defined by moderate to severe complaint of difficulty falling asleep, difficulty staying asleep, early awakening, or unrefreshing sleep [94]. The objective which measured short sleep duration was associated with a significantly higher prevalence for persistent insomnia as compared to normal sleep with an odds ratio of 3.19 [95]. Further studies are needed to confirm the relationship or influence of sex on insomnia or sleep deprivation.
This study considered potential associations between several co-morbidities and sleep deprivation but, none were significantly associated with sleep deprivation. In this study, several bivariate associations (p < 0.10) with sleep deprivation such as high blood pressure (hypertension), acid reflex, depression, sleep apnea and restless legs syndrome were observed but not retained in the multivariate regression model. There was sufficient evidence that short sleep duration acts as a risk factor for hypertension [45,49,50]. Also, others have reported an association between short sleep duration and a high risk of depression [51,53,96]. In addition, Sun et al. [53] identified a bidirectional relationship between sleep duration and depression. One study reported that sleep deprivation increased the number and length of apneic events in patients with sleep apnea and induced apnea in patients who snore [97]. This study did not identify any relationships between obesity [[24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34]], diabetes [29,[36], [37], [38], [39], [40]], heart problems [22,[37], [38], [39], [40], [41], [42], [43], [44]] and sleep deprivation, in contrast to other authors.
Most of the associations between circumstances and sleep deprivation reported in this paper were located as mid-level or proximal determinants of health, poor housing conditions in on reserves communities have been widely reported as having an impact on the health of First Nations peoples [98,99]. Participants from the two Saskatchewan First Nation communities in this study reported poor housing conditions with more than 50% noting dampness, visible mold, and crowding. Our research suggests other situations within the home are also implicated in sleep deprivation, such as being afraid to sleep. More proximally, participants reported high rates of overweight (28%) and obesity (46.7%). In total, about 75% of the population were considered to be overweight or obese. While not significantly associated with sleep deprivation in this study, others have reported an association between sleep loss and an increased risk of obesity [32,33]. More than half of the study participants were in the age groups of 18–29 years and 30–39 years, with more than 26% unemployed. More than half reported not having enough money left at the end of the month, a marker for poverty. These factors could be reasons for some of the findings observed in this study that showed the associations with sleep deprivation. Young adults may be more vulnerable to acute sleep deprivation than older adults [100]; as well, the use of electronic devices were found to be higher in younger adults [12]. It is important to note that these results also point to the significant influence of more upstream social and structural circumstances which are of particular relevance to Indigenous peoples in Canada. Residential school attendance was significantly associated with sleep deprivation in the bivariable analysis. This specific circumstance is a marker for historical and contemporary structures of colonization policy that have long been implicated in inequitable access to resources for the attainment of optimal health and in poorer health across numerous outcomes compared to the Canadian population overall [67,68,[101], [102], [103]].
This study has several strengths including: the number of participants from the two First Nation communities participating in this study; detailed information about sleep and sleep duration in the community; social and structural information including environmental housing conditions; and exploring medical histories. According to the Statistics Canada Census Profiles [104], overall, 42% (588/1397) of individuals participated in this cross-sectional study, which would be considered to be a very good participation rate. In Community A, the 18+ years population was 752 and 418 (56%) individuals participated. In Community B, the 18+ years population was 645 and 170 (26%) individuals participated. According to the Canadian Census of 2016 [104], the participants had a similar age distribution to the general population of these communities while there were more females who participated in this study and therefore, results may not be generalized to populations of these communities. Further studies are needed to confirm the relationships observed in this study on sleep deprivation.
However, several limitations also existed in this study. First, as these are cross-sectional observations, causation can only be speculative. Another potential limitation is that this study was based on self-reported data and therefore, there is potential for recall bias. Other potential limitations are: residual confounding due to additional confounding factors such as, details about ventilation, traffic noise, household illumination that were not collected in this study; misclassification of ever diagnosed non-communicable diseases/chronic disease conditions due to recall bias; and small sample cell sizes for some of the reported chronic conditions. An objective assessment of sleep quality and duration was not obtained. Results cannot be generalized to any other First Nations although the tools and applications used could be transferrable.
