Abstract
In the wake of COVID‐19, the world has become a more uncertain environment—a breeding ground for stress and anxiety, especially for individuals with autism spectrum disorder (ASD). The study examined stress, anxiety, and coping in a data‐driven, real‐time assessment of 122 youth with and without ASD and their parents at the height of the COVID‐19 shutdown and three‐months later. Standardized measures were administered to ascertain stress and coping explicitly related to the pandemic (RSQ COVID‐19‐Child [self‐report], Adult [self‐report from the guardian of youth], Parent [report about child]) and anxiety (STAI‐C, STAI‐A). Multivariate, univariate analyses of variance and hierarchical regression were used. ASD youth endorsed more Trait anxiety and response to specific stressors (e.g., virus). Caregivers of youth with ASD (Adults) self‐reported higher anxiety, yet scores were elevated for both groups. Adults of youth with ASD reported more stress, especially related to the virus, access to healthcare, and concern for the future. In the TD group, youth and adults used more Primary and Secondary Control Coping whereas ASD youth and adults used more Disengagement Coping. Adult stress was the primary predictor of parent perception of child stress as well as Child self‐reported stress. While the ASD group was consistently high compared to the TD group, there were no significant changes over time for stress or anxiety. Results reveal striking differences in youth with ASD and their parents regarding stress, anxiety, and coping. Findings highlight the need for essential support, access to services, and strategies to enhance psychological and emotional well‐being.
Lay Summary
This study examined stress, anxiety, and coping related to the COVID‐19 pandemic in 61 youth with autism spectrum disorder (ASD) and 61 youth with typical development (TD) and their parents. Results showed that ASD youth reported more anxiety and stress. Adults of youth with ASD indicated higher self‐reported anxiety and stress than adults of TD youth. TD youth and their parents reported using more adaptive coping strategies. Findings highlight the need for strategies to enhance psychological and emotional well‐being.
Keywords: anxiety, autism, coping, COVID‐19, stress
INTRODUCTION
In the wake of the initial wave of the Coronavirus 2019 (COVID‐19) illness and efforts to limit its deadly impact, a less obvious but far reaching threat has plagued the psychological wellness of people around the world. The stress and anxiety from the multiple changes and disruption in nearly every aspect of daily life have been unprecedented. Amid the closing of schools, businesses, and stay‐at‐home mandates, the world has become a much more uncertain, unpredictable, and chaotic environment—a breeding ground for stress, anxiety, and isolation. The illness and subsequent measures to slow the spread of COVID‐19 involving quarantine, social distancing, and shelter‐at‐home strategies have changed the social, psychological, academic, occupational, and community milieu. The COVID‐19 pandemic has altered nearly every aspect of life, presenting countless threats to mental health ranging from social isolation and financial insecurity to upheaval of healthcare systems (Gordon & Borja, 2020), setting the stage for an enduring health and economic crisis. The cumulative effects of multiple stressors during the pandemic can have deleterious and far‐reaching effects on mental health (Fegert et al., 2020).
Stress is a multidimensional construct (Levine, 2005), involving psychological and physiological reactivity in response to events that are perceived to be or actually threatening to existence. Psychological variables shown to result in significant stress include loss of control and uncertainty (Dickerson & Kemeny, 2004; Mason, 1968), which are at the heart of the societal, social, and daily changes people face during the pandemic.
Anxiety can co‐occur with stress, although it is distinct in that it is defined as feelings of worry or apprehension in the absence of a direct threat (APA, 2013). Anxiety disorders are characterized by excessive worry, distress, and somatic symptoms of tension that interfere with daily functioning (APA, 2013) and are the most common mental illness in the United States and leading cause of disability globally, with approximately 31.2% of U.S. adults experiencing an anxiety disorder in their lifetime (Harvard, 2007). In the face of the many uncertainties associated with the COVID‐19 pandemic, the negative impacts on mental health, including an increase in anxiety, are a significant concern.
The way in which one responds to stress can have significant immediate and long‐term effects. Compas et al. (2001) present a robust, theoretical model in which stress response and coping are considered on three dimensions (voluntary vs. involuntary; engagement vs. disengagement; primary vs. secondary control). According to this model, coping involves voluntary responses that are controlled and under conscious awareness. In contrast, stress responses are involuntary, automatic responses to stress that involve physiological, emotional and behavioral responses. Stress responses and coping can be further characterized based on the extent of engagement (e.g., approach responses directed toward stressor) or disengagement (e.g., avoidant responses directed away from stressor) with the stressor. The model also theorizes that coping involves either primary control (e.g., directly changing a situation (problem solving) or the emotional response to it (emotional expression or emotion regulation) or secondary control (e.g., adapting to a situation) strategies (Connor‐Smith et al., 2000).
While the pandemic has forced all people to find ways to cope with the mounting challenges, persons with disabilities are particularly vulnerable (Courtenay & Perera, 2020; den Houting, 2020) with a disproportionate effect on the autism community (Pellicano & Stears, 2020). Schools in most states in the United States closed, resulting in a loss of some academic programming and services. Individuals with autism spectrum disorder (ASD), who respond poorly to change and uncertainty (APA, 2013), may be especially impacted by the loss of routine in daily life, resulting in stress (Courtenay & Perera, 2020). Children and adolescents with ASD experience significant stress in response to various social and non‐social situations (e.g., Corbett et al., 2012; Corbett et al., 2010; Muscatello & Corbett, 2018), and anxiety is common (Simonoff et al., 2008; van Steensel et al., 2011; White et al., 2009).
A recent survey from APA Stress in America specifically addressing the COVID‐19 pandemic reported significantly higher stress in parents compared to adults without children (APA, 2020). Parents of children with ASD also report poorer psychological well‐being, including increased anxiety (Abbeduto et al., 2004), especially following stressful life events (Barker et al., 2011). Thus, it is highly plausible that their stress may be magnified during the pandemic. Moreover, predictive models of parent stress indicate the extent to which a parent experiences stress can influence how they perceive the affective behavior of their child (Bishop et al., 2007; Schwartzman et al., 2021). Findings across studies suggest a positive association between parents' stress and negative perceptions of child functioning such that parents with higher stress also reported more difficulties in their child, and vice versa (De Los Reyes & Kazdin, 2006; Treutler & Epkins, 2003; Youngstrom et al., 2000). Increased parental stress has been associated with more discrepant parent–child reports of child anxiety symptoms in ASD (Ooi et al., 2016). Prior to the COVID‐19 pandemic, emerging research elucidated the influence of parenting stress on parent ratings of self, family, and child functioning in ASD (Ooi et al., 2016; Schwartzman et al., 2021; Shepherd et al., 2018). Given this, pre‐existing parenting stress may be further exacerbated by the well‐documented challenges of the COVID‐19 pandemic on family life (Brown et al., 2020; Daks et al., 2020; Park et al., 2020; Spinelli et al., 2020), which likely influences parent perceptions of their own stress and that of their child. This highlights the importance of understanding parent experiences, as well as potential shifts to their perceptions of self and others, in this vulnerable population during the pandemic.
April is Autism Awareness month, yet in the spring of 2020, COVID‐19 dominated the headlines and mental health leaders acknowledged the significant changes impacting the daily lives of individuals in the autism community (Gordon & Borja, 2020), warning that alteration of routines can lead to increased stress and difficulty coping. A brief online survey of parents (93% female) of children with ASD (80% male, mean 12‐years, 21% had ASD, and intellectual disability) reported that despite some positive impact of social distancing, families experienced significant upheaval (White et al., 2021). While such surveys are helpful, it is imperative that evidence be collected during the pandemic via rigorous approaches to learn directly from individuals with autism and their care providers to better prepare for future outbreaks (Courtenay & Perera, 2020).
Effects of the pandemic on mental health are far‐reaching, and early reports describe significant negative psychological impact of quarantine (Brooks et al., 2020; Fegert et al., 2020). Early in the pandemic, it was speculated that the pandemic effect on mental health would be especially significant for people with autism and their families (Pellicano & Stears, 2020) and that anxiety may be related to poorer psychological well‐being, particularly for mothers of children with autism (Ersoy et al., 2020). Further, environmental changes were expected to be significant sources of stress for individuals with ASD and their families and influence the ways they are able to cope with pandemic‐related stress (Ameis et al., 2020). Indeed, according to recent surveys, approximately 94% of families of individuals with ASD report increased difficulties during the pandemic, including challenges managing daily activities and an increase in behavior problems (Colizzi et al., 2020).
On January 31, 2020 the U.S. Department of Health and Human Services in response to the 2019 coronavirus cases declared a public health emergency responding to the impact of COVID‐19 (https://www.phe.gov/emergency/news/healthactions/phe/Pages/2019-nCoV.aspx). On March 11, 2020, the World Health Organization (WHO) declared the COVID‐19 outbreak a pandemic. On April 2, 2020, a safer‐at‐home executive order mandate went into effect in the state of Tennessee. At the time of writing this manuscript in November, 2020, the U.S. Department of Labor reported an October unemployment rate of 6.9% (14.7% in April and 8.4% in August). In November, 264,000 people had lost their lives in the United States (https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days).
