Abstract
BACKGROUND & AIMS:
Bleeding is the most common severe complication after endoscopic mucosal resection of large colon polyps and is associated with significant morbidity and cost. We examined whether prophylactic closure of the mucosal defect with hemoclips after polyp resection reduces the risk of bleeding.
METHODS:
We performed a multicenter, randomized trial of patients with a large nonpedunculated colon polyp (≥20 mm) at 18 medical centers in North America and Spain from April 2013 through October 2017. Patients were randomly assigned to groups that underwent endoscopic closure with a clip (clip group) or no closure (control group) and followed. The primary outcome, postprocedure bleeding, was defined as a severe bleeding event that required hospitalization, a blood transfusion, colonoscopy, surgery, or another invasive intervention within 30 days after completion of the colonoscopy. Subgroup analyses included postprocedure bleeding with polyp location, polyp size, or use of periprocedural antithrombotic medications. We also examined the risk of any serious adverse event.
RESULTS:
A total of 919 patients were randomly assigned to groups and completed follow-up. Postprocedure bleeding occurred in 3.5% of patients in the clip group and 7.1% in the control group (absolute risk difference [ARD] 3.6%; 95% confidence interval [CI] 0.7%–6.5%). Among 615 patients (66.9%) with a proximal large polyp, the risk of bleeding in the clip group was 3.3% and in the control group was 9.6% (ARD 6.3%; 95% CI 2.5%–10.1%); among patients with a distal large polyp, the risks were 4.0% in the clip group and 1.4% in the control group (ARD –2.6%; 95% CI –6.3% to –1.1%). The effect of clip closure was independent of antithrombotic medications or polyp size. Serious adverse events occurred in 4.8% of patients in the clip group and 9.5% of patients in the control group (ARD 4.6%; 95% CI 1.3%–8.0%).
CONCLUSIONS:
In a randomized trial, we found that endoscopic clip closure of the mucosal defect following resection of large colon polyps reduces risk of postprocedure bleeding. The protective effect appeared to be restricted to large polyps located in the proximal colon. ClinicalTrials.gov no: NCT01936948.
Keywords: Colonoscopy, Polyp Resection, Endoscopic Mucosal Resection, Complications
Graphical Abstract
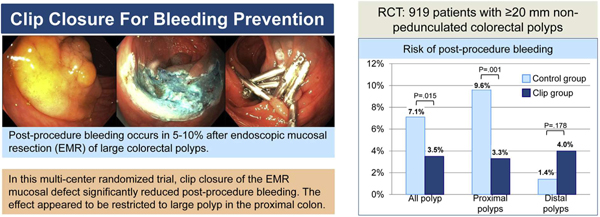
Resection of colorectal polyps is one of the most frequently performed medical interventions, and removal of precancerous polyps is an important means of reducing cancer incidence and mortality. Although most colorectal polyps are small, larger ones represent a higher cancer risk and their careful, complete, and timely removal is especially critical. Endoscopic resection has replaced surgical resection as the primary treatment for large colon polyps because of a lower morbidity and less need for hospitalization.1–4 Postprocedure bleeding is the most common severe complication, occurring in 2% to 24% of patients.5–13 Proximal polyp location in the colon, polyp size, and use of antithrombotic medications are factors that have been associated with an increased risk of postprocedure bleeding.12–17 Because of the related need for hospitalization, possible blood transfusion, and a repeat colonoscopy, and occasional death, efforts have focused on interventions to reduce the risk of postprocedure bleeding.
Preliminary research has suggested that closing the mucosal defect with clips after resection of large colon polyps might reduce the risk of postprocedure bleeding (Supplementary Figure 1). In a retrospective study, patients who underwent clip closure of the resection had a lower incidence of postprocedure bleeding compared with historical control subjects who did not undergo clip closure following polyp resection.12 Similarly, a prospective cohort study and a single-center randomized trial reported a lower risk of postprocedure bleeding following clip closure.13,18 Retrospective design, patient selection, nonstandardized resection method, and lack of a control group limit the validity and generalizability of the reported results. It is therefore unknown whether prophylactic clip closure of the mucosal defect after removal of large colon polyps truly reduces the risk of postprocedure bleeding.
We therefore conducted a multicenter randomized trial to compare the absolute risk of postprocedure bleeding of closing vs not closing the mucosal defect with clips after resection of large nonpedunculated colon polyps. We further examined the risk of overall complications between both strategies.
Methods
Patient Selection and Study Design
This multicenter randomized trial enrolled participants across 18 medical centers (16 in the United States, 1 in Canada, 1 in Spain) between April 2013 and October 2017. Participants were assigned in a 2 × 2 factorial design to endoscopic clip closure or no clip closure of the mucosal defect after resection of a large (≥20 mm) colon polyp, and to 1 of 2 electrocautery settings: a combination of cutting and coagulation current (“EndoCut”) or pure coagulation current (“forced coagulation”) using the Erbe electrocautery unit (Erbe Inc., Tübingen, Germany). Clip closure was the primary intervention. Because use of electrocautery settings varies among endoscopists, we randomized the setting to minimize an effect of electrocautery on the primary outcome. Using a computer-generated randomization list, eligible patients were assigned to 1 of 4 randomization groups in blocks of 8 stratified by center. Group assignment was kept in sequentially numbered concealed envelopes, which were opened after patient and polyp inclusion criteria were met, and after assessing the polyp for resection during the colonoscopy. The randomization was done before initiating the endoscopic mucosal resection (EMR) to minimize the potential for polyp selection bias.