5. Conclusions
In these two First Nation communities, 25% of the participants reported sleep deprivation. Associated risk factors were older age group, visible mold in the house, and males with nighttime insomnia symptoms. This was a unique study, which evolved with two First Nation communities in Canada, and will be helpful in the management of patients with sleep deprivation in these communities; as well as for co-creating policy with the communities and future research priorities.
Author contributions
Conceptualization, J.A.D., S.A., M.K., P.P., D.R., S.K., N.K., M.F., R.S. and the First Nations Sleep Health Project Team; Data curation, B.P.R., K.M.; Formal analysis, C.P.K.; Funding acquisition, J.A.D., S.A., M.K. and P.P.; Investigation, J.A.D., S.A., M.F., M.K. and P.P.; Methodology, J. A. D., P.P., S. A., M. K., C.P.K., M. F.; Project administration, P.P.; Resources, J.S., C.B., R.S., M.F., T.S.; Supervision, J.A.D. and P.P.; Visualization, S.A., J.S., C.B. and V.R.R.; Writing—original draft, C.P.K., J.A.D., P.P.; Writing—review & editing, J.A.D., C.P.K., B.P.R., K.M., S.A., D.R., S.K., N.K., J.S., C.B., V.R.R., M.F., M.K., T.S., and P.P.
Funding
This research was funded by a grant from the Canadian Institutes of Health Research—“Assess, Redress, Re-assess: Addressing Disparities in Sleep Health among First Nations People”, CIHR MOP-391913-IRH-CCAA-11829-FRN PJT-156149.
Acknowledgments
The First Nations Sleep Health Project Team consists of: James A Dosman, MD (Designated Principal Investigator, University of Saskatchewan, Saskatoon, SK Canada); Punam Pahwa, PhD (Co-Principal Investigator, University of Saskatchewan, Saskatoon SK Canada); Malcolm King, PhD (Co-Principal Investigator, University of Saskatchewan, Saskatoon, SK Canada), Sylvia Abonyi, PhD (Co-Principal Investigator, University of Saskatchewan, Saskatoon, SK Canada); Co-Investigators: Mark Fenton, MD, Chandima P Karunanayake, PhD, Shelley Kirychuk, PhD, Niels Koehncke, MD, Joshua Lawson, PhD, Robert Skomro, MD, Donna Rennie, PhD, Darryl Adamko, MD; Collaborators: Roland Dyck, MD, Thomas Smith-Windsor, MD, Kathleen McMullin, MEd; Rachana Bodani, MD; John Gjerve, MD; Bonnie Janzen, PhD; and Vivian R Ramsden, RN, PhD; Gregory Marchildon, PhD; Kevin Colleaux, MD; Project Manager: Brooke Russell; Community Partners: Jeremy Seeseequasis, BA; Clifford Bird; Roy Petit; Edward Henderson; Raina Henderson; Dinesh Khadka. We are grateful for the contributions from Elders and community leaders that facilitated the engagement necessary for the study, and all participants.
Footnotes
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleepx.2021.100037.
Contributor Information
Chandima P. Karunanayake, Email: cpk646@mail.usask.ca.
Mark Fenton, Email: mef132@mail.usask.ca.
Robert Skomro, Email: r.skomro@usask.ca.
Vivian R. Ramsden, Email: viv.ramsden@usask.ca.
Shelley Kirychuk, Email: shelley.kirychuk@usask.ca.
Donna C. Rennie, Email: donna.rennie@usask.ca.
Jeremy Seeseequasis, Email: jccquasis@willowcreehealth.com.
Clifford Bird, Email: c.bird@sasktel.net.
Kathleen McMullin, Email: kathleen.mcmullin@usask.ca.
Brooke P. Russell, Email: bpr053@mail.usask.ca.
Niels Koehncke, Email: niels.koehncke@usask.ca.
Thomas Smith-Windsor, Email: dr.tom@sasktel.net.
Malcolm King, Email: malcolm.king@usask.ca.
Sylvia Abonyi, Email: sya277@mail.usask.ca.
Punam Pahwa, Email: pup165@mail.usask.ca.
James A. Dosman, Email: james.dosman@usask.ca.