The current study directly examined these concerns by assessing stress and anxiety in youth with and without ASD and their parents at the height of the COVID‐19 stay‐at‐home mandate and 3 months later. Four aims were conducted: Aim 1, Child: examined stress, coping, and anxiety during the height of the pandemic in self‐reports of youth with and without ASD. In addition, Parent‐report of child's stress was evaluated. Aim 2, Adult: examined stress, coping, and anxiety in adults (parents of youth with and without ASD) regarding their own self‐reported stress and anxiety. Aim 3, Predictive: examined the influence of adults' self‐reported stress and coping style on the perception of their child's stress and coping skills. Aim 4, Longitudinal: examined the impact of COVID‐19 longitudinally by comparing stress and coping over two time‐points: T1 (lockdown) and T2 (partial re‐opening). Additionally, for youth, self‐report of Trait anxiety was compared over three times points: T0 (Pre‐COVID‐19), T1, and T2.
For Aim 1, it was hypothesized that youth with typical development (TD) would demonstrate higher levels of stress specifically related to the impact of COVID‐19 on social and academic functioning whereas youth with ASD would experience greater stress related to changes in routines. Differences in coping strategies were also hypothesized such that youth with TD would report more active cognitive strategies (Primary and Secondary Control Coping) whereas youth with ASD would report more avoidant, emotional responses (Disengagement Coping) as well as avoidant responses to stress (Involuntary Engagement and Involuntary Disengagement) compared to TD youth. Regarding anxiety, it was hypothesized that youth with ASD would self‐report greater Trait anxiety than youth with TD. For Aim 2, it was predicted that Adults' self‐reported stressors would mirror those reported by their children. It was predicted that Adults of youth with ASD would experience greater stress and anxiety. For Aim 3, it was hypothesized that the Adults' self‐reported stress and coping style would predict the perception of their child's stress and coping skills. Finally, for Aim 4, it was hypothesized that self‐reported stress would increase over time from T1 to T2; yet self‐reported Trait anxiety being a stable factor, would be consistently high in the ASD youth from before COVID (T0), during lockdown (T1) and during partial re‐opening (T2).
METHODS
Participants
Respondents participate in a longitudinal study of stress in pubertal development recruited from a 200 mile radius from clinics, schools and community recruitment resources and compensated at the same amount received during annual visits (Corbett, 2017). The response rate to the online standardized questionnaires was excellent at 57%. There were no significant differences between the participants in the original study and the respondents in the current study based on the following demographic characteristics (e.g., age, race and ethnicity; all p > 0.05). The study included 122 well‐characterized youth, 61 with TD (26 females, M = 13.39 years) and 61 with ASD (15 females, M = 13.23 years) and one of their parents (96.3% mothers). The distribution for race was 84.42% White, 4.92% African American, and 10.66% mixed race, and the ethnic distribution was 9.12% Hispanic and 90.88% non‐Hispanic. The social economic income distribution was: 18.8% < $50,000, 33.9% = $50,000–$100,000 and 47.3% > $100,000.
The research was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The Vanderbilt Institutional Review Board (IRB) approved the study. Informed written assent/consent was obtained from all study participants and care providers, respectively, prior to inclusion in the study.
Diagnostic procedures
The diagnosis of ASD was based on the Diagnostic and Statistical Manual‐5 (APA, 2013) and corroborated by the Autism Diagnostic Observation Schedule, Second Edition (ADOS‐2; Module 3 [Lord et al., 2012]) by research‐reliable personnel. The Social Communication Questionnaire Lifetime (SCQ; Rutter et al., 2003) was used to screen for autism in the TD group. The Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI‐II; Wechsler, 2011) provided an estimate of the child's intellectual functioning (IQ ≥ 70 required). These diagnostic measures were completed between August 2017 and August 2018.
Procedures and dependent measures
All participants enrolled in the adolescent longitudinal study were sent emails inviting their participation in the COVID study with personally invited links for REDCap electronic data capture (Harris et al., 2009). At Time 1 (T1), respondents were asked to focus on their response to COVID‐19 during a one‐month period (April 27–May 29, 2020), which overlapped with the initial peak of the stay‐at‐home orders across the United States and Tennessee. In addition, the impact of COVID‐19 was examined longitudinally by comparing stress and coping at T1 to Time 2 (T2) 3 months later (August 2–September 10, 2020) which overlapped with partial, phase‐based reopening of the community, including the start of school. Finally, Trait anxiety was compared in the youth over three times points: Time 0 (T0) baseline Trait anxiety (Pre‐COVID‐19 during the past 12‐months as part of the longitudinal study) compared to Trait anxiety T1 and T2.
Responses to Stress Questionnaire (RSQ) COVID‐19
The RSQ (Connor‐Smith et al., 2000) is a multidimensional questionnaire adapted to specific stressors or domains of stress, in this case the COVID‐19 pandemic. To assess the frequency of exposure to stressors directly associated with the pandemic, the RSQ COVID‐19 was administered to youth with ASD and TD and their parents. Three versions were administered: Adult (self‐report from the guardian of youth), Parent (report about youth's stress), and Child (self‐report from youth). The first section of the RSQ provides a list of 14 anchoring questions about COVID‐19 pertaining to areas of potential stress (e.g., economic strain, changes in daily life, uncertainty, health concerns, see Supporting Information S1). Items are rated on a scale of 1 (Not at All) to 4 (Very) representing the degree to which an individual finds each item stressful. The sum of these values equals the Total Stress score.
The second section consists of 57 items that fall onto five factors (Connor‐Smith et al., 2000). Each item is prompted by How much do you do this? and rated on a 4‐point scale: 1 (Not at All), 2 (A Little), 3 (Some) and 4 (A lot). The five total factors include three types of coping: Primary Control Engagement Coping: (i.e., emotional expression, emotion regulation, and problem solving); Secondary Control Engagement Coping (i.e., acceptance, cognitive restructuring, distraction, and positive thinking); and Disengagement Coping (i.e., avoidance, denial, and wishful thinking). The RSQ includes two types of involuntary responses to stress: Involuntary Engagement (i.e., emotional arousal, impulse action, intrusive thoughts, physiological arousal, and rumination) and Involuntary Disengagement (i.e., cognitive interference, emotional numbing, escape, and inaction) (see Supporting Information S2 for examples). Each of the five factors—Primary Coping, Secondary Coping, Disengagement Coping, Involuntary Engagement, and Involuntary Disengagement—is calculated as a ratio score of the total stress response items endorsed. Therefore, Primary Coping, for example, represents the propensity of an individual to use this coping style relative to the four other factors.
The RSQ has good reliability and validity (i.e., internal consistency ranging from α = 0.73 to 0.85 (Connor‐Smith et al., 2000)). The RSQ Child and Adolescent Social Stress Version has been used for adolescents with ASD (Khor et al., 2014). The proportion scores were used for all analyses (Connor‐Smith et al., 2000; Jaser et al., 2010; Jaser et al., 2011). For this study, the internal consistency reliabilities (Cronbach's alphas) of the five factors for Child, Adult, and Parent were α = 0.85, 0.75, and 0.73 for Primary Coping, α = 0.79, 0.79, and 0.82 for Secondary Coping, α = 0.75, 0.69, and 0.69 for Disengagement Coping, α = 0.93, 0.90, and 0.94 for Involuntary Engagement, and α = 0.84, 0.85, and 0.80 for Involuntary Disengagement, respectively. For the current study, test–retest between T1 and T2 (3 month duration) for the Total stress score was good for Adult r = 0.80, acceptable for Parent 0.73, and fair for Child r = 0.60.
State–Trait Anxiety Inventory for Children (STAI‐C)
The STAI‐C (Spielberger, 1973) is a self‐report measure of current (State) and persistent (Trait) anxiety for children and adolescents. The instrument consists of two 20‐item scales first presenting questions asking how one currently feels followed by questions asking how one usually feels. The psychometric properties are well established (e.g., reliability ranges from α = 0.78–0.91, test–retest ranges from r = 0.65–0.71). The STAI‐C has been used with children and youth with TD and ASD (Corbett et al., 2014; Lanni et al., 2012; Muris et al., 1998; Simon & Corbett, 2013). For the current study, test–retest between T1 and T2 for the STAI‐C was r = 0.80.
State–Trait Anxiety Inventory for Adults (STAI‐A)
The STAI‐A (Spielberger et al., 1983) is a frequently‐used measure to distinguish between State and Trait anxiety in adults. The internal consistency coefficients range from 0.86 to 0.95 and test–retest reliability coefficients range from 0.65 to 0.75 (Spielberger et al., 1983). For the current study, test–retest between T1 and T2 for the STAI‐A was r = 0.85.
Statistical analyses
Analyses were conducted on demographic variables using one‐way analysis of variance (ANOVA) or chi‐square (α = 0.05). For Aims 1 and 2, to examine differences based on RSQ stressors and coping between the diagnostic groups (ASD and TD), multivariate analysis of variance (MANOVA) models were conducted for Child, Parent, and Adult. If models were significant, univariate tests were analyzed based on the estimated marginal means. State and Trait Anxiety were measured with ANOVA. The assumption of homogeneity of variance was tested with Levene's test of homogeneity, with a Welch degree of freedom approximation used when the assumption was violated. Effect sizes were reported as partial η2, which estimates the proportion of the total variance accounted for by the independent factor.