All patients between 18 and 89 years of age with a ≥20-mm nonpedunculated polyp were potentially eligible for the study. Patients were excluded if they had inflammatory bowel disease, were in poor health (American Society of Anesthesiologists class IV), had a coagulopathy (international normalized ratio ≥1.5, platelets <50), or a poor bowel preparation quality.19 Polyps with a pedunculated (Paris Ip), subpedunculated (Paris Isp), or ulcerated (Paris III) morphology20 and those with proven invasive cancer were excluded. The study was approved by the institutional ethical review boards and registered at clinicaltrials.gov (NCT01936948). All participants gave written informed consent.
Procedure
Preparation for the colonoscopy followed usual care at each participating center. After identification of a potential study polyp, the polyp was assessed for eligibility and polyp characteristics were documented. Polyp size was measured by aligning a snare of known size with the polyp. All study polyps were removed by EMR.21 First, submucosal injection was performed to lift the polyp from the muscularis propria layer and provide a safety cushion for resection. The lifting solution contained a solute (eg, NaCl, or a viscous fluid such as hydroxyethyl starch) and a contrast agent (eg, methylene blue or indigo carmine). The polyp was then removed by electrocautery snare resection. Following resection of the polyp, clip closure was attempted in all patients in the clip group (Resolution clip until September 2016, Resolution 360 clips starting October 2016, both Boston Scientific, Inc., Marlborough, MA). A defect was considered completely closed when opposite defect margins were drawn together by clips that were less than 1 cm apart.12 For patients in the control group, endoscopists were permitted to deviate from the group assignment and close the mucosal defect with clips if considered clinically necessary (eg, concern about immediate or delayed perforation). The time of resection was defined as the time from starting the submucosal injection to completion of polyp removal. If more than one polyp was found that met the polyp inclusion criteria, it followed the same randomization allocation (randomization by patient). Periprocedural antithrombotic medications were managed according to professional society guidelines.22,23 The treating endoscopist instructed the patients on any postprocedure dietary restrictions and when to resume antithrombotic medications.
Histopathology examination of polyps was performed at each participating center’s pathology department.
Outcomes
The primary outcome was the occurrence of postprocedure bleeding following polyp resection. Postprocedure bleeding was defined as a severe bleeding event that required hospitalization, a blood transfusion, a colonoscopy, surgery, or any other invasive intervention to control bleeding, and that occurred after the patient left the endoscopy unit and within 30 days after completion of the colonoscopy. In prespecified subgroup analysis, we further examined whether the effect of clip closure was affected by location of the polyp in the colon (proximal vs distal location), by polyp size, electrocautery setting, and by use of periprocedural antithrombotic agents. Proximal location was defined as the hepatic flexure, the ascending colon, or the cecum, with the remainder of the colon defined as distal location.24 Antithrombotic use was defined as using an antiplatelet agent within 7 days of the resection, or an anticoagulant (warfarin or novel anticoagulant) within 5 days of the resection, and/or reinitiating these medications within 7 days following the procedure.
Secondary outcomes of interest included the incidence of overall serious adverse events.25 Complications were assessed by phone call or during a clinic visit at least 30 days after the procedure and review of medical records. All serious adverse events were reported to and reviewed by a data safety monitoring board.
Analysis
For the sample size calculation, we assumed an 8% incidence of severe delayed bleeding events among controls,5,8–10,26 and considered a reduction to 3% as clinically important. We further anticipated that clip closure would not be possible for 20% of patients related to polyp size or location. Assuming a 2-sided alpha of 0.05 and a power of 80% the study would need to randomize 920 subjects.
The primary analysis was according to the intention-to-treat principle that included all randomized patients with 30-day follow-up information (Supplementary Figure 2). In addition, we performed a per-protocol analysis of all patients who underwent the assigned treatment.
Primary and secondary outcomes are expressed as absolute risks and were compared using the χ2 test or Fisher’s exact test when appropriate. We provide absolute risk differences (ARDs) with a 95% confidence interval (CI) between the clip and control groups. Normally distributed variables are presented as means with standard deviation and compared using the Student t test. Non-normally distributed variables are presented as medians with interquartile range (IQR) and compared with the Mann-Whitney-Wilcoxon test. We applied the Mantel-Haenzel test for interaction to examine whether differences in subgroup analyses were independent of the primary comparison. We used multivariable logistic regression to determine whether the association between clip closure and bleeding risk was affected by the imbalance in antithrombotic medication use between the 2 arms. We further calculated the number needed to treat to prevent one postprocedure bleeding for relevant outcomes.