Abbreviations
- FNSHP
First Nations Sleep Health Project
- BMI
Body Mass Index
- SD
Standard Deviation
- OR
Odds Ratio
- CI
Confidence Interval
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Hafner M., Stepanek M., Taylor J. Why sleep matters-the economic costs of insufficient sleep: a cross-country comparative analysis. Rand Health Q. 2017;6(4):11. https://www.rand.org/pubs/research_reports/RR1791.html PMID: 28983434; PMCID: PMC5627640. [PMC free article] [PubMed] [Google Scholar]
- 2.Public Health Agency of Canada . Public Health Agency of Canada; Ottawa, ON: 2019. Are Canadian adults getting enough sleep? Minister of Health. Canada 2019 Cat.: HP35–92/1-2018E-PDF | ISBN: 978-0-660-27683-0 | Pub.: 180292. [Google Scholar]
- 3.Chaput J.P., Wong S.L., Michaud I. Duration and quality of sleep among Canadians aged 18 to 79. Health Rep. 2017;28(9):28–33. [PubMed] [Google Scholar]
- 4.Zhu G., Catt M., Cassidy S. Objective sleep assessment in >80,000 UK mid-life adults: associations with sociodemographic characteristics, physical activity and caffeine. PloS One. 2019;14(12) doi: 10.1371/journal.pone.0226220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lallukka T., Sares-Jäske L., Kronholm E. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Publ Health. 2012;565:12. doi: 10.1186/1471-2458-12-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stamatakis K.A., Kaplan G.A., Roberts R.E. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehlers C.L., Wills D.N., Lau P. Sleep quality in an adult American Indian community sample. J Clin Sleep Med. 2017;13:385–391. doi: 10.5664/jcsm.6486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kline C.E. The bidirectional relationship between exercise and sleep: implications for exercise adherence and sleep improvement. Am J Lifestyle Med. 2014;8(6):375–379. doi: 10.1177/1559827614544437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolezal B.A., Neufeld E.V., Boland D.M. Interrelationship between sleep and exercise: a systematic review. Adv Prev Med. 2017;2017:1364387. doi: 10.1155/2017/1364387. Erratum in: Adv Prev Med. 2017;2017:5979510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carter B., Rees P., Hale L. Association between portable screen-based media device access or use and sleep outcomes: a systematic 25 review and meta-analysis. JAMA Pediatr. 2016;170:1202–1208. doi: 10.1001/jamapediatrics.2016.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartel K.A., Gradisar M., Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Hysing M., Pallesen S., Stormark K.M. Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open. 2015;5(1) doi: 10.1136/bmjopen-2014-006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patterson F., Malone S.K., Lozano A. Hanlon AL. Smoking, screen-based sedentary behavior, and diet associated with habitual sleep duration and chronotype: data from the UK biobank. Ann Behav Med. 2016;50(5):715–726. doi: 10.1007/s12160-016-9797-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamidovic A., de Wit H. Sleep deprivation increases cigarette smoking. Pharmacol Biochem Behav. 2009;93(3):263–269. doi: 10.1016/j.pbb.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakata A., Takahashi M., Haratani T. Association of active and passive smoking with sleep disturbances and short sleep duration among Japanese working population. Int J Behav Med. 2008;81:15. doi: 10.1080/10705500801929577. [DOI] [PubMed] [Google Scholar]
- 16.Angarita G.A., Emadi N., Hodges S. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addiction Sci Clin Pract. 2016;11:9. doi: 10.1186/s13722-016-0056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Irish L.A., Kline C.E., Gunn H.E. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23–36. doi: 10.1016/j.smrv.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buysse D.J. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cappuccio F.P., D'Elia L., Strazzullo P. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grandner M.A., Hale L., Moore M. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallicchio L., Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 22.Mullington J.M., Haack M., Toth M. Cardiovascular, inflammatory and metabolic consequences of sleep deprivation. Prog Cardiovasc Dis. 2009;51(4):294–302. doi: 10.1016/j.pcad.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall M.H., Muldoon M.F., Jennings J.R. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31:635–643. doi: 10.1093/sleep/31.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaput J.-P., Leblanc C., Perusse L. Risk factors for adult overweight and obesity in the Quebec Family Study: have we been barking up the wrong tree? Obesity (Silver Spring) 2009;17:1964–1970. doi: 10.1038/oby.2009.116. [DOI] [PubMed] [Google Scholar]