For Aim 3, hierarchical regression models were performed to predict Parent reported child stress and coping based on various predictors (e.g., age, IQ, diagnosis, Adult Total stress, Child Total stress). For Aim 4, repeated measures ANOVA/MANCOVA for T1 and T2 RSQ Total stress measured stress over 2‐timepoints and T0, T1, T2 anxiety examined the change in anxiety over 3‐timepoints.
RESULTS
Demographic variables are presented in Table 1. There were no differences in age between the youth with and without ASD. There were anticipated differences in IQ and SCQ.
TABLE 1.
Demographics
| ASD | TD | t | p | |
|---|---|---|---|---|
| M (SD) | M (SD) | |||
| Age | 13.24 (1.16) | 13.38 (1.20) | 0.66 | 0.51 |
| ADOS severity | 7.13 (2.03) | – | – | – |
| Full scale IQ | 107.62 (18.06) | 119.13 (12.49) | 4.10 | <0.001 |
| SCQ Total | 18.13 (8.68) | 2.51 (2.56) | 13.49 | <0.001 |
Abbreviations: ADOS, autism diagnostic observation schedule; ASD, autism spectrum disorder; IQ, intelligence quotient; SCQ = Social Communication Questionnaire; TD, typically developing.
Aim 1. Child stress, coping, and anxiety at T1 (initial peak of COVID‐19 stay‐at‐home orders)
RSQ Total stress
As shown in Table 2 and Figure 1(a), there was a trend for diagnostic differences in total reported stress on the RSQ (p = 0.06). However, when controlling for the extent to which the youth or family member experienced COVID‐19 symptoms, Total stress was not significant (F[1102] = 0.337, p = 0.56, partial η2 = 0.003).
TABLE 2.
Dependent variables at time 1 (initial peak of COVID‐19 stay‐at‐home orders)
| ASD | TD | F | p | η2 | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| RSQ‐Child | |||||
| Stress Total | 33.83 (8.63) | 30.79 (7.98) | 3.52 | 0.06 | 0.033 |
| Primary Control Coping | 0.16 (0.03) | 0.19 (0.04) | 7.81 | 0.01 | 0.070 |
| Secondary Control Coping | 0.28 (0.06) | 0.32 (0.04) | 13.64 | <0.001 | 0.117 |
| Disengagement Coping | 0.16 (0.03) | 0.14 (0.03) | 14.23 | <0.001 | 0.121 |
| Involuntary Engagement | 0.22 (0.04) | 0.19 (0.03) | 12.79 | 0.001 | 0.110 |
| Involuntary Disengagement | 0.17 (0.03) | 0.16 (0.03) | 4.14 | 0.05 | 0.039 |
| RSQ‐Adult | |||||
| Stress Total | 40.74 (8.45) | 33.33 (7.82) | 22.38 | < 0.001 | 0.175 |
| Primary Control Coping | 0.19 (0.03) | 0.21 (0.03) | 7.03 | 0.01 | 0.062 |
| Secondary Control Coping | 0.28 (0.05) | 0.31 (0.05) | 11.44 | 0.001 | 0.097 |
| Disengagement Coping | 0.14 (0.02) | 0.13 (0.02) | 14.04 | <0.001 | 0.117 |
| Involuntary Engagement | 0.22 (0.04) | 0.21 (0.04) | 4.16 | 0.04 | 0.038 |
| Involuntary Disengagement | 0.16 (0.03) | 0.15 (0.03) | 7.00 | 0.01 | 0.062 |
| RSQ‐Parent | |||||
| Stress Total | 37.81 (7.72) | 31.53 (7.35) | 19.78 | <0.001 | 0.15 |
| Primary Control Coping | 0.18 (0.03) | 0.19 (0.04) | 1.78 | 0.19 | 0.02 |
| Secondary Control Coping | 0.25 (0.06) | 0.31 (0.06) | 27.93 | <0.001 | 0.20 |
| Disengagement Coping | 0.16 (0.03) | 0.14 (0.02) | 11.05 | 0.001 | 0.09 |
| Involuntary Engagement | 0.23 (0.05) | 0.20 (0.05) | 15.62 | <0.001 | 0.12 |
| Involuntary Disengagement | 0.18 (0.03) | 0.16 (0.03) | 9.12 | 0.003 | 0.08 |
| STAI‐Child | |||||
| State anxiety | 31.16 (5.85) | 31.45 (7.45) | 0.05 | 0.83 | 0.000 |
| Trait anxiety | 34.80 (7.49) | 31.53 (7.90) | 4.74 | 0.03 | 0.043 |
| STAI‐Adult | |||||
| State anxiety | 44.00 (14.13) | 38.95 (11.76) | 4.03 | 0.05 | 0.037 |
| Trait anxiety | 43.45 (11.73) | 39.76 (9.64) | 3.15 | 0.08 | 0.029 |
Abbreviations: ASD, Autism Spectrum Disorder; RSQ, Responses to Stress Questionnaire; STAI, State–Trait Anxiety Inventory; TD, typically developing.
FIGURE 1.
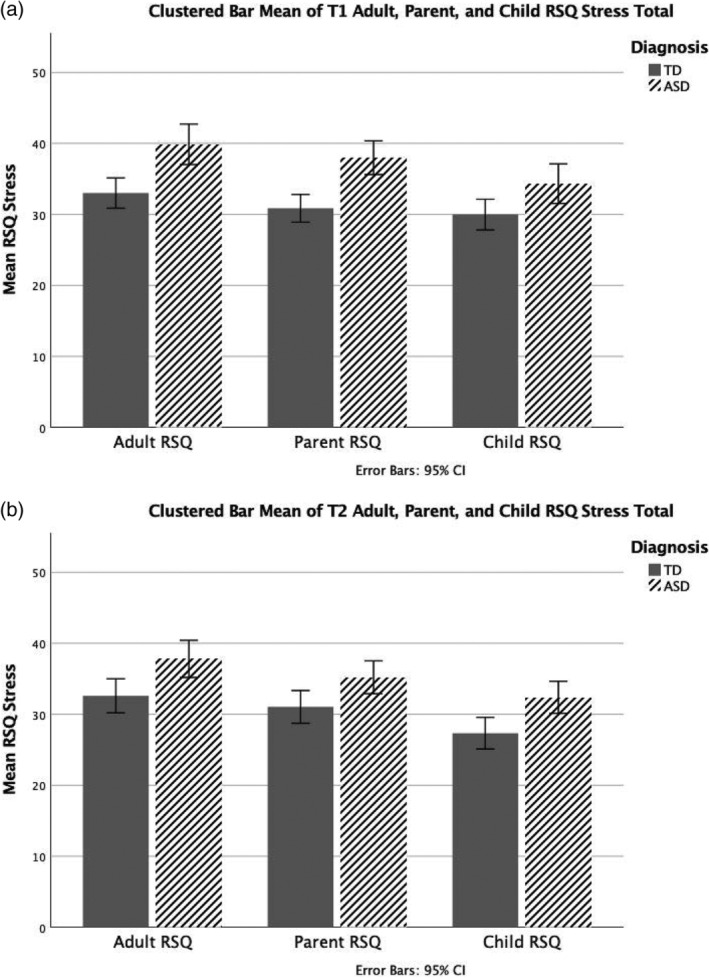
Clustered bar graph of Adult, Parent, and Child RSQ Total stress at T1 and T2. (a) Clustered bar mean of T1 Adult, Parent, and Child RSQ Total stress. T1 refers to the one‐month period (April 27–May 29, 2020) which overlapped with the initial peak of the COVID‐19 stay‐at‐home orders. (b) Clustered bar mean of T2 Adult, Parent, and Child RSQ Total stress. T2 refers to the period three months after the initial peak of the stay‐at‐home orders (i.e., August 2–September 10, 2020) which overlapped with partial, phase‐based reopening of the community. ASD, autism spectrum disorder; RSQ, responses to stress questionnaire; TD, typically developing
When examining the parent's perception of youth Total stress, there was a significant effect for diagnosis (F[1114] = 20.43, p < 0.001, partial η2 = 0.15), with elevated Parent reported stress in youth with ASD. Significant findings held when controlling for previous experiences with COVID‐19 symptoms or diagnosis (F[1113] = 15.41, p < 0.001, partial η2 = 0.12).
Types of stressors
Overall, there was a statistically significant difference for the type of stressors endorsed (F[14,91] = 2.82, p = 0.002; Λ = 0.698, partial η2 = 0.302). The youth were relatively similar with regards to 10 of 14 stressors; however, notable differences emerged for youth with ASD, who reported greater concern pertaining to COVID‐19 illness, symptoms, access to healthcare, and the news. Thus, hypotheses related to the type of stressors for the TD versus ASD youth were not confirmed.
Coping and response to stress
Regarding coping and response to stress on the RSQ, there were significant group differences (F[5,99] = 5.37, p < 0.001, Λ = 0.787, partial η2 = 0.213), confirming hypotheses (Figure 2(a)). Univariate tests revealed that TD youth endorsed more Primary and Secondary Control Coping strategies. In contrast, youth with ASD reported more Disengagement Coping. For response to stress, ASD youth reported more Involuntary Engagement (i.e., emotional arousal, impulse action, intrusive thoughts, physiological arousal, and rumination) and Involuntary Disengagement (i.e., cognitive interference, emotional numbing, escape, and inaction). Thus, these results supported the relevant hypotheses, as TD youth were more likely to endorse using Primary and Secondary Coping strategies, while ASD youth reported Disengagement and Involuntary stress response in favor of more adaptive coping strategies. Similar differences in coping strategies were observed by examining the parent perception of the child's coping (F[5108] = 6.29, p < 0.001, Λ = 0.774, partial η2 = 0.226).