Two interim analyses were performed and reviewed by an independent data safety monitoring board after 25% and 50% of enrollment goal was achieved. The analyses assessed for futility for the entire cohort and among subgroups of patients on antithrombotic agents, patients with polyps ≥40 mm in size, and by polyp location in the colon. Because interim analyses required “alpha spending,” a 2-sided P value of .044 was considered significant for the primary analysis. To facilitate text presentation, results were rounded; the tables provide more precision. All authors reviewed and approved the final manuscript.
All co-authors had access to the study data and had reviewed and approved the final manuscript.
Results
Patients
A total of 1390 patients were assessed for eligibility and 928 patients were randomized at 18 centers (Supplementary Figure 2). Follow-up was not available for 9 patients; 919 patients with 989 study polyps were included in the intention-to-treat analysis. Of these, 902 patients (98%) were referred for polyp resection. Forty-four endoscopists removed a median of 11 study polyps (IQR 2, 32). Before study commencement these endoscopists performed a median of 40 colorectal EMRs annually (IQR 20, 80). Baseline characteristics between the groups were similar, except for the proportion of patients on antithrombotic medications was greater in the control group (Table 1). Characteristics of study polyps and their mode of resection were comparable (Table 2).
Table 1.
Characteristics of the Patients at Baseline
| Characteristics | Clip group (n = 455) |
Control group (n = 464) |
|---|---|---|
| Patients | ||
| Age, y, mean (SD) | 65.1 (9.5) | 65.1 (9.8) |
| Male sex, n (%) | 265 (58.2) | 282 (60.8) |
| Race or ethnic group, n (%) | ||
| Non-Hispanic white | 399 (87.7) | 415 (89.4) |
| Non-Hispanic black | 34 (7.3) | 28 (6.0) |
| Hispanic | 12 (2.6) | 14 (3.0) |
| Asian | 4 (0.9) | 3 (0.6) |
| Other/Unknown | 6 (1.3) | 4 (0.9) |
| Body mass index, mean (SD) | 29.1 (6.0) | 29.2 (5.9) |
| ASA class, n (%) | ||
| I | 40 (8.8) | 39 (8.4) |
| II | 255 (56.0) | 251 (54.1) |
| III | 160 (35.2) | 174 (37.5) |
| Periprocedural antithrombotic medications, n (%) | 116 (25.5) | 152 (32.8)a |
| Antiplatelet agents | 101 (22.2) | 130 (28.0)b |
| Anticoagulants | 20 (4.4) | 29 (6.2) |
| Procedure | ||
| Sedation, n (%) | ||
| No sedation | 5 (1.1) | 1 (0.2) |
| Moderate sedation | 57 (12.6) | 58 (12.5) |
| Monitored anesthesia care | 393 (86.4) | 405 (87.3) |
| Quality of bowel preparation, n (%) | ||
| Excellent | 126 (27.7) | 119 (25.6) |
| Good | 254 (55.9) | 271 (58.4) |
| Fair | 75 (16.5) | 74 (15.9) |
| Electrocautery, n (%) | ||
| Forced coagulation | 228 (50.1) | 230 (49.6) |
| EndoCut | 227 (49.9) | 234 (50.4) |
| Any additional polyp (any size), n (%) | 197 (43.4) | 206 (44.4) |
| More than one ≥20-mm study polyp, n (%) | 28 (6.2) | 32 (6.9) |
ASA, American Society of Anesthesiologists.
P = .015.
P = .042.
Table 2.
Characteristics of Study Polyps and Polyp Resection
| Characteristics | Clip group (n = 490) |
Control group (n = 499) |
|---|---|---|
| Size, median, mm (IQR) | 30 (22,35) | 28 (22,35) |
| Location, n (%) | ||
| Proximal | 327 (66.7) | 331 (66.3) |
| Distal | 163 (33.3) | 168 (33.7) |
| Morphology,a n (%) | ||
| Sessile | 208 (42.4) | 210 (42.1) |
| Flat | 282 (57.6) | 289 (57.9) |
| Histology, n (%) | ||
| Tubular adenoma | 213 (43.5) | 216 (43.3) |
| Tubulo-villous or villous adenoma | 104 (21.2) | 108 (21.6) |
| Serrated lesionb | 115 (23.5) | 105 (21.0) |
| High grade dysplasia | 42 (8.6) | 50 (10.0) |
| Cancer | 13 (2.7) | 13 (2.6) |
| Other | 3 (0.6) | 7 (1.4) |
| Prior resection attempts, n (%) | 65 (13.3) | 59 (11.8) |
| Difficulties with position during resection,n (%) | ||
| Minor | 314 (64.1) | 334 (66.9) |
| Moderate/severe | 176 (35.9) | 165 (33.1) |
| Submucosal lifting,c n (%) | ||
| Complete | 391 (80.5) | 400 (81.0) |
| Partial | 89 (18.3) | 90 (18.2) |
| Non-lifting | 6 (1.2) | 4 (0.8) |
| Adjunctive ablation,d n (%) | ||
| Residual polyp | 107 (21.8) | 118 (23.6) |
| Blood vessels for bleeding prevention | 41 (8.4) | 53 (10.6) |
| Time of Resection, median minutes (IQR)e | 17 (10, 30) | 17 (10, 29) |
| Clip closure of the mucosal defect, n (%) | ||
| Complete | 335 (68.4) | 29 (5.8) |
| Partial | 90 (18.4) | 21 (4.2) |
| Not closed | 65 (13.3) | 449 (90.0) |
Sessile was defined as a polyp with a Paris Is component. Flat was defined as a polyp with Paris IIa, IIB, or IIc components.20
Includes 8 hyperplastic polyps, 198 sessile serrated adenomas/polyps, and 14 traditional serrated adenomas.