- 25.Chaput J.-P., Després J.P., Bouchard C. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity. 2007;15(1):253–261. doi: 10.1038/oby.2007.512. [DOI] [PubMed] [Google Scholar]
- 26.Chaput J.-P., Tremblay A. Insufficient sleep as a contributor to weight gain: an update. Curr Obes Rep. 2012;1(4):245–256. doi: 10.1007/s13679-012-0026-7. [DOI] [Google Scholar]
- 27.Spiegel K., Tasali E., Penev P. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 28.Taheri S., Lin L., Austin D. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. Publ Lib Sci Med. 2004;1(3):210–217. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McNeil J., Doucet E., Chaput J.-P. Inadequate sleep as a contributor to obesity and type 2 diabetes. Can J Diabetes. 2013;37:103–108. doi: 10.1016/j.jcjd.2013.02.060. [DOI] [PubMed] [Google Scholar]
- 30.Colten H.R. Institute of Medicine (US) Committee on Sleep Medicine and Research. In: Altevogt B.M., editor. Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC): National Academies Press (US) Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. 2006. p. 3.https://www.ncbi.nlm.nih.gov/books/NBK19961/ Available from: [PubMed] [Google Scholar]
- 31.Hasler G., Buysse D.J., Klaghofer R. The association between short sleep duration and obesity in young adults: a 13-year prospective study. SLEEP. 2004;27(4):661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 32.Beccuti G., Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14(4):402–412. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gangwisch J.E., Malaspina D., Boden-Albala B. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–1296. doi: 10.1093/sleep/28.10.1289. PMID: 16295214. [DOI] [PubMed] [Google Scholar]
- 34.Cooper C.B., Neufeld E.V., Dolezal B.A. Sleep deprivation and obesity in adults: a brief narrative review. BMJ Open Sport Exerc Med. 2018;4(1) doi: 10.1136/bmjsem-2018-000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaput J.P., Després J.P., Bouchard C. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–523. doi: 10.1093/sleep/31.4.517. PMID: 18457239; PMCID: PMC2279744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayas N.T., White D.P., Al-Delaimy W.K. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–384. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 37.Bandyopadhyay A. What is sleep deprivation? Am J Respir Crit Care Med. 2019;199:11–12. doi: 10.1164/rccm.1996P11. ATS Patient Education Series © 2019 American Thoracic Society. [DOI] [PubMed] [Google Scholar]
- 38.Gottlieb D.J., Punjabi N.M., Newman A.B. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 39.Spiegel K., Leproult R., Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 40.Reutrakul S., Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56–66. doi: 10.1016/j.metabol.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 41.Ayas N.T., White D.P., Manson J.E. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 42.Yaggi H.K., Concato J., Kernan W.N. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 43.Grandner M.A., Sands-Lincoln M.R., Pak V.M. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013;5:93–107. doi: 10.2147/NSS.S31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nagai M., Hoshide S., Kario K. Sleep duration as a risk factor for cardiovascular disease- a review of the recent literature. Curr Cardiol Rev. 2010;6(1):54–61. doi: 10.2174/157340310790231635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ko K.D. Link between short sleep duration and hypertension. Kr J Fam Med. 2017;38(3):169–170. doi: 10.4082/kjfm.2017.38.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gangwisch J.E., Heymsfield S.B., Boden-Albala B. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 47.Grandner M., Mullington J.M., Hashmi S.D. Sleep duration and hypertension: analysis of > 700,000 adults by age and sex. J Clin Sleep Med. 2018;14(6):1031–1039. doi: 10.5664/jcsm.7176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Faraut B., Touchette E., Gamble H. Short sleep duration and increased risk of hypertension: a primary care medicine investigation. J Hypertens. 2012;30(7):1354–1363. doi: 10.1097/HJH.0b013e32835465e5. [DOI] [PubMed] [Google Scholar]