FIGURE 2.
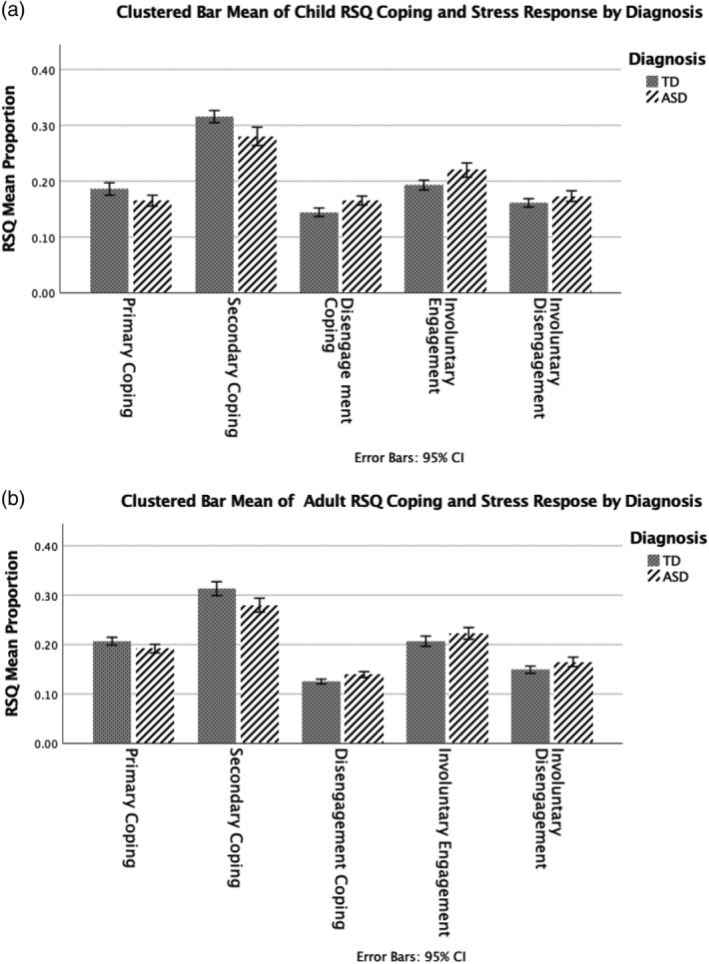
Clustered bar graph of RSQ coping factors for children and adults. (a) RSQ COVID‐19 coping factors based on diagnosis for children. (b) RSQ COVID‐19 coping factors based on diagnosis for adults. ASD, autism spectrum disorder; RSQ, Responses to Stress Questionnaire; TD, typically developing
Anxiety (STAI‐C)
As shown in Table 2, differences were observed for Trait Anxiety but not State Anxiety, as predicted.
Aim 2. Adult stress, coping, and anxiety at T1
RSQ Total stress
The results for the Adult self‐reports are presented in Table 2 and Figure 1(a). There were significant between‐group differences on the RSQ Total stress (F[1106] = 22.38, p < 0.001, partial η2 = 0.174), revealing Adults in the ASD group reported significantly more personal stress than Adults of youth with TD, supporting the hypothesis. Controlling for the extent to which the youth or family member experienced COVID‐19 symptoms, did not change the results.
Types of stressors
There were significant differences between the type of stressors the adults endorsed (F[14, 93] = 2.53, p = 0.004; Λ = 0.724, partial η2 = 0.276). It was predicted that adult stressors would largely mirror their youth's stress, which was partially supported. Specifically, Adults in the ASD group reported concerns pertaining to the distressing news, the illness, symptoms, and access to health care. However, they also showed higher endorsement of stress related to the future, working remotely, difficulty completing work/school, access to supplies, home conflicts, as well as change in routines and plans.
Coping and response to stress
Regarding response to COVID‐19 in Adult stressors, there were significant differences (F[5, 102] = 5.44, I < 0.001; Λ = 0.789, partial η2 = 0.211). As shown in Table 2 and Figure 2(b), Adults of TD youth reported a propensity to utilize significantly more Primary and Secondary Control Coping than Adults of ASD youth. In contrast, Adults of ASD youth used more Disengagement Coping, as well as significantly more Involuntary Engagement and Involuntary Disengagement responses to stress.
Anxiety (STAI‐A)
As shown in Table 2, there was a significant difference for State but not Trait Anxiety, partially supporting the hypothesis. The mean values for the Adults ranged from TD = 38 and ASD = 44.
Aim 3. Adult stress on perception of child stress and coping at T1 and T2 (3 months later, partial re‐opening)
Using hierarchical regression models (controlling for age, IQ and diagnosis) both Child self‐reported stress (β = 0.28, p < 0.001) and Adult stress (β = 0.55, p < 0.001) were significant predictors of Parent perceptions of child stress, with the total model accounting for 60% of the variance in Parent perception of child stress. In the second step of the model (step one including control variables only), Child self‐reported stress on the RSQ accounted for an additional 15% of the variance of Parent perception of child stress (ΔF [1,88] = 21.76, p < 0.001); however, it was Adult stress in the third step that was the strongest predictor accounting for an additional 24% of the model variance (ΔF [1,87] = 55.31, p < 0.001). Additionally, separate models predicting T1 Child stress demonstrated a significant effect for Adult stress (β = 0.25, p = 0.03), where higher stress in the adults is related to more stress in their child. For full T1 regression model results, see Table 3.
TABLE 3.
Regression models predicting scores on affective subscale of CBCL in ASD
| Dependent variable: Parent report of child stress | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| Variable | β | p | β | p | β | p |
| Age | 0.90 | 0.35 | 0.08 | 0.92 | 0.03 | 0.71 |
| IQ | −0.16 | 0.12 | −0.18 | 0.05 | −0.14 | 0.05 |
| Diagnosis | 0.40 | <0.001 | 0.30 | 0.002 | 0.14 | 0.07 |
| Child stress | – | – | 0.42 | <0.001 | 0.31 | <0.001 |
| Adult stress | – | – | – | – | 0.54 | <0.001 |
| Model 1 | Model 2 | Model 3 | ||||
| R 2 | 0.22 | 0.39 | 0.63 | |||
| ∆R 2 | 0.22 | 0.17 | 0.24 | |||
| ∆F (df) | 8.14(3,85) ** | 22.82(1,84) ** | 53.92(1,83) ** | |||
| Dependent variable: Child stress | ||||
|---|---|---|---|---|
| Model 1 | Model 2 | |||
| Variable | β | p | β | p |
| Age | 0.03 | 0.78 | 0.01 | 0.95 |
| IQ | −0.01 | 0.96 | 0.02 | 0.84 |
| Diagnosis | 0.26 | 0.02 | 0.17 | 0.13 |
| Adult stress | – | – | 0.25 | 0.03 |
| Model 1 | Model 2 | |||
| R 2 | 0.07 | 0.12 | ||
| ∆R 2 | 0.07 | 0.05 | ||
| ∆F (df) | 2.17(3,90) | 5.07(1,89) * | ||
* p < 0.05; ** p < 0.001.
For Primary Coping style, Child self‐reported use of primary coping was not a significant predictor (β = 0.09, p = 0.37); however, Adult self‐reported primary coping style was a significant predictor (β = 0.33, p < 0.001) and accounted for 10% of the model variance (ΔF[1,87] = 11.03, R 2 = 0.20, p < 0.001). Similarly, for Secondary Coping, Child coping was not a significant predictor; however, Adult self‐reported use of secondary coping was a significant predictor (β = 0.45, p < 0.001) and accounted for 18% of the model variance (ΔF[1,87] = 28.01, R 2 = 0.45, p < 0.001).
To further examine the directionality of these relationships and the extent to which Child and Adult stress predicts later Parent‐report of child stress, regression models were repeated with T2 Parent perception of child stress, predicted by T1 Child and Adult stress. At T2, Child stress at the beginning of the COVID‐19 pandemic was not a significant predictor of Parent perception of child's stress 3 months later (β = 0.18, p = 0.11). Elevated Adult stress, however, significantly predicted increased Parent report of child stress at T2 (β = 0.48, p < 0.001), accounting for 18% of the model variance (ΔF[1,69] = 19.67, R 2 = 0.37, p < 0.001). Interestingly, Child stress at T2 was significantly predicted by Child stress at T1 (β = 0.59, p < 0.001) but not T1 Adult stress (β = 0.12, p = 0.23).
As personal experiences with COVID‐19 may impact perceptions and stress responses, all analyses were re‐run while controlling for Item I on the RSQ‐ “Myself or someone close to me experience symptoms or being diagnosed with COVID‐19.” Significant results were unchanged when controlling for responses on this item. For all models, tests to see if the assumption of collinearity was met indicated that multicollinearity was not a concern.