Missing: n = 9.
Ablative therapies include argon plasma coagulation, hot forceps avulsion, and snare tip soft coagulation.
Defined as the time from starting the submucosal injection to completion of resection (does not include clipping).
Clip closure was not performed in 58 patients (13%) in the clip arm. In most cases, this was related to the size of the postpolypectomy defect (Supplementary Figure 2). The proportion of resection defects that could not be closed was similar in the proximal and distal colon (13% vs 14%), and greater for ≥40-mm polyps than for <40-mm polyps (33% vs 7%, P < .001). In the control group, 47 patients (10%) underwent clip closure of the resection defect, mostly related to concerns for bleeding or perforation.
Primary Outcome
Postprocedure bleeding was observed in 16 patients (3.5%) in the clip group, and in 33 patients (7.1%) in the control group (P = .015), with an ARD of 3.6% (95% CI 0.7–6.5) (Figure 1). Among those with postprocedure bleeding, bleeding started at a median of 7 days after the procedure in the clip group and 1 day in the control group (P = .008) (Supplementary Table 1). There was no difference in length of stay or need for blood transfusions. A higher proportion of patients in the control group underwent a colonoscopy to control bleeding compared with the intervention group, but this was not statistically significant. The number of patients who needed to be treated to prevent 1 postprocedure bleeding episode was 28.
Figure 1.
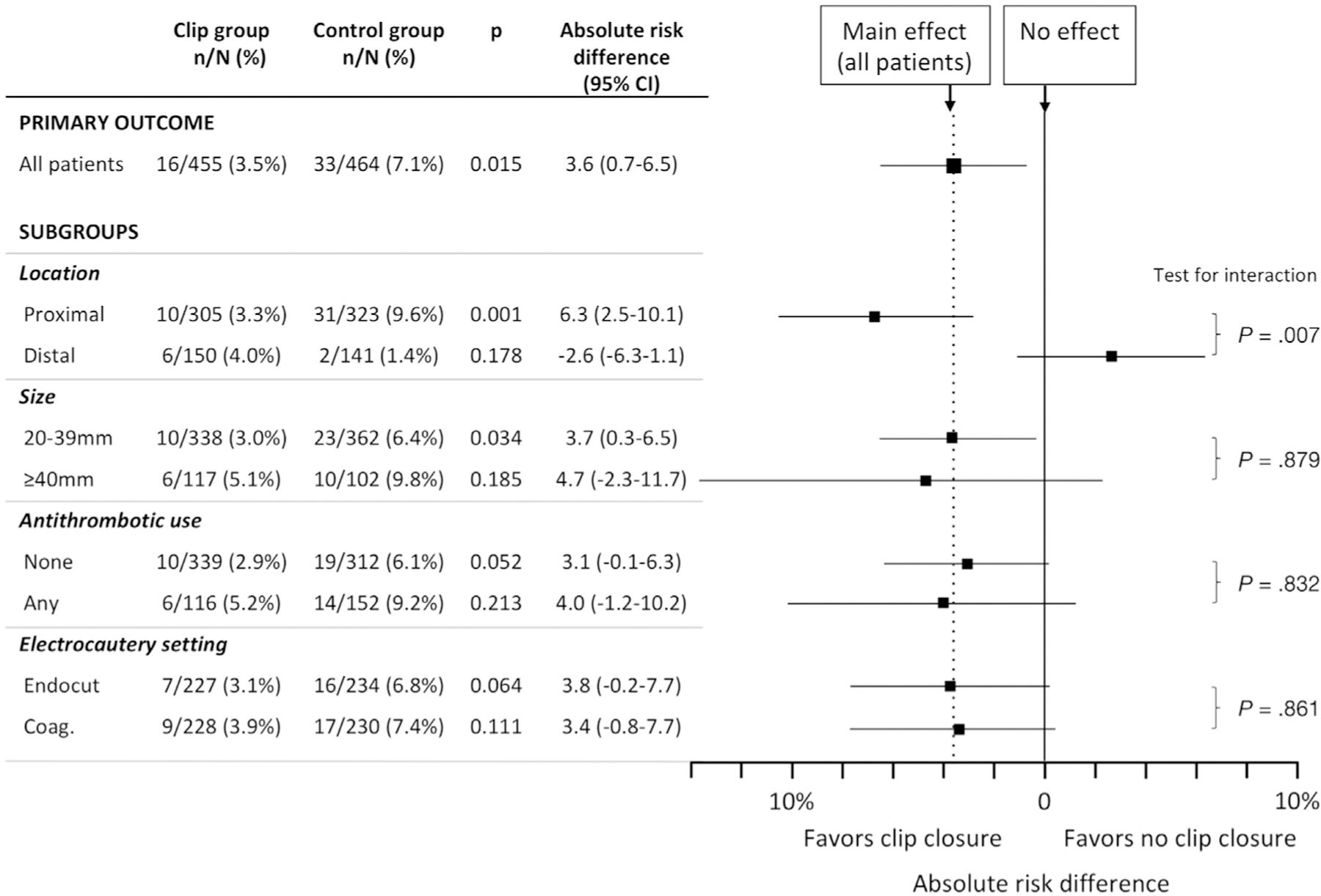
Postprocedure bleeding, primary outcome and subgroup analyses.