- 49.Hwang H., Lee J., Lee S. The relationship between hypertension and sleep duration: an analysis of the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-3) Clin Hypertens. 2015;21(8) doi: 10.1186/s40885-015-0020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kumar A., Goel H., Nadar S.K. Short sleep duration and the risk of hypertension: snoozing away high blood pressure? J Hum Hypertens. 2019;33:174–176. doi: 10.1038/s41371-019-0177-z. [DOI] [PubMed] [Google Scholar]
- 51.Al-Abri M.A. Sleep deprivation and depression: a bi-directional association. Sultan Qaboos University Med J. 2015;15(1):e4–e6. [PMC free article] [PubMed] [Google Scholar]
- 52.Pilcher J.J., Huffcutt A.I. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19(4):318–326. doi: 10.1093/sleep/19.4.318. [DOI] [PubMed] [Google Scholar]
- 53.Sun Y., Shi L., Bao Y. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018;52:221–229. doi: 10.1016/j.sleep.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 54.Wu H., Dunnett S., Ho Y.S. The role of sleep deprivation and circadian rhythm disruption as risk factors of Alzheimer's disease. Front Neuroendocrinol. 2019;54:100764. doi: 10.1016/j.yfrne.2019.100764. [DOI] [PubMed] [Google Scholar]
- 55.Lemke M.K., Apostolopoulos Y., Hege A. Understanding the role of sleep quality and sleep duration in commercial driving safety. Accid Anal Prev. 2016;97:79–86. doi: 10.1016/j.aap.2016.08.024. [DOI] [PubMed] [Google Scholar]
- 56.Kling R.N., McLeod C.B., Koehoorn M. Sleep problems and workplace injuries in Canada. Sleep. 2010;33(5):611–618. doi: 10.1093/sleep/33.5.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Uehli K., Miedinger D., Bingisser R. Sleep quality and the risk of work injury: a Swiss case–control study. J Sleep Research. 2014;23:545–553. doi: 10.1111/jsr.12146. [DOI] [PubMed] [Google Scholar]
- 58.Graves J.M., Miller M.E. Reduced sleep duration and history of work-related injuries among Washington State adolescents with a history of working. Am J Ind Med. 2015;58:464–471. doi: 10.1002/ajim.22416. [DOI] [PubMed] [Google Scholar]
- 59.Choi S.W., Peek-Asa C., Sprince N.L. Sleep quantity and quality as a predictor of injuries in a rural population. Am J Emerg Med. 2006;24(2):189–196. doi: 10.1016/j.ajem.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 60.Lian Y., Xiao J., Liu Y. Associations between insomnia, sleep duration and poor work ability. J Psychosom Res. 2015;78(1):45–51. doi: 10.1016/j.jpsychores.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 61.Lockley S.W., Barger L.K., Ayas N.T. Harvard Work Hours, Health and Safety Group. Effects of health care provider work hours and sleep deprivation on safety and performance. Joint Comm J Qual Patient Saf. 2007;33(11 Suppl):7–18. doi: 10.1016/s1553-7250(07)33109-7. [DOI] [PubMed] [Google Scholar]
- 62.Chapman D.P., Croft J.B., Liu Y. Excess frequent insufficient sleep in American Indians/Alaska natives. J Environ Public Health. 2013;2013:259645. doi: 10.1155/2013/259645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y., Wheaton A.G., Chapman D.P. Prevalence of healthy sleep duration among adults – United States. MMWR Morb Mortal Wkly Rep. 2014;2016(65):137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 64.Aboriginal Affaires and Northern Development Canada (AANDC) Terminology. https://www.aadnc-aandc.gc.ca/eng/1358879361384/1358879407462 Available online:
- 65.University of British Columbia . 2020. First Nations studies program. Aboriginal identity & terminology.http://indigenousfoundations.arts.ubc.ca/aboriginal_identity__terminology/ Available online: [Google Scholar]
- 66.Greenwood M., de Leeuw S., Lindsay N.M., editors. Determinants of indigenous peoples' health in Canada: beyond the social. Canadian Scholars’ Press; Toronto, ON, Canada: 2015. p. 279. [Google Scholar]
- 67.Loppie Reading C., Wien F. National collaborating Centre for aboriginal health, University of Northern British Colombia; Prince George, BC: 2009. Health inequalities and social determinates of aboriginal peoples' health.https://www.ccnsa-nccah.ca/docs/determinants/RPT-HealthInequalities-Reading-Wien-EN.pdf Available online: [Google Scholar]