Aim 4. Longitudinal examination of stress and anxiety during COVID‐19
Over two thirds of the initial T1 sample (N = 85) provided T2 COVID‐19 timepoint data (TD = 47, ASD = 38). Results suggest persistently higher Child RSQ Total stress in children with ASD (F[1,77] = 7.41, p = 0.008, partial η2 = 0.088), Adult stress (F[1,79] = 15.55, p = 0.004, partial η2 = 0.164), and Parent (F[1,86] = 14.31, p < 0.001, partial η2 = 0.143) relative to the TD groups (Figure 1(b)). However, for Adult stress, there was a significant effect of time (F[1,79] = 4.67, p = 0.03, partial η2 = 0.056) in which total stress decreased from the initial peak of the COVID‐19 pandemic to 3 months later. In all cases, there was no diagnosis × time interaction (all p > 0.05), suggesting change in stress over time did not differ based on diagnosis.
Anxiety at T0, T1, T2
For Trait anxiety comparing T0, T1, T2, the ASD youth revealed a main effect for diagnosis (F[1,68] = 8.543, p = 0.005, partial η2 = 0.112) showing consistently higher Trait anxiety compared to TD youth (see Figure 3); however, there was not a time x diagnosis interaction (p > 0.05). Furthermore, there was no significant effect of time (F[2136] = 1.02, p = 0.036, partial η2 = 0.015). Adult State anxiety was no longer significant at T2 but Adults of ASD youth reported higher Trait anxiety (F[1,78] = 5.91, p = 0.02, partial η2 = 0.070); however, there was no time or diagnosis x time effect (p > 0.05).
FIGURE 3.
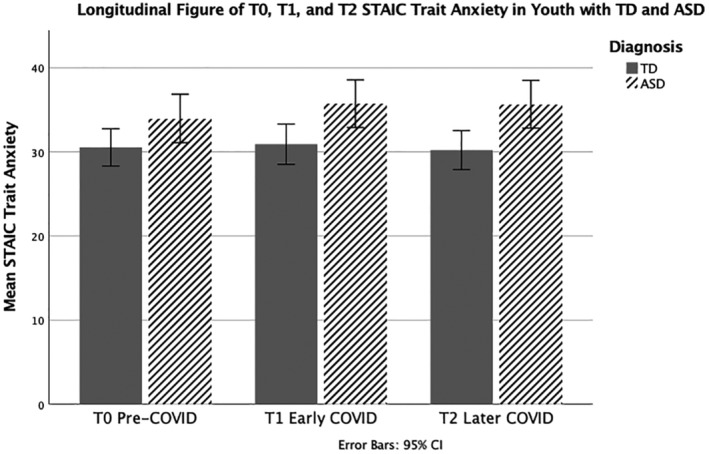
STAIC‐Trait across three timepoints. T0 refers to baseline Trait anxiety (pre‐COVID‐19 during the past 12‐months) compared to Trait anxiety at T1 (one‐month period (April 27–May 29, 2020) which overlapped with the initial peak of the COVID‐19 stay‐at‐home orders) and T2 (period 3 months after the initial peak of the stay‐at‐home orders (i.e., August 2–September 10, 2020) which overlapped with partial, phase‐based reopening of the community). ASD, autism spectrum disorder; STAIC, State‐Trait Anxiety Inventory for Children; TD, typically developing
DISCUSSION
The objective of the study was to examine stress and anxiety in youth with and without ASD and their parents at the height of the COVID‐19 stay‐at‐home social distancing mandate in the United States. It was hypothesized that TD youth would demonstrate higher stress specifically related to the impact of COVID‐19 on social and academic functioning whereas youth with ASD would experience greater stress related to changes in routines, yet neither hypothesis was supported. The groups were relatively similar with regards to 10 of the 14 stressors (see Supporting Information S1); however, notable exceptions included greater endorsement by youth with ASD regarding concern of COVID‐19 illness, symptoms, access to health care, and distressing news. Children with ASD can be rather concrete in their thoughts and behavior (APA, 2013), which may contribute to valid—although heightened—fears about what they learn about the virus. Although individuals with ASD are often characterized as displaying behavioral inflexibility (e.g., adapt poorly to changes in routine), this tendency does not necessarily imply cognitive inflexibility (Geurts et al., 2009). Therefore, the tenets of cognitive behavior therapy (CBT) aimed at restructuring their thought processes (e.g., the fears associated with the virus and educating youth with ASD on how to protect themselves with personal protective equipment [PPE]) may be helpful.
Differences in coping strategies were also hypothesized such that TD youth would report more Primary and Secondary Control Coping whereas youth with ASD would report more Disengagement Coping. Indeed, these hypotheses were supported, showing that TD youth used more active (primary) and cognitive (secondary) strategies to cope with the stress related to the pandemic. In the context of COVID‐19, directly changing the situation may not be feasible, but an individual can change his or her response to the situation through, for example, emotional expression or emotion regulation. Higher levels of Primary and Secondary Control Coping have been related to lower internalizing and externalizing symptoms (e.g., Compas et al., 2017; Jaser et al., 2005; Langrock et al., 2002). Conversely, youth with ASD used avoidant (Disengagement) coping in response to COVID‐19, suggesting they may benefit from interventions to increase their use of Primary and Secondary Control Coping skills. For example, explicit teaching of strategies aimed at learning to express how they feel (e.g., emotional expression of fears related to the virus) or engage in healthy distracting activities (e.g., playing, exercising) may be beneficial. Coping style has been associated with resilience in families of individuals with ASD who use a more problem‐focused approach (Bekhet et al., 2012; Iacob et al., 2020), especially during significant life events, to include adapting to a pandemic. However, it should be recognized that individuals on the spectrum and their families routinely show resilience by navigating the dynamic social world in spite of elevated stress and anxiety (den Houting, 2020). While research examining the intersection between ASD and resilience is limited (Lai & Szatmari, 2019), it is possible that some positive outcomes from the pandemic may evolve (Chung, 2020) to include innovative and effective ways to engage individuals with ASD via remote technology for education (e.g., virtual learning), health care (e.g., telehealth visits), and service delivery (e.g., online therapy).
Regarding response to stressors, ASD youth reported more Involuntary Engagement and Involuntary Disengagement compared to TD youth, which also supported hypotheses. Such responses are often linked to emotional and physiological arousal or escape behavior (Connor‐Smith et al., 2000) and anxious, depressed, and somatic complaints (Dufton et al., 2011). Involuntary Engagement can present as disruptive behavior: Colizzi et al. (2020) found that the presence of pre‐pandemic behavior problems in youth (M = 13 years old) with ASD (33% of sample able to use fluent speech) predicted an increased risk for exacerbation of an increase in these disruptive behaviors during the pandemic. Strategies to modify Involuntary Engagement could involve teaching relaxation or mindfulness practices to reduce emotional and physiological arousal and redirection of negative or fearful thought processes related to getting sick or hearing distressing news pertaining to the virus. Youth with ASD also endorsed more Involuntary Disengagement responses and therefore may benefit from the establishment of new routines and staying engaged in enjoyable activities with family.
It was hypothesized that ASD youth would endorse more Trait anxiety than TD peers, which was supported by the finding. However, neither group reported what may be interpreted as clinically significant anxiety on the STAI‐C. Based on the manual, children report a total score of 36–38 on the Trait subscale and 30–31 on the State (Spielberger, 1973), indicating that both groups fall broadly within the average range. Although stress and anxiety both include fear (i.e., an emotional response to a real or perceived imminent threat), anxiety is the anticipation of a future threat. Findings from the present study suggest that youth with and without ASD may experience stress/threats similarly at T1, but youth with ASD may experience heightened anticipation of future threats. This suggests that anticipation of threat is an important concept to explore further in youth with ASD, and may guide treatment planning (i.e., cognitive restructuring to challenge anticipated fears in CBT).
It was anticipated that Adult stress and anxiety would be high and differentiate the groups, which was supported. Adults of youth with ASD indicated greater perceived stress and State Anxiety than parents of TD youth. In a recent APA Stress in America COVID‐19 survey, parents reported significantly higher levels of stress than adults without children, especially pertaining to concerns over access to healthcare, food and housing, education, and missing important milestones (APA, 2020). Additionally, parents of children with ASD have higher rates of stress in general (Abbeduto et al., 2004), which may be magnified during stressful life events (Barker et al., 2011) such as a pandemic. Emerging research on interventions for parents of youth with ASD suggests that mindfulness (Benn et al., 2012; Dykens et al., 2014), resilience (Kuhlthau et al., 2020; Schwartzman et al., 2021), and Acceptance and Commitment Therapy (ACT; Kowalkowski, 2012) are effective strategies for reducing parental stress. Interestingly, differences in Adult stress emerged across groups but not across youth. The finding may be accounted for by several reasons. First, interrater disagreement has been well‐documented in youth with (Kalvin et al., 2020) and without (Dirks et al., 2014) ASD and may explain, in part, why differences did not emerge in Child stress. Parent–child agreement has been associated with better youth outcomes (e.g., anxiety; Burrows et al., 2018) and highlights the importance of understanding multiple perspectives. Second, some youth may not be cognizant of all consequences of the COVID‐19 pandemic, despite school closures and social distancing guidelines, and therefore, may not report as much stress as their parents. Finally, it is also possible that self‐report measures may not fully capture a youth's difficulties as the use of self‐report measures has been questioned by some investigators (Hambrick et al., 2014; Kormos & Gifford, 2014; Mazefsky et al., 2011).