Subgroup Analyses
In subgroup analysis, a lower risk of postprocedure bleeding in the clip group compared with the control group was observed only among patients who had a proximal polyp with an ARD of 6.3% (95% CI 2.5–10.1) (Figure 1). No significant difference between the clip and control groups was seen following resection of distal polyps, with an ARD of −2.6 (95% CI −6.3 to 1.1). Although we observed a greater bleeding risk with increased polyp size and use of antithrombotic medications, the ARDs in post-procedure bleeding events between the clip and control groups were similar. The 2 types of applied electrocautery settings resulted in a similar risk of postprocedure bleeding overall and a similar reduction in the risk of postprocedure bleeding in the clip group compared with the control group.
When testing for independence, the effect of clip closure on postprocedural bleeding was dependent on proximal location (P = .007), but not on size, use of antithrombotic medications, or electrocautery setting. The main result did not change when adjusting for antithrombotic use (crude odds ratio 0.48, 95% CI 0.32–0.71; adjusted odds ratio 0.50, 95% CI 0.34–0.73).
The number of patients with a proximal large polyp who needed to be treated to prevent 1 postprocedure bleeding is 16.
The median number of clips to completely close the resection defect for any polyp was 4 (IQR 3, 6), with no difference in the number of clips used for distal or proximal polyps. In explorative analysis we did not find a difference in the frequency of postprocedure bleeding during the time the Resolution clip was used (ARD between groups 3.4%) and the Resolution-360 clip was used (ARD 3.8%; P [test for interaction] = .618).
Serious Adverse Events
Any serious adverse event occurred in 22 patients (4.8%) in the clip group and in 44 patients (9.5%) in the control group (P = .006) (Table 3). Aside from post-procedure bleeding, 6 patients (1.3%) in the clip group and 11 patients (2.4%) in the control group suffered a serious adverse event. There were no significant differences with respect to type of adverse events; however, perforations were more frequently observed in the control group (n = 6) than in the clip group (n = 3). All delayed perforations (n = 3) and all patients who required surgery (n = 3) occurred in the control group. As a result of a severe adverse event, a greater proportion of patients in the control group underwent a colonoscopy when compared with the clip group (4.5% vs 1.5%, P = .011). When colonoscopy was performed for postprocedure bleeding, signs of prior or ongoing bleeding were seen at the prior polyp resection site in 86% of patients in both groups. A similar proportion in either group received a blood transfusion (95% CI 1.5% vs 0.7%, P = .341).
Table 3.
Severe Adverse Events
| Outcomes | Clip group (n = 455) |
Control group (n = 464) |
P |
|---|---|---|---|
| SAE, n (%) | 22 (4.8) | 44 (9.5) | .006 |
| Postprocedure hemorrhage | 16 (3.5) | 33 (7.1) | .015 |
| Other SAE | 6 (1.3) | 11 (2.4) | .237 |
| Intraprocedural bleeding | 1 (0.2) | 0 | .312 |
| Abdominal pain | 1 (0.2) | 2 (0.4) | .575 |
| Perforation | 3 (0.7) | 6 (1.3) | .329 |
| Postpolypectomy syndrome | 1 (0.2) | 1 (0.2) | .989 |
| Other | 0 | 2 (0.4)a | .161 |
| SAE intervention, n (%) | |||
| Colonoscopy | 7 (1.5) | 21 (4.5) | .011 |
| Bleeding at resection site | 6 of 7 | 18 of 21 | |
| Blood transfusion | 3 (0.7) | 7 (1.5) | .341 |
| SAE outcome, n (%) | |||
| Resolved (no surgery) | 22 (100) | 38 (86.4) | .069 |
| Surgery | 0 | 4 (9.1) | .144 |
| Death | 0 | 2 (0.5) | .310 |
SAE, severe adverse event.
One patient with infection, admitted with fever, no source of infection identified, responded to antibiotics; 1 patient was found dead 18 days after the colonoscopy, unclear cause.
All patients with a severe adverse event in the clip group recovered with medical management. In the control group, 4 patients required surgery (3 for perforation, 1 for resection of an inflammatory mass at the site of the resected polyp), and 2 patients died. A previously healthy patient was found dead at home 18 days after the colonoscopy without any apparent cause of death (no autopsy performed). The other patient died after developing a myocardial infarction following postprocedure bleeding with high-volume blood loss. Albeit in the control group, the patient received complete clip closure of the defect because of concerns related to restarting anticoagulation medications.