- 68.Canada’s Residential Schools . vol. 1. McGill-Queen’s University Press; Montreal & Kingston, ON, Canada: 2015. http://www.trc.ca/assets/pdf/Volume_1_History_Part_2_English_Web.pdf (The history, Part 2 1939 to 2000. The final report of the truth and reconciliation commission of Canada). Available online: [Google Scholar]
- 69.Statistics Canada. Census in brief: the housing conditions of aboriginal people in Canada; catalogue no. 98-200-X2016021. Statistics Canada; Ottawa, ON, Canada: 2017. http://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016021/98-200-x2016021-eng.pdf Available online: [Google Scholar]
- 70.Carrière G.M., Garner R., Sanmartin C. Housing conditions and respiratory hospitalizations among First Nations people in Canada. Health Rep. 2017;28:9–15. [PubMed] [Google Scholar]
- 71.Larcombe L., Nickerson P., Singer M. Housing conditions in 2 Canadian first Nations communities. Int J Circumpolar Health. 2011;70:141–153. doi: 10.3402/ijch.v70i2.17806. [DOI] [PubMed] [Google Scholar]
- 72.Packer C.N., Stewart-Brown S., Fowle S.E. Damp housing and adult health: results from a lifestyle study in Worcester, England. J Epidemiol Commun Health. 1994;48:555–559. doi: 10.1136/jech.48.6.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tiesler C.M.T., Thiering E., Tischer C. Exposure to visible mould or dampness at home and sleep problems in children: results from the LISAplus study. Environ Res. 2015;137:357–363. doi: 10.1016/j.envres.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 74.Canadian Institutes of Health Research . December 2018. Natural sciences and engineering research council of Canada, and social sciences and humanities research council. Tri-council policy statement: ethical conduct for research involving humans. [Google Scholar]
- 75.Hirshkowitz M., Whiton K., Albert S.M. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 76.Hosmer D.W., Lemeshow S., Sturdivant R.X. 3rd ed. John Wiley & Sons, Inc; Hoboken, NJ: 2013. Applied logistic regression. [Google Scholar]
- 77.Gooneratne N.S., Vitiello M.V. Sleep in older adults: normative changes, sleep disorders, and treatment options. Clin Geriatr Med. 2014;30(3):591–627. doi: 10.1016/j.cger.2014.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lavoie C.J., Zeidler M.R., Martin J.L. Sleep and aging. Sleep Sci Pract. 2018;3:2. doi: 10.1186/s41606-018-0021-3. [DOI] [Google Scholar]
- 79.Gadie A., Shafto M., Leng Y. How are age-related differences in sleep quality associated with health outcomes? An epidemiological investigation in a UK cohort of 2406 adults. BMJ Open. 2017;7(7):e014920. doi: 10.1136/bmjopen-2016-014920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patterson D.G., Dyck L.E. Standing Senate Committee on Aboriginal Peoples; 2015. On-reserve housing and infrastructure: recommendations for change.https://sencanada.ca/content/sen/Committee/412/appa/rep/rep12jun15-e.pdf Available online: [Google Scholar]
- 81.Wan G.H., Li C.S. Indoor endotoxin and glucan in association with airway inflammation and systemic symptoms. Arch Environ Health. 1999;54:172–179. doi: 10.1080/00039899909602256. [DOI] [PubMed] [Google Scholar]
- 82.Janson C., Norback D., Omenaas E. Insomnia is more common among subjects living in damp buildings. Occup Environ Med. 2005;62:113–118. doi: 10.1136/oem.2003.011379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thorn J., Rylander R. Airways inflammation and glucan in a rowhouse area. Am J Respir Crit Care Med. 1998;157:1798–1803. doi: 10.1164/ajrccm.157.6.9706081. [DOI] [PubMed] [Google Scholar]
- 84.Walinder R., Norback D., Wessen B. Nasal lavage biomarkers: effect of water damage and microbial growth in an office building. Arch Environ Health. 2001;56:30–36. doi: 10.1080/00039890109604052. [DOI] [PubMed] [Google Scholar]
- 85.Wieslander G., Norback D., Nordstrom K. Nasal and ocular symptoms, tear film stability and biomarkers in nasal lavage, in relation to building-dampness and building design in hospitals. Int Arch Occup Environ Health. 1999;72:451–461. doi: 10.1007/s004200050398. [DOI] [PubMed] [Google Scholar]
- 86.WHO . World Health Organization; Geneva: 2009. WHO guidelines for indoor air quality: dampness and mould. [PubMed] [Google Scholar]
- 87.Wieslander G., Norback D., Venge P. Changes of symptoms, tear film stability and eosinophilic cationic protein in nasal lavage fluid after re-exposure to a damp office building with a history of flooding. Indoor Air. 2007;17:19–27. doi: 10.1111/j.1600-0668.2006.00441.x. [DOI] [PubMed] [Google Scholar]