Importantly, Adult stress was the strongest predictor of parent perceptions of child stress, even beyond diagnosis. Findings suggest that the mental health of parents impacts the perception of, and response to, the stress and anxiety of their child. This appears consistent with previous findings of more negative perceptions of child functioning among parents with higher stress and anxiety (Ooi et al., 2016; Schwartzman et al., 2021; Shine & Perry, 2010). Given this, mental health support strategies must consider parental well‐being in addressing the needs of the child. For example, parents could utilize mindful breathing exercises (Kuhlthau et al., 2020), engage in exercises of values and committed actions (Kowalkowski, 2012), or cognitive restructuring techniques (e.g., Double Standard Method, Examining Alternatives) to reduce stress or challenge unhelpful thoughts. Recent investigations of resilience interventions for parents of youth with ASD demonstrate promise, with particular benefits in decreasing parental stress and anxiety (Kuhlthau et al., 2020; Schwartzman et al., 2021). Preliminary evidence in one trial suggested the potential for altered parent perceptions of child functioning following participation in a resilience intervention (Schwartzman et al., 2021). In working with parents of youth with ASD, care providers may consider strategies to acknowledge, validate, and remediate parent stress. For example, care providers may check in with parents about stressors or teach parents a variety of coping skills, such as mindful breathing or leaves on a stream.
The type of stressors differentiated the groups with Adults of youth with ASD reporting concerns pertaining to distressing news, the illness, symptoms, and access to healthcare, which were similar to those reported by their children. Additionally, they reported greater stress related to the future, working remotely, completing work/school, access to supplies, home conflicts, and change in routines, consistent with a recent commentary on the impact of the pandemic on people with autism and their families (Ameis et al., 2020).
While Adults of youth with ASD reported greater State Anxiety, both parent groups reported similar Trait Anxiety. Normative data for the STAI‐A (Spielberger et al., 1983) suggests average middle‐aged adults endorse scores of 34–36 on either subscale indicating Adults in both groups endorsed high levels of anxiety pertaining to COVID‐19. The pandemic has contributed to significant anxiety in parents around the world as they attempt to simultaneously nurture themselves and their children (Coyne et al., 2020) and find ways to cope.
Parents in the current study employed distinct types of coping strategies in response to COVID‐19. Specifically, Adults of TD youth made greater use of Primary and Secondary Control Coping. In contrast, Adults of youth with ASD endorsed greater use of Disengagement Coping (i.e., avoidance, denial, and wishful thinking) and, similar to their children, used fewer Secondary Control Coping strategies. The stressors most identified in youth with ASD pertain to uncertainty and a loss of control with regards to health status, resulting in involuntary emotional responses and limited cognitive strategies. Indeed, the primary differences between the groups fall on the dimensions of voluntary or involuntary and engagement or disengagement that both explain and guide adaptive responding. The manner in which an individual adapts to stress is closely tied to mental health and psychopathology. Fundamentally, engagement with a stressor and cognitive approaches have been aligned with better psychological adjustment; conversely, disengagement from a stressor and emotion‐focused coping has been associated with poorer psychological adaptation (e.g., Compas et al., 2001; Compas et al., 2017).
Primary coping strategies are those in which an individual takes an active role in engaging with the stressor, fostering a sense of personal control over the situation (Compas et al., 2001). Secondary control, also an adaptive strategy, relies on cognitive methods to adapt via strategies such as acceptance, reframing, or distraction using positive thoughts. Both of these strategies involve engaging with the stressor in a conscious way. Disengagement coping, on the other hand, is less adaptive such that an individual attempts to avoid or disengage from the stressor or emotional response to the stressful situation (Connor‐Smith et al., 2000). In times of crisis, it is essential to implement strategies to reduce long‐term impacts of trauma on mental health, such as communicating with others, creating realistic expectations, and exercising (Gordon & Borja, 2020).
Results from the longitudinal aspect of the study indicate that child stress and anxiety, especially for the ASD group, persisted. The negative psychological impact of quarantine has shown a host of negative effects involving confusion, anger, and symptoms of post‐traumatic stress disorder (Brooks et al., 2020). Therefore, it is imperative to keep mental health wellness and illness at the forefront of the headlines and in the minds of policy makers to demand the essential attention it deserves. During the acute and long‐term phases of the pandemic, mental health providers are essential workers that must ensure continuity of care and access to needed services. It is important that telepsychiatry or other methods are available to prevent long‐term consequences (Fegert et al., 2020).
Factors shown to reduce the impact of isolation and quarantine include reducing the duration of quarantine, maintaining clear communication, and providing access to necessary supplies (Brooks et al., 2020). Parents, as they attempt to juggle enduring and new roles, may benefit from simple but impactful strategies such as practicing psychological flexibility and self‐care, which are foundational to psychological health (Coyne et al., 2020). During times of uncertainty, providing structure in daily activities even during remote learning and maintaining contact with schools, peers, and access to online services is important (Narzisi, 2020). Concrete explanations and reassurance to normalize the legitimate anxiety and fears that youth and their families may experience can be helpful. Resources are also available online on ways to minimize stress and anxiety for children and adolescents (e.g., Psychiatry, 2020). Importantly, times of crisis offer opportunities for posttraumatic growth and resilience such that overcoming adversity may bolster personal competence thereby acting as a protective factor for future stressors (Zoellner & Maercker, 2006).
Strengths of the study include a well‐characterized sample with confirmed diagnosis and longitudinal measurement from multiple perspectives. Limitations include an ASD sample not fully representative (IQ ≥ 70), predominantly White, and generally from middle‐to‐upper‐middle income families from one region of the United States. Further, a priori power analyses were not conducted prior to the study; however, post hoc observations suggest the sample size was sufficient for the multivariate analyses, with observed power consistently at 95% or higher for significant findings. In addition, due to the preliminary nature of the study, we did not control for multiple comparisons, increasing the likelihood of Type 1 error. It may also be argued that other statistical approaches, (e.g., Structural Equation Modeling) may have been useful. In addition, some of the reported effect sizes are small as well as the amount of variance accounted for by the predictors; therefore, the findings must be interpreted with caution and replicated. While additional information regarding the individual circumstances experienced by the families may have been enlightening, the COVID‐19 shutdown significantly impacted the way in which research could be conducted including interviews to obtain personal or medical information not captured by the primary dependent measure, the RSQ‐COVID‐19. While there are many limitations in such a study, the experiences reflected in the findings underscore the notable impact of the pandemic on children and parents with and without ASD.
Future directions for research on COVID‐19 highlight the need for ongoing monitoring via longitudinal studies of the impact on youth with and without ASD and their adult care providers as they adapt, struggle and overcome the multitude of threats to social, psychological, financial, educational, medical and mental health. The pandemic will undoubtedly have far‐reaching effects on mental health (Fegert et al., 2020); however, it will also be important to study interventions, adaptations and methods of coping that lead to better outcomes.
In conclusion, the current project examined stress, anxiety, and coping during the COVID‐19 pandemic to uncover the psychological health of youth and their parents revealing a largely deleterious and persistent impact. A population that responds poorly to change and is forced to adapt to an unpredictable world is bound to have difficulty coping, and it is essential to provide support, access to services, and helpful strategies to enhance psychological well‐being in youth with ASD and their families.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Blythe A. Corbett conceived of the study, supervised the implementation of study protocols and data collection, contributed to diagnostic assessments, analyzed and interpreted statistical analyses and drafted and finalized the manuscript. Rachael A. Muscatello facilitated the implementation of the online questionnaires, recruited participants from longitudinal study, participated in statistical analyses and interpretation, and contributed to the final manuscript. Mark E. Klemencic conducted literature review of key study measures, data collection and management, editing, and contributed to the final manuscript. Jessica M. Schwartzman conducted literature review regarding parent stress, participated in assessments and interpretation of relevant findings, and contributed to the final manuscript.
ETHICS STATEMENT
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.Informed ConsentInformed written consent and assent was obtained from all parents and study participants, respectively, prior to inclusion in the study.
Supporting information
TABLE S1 COVID‐19 concerns and stressors
TABLE S2. Sample Items from COVID‐19 Responses to Stress Questionnaire (based Connor‐Smith et al., 2000).
TABLE S3. Correlations among primary Adult outcome measures at T1
TABLE S4. Correlations among primary Child outcome measures at T1
ACKNOWLEDGMENTS AND FUNDING
This work was supported in part by the National Institute of Mental Health (NIMH) R01 MH111599 (Corbett), NICHD Grant U54HD083211 to Vanderbilt Kennedy Center, and NCATS/NIH Grant UL1 TR000445 to REDCap. The Authors express their sincere gratitude to Bruce Compas, Ph.D. and the Stress and Coping lab, Abby Ciriegio, M.Ed. and Tori Grice, for generously sharing their new COVID‐19 RSQ measures for our project.