Per-Protocol Analysis
In the clip group, 396 patients (87%) underwent the assigned treatment with complete (n = 305) or partial (n = 91) closure of the resection site (Supplementary Table 2). In the control group, 414 patients (90%) underwent the assigned treatment without closure of the resection defect. Following a per-protocol analysis, post-procedure bleeding occurred in 10 patients (2.5%) in the clip group and 29 patients (7.0%) in the control group (ARD 4.5, 95% CI 1.6–7.4). Similar to the intention-to-treat analysis, a reduced risk of postprocedure bleeding was seen only after resection of proximal, but not distal polyps.
Discussion
This multicenter randomized trial provides strong evidence to support endoscopic clip closure of the mucosal defect following resection of ≥20-mm nonpedunculated polyps. The study further provides clear evidence that this protective effect applies separately to patients with proximal lesions. Clip closure of the mucosal defect reduced the incidence of serious postprocedural bleeding events from 7.3% to 3.5% overall, and in the proximal colon from 9.9% to 3.3%. Clip closure did not lower the risk of postprocedure bleeding following resection of large polyps in the distal colon. The effect of clip closure appeared to be independent of polyp size, electrocautery setting, and use of periprocedural antithrombotic medications.
Endoscopic resection has replaced surgery as the primary approach for the resection of large colon polyps; however, the incidence of serious adverse events has remained a major concern. Postprocedure bleeding is the most frequent complication, with reported rates between 2% and 24%.5–13 A few prior studies have suggested a benefit of closing the mucosal defect following the polyp resection,12,13,18 whereas others have not.27,28 However, these studies were limited by retrospective design,12,27,28 lack of a control group,13 potential bias for patient selection,12,13,28 inclusion of smaller polyps,18 use of variable resection techniques,18 and unclear definition of outcomes.18
In contrast, our trial was methodologically rigorous, adequately powered, and all polyps were removed by EMR, which is considered the standard technique for large colon polyps in Western countries. The results of the study are therefore broadly applicable to current practice. Furthermore, conduct of the study at different centers with multiple endoscopists strengthens generalizability of the findings.
The risk of postprocedural hemorrhage in the control group of 7.3% was similar to the risk reported in previous studies.5–13 Proximal polyp location has been consistently reported to increase the risk of delayed bleeding at least 2-fold.12–14,29 Use of antiplatelet agents has been reported in some but not other studies.13,14 Limited data suggest that intraprocedural bleeding and type of cautery setting may represent additional risk factors.14 In our study, the greatest risk of postprocedure bleeding was seen among patients with a proximal polyp, those on periprocedural antithrombotic medications, or patients with larger polyp size. Although the benefit of clip closure was limited to large polyps in the proximal colon, the benefit of clip closure appeared to be independent of the use of antithrombotic medications or polyp size.
We found that clipping of the mucosal defect in the distal colon was not associated with a reduction in postprocedure bleeding. In contrast to our hypothesis, we observed a small increase in the risk of bleeding in the clip group. The low risk of bleeding and the low number of events among patients with distal lesions makes it impossible to draw a firm conclusion either way regarding any effect of clip closure in this population separately. Potential explanations include a poorer quality of clipping and a shorter clip retention time, possibly related to a thicker colon wall in the distal compared with the proximal colon. These considerations are worthy of further study.
The difference in median days to onset of bleeding is an interesting additional finding. Bleeding in the clip group occurred at a median 7 days after polyp resection, at a time when clips may have already fallen off,30 yet when the resection site ulcer is still vulnerable for delayed bleeding.
Even if a strategy of clip closure was applied, some mucosal resection defects cannot be closed. In our study, clip closure was not performed in 13% of patients and only partial closure achieved in 20% of patients. In most, this was related to the size of the defect, and one-third of resection sites of ≥40-mm polyps could not be closed. Notably, the proportion of resection sites that could not be clipped was not different between the proximal and distal colon. Although it is important to understand what factors are associated with complete closure or failure, such analysis was beyond the goals of the current study and should be subject to further investigation. Despite incomplete closure, the overall benefit of clip closure in an intention-to-treat analysis was apparent, particularly for proximal polyps (number needed to treat is 16). A formal cost-effectiveness analysis is needed to better understand the value of clip closure. Such analysis can then also examine possible thresholds, for instance regarding the minimum proportion of polyp resections, for which complete closure should be achieved, or the maximum number of clips to close a defect.
Some may argue that participating endoscopists were experts in EMR, and it is unclear whether the observed benefit is applicable to community practice. However, the annual volume of EMR among participating endoscopists varied broadly, and the findings cannot just be considered the results of a few highly experienced expert endoscopists. Although most 20- to 40-mm polyp sites could be closed, closure was not possible for one-third of ≥40-mm polyps. To further minimize bleeding risk, future efforts need to focus on achieving complete defect closure, even for larger polyps, and clipping should be a required skill for performing complex endoscopic resections.