- 88.Wieslander G., Kumlin A., Norback D. Dampness and 2-ethyl-1-hexanol in floor construction of rehabilitation center: health effects in staff. Arch Environ Occup Health. 2010;65:3–11. doi: 10.1080/19338240903390248. [DOI] [PubMed] [Google Scholar]
- 89.Bengtsson C., Jonsson L., Holmstrom M. Impact of nasal obstruction on sleep quality: a community-based study of women. Eur Arch Otorhinolaryngol. 2015;272:97–103. doi: 10.1007/s00405-014-3067-6. [DOI] [PubMed] [Google Scholar]
- 90.Hellgren J., Omenaas E., Gislason T. Perennial non-infectious rhinitis–an independent risk factor for sleep disturbances in Asthma. Respir Med. 2007;101:1015–1020. doi: 10.1016/j.rmed.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 91.Shiue I. Indoor mildew odour in old housing was associated with adult allergic symptoms, asthma, chronic bronchitis, vision, sleep and self-rated health: USA NHANES, 2005-2006. Environ Sci Pollut Res Int. 2015;22:14234–14240. doi: 10.1007/s11356-015-4671-8. [DOI] [PubMed] [Google Scholar]
- 92.Sabanayagam C., Shankar A., Buchwald D. Insomnia symptoms and cardiovascular disease among older American Indians: the Native Elder Care Study. J Environ Public Health. 2011;2011:964617. doi: 10.1155/2011/964617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Froese C.L., Butt A., Mulgrew A. Depression and sleep-related symptoms in an adult, indigenous, North American population. J Clin Sleep Med. 2008;4(4):356–361. [PMC free article] [PubMed] [Google Scholar]
- 94.Fernandez-Mendoza J., Vgontzas A.N., Bixler E.O. Clinical and polysomnographic predictors of the natural history of poor sleep in the general population. Sleep. 2012;35(5):689e97. doi: 10.5665/sleep.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vgontzas A.N., Fernandez-Mendoza J., Bixler E.O. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35(1):61–68. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li Y., Wu Y., Zhai L. Longitudinal association of sleep duration with depressive symptoms among middle-aged and older Chinese. Sci Rep. 2017;11794:7. doi: 10.1038/s41598-017-12182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bonnet M.H., Arand D.L. Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Med Rev. 2003;7(4):297–310. doi: 10.1053/smrv.2001.0245. [DOI] [PubMed] [Google Scholar]
- 98.National Collaborating Centre for Aboriginal Health . National Collaborating Centre for Aboriginal Health; Prince George, BC: 2017. Housing as a social determinant of first Nations, Inuit and Métis health.https://www.ccnsa-nccah.ca/docs/determinants/FS-Housing-SDOH2017-EN.pdf Available from: [Google Scholar]
- 99.Office of the Auditor General of Canada . Ministry of Public Works and Government Services; Ottawa, ON: 2003. Report of the auditor general of Canada to the house of commons: chapter 6- federal government support to first Nations – housing on reserves.https://www.oag-bvg.gc.ca/internet/docs/20030406ce.pdf Available from: [Google Scholar]
- 100.Zitting K.M., Münch M.Y., Cain S.W. Young adults are more vulnerable to chronic sleep deficiency and recurrent circadian disruption than older adults. Sci Rep. 2018;8(1):11052. doi: 10.1038/s41598-018-29358-x. Published 2018 Jul 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Leeuw S., Lindsay N.M., Greenwood M. Introduction: rethinking determinants of indigenous people's health in Canada. In: Greenwood M., de Leeuw S., Lindsay N.M., editors. Determinants of indigenous peoples' health in Canada: beyond the social. Canadian Scholars’ Press Inc; Toronto: 2015. [Google Scholar]
- 102.Reading C. Chapter 1: structural determinants of aboriginal people's health. In: Greenwood M., de Leeuw S., Lindsay N.M., editors. Determinants of indigenous peoples' health in Canada: beyond the social. Canadian Scholars’ Press Inc; Toronto: 2015. [Google Scholar]
- 103.Kim P.J. Social determinants of health inequities in Indigenous Canadians through a life course approach to colonialism and the residential school system. Health Equity. 2019;3(1):378–381. doi: 10.1089/heq.2019.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Statistics Canada. Census Profile . 2016. Census.https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E Available online from: Date modified: 2020-03-31. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1