Corbett BA, Muscatello RA, Klemencic ME, Schwartzman JM. The impact of COVID‐19 on stress, anxiety, and coping in youth with and without autism and their parents. Autism Research. 2021;14:1496–1511. 10.1002/aur.2521
Funding information Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant/Award Number: U54HD083211; National Center for Advancing Translational Sciences, Grant/Award Number: UL1 TR000445; National Institute of Mental Health, Grant/Award Number: R01 MH111599
REFERENCES
- Abbeduto, L. , Seltzer, M. M. , Shattuck, P. , Krauss, M. W. , Orsmond, G. , & Murphy, M. M. (2004). Psychological well‐being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. American Journal of Mental Retardation, 109(3), 237–254. [DOI] [PubMed] [Google Scholar]
- Ameis, S. H. , Lai, M. C. , Mulsant, B. H. , & Szatmari, P. (2020). Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID‐19 pandemic and beyond. Molecular Autism, 11(1), 61. 10.1186/s13229-020-00365-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA . (2013). Diagnostic and statistical manual of mental disorders, fifth edition (DSM‐5). American Psychiatric Association. [Google Scholar]
- APA . (2020). Stress in America. Stress in Amercia in Time of COVID‐19. Retrieved from https://www.apa.org/news/press/releases/stress/2020/report
- Barker, E. T. , Hartley, S. L. , Seltzer, M. M. , Floyd, F. J. , Greenberg, J. S. , & Orsmond, G. I. (2011). Trajectories of emotional well‐being in mothers of adolescents and adults with autism. Developmental Psychology, 47(2), 551–561. 10.1037/a0021268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekhet, A. K. , Johnson, M. L. , & Zauszniewski, J. A. (2012). Reslience in family members of person with autism spectrum disorder: A review of the literature. Issues in Mental Health Nursing, 33(10), 650–656. [DOI] [PubMed] [Google Scholar]
- Benn, R. , Akiva, T. , Arel, S. , & Roeser, R. W. (2012). Mindfulness training effects for parents and educators of children with special needs. Developmental Psychology, 48(5), 1476–1487. 10.1037/a0027537 [DOI] [PubMed] [Google Scholar]
- Bishop, S. L. , Richler, J. , Cain, A. C. , & Lord, C. (2007). Predictors of perceived negative impact in mothers of children with autism spectrum disorder. American Journal of Mental Retardation, 112(6), 450–461. 10.1352/0895-8017(2007)112[450:POPNII]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. M. , Doom, J. R. , Lechuga‐Pena, S. , Watamura, S. E. , & Koppels, T. (2020). Stress and parenting during the global COVID‐19 pandemic. Child Abuse & Neglect, 110(Pt 2), 104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrows, C. A. , Usher, L. V. , Becker‐Haimes, E. M. , McMahon, C. M. , Mundy, P. C. , Jensen‐Doss, A. , & Henderson, H. A. (2018). Profiles and correlates of parent‐child agreement on social anxiety symptoms in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(6), 2023–2037. 10.1007/s10803-018-3461-9 [DOI] [PubMed] [Google Scholar]
- Chung, W. (2020). Impact of COVID‐19 on families and children with autism. https://sparkforautism.org/discover_article/covid-19-impact-asd/. [Google Scholar]
- Colizzi, M. , Sironi, E. , Antonini, F. , Ciceri, M. L. , Bovo, C. , & Zoccante, L. (2020). Psychosocial and behavioral impact of COVID‐19 in autism Spectrum disorder: An online parent survey. Brain Sciences, 10(6), 341. 10.3390/brainsci10060341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas, B. E. , Connor‐Smith, J. K. , Saltzman, H. , Thomsen, A. H. , & Wadsworth, M. E. (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127(1), 87–127. [PubMed] [Google Scholar]
- Compas, B. E. , Jaser, S. S. , Bettis, A. H. , Watson, K. H. , Gruhn, M. A. , Dunbar, J. P. , Williams, E. , & Thigpen, J. C. (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta‐analysis and narrative review. Psychological Bulletin, 143(9), 939–991. 10.1037/bul0000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor‐Smith, J. K. , Compas, B. E. , Wadsworth, M. E. , Thomsen, A. H. , & Saltzman, H. (2000). Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology, 68(6), 976–992. [PubMed] [Google Scholar]
- Corbett, B. A. (2017). Examining stress and arousal across pubertal development in ASD. National Institute of Mental Health. [Google Scholar]
- Corbett, B. A. , Schupp, C. W. , & Lanni, K. E. (2012). Comparing biobehavioral profiles across two social stress paradigms in children with and without autism spectrum disorders. Molecular Autism, 3(1), 13. 10.1186/2040-2392-3-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett, B. A. , Schupp, C. W. , Simon, D. , Ryan, N. , & Mendoza, S. (2010). Elevated cortisol during play is associated with age and social engagement in children with autism. Molecular Autism, 1(1), 13. 10.1186/2040-2392-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett, B. A. , Swain, D. M. , Coke, C. , Simon, D. , Newsom, C. , Houchins‐Juarez, N. , Jenson, A. , Wang, L. , & Song, Y. (2014). Improvement in social deficits in autism Spectrum disorders using a theatre‐based, peer‐mediated intervention. Autism Research, 7, 4–16. 10.1002/aur.1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay, K. , & Perera, B. (2020). COVID‐19 and people with intellectual disability: Impacts of a pandemic. Irish Journal of Psychological Medicine, 37, 1–21. 10.1017/ipm.2020.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne, L. W. , Gould, E. R. , Grimaldi, M. , Wilson, K. G. , Baffuto, G. , & Biglan, A. (2020). First things first: Parent psychological flexibility and self‐compassion during COVID‐19. Behavior Analysis in Practice, 1–7. 10.1007/s40617-020-00435-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daks, J. S. , Peltz, J. S. , & Rogge, R. D. (2020). Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID‐19 stress on family systems with a contextual behavioral science lens. Journal of Contextual Behavioral Science, 18, 16–27. 10.1016/j.jcbs.2020.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes, A. , & Kazdin, A. E. (2006). Informant discrepancies in assessing child dysfunction relate to dysfunction within mother‐child interactions. Journal of Child and Family Studies, 15(5), 643–661. 10.1007/s10826-006-9031-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Houting, J. (2020). Stepping out of isolation: Autistic people and COVID‐19. Autism in Adulthood, 2(2), 103–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson, S. S. , & Kemeny, M. E. (2004). Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin, 130(3), 355–391. 10.1037/0033-2909.130.3.355 [DOI] [PubMed] [Google Scholar]
- Dirks, M. A. , Weersing, V. R. , Warnick, E. , Gonzalez, A. , Alton, M. , Dauser, C. , Scahill, L. , & Woolston, J. (2014). Parent and youth report of youth anxiety: Evidence for measurement invariance. Journal of Child Psychology and Psychiatry, 55(3), 284–291. 10.1111/jcpp.12159 [DOI] [PubMed] [Google Scholar]
- Dufton, L. M. , Dunn, M. J. , Slosky, L. S. , & Compas, B. E. (2011). Self‐reported and laboratory‐based responses to stress in children with recurrent pain and anxiety. Journal of Pediatric Psychology, 36(1), 95–105. 10.1093/jpepsy/jsq070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykens, E. M. , Fisher, M. H. , Taylor, J. L. , Lambert, W. , & Miodrag, N. (2014). Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics, 134(2), e454–e463. 10.1542/peds.2013-3164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersoy, K. , Altin, B. , Sarikaya, B. B. , & Ozkardas, O. G. (2020). The comparison of impact of health anxiety on dispositional Hope and psychological well‐being of mothers who have children diagnosed with autism and mothers who have Normal children, in Covid‐19 pandemic. Sosyal Bilimler Araştırma Dergisi, 9(2), 117–126. [Google Scholar]
- Fegert, J. M. , Viteiello, B. , Piener, P. L. , & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID‐19) pandemic for child and adolescent mental health: A narrative review to clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14(20). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geurts, H. M. , Corbett, B. , & Solomon, M. (2009). The paradox of cognitive flexibility in autism. Trends in Cognitive Sciences, 13(2), 74–82. 10.1016/j.tics.2008.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon, J. A. , & Borja, S. E. (2020). The COVID‐19 pandemic: Setting the Mental Health Research agenda. Biological Psychiatry, 88, 130–131. 10.1016/j.biopsych.2020.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hambrick, E. P. , Tunno, A. M. , Gabrielli, J. , Jackson, Y. , & Belz, C. (2014). Using multiple informants to assess child maltreatment: Concordance between case file and youth self‐report. Journal of Aggression Maltreatment & Trauma, 23(7), 751–771. 10.1080/10926771.2014.933463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvard . (2007). Data Table 1: Lifetime prevalence DSM‐IV/WMH‐CIDI disorders by sex and cohort . Retrieved from https://www.hcp.med.harvard.edu/ncs/index.php
- Jacob, C. I. , Avram, E. , Cojocaru, D. , & Podina, I. R. (2020). Resilience in familial caregivers of children with developmental disabilities: A meta‐analysis. Journal of Autism and Developmental Disorders, 50(11), 4053–4068. [DOI] [PubMed] [Google Scholar]
- Jaser, S. S. , Champion, J. E. , Dharamsi, K. R. , Riesing, M. M. , & Compas, B. E. (2011). Coping and positive affect in adolescents of mothers with and without a history of depression. Journal of Child and Family Studies, 20(3), 353–360. 10.1007/s10826-010-9399-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser, S. S. , Faulkner, M. S. , Whittemore, R. , Jeon, S. , Grey, M. , Delamater, A. , & Murphy, K. M. (2010). Coping, self‐management, and adaptation in adolescents with type 1 diabetes. Diabetes, 59, A516–A516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser, S. S. , Langrock, A. M. , Keller, G. , Merchant, M. J. , Benson, M. A. , Reeslund, K. , Champion, J. E. , & Compas, B. E. (2005). Coping with the stress of parental depression II: Adolescent and parent reports of coping and adjustment. Journal of Clinical Child and Adolescent Psychology, 34(1), 193–205. 10.1207/s15374424jccp3401_18 [DOI] [PubMed] [Google Scholar]
- Kalvin, C. B. , Marsh, C. L. , Ibrahim, K. , Gladstone, T. R. , Woodward, D. , Grantz, H. , Ventola, P. , & Sukhodolsky, D. G. (2020). Discrepancies between parent and child ratings of anxiety in children with autism spectrum disorder. Autism Research, 13(1), 93–103. 10.1002/aur.2220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khor, A. S. , Melvin, G. A. , Reid, S. C. , & Gray, K. M. (2014). Coping, daily hassles and behavior and emotional problems in adolescents with high‐functioning autism/Asperger's disorder. Journal of Autism and Developmental Disorders, 44(3), 593–608. 10.1007/s10803-013-1912-x [DOI] [PubMed] [Google Scholar]
- Kormos, C. , & Gifford, R. (2014). The validity of self‐report measures of proenvironmental behavior: A meta‐analytic review. Journal of Environmental Psychology, 40, 359–371. 10.1016/j.jenvp.2014.09.003 [DOI] [Google Scholar]
- Kowalkowski, J. D. (2012). Group‐based acceptance and commitment therapy intervention on parents of children diagnosed with an autism Spectrum disorder. (ProQuest Dissertations and Theses).