Several limitations should be noted. The imbalance of antithrombotic medication use between groups is a concern. However, the benefit of clip closure was independent of antithrombotic use, and adjusting for antithrombotics did not affect the main result. The study was also not sufficiently powered to examine a possible association between different antithrombotic medications and/or an interaction with the time medications were stopped or restarted. The observed crossover rate of 10% from the control to the intervention group may have been related to the assumed benefit of clipping, and higher-risk polyps were probably more likely to be clipped. As a result, the observed difference in the bleeding rate may in fact underestimate the benefit of clipping. It is also conceivable that bleeding occurred at a different polyp resection site. However, each group had a very similar proportion of additional polyps and evidence of bleeding was found in 86% of patients who underwent a colonoscopy for bleeding at the prior large polyp resection site. Therefore bleeding at a nonstudy polyp site should have been infrequent and balanced between groups, if it occurred at all. Finally, all study polyps were removed using microprocessor-controlled electrocautery. There were no differences in postprocedure bleeding between the 2 applied settings. It has been shown that microprocessor-controlled electrocautery may decrease the risk of postprocedure bleeding14; therefore, the benefit of clip closure with other processors that are not microprocessor controlled may potentially be greater.12
In summary, this multicenter trial provides strong evidence that endoscopic clip closure of the mucosal defect after resection of large (≥20-mm) nonpedunculated colon polyps in the proximal colon significantly reduces the risk of postprocedure bleeding, irrespective of polyp size, electrocautery setting, or use of periprocedural antithrombotic medications.
Supplementary Material
WHAT YOU NEED TO KNOW.
BACKGROUND AND CONTEXT
Complete and safe removal of large colon polyps is important, because of their increased risk of cancer. Delayed bleeding is the major challenge, occurring in up to 10% of patients.
NEW FINDINGS
This randomized trial compared closing the resection defect with clips to not closing it among 918 patients undergoing resection of large (≥20mm) polyps. Clip closure reduce the risk of delayed bleeding compare to no clip closure from 7.1% to 3.5%. The reduced bleeding rate was only seen for polyp that were located in the right side of the colon.
LIMITATIONS
Complete closure of the defect, via clip, was only possible in approximately two thirds of polyp resections.
IMPACT
Closure via clip should be attempted in all patients undergoing resection of large non-pedunculated colon polyps in the proximal colon.
Acknowledgments
Funding
The study was supported by a research grant from Boston Scientific. Boston Scientific was not involved in the design of the study, its conduct, analysis, or interpretation of study results.
Abbreviations used in this paper:
- ARD
absolute risk difference
- CI
confidence interval
- EMR
endoscopic mucosal resection
- IQR
interquartile range
Footnotes
Supplementary Material
To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2019.03.019.
Conflicts of interest
These authors disclose the following: Heiko Pohl has received research funding from Boston Scientific and US Endoscopy. Ian Grimm, Matthew T. Moyer, and Abraham Mathew are consultants for Boston Scientific. Douglas Pleskow is a consultant for Olympus, Boston Scientific, and Medtronic. Mouen Khashab is a consultant and on the medical advisory board for Boston Scientific and Olympus, and a consultant for Medtronic. Seth Crockett is supported in part by a grant from the National Institutes of Health (KL2TR001109), and received research funding from Exact Sciences, Colowrap. Daniel von Renteln is supported by a Fonds de Recherche du Québec Santé career development award, has received research funding from Erbe, Ventage Pentax and is a consultant for Boston Scientific. Maria Pellise is a consultant for Norgine Iberia. Douglas Pleskow is a consultant for Olympus, Boston Scientific, and Medtronic. Douglas K. Rex is a consultant for Olympus Corp and Boston Scientific; and a research support recipient from Boston Scientific, Endochoice, EndoAid, Medtronic, and Colonary Solutions. The remaining authors disclose no conflicts. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the US government.
References
- 1.Hassan C, Repici A, Sharma P, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut 2016;65:806–820. [DOI] [PubMed] [Google Scholar]
- 2.Peery AF, Shaheen NJ, Cools KS, et al. Morbidity and mortality after surgery for nonmalignant colorectal polyps. Gastrointest Endosc 2018;87:243–250.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grimm I, Peery AF, Kaltenbach T, et al. Quality matters: improving the quality of care for patients with complex colorectal polyps. Am J Gastroenterol 2018; 113:317–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2017;49:270–297. [DOI] [PubMed] [Google Scholar]
- 5.Brooker JC, Saunders BP, Shah SG, et al. Treatment with argon plasma coagulation reduces recurrence after piecemeal resection of large sessile colonic polyps: a randomized trial and recommendations. Gastrointest Endosc 2002;55:371–375. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad NA, Kochman ML, Long WB, et al. Efficacy, safety, and clinical outcomes of endoscopic mucosal resection: a study of 101 cases. Gastrointest Endosc 2002;55:390–396. [DOI] [PubMed] [Google Scholar]
- 7.Arebi N, Swain D, Suzuki N, et al. Endoscopic mucosal resection of 161 cases of large sessile or flat colorectal polyps. Scand J Gastroenterol 2007; 42:859–866. [DOI] [PubMed] [Google Scholar]
- 8.Swan MP, Bourke MJ, Alexander S, et al. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc 2009;70:1128–1136. [DOI] [PubMed] [Google Scholar]
- 9.Ferrara F, Luigiano C, Ghersi S, et al. Efficacy, safety and outcomes of ‘inject and cut’ endoscopic mucosal resection for large sessile and flat colorectal polyps. Digestion 2010;82:213–220. [DOI] [PubMed] [Google Scholar]
- 10.Moss A, Bourke MJ, Williams SJ, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 2011;140:1909–1918. [DOI] [PubMed] [Google Scholar]
- 11.Buchner AM, Guarner-Argente C, Ginsberg GG. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest Endosc 2012; 76:255–263. [DOI] [PubMed] [Google Scholar]
- 12.Liaquat H, Rohn E, Rex DK. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: experience in 277 clipped large sessile or flat colorectal lesions and 247 control lesions. Gastrointest Endosc 2013;77:401–407. [DOI] [PubMed] [Google Scholar]
- 13.Albeniz E, Fraile M, Ibanez B, et al. A scoring system to determine risk of delayed bleeding after endoscopic mucosal resection of large colorectal lesions. Clin Gastroenterol Hepatol 2016;14:1140–1147. [DOI] [PubMed] [Google Scholar]
- 14.Burgess NG, Metz AJ, Williams SJ, et al. Risk factors for intraprocedural and clinically significant delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin Gastroenterol Hepatol 2014; 12:651–661; e1–3. [DOI] [PubMed] [Google Scholar]
- 15.Heldwein W, Dollhopf M, Rosch T, et al. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy 2005; 37:1116–1122. [DOI] [PubMed] [Google Scholar]
- 16.Buddingh KT, Herngreen T, Haringsma J, et al. Location in the right hemi-colon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am J Gastroenterol 2011; 106:1119–1124. [DOI] [PubMed] [Google Scholar]
- 17.Sawhney MS, Salfiti N, Nelson DB, et al. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy 2008;40:115–119. [DOI] [PubMed] [Google Scholar]
- 18.Zhang QS, Han B, Xu JH, et al. Clip closure of defect after endoscopic resection in patients with larger colorectal tumors decreased the adverse events. Gastrointest Endosc 2015;82:904–909. [DOI] [PubMed] [Google Scholar]
- 19.Aronchick CA, Lipshutz WH, Wright SH, et al. Validation of an instrument to assess colon cleansing [abstract]. Am J Gastroenterol 1999;94:2667. [Google Scholar]
- 20.Participants PW. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58:S3–S43. [DOI] [PubMed] [Google Scholar]
- 21.Holt BA, Bourke MJ. Wide field endoscopic resection for advanced colonic mucosal neoplasia: current status and future directions. Clin Gastroenterol Hepatol 2012; 10:969–979. [DOI] [PubMed] [Google Scholar]
- 22.ASGE Standard of Practice Committee, Anderson MA, Ben-Menachem T, et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc 2009;70:1060–1070. [DOI] [PubMed] [Google Scholar]
- 23.ASGE Standard of Practice Committee, Khashab MA, Chithadi KV, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 2015;81:81–89. [DOI] [PubMed] [Google Scholar]
- 24.Bahin FF, Rasouli KN, Byth K, et al. Prediction of clinically significant bleeding following wide-field endoscopic resection of large sessile and laterally spreading colorectal lesions: a clinical risk score. Am J Gastroenterol 2016;111:1115–1122. [DOI] [PubMed] [Google Scholar]
- 25.US Food and Drug Administration. What is a serious adverse event? 2016. Available at: https://www.fda.gov/Safety/MedWatch/HowToReport/ucm053087.htm. Accessed March 30, 2018.
- 26.Conio M, Repici A, Demarquay JF, et al. EMR of large sessile colorectal polyps. Gastrointest Endosc 2004; 60:234–241. [DOI] [PubMed] [Google Scholar]
- 27.Feagins LA, Nguyen AD, Iqbal R, et al. The prophylactic placement of hemoclips to prevent delayed postpolypectomy bleeding: an unnecessary practice? A case control study. Dig Dis Sci 2014;59:823–828. [DOI] [PubMed] [Google Scholar]
- 28.Qumseya BJ, Wolfsen C, Wang Y, et al. Factors associated with increased bleeding post endoscopic mucosal resection. J Dig Dis 2013;14:140–146. [DOI] [PubMed] [Google Scholar]
- 29.Sidhu M, Tate DJ, Desomer L, et al. The size, morphology, site, and access score predicts critical outcomes of endoscopic mucosal resection in the colon. Endoscopy 2018;50:684–692. [DOI] [PubMed] [Google Scholar]
- 30.Jensen DM, Machicado GA. Hemoclipping of chronic canine ulcers: a randomized, prospective study of initial deployment success, clip retention rates, and ulcer healing. Gastrointest Endosc 2009;70:969–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