- Kuhlthau, K. A. , Luberto, C. M. , Traeger, L. , Millstein, R. A. , Perez, G. K. , Lindly, O. J. , Chad‐Friedman, E. , Proszynski, J. , & Park, E. R. (2020). A virtual resiliency intervention for parents of children with autism: A randomized pilot trial. Journal of Autism and Developmental Disorders, 50(7), 2513–2526. 10.1007/s10803-019-03976-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, M. C. , & Szatmari, P. (2019). Resilience in autism: Research and practice prospects. Autism, 23(3), 539–541. 10.1177/1362361319842964 [DOI] [PubMed] [Google Scholar]
- Langrock, A. M. , Compas, B. E. , Keller, G. , Merchant, M. J. , & Copeland, M. E. (2002). Coping with the stress of parental depression: parents' reports of children's coping, emotional, and behavioral problems. Journal of Clinical Child and Adolescent Psychology, 31(3), 312–324. 10.1207/S15374424JCCP3103_03 [DOI] [PubMed] [Google Scholar]
- Lanni, K. E. , Schupp, C. W. , Simon, D. , & Corbett, B. A. (2012). Verbal ability, social stress, and anxiety in children with autistic disorder. Autism, 16(2), 123–138. 10.1177/1362361311425916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine, S. (2005). Developmental determinants of sensitivity and resistance to stress. Psychoneuroendocrinology, 30(10), 939–946. [DOI] [PubMed] [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. C. , Risi, S. , Gotham, K. , & Bishop, S. L. (2012). Autism diagnostic observation schedule (ADOS‐2) (2nd ed.). Western Psychological Services. [Google Scholar]
- Mason, J. W. (1968). A review of psychoendocrine research on the sympathetic‐adrenal medullary system. Psychosomatic Medicine, 30(5), Suppl:631–653. [DOI] [PubMed] [Google Scholar]
- Mazefsky, C. A. , Kao, J. , & Oswald, D. P. (2011). Preliminary evidence suggesting caution in the use of psychiatric self‐report measures with adolescents with high‐functioning autism spectrum disorders. Research in Autism Spectrum Disorder, 5(1), 164–174. 10.1016/j.rasd.2010.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris, P. , Steerneman, P. , Merckelbach, H. , Holdrinet, I. , & Meesters, C. (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12(4), 387–393. [DOI] [PubMed] [Google Scholar]
- Muscatello, R. A. , & Corbett, B. A. (2018). Comparing the effects of age, pubertal development, and symptom profile on cortisol rhythm in children and adolescents with autism spectrum disorder. Autism Research, 11(1), 110–120. 10.1002/aur.1879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi, A. (2020). Handle the autism Spectrum condition during coronavirus (COVID‐19) stay at home period: Ten tips for helping parents and caregivers of young children. Brain Sciences, 10(4), 207. 10.3390/brainsci10040207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ooi, Y. P. , Weng, S. J. , Magiati, I. , Ang, R. P. , Goh, T. J. , Fung, D. S. , & Sung, M. (2016). Factors influencing agreement between parent and child reports of anxiety symptoms among children with high‐functioning autism spectrum disorders. Journal of Developmental and Physical Disabilities, 28(3), 407–424. 10.1007/s10882-016-9481-5 [DOI] [Google Scholar]
- Park, C. L. , Russell, B. S. , Fendrich, M. , Finkelstein‐Fox, L. , Hutchison, M. , & Becker, J. (2020). Americans' COVID‐19 stress, coping, and adherence to CDC guidelines. Journal of General Internal Medicine, 35(8), 2296–2303. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicano, E. , & Stears, M. (2020). The hidden inequalities of COVID‐19. Autism, 24(6), 1309–1310. 10.1177/1362361320927590 [DOI] [PubMed] [Google Scholar]
- Psychiatry, A. A. O. C. A. A . (2020). Coronavirus/COVID‐19 Resource. Retrieved from https://www.aacap.org/coronavirus
- Rutter, M. , Bailey, A. , & Lord, C. (2003). The Social Communication Questionnaire. Western Psychological Services. [Google Scholar]
- Schwartzman, J. M. , Millan, M. E. , Uljarevic, M. , & Gengoux, G. W. (2021). Resilience intervention for parents of children with autism: Findings from an RCT of the AMOR method. Journal of Autism and Developmental Disorders. 10.1007/s10803-021-04977-y. [DOI] [PubMed] [Google Scholar]
- Shepherd, D. , Landon, J. , Taylor, S. , & Goedeke, S. (2018). Coping and care‐related stress in parents of a child with autism spectrum disorder. Anxiety, Stress, and Coping, 31(3), 277–290. 10.1080/10615806.2018.1442614 [DOI] [PubMed] [Google Scholar]
- Shine, R. , & Perry, A. (2010). Brief report: The relationship between parental stress and intervention outcome of children with autism. Journal on Developmental Disabilities, 16(2), 64–66. [Google Scholar]
- Simon, D. M. , & Corbett, B. A. (2013). Examining associations between anxiety and cortisol in high functioning male children with autism. Journal of Neurodevelopmental Disorders, 5(1), 32. 10.1186/1866-1955-5-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff, E. , Pickles, A. , Charman, T. , Chandler, S. , Loucas, T. , & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population‐derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47(8), 921–929. 10.1097/CHI.0b013e318179964f [DOI] [PubMed] [Google Scholar]
- Spielberger, C. D. (1973). Manual for the state‐trait anxiety inventory for children. Consulting Psychologists Press. [Google Scholar]
- Spielberger, C. D. , Gorsuch, R. L. , Lushene, R. , Vagg, P. R. , & Jacobs, G. A. (1983). Manual for the state‐trait anxiety inventory. Consulting Psychologists Press. [Google Scholar]
- Spinelli, M. , Lionetti, F. , Setti, A. , & Fasolo, M. (2020). Parenting stress during the COVID‐19 outbreak: Socioeconomic and environmental risk factors and implications for children emotion regulation. Family Process. 10.1111/famp.12601 [DOI] [PubMed] [Google Scholar]
- Treutler, C. M. , & Epkins, C. C. (2003). Are discrepancies among child, mother, and father reports on children's behavior related to parents' psychological symptoms and aspects of parent‐child relationships? Journal of Abnormal Child Psychology, 31(1), 13–27. 10.1023/A:1021765114434 [DOI] [PubMed] [Google Scholar]
- van Steensel, F. J. , Bogels, S. M. , & Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta‐analysis. Clinical Child and Family Psychology Review, 14(3), 302–317. 10.1007/s10567-011-0097-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler, D. (2011). Wechsler abbreviated scale of intelligence II (2nd ed.). PsychCorp. [Google Scholar]
- White, L. C. , Law, J. K. , Daniels, A. M. , Toroney, J. , Vernoia, B. , Xiao, S. , … Chung, W. K. (2021). Brief report: Impact of COVID‐19 on individuals with ASD and their caregivers: A perspective from the SPARK cohort. Journal of Autism and Developmental Disorders. 10.1007/s10803-020-04816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, S. W. , Oswald, D. , Ollendick, T. , & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229. 10.1016/j.cpr.2009.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom, E. , Loeber, R. , & Stouthamer‐Loeber, M. (2000). Patterns and correlates of agreement between parent, teacher, and male adolescent ratings of externalizing and internalizing problems. Journal of Consulting and Clinical Psychology, 68(6), 1038–1050. 10.1037//0022-006x.68.6.1038 [DOI] [PubMed] [Google Scholar]
- Zoellner, T. , & Maercker, A. (2006). Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clinical Psychology Review, 26(5), 626–653. 10.1016/j.cpr.2006.01.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1 COVID‐19 concerns and stressors
TABLE S2. Sample Items from COVID‐19 Responses to Stress Questionnaire (based Connor‐Smith et al., 2000).
TABLE S3. Correlations among primary Adult outcome measures at T1
TABLE S4. Correlations among primary Child outcome measures at T1


